Abstract
A 46-year-old Japanese man was admitted to our hospital with a 1-year history of dyspnea and persistent right-dominant bilateral pleural effusions. Chest and abdominal computed tomography (CT) revealed no notable findings apart from the bilateral pleural effusions. 2-deoxy-2-[18F]-fluoro-D-glucose (FDG) positron emission tomography-CT showed no accumulation of FDG in the thorax and abdomen. Thoracoscopy revealed numerous small (approximately 2-3 mm in size), blister-like nodules on the left parietal pleura extending from the lower third of the chest wall to the diaphragm. A pathological examination revealed lymphocyte and plasma cell infiltrates with increasing numbers of IgG4-positive plasma cells in the fibrotic pleura, indicating IgG4-related pleuritis.
Keywords: IgG4-related disease, thoracoscopy, pleural effusion
Introduction
IgG4-related disease has recently been recognized as a fibroinflammatory condition characterized by lymphoplasmacytic infiltrates of IgG4-positive cells (1). IgG4-related disease has been described in various organs. In the lungs, it variably presents as interstitial pneumonia, inflammatory pseudotumor, bronchial inflammation, and pleuritis (2), although pleuritis is a rare finding.
We herein report a patient with bilateral pleural effusions as the only lung manifestation of IgG4-related disease. The thoracoscopic pleural findings in this patient were quite interesting.
Case Report
A 46-year-old Japanese man was admitted to our hospital with a 1-year history of dyspnea and persistent right-dominant bilateral pleural effusions. The right pleural effusion remained unchanged; however, the left pleural effusion had increased. Thus, the disease activity was judged to be higher in the left than in the right lung. Therefore, we performed left thoracic puncture and examined the left pleural effusion.
The left pleural effusion was clear-yellow with a predominance of lymphocytes (68%); total protein (TP) and lactic acid dehydrogenase (LDH) levels were 5.3 g/dL and 85 U/L, respectively (indicating exudative pleural effusion, as expected). The adenosine deaminase (ADA) level was 36.4 U/L, which was within normal limits (<40 U/L). Although high ADA levels in the pleural effusion are usually suggestive of tuberculous pleurisy, few cases of IgG4-related pleuritis with high ADA levels in the pleural effusion have been reported (3). No pathogenic organisms or malignant cells were detected.
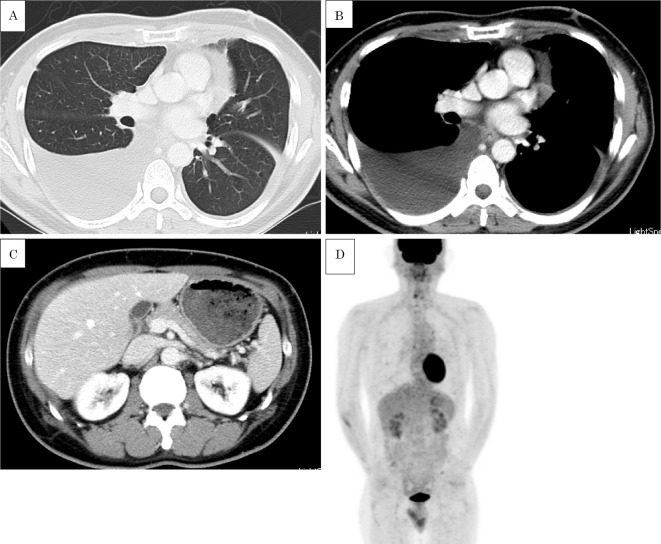
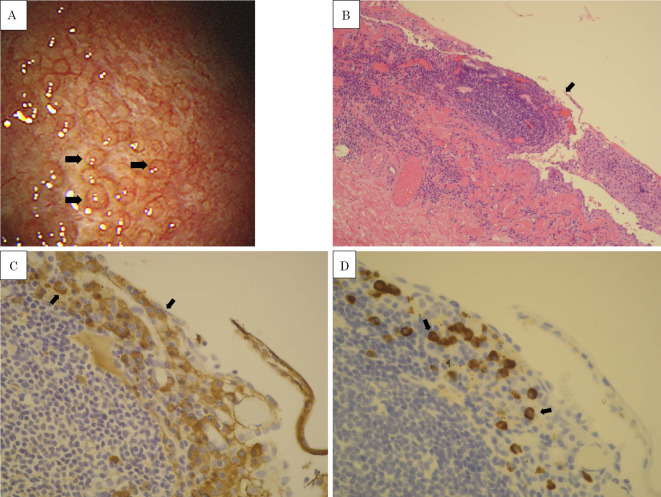
The chest and abdominal computed tomography (CT) findings were unremarkable except for the bilateral pleural effusion (Fig. 1A-C). 2-deoxy-2-[18F]-fluoro-D-glucose (FDG) positron emission tomography (PET)-CT showed no FDG accumulation within the thorax (Fig. 1D). Thoracoscopy revealed numerous small (approximately 2-3 mm in size), blister-like nodules on the left parietal pleura extending from the lower third of the chest wall to the diaphragm (Fig. 2A). A pathological examination revealed lymphocyte and plasma cell infiltrates in the fibrotic pleura (Fig. 2B). Immunohistochemical staining indicated that approximately half of the IgG-positive plasma cells were IgG4-positive, with 22 IgG4-positive plasma cells observed per high-power field (HPF), and the percentage of IgG4/IgG was 42% (22/52) (Fig. 2C, D). The IgG4 level was 142 mg/dL in the serum (reference range, 4.5-117 mg/dL) and 256 mg/dL in the pleural effusion. These findings were consistent with IgG4-related pleuritis.
