Abstract
BACKGROUND:
Acute healthcare interventions for residents of Skilled Nursing Facilities (SNFs) are often unwarranted, unwanted and/or harmful. We describe a provider-focused care model to reduce unwarranted or unwanted acute healthcare utilization.
OBJECTIVE:
Assess the capability of the Reducing Avoidable Facility Transfers (RAFT) model to reduce unwanted and unwarranted acute healthcare utilization among residents in three rural SNFs between January 1, 2016 and June 30, 2017.
DESIGN:
Prospective cohort, pre/post study.
SETTING:
Three rural SNFs in collaboration with a geriatric practice in a tertiary academic medical center.
PARTICIPANTS:
Post-Acute Care (PAC) and Long Term Care (LTC) residents of three rural SNFs.
INTERVENTION:
RAFT includes the following components: (1) a small team of providers who manage longitudinal care and after hours call; (2) elicitation of advance care plans and preferences regarding acute care; (3) standardized communication process engaging the provider at the identification of an acute care event; (4) a biweekly case review of all ED transfers.
MEASURES:
ED and hospital utilization.
RESULTS:
RAFT demonstrated a 35% reduction in monthly ED transfers and a 30.5% reduction in monthly hospitalizations. These reductions were greatest for Long Term Care (LTC) residents.
CONCLUSIONS/IMPLICATIONS:
The RAFT approach substantially reduced unwarranted ED and hospital utilization in this study. Results support replication and evaluation in a larger, more diverse setting and population.
Keywords: Skilled Nursing Facilities, Hospitalizations, Emergency Department Utilization, Quality Improvement, Goals of Care, Patient Transfers, Provider
Brief Summary
This study demonstrated the feasibility and effectiveness of a provider-focused, goal driven care model to reduce ED transfers for residents of SNFs. Results support replication in a diverse setting and population.
INTRODUCTION
Illnesses, injuries or healthcare interventions that are easily tolerated by robust individuals frequently have markedly debilitating results for frail older adults; a narrow window exists between the potential to help and the potential to harm.1–3 This is frequently observed when a frail older adult is acutely transferred to the Emergency Department (ED). Though the potential for life saving is greatest in this environment, so also is the chance for increased suffering and debility.4, 5 This is seen most prominently in the Skilled Nursing Facility (SNF) population where frail elders represent the majority of residents and where the complications associated with ED transfer have been well documented.5, 6 Moreover, many studies have shown that a large proportion of ED transfers from SNFs are unwarranted and avoidable.7–17 An effective means is needed for determining whether ED transfer or hospitalization is warranted or desired by the patient. Unfortunately, current processes in SNFs have a limited ability to establish and implement a customized plan of care when a resident experiences an acute health care crisis.18, 19 The standard response typically defaults to transfer to an ED initiating a cascade of tests and treatments that may carry undue risk or not correspond to the resident’s preferences and goals.4, 20
Emerging models of SNF-based care have shown promise. INTERACT provides tools and training to improve care coordination for residents and reduce inappropriate or unwanted interventions.21, 22 The Missouri Quality Initiative for Nursing Homes embeds a full-time nurse practitioner in SNFs and has reduced hospitalizations, improved clinical outcomes and reduced total expenditures for long-term patients.23, 24 Training SNF staff in advance care planning and end of life care has been associated with reduced avoidable ED transfers.19, 25, 26 On-site nurse-trainers and policy development have also demonstrated fewer hospital transfers, improved quality of care and reduced cost.27
These models all share a focus on the staff and workflows of SNFs. There has been less focus on the physicians, nurse practitioners and physician assistants who oversee patient care and manage acute crises. These clinicians, often employed outside the facility, have a unique skillset for evaluating acute events in the light of disease trajectory and care goals. Moreover, their role within the healthcare system makes them uniquely able to alleviate the fear and anxiety of patients, family and staff that can dominate decision making. Yet no model has been developed which maximizes their role toward ensuring high quality patient centered care.
An approach developed in a Continuing Care Retirement Community (CCRC) in New England provides a potential new model for SNFs. In this model, the delivery of on-site, goal-driven primary and on-call care by a small team of providers was associated with improved concordance with patients’ wishes and lower rates of hospitalization and ED visits for a socioeconomically advantaged population.28 Building on the success of this model, a team of clinicians at a tertiary academic hospital in rural New Hampshire developed the RAFT (Reducing Avoidable Facility Transfers) model with the goal of reducing unwarranted ED and hospital transfers for a more diverse population of residents at three rural SNFs.
METHODS
Pre-RAFT Care Model
Prior to implementing RAFT, physicians on our geriatric team served as medical director at each of the three facilities. Providers were assigned 1–2 facilities and at least one member of the team was on site every business day. After-hours call was covered broadly by the 29 physicians in our internal medicine practice. Many of these physicians spent no time in these facilities and had little training in geriatrics or SNFs. Elicitation of advance directives was left to the discretion of the individual providers and the SNF staff.
