Abstract
Purpose
To characterize perceived social support for young men and transgender women who have sex with men (YM/TWSM) taking HIV pre-exposure prophylaxis (PrEP).
Methods
Mixed-methods study of HIV-negative YM/TWSM of color prescribed oral PrEP. Participants completed egocentric network inventories characterizing their social support networks and identifying PrEP adherence-support figures. A subset (n=31) completed semi-structured interviews exploring adherence support and qualities of PrEP support figures. We calculated proportions of role types (e.g. family), individuals disclosed to regarding PrEP use, and PrEP-supportive individuals within each participant network. Interviews were analyzed using an inductive approach.
Results
Participants (n=50) were predominately African-American men who have sex with men (MSM). Median age was 22 years (Interquartile range [IQR]: 20–23). Biologic family were the most common support figures, reported by 75% of participants (mean family proportion 0.37 [Standard deviation (SD): 0.31]), followed by 67% reporting friends (mean friend proportion 0.38 [SD: 0.36]). The majority of network members were aware (mean disclosed proportion 0.74 [SD: 0.31]), and supportive (mean supportive proportion 0.87 [SD: 0.28]) of the participants’ PrEP use. Nearly all (98%) participants identified ≥1 figure who provided adherence support; more often friends (48%) than family (36%). Participants characterized support as instrumental (e.g. transportation); emotional, (e.g. affection); and social interaction (e.g. taking medication together). Key characteristics of PrEP support figures included closeness, dependability, and homophily (alikeness) with respect to sexual orientation.
Conclusions
While most YM/TWSM identified family in their support networks, friends were most often cited as PrEP adherence-support figures. Interventions to increase PrEP adherence should consider integrated social network and family-based approaches.
Implications and Contributions
This mixed-methods study of young men and transgender women of color using PrEP identified diversity in support network composition, with family members occurring most commonly but friends most often providing adherence support. Clinicians and researchers should be cognizant of support structures in the design and delivery of PrEP adherence interventions.
INTRODUCTION
The structure and characteristics of social networks play important roles in the HIV epidemic among young men and transgender women of color who have sex with men (YM/TWSM).1,2 Despite lower rates of condomless sex and partner concurrency, youth of color acquire HIV at a rate three-times higher than their white peers.3 This inequity in transmission is partly driven by social and sexual network structures among YM/TWSM of color, which are characterized by high degrees of both interconnectedness (density),1,2 and alikeness (homophily) on characteristics such as race and substance use. As a result, health disparities, such as HIV infection, are easily potentiated among network members.1,2
However, these same network characteristics serve as effective targets for HIV prevention.4,5 Interventions using peer change agents and popular opinion leaders utilize key network members to introduce change throughout networks and have shown success in HIV prevention outcomes.6 As the HIV prevention landscape has shifted to include biomedical options such as pre-exposure prophylaxis (PrEP), network interventions are a promising strategy to improve PrEP uptake and adherence. Since licensure in 2012, PrEP has emerged at the forefront of HIV prevention efforts, with >90% efficacy in preventing HIV acquisition in highly adherent users.7,8
PrEP uptake among YM/TWSM is a public health priority, yet studies demonstrate that uptake in the absence of adherence will not move the needle sufficiently to reduce population HIV incidence. Unfortunately, studies demonstrate that African-American and Latinx YM/TWSM have lower PrEP adherence rates.9–12 Adherence challenges among YM/TWSM have been linked to structural (e.g., homelessness, intersectional stigma), behavioral (e.g., depression, substance abuse), and, importantly, network characteristics.13–15 However, data demonstrate associations between network factors such as size and increased PrEP uptake.5 Modeling studies also indicate that increases in uptake and adherence within dense networks will result in the desired reduction of HIV.16 Network social support may counteract the aforementioned adherence barriers by decreasing the negative appraisal of stressful life events, reinforcing normative adherence behavior, buffering against stigma, and ameliorating structural barriers.17 At present, however, network studies of PrEP uptake and adherence in YM/TWSM are limited.
To develop network-based PrEP adherence interventions, it is essential to understand the structure, composition, and function of social support networks for YM/TWSM receiving PrEP. While there has been a strong emphasis on engaging biologic families in HIV prevention interventions for heterosexual youth,18,19 little is known about biologic families’ role in support networks vis-a-vis PrEP adherence for YM/TWSM. In the presence of stigma related to sexuality and gender identity, YM/TWSM may separate from their biologic families and, in their place, create de novo elective kinship families who provide emotional, social, and structural support.19–21 Examining who YM/TWSM turn to for PrEP support may allow for interventions focused on strengthening endogenous support within networks. Thus, the primary goal of our research was to characterize the structure, composition, and function of social support networks among YM/TWSM using PrEP. Secondarily, we aimed to identify characteristics of PrEP-specific support figures within these networks.
