Abstract
The human papillomavirus (HPV) vaccination, sexually transmitted infection (STI) tests, and Papanicolaou (Pap) testing rates vary by sexual orientation, which may be due in part to healthcare providers (HCP) recommending this care unevenly. Data (N=17,675) came from the Growing Up Today Study (GUTS) (N=8,039) and Nurses’ Health Study 3 (NHS3) (N=9,636). Among participants who met clinical guidelines to receive the care in question, we estimated the probability of an HCP encouraging participants to have the HPV vaccination, STI tests, or Pap test. Regardless of sexual orientation, participants whose HCP knew their sexual orientation were more likely to have been encouraged to get care compared to those whose HCP did not know the participant’s sexual orientation. Sexual minority men and women were more likely to be encouraged to obtain HPV vaccination, STI tests, and Pap test than same-gender, completely heterosexuals with no same-sex partners, with some variation by gender and the care in question. Lesbian women were the sole sexual orientation subgroup that was less likely to be encouraged to receive care (HPV vaccination and Pap test) than their same gender, completely heterosexual counterparts with no same-sex partners (odds ratio [95% confidence interval]: 0.90 [0.80–1.00] and 0.94 [0.91–0.98], respectively). The differences across sexual orientation in HCPs’ encouragement of care indicate a possible explanation for differences in utilization across sexual orientation. Across the US, HCPs under-encourage HPV vaccination, STI tests, and Pap test for all sexual orientation groups. Lesbian patients appear to be at high risk of under-encouragement for the Pap test.
INTRODUCTION
Previous studies have noted disparities in sexual and reproductive health care across sexual orientation groups [1–7]. Gay and bisexual men, as well as bisexual women, often experience higher rates of human papillomavirus (HPV) vaccination and sexually transmitted infection (STI) tests [1, 2, 4, 7]. In contrast, lesbian women have lower rates of Pap test and HPV vaccination compared to heterosexuals [1–3, 6]. For example, lesbian women have three-quarters odds of having a timely Pap test compared to heterosexual women [3]. These tests are important in the prevention and early detection of cancers. Unequal treatment and tests could place certain sexual orientation groups at outsized risk for cancer and later detection of cancer. Sexual minorities are also at increased risk of STIs compared to heterosexuals [5], which makes these tests especially important.
Health care providers’ (HCP) encouragement to obtain HPV vaccination, STI tests, and the Pap test may be particularly important for lesbian women, who have more sexual health misinformation than their heterosexual peers [6, 8]. For example, sexual minorities who were assigned female at birth (AFAB) reported misperceptions surrounding the transmission of HPV between AFAB partners, and therefore misperceived their need for HPV vaccination and the Pap test [9]. Positive patient-provider communication, HCPs offering HPV vaccination and the Pap test, and educating sexual minority patients have been found to be important mechanisms to reducing misperceptions surrounding HPV transmission between AFAB partners and increasing HPV vaccination completion and Pap tests [6, 9–12].
An HCP’s knowledge of participant’s sexual orientation could have influenced their decision to encourage specific care due to beliefs about that sexual orientation group [13]. Knowledge of a participant’s sexual orientation could also be indicative of a participant’s comfort with an HCP or the HCP taking a comprehensive sexual history, which may be more common during a visit related to sexual and reproductive health [14, 15]. In recent years, a number of professional societies have also set guidelines that HCPs should inquire about sexual orientation and be aware of specific health risks that sexual minorities experience [16–18]. An HCP knowing about sexual orientation may therefore indicate closer adherence to professional society guidelines.
However, limited research has examined whether HCPs encourage sexual minorities to have HPV vaccination, STI tests, or Pap test more or less frequently than heterosexuals. Difference in encouragement of care may represent an important mechanism to understanding disparities in sexual and reproductive health care across sexual orientation groups. In response to this gap in the literature, this paper examines whether HCPs encourage patients to receive HPV vaccination (men and women), STI tests (men and women), or the Pap test (women only) differently across sexual orientation and whether this varies based on HCP knowledge of sexual orientation.
METHODS
Study Population
Data came from the Growing Up Today Study (GUTS) (N=8,039) and Nurses’ Health Study 3 (NHS3) (N=9,636), which are ongoing, biannual, US-based longitudinal cohort studies. GUTS was established in 1996 with the children of an earlier cohort study, Nurses’ Health Study 2. The original GUTS cohort contained 27,706 individuals. NHS3 is a cohort study of nurses and nursing students that began in 2010 and continues to recruit new participants. The 2016 and eighth biannual questionnaires that this paper drew upon were both conducted online. More information on GUTS and NHS3 can be found at the following references [19, 20]. The current analysis was limited to GUTS and NHS3 men and women who gave information on sexual orientation, at least one of the outcome variables, and reported that their HCP either knew or did not know their sexual orientation. We also included only participants who were cisgender (i.e., reported that their gender identity was the same as the sex assigned at birth).
