Abstract
Purpose:
There are disparities in mental health of refugee youth compared to the general US population. We conducted a pilot feasibility and acceptability trial of the home-visiting Family Strengthening Intervention for refugees (FSI-R) using a community-based participatory research approach. The FSI-R aims to promote youth mental health and family relationships. We hypothesized that FSI-R families would have better psychosocial outcomes and family functioning post-intervention compared to care-as-usual (CAU) families. We hypothesized that FSI-R would be feasible to implement and accepted by communities.
Methods:
40 Somali Bantu (n=102 children, 58.4% female; n=43 caregivers, 79.0% female) and 40 Bhutanese (n=53 children, 55.3% female; n=67 caregivers, 54.0% female) families were randomized to receive FSI-R or CAU. Refugee research assistants conducted psychosocial assessments pre- and post-intervention and home visitors delivered the preventive intervention. Multilevel modeling assessed effects of FSI-R. Feasibility was measured from retention and acceptability was measured from satisfaction surveys.
Results:
The retention rate of 82.5% indicates high feasibility and high reports of satisfaction (81.5%) indicate community acceptance. Across communities, FSI-R children reported reduced traumatic stress reactions and caregivers reported fewer child depression symptoms compared to CAU families (β=−0.42; p=0.03; β=−0.34; p=0.001). Bhutanese FSI-R children reported reduced family arguing (β=−1.32; p=0.035) and showed fewer depression symptoms and conduct problems by parent report (β= −9.20; p=0.038; β=−0.92; p=0.01) compared to CAU. There were no significant differences by group on other measures.
Conclusion:
A family-based home-visiting preventive intervention can be feasible and acceptable and has promise for promoting mental health and family functioning among refugees.
Keywords: Refugees, family functioning, youth mental health, prevention, intervention
Roughly 3.3 million refugees have resettled in the US since 1975 [1], half of them children [2]. Refugee youth have poorer mental health compared to the general population [3, 4]. In addition to experiencing trauma such as war-related violence, family loss, and displacement, refugee families encounter stressors after third-country resettlement [5, 6]. Post-resettlement stressors may be compounded by anti-refugee attitudes associated with growing nationalism in many countries [7], which can have a major impact on the mental health of refugees. Finally, both health-system and societal-level barriers contribute to poor access to and underutilization of mental health services [8].
There are few interventions that explicitly promote family functioning and mental health in refugee youth and families. Existing interventions focus overwhelmingly on trauma experiences [5], while an ecological model that also addresses daily stressors of resettlement might be more effective [9]. There is a need to develop flexible preventive interventions that can be done for refugees by refugees and adjusted to work with multiple groups, languages, and cultures at once, rather than highly specified models that can only be used with single cultural groups [10].
Somali Bantu and Bhutanese Refugees
Somali Bantu, most of whom were brought to Somalia as slaves in the 1800s, worked largely as subsistence farmers in the Jubba Valley. When the Somali government collapsed in the 1990s, many fled to Kenyan refugee camps. The US government identified Somali Bantus as a persecuted minority group and accepted approximately 10,000 refugees between 2004 and 2006 [11]. Bhutanese refugees are an ethnic-Nepalese population expelled from Bhutan starting in the 1980s [12]. Victims of cultural persecution, they fled to refugee camps in Nepal [12] where they remained until third-country resettlement began in 2008. Around 100,000 Bhutanese refugees have since resettled to the US [13]. . Bhutanese refugees have a high suicide rate across ages and genders, which the CDC found to be associated with mental health disorders and post-migration stressors [14].
There is limited information on the psychosocial functioning of youth in these refugee populations. Research indicates that Somali Bantu youth experience challenges in negotiating their complex identities as US citizens with African heritage, Somali minority status, and of Muslim faith [6]. Our qualitative work among Somali Bantu suggests that youth experience mental health difficulties aligning with Western constructs of depression (takoor), anxiety (welwel), anger (dherif), and conduct disorders (aasiwaalidin) [15]. To our knowledge there is limited to no information on the scope of challenges affecting Bhutanese refugee youth. Our qualitative research found that youth mental health challenges include depression (dookhit), anxiety (chinteet), and behavior problems (badmaas) [15]. Suicidal ideation and attempts among Bhutanese youth have been attributed to acculturation stress and pressure to support older family members [16].
Current Study
We used a community-based participatory research (CBPR) approach [17, 18] to adapt an evidence-based home-visiting intervention, the Family Based Preventive Intervention (FBPI), originally developed for preventing depression in children of depressed caregivers and listed in the National Registry of Effective Programs, into the Family Strengthening Intervention for Refugees (FSI-R) for Somali Bantu and Bhutanese refugees [15, 19, 20]. The FBPI has been used with diverse communities [21], but this is the first adaptation and implementation with refugee communities. Extensive qualitative work, including free list interviews, focus groups, and key informant interviews assessed the needs, strengths, and challenges of each community to adapt the intervention accordingly [15]. The FBPI conceptual model posits that poor communication and negative parent-child dynamics can lead to increased risk of mental health problems in offspring. Like the original FBPI, the FSI-R is strengths-based with core-components including a family narrative that draws out family challenges, strengths, and collective future hopes that can be achieved through improved communication. The narrative and strengths-focus of the FBPI were in alignment with views of resilience among refugee families [6, 16, 22].
