Abstract
Following a request from the European Commission, the EFSA Panel on Nutrition, Novel Foods and Food Allergens (NDA) was asked to deliver an opinion on lacto‐N‐tetraose (LNT) as a novel food (NF) pursuant to Regulation (EU) 2015/2283. The NF is a powdered mixture mainly composed by LNT, but also containing d‐lactose and other oligosaccharides such as para‐lacto‐N‐hexaose‐2 (para‐LNH‐2), lacto‐N‐triose II and a small fraction of other carbohydrates. It is produced by fermentation with a genetically modified strain of Escherichia coli K‐12. The information provided on the manufacturing process, composition and specifications of the NF does not raise safety concerns. The applicant intends to add the NF in a variety of foods, including infant and follow‐on formula, foods for infants and toddlers, foods for special medical purposes and food supplements. The target population is the general population except for food supplements, for which the target population is individuals above 1 year of age. The intake of LNT from the NF at the proposed use levels is unlikely to exceed the intake level of naturally occurring LNT in breastfed infants on a body weight basis. The intake of other carbohydrate‐type compounds structurally related to LNT is considered of no safety concern. The Panel concludes that the NF is safe under the proposed conditions of use for the proposed target populations.
Keywords: lacto‐N‐tetraose, LNT, human milk oligosaccharide, HMO, novel food, safety
Summary
Following a request from the European Commission, the EFSA Panel on Nutrition, Novel Foods and Food Allergens (NDA) was asked to deliver a scientific opinion on lacto‐N‐tetraose (LNT) as a novel food (NF) pursuant to Regulation (EU) 2015/2283. The assessment of the safety of this NF that is a powdered mixture mainly composed of LNT, but also containing d‐lactose and other oligosaccharides such as para‐lacto‐N‐hexaose‐2 (para‐LNH‐2), lacto‐N‐triose II and a small fraction of other carbohydrates, follows the methodology set out in the EFSA Guidance on the preparation and presentation of an application for authorisation of a novel food Regulation (EU) 2015/2283 and in the Commission Implementing Regulation (EU) 2017/2469 and it is based on the data supplied in the application, information submitted by the applicant following the European Food Safety Authority (EFSA) requests for supplementary information and additional data identified by the Panel.
The NF contains LNT as the primary ingredient (around 78% w/w dry matter) and it is considered to be a mixture with fully characterised and related substances such as d‐lactose and lacto‐N‐triose II. The remaining portion of the product consists mainly of other carbohydrate‐type compounds structurally related to LNT, e.g. para‐lacto‐N‐hexaose‐2 and the ‘LNT fructose isomer’. Overall, the dry total specified carbohydrates fraction of the LNT product adds up to 97% of the total weight. The NF is obtained by fermentation with a genetically modified strain of Escherichia coli (K‐12 DH1 MDO).
The information provided on the manufacturing process, composition and specifications of the NF does not raise safety concerns.
The applicant intends to add the NF in a variety of foods, including infant and follow‐on formula (IF and FOF), foods for infants and young children, foods for special medical purposes and food supplements. The target population is the general population except for food supplements, for which the target population is individuals above 1 year of age.
Considering that LNT is a naturally occurring oligosaccharide present in human milk, the history of human exposure to LNT concerns breastfed infants.
The Panel considers that there are no concerns regarding genotoxicity of the NF and that a no observed adverse effect level (NOAEL) from the 90‐day oral toxicity study with the NF can be established at the highest dose of 4,000 mg/kg body weight (bw) per day.
The anticipated daily intake of LNT from the consumption of IF (only), in infants up to 16 weeks of age, does not exceed the high intake level in breastfed infants per kg bw. The anticipated daily intake of LNT for the proposed uses at their respective maximum use levels is unlikely to exceed the high intake level of LNT in breastfed infants per kg bw. The maximum daily intake of the NF as food supplements (i.e. 2 g/day) for individuals above 1 year of age also does not exceed the maximum intake level of LNT in breastfed infants per kg bw. The intake of LNT in breastfed infants on a body weight basis is expected to be safe also for other population groups.
The Panel notes that for other oligosaccharides present as a small fraction in the NF (i.e. lacto‐N‐triose II and para‐LNH‐2) a comparison with exposures from human milk cannot be performed.
It is also noted that with substances of this nature the maximum feasible doses that can be used in subchronic studies (because of viscosity and risk of nutritional imbalance) are only able to ensure a relatively low safety margin with respect to the highest estimated daily intakes in the intended population. However, taking into account the intrinsic nature of human milk oligosaccharides (HMOs) with their limited absorption, the low levels in the NF, the absence of toxicologically relevant effects in the subchronic study up to the highest dose tested and considering that infants are naturally exposed to these substances, the Panel considers that no safety concerns arise.
