Abstract
Introduction
Stress and obesity are two public health issues. The relationship between obesity and stress is biological through the actions of stress on the major hormones that regulate appetite (leptin and ghrelin). Many spa resorts in France specialise in the treatment of obesity, but no thermal spa currently proposes a specific programme to manage stress in obesity. The ObesiStress protocol has been designed to offer a new residential stress management programme. This thermal spa treatment of obesity implements stress management strategies as suggested by international recommendations.
Methods and analysis
140 overweight or obese participants with a Body Mass Index of >25 kg/m2 and aged over 18 years will be recruited. Participants will be randomised into two groups: a control group of usual practice (restrictive diet, physical activity and thermal spa treatment) and an intervention group with stress management in addition to the usual practice. In the present protocol, parameters will be measured on five occasions (at inclusion, at the beginning of the spa (day 0), at the end of the spa (day 21), and at 6 and 12 months). The study will assess the participants’ heart rate variability, cardiac remodelling and function, electrodermal activity, blood markers, anthropometric profile, body composition, psychology and quality of life via the use of questionnaires and bone parameters.
Ethics and dissemination
The ObesiStress protocol complies with the ethics guidelines for Clinical Research and has been approved by the ethics committee (CPP Sud-Est VI, Clermont-Ferrand - ANSM: 2016-A01774-47). This study aimed to highlight the efficacy of a 21-day thermal spa residential programme of stress management in obesity through objective measurements of well-being and cardiovascular morbidity. Results will be disseminated during several research conferences and articles published in peer-reviewed journals.
Trial registration number
Keywords: obesity, stress, prevention, heart rate variability, spa bath
Strengths and limitations of this study.
Reliability and validity of a 21-day specific thermal spa residential programme on stress management in the treatment of obesity.
Better comprehension of the psychology and psychological mechanisms involved in stress management in obesity.
A 12-month mixed gender longitudinal study.
Inability to accurately account for the long-term cost-effective benefits of the study.
Introduction
Stress and obesity are two public health issues.1 2 Stress can lead to obesity, a major stress factor,3 via inappropriate eating behaviours.4 Furthermore, stressed people are also those who have the greatest difficulty losing weight.5 The relationship between obesity and stress is biological through the action of stress on the major hormones which regulate appetite (leptin and ghrelin).6 7 The relationship between obesity and stress is so strong that proposals for international recommendations suggest the implementation of stress management programmes in obesity for sustainable weight loss.8
Among the multiple physical and psychological consequences of stress and obesity, increased mortality and cardiovascular morbidity seem to be the main concern.9 Stress and obesity alter the functioning of the autonomic nervous system.10–12 A deregulation of the sympathovagal balance is a major factor of morbidity cardiovascular mortality.13 Conveniently, the sympathovagal balance can be measured easily and without pain using heart rate variability (HRV), which is a biomarker of both stress and morbidity/mortality.10 14 15 Stress and obesity also cause arterial ischaemic pathology16 through complex mechanisms involving changes in endothelial and arterial atheroscleroses.16 These microvascular changes are linked to systemic inflammation caused by stress17 and obesity.18
The thermal spa resort in Vichy, as well as other spa centres in France, already possesses expertise in obesity treatment through physical activity, diet and hydrotherapy. However, no spa resort has ever proposed the inclusion of a stress-management programme in obesity treatment. Non-pharmacological stress management can be achieved through psychological interventions (ie, physical19 and psychoanalytical approaches,20 cognitive–behavioural therapy,21 acceptance and commitment therapy,22 23 or mindfulness,24 25 physical activity26 27 and the improvement of eating disorders induced by stress).28 The benefits of physical activity on physical and mental health are indisputable, at any age, and with any activity.29
The main hypothesis of this project is that a thermal spa residential programme (21 days) of stress management in obesity will demonstrate its efficacy through objective measurements of well-being and cardiovascular morbidity via a randomised controlled design that compares a group with stress management and a group without stress management (both groups will benefit from the same spa treatments, physical activity and diet).
Objectives
The main objective was to assess the ability of a 21-day residential spa programme of stress management in the treatment of obesity to increase HRV, a biomarker of both stress and morbidity/mortality.
Secondary outcomes were (1) to demonstrate an improvement in stress-related and obesity-related variables following the short residential spa programme; (2) to study the influence of genetic polymorphisms on stress, obesity, and response to our stress management programme; (3) to examine the relationship between stress-related and obesity-related variables; (4) to propose a salient biomarker or a salient composite index of biomarkers of stress in obesity; and (5) to study the effect of adherence to the programme during follow-up on stress-related and obesity-related variables.
Methods
The TIDieR checklist can be found in online supplementary file S1.
bmjopen-2018-027058supp001.pdf (646.8KB, pdf)
Protocol design
This 1-year randomised controlled study with repeated measurements at five time points (inclusion, at the start and the end of the spa programme, and at 6 and 12 months) will allow us to understand the effect of a 21-day residential spa programme of stress management in the treatment of obesity through the measurement of well-being and cardiovascular morbidity.
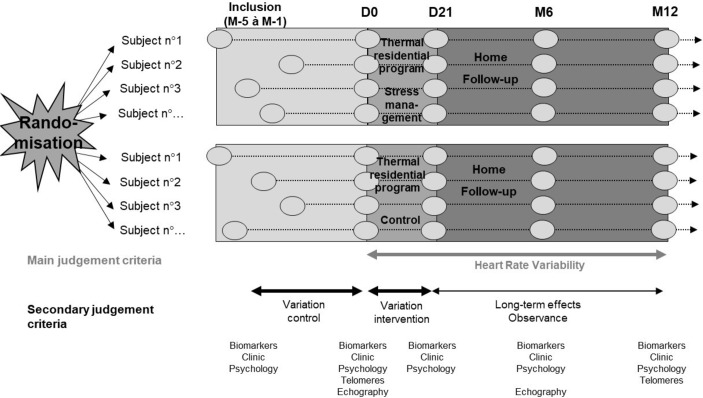
For this study, two randomised groups of overweight or obese participants will be compared: one will receive the usual 21-day thermal spa residential programme, while the other will receive the 21-day thermal spa residential programme plus a psychological intervention (figure 1).
Figure 1.
The ObesiStress protocol. M month, D day.