Our goal was to assess the feasibility and acceptability of the FSI-R, done by refugees for refugees, in a pilot study using a randomized design with 40 families from each community in the Greater Boston and Springfield, MA areas. The Somali Bantu and Bhutanese communities were selected based on a history of mental health research with these two groups. Refugee community members were engaged at every phase of the pilot and worked as interventionists, research assistants (RAs), and community advisory board (CAB) members.
We hypothesized that the intervention would be feasible to implement using this CBPR approach and acceptable to families from the target communities. We also hypothesized that participation in the FSI-R would demonstrate patterns of improved caregiver-child relationships and improved parenting skills, parental self-efficacy, and monitoring. Lastly, we hypothesized improved child functioning and reduced internalizing and externalizing problems among school-aged refugee youth; however, our pilot would not be powered to detect small or medium changes.
METHODS
Participants and Settings
Inclusion criteria were: (1) having formal US government refugee status; (2) having at least one school-aged child (7–17 years), and (3) residing in the US for at least three months. Families were excluded if experiencing a severe crisis at time of enrollment (e.g., suicidality, divorce proceedings).
Ethical Considerations
Participants aged 18 and older provided oral consent, eligible children 17 and under provided oral assent, and primary caregivers provided oral consent. IRB approval was obtained from the Harvard T. H. Chan School of Public Health (Protocol #15860). Special consideration was given to ethical challenges encountered as a CBPR project that employs members of the community as staff. Regarding confidentiality-related risk, all RAs and interventionists completed required on-line ethics training, in addition to comprehensive staff-led trainings and ongoing supervision. Furthermore, all study participants were assigned anonymous identification numbers that were used throughout the study and for all communication.
Procedures
Staff was from the two communities and affiliated with community advocacy and social service agencies in the area. RAs drawn from the two communities and trained by the management staff, conducted outreach via phone calls, home visits, and events organized by the program manager and community leaders, and recruited all participants. RAs conducted blinded child and caregiver assessments via in-person interviews in three languages (Nepali, Maay Maay, and English) with Android tablets and the data collection software KoBo Collect [23]. All families were assessed pre- and post-FSI-R delivery.
Randomization to group, FSI-R vs. care-as-usual (CAU), occurred after pre-test assessment using a randomization sequence in Microsoft Excel. The CAU families did not receive FSI-R, but they could continue seeking agency support services; RAs were instructed to refer families to services as needed. All families assigned to CAU or FSI-R received the same stipend for participating in data collection: $50 at two time-points. Specific to the Somali Bantu families, there were three instances in which a male caregiver had more than one wife and children in separate households. After consultation with community advisors and careful consideration of the implications, we decided that both linked families could participate and be randomized to the same study arm. If assigned to receive FSI-R, the families could choose to receive it together or separately.
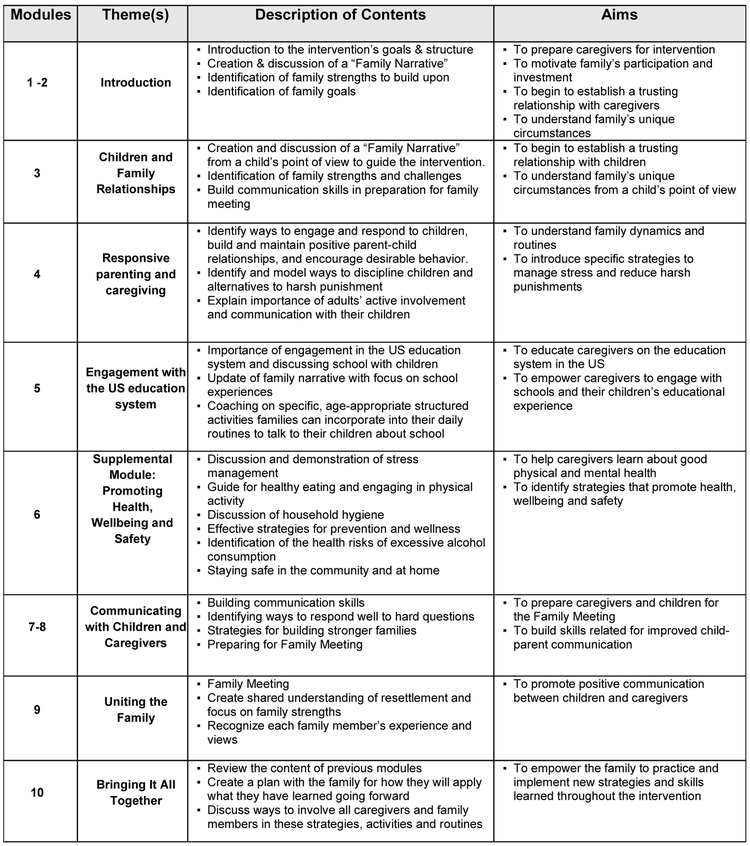
The FSI-R was delivered in approximately ten 90-minute weekly home-visiting sessions by well-trained interventionists from each community. FSI-R interventionists had prior experience in social services or case management, but no advanced mental health degrees. Each module covers topics such as improving communication, navigating the US education system, and learning positive parenting strategies (Figure 1). The family narrative component of the FSI-R allows families to choose important family events to discuss, while the interventionist highlights the family’s unique strengths and resiliency. Sessions could be added for families that needed additional support to master certain concepts [24].
Figure 1. FSI-R Intervention Modules.