METHODS
Study Design, Participants, and Setting
The PrEP Together mixed-methods cohort study explored relationships between social support, network structure, and adherence to daily oral, tenofovir-emtricitabine (TDF-FTC)-based PrEP among YM/TWSM. Eligible participants were aged 15–24 years; African-American, Latinx, and/or a person of color with HIV-negative status by self-report; assigned male sex at birth; reporting sex with cisgender men and/or transgender women; and prescribed TDF-FTC-based PrEP for ≥three months (verified by clinical and pharmacy records). Participants understood written and spoken English. The primary recruitment site was the Youth Health Empowerment Project, a community-based federally-qualified health center in Philadelphia. Participants were also recruited from area clinical sites, social media, venues, and mobile dating applications. We excluded one participant who did not complete any social network measures. Approval was received from the Institutional Review Boards of the Children’s Hospital of Philadelphia, Philadelphia FIGHT Community Health Centers, and the City of Philadelphia Department of Public Health. The present analysis consists of qualitative interview and quantitative data from the baseline study visit.
Procedures
All participants provided informed consent prior to completing computer-assisted survey instruments (CASIs). A subsample of participants completed a semi-structured interview further characterizing how and from whom they received PrEP adherence support. Participants received $25 for the study visit and an additional $10 if they completed an interview.
Measures
Race, age, gender, housing, education status, and time on PrEP were obtained via CASI. Social support was measured by the Medical Outcomes Study Social Support Survey (MOSS-S), a 19-item questionnaire measuring four domains (emotional/informational, tangible, affectionate, and positive social interaction). Stigma was measured by a modified version of the Every Day Discrimination Scale.22,23 Participants experiencing stigma selected reasons for discrimination including race, age, appearance, gender, sexual orientation, and PrEP use.
Network Inventory
Participants self-completed a network inventory on a secure tablet to create an egocentric sociogram characterizing individuals in their support networks and relationships among them. Network members (alters) were elicited by a name generator prompt asking them to list up to five people “who you can share important information with and you would expect to give you emotional support in a time of need.” The limit of five was chosen per prior research demonstrating this number is sufficient to enumerate support figures.24 We defined network size as the total number of listed alters for each participant. For each alter, questions assessed their race, age, gender, sexual orientation, perceived HIV status, and role in the participant’s life (friend, biologic family, chosen/gay family, sexual or romantic partner, other). Participants were allowed to choose >1 role category. Closeness was measured as the participant’s perceived emotional closeness to each alter on a Likert scale. Participants noted whether they had disclosed their PrEP use and sexual orientation to each alter, and perceived supportiveness of the participant’s PrEP use was assessed by the question: “Now let’s imagine all your support people know you are on PrEP. How supportive are they or would they be of your PrEP use?” To identify PrEP-adherence support figures within the networks, participants were asked: “Out of all your support people, which could you most depend upon for supporting you in taking your PrEP?”
Semi-structured Interviews
At consent, participants had the option of completing an audio-recorded, semi-structured, individual interview, with a target interview sample size of n=30 for saturation of content themes.25,26 The script was developed in an iterative process with review by PrEP content experts, and piloted in a sample of n=5 YM/TWSM prior to study use. The sociogram portion of the interview elucidated how network alters provided PrEP adherence support, and the rationale for choosing the PrEP-specific support figures in the network.
Data Analysis
We calculated the proportion of each role type within the network as the number of alters characterized by each role (numerator) divided by the total number of alters (denominator).27 This approach was repeated to determine proportions of alters characterized as very/extremely close to the participant (close ties), PrEP-disclosed alters, and PrEP-supportive alters. These proportions, as continuous numbers, were compared between the general support figures and PrEP-support figures using t-testing. Density, a measure of how socially related the various alters within the networks are to one another, was calculated as the number of actual connections divided by the number of potential connections between network alters.28 Homophily by age, sexual orientation, and PrEP use was calculated by Newman’s assortativity coefficient,29 a measure of correlation between network members by selected characteristics. The coefficient, which characterizes the overlap between network members on selected characteristics, ranges from −1 to 1, with 1 representing complete assortative mixing, 0 random mixing, and −1 complete disassortative mixing. We used bootstrapped node label permutations to test the null hypothesis that these coefficients were equal to zero30 using R statistical software.31
Interview recordings were transcribed, reviewed for accuracy, and imported into Nvivo (QSR International Pty Ltd. Version 10, 2012). We used an inductive, open-coding approach to identify emerging content themes regarding the mechanisms of social support and characteristics of support network members. We developed codes by independently reading each of the first ten transcripts line-by-line and reaching consensus on codes that we then applied to all transcripts with iterative revision as needed. All transcripts were double-coded until each of three two-person coding teams reached satisfactory inter-rater reliability (kappa statistic>0.9) across ten transcripts. We resolved coding discrepancies by consensus. The overall weighted kappa and inter-rater agreement for the interviews was 0.9 (98.3% agreement). Exemplar quotes are anonymized and accompanied by randomly-generated initials.