RAFT Model of SNF Care
The development, implementation, and evaluation of RAFT began in January 2016 and was completed in June 2017. Verbal support for the intervention was obtained from the Administrators and Directors of Nursing at each building at the outset and results were periodically reported by the medical director at Quality Assurance Performance Improvement (QAPI) meetings.
The Dartmouth College Committee for the Protection of Human Subjects (CPHS) determined that this work was exempt from review as human subjects research.
RAFT consists of the following components:
1). Small team of providers who manage longitudinal care and after-hours call.
All the care in the 3 facilities was managed by a team of 5 physicians, 3 nurse practitioners and 1 physician’s assistant (3.6 full-time equivalents). 2–3 providers were regularly assigned to each building and at least one provider was on site every business day. After hours call was managed exclusively by this team.
2). Systematic elicitation of advance care plans including acute care preferences.
The task of completing advance care plans and Provider Orders for Life Sustaining Treatment (POLST) forms was presented to residents as standard practice at the SNF. Early in care, providers were encouraged to prioritize the need to conduct a goals of care meeting as high, medium or low. Higher priority was assigned to residents deemed to have a poorer understanding of their condition or a higher risk of an acute decline. Advance care plans were established formally in meetings with the provider unless care goals were thought to be unambiguous and appropriate. In these instances, a social worker or nurse would facilitate the process and the POLST was signed later by the provider. Orders established through the POLST were formally entered into the SNF medical record. Advance care plans were documented in the providers electronic medical record (EMR) in a standard location and to which all providers had 24/7 access. Providers received monthly reports of patients whose plans were missing key items. Rates of completion by facility and provider were tracked over time and reviewed monthly.
Plans were considered complete if they included the following five domains:
Resuscitation status [Full or DNR];
Healthcare agent name, contact information and activation status
General care goals as per the POLST form [Full, Limited, Comfort]
Hospitalization preference [Hospitalize: Unlimited Interventions, Hospitalize: Limited Interventions, Do Not Hospitalize: Treat in Place, Do Not Hospitalize Comfort Focused]
Hospice enrollment [Yes or No]
3). Increased engagement of the provider during an acute care event.
A nurse-led education session was held with all nursing staff to explain the benefits of engaging the provider early. Nurses were strongly encouraged to call the provider before contacting the family or arranging for transfer. No formal tool was used to facilitate nurse/provider communication. Providers were encouraged to directly engage with the patient rather than through SNF staff.
4). Case Review.
The team met twice monthly to discuss the most recent hospital transfers which were tracked through the hospital EMR. Facilitated by the team leader, each meeting lasted one hour during which approximately 15–20 cases were discussed. The meeting’s focus was to exchange skills for managing an acute decline within the context of patient goals and to identify missed opportunities to safely and reasonably prevent ED transfers. Two questions were routinely put to the group as each transfer was reviewed: 1) Before the acute event, were there actions the provider team could have safely and reasonably taken to have prevented this transfer? (Examples: treating symptoms earlier, clarifying goals) 2) During the acute event were there actions the provider team could have safely and reasonably taken to have prevented this transfer? (Examples: treating on site, engaging directly with patient or family rather than through staff)
Measures and Data Analytic Plan
Our primary outcomes included ED transfers and hospitalizations for SNF residents overall, and for Post-Acute Care (PAC) and Long Term Care (LTC) subgroups. Secondary outcomes included advanced care planning status, hospital charges and standard Minimum Data Set (MDS) quality metrics. We used student t-tests to assess for significant differences in outcomes and population characteristics that could influence outcomes.
RESULTS
Three SNFs were enrolled in the pilot study. Our team managed 95–100% of the patients in each facility. As seen in Table 1, facilities varied across descriptive characteristics.
Table 1.