Randomisation
Randomisation will be stratified by Body Mass Index (BMI) category (25–30, 30–35 and >35), sex and levels of stress (Visual Analogue Scale of stress <50, between 50 and 80, and >80) using a minimisation approach. A permuted-block randomisation (ie, random block sizes) will be conducted using a computer-generated random allocation (STATA software V.13), with a 1:1 allocation ratio, ensuring the complete randomness of the assignment of a participant to each randomised group. To guarantee the concealment of the allocation, the participants will be randomised after they have clearly met the inclusion criteria and have provided written consent (online supplementary file S2).
bmjopen-2018-027058supp002.pdf (67.2KB, pdf)
Selection criteria
Inclusion criteria
Volunteers will be overweight or obese participants aged over 18 years who wish to follow a thermal spa residential programme for the treatment of obesity. We will also promote the study through advertisements in local newspapers and on the radio. Volunteers will be screened by telephone interview or directly by spa physicians. A participant’s weight must have been stable over the last 3 months, with no uncontrolled cardiac, hepatic, renal or endocrine diseases.2 Stress at baseline will not be an inclusion criteria but an explanatory/independent variable. In compliance with human ethics guidelines, participants will have to be covered by social health insurance and will have to sign consent forms.
Exclusion criteria
Volunteers participating in the study will be excluded if major treatment and protocol deviations are observed.14 Drugs and medical conditions that significantly affect the primary outcome (HRV) will also be exclusion criteria (eg, alpha or beta blockers, arrhythmia or conduction disorders such as bundle branch block and atrioventricular heart block).30 Bariatric surgery is also an exclusion criterion.
Power analysis
The rationale for the sample size calculation is based on HRV, which is a biomarker of both stress and morbidity/mortality.10 14 15 Specifically, within the multiple parameters of HRV, we considered the log low frequency (LF)/high frequency (HF) for the sample size calculation because it is the parameter that traditionally represents sympathovagal balance (see description of LF/HF below in the description of the primary outcome).10 14 A log LF/HF with low values is associated with a good adaptation of the autonomic nervous system. Based on our results from a pilot study (data not published),2 we hope to highlight an absolute difference of 12% between the groups with regard to the decrease of log LF/HF at 1 year after the stress management programme. For an SD of 20%, the expected size will be around 0.60. For a two-sided type I error of 5%, we will need to include 59 participants per group to achieve a statistical power of 90%. Finally, the recruitment of 70 patients per arm is proposed in order to take into account lost to follow-up.
Participants
As previously stated, participants engaged in this protocol will be mixed gender overweight or obese volunteers aged over 18 years. Following approval from the ethics committee, and based on our calculation, a total of 70 volunteers will be enrolled per group (ie, a total of 140 participants) to account for potential dropouts. All participants will be given written information regarding the project and will have to sign consent forms before enrolment. Participants will be recruited from the usual clients at the spa resort in Vichy, through healthcare workers (physicians, dietitians and physiotherapists), or through advertisements. Inclusions will be carried out at the University Hospital in Clermont-Ferrand or at the thermal spa resort in Vichy.
Usual thermal spa care
All participants will undergo the usual thermal spa treatment that combines the correction of eating disorders (and a negative energy balance of 500 kcal/day), physical activity (2 hours 30 min/day, minimum), thermal spa treatment (2 hours/day, minimum) and health education (1 hour 30 min/day, minimum: cooking, nutrition and physical activity classes). Physical activity will be diverse (endurance, strength and circuit training) and personalised for each participant.
Psychological interventions
Participants randomised to the intervention group will benefit from psychological interventions based on validated approaches to stress (3×1 hour 30 min/week, ie, nine sessions in total). Participants will attend psychological sessions in groups of fewer than 10 individuals. Individual meetings with the psychologist will occur at least twice: at the beginning of the residential programme and at the end. Psychological interventions will include various validated approaches to work-related stress: physical19 and psychoanalytic20 approaches, cognitive–behavioural therapy,21 acceptance and commitment therapy23 31 and mindfulness.24 25 Participants will have to acquire techniques in order to become autonomous and pursue at-home psychological training. The nine psychological sessions will be the following: (1) stress management and lack of self-confidence, (2) cognitive–behavioural therapy, (3) body-centred approach: body language, (4) management of emotions, (5) identity approach: concept and self-image, (6) cognitive approach (information processing), (7) sophrology: relaxation, (8) food and addictive behaviour, and (9) psychopathological approach and anxiety disorders. Each session will be constructed and validated by a psychologist specialised in the session’s field and already working in the management of obese individuals. The aim was to build a psychological programme that can be easily replicated for long-term use after evidence-based proof of success.
Follow-up
After the intervention phase of the study, participants will undergo a 1-year at-home follow-up with measurements at 6 and 12 months.
Measurements
Each participant will perform a battery of tests (described further). As previously described, data collection will be performed five times (at inclusion, at the start and the end of the spa programme, and at 6 and 12 months), with the exception of dual-energy X-ray absorptiometry (DXA) and peripheral quantitative CT (pQCT), which will be performed at inclusion and after 12 months, and cardiac remodelling and function, which will be performed at inclusion and after 6 months.
Primary outcome
HRV
Our primary outcome will be changes in HRV parameters. HRV parameters will be assessed over 26 hours with a heart rate transmitter belt simply positioned on the chest, with a 26-hour recording time, a beat per min range of 25–240, and a respiratory rate range of 3–70 (Zephyr BioHarness BT; Zephyr Technology, Annapolis, USA). The HRV data will be examined according to the recommendations of the European Society of Cardiology and the North American Society (Task Force). HRV will be explored in two domains: time and frequency.32 The methodology developed by our team will also be applied.33 Premature beats will be visually checked and automatically discarded. In the time domain, we will analyse R–R intervals, the SD of the R–R intervals, the square root of the mean squared difference of successive R–R intervals (rMSSD) and the number of adjacent N–N differing by more than 50 ms divided by the total number of N–N intervals (pNN50). The rMSSD and pNN50 are associated with HF power and hence parasympathetic activity. In the spectral domain, we will analyse LF (0.04–0.15 Hz) and HF (0.15–0.4 Hz) power. LF is an index of both sympathetic and parasympathetic activities, and HF represents the main efferent parasympathetic (vagal) activity to the sinus node. Very low frequency (VLF, 0.003–0.04 Hz) partially reflects variations in the activity of the renin–angiotensin system, thermoregulatory mechanisms and the function of peripheral chemoreceptors. LF and HF will also be assessed in normalised units (nu), that is, the relative value of each power component in proportion to the total power minus the VLF component. Thus, LFnu and HFnu are suggested to represent the best sympathetic and parasympathetic activity, respectively. The LF:HF ratio, that is, the sympathovagal balance, will also be calculated.14
Secondary outcomes
Table 1 summarises the secondary outcomes of the project. Anthropometry and clinical parameters will be measured, including height (m), body mass (kg) or blood pressure (mm Hg). Waist circumference (cm) will be measured at mid-abdomen, that is, the midpoint between the subcostal and suprailiac landmarks, in accordance with the WHO protocol.34
Table 1.