In exploratory analyses, we sought to determine how participants who did and did not identify a family member as a PrEP adherence support figure differed based on the presence of key characteristics derived from the qualitative data within their support network. We defined closeness as the close ties proportion, dependability as the MOSS-S total and subscale scores and duration of relationship with network alters, and homophily as the Newman’s assortivity coefficient for sexual orientation within the network. We used t-tests to assess for statistical significance of observed differences between those with and without family members as PrEP adherence support figures.
RESULTS
Participant Characteristics
Participants (n=50) were predominantly African-American YM/TWSM with a median age of 22 years. The demographic characteristics of participants are displayed in Table 1, n=31 (62%) completed interviews. Over half of participants reported race-based and sexual orientation-based stigma within the last year.
Table 1:
Characteristics of Study Participants
| Characteristic | Full Sample n=50 | Interview Sub Sample n=31 |
|---|---|---|
| Median (IQR)/Number (%) | ||
| Age | 22 years (20–23) | 22 years (20–23) |
| Gender | ||
| Male | 45 (90%) | 28 (90%) |
| Transgender Female | 5 (10%) | 3 (10%) |
| Race/Ethnicity1 | ||
| White | 4 (8%) | 2 (6%) |
| African American | 34 (68%) | 21 (68%) |
| Latinx | 6 (12%) | 2 (6%) |
| Asian | 2 (4%) | 2 (6%) |
| American Indian | 1 (2%) | 0 (0%) |
| Mixed Race | 12 (24%) | 8 (26%) |
| Person of color | 5 (10%) | 5 (16%) |
| Education | ||
| Some high school | 9 (18%) | 4 (13%) |
| Graduated high school or GED2 | 19 (38%) | 13 (42%) |
| Some college | 14 (28%) | 9 (29%) |
| College graduate | 8 (16%) | 5 (16%) |
| Site of recruitment | ||
| YHEP Clinic3 | 35 (70%) | 22 (71%) |
| Geosocial mobile applications | 5 (10%) | 5 (16%) |
| Other community and clinical venues | 10 (20%) | 4 (13%) |
| Unstable housing in past year | 18 (36%) | 13 (42%) |
| Time on PrEP (months) | 10 (6–24) | 10 (6–24) |
| MOSS-S4 Score | 77.6 (63.2–94.7) | 78.9 (71.1–97.4) |
| Experienced Stigma (more than a few times in past year)1 | ||
| Race-based | 29 (58%) | 17 (55%) |
| Sexual orientation-based | 27 (54%) | 19 (61%) |
| Gender-based | 14 (28%) | 7 (23%) |
| Age-based | 12 (24%) | 7 (23%) |
| PrEP5– based | 1 (2%) | 1 (3%) |
Percentages sum to >100% because categories were not mutually exclusive.