Characteristics of Participating Skilled Nursing Facilities (SNFs) January 1, 2016-June 30, 2017
| SNF 1 | SNF 2 | SNF 3 | |
|---|---|---|---|
| Family Owned | Large National Chain | Small Chain | |
| Ownership | For Profit | For Profit | For Profit |
| Avg Daily Census | 39.58 | 107.08 | 85.58 |
| Avg Admits Per Month | 3.92 | 24.67 | 22.10 |
| Avg Discharges Per Month | 3.74 | 24.92 | 22.42 |
| Avg Deaths Per Month | 0.42 | 3.83 | 3.08 |
| Avg Case Mix (Acuity)* | 1.0000 | 1.0190 | 0.9913 |
| Avg Age | 81.24 | 78.98 | 76.48 |
| Avg Female/Male Ratio | 3.29 | 2.10 | 2.27 |
| Avg LTC/PAC Ratio | 2.10 | 2.65 | 1.87 |
| Avg Qtrly Star Rating | 4.50 | 3.25 | 2.00 |
Resource Utilization Group (RUG) Score
Primary Outcomes
Figure 2 demonstrates the impact on ED and hospital utilization. Mean monthly ED transfers decreased from 24.8 (SD=6.5) at baseline to 15.9 (SD=3.0) post intervention, representing a 35.8% reduction (t-5.09, df= 28, p<0.01). Mean monthly LTC ED transfers reduced from 11.1 (SD=3.9) at baseline to 4.2 (SD=2.3) post-intervention, representing a 61.9% reduction (t= 6.13, df= 28, p<0.01). Mean monthly ED transfers of PAC patients did not change significantly post-intervention (t= 1.39, df=28, p=0.18). Mean monthly hospitalizations decreased by 30.5% from 15.8 (SD=6.2) in 2015 to 10.9 (SD=3.7) post-intervention (t-2.65, df= 28, p<0.01) LTC hospitalizations decreased from a monthly average of 6.5 (SD=2.9) at baseline to 2.4 (SD=1.5) post-intervention (t= 4.95, df= 28, p<0.01), a 62.4% reduction. PAC average monthly hospitalizations decreased slightly from 9.3 (SD=4.8) at baseline to 8.5 (SD=3.0) post-intervention (t=0.53, df= 28, p=0.29), representing an 8.1% reduction.
Figures 2a-2b. Overall average monthly ED and hospitalization transfer frequencies for pre-intervention baseline in 2015 (Pre) and post-intervention 2016-June 2017 (Post).
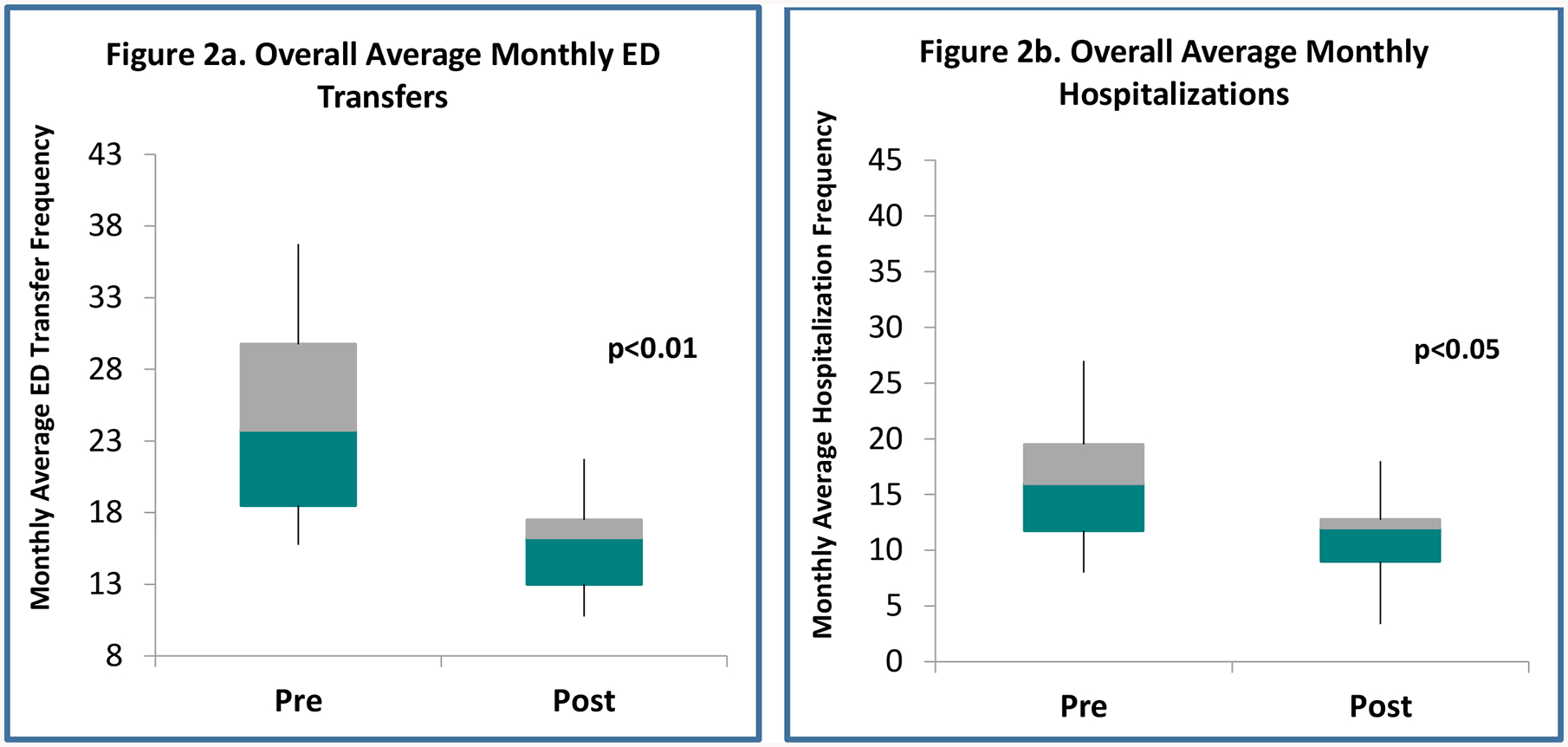
Overall= Long Term Care (LTC) + Post-Acute Care (PAC) populations. ED= Emergency Department. Significance determined by 2-tailed between subjects t tests assuming equal variances (df=28). Grey zone displays 75th percentile above the mean and blue zone displays 75th percentile below the mean. Whiskers depict the 99th percentile range of the distribution.
