Abstract
Aim:
The aim of this study is to assess the influence of different implant placement techniques to improve primary implant stability (PIS) in the low-density bone.
Materials and Methods:
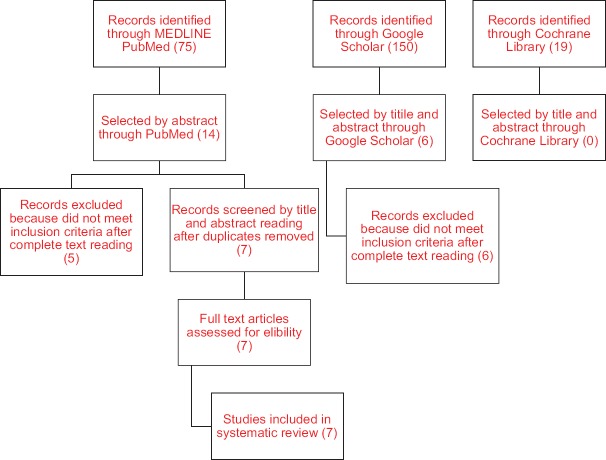
Citations published in English and those available in full text were searched from electronic databases (PubMed and Google Scholar) from the year 2000–2017 by which 75 manuscripts were revealed. After applying inclusion and exclusion criteria, seven were selected for the present review. The whole process was conducted by the following preferred reporting items for systematic reviews and meta-analyses guidelines.
Results:
The measurement of primary stability showed significant correlations with different bone densities and with implant outcome; however, these two parameters have not been investigated at the same time frequently. Of the seven manuscripts, three discussed standard drilling protocol, two used undersized drilling, one used guided drilling, and one compared standard drilling with undersized drilling. Several intraoperative methods of jaw bone-density assessment were reported, and resonance frequency analysis, periotest, and insertion torque values were used to quantify PIS.
Conclusion:
The use of undersized drilling has proven advantageous for increasing initial implant stability in the low-density bone. Although the PIS may be lower, the secondary implant stability is found to be correlated to acceptable values.
Keywords: Bone density, guided drilling, osseointegration, primary implant stability
INTRODUCTION
Primary implant stability (PIS) is a critical factor that determines the long-term success of dental implants. PIS is defined as the absence of mobility in the bone bed after the implant has been placed.[1] According to the Glossary of Prosthodontic Terms, Ninth Edition, PIS is a contributing factor to the mechanical stabilization of a dental implant during the healing phase.[2]
An implant exhibiting minimum micromotion after surgical placement and during the initial healing phase has greater longevity with reduced bone loss. To achieve predictable success with dental implants, PIS is required. Low values of PIS may increase the risk of early failure to osseointegrate, while good initial stability provides better conditions for success since it allows for smaller micromotions between the implant and the bone.[3]
The quality of bone plays a major role in the initial bone-to-implant contact. Trabecular bone is less dense compared with the cortical bone. In certain areas of the jaws (particularly the maxillary posterior region) and in certain condition (e.g., osteoporosis), the bone may have trabecular morphology.[4] This, in turn, will affect the degree of firmness with which the implant has been placed, thus influencing PIS. Other factors that influence PIS are length and diameter of the implant, implant design, micromorphology of the implant surface, insertion technique, and congruity between the implant and the surrounding bone.[5]
Implant stability can be further divided into primary and secondary stability. Primary stability is mostly derived from mechanical engagement with cortical bone and the absence of mobility in the bone bed on the insertion of the implant and depends on the quantity and quality of bone, surgical technique, and implant design. Secondary stability depends on bone formation and remodeling at the implant-to-bone interface and is influenced by the implant surface and the wound healing time. The former is a requirement for successful secondary stability; the latter dictates the time to functional loading.