General Education Development test
Youth Health Empowerment Project
Medical Outcomes Social Support Survey
PrEP: HIV pre-exposure prophylaxis
Structure of Social Support Networks
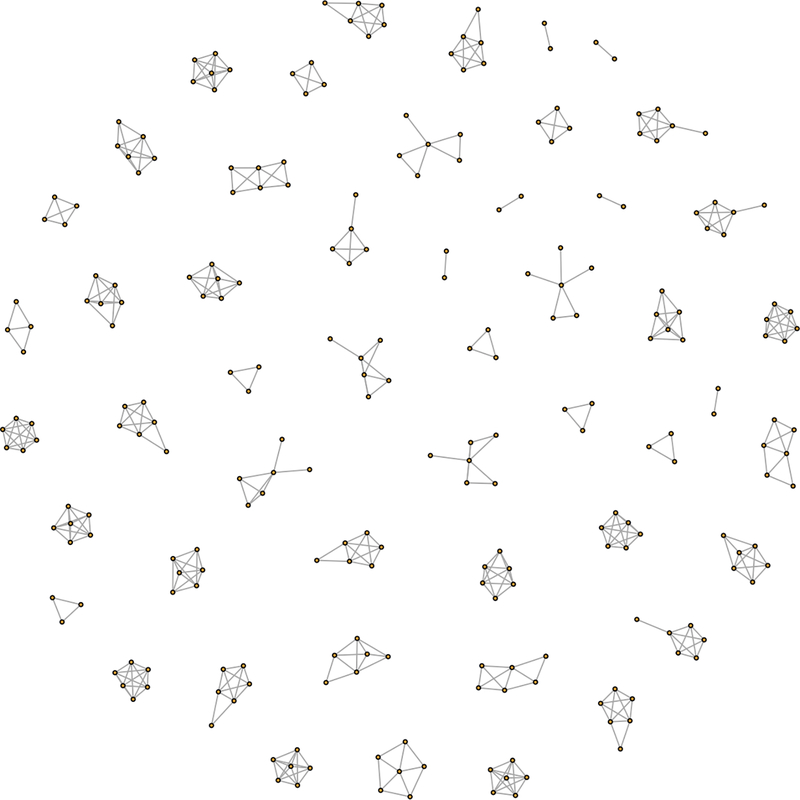
Characteristics of the social support networks are displayed in Table 2. The median network size was 5 (Interquartile range [IQR]: 3–5), with a median density of 0.85 (IQR: 0.7–1), reflecting a high degree of inter-connectedness among network members (Figure 1). Biologic family members were the most commonly reported support figures in the networks, with 75% of participants identifying ≥1 family member in their network, most often their mother. Friends were identified in 67% of networks. Most individuals had disclosed PrEP use to a substantial proportion of their network, and alters were perceived to be highly supportive of the participant’s PrEP use. With respect to homophily, the assortativity coefficient by sexual orientation was 0.11 (p=0.02), demonstrating a small but significant degree of assortative mixing. The assortativity coefficients for age (−0.03, p=0.53) and PrEP use (−0.06, p=0.14) indicated random mixing by these characteristics.
Table 2:
Network proportions of General Support and PrEP Support Alters
| Network Characteristic | Mean (SD) Proportion among General Support Alters n=49 | Mean (SD) Proportion among PrEP Support Alters n=49 | p-Value |
|---|---|---|---|
| Biologic family | 0.37 (0.31) | 0.27 (0.40) | 0.01 |
| Friends | 0.39 (0.36) | 0.37 (0.43) | 0.58 |
| Chosen/gay family | 0.22 (0.32) | 0.23 (0.40) | 0.37 |
| Sexual partners | 0.07 (0.17) | 0.15 (0.32) | 0.01 |
| Romantic partners | 0.08 (0.13) | 0.18 (0.33) | 0.01 |
| Close ties | 0.90 (0.20) | 0.87 (0.32) | 0.43 |
| Known longer than 2 years | 0.72 (0.35) | 0.68 (0.42) | 0.28 |
Figure 1: Ego Network Sociograms.
Each cluster represents an individual participant’s social network. Each circle represents an individual in the network. Each line represents a relationship between individuals in the networks.
Function of Social Support Networks
In the qualitative interviews, the predominant thematic categories of PrEP adherence support were 1) instrumental, 2) emotional, and 3) positive social interaction.
Instrumental support was characterized as tangible assistance with adherence including rides to clinic and help navigating insurance. For one participant, this included assistance with pharmacy refills from their partner:
“Like he always reminds me or he always asks me or stuff like that. Like he picks up my medicine or I will pick up his medicine.” (HJ)
Emotional support included encouragements to be healthy and reminders for medication-taking. One participant discussed emotional support from their partner as:
“…Just general positive reinforcement. Taking interest in my health, my personal life. Making sure I make good decisions.” (IX)
Most participants characterized emotional support emerging in the form of “tough love” or a verbal “thrashing” if their adherence slipped. Participants characterized this support more as enforcement than nurturance; however, it was perceived as positive emotional support. One participant talked about friends living with HIV fulfilling this role:
“I have a few friends who are HIV positive. So they’re basically the mediators like oh, well, maybe if they was told more about PrEP, they wouldn’t be in this position. They basically enforce it sometimes, too. Literally, enforces it like did you take your PrEP yet or no, go take your PrEP. I just be like all right.” (KL)
Positive social interaction emerged as collective engagement in activities that promoted adherence, such as taking medication together. For some participants, this included taking PrEP with support figures on antiretroviral therapy for HIV.