Additionally, each outcome variable had its own inclusion criteria based on whether or not the participant ever met the US Centers for Disease Control and Prevention (CDC) or US Preventive Services Task Force’s relevant guidelines. The first HPV vaccine, Gardasil, was recommended by the CDC for girls age 9 to 26 years in 2006 and boys aged 9 to 26 years in 2011 [21]. Based on this, our analytic sample for the HPV vaccination analysis was limited to women who were 26 years old or younger in 2006 and boys who were 26 years old or younger in 2011. The analytic sample for HCP encouragement of an STI test was limited to those who were sexually active or reported sexual contact, as per CDC guidelines [22]. Finally, the analytic sample for the Pap test analysis included women who at any point in their life had met the US Preventive Services Task Force’s guidelines for Pap tests, which center around age and sexual history [23, 24]. The study protocol was approved by the Institutional Review Boards of the Brigham and Women’s Hospital and the Harvard T.H. Chan School of Public Health.
Measures
Sexual Orientation
Detailed information about sexual orientation was collected in GUTS and NHS3 using an item adapted from the Minnesota Adolescent Health Survey [25], which asked about feelings of attraction and identity with six mutually exclusive response options (completely heterosexual, mostly heterosexual, bisexual, mostly homosexual, completely homosexual, and unsure). Mostly homosexual and completely homosexual were combined into a single group, gay/lesbian, due to small sample size. The question of sexual attraction and identity was combined with a question about the sex of sexual partners to create an additional sexual minority group (completely heterosexuals with same-sex partners). In total, there are five sexual orientation groups: completely heterosexual with no same-sex partners, completely heterosexual with same-sex partners, mostly heterosexual, bisexual, and gay/lesbian. Sexual orientation groups were modelled using the most recent information on sexual orientation (GUTS 2016 and NHS3’s fifth biannual questionnaire). If data were missing, then sexual orientation was imputed from prior questionnaires.
HCP Knows Sexual Orientation
Participants were asked if their primary care provider (PCP) knew their sexual orientation on the 2016 GUTS questionnaire and NHS3’s eighth biannual questionnaire with: yes, not sure, no, and I don’t have a PCP, as possible response options. Participants reporting that they were not sure or did not have a PCP were excluded. We refer to this variable as “HCP knows sexual orientation” throughout this manuscript because PCPs are a type of HCP and to reduce confusion with outcome variables centered around HCP encouragement of care.
Outcomes: Encouragement of HPV vaccination, STI test, Pap test
Participants were asked on the 2016 GUTS and NHS3’s eighth biannual questionnaire “whether a health care provider ever encouraged you to get any of the following care:” STI tests, HPV vaccination, or pelvic exam/Pap test (for women only). Responses for each included no, yes, and not sure. Participants who reported they were “not sure” were treated as missing. Although participants from NHS3 were nurses, these questions specifically referred to their experiences as patients.
Covariates
Previous research has found that sexual and reproductive health care varies by race, age, and region, so we included these measures as potential confounders, measured as follows: age (22 to 54 years), race/ethnicity (non-Hispanic white, another race/ethnicity), and region of residence (Northeast or International, Midwest, West, South) [26, 27]. Additionally, differences may exist across cohorts that would influence the results. To this end, we included cohort (GUTS, NHS3) as a covariate for women. Cohort was not included as a covariate for men because there were no men in NHS3. Sensitivity analyses were conducted using lifetime sexual partner as a covariate (0 to 6 or more). If data were missing for potential confounders, they were imputed from previous questionnaire years. Data that remained missing were multiply imputed using fully conditional statements and 20 stacked data sets.
Statistical Analysis
Descriptive statistics were produced and stratified by sexual orientation and gender. We used generalized estimating equations to account for sibling clusters from GUTS, with nurses from NHS3 included as their own cluster. Analysis for each outcome variable was restricted to those that met clinical guidelines to receive the care in question, as well as stratified by gender (men, women). We calculated the odds ratios (OR) and confidence interval (CI) for each sexual orientation and gender category of an HCP encouraging participants to have HPV vaccination, STI tests, or a pelvic exam/Pap test, with same gender, completely heterosexual participants with no same-sex partners as the reference group. Models also included HCPs knowing the participant’s sexual orientation and were adjusted for confounders (age, race, region of residence, cohort). To further explore the association between sexual orientation, HCP knowing the participant’s sexual orientation, and encouragement of the care in question, we interacted sexual orientation and HCP knowing participant’s sexual orientation for men and women on all three outcome variables. Only significant interaction results are presented. All analyses were conducted in SAS 9.4.