Several classifications for bone density have been recommended. According to Misch[6] in 1988, bone quality can be classified into four types (D1–D4) based on macroscopic and trabecular characteristics. D4 bone is finely trabecular and often lacks cortical bone. This type of bone is commonly found in the posterior maxilla, shows a Hounsfield unit (HU) reading between 150 and 350 units, exhibits the lowest implant-to-bone contact, and has the maximum failure rate of the four types of bone. Implant failure rates range from approximately 3% after insertion of implants into bone Types 1, 2, or 3, to approximately 35% after insertion into bone Type 4.[7] It has been observed that PIS is lower in Type 4 bone than in types 1-3.[8] Various techniques have been used to improve the PIS in type 4 bone.
Friberg et al. recommended the use of undersized drilling to optimize implant stability in less dense bone.[9] Summers, (1994) proposed the use of a bone condensing technique using condensers after a pilot drill to displace the bone at the periphery of the cavity.[10] Fully guided surgery has been suggested, using templates to translate the precise positioning into clinical reality and to allow for exact, guided preparation of the implant site. This affects the regions with poor bone qualities and may lead to smaller micromotions between the implant and the bone. Other methods use cylindrical implants instead of tapered implants and the additional incorporation of surface treatments. The bone quality of the receptor site influences the primary stability of implants, and bone density. Hence, the present systematic review was conducted to evaluate and compare different techniques that are presently in use to enhance the primary stability of implants placed in regions of poor bone mineral density. In addition, a critical review of methods of measuring PIS has also been undertaken.
MATERIALS AND METHODS
Search strategy
A MEDLINE (PubMed), Google Scholar, and Cochrane library search were conducted to identify all articles that investigated PIS immediately after implant placement in regions of compromised bone density from January 2000 to July 31, 2017. The search strategy included appropriate changes in the key words following the syntax rules of each database. Since bone density has been also referred to as bone quality, the following search parameters were used: “assessment of bone quality in human jaw bone,” “surgical protocol,” “adapted surgical protocol,” “insertion torque (IT),” “resonance frequency analysis,” and “jaw bone quality.” This systematic review was performed in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement.
The inclusion criteria were observational clinical studies on patients who had dental implants placed in regions with poor bone mineral density, including conventional procedure and any adapted protocol. The exclusion criteria were unspecified bone mineral density, lack of comment on bone quality, nonhuman studies, and studies in which PIS had not been objectively defined.
Of the 75 retrieved articles, those reporting of comparisons of PIS among cases with poor bone mineral density were selected. The selected articles discussed varying protocols for surgical placement. After the review of titles and abstracts, 20 articles were chosen for further study. Finally, seven articles were shortlisted for the final review, as the rest did not meet the inclusion criteria.
Figure 1 provides a PRISMA flowchart of the identification and selection of the study. A summary of the selected articles is presented in Table 1.
Figure 1.
Selection of articles
Table 1.
Studies on primary implant stability
| Author and year | Implant and manufacturer | Implant size | Implant number | Region | Bone type | Technique of evaluation of stability | Result of evaluation | Insertion technique | Other findings |
|---|---|---|---|---|---|---|---|---|---|
| Pozzi et al., 2012[11] | 57 nobel speedy replace implants and 24 nobel speedy groovy (PS1) | Not specified | 29 axial and 42 straight | Atrophied maxillary posterior | Not specified | IT | 40-50 Ncm | Underprepared osteotomy | |
| Alghamdi et al., 2011[5] | Straumann (standard plus) (PS2) | 4.1 mm × 12 mm | 26 | Posterior maxilla and mandible | Lekholm and Zarb 3 and 4 according to radiographic assessment and drilling resistance | IT and RFA | IT - 35.19±4.79 ISQ - 68.58±4.81 | Undersized drilling | Comparison of standard osteotomy in normal bone and undersized osteotomy in bone with low bone mineral density |