“My best friend and my gay brother, they’re both positive. So we talk first thing in the morning. As soon as we wake up, somebody’s calling somebody. So it’s just like, did you all take you all medicine? Did you take yours? So it’s just like open conversation.” (AQ)
Characteristics of PrEP Support Figures
Nearly all (98%) participants could identify ≥1 alter whom they would turn to for PrEP adherence support (Table 2). These individuals were more often friends than biologic family. In the qualitative data, the predominant characteristics of the individuals chosen for PrEP adherence support included emotional closeness, dependability, and sexual orientation-based homophily.
Closeness
Participants discussed the concept of closeness as an emotional bond to the support person. For some participants, this drew them toward biologic family members, who had been the longest standing support figures in their lives:
“I was always around my mom. It’s not nothing that my mom don’t know about me that I don’t know about her. So I picked her.” (IZ)
One participant discussed choosing their PrEP adherence counselor based not only on her professional knowledge, but on a sense that they could turn to her for emotional matters beyond PrEP use:
“Because she’s the one who knows about the whole process. She’s the one who was there that I could really talk to about my breakup and all the craziness that was going on. And, I just feel like anything that comes up, I can let her know, and she’ll be able to assist me.” (XG)
Dependability
This theme was characterized as having past demonstrations of being consistently available and having provided support across multiple life domains, as one participant described in choosing a friend:
“She’s just – she’s very dependable. I can’t think of a time where I asked her for help or a phone call – if I called her right now, even though I know she’s at work…I know if I called her right now she would answer the phone. And if she didn’t answer her cell phone, I would call her work phone and she’ll stop whatever she’s doing and she’ll answer it.” (IL)
Homophily
Participants discussed the importance of having a PrEP support figure who shared their experience as a sexual or gender minority individual. Participants described this commonality as engendering a sense of trust and understanding:
“The trust, like I said, he understands me. I feel better considering the fact that he’s a bisexual man himself. And the experience that he has lived through, the moral support that’s there.” (AY)
While more than half of participants (58%) chose a single individual as their PrEP support figure, others chose multiple alters, focusing on the collaborative nature of support. One participant discussed choosing their entire support network, consisting of biologic family, gay family, and their partner:
“It’s a group collective, family bond kind of thing. It was just … everybody just seems to make sure I’m good.” (AQ)
Finally, participants discussed non-disclosure of PrEP use as a potential barrier to receiving adherence support. Disclosure was often not face-to-face (e.g. posting PrEP status on mobile dating applications) or accidental (e.g. family members finding their medication). Participants less commonly disclosed PrEP use in direct conversations about sex and intimacy or as a means of obtaining support from network members. Disclosure as a barrier emerged most often when participants discussed not choosing biologic family members as PrEP support figures. One participant discussed not disclosing PrEP use to their mother:
“…I guess I’m afraid of kind of worrying her or something. She doesn’t know that I’m in a relationship now and have sex with other people than my boyfriend, who she knows. I just wouldn’t wanna talk about that with my mom or my other family members. And so PrEP feels like it’s sort of a part of that… I wish I could talk to my family more about it I guess.” (YI)
In the exploratory analysis comparing network characteristics with having a family member identified as a PrEP support figure versus not (Table 3), individuals identifying their family members as sources of adherence support had a greater proportion of close ties; higher overall, emotional, and affectionate social support; and longer duration of relationships with their alters. There was no difference in sexual orientation-based homophily between groups, suggesting that participants with a higher proportion of YM/TWSM in their networks were no less likely to turn to family for PrEP support.
Table 3:
Bivariate analysis of associations between identification of family as PrEP support figures based on key characteristics
| Measure of Characteristic | Family chosen as PrEP1 Support Figure Mean (SD)2 n=18 | Family not chosen as PrEP Support Figure Mean (SD) n=32 | p-Value |
|---|---|---|---|
| Closeness | |||
| Network close ties proportion | 0.98 (0.06) | 0.84 (0.26) | 0.03 |
| Dependability | |||
| Participant MOSS-S3 Score | 83.26 (20.74) | 72.62 (16.84) | 0.05 |
| Emotional Support Index | 84.20 (23.83) | 72.17 (17.59) | 0.05 |
| Tangible Support Scale | 78.13 (30.26) | 68.94 (24.97) | 0.25 |
| Affectionate Support Scale | 89.35 (19.76) | 77.08 (20.74) | 0.05 |
| Positive Social Interaction scale | 87.5 (23.09) | 79.95 (17.69) | 0.20 |
| Proportion of ties known >2 years | 0.85 (0.24) | 0.65 (0.38) | 0.04 |
| Homophily | |||
| Proportion of sexual and gender minority figures in network | 0.72 (0.46) | 0.90 (0.30) | 0.09 |
PrEP: HIV pre-exposure prophylaxis
Standard deviation
Medical Outcomes Social Support Survey
DISCUSSION
In developing PrEP adherence interventions for YM/TWSM, there is a natural tension between interventions relying on exogenous figures such as counselors or navigators, and “intraventions” wherein individuals influence behavior change from within a network.27,32 For our participants, the most prominent features of their PrEP support figures were emotional closeness, dependability, and sexual orientation-based homophily. While models using navigators to promote PrEP adherence show promise, the qualities identified by our participants may be difficult to replicate using exogenous interventionists. Our data suggests that strengthening the capacity of endogenous network members to provide adherence support is a strategy to explore.
