Abstract
Osteoarthritis (OA) imposes a significant burden to the person, the health system and the community. Models of Care (MoCs) drive translation of evidence into policy and practice and provide a platform for health system reform. The Victorian MoC for OA of the hip and knee was developed following a best-practice framework, informed by best-evidence and iterative cross-sector consultation, including direct consumer consultation. Governance and external expert advisory committees consisting of local OA care champions facilitated the development and consultation processes. The MoC outlines key components of care, care that is not recommended, and suggests phased implementation strategies. This paper describes the MoC development process and lessons learned.
Abstract
L'arthrose est un lourd fardeau pour les personnes, le système de santé et la communauté. Les modèles de soin (MdS) permettent de transposer les données en politique ou en pratique, en plus d'offrir une plateforme pour la réforme du système de santé. Le MdS de Victoria pour l'arthrose de la hanche et du genou a été développé en suivant un cadre de pratique exemplaire, en tenant compte des meilleures données et en menant des consultations intersectorielles itératives, notamment auprès de la clientèle. Le développement et la consultation ont été facilités par des comités de gouvernance et d'experts-conseils externes formés de champions locaux des soins pour l'arthrose. Le MdS présente les éléments clés des soins, relève les soins non recommandés et propose des stratégies de mise en œuvre par phases successives. Cet article décrit le processus de développement du MdS ainsi que les leçons qui en ont été tirées.
Background
Osteoarthritis (OA) is recognized as a major health issue in Australia and across the globe (Cross et al. 2014) and an Australian National Health Priority Area since 2002. In Australia, approximately 2.2 million people live with OA, often co-morbid with other chronic health conditions. Projections estimate that this will rise to 3.1 million Australians by 2030, with the highest prevalence expected in people aged 55 years and over (Ackerman et al. 2018). The expected sharp rise in global prevalence is attributed to population aging, obesity and an increasing prevalence of risk factors for chronic health conditions (Kopec et al. 2016).
OA affects people from early middle-age onwards and symptoms associated with OA can have a profound impact on the person's ability to socialise and maintain regular work, which has significant downstream consequences for national workforce productivity and human capital (Ackerman et al. 2015; Arthritis and Osteoporosis Victoria 2013; Schofield et al. 2016; Schofield et al. 2015). In 2012, OA accounted for 41% of the $9.51 billion (AUD) spent on musculoskeletal conditions in Australia (Arthritis and Osteoporosis Victoria 2013), with a large proportion of total cost attributed to hip and knee joint replacement surgery. The lifetime risk of requiring total knee or hip joint replacement surgery has risen substantially in the 10-year period between 2003 and 2013 internationally (Ackerman et al. 2017a; Ackerman et al. 2017b). These trends will have significant implications for health service delivery quality and efficiency in Australia and other countries. In the state of Victoria, Australia, the direct healthcare costs attributed to OA care are expected to exceed $693 million (AUD) in 2030 (2015 dollars) (Ackerman et al. 2016).
Like other chronic health conditions, management of OA may be complex and require components of care to be delivered by different parts of the health system at different times over a protracted period. This approach to care collides with the historic structure and functionality of healthcare systems in high-income economies, which have had better capacity for responding to acute or episodic health needs, particularly in the context of hospital services (i.e., curative healthcare), rather than care delivery and self-management support over long periods (i.e., rehabilitative healthcare) (Briggs and Dreinhöfer 2017). As health systems internationally come to terms with the need for a paradigm shift from curative to rehabilitative healthcare, policy makers, health funders and administrators, service delivery organizations, clinicians, and consumers seek tools to support these complex transitions. Here, system-level Models of Care (MoCs) offer one such option (Briggs et al. 2016a).
An MoC is an evidence- and consultation-informed policy or framework that outlines the optimal manner in which condition-specific care should be made available and delivered to consumers within a local health system (Briggs et al. 2014). It articulates what care is appropriate, with a focus on high-value care, and how it could ideally be delivered. The implementation focus of MoCs is a substantial and important extension from clinical guidelines, which inadequately support implementation of evidence to practice (March et al. 2010; Nelson et al. 2014). Recent reviews have examined the current state of OA MoCs globally (Allen et al. 2016; Dziedzic et al. 2016; Lim et al. 2016). The aim of this paper is to describe the development of the Victorian MoC for OA of the hip and knee – a process to translate evidence and experience into a system-wide plan and summarize the lessons learned.