| Herekar et al., 2014[12] | Nobel replace select (Nobel Biocare) and GSIII/TSIII (Osstem) | Not specified | 20 | Not specified | D4 | RFA | 60±4.15 | Standard drilling protocol | Comparison of primary and secondary ISQ of the different types of bone |
| Alsaadi et al., 2007[8] | Mark III TiUnitet implants (Branemark systems, Nobel Biocare, (PS3) | Not specified | 47 | Not specified | Lekholm and Zarb 4 | Periotest | 3.28 - crestal, 5.49 - middle, 8.38 - Apical | Standard drilling protocol | |
| Makary et al., 2011[13] | Tapered Screw-Vent MTX, Zimmer Dental | 4.1 or 4.7 mm diameter | 9 | D4 | IT | 40.22 Ncm | Standard drilling protocol | Trephine drill used initially to obtain biopsy to determine the bone type | |
| Anitua et al., 2015[14] | BTI implants (BTI, Vitoria, Spain) | 8.5 mm-long | Lekholm and Zarb 4 | IT | 34.84±2.38 Ncm | Socket under-preparation by 1 mm | |||
| O’Sullivan 2004[15] | Branemark Standard implants (Nobel Biocare AB, Gothenburg, Sweden), Branemark SystemR Mk IV implant (Nobel Biocare AB) | Not specified | 9 (4 Standard implant and 5 Mk IV implant) | Not specified | Lekholm and Zarb 4 | IT RFA | 14.0 and 12.3 Ncm respectively 5.6 and 5.86 KHz | IT increases due to inherent cutting property of implant | Inducing greater stresses in cortical bone |
IT: Insertion torque, ISQ: Implant stability quotient, RFA: Resonance frequency analysis
RESULTS AND DISCUSSION
Clinical strategies to increase the implant success rates in areas of reduced bone quality include the use of longer or wider-diameter implants, the use of implants with roughened surfaces, undersizing the osteotomy followed by the placement of a self-tapping implant that is 1–2 mm wider than the initial preparation, and the use of osteocompressive techniques.[16] These techniques are intended to increase bone-to-implant contact.
The osteotome technique is mainly designed for gradual densification of the osteotomy in both the axial and lateral direction,[17] which improves bone quality. The molding of the bone around the site of implant placement is carried out by the sequential compaction of the bone.[18] The densification of bone allows for greater physical interlocking between bone and the implant which results in higher degrees of primary stability.
The placement of implants in undersized sockets to increase primary stability is controversial. Compressive forces are set up along the implant-to-bone interface, which leads to a mismatch between the hole and the implant diameter; forces are then evenly distributed along the length of the implant-to-bone interface.[19] This technique also allows for remodeling around the implant to increase the bone-to-implant contact, which also increases secondary stability.[14]
The converse view states that, when implants were placed with excessive torque (compressive forces), a greater amount of resorption was observed due to the creation of microfractures.[20,21] In addition, an in vitro study by Jimbo et al.[22] has shown that loss in biomechanical implant stability was noted due to interfacial remodeling or necrotic changes of the surrounding bone.
Möhlhenrich et al. have compared different surgical techniques for implant site preparation in different artificial bone densities (decreasing density D2, D3, and D4). On the evaluation of conventional free-hand drilling, fully guided procedures, and condensing, the authors found that condensing resulted in significantly better PIS compared with conventional and guided procedures when using short implants. In low-density bone, wide-diameter and longer implants improved stability.[21]
In another study, Falisi et al.[23] evaluated five different implant placement techniques (piezosurgery, conventional, under-preparation, bone compaction, and osteodistraction) in 10 in vitro samples and found that all methods were interchangeable; none had a major advantage over the other. Xing conducted a study on 16 patients with poor bone quality and found that there was no statistically significant difference between a conventional drilling protocol and osteotome technique using IT and resonance frequency analysis (RFA) over varying time intervals.[16]
The surgical protocol followed in the study conducted by Anitua et al.[14] adapted the implant socket preparation so that sufficient primary stability to permit osseointegration of the dental implant could be established. The underpreparation of the socket was increased according to the decrease in the quality of the hosting bone, reaching a maximum value of 1.2 mm. In the D4 type of bone, an IT of 34.84 ± 2.38 Ncm was obtained, but an adequate IT (≥30 Ncm) was not obtainable in bone with a density <400 HU.