Licensed clinical social workers provided weekly supervision to interventionists. A larger team including clinical supervisors and research staff provided twice-monthly group supervision. A child psychiatrist provided periodic consultation and a Master's-level program manager provided daily staff support. Families in both study conditions were offered referrals when appropriate for more intensive mental and physical health services (including substance abuse treatment) and case-management. CABs, composing of adults and adolescents, provided project oversight and guidance and included persons with diverse backgrounds (and for the Bhutanese, different caste representation).
Study measures
The research team selected assessments based on prior qualitative research that investigated terms for mental health problems and culturally-informed concepts of positive parenting in Somali Bantu and Bhutanese refugee communities [15]. All selected scales were previously used with immigrant or refugee populations (Supplementary Table 1). Cognitive testing, qualitative research, and consulting community advisors on comprehension and cultural appropriateness contributed to the modification of and removal and addition of certain items, yielding final adapted versions (Supplementary Table 1) [15]. Scales were forward- and-back translated into Maay Maay and Nepali using best practice guidelines [25].
Youth psychosocial functioning
Information on youth psychosocial functioning was collected from youth and caregivers. The 20-item Center for Epidemiologic Studies Depression Scale for Children (CES-DC) [26] assessed symptoms of depression and anxiety (child α=.85; caregiver α=.84). The CES-DC scale was adapted to include two additional items. Responses were on a Likert scale ranging from 0 (“Not at all”) to 3 (“A lot”) and summed for a total score. Suicidal ideation was measured using the CES-DC supplement [27]. Functional impairment was assessed using the WHO Disability Assessment Schedule for Children 2.0 (WHODAS-Child) [28] with two items added. The 14-item scale (child α=.82; caregiver α=.86) assessed six domains: understanding and communicating, mobility, self-care, getting along with people, life activities, and participation in society. Simple scoring was used in which scores of 0 (“no difficulty”) to 4 (“extreme difficulty/cannot do”) were summed. Trauma symptoms were assessed using an abbreviated 9-item University of California at Los Angeles PTSD Reaction Index by child reports [29]. Each item in the scale was scored as 0 (“No”) or 1 (“Yes”) and the scale score was the sum (α=.85). Child conduct problems were measured using the 32-item externalizing subscale of the Achenbach Youth Self Report (YSR) and Child Behavior Checklist (CBCL) assessments [30], with one item removed. Responses were on a Likert scale ranging from 0 (“Not True”) to 2 (“Very/Often True”) and summed (child α=.87; caregiver: α=.90).
Caregiver psychosocial functioning
Information was collected from caregiver self-report on caregiver psychosocial functioning. Trauma symptoms were assessed with the 17-item PTSD Symptom Scale Interview [31]. Each item in the scale was scored from 0 (“Not at all”) to 3 (“5 or more times per week/very much”) and summed (α=.93). Symptoms of anxiety and depression were assessed with the 25-item Hopkins Symptom Checklist (α=.94) [32]. Responses were on a four-point Likert scale from 1 (“Not at all) to 4 (“Extremely”), using the mean across the items as the scale score.
Family functioning
We used measures of family verbal/physical conflict and intergenerational congruence to assess family functioning from the perspective of youth and caregivers. Family conflict was measured with four items from the Family Conflict Scale [33]: “We got angry at each other;” “We argued;” “One of us got so mad, we hit the other person;” and, “I got my way by being angry.” Each item was assessed within the time frame of the past month and scored 0 (“Never”) to 6 (“More than 7 times”). Intergenerational congruence was measured with an adapted version of the Intergenerational Congruence in Immigrant Families Scale [34]. Eight items were added to the original scale to create a 17-item scale (child α=.92; caregiver α=.90). Responses were on a four-point Likert scale from 0 (“never”) to 4 (“every day”), using the mean across the items as the scale score.
We used an adapted version of the Alabama Parenting Questionnaire (APQ) [35] to assess caregiver parenting practices (6 items added, 2 items removed). Youth self-reported on three parenting domains: positive parenting, poor monitoring, and parental involvement. Positive parenting (α=.83) was 6 items, poor monitoring (α=.88) was 10 items, and parental involvement (α=.77) was 10 items. Responses were on a 5-point Likert scale from 1 (“Never”) to 5 (“Always”), and the score for each subscale was the sum of the items. A higher score for the parental involvement and positive parenting scales meant more healthy parenting practices for each domain, while a higher score on the poor monitoring practices meant less healthy practices.
Acceptability and Feasibility of the intervention
Participants in the FSI-R completed an 11-item survey assessing satisfaction with the intervention. Items were scored using two three-point Likert scales: 0 (“Dissatisfied”), 1 (“Neither Satisfied nor dissatisfied”), and 2 (“Satisfied”) (e.g., “Overall, how satisfied, if at all, are you with the FSI-R sessions you participated in?”); and 0 (“no”), 1 (“neutral”), and 2 (“yes”) (e.g., “Would you recommend the FSI-R to a friend or neighbor?”). Feasibility was assessed via the FSI-R family retention rate.
Statistical analysis
We used an intent-to-treat approach for data analysis. There was missing data due to loss-to-follow-up, where 18% (n=19) of caregivers and 19% (n=30) of children declined the post-test, and 7% (n=8) of caregivers and 4% (n=6) of children moved and could not be located for post-test. There were also challenges in tablet-based data collection. In one instance, a tablet malfunctioned and the pre-test data from 10 Bhutanese families (14 children, 18 caregivers) were lost. In other instances, errors occurred in uploading data, which led to the loss of post-test data for 6 Somali Bantu families (17 children, 6 caregivers). Due to these issues, two Bhutanese families (2 children, 3 caregivers) had neither pre-test nor post-test data and were excluded from final analyses.