RESULTS
Table 1 shows descriptive statistics of the sample stratified by sexual orientation and gender. The average age at time of questionnaire response was 35 for women and 29 for men. The majority of respondents identified as non-Hispanic white and from the Northeast or Midwest. Of the 17,552 participants in our sample, 78% (N=13,795) identified as completely heterosexual with no same-sex partners, 3.0% (N=522) identified as completely heterosexual with same-sex partners, 13.8% (N=2,447) identified as mostly heterosexual, and 2.3% (N=400) and 2.9% (N=511) as bisexual and gay/lesbian. Overall, 56.2% of all women and 78.2% of men reported that an HCP had never encouraged them to have the HPV vaccine, and 66.5% of men had never been encouraged to have an STI test, yet only 5.7% of women reported never being encouraged to have a Pap test.
Table 1:
Sociodemographic characteristics and outcome variables in relation to sexual orientation in a cohort of U.S. women and men aged 20 to 54 (N=17,675)
| Women | ||||||||||
| % (N), unless noted | Total (N=15,572) | Completely heterosexual with no same-sex partners(N=12,159) | Completely heterosexual with same-sex partners(N=472) | Pa | Mostly heterosexual(N=2,215) | Pa | Bisexual(N=377) | Pa | Lesbian(N=349) | Pa |
| Age (range: 22 to 54), mean (SD)b | 35.2 (7.6) | 35.6 (7.7) | 35.0 (6.4) | 0.0366 | 33.1 (6.5) | <.0001 | 32.9 (7.3) | <.0001 | 35.9 (8.0) | 0.50 |
| Race/ethnicityc | ||||||||||
| Non-Hispanic White | 91.9 (14168) | 92.2(11092) | 90.8 (423) | 0.28 | 91.4 (2001) | 0.24 | 91.7 (342) | 0.75 | 89.3 (310) | 0.06 |
| Geographic regionc | ||||||||||
| Northeast | 28.0 (4235) | 27.1 (3199) | 26.6 (122) | <.0001 | 31.6 (689) | <.0001 | 31.2 (116) | <.0001 | 32.0 (109) | 0.0008 |
| Midwest | 30.4 (4595) | 32.1 (3779) | 21.8 (100) | 25.5 (556) | 22.0 (82) | 22.9 (78) | ||||
| West | 20.5 (3100) | 19.0 (2240) | 27.2 (125) | 25.1 (546) | 28.5 (106) | 24.3 (83) | ||||
| South | 21.2 (3209) | 21.8 (2569) | 24.4 (112) | 17.8 (389) | 18.3 (68) | 20.8 (71) | ||||
| Cohortd | ||||||||||
| GUTS | 38.1 (5936) | 34.1 (4150) | 48.3 (228) | <.0001 | 54.5 (1206) | <.0001 | 57.0 (215) | <.0001 | 39.3 (137) | 0.0468 |
| NHS3 | 61.9 (9636) | 65.9 (8009) | 51.7 (244) | 45.6 (1009) | 43.0 (162) | 60.7 (212) | ||||
| HCP knows sexual orientationc | 87.7(13653) | 90.2 (10964) | 89.6 (423) | 0.69 | 80.3 (1779) | <.0001 | 50.9 (192) | <.0001 | 84.5 (295) | 0.0005 |
| HCP encouraged care with: | ||||||||||
| HPV vaccinationc | 43.8 (6560) | 41.4 (4843) | 46.4 (211) | 0.0344 | 55.9 (1185) | <.0001 | 55.0 (197) | <.0001 | 37.2 (124) | 0.13 |
| STI testc | 51.1 (7637) | 47.0 (5488) | 64.8 (295) | <.0001 | 68.4 (1458) | <.0001 | 66.0 (233) | <.0001 | 49.2 (163) | 0.42 |
| 94.3 (14600) | 94.2 (11380) | 95.1 (447) | 0.39 | 96.0 (2116) | 0.0005 | 94.1 (351) | 0.96 | 88.7 (306) | <.0001 | |
| Men | ||||||||||
| Total (N=2,103) | Completely heterosexual with no same-sex partners(N=1,636) | Completely heterosexual with same-sex partners(N=50) | Pa | Mostly heterosexual(N=232) | Pa | Bisexual(N=23) | Pa | Gay(N=162) | Pa | |
| 29.0 (3.5) | 29.0 (3.5) | 30.6 (2.8) | 0.0002 | 28.7 (3.7) | 0.33 | 28.8 (3.6) | 0.84 | 29.1 (3.4) | 0.73 | |
| Race/ethnicityc | ||||||||||
| Non-Hispanic White | 93.2 (1945) | 93.9(1526) | 94.0 (47) | 0.97 | 93.5 (214) | 0.81 | 82.6 (19) | 0.0276 | 87.4 (139) | 0.002 |
| Geographic regionc | ||||||||||