Thus, the Panel concludes that the NF, mainly composed of LNT, but also containing D‐lactose and other oligosaccharides such as para‐lacto‐N‐hexaose‐2 (para‐LNH‐2), lacto‐N‐triose II and a small fraction of other carbohydrates, is safe under the proposed conditions of use. The target population is the general population, except for food supplements for which the target population is individuals above 1 year of age. Food supplements are not intended to be used if other foods with added NF or breast milk are consumed the same day.
1. Introduction
1.1. Background and Terms of Reference as provided by the European Commission
On 16 July 2018, the company Glycom A/S submitted a request to the European Commission in accordance with Article 10 of Regulation (EU) 2015/22831 to place on the EU market lacto‐N‐tetraose as a novel food.
In accordance with Article 10(3) of Regulation (EU) 2015/2283, the European Commission asks the European Food Safety Authority to provide a scientific opinion by carrying out the assessment for lacto‐N‐tetraose as a novel food ingredient.
2. Data and methodologies
2.1. Data
The safety assessment of this novel food (NF) is based on data supplied in the application and information submitted by the applicant following EFSA requests for supplementary information.
During the assessment, the Panel identified additional data which were not included in the application (Gorbach, 1978; Strecker et al., 1989; Rudloff et al., 1996, 2012; Gnoth et al., 2000; Chai et al., 2001; Pfenniger et al., 2002; Asakuma et al., 2008, 2011; De Leoz et al., 2012; Rudloff and Kunz, 2012; Goehring et al., 2014; Vazquez et al., 2017; Phipps et al., 2018).
Administrative and scientific requirements for NF applications referred to in Article 10 of Regulation (EU) 2015/2283 are listed in the Commission Implementing Regulation (EU) 2017/2469.2
A common and structured format on the presentation of NF applications is described in the EFSA guidance on the preparation and presentation of a NF application (EFSA NDA Panel, 2016). As indicated in this guidance, it is the duty of the applicant to provide all available (proprietary, confidential and published) scientific data, including both data in favour and not in favour to supporting the safety of the proposed NF.
This NF application includes a request for protection of proprietary data in accordance with Article 26 of Regulation (EU) 2015/2283. Data claimed to be proprietary by the applicant include:
Detailed description of the production process – raw materials and schematic overview of the processing (section of the dossier 2.b.1.1‐4).
Annexes to the dossier which relate to the identity, the production process, production microorganism, composition and specifications of the NF (annex I ‘NMR analytical reports’, annex II ‘production strain data’, annex III ‘production strain certificates’, annex IV ‘raw materials and processing aids’, annex V ‘Certificate of Analysis and batch data’, annex VI ‘analytical methods and validation reports’, annex VII ‘Stability reports’, annex VIII ‘Laboratory accreditation certificates’).
‘Intakes assessment report’ (annex X to the dossier).
-
Unpublished toxicological study reports:
-
–
Lacto‐N‐tetraose – Bacterial Reverse Mutation Test (Study report 2018a); In Vitro Mammalian Cell Micronucleus Test (Study report 2018b, 2019); 14‐Day Toxicity Study in the Neonatal Rat (Study report, 2018c); 90‐Day Toxicity Study in the Neonatal Rat (Study report, 2018d);
-
–
Lacto‐N‐neotetraose ‐ In Vitro Mammalian Cell Micronucleus Test (Study report, 2016a), 90‐Day Toxicity Study in the Neonatal Rat (Study report 2016b).
-
–
Appendix B.3 to the dossier referring to the summary table of statistically significant observations in toxicity studies with lacto‐N‐tetraose (LNT).
2.2. Methodologies
The assessment follows the methodology set out in the EFSA guidance on NF applications (EFSA NDA Panel, 2016) and the principles described in the relevant existing guidance documents from the EFSA Scientific Committee. The legal provisions for the assessment are laid down in Article 11 of Regulation (EU) 2015/2283 and in Article 7 of the Commission Implementing Regulation (EU) 2017/2469.
This assessment concerns only risk that might be associated with consumption of the NF under the proposed conditions of use and is not an assessment of the efficacy of LNT with regard to any claimed benefit.