Outcomes
| Variables | Type of measurements | Modalities of measurement | References |
| Stress and cardiovascular risk biomarkers | Heart rate variability | Holter | 81 |
| Skin conductance | Wristband electrodes – Movisens | 37 | |
| Blood flow velocity | Laser speckle contrast imaging | 82 83 | |
| Myocardial longitudinal strain | Speckle tracking echocardiography | 38 39 | |
| Genetic polymorphisms | Polymorphism of the ACE | Blood cells | 48–51 |
| Polymorphism of the serotonin | Blood cells | 52–54 | |
| Demographics* | Age, gender, qualification, personal work status, ethnicity, life and occupational events | Questionnaire | 10 |
| Clinical measurements | Height, weight, blood pressure, heart rate and waist circumference | ||
| Body composition | Muscle mass, fat mass and bone structure | Impedance metre | 36 |
| Densitometry X-ray absorption | 35 | ||
| Peripheral quantitative computed tomography | 73–75 | ||
| Quantitative ultrasounds | 84 | ||
| Psychology and quality of life | Depression | HAD (seven items) | 57 |
| Anxiety | HAD (seven items) Hamilton Scale for Anxiety (seven items) |
57 | |
| State and Trait Anxiety Inventory | 58 59 | ||
| General health | General Health Questionnaire SF-36 (36 items) |
71 | |
| Quality of life | Brief Multidimensional Life Satisfaction Scale (11 items) | 85 | |
| Stress, fatigue and sleep | 100 mm Visual Analogue Scale | 10 | |
| Burnout | Maslach Burnout Inventory | 56 | |
| Mindfulness | Mindfulness Fribourg Mindfulness Inventory | 22 23 | |
| Coping | Brief COPE questionnaire | 60 | |
| Emotions | Emotion Regulation Questionnaire | 61 | |
| Perception of work | Karasek’s Job Content Questionnaire | 63 | |
| Self-efficacy | Perceived Self-efficacy Scale | 64 | |
| Alexithymia | Toronto Alexithymia Scale | 65–67 | |
| Illness perception | Brief Illness Perception Questionnaire | 68 69 | |
| Metacognition | Metacognition Questionnaire | 70 | |
| Personal resources | Trait perception of workplace stress | Inner Correspondence/Peaceful Harmony with practices (17 items) |
86 |
| Lifestyle | Smoking, alcohol, coffee and food intake | Questionnaires | 10 |
| Physical activity | Recent Physical Activity Questionnaire | 72 | |
| Alloplastic load | HbA1c, HDLC and LDLC and TG | EDTA tube | 35 |
| Cortisol | Dry tube, serum isolation and deep-freezing | 46 47 | |
| DHEAS | Dry tube, serum isolation and deep-freezing | 46 47 | |
| Leptin | Dry tube, serum isolation and deep-freezing | 35 | |
| Ghrelin | Dry tube, serum isolation and deep-freezing | 7 41 | |
| BDNF | Dry tube, serum isolation and deep-freezing | 42–44 | |
| Proinflammatory cytokines: IL-1β, IL-6, IL-1 and TNFα | Dry tube, serum isolation and deep-freezing | 35 | |
| NPY | Dry tube, serum isolation and deep-freezing | 45 | |
| Telomere length | Blood, analysis by southern blot or PCR | 55 |
*Adjustment variables.
BDNF, brain-derived neurotrophic factor; COPE, Coping Orientation to Problems Experienced; COPE, Coping Orientation to Problems Experienced; DHEAS, Dehydroepiandrosterone-sulfate; HAD, Hospital Anxiety and Depression scale; HbA1c, hemoglobin A1c; HDLC, high-density lipoprotein cholesterol; IL, interleukin; LDLC, low-density lipoprotein cholesterol; NPY, Neuropeptide Y; SF-36, 36-Item Short Form health survey; TG, triglyceride; TNFα, tumour necrosis factor alpha.
Body composition
Body composition (muscle mass and fat mass) will be measured by DXA (QDR-4500A; Hologic, Waltham, MA)35 and by an impedance metre.36
Biomarkers of stress and cardiovascular risk
Skin conductance will be measured using wrist band electrodes with sampling rates at 2, 4, 8, 16 and 32 Hz during phases I–III. The SC sensor (Q-Sensor-Affectiva; Massachusetts Institute of Technology, USA) is set on a wristband and has a 24-hour battery life when recording. In addition, it will measure wrist movements with a built-in three-axis accelerometer.37
Blood flow velocity and myocardial longitudinal strain
Blood flow velocity and myocardial longitudinal strain will be measured by speckle echocardiography (Vivid Q; GE Healthcare, USA). All two-dimensional (2D), time motion, Doppler and 2D-strain acquisitions and measurements will be performed according to recent guidelines.38 39 Left ventricular (LV) volumes and ejection fractions will be measured using the Simpson biplane method. LV mass will be calculated with the Devereux formula and indexed for height (Cornell adjustment). Pulsed Doppler LV transmitral velocities, including early (E) and atrial (A) waves, will be obtained in the apical four-chamber view. Tissue Doppler imaging measurements of myocardial systolic (S’), early diastolic (E’) and atrial (A’) velocities will be assessed at the mitral annulus level in the apical four-chamber and two-chamber views. The E:Em ratio (ratio of early transmitralflow velocity to mitral annular early diastolic myocardial velocity) will be used as an index of LV filling pressure.40 Left atrium volume will be assessed on apical four-chamber and two-chamber views. A graduation of LV diastolic dysfunction will be obtained according to recent guidelines.40 2D cine loops (frame rate >70 ips) of at least five cycles will be recorded in the short-axis views (base, md and apex), as well as in the apical four-chamber, three-chamber and two-chamber views. 2D-strain analysis will be performed postprocessing using EchoPAC 201 TM software (GE Healthcare). Longitudinal and circumferential strains and strain rates, as well as rotations at the apex and base, will be directly obtained from the six-segment model. Twist mechanics will be computed from apical and basal rotational data using dedicated software (Scilab, Paris, France). For each view, the three cardiac cycles displaying the best image quality will be selected. Blood pressure and heart rate will be continuously monitored, and the systolic meridional wall stress, an index of afterload, will be calculated. LV end-diastolic volumes will also be obtained as preload indices.