Secondary Outcomes
Overall, all three SNFs demonstrated substantial reductions in ED transfers and hospitalizations, however results varied across these categories and in stratified analyses (Table 2). All three facilities experienced significant reductions in total ED transfers post-intervention in the LTC population but only one achieved a significant reduction in the PAC population. Two of the three facilities realized a significant reduction in total hospitalizations. All three facilities achieved significant reductions in hospitalizations for the LTC subgroup, and only one realized significant reductions for the PAC subgroup.
Table 2.
Primary Outcomes by Skilled Nursing Facility (SNF)
| SNF 1 Pre | SNF 1 Post | t | SNF 2 Pre | SNF 2 Post | t | SNF 3 Pre | SNF 3 Post | t | |
|---|---|---|---|---|---|---|---|---|---|
| Monthly Outcomes | |||||||||
| Mean (SD) | |||||||||
| Total ED Transfers | 4.6 (2.8) | 2.2 (2.1) | 2.70** | 11.4 (4.8) | 7.9 (2.5) | 2.60** | 8.0 (3.8) | 5.6 (2.5) | 2.10* |
| PAC ED Transfers | 2.6 (2.1) | 1.2 (1.6) | 2.00* | 6.7 (3.7) | 6.5 (3.2) | 0.13 | 3.8 (1.7) | 3.75 (2.2) | −0.40 |
| LTC ED Transfers | 2.0 (2.1) | 0.9 (0.8) | 1.90* | 4.8 (2.3) | 1.4 (1.5) | 4.80** | 4.3 (3.0) | 1.8 (1.2) | 3.10** |
| Total Hospitalizations | 2.7 (2.1) | 1.4 (1.7) | 1.80* | 7.4 (3.9) | 5.8 (2.5) | 1.40 | 5.7 (2.6) | 3.6 (2.3) | 2.30* |
| PAC Hospitalizations | 1.3 (1.1) | 0.8 (1.1) | 1.40 | 4.7 (2.8) | 4.9 (2.8) | −0.30 | 3.1 (2.0) | 2.6 (2.2) | 0.60 |
| LTC Hospitalizations | 1.3 (1.2) | 0.7 (0.8) | 1.80* | 2.8 (1.9) | 0.9 (1.0) | 3.50** | 2.6 (1.7) | 0.9 (0.7) | 3.60** |
Pre= Baseline period (2015). Post= Intervention period (2016-June 2017). SNF= Skilled Nursing Facility. ED= Emergency department. LTC= Long Term Care. PAC= Post Acute Care. Total Cost = ED and hospitalization related costs for LTC and PAC transfers combined. t= t Test statistic (Degrees of Freedom = 28 for all analyses). Statistical significance determined via one-sided Student t-test.
= p<0.05,
= p<0.01
We gathered a cross-sectional sample at the end of the study (June 30, 2017) describing formal preferences for acute care management. Of the 216 residents (65 PAC and 151 LTC) under our care 164 (75.9%) had formally registered a recorded a preference. Of the 151 LTC residents, 132 (87.3%) had registered a preference. Of the 65 PAC residents, 32 (49.3%) had registered a preference. Overall, 32.3% of those with a documented preference chose hospitalization. In the PAC subgroup, 69.7% of the PAC subgroup chose hospitalization; only 22.7% of the LTC subgroup chose hospitalization. The LTC subgroup preferred alternatives to hospitalization most. 45.5% chose comfort care options and 31.8% chose the Treat in Place (TIP) option. Only 12.5% of PAC residents chose comfort care and 15.6% chose TIP.