Objective
Recognizing the burden of disease of OA in Victoria, Australia, the Department of Health and Human Services (DHHS) commissioned the development of an MoC in 2015 under the auspices of the Victorian Musculoskeletal Clinical Leadership Group (CLG). The Musculoskeletal CLG, established in 2013, consists of a multidisciplinary group of clinicians, consumers, and policy makers who represent a range of peak bodies tasked with providing advice to government regarding musculoskeletal health service delivery issues. “Peak” bodies refer to those that undertake a national or jurisdictional leadership, advocacy or representation role, such as professional societies or non-government consumer organizations.
Setting
The setting for this initiative was the Victorian health system, comprising all levels of the system – primary care and community care, hospital services and private health settings. In Australia, health services are delivered through a mixed public and private model. Primary care services are administered by the Commonwealth government, while hospital services are predominantly managed by state and territory governments. Importantly, the focus of the MoC was on the broader health system, not just components of the system for which the DHHS has responsibility. While recognizing the burden of OA at all joints, the focus of the MoC was hip and knee joint OA as the majority of the prevalence of OA and health expenditure relates to these sites and the associated population-level burden of disease is high and increasing (Cross et al. 2014).
Methods
Governance
The DHHS and St Vincent's Hospital, Melbourne (SVHM), provided financial support to appoint two part-time project leads from October 2015 to March 2017 (AMB, CJP). A project governance sub-committee, supported by a DHHS secretariat, was established comprising CLG members, project leads and representatives from SVHM, to oversee the management of the project and facilitate a reporting line to the CLG. The subcommittee was responsible for monitoring milestones, reporting and overseeing contractual obligations. Once the project commenced, an External Expert Advisory Committee (EEAC) was established to provide independent clinical and health service advice and facilitate consultation across the life of the project (n=25 multidisciplinary members identified as local OA clinical/service champions). The EEAC members ascribed to a Terms of Reference, which included the requirement for them to act as liaisons with their professional/peak organizations.
Development process
The MoC was developed following a best-practice framework (Briggs et al. 2016b). This Framework was developed as a global initiative through the Global Alliance for Musculoskeletal Health of the Bone and Joint Decade. It provides an empirically defined, best-practice approach to development, implementation and evaluation of MoCs and policy for non-communicable conditions, with a focus on musculoskeletal health. It was informed by 93 individuals across 30 countries and is publicly supported by 54 peak international organizations.
The MoC development process comprised four sequential phases, underpinned by the guiding principles of i) continuous consultation; ii) continuous incorporation of best available evidence as it became available; and iii) alignment with existing and emerging relevant policy, frameworks or position statements.
Consultation process
Each phase of development involved consultation.
Phase 1
In phase 1, an electronic survey was disseminated to 17 peak Victorian and national bodies, public and private health services, Victorian Primary Health Networks, four consumer organizations and Victorian government departments. The survey was open-ended, allowing respondents (n=75) to describe key issues in OA care (Box 1).
Box 1. Components of the phase 1 consultation survey.
What is currently working well in OA service delivery in Victoria?
What needs improvement in OA service delivery in Victoria?
- What are the current barriers to consumers accessing/receiving:
- The right care for their OA?
- Care at the right time for their OA?
- Care from the right team for their OA?
Phase 1 also involved an initial scoping of consumers' views on OA care (data not shown).
These phase 1 consultation data were analyzed deductively using a summative content-analysis approach (Hsieh and Shannon 2005), consistent with the method reported by Cunningham and Wells (2017) to develop an initial framework for the MoC, which outlined important components of the MoC.
Phase 2
The phase 1 initial framework for the MoC was presented to the EEAC for initial discussion at an inception workshop in April 2016. At the conclusion of this workshop, the following outcomes were achieved:
A defined scope for the MoC, including a population definition and continuum of care boundaries.