Endocrine assays
Blood samples will be collected by a qualified nurse after participants have fasted overnight. Blood will be collected using a venipuncture of the brachial vein. After collection, blood will be centrifuged and aliquots will be stored (−80°) for subsequent analysis. Basic biology (eg, triglycerides, cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol and haemoglobin A1c),35 as well as all other biochemical determinants (eg, leptin,35 ghrelin,7 41 brain-derived neurotrophic factor,42–44 interleukin (IL)-1β,35 IL-6,35 IL-1,35 tumour necrosis factor alpha,35 NPY,45 cortisol46 47 and DHEAS46 47), will be assessed in the biochemistry laboratory at the University Hospital in Clermont-Ferrand. All analyses will be conducted by the same technician. Polymorphism of the ACE48–51 and polymorphism of the serotonin,52–54 as well as telomere lengths,55 will be measured via blood cells, all of which are linked with stress.
Complementary measurements
Stress, fatigue and sleep (Visual Analogue Scale of 100 mm)10; burnout (Maslach Burnout Inventory)56; depression and anxiety (Hospital Anxiety and Depression Scale, State and Trait Anxiety Inventory-Y (STAI-Y) and the 7-Item Hamilton Scale for Anxiety)57–59; mindfulness (Freiburg Mindfulness Inventory)22 23; coping strategies (Brief Coping Orientation to Problems Experienced Questionnaire)60; emotions (Emotion Regulation Questionnaire)61; perception of work (Karasek’s Job Content Questionnaire)62 63; self-efficacy (Perceived Self-Efficacy Scale)64; alexithymia (Toronto Alexithymia Scale)65–67; illness perception (Brief Illness Perception Questionnaire)68 69; metacognition (Metacognition Questionnaire)70; general health (36-Item General Health Questionnaire)71; lifestyle (smoking and alcohol)10; demographics (such as marital status and number of children); nutrition (3-day Self-Report Questionnaire with a face-to-face validation with a dietitian)2; and physical activity (Recent Physical Activity Questionnaire (RPAQ))72 will be obtained through questionnaires.
Bone parameters
Bone microarchitecture will be measured by pQCT (XCT 3000; Stratec Medizintechnik, Pforzheim, Germany).73–75 Bone mineral content (BMC) (g/cm), volumetric cortical and trabecular BMC (mg/cm3), total area (mm2), cortical and trabecular area (mm2) and density (g/cm²), and bone strength (mm3) will be assessed by 2 mm thick tomographic slices at the distal (4%) and proximal (66%) sites of the non-dominant tibia and radius. Scan speed and voxel size will be 20 mm/s and 0.4 mm, respectively. To ensure the quality of the measurements, calibration checks will be performed by scanning a standard phantom with known densities prior to each scan. Bone densitometry will be measured by DXA (QDR-4500A, Hologic). Bone mineral density (g/cm2) BMC (g) and bone area (cm2) will be determined for each participant. The DXA measurements will be taken for whole body, lumbar spine (L2–L4) and non-dominant hip (including the femoral neck and trochanteric and intertrochanteric regions). All DXA scans will be conducted by the same technician, and quality assurance checks will be routinely performed. The in vivo coefficient of variation is 0.5%.
Adherence to the physical activity, nutrition and psychological techniques will be retrieved. Physical activity will be assessed using the RPAQ at M6 and M12.72 Nutrition will be assessed at M6 and M12 through a 3-day self-report questionnaire with a face-to-face validation with a dietitian.2 The use of psychological techniques will be measured by monthly self-report questionnaires (number of times each technique was used per month).
Statistical analysis
Statistical analysis will be performed using the STATA software V.13. All statistical tests will be two-sided and p<0.05 will be considered significant. The data will be analysed as intention to treat. After testing for normal distribution (Shapiro-Wilk test), the data will be treated either by parametric or non-parametric analysis according to statistical assumptions. Intergroup comparisons will be performed (1) without adjustment and (2) adjusting on possible confounding factors.
To highlight that the spa residential programme will have long-term benefits (1 year) on the biomarkers of stress, the comparisons will be performed using the Student t-test or the Mann-Whitney test if the t-test assumptions are not respected (normality and homoscedasticity were analysed using the Fisher-Snedecor test). The results will be expressed as effect size and 95% CIs. This primary analysis will be completed by multivariable analyses (linear regression with logarithmic transformation of dependent outcomes if necessary) considering an adjustment on covariates fixed according to univariate results, clinical and epidemiological relevance (notably, age, gender, baseline BMI and baseline stress levels), and adherence to physical activity, nutrition and the use of psychological techniques. The results will be expressed as regression coefficients and 95% CIs.
Comparisons between groups will be performed in a similar way as presented previously for quantitative outcomes. Comparisons concerning categorical variables will be performed using χ2 or, when appropriate, the Fischer exact test. The results will be expressed as absolute risk differences and 95% CIs. The multivariable analysis will then be conducted using linear and generalised linear models according to the statistical nature of the dependent endpoint. The results will be expressed as regression coefficients or relative risks and 95% CIs.
Moreover, the relationships between the quantitative parameters will be analysed using correlation coefficients (Pearson or Spearman depending on the statistical distribution). Considering the several multiple comparisons, a correction of the type I error will be applied (Sidak’s correction). The comparisons of the correlation coefficients (in different groups of subjects and within a single group of subjects) will be performed using a Fisher’s Z transformation76 and Williams’ T2 statistic.77 Multidimensional factorial analyses will be performed to complete these statistical analyses.
Concerning the longitudinally collected parameters, mixed models will be performed to study fixed effects (group, time point evaluations and their interactions), taking into account the between-subject and within-subject variabilities (as random effect). For continuous endpoints, the normality of the residuals will be assessed using the Shapiro-Wilk test.
In addition, these analyses will be completed using analysis of covariance with the baseline values to study the differences during follow-up (end of the spa programme, 6 and 12 months).78 Normality of residuals will be verified.
A sensitivity analysis will be carried out to study the statistical nature of missing data (random or not) and then to apply the most appropriate imputation data method (multiple imputation data, last observation carried out). The baseline characteristics of participants with a complete follow-up and those lost to follow-up will be compared with the aforementioned statistical tests.