Cost was approximated using all charges from the time of arrival in the ED to hospital discharge at the one hospital that provided 93% of all ED visits and hospitalizations from these facilities. We did not have access to claims data. Overall mean monthly charges decreased by 51.1% from approximately $1M (SD=$47,630) at baseline to $488,588 (SD=$9,302) post intervention (t=4.0, df=28, p<0.01). Average monthly LTC charges reduced by 66.8% from $410,660 (SD=$30,468) at baseline to $136,123 (SD=$5,200) post-intervention (t=3.0, df=27, p<0.01). Average monthly PAC charges decreased by 36.9% from $633,126 (SD=$30,933) at baseline to $399,460 (SD=$11,657) post-intervention (t=2.18, df=27, p<0.05).
Finally, we measured key characteristics that could potentially influence ED and hospital utilization. These included reported MDS quality measures, staffing ratio and case mix. We observed no significant changes in any of these factors during the intervention period when compared to previous years.
DISCUSSION
This pilot study of the RAFT intervention found a statistically significant reduction in ED and hospital use among LTC residents of SNFs. This was seen without a related impact on key quality measures. Like other models, RAFT provides evidence that much of the acute care provided to SNF residents can be provided more safely, more effectively and more inexpensively than is currently the norm. This study showed limited benefit with PAC patients. While there was some utilization reduction among this population, the reduction was not statistically significant across facilities. Much of the benefit of RAFT hinged on systematic goals of care discussions. Scheduling a meeting shortly after SNF admission when risk of re-hospitalization is highest often proved unfeasible in the midst the other more pressing details. Further modifications to better identify high-risk patients and facilitate early conversations could prove very helpful.
While our study was small, the magnitude of our results is equal or greater than in larger studies. INTERACT demonstrated a 17% reduction in hospital admissions.22 RAFT showed a 29% reduction in year 1 and a 35% reduction in year 2. The Missouri Quality Initiative for Nursing Homes showed a 30% reduction in hospitalizations for long-term SNF residents. In our model LTC hospitalizations reduced by 67% in year 1 and 69% in year 2.23, 24 Despite different populations, staffing levels and quality ratings, LTC patients in all three facilities experienced significant and sustained reduction in ED transfers, hospitalizations and charges. While our study did not have the scale or diversity of larger studies, the strength and consistency of our results suggest that RAFT may be effective in reducing unwanted and unwarranted hospital transfers more broadly.
Several components of our model are noteworthy. First, we limited the on-call pool to a small team of clinicians familiar with the care of frail individuals and SNFs. For most clinicians, a phone call about an acutely ill and vulnerable patient represents a high-risk situation for which ED transfer can seem the only alternative. The “SNFist,” armed with a deep understanding of the patients, schedule, culture and resources in residential care, is better able to implement a practicable alternative than the clinician who has little SNF experience.
The addition of “Do Not Hospitalize – Treat In Place” as a formal option was critical to our success. Many patients and their families expressed an explicit interest in limiting aggressive interventions; at the end of the study only 14% of directives elected unlimited life prolonging interventions. But while most were disinclined toward unlimited care, many were not ready for a purely comfort focused approach either. They wanted some interventions taken to prolong life, particularly if those interventions offered limited risk of distress. The option of “Limited Interventions -Treat in Place” provided an attractive middle road that matched the values of 32% percent of our long-term patients; together with those who elected “Do Not Hospitalize - Comfort Only” this accounted for 77% of the LTC patients having formal “Do Not Hospitalize” orders at the completion of our study.
The active and early engagement of the on-call provider when an acute issue arose was also important. Providers were encouraged to speak directly to family rather than through nurses. Prior to RAFT, clinicians often received calls stating “the family wants the patient sent to the ED.” At this point it was generally too late to do otherwise, the family was sufficiently alarmed so that keeping the patient on site seemed like negligence and conveyed an unhelpful lack of confidence in the nurse’s assessment. Engaging the provider early provided time to attempt gentler interventions, carefully assess goals and strengthen families’ confidence that a reasonable and safe plan was in place.
Finally, the regular review of all ED transfers was extremely productive. Twice monthly we systematically reviewed the events prior to and during the acute event. Unlike other interventions, our focus was not on whether the transfer was clinically indicated but rather what the team might have reasonably and safely done differently to change the outcome.29–30 This helped team members learn from each other and develop skills in de-escalation, patient centered communication and care coordination. It also introduced some accountability where previously there was very little. Before RAFT, providers had little disincentive to ED transfer. Unsure of the patient’s condition, the nurse’s reliability or the family’s litigiousness transfer represented the safest path that few would question. With RAFT, though providers were free to make any decision they thought best, that decision was made with the knowledge that they would soon be called upon to explain their actions to their peers.