We identified a high proportion of biologic family members in support networks of YM/TWSM on PrEP. While there are a wealth of HIV prevention interventions demonstrating associations between family involvement and reduced adolescent sexual risk behavior,33,34 these interventions have been conducted almost exclusively in heterosexual youth. Our data found that 75% of YM/TWSM identified a biologic family member in their support network, paralleling the few other studies examining support network structure in YM/TWSM. In the p18 cohort, Kapadia et al found that 90% of participants reported family in their support networks.35 Family presence in egocentric support networks has been associated with decreased sexual risk behavior in African-American men who have sex with men (MSM), 27 and family awareness of PrEP use has been associated with higher adherence.36 In our study, participants who turned to family for PrEP adherence support had higher measured social support, suggesting that family members may be a rich source of support across other life domains. The absence of family-based PrEP uptake and adherence interventions that are culturally tailored for sexual and gender minority youth of color, a population at highest risk for HIV in the United States, is a potential missed opportunity for HIV prevention.
For youth, the impact of family context is perhaps more salient for PrEP than condom use, which requires minimal healthcare utilization. Particularly in light of the recent FDA licensure of PrEP for minor adolescents, researchers and health systems should consider that adolescents and young adults may initiate PrEP while living with their families, using their parent’s insurance, and/or accessing sexual healthcare within pediatric clinics.37,38 In this sociobehavioral context, the support of family caregivers will likely be essential for successful PrEP uptake, adherence, and persistence.
We found that family members represented a smaller proportion of PrEP supportive network members compared to overall support network members. Our interview data suggest this discordance may be due to PrEP non-disclosure, driven by concerns about privacy, judgment, and adding stress to vulnerable family systems.20 Sexual and gender minority youth, fearing stigma and homophobia from family members, may instead turn to peers as alternative support sources.39 Future research is needed to determine how different sources and forms of social support affect dynamic PrEP adherence for YM/TWSM, and how both peer-based and family-based interventions may be utilized to support sustained adherence.
Our study has limitations and strengths. We used egocentric rather than sociometric data, which limited our ability to assess network characteristics such as centrality. However, our aim was to describe our participants’ perceived support and network characteristics, for which egocentric methods are sufficient. We did not assess mode of communication among network members, which should be investigated in future studies to identify optimal means for intervention delivery. Our sample size resulted in our being underpowered for comparisons between groups of participants. This resulted from challenges in recruiting YM/TWSM of color who had already initiated PrEP. National data9,12 demonstrate that PrEP uptake in these populations is well below target goals, and the low utilization of PrEP is reflected in our sample size. Although we felt it critical to include young transgender women (YTW) in the study given the underrepresentation of YTW in PrEP research,40 we are unable to draw inferences about differences between these transwomen and cisgender MSM given our small sample size. Most participants came from an urban PrEP clinic. The social support networks of rural youth may differ significantly, and warrant attention given the need for PrEP supportive interventions in rural HIV hotspots such as the Deep South. For this analysis, we did not compare adherence outcomes by network characteristics or social support. This decision was by design as our aim was to identify and describe endogenous support figures who may be engaged in future interventions, rather than ascribing efficacy to relationships in which the support figures had not been primed for delivery of adherence support. Finally, our data are cross-sectional and do not account for the dynamic nature of networks, which may shift over time.
In conclusion, we identified novel findings regarding the structure and function of support networks for youth on PrEP, which identify domains to be targeted in future interventions. In particular, future research should focus on the dynamic effect of family support on PrEP adherence, to determine whether family-based interventions to support PrEP adherence are an effective strategy within the developmental and social milieu of adolescence and young adulthood.
Acknowledgements
Funding Sources: NIMH F32 MH111341 (Wood); P30 AI 045008, Center for AIDS Research Pilot Award (Wood); Penn Mental Health AIDS Research Center Pilot Award P30 MH 097488 (Wood); CHOP Research Institute Pilot Award (Wood), NIMH K23MH102128 (Dowshen).