| Northeast | 32.8 (687) | 33.3 (543) | 30.0 (15) | 0.52 | 29.4 (68) | 0.0189 | 26.1 (6) | 0.66 | 34.2 (55) | 0.36 |
| Midwest | 30.5 (640) | 31.4 (512) | 26.0 (13) | 29.0 (67) | 26.1 (6) | 26.1 (42) | ||||
| West | 19.8 (414) | 18.2 (296) | 26.0 (13) | 26.8 (62) | 26.1 (6) | 23.0 (37) | ||||
| South | 16.9 (355) | 17.2 (280) | 18.0 (9) | 14.7 (34) | 21.7 (5) | 16.8 (27) | ||||
| HCP knows sexual orientationc | 72.0 (1514) | 74.6 (1221) | 68.0 (34) | 0.29 | 55.6 (129) | <.0001 | 26.1 (6) | <.0001 | 76.5 (124) | 0.59 |
| HCP encouraged care with: | ||||||||||
| HPV vaccinationc | 21.8 (419) | 19.4 (290) | 14.9 (7) | 0.44 | 24.0 (52) | 0.12 | 35.0 (7) | 0.08 | 44.7 (63) | <.0001 |
| STI testc | 33.5 (689) | 29.5 (472) | 34.7 (17) | 0.43 | 32.0 (72) | 0.44 | 47.8 (11) | 0.06 | 73.1 (117) | <.0001 |
SD standard deviation, HCP health care provider, ref reference, HPV human papillomavirus, STI sexually transmitted infection
Completely heterosexual with no same-sex partners is reference group;
Independent t-test used to generate p values;
Chi-square tests used to generate p-values;
Information on cohort distribution is available for women only since there are no men in NHS3.
Table 2 contains results from the generalized estimating equations analysis. Mostly heterosexual women, as well as bisexual and gay men, had higher odds of being encouraged to have the HPV vaccine than people of their same sex who were completely heterosexual with no same-sex partners. Women who reported that they were bisexual, mostly heterosexual, or completely heterosexual with same-sex partners had higher odds of being encouraged to have an STI test than completely heterosexual women with no same-sex partners, as were gay and bisexual men compared to completely heterosexual men with no same-sex partners. Mostly heterosexual women had higher odds of being encouraged to have a Pap test than completely heterosexual women with no same-sex partners (OR=1.01, 95% CI=1.00–1.03).
Table 2:
Adjusted* odds ratios of health care providers encouraging HPV vaccination, STI testing, and pelvic exam/Pap test use in relation to sexual orientation in a cohort of U.S. women and men (N=17,675)
| Women (N=15,572) |
Men (N=2,103) |
|
|---|---|---|
| OR (95% Cl) | OR (95% Cl) | |
| Encouraged to have HPV vaccine among women (N=9,462) and men (N=1,369)a | ||
| Sexual orientation | ||
| Completely heterosexual with no same-sex partners (ref) | 1.00 | 1.00 |
| Completely heterosexual with same-sex partners | 1.02 (0.94, 1.11) | 0.86 (0.37, 2.04) |
| Mostly heterosexual | 1.06 (1.03, 1.10) | 1.23 (0.97, 1.57) |
| Bisexual | 1.04 (0.97, 1.12) | 2.05 (1.33, 3.18) |
| Gay/Lesbian | 0.90 (0.80, 1.00) | 2.20 (1.77, 2.74) |
| HCP knows sexual orientation | 1.10 (1.06, 1.15) | 1.45 (1.19, 1.77) |
| Encouraged to have STI test among women (N=13,907) and men (N=1,930)a | ||
| Sexual orientation | ||
| Completely heterosexual with no same-sex partners (ref) | 1.00 | 1.00 |
| Completely heterosexual with same-sex partners | 1.27 (1.19, 1.36) | 1.12 (0.76, 1.66) |
| Mostly heterosexual | 1.27 (1.23, 1.32) | 1.15 (0.93, 1.41) |
| Bisexual | 1.30 (1.21, 1.40) | 1.81 (1.18, 2.76) |
| Gay/Lesbian | 1.01 (0.91, 1.12) | 2.32 (2.07, 2.60) |
| HCP knows sexual orientation | 1.17 (1.12, 1.23) | 1.53 (1.30, 1.80) |
| Encouraged to have pelvic exams/Pap tests among women (N=15,355)a | ||
| Sexual orientation | ||
| Completely heterosexual with no same-sex partners (ref) | 1.00 | -- |
| Completely heterosexual with same-sex partners | 1.00 (0.98, 1.02) | -- |