Limitations
Despite promising results, our study has a number of significant limitations. First, it is not possible to definitively determine the effectiveness of RAFT using a pre-/post, non-randomized design we employed in this pilot study. Second, hospitalization rates amongst SNF patients have modestly declined nationally possibly accounting for a portion of the decline observed.31 Third, a surrogate indicator of cost was used (hospital-based charges). Our study was not designed with cost as a primary outcome and did not calculate actual costs or formal cost-effectiveness. A surrogate indicator of cost was used (hospital charges). Fourth, due to the relatively small sample size, we are not able to do subgroup analyses or explore potential confounders or effect modifiers that could influence our findings. For example, we did not analyze potential interactions with diagnosis codes in identifying additional factors associated with clinically avoidable ED transfers. In a future longitudinal study, an analytic strategy utilizing regression modeling could provide adjusted multivariate analyses of cost and outcomes. Fifth, it is possible that our results may not generalize to other populations or health care delivery settings. For example, the academic medical center’s position as the sole major healthcare presence in our rural region is unique and the ethnically homogenous population may limit generalizability of our findings. Sixth, the small team of providers was made up largely of physicians (three of whom are certified in Geriatrics or Palliative Care) potentially affecting the magnitude of the results and downstream scalability of the model. Adapting it toward greater involvement by nurse practitioners, social workers and nurses could facilitate greater likelihood of broadly disseminating the RAFT model.
IMPLICATIONS AND CONCLUSION
In this pilot study, a dedicated group of clinicians substantially reduced ED and hospital utilization for SNF residents by deepening provider engagement in acute care management, aligning care with preferences and increasing transparency and accountability. Like other models, RAFT provides further evidence that much of the hospital associated care provided to SNF residents is unwarranted and could be better provided on site at lower cost. Unlike other models which direct training and new workflows toward facility staff, RAFT focuses more on the providers who oversee patient care, strengthening their awareness of, engagement with and accountability to patient values and wishes. In so doing, RAFT identifies tools, workflows and standards which can be used to train, assess and support providers who care for SNF patients. This work was a small-scale effort which yielded large results and established initial groundwork toward a model which merits future study in larger scale, more diverse populations.
Figure 1.

The RAFT Intervention
Figure 3.
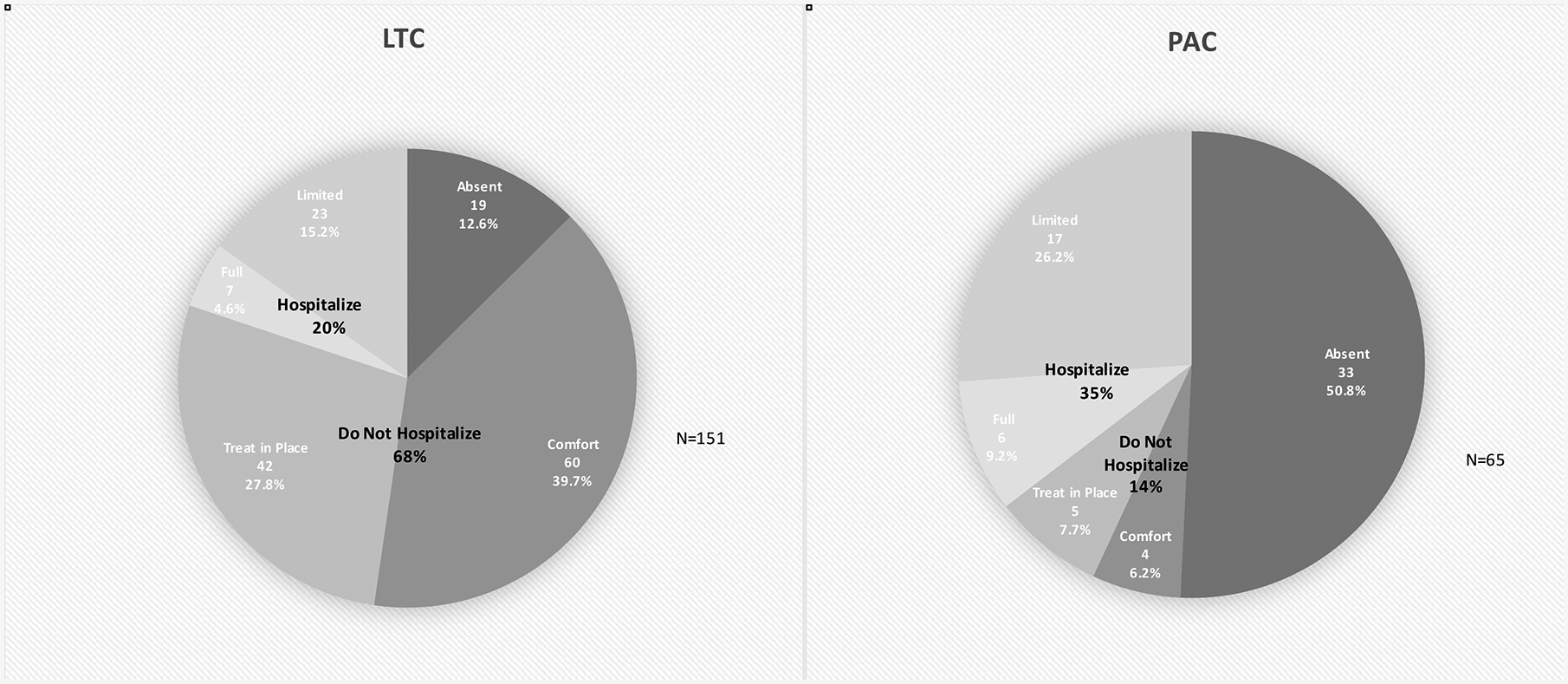
Acute Care Preferences at Study End (June 30, 2017)
Acknowledgements
The authors would like to thank the following individuals for their thoughtful assistance: Christopher Allen, Catherine Amarante, Martha Bruce, Peter DiMilia, Cheryl Elinsky, Gina Fernandez, Amy Hall, Karen Hibbard, Heather Huntley, Teresa Lewis, Stephen Liu, Barbara Lazar, Paula Marcotte, Barbara Maloney and Diane Price. The authors would also like to acknowledge the Collaboratory for Implementation Science at Dartmouth for research and mentorship support.
Financial Disclosures:
Dr. Batsis’ research reported in this publication was supported in part by the National Institute on Aging of the National Institutes of Health under Award Number K23AG051681.
