Abstract
Portals to allow patients to access their primary care medical records are necessary to achieve true collaborative care between doctors and patients. In this article, we outline a practical approach to achieving this goal that involves Ministries of Health, electronic medical record vendors, physicians and patients. Patient portals to primary care records could make possible an entirely new world of on-the-spot, customized learning. Patient portals ideally should be designed with the goal of optimizing patients' to better their ability to help themselves. Delaying implementation of these portals exacts a continued financial and personal hardship on patients and their families.
Abstract
Les portails qui permettent aux patients d'accéder à leur dossier médical de soins de première ligne sont nécessaires pour favoriser une véritable collaboration entre les médecins et les patients. Dans cet article, nous mettons de l'avant une démarche pratique pour atteindre cet objectif – démarche qui met à contribution les ministères de la Santé, les fournisseurs de dossiers médicaux électroniques, les médecins et les patients. Ces portails ouvrent la porte à un tout nouveau monde d'apprentissage personnalisé sur-le-champ. Les portails devraient idéalement permettre aux patients d'optimiser la prise en charge de leurs propres soins. Les délais de mise en œuvre de ces portails se traduisent par des difficultés financières et personnelles pour les patients et leurs familles.
There currently exists a largely untapped potential to enable patients to be better informed and more proactively involved in optimizing their primary care. With over 85% of primary care providers currently using electronic medical records (EMRs; Statistica: The Statistics Portal 2018), enabling patients to access their primary care records via a patient portal represents a key component in achieving better health for patients (Gorfinkel and Lexchin 2018). A patient portal is an online application that allows patients to view personal primary care records and to securely communicate with their primary care provider. However, with only 1 in 10 Canadians currently having access to even the most rudimentary online services (Showing Results for Resources and Web Pages Tagged: Patient Portals 2018), patient portals to primary care records remain a critical but vastly underutilized resource. Once armed with easily accessed primary care records, patients are better enabled to advocate for their needs as well as those of vulnerable dependents. However, in Canada, a patchwork of EMR systems that lack interoperability presents significant challenges to establishing universal patient portals of access to primary care records.
There are a variety of functions that patient portals serve, including allowing patients to access their clinicians, see their medical records, book appointments and obtain prescriptions written online, but due to space limitations, we focus on the value of patients having access to their clinical information. We propose a collaborative model for the creation and implementation of patient portals into primary care records (Figure 1) within the patchwork of EMRs and provide an overview of essential steps needed to implement them in Canada. We define distinct and coordinated roles that Ministries of Health, EMR vendors and physicians could embrace to help make patient portals a reality. By selectively reviewing key articles from the literature and the experiences with patient portals in other countries and some Canadian provinces, we demonstrate the educational and other benefits that can be realized from patients having ready access to their clinical information, and we outline the difficulties that could be encountered. Finally, we want to emphasize that we are advocating for preliminary steps in a process of initiating patient portals at scale and acknowledge that there remain significant challenges that will need to be worked out over time.
Figure 1.
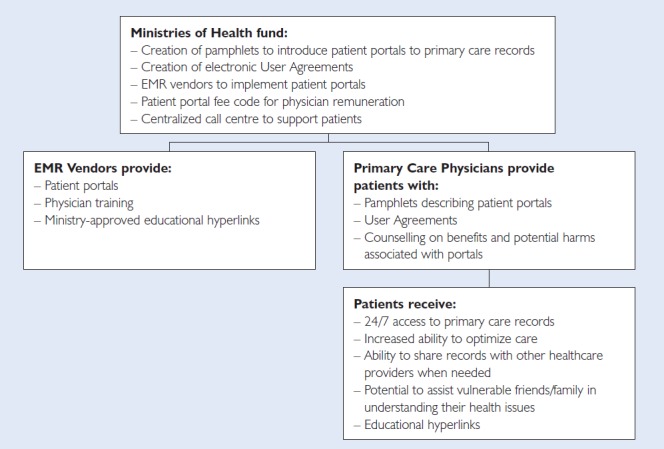
Roles and responsibilities of different stakeholders in patient portals
Patient portals need not be passive entry points to access medical data. Kildea and colleagues (Kildea et al. 2019) describe a “participatory stakeholder co-design” to expand the role of patient portals that involved patients, computer scientists, clinicians and medical physicists in their ongoing development of a smartphone app used in an oncology setting in Quebec. Their stakeholder co-design approach incorporated six core elements: (1) equal co-leadership, including a patient on treatment, (2) patient preference determination, (3) security, governance and legal input, (4) continuous user evaluation and feedback, (5) continuous staff input; and (6) end-user testing.