| Mostly heterosexual | 1.01 (1.00, 1.03) | -- |
| Bisexual | 1.01 (0.98, 1.04) | -- |
| Gay/Lesbian | 0.94 (0.91, 0.98) | -- |
| HCP knows sexual orientation | 1.05 (1.04, 1.07) | -- |
Lesbian women were the sole sexual minority subgroup that had lower odds of being encouraged to receive the care in question—lesbian women were less likely to be encouraged by an HCP to have the HPV vaccine or a Pap test than completely heterosexual women with no same-sex partners. In sensitivity analyses, the associations between sexual orientation and encouragement for care existed even after adjusting for factors that could change perceived need of care such as number of lifetime sexual partners.
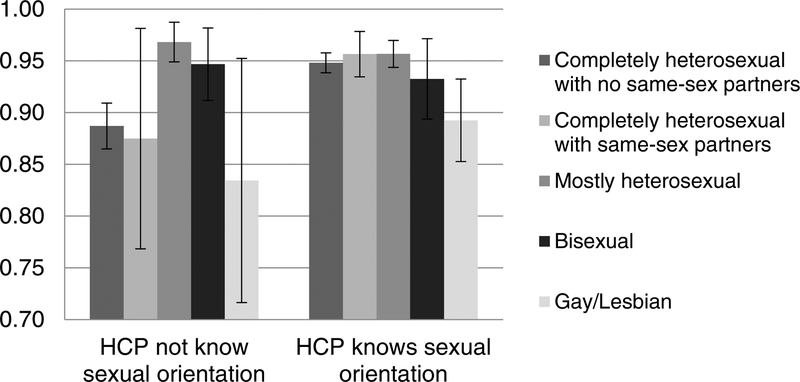
HCP knowledge of the participant’s sexual orientation increased the odds that an HCP would encourage all three outcomes studied for all sexual orientation groups. HCP knowledge of sexual orientation also modified the association between sexual orientation and encouragement of the Pap test. In other words, there was no difference in encouragement to have a Pap test across almost all sexual orientation groups among women whose HCP knew their sexual orientation. The exception was among lesbian women whose HCP knew their sexual orientation yet remained less likely to be encouraged to have Pap tests than heterosexual women with no same-sex partners whose HCP knew their sexual orientation (see Figure 1).
Figure 1: Predicted Probability of HCP Encouraging Pap Test Among Women (N=15,355).
Note: Figure 1 uses data from GUTS and NHS3 women participants who have ever been eligible for a pap test. Predicted probabilities were obtained by extracting a single imputed data set from the multiply imputed data. They are based off a regression adjusted for age, race/ethnicity, region, and cohort and calculated using the “output pred” statement in SAS. P-value of the interaction term between sexual orientation and HCP knowledge is <.001.
DISCUSSION
Previous research has found disparities in reproductive health care across sexual orientation groups among women and men. Bisexual women, as well as gay and bisexual men, often experience higher rates of HPV vaccination and STI testing, and lesbian women have lower rates of Pap testing and possibly HPV vaccination compared to heterosexual women [1–5, 28, 29].
In this study, HCP encouragement of HPV vaccination, STI tests, and the Pap test varied by patient’s sexual orientation among women and men, such that bisexual and gay men and mostly heterosexual women had higher odds of being encouraged to have the HPV vaccine than people of their same gender who were completely heterosexual with no same-sex partners. Bisexual, mostly heterosexual, and completely heterosexual women with same-sex partners had lower odds of being encouraged to have an STI test than completely heterosexual women with no same-sex partners, as were gay and bisexual men. Notably, lesbian women were less likely to be encouraged to have an HPV vaccine and Pap test than completely heterosexual women with no same-sex partners, even though they met clinical guidelines to receive the care in question. These findings are in line with current research on patterns of utilization for HPV vaccination, STI tests, and the Pap test across sexual orientation and suggest that differences in HCP encouragement may contribute to differences in utilization [1–3].