We used a chained equations method in STATA 15 [36] to impute missing data [37] and generate 20 complete datasets for the 262 participants separately by community. This approach considers the relationship of missing data to other observed characteristics in the data set, thereby preserving power and reducing bias as compared to a complete case analysis, and accounting for the sampling variability across imputations [38]. We added a variable representing time in months from pre- to post-test for all families to account for two issues: the influence of numerous political events with an adverse effect on immigrant groups, and the differences in timing between pre- and post-test assessments between CAU and intervention families. Mixed (or multilevel) models were used to assess effects of FSI-R on caregiver and child mental health and family-level functioning, accounting for refugee community and time. We used a mixed effects model to estimate the intervention effect on change in scale scores for each community from pre- to post-test and ran a combined model to estimate the intervention effect across both communities.
Results
Baseline characteristics and outcome measures
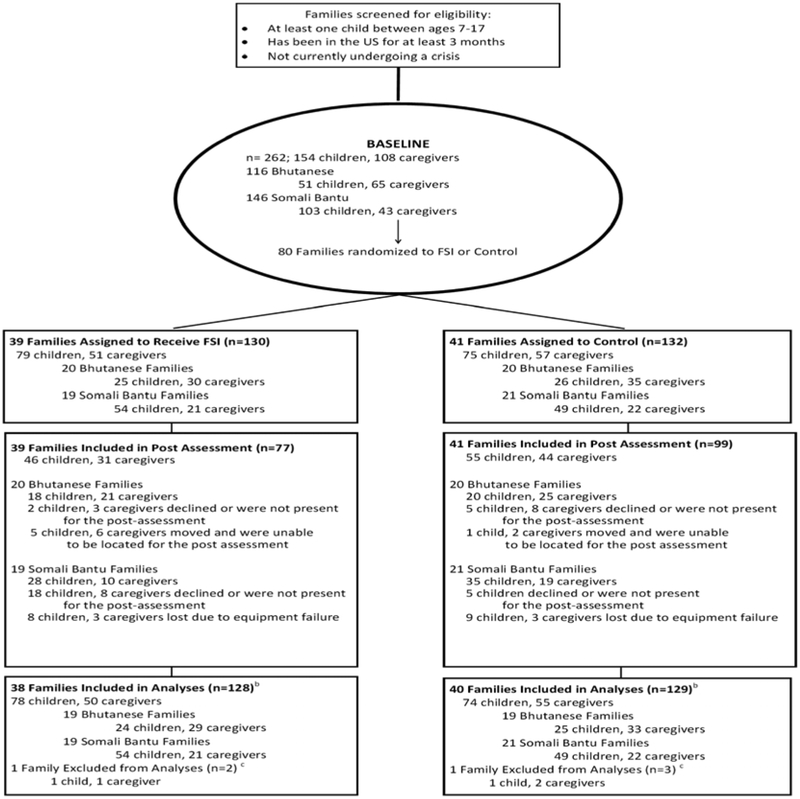
Thirty-nine families were randomized to the FSI-R. Of these, 11 families withdrew (Figure 2). Among the CAU families, 3 withdrew. Descriptive statistics are displayed in Table 1. Reporting caregivers were most frequently biological mothers for both Somali Bantu (79.00%) and Bhutanese (55.30%) families. Somali Bantu families had an average of 5.77 children compared to 2.08 children in Bhutanese families. Baseline scores on outcome measures are displayed in Table 2. In total, results were collected on 130 participants who received the intervention, and 132 participants receiving CAU (Figure 2).
Figure 2. CONSORT Flow Diagram.
a When children and caregivers moved away, the study team attempted to locate them for post-assessment
b Primary analyses included all randomized families with data for at least one time point, using 20 multiply imputed data sets to account for missingness.
c Two Bhutanese families (n= 5, 2 children, 3 caregivers) were excluded from analysis due absence of both baseline and follow up assessments. Baseline data were lost due to a technology malfunction. Post-test data were not collected because the family moved or declined to participate in the post-assessment.
Table 1.
Sociodemographic variables at baseline for child and caregiver by community
| Somali Bantu (n = 146) | Bhutanese (n =111) | |||
|---|---|---|---|---|
| Children | Caregivers | Children | Caregivers | |
| Individuals, n | 103 | 43 | 49 | 62 |
| Female, n (%) | 61 (59.2%) | 34 (79%) | 26 (53.1%) | 32 (52%) |
| Age, Mean (range) | 14.6 (8–22) | 41.77 (28–70) | 14.35 (8–18) | 40.97 (27–66) |
| Birthplace, n (%) | ||||
| Kenya | 56 (60%) | |||
| Somalia | 1 (1%) | 43 (100%) | ||
| Bhutan | 2 (5%) | 58 (98%) | ||
| Nepal | 42 (95%) | |||
| USA | 36 (39%) | |||
| India | 1 (2%) | |||
| Siblings, Mean (range) | 5.71 (0–8) | 1.98 (1–5) | ||
| Years in US, Mean (range) | 8 (8–15) | 13.29 (12–22) | 4.03 (1–8) | 4.32 (1–10) |
| US Citizen, n (%) | 91 (98%) | 36 (86%) | 5 (11%) | 11 (19%) |
| Currently Employed, n (%) | 26 (60%) | 46 (74%) | ||
Table 2.