Abbreviations
- CASI
Computer-Assisted Survey Instrument
- FDA
The Food and Drug Administration
- HIV
Human Immunodeficiency Virus
- IQR
Interquartile range
- MOSS-S
Medical Outcomes Study Social Support Survey
- MSM
Men who have sex with men
- PrEP
Pre-exposure Prophylaxis
- SD
Standard Deviation
- TDF-FTC
Tenofovir Disoproxil Fumarate/Emtricitabine
- YM/TWSM
Young men and transgender women who have sex with men
- YTW
Young transgender women
Footnotes
Disclosure of Potential Conflicts: Dr. Koenig is an Advisory Board member for Gilead Sciences. No other authors have conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Mustanski B, Birkett M, Kuhns LM, Latkin CA, Muth SQ. The Role of Geographic and Network Factors in Racial Disparities in HIV Among Young Men Who have Sex with Men: An Egocentric Network Study. AIDS Behav. 2015;19(6):1037–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mustanski B, Morgan E, D’Aquila R, Birkett M, Janulis P, Newcomb ME. Individual and Network Factors Associated with Racial Disparities in HIV Among Young Men who have sex with Men: Results from the Radar Cohort Study. J Acquir Immune Defic Syndr. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. HIV and African American Gay and Bisexual Men. Atlanta: 2018. [Google Scholar]
- 4.Kuhns LM, Hotton AL, Schneider J, Garofalo R, Fujimoto K. Use of Pre-exposure Prophylaxis (PrEP) in Young Men Who Have Sex with Men is Associated with Race, Sexual Risk Behavior and Peer Network Size. AIDS Behav. 2017;21(5):1376–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Veinot TC, Caldwell E, Loveluck J, Arnold MP, Bauermeister J. HIV Testing Behavior and Social Network Characteristics and Functions Among Young Men Who have Sex with Men (YMSM) in Metropolitan Detroit. AIDS Behav. 2016;20(11):2739–2761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Latkin CA, Davey-Rothwell MA, Knowlton AR, Alexander KA, Williams CT, Boodram B. Social network approaches to recruitment, HIV prevention, medical care, and medication adherence. J Acquir Immune Defic Syndr. 2013;63 Suppl 1:S54–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grant RM, Anderson PL, McMahan V, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14(9):820–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCormack S, Dunn DT, Desai M, et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2016;387(10013):53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siegler AJ, Mouhanna F, Giler RM, et al. The prevalence of pre-exposure prophylaxis use and the pre-exposure prophylaxis-to-need ratio in the fourth quarter of 2017, United States. Ann Epidemiol. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hosek SG, Landovitz RJ, Kapogiannis B, et al. Safety and Feasibility of Antiretroviral Preexposure Prophylaxis for Adolescent Men Who Have Sex With Men Aged 15 to 17 Years in the United States. JAMA Pediatr. 2017;171(11):1063–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hosek SG, Rudy B, Landovitz R, et al. An HIV Preexposure Prophylaxis Demonstration Project and Safety Study for Young MSM. J Acquir Immune Defic Syndr. 2017;74(1):21–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. HIV prevention pill not reaching most Americans who could benefit - especially people of color. 2018; https://www.cdc.gov/nchhstp/newsroom/2018/croi-2018-PrEP-press-release.html. Accessed 12/17/18, 2018.