Radiation exposure and harm
Both DXA and pQCT provide measurements of the body composition and bone properties by exposing participants to low-level radiation: 0.0056 mSv from DXA scans (whole body, lumbar and hip) and 0.0014 mSv from the pQCT scans (tibia and radius measurements).79 Over the duration of each study, the effective administered dose will be 0.014 mSv.
A Harms section was not considered in the protocol, but this kind of intervention was considered to be very low risk by the ethics committee.
Confidentiality and blind assessments
The participants and care providers will not be blinded to the participants' randomisation group. However, in order to reduce the level of bias, the assessors for most outcomes will be blinded to each participant’s assigned group, for example, for HRV, biological measures or bone parameters. All outcome data will remain blinded until the end of the study. Patients’ data will be deidentified, and all data will be treated anonymously.
Patient and public involvement
The thermal spa centre in Vichy, in collaboration with the Preventive and Occupational Medicine Department of the University Hospital in Clermont-Ferrand, have identified and addressed the following priorities: prevention, obesity, weight loss, stress, cardiovascular morbidity. We are grateful for the opinion of the volunteers and professionals at the Vichy Spa Centre concerning the psychological intervention. Conferences and meetings with participants will be organised in order to provide feedback from this research.
Ethical considerations and dissemination
The ObesiStress protocol complies with the ethics guidelines for clinical research and has been approved by the ethics committee (Comités de Protection des Personnes, Sud-Est VI, Clermont-Ferrand–National Agency for Medical Security: 2016-A01774-47); the protocol has also been registered on clinicaltrials.gov. In accordance with ethical considerations, the chief investigator is responsible for ensuring that participants understand the potential risks and benefits of taking part in the study. Moreover, the chief investigator is responsible for obtaining written consent from the participants. The results will be disseminated at several research conferences and in articles published in peer-reviewed journals.
Discussion
The ObesiStress protocol has been designed to provide a better understanding of the effect of a spa residential programme combined with a stress management programme on the improvement of HRV in the treatment of obesity. The creation of a new thermal programme would allow new innovative approaches for stress management in obesity. The long-term success of lifestyle interventions such as those proposed in the prevention of obesity is adherence to the treatment (nutrition, physical activity and psychology).80 We previously demonstrated that a spa programme may play a major role in sustainable lifestyle changes.35 Due to the stress management programme and because the participants will be accompanied by healthcare professionals, the adherence to treatment during a 1-year follow-up could be more efficient. In order to avoid any generalisability of our expected results, we will pay particular attention at the demographics of the participants included (particularly between participants recruited from the ‘usual spa clients’ and other participants). Secondary and sensitivity analyses will take into account where the participants were recruited.
Current study status
The trial is currently recruiting participants.
Supplementary Material
Acknowledgments
We thank Richard May for his attentive editing of the manuscript, Ms Isabelle Jourde and Janine Lauradoux for their future management of biological sampling, and Sarah De Saint Vincent for biological analysis. Moreover, we thank Ms Anne-Cecile Fournier, Christine Flouzat and Marie-Anne Cousseau for their commitment to setting up the programme.
Footnotes
Contributors: FD contributed to the study design. FD was responsible for the submission of the protocol to the ethics committee. FD and AV coordinated the recruitment of patients. DC, EC and PD were responsible for bone measurements. AA was responsible for liver-related factors. DMP and SH were responsible for the psychosocial analysis. LM and MM were responsible for mindfulness, psychological education and cognitive-compartmental therapy analysis. GTV was responsible for the analysis of memory-related data. PO, OI and GB were responsible for cardiovascular measurements. YB, NF and MM-D were responsible for nutritional measurements and analysis. DC, EC and PD were responsible for physical activity analysis. AV was responsible for the collection of psychological factors. BP was responsible for the statistical analysis. EC was responsible for the clinical trial and wrote the first draft of this manuscript. All authors read and contributed to and approved the final manuscript.
Funding: The study is integrally funded by the Auvergne Rhône-Alpes, the University Hospital of Clermont-Ferrand and by the European Regional Development Fund (Fonds Europeen de Développement Economique et Régional). The funding sources had no role in the design, conduct, or reporting of the study.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Quine L. Workplace bullying in NHS community trust: staff questionnaire survey. BMJ 1999;318:228–32. 10.1136/bmj.318.7178.228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dutheil F, Lac G, Lesourd B, et al. . Different modalities of exercise to reduce visceral fat mass and cardiovascular risk in metabolic syndrome: the RESOLVE* randomized trial. Int J Cardiol 2013;168:3634–42. 10.1016/j.ijcard.2013.05.012 [DOI] [PubMed] [Google Scholar]
- 3. Foss B, Dyrstad SM. Stress in obesity: cause or consequence? Med Hypotheses 2011;77:7–10. 10.1016/j.mehy.2011.03.011 [DOI] [PubMed] [Google Scholar]
- 4. Sinha R, Jastreboff AM. Stress as a common risk factor for obesity and addiction. Biol Psychiatry 2013;73:827–35. 10.1016/j.biopsych.2013.01.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Robinson E, Hunger JM, Daly M. Perceived weight status and risk of weight gain across life in US and UK adults. Int J Obes 2015;39:1721–6. 10.1038/ijo.2015.143 [DOI] [PubMed] [Google Scholar]