Baseline child and caregiver outcomes by community
| Children | Somali Bantu (n= 103) |
Bhutanese (n=49) |
p |
|---|---|---|---|
| Poor Monitoring (APQ) | 21.87 (0.76) | 16.12 (1.11) | <0.001 |
| Positive Parenting (APQ) | 18.27 (0.53) | 22.11 (1.02) | <0.001 |
| Parental Involvement (APQ) | 28.88 (0.76) | 30.38 (1.51) | 0.35 |
| Intergenerational Congruence | 3.94 (0.06) | 3.68 (0.12) | 0.04 |
| We got angry at each other | 0.80 (0.14) | 0.66 (0.21) | 0.60 |
| We argued | 1.38 (0.17) | 0.57 (0.26) | 0.03 |
| One of us got so mad, we hit the other person | 0.65 (0.11) | 0.19 (0.17) | 0.03 |
| I got my way by being angry | 0.52 (0.11) | 0.40 (0.20) | 0.58 |
| Suicidal Ideation (CES-D) | 0.09 (0.06) | 0.49 (0.24) | 0.06 |
| Depression (CES-D) | 19.04 (0.87) | 10.59 (1.01) | <0.001 |
| Depression Caregiver Report on Child (CES-D) | 15.15 (0.91) | 12.54 (1.13) | 0.09 |
| Functional Impairment (WHODAS) | 18.75 (0.70) | 17.92 (1.19) | 0.56 |
| Functional Impairment Caregiver Report on Child (WHODAS) | 24.31 (0.54) | 22.95 (0.96) | 0.25 |
| Conduct Problems Caregiver Report on Child (YSR) | 67.09 (1.17) | 61.71 (2.16) | 0.05 |
| Conduct Problems (YSR) | 3.13 (.043) | 5.61 (0.76) | <0.001 |
| Caregivers | Somali Bantu (n=43) |
Bhutanese (n=62) |
|
| Intergenerational Congruence | 4.17 (0.09) | 3.43 (0.09) | <0.001 |
| We got angry at each other | 0.77 (0.21) | 0.64 (0.22) | 0.65 |
| We argued | 0.90 (0.21) | 0.46 (0.18) | 0.10 |
| One of us got so mad, we hit the other person | 0.25 (0.08) | 0.00 (0.00) | <0.001 |
| I got my way by being angry | 0.32 (0.15) | 0.04 (0.03) | 0.03 |
| Mental Health Problems (HSCL) | 4.25 (0.96) | 8.62 (2.25) | 0.12 |
| Trauma Symptoms | 0.92 (0.23) | 1.64 (0.75) | 0.37 |
Mixed Models
The estimated coefficients and standard errors of the mixed models for the primary outcomes of youth psychosocial functioning are presented in Table 3 separated by community. The β coefficients are point estimates that compare the trajectories, or changes in outcome scores from pre- to post-test, of the intervention individuals to the CAU individuals. The remaining findings on the secondary outcomes of caregiver psychosocial functioning and family functioning are presented in Supplementary Table 2.
Table 3.
Estimated coefficients and standard errors from mixed models for child and caregiver outcomes by community
| Somali Bantu (n=103) | Bhutanese (n=49) | |||||||
|---|---|---|---|---|---|---|---|---|
| β | SE | t | p | β | SE | t | p | |
| Depression (CES-DC) | ||||||||
| Child Report | 0.18 | 0.10 | 1.82 | 0.07 | −0.07 | 0.20 | −0.35 | 0.73 |
| Adult Report on Child | −0.06 | 0.12 | −0.49 | 0.62 | −9.20 | 4.42 | −2.08 | 0.04 |
| Functional Impairment (WHODAS) | ||||||||
| Child Report | −0.01 | 0.11 | −0.10 | 0.92 | 0.13 | 0.14 | 0.89 | 0.37 |
| Adult Report on Child | −0.02 | 0.11 | −0.14 | 0.89 | −0.15 | 0.16 | −0.95 | 0.34 |
| Conduct Problems | ||||||||
| Child Report (YSR) | 0.17 | 0.35 | 0.47 | 0.64 | −0.34 | 0.29 | −1.16 | 0.24 |
| Adult Report on Child (CBCL) | 1.48 | 0.32 | 4.57 | <0.001 | −0.92 | 0.33 | −2.82 | 0.01 |
Youth psychosocial functioning
Children who received the intervention, for both communities combined in the mixed model multiple regressions, reported significant improvements in mental health, indicated by lower levels of traumatic stress reactions (β=−0.42; p=0.03) compared to CAU children. Caregivers from families across both communities reported that children in the intervention also exhibited fewer depression symptoms (β=−0.34; p=<0.001) compared to CAU children. When analyzed separately by community, caregivers of Bhutanese intervention children reported significant improvements in child depression symptoms and child conduct symptoms compared to CAU Bhutanese children (β=−9.20.; p=0.04; β=−0.92; p=0.01). Somali Bantu CAU caregivers reported significant improvements in child conduct problems compared to intervention children. The remaining youth psychosocial outcomes for intervention children compared to CAU children were nonsignificant.