- A defined structure for the MoC with foci of:
- What care should be delivered?
- What care should not be delivered?
- How should care be delivered?
Establishment of topic working groups to develop content.
Consultation with EEAC members continued for a period of five months, during which time the components of the MoC were drafted and refined. Content was developed by topic working groups comprised of the project leads and EEAC members. All content related to components of care needed to be supported by evidence (local data, clinical trial, systematic review or clinical guideline), rather than opinion-based, consistent with the development Framework we adopted (Briggs et al. 2016b). Over this period, EEAC members responded to two rounds of an online survey, powered by SurveyMonkey® (California, US), to provide comment on the components of the MoC (contextual information; guiding principles and standards of care; components of care including non-pharmacological care, pharmacological care and surgical care; strategies for care delivery; and background). These consultation-based data were used to further refine the MoC. Between the surveys, meetings with individual EEAC members or teleconferences with groups of EEAC members were held to further discuss and refine components on the MoC. At the conclusion of the five-month consultation and development cycle, seven clinical issues remained to be discussed and resolved at a final face-to-face workshop with all EEAC members in September 2016.
Concurrently, a consumer organization was commissioned to undertake an independent, in-depth consultation with consumers across Victoria regarding health service issues related to OA care (n=36; 75% residents of metropolitan Melbourne; 25% residents of rural or remote Victoria). The outcomes of this consultation have been published elsewhere (Nolan et al. 2016). A recent systematic review of consumers' needs in OA care was also used as a primary evidence source for the MoC (Wluka et al. 2016).
The outcome of phase 2 was the development of a full draft MoC.
Phase 3
In phase 3, the full draft of the MoC was distributed to the same stakeholder groups as phase 1 for comment using an online survey to collect quantitative and qualitative data. Specifically, respondents were asked to review each component of the MoC and provide a nominal response ranking of their level of agreement with the content (Table 1). Where respondents either did not support the content or had suggested changes, they were asked to provide free-text responses to explain their selection. These responses were reviewed to further refine the MoC. Over this 3-month consultation, 43 submissions were received and analyzed quantitatively (Table 1) and qualitatively using a content analysis method (Hsieh and Shannon 2005). EEAC members acted as liaisons for consultations with the peak bodies they represented.
Table 1.
Quantitative feedback from the phase 3 consultation, presented as proportions (%) by nominal response category
| Draft MoC section | Component | Support content in its current form | Support content, but changes required | Do not support content in its current form | Not relevant to my expertise or organization |
|---|---|---|---|---|---|
| Part 1: Introduction | Context description | 88.0 | 12.0 | 0 | 0 |
| Part 2A: Context of the MoC | Structure, guiding principles, approach to OA care and diagnosis | 84.0 | 16.0 | 0 | 0 |
| Part 2B: Components of care (what care) | Non-pharmacologic care | 80.0 | 20.0 | 0 | 0 |
| Pharmacologic care | 68.0 | 16.0 | 4.0 | 12.0 | |
| Surgical care | 64.0 | 20.0 | 4.0 | 12.0 | |
| Care that should not be delivered | 64.0 | 16.0 | 4.0 | 16.0 | |
| Part 2C: Enablers to care delivery (how to deliver care) | Building peoples' capacity to more effectively participate in care | 92.0 | 8.0 | 0 | 0 |
| Models of health service delivery | 92.0 | 8.0 | 0 | 0 | |
| Information and communication technology | 84.0 | 12.0 | 0 | 4.0 | |
| Health policy and planning | 92.0 | 8.0 | 0 | 0 | |
| Part 3: Background | The case for change | 92.0 | 8.0 | 0 | 0 |
Phase 4
Following the phase 3 consultation, the MoC was revised again and re-distributed to peak Victorian and national bodies for final comment and endorsement in phase 4.