3. Assessment
3.1. Introduction
The NF is LNT, one of the most abundant oligosaccharides within the complex fraction of human milk oligosaccharides (HMO). The Panel notes that although LNT is the major component of the NF, related substances (namely lacto‐N‐triose II and para‐lacto‐N‐hexaose‐2) are also present. The NF is obtained by microbial fermentation using d‐lactose as a substrate and D‐glucose as an energy source. LNT is chemically and structurally identical to the naturally occurring LNT in human breast milk. The NF is intended to be used in foods for infants and young children (including infant formulas (IFs) and follow‐on formulas), foods for special medical purposes, total diet replacements for weight control, food supplements, beverages and in a variety of other foods (e.g. dairy products, bakery wares). The target population is the general population, except for the use as food supplement which is intended for individuals above 1 year of age.
The applicant indicated that according to Regulation (EU) 2015/2283 this NF falls under the following categories:
‘food with a new or intentionally modified molecular structure, where that structure was not used as, or in, a food within the Union before 15 May 1997’; and
‘food consisting of, isolated from or produced from microorganisms, fungi or algae’.
3.2. Identity of the NF
The NF is a powdered mixture mainly composed of LNT, but also containing d‐lactose and other oligosaccharides such as para‐lacto‐N‐hexaose‐2 (para‐LNH‐2), lacto‐N‐triose II and a small fraction of other carbohydrates. It is produced by fermentation with the genetically modified strain of Escherichia coli K12 DH1 MDO. LNT is a tetrasaccharide consisting of a terminal D‐galactose linked through a β‐(1‐3) bond to N‐acetyl‐d‐glucosamine (GlcNAc), linked through a β‐(1‐3) bond to d‐galactose, linked through a β‐(1‐4) bond to the reducing end d‐glucose, which is in equilibrium between the α and β‐anomeric forms. LNT is an isomer of LNnT (lacto‐N‐neotetraose), which contains the same monosaccharide moieties, with the linkage between the terminal galactose and GlcNAc being β‐(1‐4).
LNT is characterised by the chemical formula: C26H45O21; molecular mass: 707.63 Da; CAS No 14116‐68‐8; IUPAC name: Gal‐(β1‐3)‐GlcNAc‐(β1‐3)‐Gal‐(β1‐4)‐Glc (Figure 1).
Figure 1.
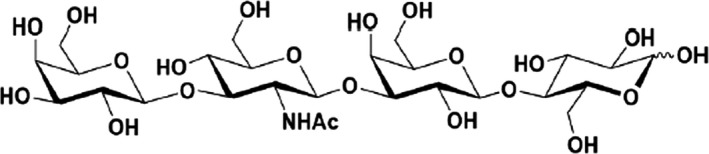
Structure of LNT
The structure has been confirmed by using monodimensional (1D) and two‐dimensional (2D) 1H and 13C nuclear magnetic resonance spectroscopy (NMR). The coupling constants (JH1,H2) indicate that the pyranose ring configurations are β for all monosaccharide units, except for the reducing end glucose, where the two anomeric forms are in equilibrium. In order to demonstrate the presence of the β‐(1‐3) linkage between the terminal galactose and N‐acetylglucosamine in LNT, a 2D 1H‐1H Nuclear overhauser effect spectroscopy (NOESY) report has been provided, indicating the steric proximity of the H‐1 atom of the terminal galactose unit and the H‐3 atom of the N‐acetyl‐glucosamine unit. In addition, the presence of the β‐(1‐3)‐bond has been confirmed by two independent reports, including two‐dimensional 1H‐1H and 1H‐13C correlation experiments: zero quantum total correlation spectroscopy (zqTOCSY), heteronuclear single quantum coherence (HSQC) and heteronuclear multiple bond correlation (HMBC) experiments. Correlations in the HSQC spectrum were identified and assigned based on the chemical shifts previously reported for LNT (Strecker et al., 1989). Also, the mass fragmentation pattern in MS/MS spectrometry for LNT has been provided and is consistent with that reported in the literature (Chai et al., 2001; Pfenneger et al., 2002; Urashima et al., 2018).
The LNT produced by microbial fermentation has been shown to be chemically and structurally identical to its counterpart present in HMOs by mono‐ and two‐dimensional NMR.
3.3. Production process
The NF is produced according to Good Manufacturing Practice (GMP) and Hazard Analysis Critical Control Points (HACCP) principles. It is also comparable to the manufacturing processes of the already authorised human identical milk oligosaccharides (HiMOs), such as LNnT and 2’‐FL (fucosyllactose), assessed by EFSA (2’‐FL/DFL (difucosyllactose), EFSA NDA Panel, 2019).
The manufacturing process can be broadly divided into two stages. In the first stage, d‐lactose and d‐glucose are converted to LNT by the adapted cellular metabolism of the production microorganism, which uses d‐glucose as an energy and carbon source, and d‐lactose as a substrate for LNT biosynthesis. The production microorganism is entirely removed from the medium by filtration at the end of the fermentation process. The second stage of the process consists of a series of purification, concentration and isolation steps to obtain the NF as a dried, amorphous powdered mixture.