Caregiver and family psychosocial functioning
Intervention caregivers did not report significant improvements in mental health outcomes for themselves compared to CAU caregivers in either community. Caregiver psychosocial functioning outcomes are further detailed in Supplementary Table 2. Supplementary Table 2 also reports the findings on family functioning outcomes for child and caregiver reports. Bhutanese intervention children reported significant reductions in family arguing compared to Bhutanese CAU children (β=−1.32; p=0.04). Intervention caregivers and children did not report any additional significant improvements in caregiver-child relationship outcomes compared to CAU caregivers and children in either community. Intervention children also did not report significant improvements in healthy parenting outcomes compared to CAU children. The mixed results of family functioning outcomes are further explained in Supplementary Table 2.
Feasibility, acceptability and satisfaction
To better understand feasibility, we measured the intervention retention rate, which was 82.50%, accounting for the 14 families that withdrew. Among those who completed the FSI-R, at least one caregiver attended all six required caregiver modules and at least one child attended both required child modules. We also measured length of time between pre- and post-test, as well as between intervention completion and post-test. On average, the length of time between pre- and post-test was 12.91 months for intervention families, while it was 9.81 months for the CAU families. Although RAs were instructed to perform post-test data collection within a week after the family’s completion of the intervention, the approximate average length of time between the intervention and post-test assessments was 37.65 days (ranging from 5-114 days). Due to a small sample size, there were two families that distorted the mean due to personal situations (e.g. hospitalization; unable to reach).
We administered a closed-ended survey to at least one caregiver per household who participated in FSI-R to measure acceptability and satisfaction. Data were obtained for 27 out of 28 families. Among caregivers, 13 were Somali Bantu (10 females) and 14 were Bhutanese (6 females). All 27 (100%) reported satisfaction with information gained during the intervention, while 22 (81.50%) reported satisfaction with FSI-R participation in general. Thirteen Bhutanese (92.80%) and 10 (77%) Somali Bantu respondents reported satisfaction with the length of the sessions. Ten Somali Bantu (77%) and 14 Bhutanese (100%) participants reported satisfaction with the exercises during the sessions and 25 participants overall (92.60%) said they would recommend the FSI-R to a neighbor or friend.
Discussion
This pilot indicates that a family home-visiting intervention administered by refugees for refugees using a CBPR approach is feasible and acceptable. The retention rate of 82.50% is comparable to retention rates of other refugee interventions [39]. Although we experienced scheduling challenges, contributing to delays in timing of both FSI-R modules and post-test assessments, that was to be expected given the community-based, home-visiting nature of this work, paired with major competing life priorities of underserved communities. Flexibility with scheduling likely contributed to higher retention in the end. Furthermore, most were satisfied with the intervention and almost all would recommend it. The use of CABs, which allow community members to voice concerns and share their thoughts to the research team throughout the study, likely contributed to acceptance by the greater community, in addition to acceptance by participating families [40].
Although our main aim was to assess the feasibility and acceptability of the pilot, we also hypothesized that participation in the FSI-R would demonstrate patterns of improved relationships between caregivers and children, improved parenting skills, and improved child functioning and mental health compared to those in CAU. We did not see trends in improved parenting skills, yet the findings did indicate that participation in FSI-R has promising outcomes at the child level on mental health and functioning. The analyses also indicated a positive impact on certain family-level outcomes, such as improved caregiver-child relationships through decreased family conflict among the Bhutanese. Several outcomes examined did not improve significantly, yet with a small sample size of 40 families per community, we did not have the statistical power to detect small differences.
The feasibility, acceptability, and potential impact of the intervention are notable for several reasons. First, outcomes indicate that lay workers from refugee communities can be trained and supported via supervision to deliver mental health interventions to peers. Second, home-visiting was an effective approach at engaging all family members. The different module topics target diverse resettlement stressors, including navigating the US education system, learning new parenting practices, and improving communication, which are concepts many other refugee mental health interventions neglect [5]. Third, the intervention was implemented in two refugee communities with different cultures, challenges, and strengths [15] and was feasible and acceptable with both groups. Initial qualitative work was instrumental in the creation of a manual with core components addressing the overlapping and unique needs of each refugee group [15], yet cross-site training and discussion between groups allowed us to improve intervention delivery, and likely aided feasibility and acceptability.
Limitations
Several limitations must be noted. As previously stated, with only 40 families from each community, the trial was not powered to detect effectiveness so trends must be considered with caution. There was a lack of significant results overall for several of the outcomes examined and a few outcomes that were potentially concerning. However, after investigating these outcomes thoroughly, two families in each community had experienced unique incidents and crises during the course of the intervention and were outliers in change scores from pre- to post-test for several of the outcomes of interest, distorting the mean and biasing the findings (Supplementary Tables 3 and 4). A larger sample size could have mitigated such effects.
In addition, data were collected at only two time points, pre- and post-test. Consequently, we could not measure longer-term changes and sustainability of effects. Important policy and media events related to refugees unfolded during the study. In January 2017, a travel ban was announced on seven Muslim countries including Somalia. Later, in September 2018, the current administration announced capping the number of refugees resettled in the US at an all-time low of 30,000 and threatened that receiving public benefits would endanger the ability of refugees to apply for citizenship. These events may have had an effect on the psychosocial well-being of refugee families, as host country policies and hostile attitudes toward refugees can impact that population’s mental health [9]. For this study, we assumed that these effects would be cumulative and approximated by a linear time effect. In a larger sample, it might be useful to explore other ways to model this history effect, such as the influence of specific events and moderation related to community membership.
It is also possible that spillover of intervention content occurred between the intervention and CAU groups. The refugee communities involved in this pilot are close in geographic proximity. Given the emphasis on community support, it is possible that information and skills were shared between study groups. Lastly, although we found it feasible and acceptable to implement FSI-R with these two different populations, we cannot generalize findings to other refugee groups.