- 6. Haleem DJ. Investigations into the involvement of leptin in responses to stress. Behav Pharmacol 2014;25:384–97. [DOI] [PubMed] [Google Scholar]
- 7. Schellekens H, Finger BC, Dinan TG, et al. . Ghrelin signalling and obesity: at the interface of stress, mood and food reward. Pharmacol Ther 2012;135:316–26. 10.1016/j.pharmthera.2012.06.004 [DOI] [PubMed] [Google Scholar]
- 8. Isasi CR, Parrinello CM, Jung MM, et al. . Psychosocial stress is associated with obesity and diet quality in Hispanic/Latino adults. Ann Epidemiol 2015;25:84–9. 10.1016/j.annepidem.2014.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Backé E-M, Seidler A, Latza U, et al. . The role of psychosocial stress at work for the development of cardiovascular diseases: a systematic review. Int Arch Occup Environ Health 2012;85:67–79. 10.1007/s00420-011-0643-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dutheil F, Boudet G, Perrier C, et al. . JOBSTRESS study: comparison of heart rate variability in emergency physicians working a 24-hour shift or a 14-hour night shift — a randomized trial. Int J Cardiol 2012;158:322–5. 10.1016/j.ijcard.2012.04.141 [DOI] [PubMed] [Google Scholar]
- 11. Karason K, Mølgaard H, Wikstrand J, et al. . Heart rate variability in obesity and the effect of weight loss. Am J Cardiol 1999;83:1242–7. 10.1016/S0002-9149(99)00066-1 [DOI] [PubMed] [Google Scholar]
- 12. Chintala KK, Krishna BH, MR N. Heart rate variability in overweight health care students: correlation with visceral fat. JCDR 2015;9 10.7860/JCDR/2015/12145.5434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tsuji H, Larson MG, Venditti FJ, et al. . Impact of reduced heart rate variability on risk for cardiac events. The Framingham heart study. Circulation 1996;94:2850–5. 10.1161/01.cir.94.11.2850 [DOI] [PubMed] [Google Scholar]
- 14. Boudet G, Walther G, Courteix D, et al. . Paradoxical dissociation between heart rate and heart rate variability following different modalities of exercise in individuals with metabolic syndrome: the resolve study. Eur J Prev Cardiol 2017;24:281–96. 10.1177/2047487316679523 [DOI] [PubMed] [Google Scholar]
- 15. Hufnagel C, Chambres P, Bertrand PR, et al. . The need for objective measures of stress in autism. Front Psychol 2017;8 10.3389/fpsyg.2017.00064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Proietti R, Mapelli D, Volpe B, et al. . Mental stress and ischemic heart disease: evolving awareness of a complex association. Future Cardiol 2011;7:425–37. 10.2217/fca.11.13 [DOI] [PubMed] [Google Scholar]
- 17. Elenkov IJ, Iezzoni DG, Daly A, et al. . Cytokine dysregulation, inflammation and well-being. Neuroimmunomodulation 2005;12:255–69. 10.1159/000087104 [DOI] [PubMed] [Google Scholar]
- 18. Dutheil F, Lesourd B, Courteix D, et al. . Blood lipids and adipokines concentrations during a 6-month nutritional and physical activity intervention for metabolic syndrome treatment. Lipids Health Dis 2010;9:148 10.1186/1476-511X-9-148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bloom L, Shelton B, Bengough M, et al. . Psychosocial outcomes of a non-dieting based positive body image community program for overweight adults: a pilot study. J Eat Disord 2013;1 10.1186/2050-2974-1-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Waysfeld B. Psychological approaches to the obese]. Presse Med 2000;29:556–63. [PubMed] [Google Scholar]
- 21. van der Klink JJ, Blonk RW, Schene AH, et al. . The benefits of interventions for work-related stress. American Journal of Public Health 2001;91:270–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Banz WJ, Maher MA, Thompson WG, et al. . Effects of resistance versus aerobic training on coronary artery disease risk factors. Exp Biol Med 2003;228:434–40. 10.1177/153537020322800414 [DOI] [PubMed] [Google Scholar]
- 23. Brinkborg H, Michanek J, Hesser H, et al. . Acceptance and commitment therapy for the treatment of stress among social workers: a randomized controlled trial. Behav Res Ther 2011;49:389–98. 10.1016/j.brat.2011.03.009 [DOI] [PubMed] [Google Scholar]
- 24. Davies WR. Mindful meditation: healing burnout in critical care nursing. Holist Nurs Pract 2008;22:32–6. [DOI] [PubMed] [Google Scholar]
- 25. Cohen-Katz J, Wiley SD, Capuano T, et al. . The effects of mindfulness-based stress reduction on nurse stress and burnout: a quantitative and qualitative study. Holist Nurs Pract 2004;18:302–8. [DOI] [PubMed] [Google Scholar]
- 26. Stults-Kolehmainen MA, Sinha R. The effects of stress on physical activity and exercise. Sports Med 2014;44:81–121. 10.1007/s40279-013-0090-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hansen Åse Marie, Blangsted AK, Hansen EA, et al. . Physical activity, job demand–control, perceived stress–energy, and salivary cortisol in white-collar workers. Int Arch Occup Environ Health 2010;83:143–53. 10.1007/s00420-009-0440-7 [DOI] [PubMed] [Google Scholar]
- 28. Stress K-GJK. Food, and inflammation: psychoneuroimmunology and nutrition at the cutting edge. Psychosomatic medicine 2010;72:365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bhui KS, Dinos S, Stansfeld SA, et al. . A synthesis of the evidence for managing stress at work: a review of the reviews reporting on anxiety, depression, and absenteeism. J Environ Public Health 2012;2012:1–21. 10.1155/2012/515874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Elghozi J-L, Girard A, Laude D. Effects of drugs on the autonomic control of short-term heart rate variability. Autonomic Neuroscience 2001;90:116–21. 10.1016/S1566-0702(01)00276-4 [DOI] [PubMed] [Google Scholar]
- 31. Bond FW, Bunce D. The role of acceptance and job control in mental health, job satisfaction, and work performance. J Appl Psychol 2003;88:1057–67. 10.1037/0021-9010.88.6.1057 [DOI] [PubMed] [Google Scholar]
- 32. Tochikubo O, Ikeda A, Miyajima E, et al. . Effects of insufficient sleep on blood pressure monitored by a new multibiomedical recorder. Hypertension 1996;27:1318–24. 10.1161/01.HYP.27.6.1318 [DOI] [PubMed] [Google Scholar]
- 33. Khalfa N, Bertrand PR, Boudet G, et al. . Heart rate regulation processed through wavelet analysis and change detection: some case studies. Acta Biotheor 2012;60:109–29. 10.1007/s10441-012-9154-4 [DOI] [PubMed] [Google Scholar]