HCP’s encouragement of care is important to patients actually receiving such care, particularly for sexual minorities [6, 10, 11, 30]. Therefore, it is a potential pathway through which differences in receipt of care may occur. Oftentimes, there can be misinformation surrounding the need for sexual and reproductive care among sexual minorities [31, 32]. For example, early qualitative research found that approximately 10% of lesbian women were told by HCPs that the Pap test was not necessary because they did not have sex with men [32]. Young sexual minority women frequently do not view information regarding STIs as relevant to their lives [33]. This perception has resulted in lesbian women frequently having less of a perceived need of the Pap test or STI tests than heterosexual women, even though they are also at risk of HPV, cervical cancer, and STIs [8, 9, 34]. This misinformation makes HCPs’ less frequent encouragement for Pap tests among lesbian women particularly important.
We also found that the HCP’s knowledge of an individual’s sexual orientation increased the likelihood of men and women being encouraged to have the care in question regardless of sexual orientation. This finding indicates that HCP knowledge of participant’s sexual orientation may be indicative of higher quality care or of HCPs taking a comprehensive sexual history rather than potential bias toward sexual minorities driving differences in encouragement of care. Previous research found that sexual minority women whose HCP knew their sexual orientation reported greater satisfaction with the care and were more likely to bring up sexual health needs [35]. However, even when an HCP knew the participant’s sexual orientation and was potentially providing higher quality care or sexual or reproductive health-centered care, lesbian women did not have as high a probability of being encouraged to have a Pap test as other women. This finding is particularly important given that lesbian women have a well-documented lower likelihood of having a routine Pap test [3]. Additionally, we found that among those who met clinical guidelines to receive the care in question, completely heterosexual women with same-sex partners, mostly heterosexual women, and bisexual women, as well as bisexual and gay men, still had higher odds of being encouraged to have STI tests or HPV vaccination than heterosexuals with no same-sex partners, regardless of whether or not the HCP knew the participant’s sexual orientation. This finding indicates there may be cases where a provider assumed a patient’s sexual orientation, but it was not overtly discussed. Additionally, although we focused on gender and bias surrounding sexual orientation for why differences in encouragement of care may exist, there may be reasons that were due to sex-linked biology for which we were unable to test.
The outcomes studied here—HPV vaccines, STI tests, and Pap test—are important in the prevention and early detection of cancers. Although certain sexual minority groups were more likely to receive this care than completely heterosexuals, they remain under-utilized by the general population. Moreover, because this analysis was limited to those who said they had a primary care doctor, it should be noted that a little over one-half of all women and three-quarters of men who had a PCP said they had never been encouraged by an HCP to have an HPV vaccine and that 67% of men had never been encouraged to have an STI test. This is the first study that we know of to look at provider encouragement of sexual and reproductive health care.
Our results show that providers should be encouraging HPV vaccines, STI tests, and the Pap test more frequently than they do. Provider training should emphasize that all people who meet clinical guidelines to receive a type of care are encouraged to do so, regardless of sexual orientation. Providers should also educate patients of all sexual orientations on the need for HPV vaccines, STI tests, and Pap tests. Finally, our results suggest that providers may be encouraging some sexual minorities to receive care more frequently than others. Providers should self-reflect on any unconscious bias that may result in them encouraging some sexual minority subgroups (e.g., bisexual men and women, gay men) to receive STI tests or HPV vaccines more than heterosexual groups.
Study Limitations
Although this study uses novel data, it does have limitations. Primarily, the sample consisted of people who were connected to the medical field, including those who were nurses, children of nurses, and those who had a PCP. There was also limited racial/ethnic and class diversity in the samples, which may limit findings to the broader population. Additionally, we were not able to match whether the HCP who knew the patient’s sexual orientation was the HCP who did or did not encourage the care in question. However, because these were part of routine, preventive care, they should have been addressed at any primary care appointment regardless of provider knowledge of patient’s sexual orientation. We also did not have information on the anal Pap test for men and whether the participants were encouraged to have an HIV test or a more general STI test. Our measure of Pap test also included encouragement of pelvic exams, which may have slightly changed the findings. Finally, previous meta-analyses have found inaccuracies in survey participants reporting Pap tests [36]. It was also possible that participants misremembered their HCP encouraging them to have a Pap test or that they had an STI test at the same time as a Pap test and did not realize it.