Conclusion and Future Direction
The CBPR process indicated that such research and intervention across multiple and diverse refugee communities is possible. Interventions can be advanced by cross-site learning and cross-fertilization despite language and cultural differences in order to be adapted and implemented with other refugee or immigrant populations in the future. The FSI-R is a promising intervention that can be delivered through a CBPR approach and may improve child mental health and family functioning among diverse refugee communities upon testing effectiveness in well-powered future trials.
Supplementary Material
IMPLICATIONS AND CONTRIBUTIONS:
This study used a community-based participatory research approach to engage communities in the delivery and testing of the Family Strengthening Intervention for Refugees. Results from this pilot trial indicate the intervention was feasible, acceptable, and has promise for promoting family functioning and mental health in refugee children and families.
Acknowledgments:
The authors would like to acknowledge the efforts of the whole research project team, the support of our partner agencies, and the generosity of the Somali Bantu and Bhutanese refugee communities in the Boston and Springfield, MA areas. This work was supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health [Grant number: R24MD008057].
Abbreviations:
- APQ
Alabama Parenting Questionnaire
- CAU
Care as Usual
- CBCL
Child Behavior Checklist
- CBPR
Community-Based Participatory Research
- CES-DC
Center for Epidemiologic Studies Depression Scale for Children
- FBPI
Family-Based Preventive Intervention
- FSI-R
Family Strengthening Intervention for Refugees
- WHODAS
World Health Organization Disability Assessment Schedule
- YSR
Youth Self-Report
Footnotes
Conflicts of Interest: All authors have declared that they have no competing or potential conflicts of interest in relation to this work.
REFERENCES
- [1].U.S. Department of State. Refugee admissions. Available at: https://www.state.gov/j/prm/ra/. Accessed February 10, 2019.
- [2].United Nations High Commissioner for Refugees. Global trends: forced displacement in 2016. Available at: https://www.unhcr.org/globaltrends2016/. Accessed February 1, 2019.
- [3].Reed RV, Fazel M, Jones L, Panter-Brick C, Stein A. Mental health of displaced and refugee children resettled in low-income and middle-income countries: risk and protective factors. Lancet 2012;379:250–265. doi: 10.1016/S0140-6736(11)60050-0. [DOI] [PubMed] [Google Scholar]
- [4].Bronstein I, Montgomery P. Psychological distress in refugee children: a systematic review. Clin Child Fam Psych 2011;14(1):44–56. doi: 10.1007/s10567-010-0081-0. [DOI] [PubMed] [Google Scholar]
- [5].Hynie M. The social determinants of refugee mental health in the post-migration context: a critical review. Can J Psychiatry 2018;63(5):297–303. doi: 10.1177/0706743717746666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Frounfelker RL, Assefa MT, Smith E, Hussein A, Betancourt TS. "We would never forget who we are": resettlement, cultural negotiation, and family relationships among Somali Bantu refugees. Eur Child Adolesc Psychiatry 2017;26(11):1387–1400. doi: 10.1007/s00787-017-0991-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Postelnicescu C. Europe's new identity: the refugee crisis and the rise of nationalism. Eur J Psychol 2016;12(2):203–209. doi: 10.5964/ejop.v12i2.1191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].de Anstiss H, Ziaian T, Procter N, Warland J, Baghurst P. Help-seeking for mental health problems in young refugees: a review of the literature with implications for policy, practice, and research. Transcult Psychiatry 2009;46(4):584–607. doi: 10.1177/1363461509351363. [DOI] [PubMed] [Google Scholar]
- [9].Silove D, Ventevogel P, Rees S. The contemporary refugee crisis: an overview of mental health challenges. World Psychiatry 2017; 16(2):130–139. doi: 10.1002/wps.20438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Murray KE, Davidson GR, Schweitzer RD. Review of refugee mental health interventions following resettlement: best practices and recommendations. Am J Orthopsychiatry 2010;80(4):576–585. doi: 10.1111/j.1939-0025.2010.01062.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Besteman C. Making refuge, Somali Bantu refugees and Lewiston, Maine. Durham, NC: Duke University Press, 2016. [Google Scholar]
- [12].Rizal D. The unknown refugee crisis: expulsion of the ethnic Lhotsampa from Bhutan. Asian Ethnicity 2004;5(2 ):151–177. doi: 10.1080/1463136042000221861. [DOI] [Google Scholar]
- [13].Embassy of the United States. US ambassador bids farewell to 90,000th refugee to resettle to the United States. Available at: https://np.usembassy.gov/u-s-ambassador-bids-farewell-90000th-refugee-resettle-united-states/. Accessed February 6, 2019.