- 34. Report of a WHO consultation Obesity: preventing and managing the global epidemic. World Health Organ Tech Rep Ser 2000;894:1–253. [PubMed] [Google Scholar]
- 35. Courteix D, Valente-dos-Santos J, Ferry B, et al. . Multilevel approach of a 1-year program of dietary and exercise interventions on bone mineral content and density in metabolic syndrome – the resolve randomized controlled trial. PLoS One 2015;10:e0136491 10.1371/journal.pone.0136491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Pateyjohns IR, Brinkworth GD, Buckley JD, et al. . Comparison of three bioelectrical impedance methods with DXA in overweight and obese Men*. Obesity 2006;14:2064–70. 10.1038/oby.2006.241 [DOI] [PubMed] [Google Scholar]
- 37. Dutheil F, Chambres P, Hufnagel C, et al. . 'Do well B.': design of well being monitoring systems. A study protocol for the application in autism. BMJ Open 2015;5:e007716 10.1136/bmjopen-2015-007716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lang RM, Badano LP, Mor-Avi V, et al. . Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr 2015;28:1–39. 10.1016/j.echo.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 39. Mor-Avi V, Lang RM, Badano LP, et al. . Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications. Journal of the American Society of Echocardiography 2011;24:277–313. 10.1016/j.echo.2011.01.015 [DOI] [PubMed] [Google Scholar]
- 40. Nagueh SF, Smiseth OA, Appleton CP, et al. . Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of echocardiography and the European association of cardiovascular imaging. Eur Heart J Cardiovasc Imaging 2016;17:1321–60. 10.1093/ehjci/jew082 [DOI] [PubMed] [Google Scholar]
- 41. Buss J, Havel PJ, Epel E, et al. . Associations of ghrelin with eating behaviors, stress, metabolic factors, and telomere length among overweight and obese women: preliminary evidence of attenuated ghrelin effects in obesity? Appetite 2014;76:84–94. 10.1016/j.appet.2014.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Karege F, Perret G, Bondolfi G, et al. . Decreased serum brain-derived neurotrophic factor levels in major depressed patients. Psychiatry Res 2002;109:143–8. 10.1016/S0165-1781(02)00005-7 [DOI] [PubMed] [Google Scholar]
- 43. Karege F, Bondolfi G, Gervasoni N, et al. . Low brain-derived neurotrophic factor (BDNF) levels in serum of depressed patients probably results from lowered platelet BDNF release unrelated to platelet reactivity. Biol Psychiatry 2005;57:1068–72. 10.1016/j.biopsych.2005.01.008 [DOI] [PubMed] [Google Scholar]
- 44. Shimizu E, Hashimoto K, Okamura N, et al. . Alterations of serum levels of brain-derived neurotrophic factor (BDNF) in depressed patients with or without antidepressants. Biol Psychiatry 2003;54:70–5. 10.1016/S0006-3223(03)00181-1 [DOI] [PubMed] [Google Scholar]
- 45. Krystal JH, Neumeister A. Noradrenergic and serotonergic mechanisms in the neurobiology of posttraumatic stress disorder and resilience. Brain Res 2009;1293:13–23. 10.1016/j.brainres.2009.03.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lac G, Dutheil F, Brousse G, et al. . Saliva DHEAS changes in patients suffering from psychopathological disorders arising from bullying at work. Brain Cogn 2012;80:277–81. 10.1016/j.bandc.2012.07.007 [DOI] [PubMed] [Google Scholar]
- 47. Danhof-Pont MB, van Veen T, Zitman FG. Biomarkers in burnout: a systematic review. J Psychosom Res 2011;70:505–24. 10.1016/j.jpsychores.2010.10.012 [DOI] [PubMed] [Google Scholar]
- 48. Montgomery H, Clarkson P, Barnard M, et al. . Angiotensin-Converting-Enzyme gene insertion/deletion polymorphism and response to physical training. The Lancet 1999;353:541–5. 10.1016/S0140-6736(98)07131-1 [DOI] [PubMed] [Google Scholar]
- 49. Henrion D, Benessiano J, Philip I, et al. . The deletion genotype of the angiotensin I-converting enzyme is associated with an increased vascular reactivity in vivo and in vitro. J Am Coll Cardiol 1999;34:830–6. 10.1016/S0735-1097(99)00299-5 [DOI] [PubMed] [Google Scholar]
- 50. Gard PR. The role of angiotensin II in cognition and behaviour. Eur J Pharmacol 2002;438:1–14. 10.1016/S0014-2999(02)01283-9 [DOI] [PubMed] [Google Scholar]
- 51. Thayer JF, Merritt MM, Sollers JJ, et al. . Effect of angiotensin-converting enzyme insertion/deletion polymorphism DD genotype on high-frequency heart rate variability in African Americans. Am J Cardiol 2003;92:1487–90. 10.1016/j.amjcard.2003.08.069 [DOI] [PubMed] [Google Scholar]
- 52. Hariri AR, Drabant EM, Weinberger DR. Imaging genetics: perspectives from studies of genetically driven variation in serotonin function and corticolimbic affective processing. Biol Psychiatry 2006;59:888–97. 10.1016/j.biopsych.2005.11.005 [DOI] [PubMed] [Google Scholar]
- 53. Hariri AR, Weinberger DR. Functional neuroimaging of genetic variation in serotonergic neurotransmission. Genes Brain Behav 2003;2:341–9. 10.1046/j.1601-1848.2003.00048.x [DOI] [PubMed] [Google Scholar]
- 54. McCaffery JM, Bleil M, Pogue-Geile MF, et al. . Allelic variation in the serotonin transporter gene-linked polymorphic region (5-HTTLPR) and cardiovascular reactivity in young adult male and female twins of European-American descent. Psychosom Med 2003;65:721–8. 10.1097/01.PSY.0000088585.67365.1D [DOI] [PubMed] [Google Scholar]
- 55. Epel ES, Blackburn EH, Lin J, et al. . Accelerated telomere shortening in response to life stress. Proc Natl Acad Sci U S A 2004;101:17312–5. 10.1073/pnas.0407162101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Choron G, Dutheil F, Lesage FX. Are nurses burned out? Int J Nurs Stud 2016;58:80–1. 10.1016/j.ijnurstu.2016.02.002 [DOI] [PubMed] [Google Scholar]
- 57. Hung C-I, Liu C-Y, Wang S-J, et al. . The cut-off points of the depression and somatic symptoms scale and the hospital anxiety and depression scale in detecting non-full remission and a current major depressive episode. Int J Psychiatry Clin Pract 2012;16:33–40. 10.3109/13651501.2011.617456 [DOI] [PubMed] [Google Scholar]
- 58. Julian LJ. Measures of anxiety: State-Trait anxiety inventory (STAI), Beck anxiety inventory (BAI), and hospital anxiety and depression Scale-Anxiety (HADS-A). Arthritis Care Res 2011;63:S467–72. 10.1002/acr.20561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Spiess K, Sachs G, Moser G, et al. . Psychological moderator variables and metabolic control in recent onset type 1 diabetic patients—a two year longitudinal study. J Psychosom Res 1994;38:249–58. 10.1016/0022-3999(94)90120-1 [DOI] [PubMed] [Google Scholar]