Support was also provided by the Dartmouth Health Promotion and Disease Prevention Research Center supported by Cooperative Agreement Number U48DP005018 from the Centers for Disease Control and Prevention. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or represent the official position of the Centers for Disease Control and Prevention.
Dr. Bartels receives funding from the National Institute of Mental Health (K12 HS0217695 (AHRQ), NIMH: T32 MH073553, R01 MH078052, R01 MH089811; R24 MH102794 CDC U48DP005018.
Funding sources
This work was supported by the National Institute on Aging (NIA K23AG051681); and the Dartmouth Health Promotion and Disease Prevention Research Center (CDC U48DP005018).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICTS OF INTEREST
The authors do not have any Conflicts of Interest to disclose.
REFERENCES
- 1.Fried LP, Ferrucci L, Darer J, et al. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci 2004;59(3):255–263. [DOI] [PubMed] [Google Scholar]
- 2.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56(3):M146–156. [DOI] [PubMed] [Google Scholar]
- 3.Hogan DB, MacKnight C, Bergman H, et al. Models, definitions, and criteria of frailty. Aging Clin Exp Res 2003;15(3 Suppl):1–29. [PubMed] [Google Scholar]
- 4.Ishihara KK, Wrenn K, Wright SW, et al. Advance directives in the emergency department: too few, too late. Acad Emerg Med 1996;3(1):50–53. [DOI] [PubMed] [Google Scholar]
- 5.Lakin JR, Isaacs E, Sullivan E, et al. Emergency Physicians’ Experience with Advance Care Planning Documentation in the Electronic Medical Record: Useful, Needed, and Elusive. J Palliat Med 2016;19(6):632–638. [DOI] [PubMed] [Google Scholar]
- 6.Carter L, Skinner J, Robinson S. Patients from care homes who attend the emergency department: could they be managed differently. Emerg Med J 2009;26(4):259–262. [DOI] [PubMed] [Google Scholar]
- 7.Ashcraft AS, Champion JD. Nursing home resident symptomatology triggering transfer: avoiding unnecessary hospitalizations. Nursing research and practice 2012;2012:495103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Givens JL, Selby K, Goldfeld KS, et al. Hospital transfers of nursing home residents with advanced dementia. J Am Geriatr Soc 2012;60(5):905–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hullick C, Conway J, Higgins I, et al. Emergency department transfers and hospital admissions from residential aged care facilities: a controlled pre-post design study. BMC Geriatr 2016;16:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ingber MJ, Feng Z, Khatutsky G, et al. Initiative To Reduce Avoidable Hospitalizations Among Nursing Facility Residents Shows Promising Results. Health Aff (Millwood) 2017;36(3):441–450. [DOI] [PubMed] [Google Scholar]
- 11.Intrator O, Zinn J, Mor V. Nursing home characteristics and potentially preventable hospitalizations of long-stay residents. J Am Geriatr Soc 2004;52(10):1730–1736. [DOI] [PubMed] [Google Scholar]
- 12.Kada O, Janig H, Wiedermann W, et al. [Project to reduce preventable hospital transfer from homes for the aged and nursing home. Is it really always necessary?]. Pflege Z 2012;65(3):176–178. [PubMed] [Google Scholar]
- 13.Mathew R, Young Y, Shrestha S. Factors associated with potentially preventable hospitalization among nursing home residents in New York State with chronic kidney disease. J Am Med Dir Assoc 2012;13(4):337–343. [DOI] [PubMed] [Google Scholar]
- 14.McAndrew RM, Grabowski DC, Dangi A, et al. Prevalence and patterns of potentially avoidable hospitalizations in the US long-term care setting. International journal for quality in health care : journal of the International Society for Quality in Health Care 2016;28(1):104–109. [DOI] [PubMed] [Google Scholar]