Figure 1.
CT and PET/CT findings. A, B) Chest CT showed only bilateral effusion. C) Abdominal CT showed no specific findings. D) FDG-PET showed no accumulation of FDG within the thorax.
Figure 2.
Thoracoscopic and pathological findings. A) Thoracoscopic findings showing numerous small, blister-like nodules on the parietal pleura (arrows). B) Pleural tissues stained with hematoxylin and eosin showing lymphocyte and plasmacyte infiltrations in the fibrotic pleura (Original magnification, ×100). The arrow indicates a small, blister-like nodule. C) Immunohistochemical staining of the biopsies for IgG showing dense infiltration of IgG-positive plasmacytes just below a layer of mesothelial cells (Original magnification, ×400). D) Immunohistochemical staining showing that 42% of the IgG-positive plasmacytes were IgG4-positive (Original magnification, ×400).
The comprehensive clinical diagnostic criteria for IgG4-related disease were as follows: 1) a clinical examination showing characteristic diffuse/localized swelling or masses in a single or multiple organs; 2) a hematological examination showing elevated serum IgG4 concentrations (≥135 mg/dL); and 3) a histopathologic examination showing (i) marked lymphocyte and plasmacyte infiltration and fibrosis and (ii) infiltration of IgG4+plasma cells: ratio of IgG4+/IgG+cells >40% and >10 IgG4+plasma cells/HPF. The present case met all of these diagnostic criteria. Therefore, treatment was started with oral prednisolone (30 mg/day). Approximately one month later, the pleural effusion disappeared. The prednisolone dose was gradually tapered to 10 mg/day; there has since been no recurrence of the pleural disease.
Discussion
Common radiologic findings in IgG4-related lung disease include mediastinal lymphadenopathy and thickening of the perilymphatic interstitium with or without subpleural and/or peribronchovascular consolidation (2). However, our patient exhibited only pleural effusion on chest CT; given the rarity of pleuritis as a form of IgG4-related disease (3-13), the diagnosis was not immediately obvious. Interestingly, the pleura was studded with numerous small, blister-like nodules, which was histopathologically consistent with IgG4-related pleuritis.
There have been five previous reports including thoracoscopic findings in patients with this condition. One reported milky pleural plaques suggestive of hyalinized collagen fiber deposits (12). The other three reported diffuse inflammatory thickening of the pleura (8, 10, 14, 15). In addition, nodules on the parietal pleura were noted in two cases (15, 16). In our patient, however, thoracoscopy revealed a nodular pattern of pleuritis across an extensive area. Kondo and Uehara noted the accumulation of FDG in the pleura on PET-CT, which was not observed in our patient. Among previously reported cases of pleuritis, three did not have FDG accumulation (5, 9, 13), but two did (11, 12). The serum IgG4 levels did not differ markedly between cases with and without positive PET scans. Data were not available on the IgG4 levels in the pleural effusion in cases with a positive PET scan. The difference in thoracoscopic findings between our case and the previously reported cases in which nodules were not noted is attributable to the stage or degree of activity of the IgG4-related disease. However, our findings may simply be more possible manifestations of IgG4-related pleuritis, as two previous reports have also described the presence of nodules on part of the pleura.