- 60. Endler NS, Parker JD. Multidimensional assessment of coping: a critical evaluation. J Pers Soc Psychol 1990;58:844–54. 10.1037/0022-3514.58.5.844 [DOI] [PubMed] [Google Scholar]
- 61. Ioannidis CA, Siegling AB. Criterion and incremental validity of the emotion regulation questionnaire. Front Psychol 2015;6:247 10.3389/fpsyg.2015.00247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Lesage F-X, Choron G, Dutheil F. Multifaceted program to reduce job strain in ICU nurses. JAMA 2019;321:1410–1. 10.1001/jama.2019.0570 [DOI] [PubMed] [Google Scholar]
- 63. Trousselard M, Dutheil F, Naughton G, et al. . Stress among nurses working in emergency, anesthesiology and intensive care units depends on qualification: a job Demand-Control survey. Int Arch Occup Environ Health 2016;89:221–9. 10.1007/s00420-015-1065-7 [DOI] [PubMed] [Google Scholar]
- 64. Luszczynska A, Scholz U, Schwarzer R. The general self-efficacy scale: multicultural validation studies. J Psychol 2005;139:439–57. 10.3200/JRLP.139.5.439-457 [DOI] [PubMed] [Google Scholar]
- 65. Li S, Zhang B, Guo Y, et al. . The association between alexithymia as assessed by the 20-item Toronto Alexithymia scale and depression: a meta-analysis. Psychiatry Res 2015;227:1–9. 10.1016/j.psychres.2015.02.006 [DOI] [PubMed] [Google Scholar]
- 66. Bagby RM, Parker JDA, Taylor GJ. The twenty-item Toronto Alexithymia scale—I. item selection and cross-validation of the factor structure. J Psychosom Res 1994;38:23–32. 10.1016/0022-3999(94)90005-1 [DOI] [PubMed] [Google Scholar]
- 67. Bagby RM, Taylor GJ, Parker JDA. The twenty-item Toronto Alexithymia scale—II. convergent, discriminant, and concurrent validity. J Psychosom Res 1994;38:33–40. 10.1016/0022-3999(94)90006-X [DOI] [PubMed] [Google Scholar]
- 68. Broadbent E, Petrie KJ, Main J, et al. . The brief illness perception questionnaire. J Psychosom Res 2006;60:631–7. 10.1016/j.jpsychores.2005.10.020 [DOI] [PubMed] [Google Scholar]
- 69. Broadbent E, Wilkes C, Koschwanez H, et al. . A systematic review and meta-analysis of the brief illness perception questionnaire. Psychol Health 2015;30:1361–85. 10.1080/08870446.2015.1070851 [DOI] [PubMed] [Google Scholar]
- 70. Wells A, Cartwright-Hatton S. A short form of the metacognitions questionnaire: properties of the MCQ-30. Behav Res Ther 2004;42:385–96. 10.1016/S0005-7967(03)00147-5 [DOI] [PubMed] [Google Scholar]
- 71. Amiel R, Lebigre F. A new rapid test for the evaluation of mental health. its use for early detections Its importance in health surveys]. Ann Med Psychol 1970;1:565–80. [PubMed] [Google Scholar]
- 72. Golubic R, May AM, Benjaminsen Borch K, et al. . Validity of electronically administered recent physical activity questionnaire (RPAQ) in ten European countries. PLoS One 2014;9:e92829 10.1371/journal.pone.0092829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Sornay-Rendu E, Boutroy S, Munoz F, et al. . Cortical and trabecular architecture are altered in postmenopausal women with fractures. Osteoporos Int 2009;20:1291–7. 10.1007/s00198-009-1008-9 [DOI] [PubMed] [Google Scholar]
- 74. Boutroy S, Bouxsein ML, Munoz F, et al. . In vivo assessment of trabecular bone microarchitecture by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab 2005;90:6508–15. 10.1210/jc.2005-1258 [DOI] [PubMed] [Google Scholar]
- 75. Stein EM, Liu XS, Nickolas TL, et al. . Abnormal microarchitecture and reduced stiffness at the radius and tibia in postmenopausal women with fractures. J Bone Miner Res 2010;25:2572–81. 10.1002/jbmr.152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Kullback S. Information theory and statistics. New York: John Wiley & Sons, 1959. [Google Scholar]
- 77. Steiger JH. Tests for comparing elements of a correlation matrix. Psychol Bull 1980;87:245–51. 10.1037/0033-2909.87.2.245 [DOI] [Google Scholar]
- 78. Vickers AJ, Altman DG. Statistics notes: analysing controlled trials with baseline and follow up measurements. BMJ 2001;323:1123–4. 10.1136/bmj.323.7321.1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Damilakis J, Adams JE, Guglielmi G, et al. . Radiation exposure in X-ray-based imaging techniques used in osteoporosis. Eur Radiol 2010;20:2707–14. 10.1007/s00330-010-1845-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Fappa E, Yannakoulia M, Pitsavos C, et al. . Lifestyle intervention in the management of metabolic syndrome: could we improve adherence issues? Nutrition 2008;24:286–91. 10.1016/j.nut.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 81. Elefteriou F, Ahn JD, Takeda S, et al. . Leptin regulation of bone resorption by the sympathetic nervous system and CART. Nature 2005;434:514–20. 10.1038/nature03398 [DOI] [PubMed] [Google Scholar]
- 82. Puissant C, Abraham P, Durand S, et al. . Reproducibility of non-invasive assessment of skin endothelial function using laser Doppler flowmetry and laser speckle contrast imaging. PLoS One 2013;8:e61320 10.1371/journal.pone.0061320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Souza EG, De Lorenzo A, Huguenin G, et al. . Impairment of systemic microvascular endothelial and smooth muscle function in individuals with early-onset coronary artery disease. Coron Artery Dis 2014;25:23–8. 10.1097/MCA.0000000000000055 [DOI] [PubMed] [Google Scholar]
- 84. Wu C, Glüer C, Lu Y, et al. . Ultrasound characterization of bone Demineralization. Calcif Tissue Int 1998;62:133–9. 10.1007/s002239900406 [DOI] [PubMed] [Google Scholar]
- 85. Büssing A, Fischer J, Haller A, et al. . Validation of the brief multidimensional life satisfaction scale in patients with chronic diseases. Eur J Med Res 2009;14:171–7. 10.1186/2047-783X-14-4-171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Büssing A, Edelhäuser F, Weisskircher A, et al. . Inner correspondence and Peacefulness with practices among participants in Eurythmy therapy and yoga: a validation study. Evidence-Based Complementary and Alternative Medicine 2011;2011:1–9. 10.1155/2011/329023 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-027058supp001.pdf (646.8KB, pdf)
bmjopen-2018-027058supp002.pdf (67.2KB, pdf)