Drawing on the experience of in-patient portals may help to optimize the design of outpatient portals. In the in-patient setting, researchers interviewed patients provided with a patient portal during their hospitalization. Patients were taught to use the portal and to access health information as well as to learn about their care team members. As a result, patients reported feeling more independent, having reduced anxiety, feeling that their families were better informed and having an increased sense of empowerment (McAlearney et al. 2019).
Problem areas in developing portals are recognized in the literature; however, there are only a few studies that systematically report on the patient portal development process. Ongoing work in this area is necessary to ensure that portals are a success for patients, clinicians and the healthcare system (Otte-Trojel et al. 2016). In the collaborative model that we envision, Ministries of Health would fund EMR vendors and resources for both physicians and patients. EMR vendors would receive Ministry funding to incorporate patient portals into their software and to educate physicians on their utilization. Participating physicians would be provided with a novel “patient portal fee code” by Ministries to compensate them for counselling patients about the benefits and potential risks of portals. Ministries would fund patient resources, including the production, updating and dissemination of pamphlets to educate patients on patient portals. Ministries would create and provide EMR vendors with an electronic user agreement that would formalize patients' access to their primary care records. Finally, Ministries would fund centralized call centres to address patients' questions regarding portal access.
EMR vendors would be responsible for providing and maintaining the required software infrastructure for patient portals. This would include the implementation of preset standards defined by the Ministry that are compliant with the Ontario Personal Health Information Protection Act (Government of Ontario 2018) or its equivalent in other provinces. EMR vendors would be incentivized to participate through funding from Ministries and annual fees paid by physicians for EMR support. In return, EMR providers would be responsible for supporting physicians' implementation of patient portals, including providing doctors and their staff with training in their use.
Physicians would be expected to ensure that patients are provided with the necessary tools to enable them to successfully use their portals. They would provide patients with the Ministry-produced pamphlet, review this information with them and obtain their consent to the electronic user agreement. An example of such a user agreement is the one in systems such as MyChart (MyChart User Agreement nd). Physicians would also be responsible for counselling patients on the advantages and potential disadvantages of using patient portals, including the potential for a security breech. The new fee code mentioned earlier would compensate physicians for these activities. This same model could be utilized for other primary care providers, for example, nurse practitioners, but with payment models appropriate to the individual profession.
Although such a collaboration endeavours to minimize potential pitfalls, difficulties in implementing patient portals are expected. Ministries may be concerned about the initial cost outlay, especially at a time when provinces are struggling to control their budgets. Over time, this initial cost outlay is expected to be more than compensated by greater patient satisfaction and improved outcomes (Sorondo et al. 2017). EMR vendors may be concerned about whether the funding that they are provided with is adequate to support the various functions that they are being asked to undertake, including dealing with cyber-security issues. Physicians may be hesitant to pay additional fees to support EMR vendors. There may also be concerns that when patients see abnormal test results, they may experience increased patient stress.
Fortunately, this concern has not been borne out by retrospective studies examining the effects on patients of patient portals. These studies have not demonstrated a major increase in patient anxiety related to the direct release of laboratory results through patient portals (Christensen and Sue 2013). On the contrary, patients consistently find the test result feature among the most useful on patient portals and express interest in obtaining further information about interpreting the relevance of results (Giardina et al. 2015). To obtain this help, patients should be provided with opportunities to get additional health information. This engagement could come from physicians; clinicians could provide a hyperlink to explain the utility of tests that they have ordered and mark abnormal results as “clinically significant” or “not clinically significant” on the EMR, so that patients are able to see this information. Some physicians may have concerns about the potential additional workload that patient portals could represent. To mitigate this worry, abnormal results could be directly addressed by utilizing other healthcare professionals such as nurse practitioners to help explain information to patients.