Outcome: Final drafting and public support
The MoC describes appropriate assessment and key components of care for OA, including: non-pharmacologic and non-surgical care for all (education, reassurance and support for appropriate self-management, physical activity and exercise, weight loss/nutrition management, management of persistent pain based on contemporary pain science); pharmacologic care; and total joint replacement surgery (Victorian Musculoskeletal Clinical Leadership Group 2018). Knee arthroscopy, as a primary intervention, and the routine use of magnetic resonance imaging (MRI) are specifically not recommended. Enablers to care delivery are summarized in Figure 1. Each enabler is supported by suggested implementation strategies within the MoC. The MoC is publicly supported by 20 peak organizations.
Figure 1.
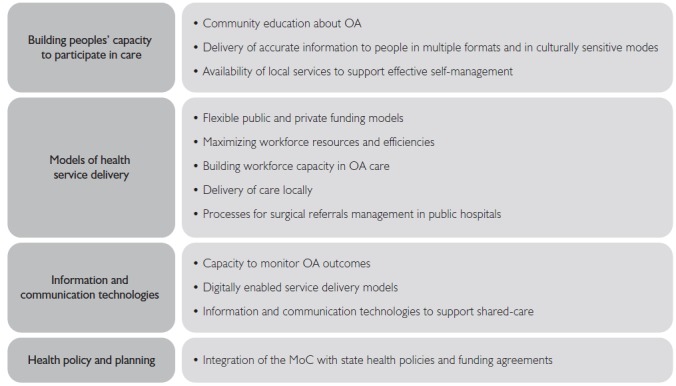
Enablers to OA care delivery in Victoria
Discussion
The Victorian MoC for OA of the hip and knee describes an evidence and consultation-informed blueprint for OA care delivery for the state of Victoria, supported by local stakeholders. Importantly, the MoC aligns with existing state health policy, MoCs in other jurisdictions (Department of Health [Western Australia) 2010; NSW Agency for Clinical Innovation 2012) and nations (Allen et al. 2016), recent national initiatives aimed at optimizing care for OA (Arthritis Australia 2014; Australian and New Zealand College of Anaesthetists 2010; Royal Australian College of General Practitioners 2009; Therapeutic Guidelines 2017) and contemporary OA guidelines and clinical care standards (Australian Commission on Safety and Quality in Health Care 2017; March et al. 2010; Nelson et al. 2014; Stoffer et al. 2015), building momentum for national service improvement. A seminal review of OA MoCs highlights international progress in developing and implementing innovative service models that prioritize first-line, high-value management strategies for OA, such as exercise, weight loss and support for self-management; appropriate pain management; and pathways that facilitate timely and appropriate selection of suitable candidates for joint replacement surgery (Allen et al. 2016). That review also identified the need to contextualize service models according to the local environment. The Victorian MoC incorporates these components of care (i.e., “what care”). and outlines strategies to implement care in the Victorian context (i.e., "how to deliver the care’).
The MoC now provides a platform for the Victorian health sector to collaboratively engage in system and service reform to improve care for people with hip or knee OA. While supported by the DHHS, the MoC is not intended as implementation responsibility for state government, but rather an enabler for all participants in the health system to work in partnership towards health service improvements. In this context, it is affirming that a multidisciplinary EEAC and 20 peak organizations have publicly supported the MoC.
The development process was guided by an existing Framework, which ensured an appropriate, inclusive and transparent approach to development (Briggs et al. 2016b). We suggest this same best-practice Framework be used to guide implementation activities for the MoC under the stewardship of a representative implementation advisory group. Our ability to comply with all the recommendations in the best-practice Framework was limited by project resourcing and timeline restrictions. For example, while the use of online consultations was efficient, a greater face-to-face presence would have been preferred as a mechanism to facilitate engagement by external stakeholders, particularly those in rural areas and to expand the scope of the consumer consultation.
The establishment of a governance framework for the project provided context about the project to both internal (e.g., government) and external stakeholders and an explicit description of project management. The governance subcommittee provided an important structure to the project, ensuring reporting responsibilities and milestones were met and a formal mechanism for troubleshooting established. The establishment of the EEAC was similarly a critical component of the MoC development process. This group provided independent, expert advice on components of care, assisted with content development and facilitated consultation with, and endorsement by, peak bodies. Engaging nominees from peak organisations from inception of the project ensured sustained engagement with the development process and will likely facilitate the implementation stage.