- [14].Center for Disease Control. Suicide and suicidal ideation among Bhutanese refugees – United States, 2009-2012. MMWR 2013;62(26):533–536. [PMC free article] [PubMed] [Google Scholar]
- [15].Betancourt TS, Frounfelker R, Mishra T, Hussein A, Falzarano R. Addressing health disparities in the mental health of refugee children and adolescents through community-based participatory research: a study in 2 communities. Am J Public Health 2015;105(S3):S475–482. doi: 10.2105/AJPH.2014.302504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Brown FL, Mishra T, Frounfelker RL, et al. 'Hiding their troubles': a qualitative exploration of suicide in Bhutanese refugees in the USA. Glob Ment Health (Camb) 2019;6:e1. doi: 10.1017/gmh.2018.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Israel BA, Coombe CM, Cheezum RR, et al. Community-based participatory research: a capacity-building approach for policy advocacy aimed at eliminating health disparities. Am J Public Health 2010; 100(11):2094–2102. doi: 10.2105/AJPH.2009.170506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Minkler M. Linking science and policy through community-based participatory research to study and address health disparities. Am J Public Health 2010;1(S1):S81–87. doi: 10.2105/AJPH.2009.165720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Beardslee WR, Wright EJ, Gladstone TR, Forbes P. Long-term effects from a randomized trial of two public health preventive interventions for parental depression. J Fam Psychol 2007;21(4 ):703–713. doi: 10.1037/0893-3200.21.4.703. [DOI] [PubMed] [Google Scholar]
- [20].Betancourt TS, Ng LC, Kirk CM, et al. Family-based promotion of mental health in children affected by HIV: a pilot randomized controlled trial. J Child Psychol Psychiatry 2017;58(8):922–930. doi: 10.1111/jcpp.12729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Podorefsky D, McDonald-Dowdell M, Beardslee WR. Adaptation of preventive interventions for a low-income, culturally diverse community. J Am Acad Child Adolesc Psychiatry 2001;40(8):879–886. doi: 10.1097/00004583-200108000-00008. [DOI] [PubMed] [Google Scholar]
- [22].Betancourt TS, Newnham EA, Birman D, Lee R, Ellis BH, Layne CM. Comparing trauma exposure, mental health needs, and service utilization across clinical samples of refugee, immigrant, and U.S.-origin children. J Trauma Stress 2017;30(3):209–218. doi: 10.1002/jts.22186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].KoBoToolbox [computer program]. Cambridge, MA: KoBoToolbox; 2012. [Google Scholar]
- [24].Betancourt T, Frounfelker RL, Berent JM, Suarez-Orozco MM. Addressing mental health disparities in refugee children through family and community-based prevention In: Suarez-Orozco MM, ed. Humanitarianism and Mass Migration: Confronting the World Crisis. Oakland, CA: University of California Press, 2018:137–164. [Google Scholar]
- [25].World Health Organization. Process of translation and adaptation of instruments. Available at: http://www.who.int/substance_abuse/research_tools/translation/en/index.html. Accessed February 5, 2019.
- [26].Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- [27].Eaton WW, Smith C, Ybarra M, Muntaner C, Tien A. Center for Epidemiologic Studies depression scale: review and revision (CESD and CESD-R). In: Maruish ME, ed. The use of psychological testing for treatment planning and outcomes assessment: Instruments for adults. Mahwah, NJ: Lawrence Erlbaum Associates Publishers, 2004:363–377. [Google Scholar]
- [28].World Health Organization. WHO disability assessment schedule 2.0 WHODAS 2.0. Available at: http://www.who.int/classifications/icf/whodasii/en/index4.html. Accessed February 2, 2019.
- [29].Pynoos RS, Rodriguez N, Steinberg AS, et al. The UCLA PTSD reaction index for DSM IV (Revision 1). Los Angeles, CA: UCLA Trauma Psychiatry Program, 1998. [Google Scholar]
- [30].Achenbach TM. Manual for the youth self-report and 1991 profile. Burlington, VT: Department of Psychiatry, University of Vermont, 1991. [Google Scholar]
- [31].Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J Trauma Stress 1993;6(4):459–473. doi: 10.1002/jts.2490060405. [DOI] [Google Scholar]
- [32].Derogatis LR, Lipman R, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behav Sci 1974; 19(1): 1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- [33].Fosco GM, Van Ryzin MJ, Connell AM, Stormshak EA. Preventing adolescent depression with the family check-up: Examining family conflict as a mechanism of change. J Fam Psychol 2016;30(1):82–92. doi: 10.1037/fam0000147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Ying Y-W, Lee PA, Tsai JL. Psychometric properties of the intergenerational congruence in immigrant families: child scale in Chinese Americans. J Comp Fam Stud 2004;35(1):91–103. doi: 10.1093/swr/28.1.56. [DOI] [Google Scholar]
- [35].Essau CA, Sasagawa S, Frick PJ. Psychometric properties of the Alabama Parenting Questionnaire. J Child Fam Stud 2006;15(5):595–614. doi: 10.1007/s10826-006-9036-y. [DOI] [Google Scholar]
- [36].StataCorp [computer program]. Stata Statistical Software: Release 15. College Station, TX: StataCorp; 2017. [Google Scholar]
- [37].Plumpton CO, Morris T, Hughes DA, White IR. Multiple imputation of multiple multi-item scales when a full imputation model is infeasible. BMC Res Notes 2016;9:45. doi: 10.1186/s13104-016-1853-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Rubin DB. Multiple imputation for nonresponse in surveys. New York, NY: Wiley & Sons, 1987. [Google Scholar]
- [39].Pfeiffer E, Sachser C, Rohlmann F, Goldbeck L. Effectiveness of a trauma-focused group intervention for young refugees: a randomized controlled trial. J Child Psychol Psychiatry 2018;59(11):1171–1179. doi: 10.1111/jcpp.12908. [DOI] [PubMed] [Google Scholar]
- [40].Newman SD, Andrews JO, Magwood GS, Jenkins C, Cox MJ, Williamson DC. Community advisory boards in community-based participatory research: a synthesis of best processes. Prev Chronic Dis 2011;8(3):A70. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.