O'Sullivan et al.[15] used two different types of implants and proposed varied implant placement protocols to assess implant stability. Standard Brånemark System® implants (Nobel Biocare AB, Gothenburg, Sweden) were inserted with a technique designed to enhance primary stability.
Cavallaro et al. and Engelke et al. concluded that changes in the drilling protocol are necessary to improve PIS for different bone densities.[24,25] This includes an undersized osteotomy and to submerge the implant to allow for osseointegration.
The value of PIS allows a comparison of the PIS at various time intervals and in different bone types. The commonly used methods are measurement of the IT, RFA, and Periotest. High values of IT, RFA, percussion energy response, or removal torque indicate good stability, while lower values indicate less than optimum stability.
The force used to insert a dental implant is called IT.[26] It can be assessed by electronic devices incorporated with the physiodispenser or with a torque gauge incorporated with manual ratchets.[27] A disadvantage of this method is that IT varies depending on the cutting properties of the implant and the presence of fluid at the osteotomy site. However, the method does provide some information about the energy used when placing the implant. Its main disadvantage is that, like the surgeon's perception, IT measurements can only be assessed at the time of implant placement; torque measurements cannot be repeated during follow-up appointments and hence, longitudinal data cannot be obtained.
The RFA technique is fundamentally a bending test in which a minute tilting force, on the bone-implant system, is applied by stimulating a transducer. It is a nonintrusive diagnostic technique that measures implant stability at various points in time using vibration and principles of analysis of structural form. The advantage of RFA is that it can be evaluated at various time intervals.
Choosing an appropriate stability measuring tool depending on local anatomic factors enables a more accurate estimation and better prediction of implant success. Studies have shown that RFA is the only method that can detect significantly different effects of various factors on primary stability. Further, it has been reported that RFA may be difficult to interpret in the evaluation of implant stability in softer bone density. RFA and IT measure the implant stability at different levels of the bone-implant interface.[16] RFA is dependent on the cortical thickness of the bone, while IT quantifies trabecular bone quality.[16] Thus, RFA may show varying values in low-density bone depending on cortical bone density.
Of the articles included in the study, three studies used implants with anodized surfaces (thickened layer of titanium dioxide coated on the surface),[8,11,12] study by O'Sullivan et al. used sandblasted and acid-etched implants,[15] study by Alghamdi et al. used sandblasted implants,[5] study by Anitua et al. used implants chemically treated with calcium ions,[14] and study by Makary et al. used implants with machined surfaces.[13] The studies using implants with different surface treatments showed high PIS. In contrast, the study by O'Sullivan et al.,[15] in which Standard Nobel Biocare implants were used, exhibited low PIS. This implies that to attain high PIS in low-density bone, it is always recommended to use implants with some surface treatment, as opposed to machined implants.
In order to improve primary stability, the use of implants with a thread design is preferred. Of the articles included in the current review, all the implants had a threaded design. The Nobel Speedy implants are designed to provide increased primary stability since they allow for underpreparation.[11] The Straumann Standard Plus implants provide a cutting surface.[5] On the other hand, the Brånemark System Mk III implants are indicated for medium to hard bone and are provided with three cutting chambers. Thus, in poor-quality bone, an implant type that allows for osseodensification by the compression of the bone is preferred. Straumann Standard Plus implants were used by Alghamdi et al.[5] in an under-prepared socket by placing a 4.1-mm diameter implant in a 2.8-mm osteotomy site to achieve improved IT.
In cases of low bone mineral density, the initial evaluation must include both IT and RFA since the RFA has been found difficult to interpret. The IT will give an initial assessment of PIS while further evaluation can be conducted by RFA to assess secondary implant stability and in turn, evaluate time to implant loading.