- 15.Spector WD, Limcangco R, Williams C, et al. Potentially avoidable hospitalizations for elderly long-stay residents in nursing homes. Medical care 2013;51(8):673–681. [DOI] [PubMed] [Google Scholar]
- 16.Tena-Nelson R, Santos K, Weingast E, et al. Reducing potentially preventable hospital transfers: results from a thirty nursing home collaborative. J Am Med Dir Assoc 2012;13(7):651–656. [DOI] [PubMed] [Google Scholar]
- 17.Xing J, Mukamel DB, Temkin-Greener H. Hospitalizations of nursing home residents in the last year of life: nursing home characteristics and variation in potentially avoidable hospitalizations. J Am Geriatr Soc 2013;61(11):1900–1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McGlade C, Daly E, McCarthy J, et al. Challenges in implementing an advance care planning programme in long-term care. Nurs Ethics 2017;24(1):87–99. [DOI] [PubMed] [Google Scholar]
- 19.Molloy DW, Guyatt GH, Russo R, et al. Systematic Implementation of an Advance Directive Program in Nursing Homes. Jama 2000;283(11):1437. [DOI] [PubMed] [Google Scholar]
- 20.Burkle CM, Mueller PS, Swetz KM, et al. Physician perspectives and compliance with patient advance directives: the role external factors play on physician decision making. BMC Med Ethics 2012;13:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kane RL, Huckfeldt P, Tappen R, et al. Effects of an Intervention to Reduce Hospitalizations From Nursing Homes: A Randomized Implementation Trial of the INTERACT Program. JAMA internal medicine 2017;177(9):1257–1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ouslander JG, Lamb G, Tappen R, et al. Interventions to reduce hospitalizations from nursing homes: evaluation of the INTERACT II collaborative quality improvement project. J Am Geriatr Soc 2011;59(4):745–753. [DOI] [PubMed] [Google Scholar]
- 23.Rantz MJ, Birtley NM, Flesner M, et al. Call to action: APRNs in U.S. nursing homes to improve care and reduce costs. Nursing outlook 2017;65(6):689–696. [DOI] [PubMed] [Google Scholar]
- 24.Rantz MJ, Popejoy L, Vogelsmeier A, et al. Successfully Reducing Hospitalizations of Nursing Home Residents: Results of the Missouri Quality Initiative. J Am Med Dir Assoc 2017;18(11):960–966. [DOI] [PubMed] [Google Scholar]
- 25.Hanson LC, Zimmerman S, Song M-K, et al. Effect of the Goals of Care Intervention for Advanced Dementia. JAMA internal medicine 2017;177(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Teno JM, Gozalo P, Mitchell SL, et al. Terminal hospitalizations of nursing home residents: does facility increasing the rate of do not resuscitate orders reduce them? J Pain Symptom Manage 2011;41(6):1040–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoben M, Chamberlain SA, Knopp-Sihota JA, et al. Impact of Symptoms and Care Practices on Nursing Home Residents at the End of Life: A Rating by Front-line Care Providers. J Am Med Dir Assoc 2016;17(2):155–161. [DOI] [PubMed] [Google Scholar]
- 28.Bynum JPW, Andrews A, Sharp S, et al. Fewer Hospitalizations Result When Primary Care Is Highly Integrated Into A Continuing Care Retirement Community. Health Affairs 2011;30(5):975–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burke RE, Rooks SP, Levy C, et al. Identifying Potentially Preventable Emergency Department Visits by Nursing Home Residents in the United States. J Am Med Dir Assoc 2015; 16(5):395–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Trahan LM, Spiers JA, Cummings GG. Decisions to Transfer Nursing Home Residents to Emergency Departments: A Scoping Review of Contributing Factors and Staff Perspectives. J Am Med Dir Assoc 2016; 17(11):994–1005. [DOI] [PubMed] [Google Scholar]
- 31.Nakashima T, Young Y, Hsu WH. Are Hospital/ED Transfers Less Likely Among Nursing Home Residents with Do-Not-Hospitalize Orders? J Am Med Dir Assoc 2017;18(5):438–41. [DOI] [PubMed] [Google Scholar]