In 20-25% cases of pleural effusion, a definitive diagnosis cannot be made, despite a pleural fluid analysis and closed pleural biopsy. Thoracoscopy increases the diagnostic yield (14); therefore, it is an important approach that may help determine the etiology of pleuritis (14). If numerous small, blister-like nodules are observed on the pleura, a biopsy should be performed, which may indicate IgG4-related pleuritis, as in our patient.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med 366: 539-551, 2012. [DOI] [PubMed] [Google Scholar]
- 2. Matsui S, Hebisawa A, Sakai F, et al. Immunoglobulin G4-related lung disease: Clinicoradiological and pathological features. Respirology 18: 480-487, 2013. [DOI] [PubMed] [Google Scholar]
- 3. Nagayasu A, Kubo S, Nakano K, et al. IgG4-related pleuritis with elevated adenosine deaminase in pleural effusion. Intern Med 57: 2251-2257, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yamashita K, Haga H, Kobashi Y, Miyagawa-Hayashino A, Yoshizawa A, Manabe T. Lung involvement in IgG4-related lymphoplasmacytic vasculitis and interstitial fibrosis: report of 3 cases and review of the literature. Am J Surg Pathol 32: 1620-1626, 2008. [DOI] [PubMed] [Google Scholar]
- 5. Yamamoto H, Suzuki T, Yasuo M, et al. IgG4-related pleural disease diagnosed by a re-evaluation of chronic bilateral pleuritis in a patient who experienced occasional acute left bacterial pleuritis. Intern Med 50: 893-897, 2011. [DOI] [PubMed] [Google Scholar]
- 6. Sekiguchi H, Horie R, Utz JP, Ryu JH. IgG4-related systemic disease presenting with lung entrapment and constrictive pericarditis. Chest 142: 781-783, 2012. [DOI] [PubMed] [Google Scholar]
- 7. Ishida M, Hodohara K, Furuya A, et al. Concomitant occurrence of IgG4-related pleuritis and periaortitis: a case report with review of the literature. Int J Clin Exp Pathol 7: 808-814, 2014. [PMC free article] [PubMed] [Google Scholar]
- 8. Ishida A, Furuya N, Nishisaka T, Mineshita M, Miyazawa T. IgG4-related pleural disease presenting as a massive bilateral effusion. J Bronchology Interv Pulmonol 21: 237-241, 2014. [DOI] [PubMed] [Google Scholar]
- 9. Kato E, Takayanagi N, Ishiguro T, Kagiyama N, Shimizu Y, Sugita Y. IgG4-related pleuritis with chylothorax. Intern Med 53: 1545-1548, 2014. [DOI] [PubMed] [Google Scholar]
- 10. Corcoran JP, Culver EL, Psallidas I, et al. A 63-year-old man with a recurrent right-sided pleural effusion. Thorax 70: 504-507, 2015. [DOI] [PubMed] [Google Scholar]
- 11. Gajewska ME, Rychwicka-Kielek BA, Sørensen K, Kubik M, Hilberg O, Bendstrup E. Immunoglobulin G4-related pleuritis - a case report. Respir Med Case Rep 24: 18-20, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kondo T, Uehara T. Immunoglobulin G4-related disease with fibroinflammatory lesions in the pleura, bile ducts and pericardium. CMAJ 188: 972, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kita T, Araya T, Ichikawa Y, et al. IgG4-Related pleuritis with no other organ involvement. Am J Med Sci 365: 487-492, 2018. [DOI] [PubMed] [Google Scholar]
- 14. Lee P, Colt HG. Rigid and semirigid pleuroscopy: the future is bright. Respirology 10: 418-425, 2005. [DOI] [PubMed] [Google Scholar]
- 15. Tong X, Bai M, Wang W, Han Q, Tian P, Fan H. IgG4-related disease involving polyserous effusions with elevated serum interleukin-6 levels: a case report and literature review. Immunol Res 65: 944-950, 2017. [DOI] [PubMed] [Google Scholar]
- 16. Ramponi S, Gnetti L, Marvisi M. Lung manifestations of IgG4-related disease. A multifaceted disorder. Sarcoidosis Vasc Dif 35: 74-80, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]