The experience of some countries implementing patient portals has been variable. Australia initially struggled with low rates of adoption with My Health Record. Four years after its introduction in 2012, only 17% of Australians had registered when it was an “opt-in” system (van Kasteren et al. 2017). Since switching to an opt-out model, national participation is now in the 90% range (Australian Digital Health Agency 2019), but there remains ongoing criticism from both clinicians (Janakiramanan 2019) and academics (Kemp et al. 2018), who point out that it is not up-to-date, that it creates a security risk and that My Health Record does not seek patients' express consent because of its “opt-out” system. Other criticisms include that patients may edit their own records, thereby reducing their reliability. A further major concern is that My Health Record was not designed to be compatible with existing medical programs (Kemp et al. 2018).
In contrast, Denmark's National eHealth Portal is an example of success in the implementation of patient portals. There is near complete clinician engagement, with 98% of primary clinicians and all pharmacists having access to a centralized database accessible to patients. Citizens are empowered to log in to a personal web space to book appointments, renew prescriptions, review medication records and health data and communicate with healthcare authorities. Clinicians are able to obtain records from hospitals, laboratory results and data from electronic patient records (Khan et al. 2018).
Here in Canada, Ministries of Health in Alberta and in Quebec have demonstrated their willingness to work with EMR vendors, physicians and patients to generate patient portals. Although still in its infancy, Alberta currently is leading the way with its investment in a unified EMR that incorporates patient portals with Alberta Netcare (Alberta Netcare EHR 2019). Connect Care, the bridge between information, healthcare teams and patients, will allow healthcare providers a central access point to patient information, common clinical standards and best healthcare practices. Implementation is expected to be gradually rolled out over the next three to four years to minimize disruptions for patients and healthcare providers (Alberta Health Services nd).
Quebec has instituted a patient portal through Quebec Health Record (Québec Health Booklet 2019). The portal is to be introduced over two years and will allow patients to view their medications, lab results, medical imaging results, doctors' and hospital billings and wait lists for surgery. This system will further enable nurse practitioners, nurses and pharmacists to optimize follow-up of chronic conditions. The eventual goal is to incorporate patient health information and information regarding tests and treatments. Because the regulation of the delivery of healthcare is a provincial function, precisely what information a patient will have access to when using the patient portal will be determined at the provincial level. Differences may also exist between what information is available through hospital and primary care patient portals. Our focus here is on the latter, and it is our belief that it should include their social, medical and surgical histories, current medication list, prescription history, drug allergies/intolerances, laboratory and radiology reports and consultation notes.
The development of universal access to patient portals in Canada should be understood as an ongoing and evolving process. Patient portals need to first be implemented before they can be further developed with efforts that will optimize the provision of patient health information and relevant educational material.
Despite possible roadblocks, we strongly advocate for provinces to proceed with implementing patient portals using the model we have outlined or some variation of it. Patient portals to primary care records make possible an entirely new world of on-the-spot, customized learning. Each problem listed in a patient's electronic medical history could be directly linked to educational resources that are specific to that problem. Such resources would be available to patients precisely at the moment that they are most needed, when patients are reading their chart. Accurate and reliable hyperlinks for patients to topics such as smoking cessation, insomnia, exercise, diet, hypertension, support groups, depression and anxiety, to name a few, could be accessed by simply clicking on that problem in their medical history. The information contained in these hyperlinks could be customized according to the patient's language of preference and level of education. Patient portals ideally should be designed with the goal of optimizing patients' ability to help themselves. The combined experience of countries that have implemented patient portals demonstrates the critical need for clinical engagement about health record content and standards (Khan et al. 2018). Much of the value that patients derived from the use of portals will be directly affected by the attitudes and actions of physicians, nurse practitioners, nurses and pharmacists (Shah and Liebovitz 2017).
The time has arrived for all stakeholders in Canada – provincial Ministries, EMR providers, clinicians and patients – to embrace patient portals. Delaying implementation of patient portals exacts a continued financial and personal hardship on patients and their families. Having the will to implement a collaborative model of care centred on patient portals moves us closer to achieving truly patient-centric care.
Contributor Information
Iris GorFinkel, PrimeHealth Clinical Research, Toronto, ON.
Joel Lexchin, Professor Emeritus, Faculty of Health, York University, Toronto, ON.