CONCLUSIONS
HCP encouragement of care is important to the receipt of care—patients may be uncomfortable bringing up that they need such care or may misunderstand their care needs and risks [6, 8, 9]. The differences across sexual orientation in HCPs’ encouragement of care indicated a possible explanation for differences in utilization across sexual orientation. Across the US, HCPs under-encourage HPV vaccines, STI tests, and Pap test for all sexual orientation groups. Lesbian patients appear to be at high risk of under-encouragement for Pap tests. Future research should seek to understand why HCPs encourage certain sexual orientation groups to obtain HPV vaccines, STI tests, and Pap tests more than other groups, with particular attention paid to variation between the various heterosexual groups (no same-sex partners, same-sex partners, mostly heterosexual). Qualitative research would be particularly helpful to understanding these patterns, as well as elucidating barriers that prevent HCPs from encouraging care. Research should also examine the role of an HCP’s gender and sexual orientation in encouraging care.
HPV human papillomavirus, STI sexually transmitted infection, HCP health care provider, ref reference
Adjusted for age, race/ethnicity, region, and cohort (women only); multiple imputation used for missing covariates
Sample sizes vary due to restricting sample to include only those who meet eligibility criteria for the care outcome being tested
Highlights.
Participants whose HCP knew their sexual orientation were encouraged to get care more Sexual minorities except lesbians were more likely to receive encouragement for care Lesbian patients appear to be at high risk of under-encouragement for the Pap test
Acknowledgments:
This work was supported by National Cancer Institute, National Institutes of Health T32CA009001; the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health R01HD057368 and R01HD066963; the Maternal and Child Health Bureau, Health Resources and Services Administration T71MC00009 and T76MC00001; American Cancer Society MRSG CPHPS 130006; GLMA’s Lesbian Health Fund; the National Cancer Institute, National Institutes of Health K01 CA234226–01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Charlton BM, et al. , Reproductive health screening disparities and sexual orientation in a cohort study of U.S. adolescent and young adult females. Journal of Adolescent Health, 2011. 49(5): p. 505–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agénor M, et al. , Sexual orientation and sexual health services utilization among women in the United States. Preventive Medicine, 2017. 95: p. 74–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Solazzo A, Gorman B, and Denney J, Cancer screening utilization among U.S. women: how mammogram and Pap test use varies among heterosexual, lesbian, and bisexual women. Population Research & Policy Review, 2017. 36(3): p. 357–377. [Google Scholar]
- 4.Charlton B, et al. , Sexual orientation disparities in human papillomavirus vaccination in a longitudinal cohort of U.S. males and females. LGBT Health, 2017. 4(3): p. 202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Everett BG, Sexual orientation disparities in sexually transmitted infections: examining the intersection between sexual identity and sexual behavior. Archives of sexual behavior, 2013. 42(2): p. 225–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agénor M, et al. , Sexual orientation identity disparities in awareness and initiation of the human papillomavirus vaccine among U.S. women and girls: A national survey. Annals of Internal Medicine, 2015. 163(2): p. 99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agénor M, et al. , Sexual orientation identity disparities in human papillomavirus vaccination initiation and completion among young adult US women and men. Cancer Causes & Control, 2016. 27(10): p. 1187–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Power J, McNair R, and Carr S, Absent sexual scripts: lesbian and bisexual women’s knowledge, attitudes and action regarding safer sex and sexual health information. Culture, Health & Sexuality, 2009. 11(1): p. 67–81. [DOI] [PubMed] [Google Scholar]
- 9.Agénor M, et al. , Human papillomavirus risk perceptions among young adult sexual minority cisgender women and nonbinary individuals assigned female at birth. Perspectives on Sexual and Reproductive Health, 2019. 51(1): p. 27–34. [DOI] [PubMed] [Google Scholar]
- 10.Apaydin KZ, et al. , Three-dose HPV vaccine completion among sexual and gender minority young adults at a Boston community health center. Vaccine, 2018. 36(32, Part B): p. 4897–4903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nadarzynski T, et al. , Men who have sex with men who do not access sexual health clinics nor disclose sexual orientation are unlikely to receive the HPV vaccine in the UK. Vaccine, 2018. 36(33): p. 5065–5070. [DOI] [PubMed] [Google Scholar]
- 12.Tabaac AR, Benotsch EG, and Barnes AJ, Mediation models of perceived medical heterosexism, provider-patient relationship quality, and cervical cancer screening in a community sample of sexual minority women and gender nonbinary adults. LGBT Health, 2019. 6(2): p. 77–86. [DOI] [PubMed] [Google Scholar]
- 13.Reuel FM, et al. , From bias to bisexual health disparities: attitudes toward bisexual men and women in the United States. LGBT Health, 2014. 1(4): p. 309–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bjorkman M and Malterud K, Being lesbian – does the doctor need to know? Scandinavian Journal of Primary Health Care, 2007. 25(1): p. 58–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Polek CA, Hardie TL, and Crowley EM, Lesbians’ disclosure of sexual orientation and satisfaction with care. Journal of Transcultural Nursing, 2008. 19(3): p. 243–249. [DOI] [PubMed] [Google Scholar]
- 16.Knight DA and Jarrett D, Preventive health care for women who have sex with women. Am Fam Physician, 2017. 95(5): p. 314–321. [PubMed] [Google Scholar]
- 17.American College of Obstetrics and Gynecology, Health care for lesbians and bisexual women, in Committee Opinion No. 525. 2012. [DOI] [PubMed]
- 18.Frankowski BL, Sexual orientation and adolescents. Pediatrics, 2004. 113(6): p. 1827. [DOI] [PubMed] [Google Scholar]
- 19.Bao Y, et al. , Origin, methods, and evolution of the three Nurses’ Health Studies. Am J Public Health, 2016. 106(9): p. 1573–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Growing Up Today Study. 2019; Available from: https://nhs2survey.org/gutswordpress/.