- 13.Conron KJ, Mimiaga MJ, Landers SJ. A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health. 2010;100(10):1953–1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haire BG. Preexposure prophylaxis-related stigma: strategies to improve uptake and adherence - a narrative review. HIV AIDS (Auckl). 2015;7:241–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Committee on Lesbian G, Bisexual, and Transgender Health Issues and, Select RGaOBotHo, Populations; Institute of Medicine. Childhood/Adolescence In: Institute of Medicine, ed. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, D.C: : National Academy of Sciences; 2011:141–185. [Google Scholar]
- 16.Jenness SM, Goodreau SM, Rosenberg E, et al. Impact of the Centers for Disease Control’s HIV Preexposure Prophylaxis Guidelines for Men Who Have Sex With Men in the United States. J Infect Dis. 2016;214(12):1800–1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lazarus R, Folkman S. Stress, Appraisal and Coping New York: Springer; 1984. [Google Scholar]
- 18.Flores D, Barroso J. 21st Century Parent-Child Sex Communication in the United States: A Process Review. J Sex Res. 2017;54(4–5):532–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Horne SG, Levitt HM, Sweeney KK, Puckett JA, Hampton ML. African American Gay Family Networks: An Entry Point for HIV Prevention. J Sex Res. 2014:1–14. [DOI] [PubMed] [Google Scholar]
- 20.Soler JH, Caldwell CH, Cordova D, Harper G, Bauermeister JA. Who counts as family? Family typologies, family support, and family undermining among young adult gay and bisexual men. Sex Res Social Policy. 2018;15(2):123–138. [PMC free article] [PubMed] [Google Scholar]
- 21.Dickson-Gomez J, Owczarzak J, St Lawrence J, et al. Beyond the ball: implications for HIV risk and prevention among the constructed families of African American men who have sex with men. AIDS Behav. 2014;18(11):2156–2168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61(7):1576–1596. [DOI] [PubMed] [Google Scholar]
- 23.Williams DR, Yan Y, Jackson JS, Anderson NB. Racial Differences in Physical and Mental Health: Socio-economic Status, Stress and Discrimination. J Health Psychol. 1997;2(3):335–351. [DOI] [PubMed] [Google Scholar]
- 24.Burt RS. Network Items and the General Social Survey Social Networks. 1984;Six(Four):293–339. [Google Scholar]
- 25.Mason M Sample size and saturation in PhD studies using qualitative interviews. Forum: qualitative social research. 2010;11(3). [Google Scholar]
- 26.Glaser B Theoretical Sensitivity: Advances in the methodology of grounded theory. Mill Valley, CA: Sociology Press; 1978. [Google Scholar]
- 27.Schneider J, Michaels S, Bouris A. Family network proportion and HIV risk among black men who have sex with men. J Acquir Immune Defic Syndr. 2012;61(5):627–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O’Malley AJ, Marsden PV. The Analysis of Social Networks. Health Serv Outcomes Res Methodol. 2008;8(4):222–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Newman ME. Assortative mixing in networks. Phys Rev Lett. 2002;89(20):208701. [DOI] [PubMed] [Google Scholar]
- 30.Croft DP, Madden JR, Franks DW, James R. Hypothesis testing in animal social networks. Trends Ecol Evol. 2011;26(10):502–507. [DOI] [PubMed] [Google Scholar]
- 31.R: A language and environment for statistical computing. [computer program]. R Foundation for Statistical Computing, Vienna, Austria: 2018. [Google Scholar]
- 32.Arnold EA, Sterrett-Hong E, Jonas A, Pollack LM. Social networks and social support among ball-attending African American men who have sex with men and transgender women are associated with HIV-related outcomes. Glob Public Health. 2018;13(2):144–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kogan SM, Lei MK, Brody GH, Futris TG, Sperr M, Anderson T. Implementing Family-Centered Prevention in Rural African American Communities: a Randomized Effectiveness Trial of the Strong African American Families Program. Prev Sci. 2016;17(2):248–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Prado G, Pantin H, Huang S, et al. Effects of a family intervention in reducing HIV risk behaviors among high-risk Hispanic adolescents: a randomized controlled trial. Arch Pediatr Adolesc Med. 2012;166(2):127–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kapadia F, Halkitis P, Barton S, Siconolfi D, Figueroa RP. Associations between social support network characteristics and receipt of emotional and material support among a sample of male sexual minority youth. J Gay Lesbian Soc Serv. 2014;26(3):279–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mehrotra ML, Rivet Amico K, McMahan V, et al. The Role of Social Relationships in PrEP Uptake and Use Among Transgender Women and Men Who Have Sex with Men. AIDS Behav. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Copen CE, Dittus PJ, Leichliter JS. Confidentiality Concerns and Sexual and Reproductive Health Care Among Adolescents and Young Adults Aged 15–25. NCHS Data Brief. 2016(266):1–8. [PubMed] [Google Scholar]
- 38.Pearson WS, Cramer R, Tao G, Leichliter JS, Gift TL, Hoover KW. Willingness to Use Health Insurance at a Sexually Transmitted Disease Clinic: A Survey of Patients at 21 US Clinics. Am J Public Health. 2016;106(8):1511–1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ryan C, Russell ST, Huebner D, Diaz R, Sanchez J. Family acceptance in adolescence and the health of LGBT young adults. J Child Adolesc Psychiatr Nurs. 2010;23(4):205–213. [DOI] [PubMed] [Google Scholar]
- 40.Escudero DJ, Kerr T, Operario D, Socias ME, Sued O, Marshall BD. Inclusion of trans women in pre-exposure prophylaxis trials: a review. AIDS Care. 2015;27(5):637–641. [DOI] [PMC free article] [PubMed] [Google Scholar]