References
- Alberta Health Services. n.d. Connect Care: Frequently Asked Questions: General. Retrieved February 25, 2019. <https://www.albertahealthservices.ca/assets/info/cis/if-cis-faq.pdf>.
- Alberta Netcare EHR. 2019. Retrieved February 25, 2019. <http://www.albertanetcare.ca/#Alberta%20Netcare>.
- Australian Digital Health Agency. 2019. “My Health Record.” Retrieved February 25, 2019. <https://www.myhealthrecord.gov.au/statistics>.
- Christensen K., Sue V. 2013. “Viewing Laboratory Test Results Online: Patients' Actions and Reactions.” Journal of Participatory Medicine 5: e38. [Google Scholar]
- Giardina T., Modi V., Parrish D., Singh H. 2015. “The Patient Portal and Abnormal Test Results: An Exploratory Study of Patient Experiences.” Patient Experience Journal 2: 148–54. [PMC free article] [PubMed] [Google Scholar]
- Gorfinkel I., Lexchin J. 2018. “A Call to Mandate Patient Access to Personal Primary Care Medical Records across Canada.” CMAJ 190: E869–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Ontario. 2018. “Personal Health Information Protection Act, 2004, S.O. 2004, c. 3, Sched. A.” Retrieved February 25, 2019. <https://www.ontario.ca/laws/statute/04p03>.
- Janakiramanan J. 2019. “Opting Out of My Health Record.” The Saturday Paper. Retrieved February 25, 2019. <https://www.thesaturdaypaper.com.au/opinion/topic/2019/02/02/opting-out-my-healthrecord/15490260007388>.
- Kemp K., Arnold B., Vaile D. 2018. “My Health Record: The Case for Opting Out.” Retrieved February 25, 2019. <https://theconversation.com/my-health-record-the-case-for-opting-out-99302>.
- Khan U., Zia T., Pearce C., Perera K. 2018. “The My Health Record (MyHR) Adoption in General Practices: Literature Review and Future Research Direction.” International Technology Management Review 7: 81–92. [Google Scholar]
- Kildea J., Battista J., Cabral B., Hendren L., Herrera D., Hijal T. et al. 2019. “Design and Development of a Person-Centered Patient Portal Using Participatory Stakeholder Co-Design.” Journal of Medical Internet Research 21: e11371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAlearney A., Fareed N., Gaughan A., MacEwan S., Volney J., Sieck C. 2019. “Empowering Patients During Hospitalization: Perspectives on Inpatient Portal Use.” Applied Clinical Informatics 10: 103–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MyChart User Agreement. n.d. Retrieved February 25, 2019. <https://www.mychart.ca/pages/registration/PatientAgreement.html>.
- Otte-Trojel T., de Bont A., Rundall T., van de Klundert J. 2016. “What Do We Know about Developing Patient Portals? A Systematic Literature Review.” Journal of the American Medical Informatics Association 23: e162–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Québec Health Booklet. 2019. Retrieved February 25, 2019. <https://www.quebec.ca/en/health/your-health-information/quebec-health-booklet/>.
- Shah S., Liebovitz D. 2017. “It Takes Two to Tango: Engaging Patients and Providers with Portals.” Clinical Informatics in Physiatry 9(5S): S85–97. [DOI] [PubMed] [Google Scholar]
- Showing Results for Resources and Web Pages Tagged: Patient Portals. 2018. Retrieved February 25, 2019. <https://www.betterhealthtogether.ca/component/tags/tag/31-patient-portals>.
- Sorondo B., Allen A., Fathima S., Bayleran J., Sabbagh I. 2017. “Patient Portals as a Tool for Enhancing Patient Experience and Improving Quality of Care in Primary Care Practices. EGEMS 4: 1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistica: The Statistics Portal. 2018. “Usage of Electronic Medical Records (EMR) among Primary Care Physicians in Canada from 2004 to 2017.” Retrieved February 25, 2019. <https://www.statista.com/statistics/788509/primary-care-physicians-usage-of-emr-in-canada/>.
- van Kasteren Y., Maeder A., Williams P., Damarell R. 2017. “Consumer Perspectives on MyHealth Record: A Review.” Studies in Health Technology and Informatics 239: 146–52. [PubMed] [Google Scholar]