Engaging a consumer organization to lead and undertake targeted consumer consultation minimized any possible or perceived bias and allowed project leads to focus on other components of work. We recommend that future endeavours allocate a greater proportion of funds to consumer consultation activities and plan these budgets with consumer organizations to ensure feasibility.
While engagement with the DHHS was facilitated by a secretariat role, the progress of the project was impacted by a change of government and the dynamic nature of strategic priorities. The process of developing the MoC and use of the development and implementation Framework can be applied across conditions and across settings. While some modifications in processes will be important to align with local sociocultural factors, the use of evidence and phased consultation is broadly transferable.
Acknowledgements
The Victorian Department of Health and Human Services and St Vincent's Hospital Melbourne are acknowledged for financially supporting this project under the auspices of the Victorian Musculoskeletal Clinical Leadership Group. The members of the External Expert Advisory Group are gratefully acknowledged for their time and expertise: Associate Professor Ilana Ackerman, Mr. Nigel Broughton, Ms. Robyn Blackmore, Dr. Stephen Bunker, Professor Flavia Cicuttini, Ms. Lisa Collison, Professor Richard de Steiger, Associate Professor Michelle Dowsey, Dr. Chris Fong, Ms. Naomi Gandler, Dr. Naomi Harris, Professor Rana Hinman, Clinical Associate Professor Malcolm Hogg, Ms. Naomi Kubina, Clinical Associate Professor Keith Lim, Clinical Associate Professor Susan Liew, Dr. Helen Lindner, Dr. Anita Munoz, Ms. Genevieve Nolan, Dr. Vanessa J Rice, Dr. Debra Schulz, Dr. Janice Sheringham, Dr. Jane Simms, Mr. Bill Suen, and Mr. Jason Wallis. Musculoskeletal Australia is acknowledged for independently conducting the consumer consultation to inform the Model of Care. Tim Buckley, Barbara Whyte and Sharon Christie (Department of Health and Human Services, Victoria) are acknowledged for their role as project secretariat. AMB is supported by a fellowship awarded by the Australian National Health and Medical Research Council (#1132548).
Contributor Information
Andrew M. Briggs, Professor, School of Physiotherapy and Exercise Science, Curtin University, Perth, St Vincent's Hospital, Melbourne, Australia.
Carolyn J. Page, Advanced Musculoskeletal Physiotherapist, St Vincent's Hospital, Melbourne, Australia.
Bridget R. Shaw, Past President Australian Physiotherapy Association, (Victorian Branch), Melbourne, Australia.
Andrea Bendrups, Rheumatologist and medical educator, Australian Rheumatology Association, University of Melbourne, Department of Medicine, Royal Melbourne Hospital, Melbourne, Australia.
Kathleen Philip, Chief Allied Health Advisor, Department of Health and Human Services, Victoria, Australia.
Belinda Cary, Physiotherapy Manager, St Vincent's Hospital, Melbourne, Australia.
Peter F. Choong, Orthopaedic Surgeon, St Vincent's Hospital, Professor of Surgery, University of Melbourne, Department of Surgery, Melbourne, Australia.