- 21.Centers for Disease Control and Prevention, Quadrivalent human papillomavirus vaccine recommendations of the Advisory Committee on Immunization Practices (ACIP) in MMWR. 2007. [PubMed]
- 22.Centers for Disease Control and Prevention. STD & HIV screening recommendations. 2017; Available from: https://www.cdc.gov/std/prevention/screeningreccs.htm.
- 23.Preventive US Services Task Force. Cervical cancer: screening. 2018; Available from: https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/cervical-cancer-screening2.
- 24.American Cancer Society. History of ACS recommendations for the early detection of cancer in people without symptoms. 2018; Available from: https://www.cancer.org/health-care-professionals/american-cancer-society-prevention-early-detection-guidelines/overview/chronological-history-of-acs-recommendations.html.
- 25.Remafedi G, et al. , Demography of sexual orientation in adolescents. Pediatrics, 1992. 89(4 Pt 2): p. 714–21. [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Use of Pap smears among women aged 18 and over, by selected characteristics: United States, selected years 1987–2015. 2017; Available from: https://www.cdc.gov/nchs/data/hus/2017/071.pdf. [Google Scholar]
- 27.Centers for Disease Control and Prevention, National and state vaccination coverage among adolescents aged 13–17 years--United States, 2011. MMWR Morb Mortal Wkly Rep, 2012. 61(34): p. 671–7. [PubMed] [Google Scholar]
- 28.Agenor M, et al. , Sexual orientation identity disparities in human papillomavirus vaccination initiation and completion among young adult US women and men. Cancer Causes Control, 2016. 27(10): p. 1187–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldberg SK, Reese BM, and Halpern CT, Teen pregnancy among sexual minority women: results from the National Longitudinal Study of Adolescent to Adult Health. Journal of Adolescent Health, 2016. 59(4): p. 429–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Everett BG, et al. , Do sexual minorities receive appropriate sexual and reproductive health care and counseling? Journal of Women’s Health, 2018. 28(1): p. 53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Greene MZ, et al. , Health care-related correlates of cervical cancer screening among sexual minority women: an integrative review. 2018. p. 550–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marrazzo J, et al. , Papanicolaou test screening and prevalence of genital human papillomavirus among women who have sex with women. American Journal of Public Health, 2001. 91(6): p. 947–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Magee JC, et al. , Sexual health information seeking online: A mixed-methods study among lesbian, gay, bisexual, and transgender young people. Health Education & Behavior, 2011. 39(3): p. 276–289. [DOI] [PubMed] [Google Scholar]
- 34.Charlton BM, et al. , Influence of hormonal contraceptive use and health beliefs on sexual orientation disparities in papanicolaou test use. American Journal of Public Health, 2014. 104(2): p. 319–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mosack KE, Brouwer AM, and Petroll AE, Sexual identity, identity disclosure, and health care experiences: is there evidence for differential homophobia in primary care practice? Women’s Health Issues, 2013. 23(6): p. e341–e346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rauscher GH, et al. , Accuracy of self-reported cancer-screening histories: a meta-analysis. Cancer Epidemiology Biomarkers & Prevention, 2008. 17(4): p. 748–757. [DOI] [PubMed] [Google Scholar]