CONCLUSION
The use of undersized drilling has proven advantageous for increasing initial implant stability in the low-density bone. Although the primary implant stability may be lower, the secondary implant stability is found to be correlated to acceptable values.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Javed F, Romanos GE. The role of primary stability for successful immediate loading of dental implants. A literature review. J Dent. 2010;38:612–20. doi: 10.1016/j.jdent.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 2.The glossary of prosthodontic terms: Ninth edition. J Prosthet Dent. 2017;117:e1–105. doi: 10.1016/j.prosdent.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 3.Glauser R, Sennerby L, Meredith N, Rée A, Lundgren A, Gottlow J, et al. Resonance frequency analysis of implants subjected to immediate or early functional occlusal loading Successful vs failing implants. Clin Oral Implants Res. 2004;15:428–34. doi: 10.1111/j.1600-0501.2004.01036.x. [DOI] [PubMed] [Google Scholar]
- 4.Misch C.E. 3rd Edition. Mosby, St. Louis: 2007. Contemporary Implant Dentistry. [Google Scholar]
- 5.Alghamdi H, Anand PS, Anil S. Undersized implant site preparation to enhance primary implant stability in poor bone density: A prospective clinical study. J Oral Maxillofac Surg. 2011;69:e506–12. doi: 10.1016/j.joms.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 6.Misch CE. Bone classification, training keys to implant success. Dent Today. 1989;8:39–44. [PubMed] [Google Scholar]
- 7.Jaffin RA, Berman CL. The excessive loss of Branemark fixtures in type IV bone: A 5-year analysis. J Periodontol. 1991;62:2–4. doi: 10.1902/jop.1991.62.1.2. [DOI] [PubMed] [Google Scholar]
- 8.Alsaadi G, Quirynen M, Michiels K, Jacobs R, van Steenberghe D. A biomechanical assessment of the relation between the oral implant stability at insertion and subjective bone quality assessment. J Clin Periodontol. 2007;34:359–66. doi: 10.1111/j.1600-051X.2007.01047.x. [DOI] [PubMed] [Google Scholar]
- 9.Friberg B, Ekestubbe A, Mellström D, Sennerby L. Brånemark implants and osteoporosis: A clinical exploratory study. Clin Implant Dent Relat Res. 2001;3:50–6. doi: 10.1111/j.1708-8208.2001.tb00128.x. [DOI] [PubMed] [Google Scholar]
- 10.Summers RB. A new concept in maxillary implant surgery: The osteotome technique. Compendium. 1994;15:152–154-6. 158. [PubMed] [Google Scholar]
- 11.Pozzi A, Sannino G, Barlattani A. Minimally invasive treatment of the atrophic posterior maxilla: A proof-of-concept prospective study with a follow-up of between 36 and 54 months. J Prosthet Dent. 2012;108:286–97. doi: 10.1016/S0022-3913(12)60178-4. [DOI] [PubMed] [Google Scholar]
- 12.Herekar M, Sethi M, Ahmad T, Fernandes AS, Patil V, Kulkarni H. A correlation between bone (B), insertion torque (IT), and implant stability (S): BITS score. J Prosthet Dent. 2014;112:805–10. doi: 10.1016/j.prosdent.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 13.Makary C, Rebaudi A, Mokbel N, Naaman N. Peak insertion torque correlated to histologically and clinically evaluated bone density. Implant Dent. 2011;20:182–91. doi: 10.1097/ID.0b013e31821662b9. [DOI] [PubMed] [Google Scholar]
- 14.Anitua E, Alkhraisat MH, Piñas L, Orive G. Efficacy of biologically guided implant site preparation to obtain adequate primary implant stability. Ann Anat. 2015;199:9–15. doi: 10.1016/j.aanat.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 15.O’Sullivan D, Sennerby L, Jagger D, Meredith N. A comparison of two methods of enhancing implant primary stability. Clin Implant Dent Relat Res. 2004;6:48–57. doi: 10.1111/j.1708-8208.2004.tb00027.x. [DOI] [PubMed] [Google Scholar]