References
- Ackerman I.N., Bohensky M.A, de Steiger R., Brand C.A., Eskelinen A., Fenstad A.M. et al. 2017a. “Substantial Rise in the Lifetime Risk of Primary Total Knee Replacement Surgery for Osteoarthritis from 2003 to 2013: An International, Population-Level Analysis.” Osteoarthritis and Cartilage 25(4): 455–61. 10.1016/j.joca.2016.11.005. [DOI] [PubMed] [Google Scholar]
- Ackerman I.N., Bohensky M.A., de Steiger R., Brand C.A., Eskelinen A., Fenstad A.M. et al. 2017b. “Lifetime Risk of Primary Total Hip Replacement Surgery for Osteoarthritis from 2003–2013: A Multi-National Analysis Using National Registry Data.” Arthritis Care & Research 69(11): 1659–67. 10.1002/acr.2319.7 [DOI] [PubMed] [Google Scholar]
- Ackerman I.N., Bohensky M.A., Pratt C., Gorelik A., Liew D. 2016. Counting the Cost: Part 1 – Healthcare Costs. The Current and Future Burden of Arthritis. Sydney: Arthritis Australia. [Google Scholar]
- Ackerman I.N., Bucknill A., Page R.S., Broughton N.S., Roberts C., Cavka B. et al. 2015. “The Substantial Personal Burden Experienced by Younger People with Hip or Knee Osteoarthritis.” Osteoarthritis and Cartilage 23(8): 1276–84. 10.1016/j.joca.2015.04.008. [DOI] [PubMed] [Google Scholar]
- Ackerman I.N., Pratt C., Gorelik A., Liew D. 2018. “Projected Burden of Osteoarthritis and Rheumatoid Arthritis in Australia: A Population-Level Analysis.” Arthritis Care & Research 70(6): 877–83. 10.1002/acr.23414. [DOI] [PubMed] [Google Scholar]
- Allen K.D., Choong P.F., Davis A.M., Dowsey M.M., Dziedzic K.S., Emery C. et al. 2016. “Osteoarthritis: Models for Appropriate Care across the Disease Continuum.” Best Practice & Research: Clinical Rheumatology 30(3): 503–35. 10.1016/j.berh.2016.09.003. [DOI] [PubMed] [Google Scholar]
- Arthritis and Osteoporosis Victoria. 2013. A Problem Worth Solving. The Rising Cost of Musculoskeletal Conditions in Australia. Melbourne, Australia: Author. [Google Scholar]
- Arthritis Australia. 2014. Time to Move: Osteoarthritis. Sydney: Arthritis Australia. [Google Scholar]
- Australian and New Zealand College of Anaesthetists. 2010. National Pain Strategy. Melbourne: Faculty of Pain Medicine. [Google Scholar]
- Australian Commission on Safety and Quality in Health Care (ACSQHC). 2017. Osteoarthritis of the Knee Clinical Care Standard. Sydney, Australia: Author. [Google Scholar]
- Briggs A.M., Chan M., Slater H. 2016a. “Models of Care for Musculoskeletal Health: Moving towards Meaningful Implementation and Evaluation across Conditions and Care Settings.” Best Practice & Research: Clinical Rheumatology 30(3): 359–74. 10.1016/j.berh.2016.09.00.9 [DOI] [PubMed] [Google Scholar]
- Briggs A.M., Jordan J.E., Jennings M., Speerin R., Chua J., Bragge P. et al. 2016b. A Framework to Evaluate Musculoskeletal Models of Care. Cornwall: Global Alliance for Musculoskeletal Health of the Bone and Joint Decade.
- Briggs A.M., Jordan J.E., Jennings M., Speerin R., Bragge P., Chua J. et al. 2017. “Supporting the Evaluation and Implementation of Musculoskeletal Models of Care: A Globally Informed Framework for Judging Readiness and Success.” Arthritis Care & Research 69(4): 567–77. 10.1002/acr.22948. [DOI] [PubMed] [Google Scholar]
- Briggs A.M., Towler S.C., Speerin R., March L.M. 2014. “Models of Care for Musculoskeletal Health in Australia: Now More Than Ever to Drive Evidence into Health Policy and Practice.” Australian Health Review 38(4): 401–05. 10.1071/AH14032. [DOI] [PubMed] [Google Scholar]
- Cross M., Smith E., Hoy D., Nolte S., Ackerman I., Fransen M. et al. 2014. “The Global Burden of Hip and Knee Osteoarthritis: Estimates from the Global Burden of Disease 2010 Study.” Annals of the Rheumatic Diseases 73(7): 1323–30. 10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- Cunningham M., Wells M. 2017. “Qualitative Analysis of 6961 Free-Text Comments from the First National Cancer Patient Experience Survey in Scotland.” BMJ Open 7(6): e015726. 10.1136/bmjopen-2016-015726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health (Western Australia). 2010. Elective Joint Replacement Service Model of Care. Perth: Health Networks Branch. [Google Scholar]
- Dziedzic K.S., French S., Davis A.M., Geelhoed E., Porcheret M. 2016. “Implementation of Musculoskeletal Models of Care in Primary Care Settings: Theory, Practice, Evaluation and Outcomes for Musculoskeletal Health in High-Income Economies.” Best Practice & Research: Clinical Rheumatology 30(3): 375–97. 10.1016/j.berh.2016.08.004. [DOI] [PubMed] [Google Scholar]
- Hsieh H.F., Shannon S.E. 2005. “Three Approaches to Qualitative Content Analysis.” Qualitative Health Research 15(9): 1277–88. 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Kopec J.A., Sayre E.C., Fines P., Flanagan W.M., Nadeau C., Okhmatovskaia A. et al. 2016. “Effects of Reductions in Body Mass Index on the Future Osteoarthritis Burden in Canada: A Population-Based Microsimulation Study.” Arthritis Care & Research 68(8): 1098–105. 10.1002/acr.22796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim K.K., Chan M., Navarra S., Haq S.A., Lau C.S. 2016. “Development and Implementation of Models of Care for Musculoskeletal Conditions in Middle-Income and Low-Income Asian Countries.” Best Practice & Research: Clinical Rheumatology 30(3): 398–419. 10.1016/j.berh.2016.08.007. [DOI] [PubMed] [Google Scholar]
- March L., Amatya B., Osborne R.H., Brand C. 2010. “Developing a Minimum Standard of Care for Treating People with Osteoarthritis of the Hip and Knee.” Best Practice & Research: Clinical Rheumatology 24(1): 121–45. 10.1016/j.berh.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Nelson A.E., Allen K.D., Golightly Y.M., Goode A.P., Jordan J.M. 2014. “A Systematic Review of Recommendations and Guidelines for the Management of Osteoarthritis: The Chronic Osteoarthritis Management Initiative of the U.S. Bone and Joint Initiative.” Seminars in Arthritis and Rheumatism 43(6): 701–12. 10.1016/j.semarthrit.2013.11.012. [DOI] [PubMed] [Google Scholar]
- Nolan G., Koutsimanis H., Page C., Briggs A.M., Harris B. 2016. “Consumer Feedback on the Current and Future Management of Hip and/or Knee Osteoarthritis in Victoria.” Melbourne: MOVE: Muscle, Bone & Joint Health. [Google Scholar]
- NSW Agency for Clinical Innovation. 2012. Musculoskeletal Network: Osteoarthritis Chronic Care Program Model of Care. Sydney, Australia: Author. [Google Scholar]
- Royal Australian College of General Practitioners. 2009. Guideline for the Non-Surgical Management of Hip and Knee Osteoarthritis. Melbourne, Australia: Author. [Google Scholar]
- Schofield D., Shrestha R., Cunich M. 2016. Counting the Cost: Part 2 – Economic Costs. The Current and Future Burden of Arthritis. Sydney: Arthritis Australia. [Google Scholar]
- Schofield D.J., Shrestha R.N., Cunich M., Tanton R., Kelly S., Passey M.E. et al. 2015. “Lost Productive Life Years Caused by Chronic Conditions in Australians Aged 45–64 Years, 2010–2030.” Medical Journal of Australia 203(6): 260. [DOI] [PubMed] [Google Scholar]
- Stoffer M.A., Smolen J.S., Woolf A., Ambrozic A., Berghea F., Boonen A. et al. 2015. “Development of Patient-Centred Standards of Care for Osteoarthritis in Europe: The Eumusc.net-project.” Annals of the Rheumatic Diseases 74(6): 1145–9. 10.1136/annrheumdis-2014-206176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Therapeutic Guidelines. 2017. Rheumatology (3rd ed.). Melbourne: Therapeutic Guidleines. [Google Scholar]
- Victorian Musculoskeletal Clinical Leadership Group. 2018. Victorian Model of Care for Osteoarthritis of the Hip and Knee. Melbourne: MOVE Muscle, Bone & Joint Health. [Google Scholar]
- Wluka A.E., Chou L., Briggs A.M., Cicuttini F.M. 2016. “Consumers' Perceived Needs of Health Information, Health Services and Other Non-Medical Services: A Systematic Scoping Review. Melbourne: MOVE Muscle, Bone & Joint Health. [Google Scholar]