- 16.Xing Y, Khandelwal N, Petrov S, Drew HJ, Mupparapu M. Resonance frequency analysis (RFA) and insertional torque (IT) stability comparisons of implants placed using osteotomes versus drilling techniques: A preliminary case study. Quintessence Int. 2015;46:789–98. doi: 10.3290/j.qi.a34453. [DOI] [PubMed] [Google Scholar]
- 17.Tabassum A, Meijer GJ, Walboomers XF, Jansen JA. Biological limits of the undersized surgical technique: A study in goats. Clin Oral Implants Res. 2011;22:129–34. doi: 10.1111/j.1600-0501.2010.02016.x. [DOI] [PubMed] [Google Scholar]
- 18.Pai UY, Rodrigues SJ, Talreja KS, Mundathaje M. Osseodensification – A novel approach in implant dentistry. J Indian Prosthodont Soc. 2018;18:196–200. doi: 10.4103/jips.jips_292_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Toyoshima T, Tanaka H, Ayukawa Y, Howashi M, Masuzaki T, Kiyosue T, et al. Primary stability of a hybrid implant compared with tapered and cylindrical implants in an ex vivo model. Clin Implant Dent Relat Res. 2015;17:950–6. doi: 10.1111/cid.12205. [DOI] [PubMed] [Google Scholar]
- 20.Trisi P, Todisco M, Consolo U, Travaglini D. High versus low implant insertion torque: A histologic, histomorphometric, and biomechanical study in the sheep mandible. Int J Oral Maxillofac Implants. 2011;26:837–49. [PubMed] [Google Scholar]
- 21.Möhlhenrich SC, Kniha K, Heussen N, Hölzle F, Modabber A. Effects on primary stability of three different techniques for implant site preparation in synthetic bone models of different densities. Br J Oral Maxillofac Surg. 2016;54:980–6. doi: 10.1016/j.bjoms.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 22.Jimbo R, Tovar N, Anchieta RB, Machado LS, Marin C, Teixeira HS, et al. The combined effects of undersized drilling and implant macrogeometry on bone healing around dental implants: An experimental study. Int J Oral Maxillofac Surg. 2014;43:1269–75. doi: 10.1016/j.ijom.2014.03.017. [DOI] [PubMed] [Google Scholar]
- 23.Falisi G, Severino M, Rastelli C, Bernardi S, Caruso S, Galli M, et al. The effects of surgical preparation techniques and implant macro-geometry on primary stability: An in vitro study. Med Oral Patol Oral Cir Bucal. 2017;22:e201–6. doi: 10.4317/medoral.21286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cavallaro J, Jr, Greenstein B, Greenstein G. Clinical methodologies for achieving primary dental implant stability: The effects of alveolar bone density. J Am Dent Assoc. 2009;140:1366–72. doi: 10.14219/jada.archive.2009.0071. [DOI] [PubMed] [Google Scholar]
- 25.Engelke W, Müller A, Decco OA, Rau MJ, Cura AC, Ruscio ML, et al. Displacement of dental implants in trabecular bone under a static lateral load in fresh bovine bone. Clin Implant Dent Relat Res. 2013;15:160–5. doi: 10.1111/j.1708-8208.2011.00338.x. [DOI] [PubMed] [Google Scholar]
- 26.Cehreli MC, Kökat AM, Comert A, Akkocaoǧlu M, Tekdemir I, Akça K. Implant stability and bone density: Assessment of correlation in fresh cadavers using conventional and osteotome implant sockets. Clin Oral Implants Res. 2009;20:1163–9. doi: 10.1111/j.1600-0501.2009.01758.x. [DOI] [PubMed] [Google Scholar]
- 27.Goswami MM, Kumar M, Vats A, Bansal AS. Evaluation of dental implant insertion torque using a manual ratchet. Med J Armed Forces India. 2015;71:S327–32. doi: 10.1016/j.mjafi.2013.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]