The producing strain E. coli (K‐12 DH1 MDO) used in the fermentation process for the production of the NF, is a genetically modified derivative of the parental strain E. coli K‐12 DH1(ʎ‐ gyrA96 recA1 relA1 endA1 thi‐1 hsdR17 supE44) that was obtained by the applicant from the German Collection of Microorganisms and Cell cultures (DSMZ) and deposited under DSM No. 4235.
The parental strain E. coli K‐12 DH1 derives from E. coli K‐12 by forced random mutagenesis. Although the species E. coli was considered not suitable for qualified presumption of safety (QPS) status (EFSA BIOHAZ Panel, 2018), E. coli K‐12 is considered as a safe and non‐pathogenic or toxigenic microorganism widely used for biotechnological applications (Gorbach, 1978; OECD, 1986; Muhldorfer and Hacker, 1994; U.S. EPA, 1997). The whole genomes of E. coli K‐12 and of other derivative strains, including E. coli K‐12 DH1, were sequenced and compared with other E. coli strains. The results indicate that E. coli K‐12 and its derivatives show genomic differences compared to pathogenic strains (Blattner et al., 1997; Lukjancenko et al., 2010).
The genetically modified producing strain E. coli (K‐12 DH1 MDO), has been deposited in the DSMZ in Braunschweig, Germany, under DSM No. 32776. The applicant provided a detailed description of the genetic modification process applied to the parental strain E. coli K‐12 DH1 to obtain an intermediate platform strain E. coli (K‐12 DH1) MDO and the final producing microorganism E. coli (K‐12 DH1 MDO).
The absence of viable cells of the producing microorganism in the NF was demonstrated by testing five batches of the NF for bacteria from the Enterobacteriaceae family according to internationally recognised methods (ISO 21528‐1:2004, MSZ ISO 21528‐2:2004). To increase the level of reassurance, an additional and E. coli‐specific method (ISO 7251:2005) has been applied for all batches and the success criteria have been set and confirmed to be ‘absent in 10 g’ of tested product. Furthermore, the absence of residual proteins is confirmed by an adaptation of the Bradford protein method which has been validated to detect residual protein down to a level of 0.01%. Residual proteins cannot be detected in the final product.
In addition, no residual DNA from the production organism was detected in five independent batches of the NF using three quantitative polymerase chain reaction (PCR) assays (limit of quantification (LOQ) = 0.4 pg/mg). Upon EFSA's request, the applicant provided data to demonstrate the validity of the method in accordance to the EFSA guidance on microorganisms used as production organisms (EFSA FEEDAP Panel, 2018).
The Panel considers that the production process is sufficiently described and does not raise safety concerns.
3.4. Compositional data
The NF contains LNT as the primary ingredient (around 78% w/w dry matter) and is considered to be a mixture of fully characterised and related substances such as d‐lactose and lacto‐N‐triose II, comprising an average of 93% of the total batch weight. The remaining portion of the product consists mainly of other carbohydrate‐type compounds structurally related to LNT, e.g. para‐LNH‐2 and the ‘LNT fructose isomer’. Overall, the dry total specified carbohydrates fraction of the LNT product adds up to 97% of the total weight (mean from five batches of the NF).
Lacto‐N‐triose II is a metabolic intermediate of LNT (and LNnT) biosynthesis and one of the products of LNT (or LNnT) hydrolysis (Kuhn et al., 1956), and as such occurs also naturally in breast milk (Dabrowski et al., 1983; Hosomi and Takeya, 1988; Miwa et al., 2010). The hexasaccharide, para‐LNH‐2), is an isomer/analogue of the para‐LNH naturally present in human milk, firstly isolated and described in 1977 by Yamashita et al. (1977). The ‘LNT fructose isomer’ is a product derived from LNT by isomerisation, where the terminal glucose moiety has been isomerised to a fructose unit.
As regard to the physico‐chemical properties, the LNT product can be described as white to off‐white amorphous powder or agglomerate. It is readily soluble in aqueous solutions (max. 400 mg/mL, 25°C), with poor solubility in any organic solvents.
The applicant provided batch‐to‐batch compositional analysis for five batches of the NF (Table 1). LNT and the carbohydrate‐type compounds have been analysed by high‐performance anion exchange chromatography coupled to pulsed amperometric detection (HPAEC‐PAD) using ‘in house’ validated methods as well as analysis by certified external international laboratories.
Table 1.
Batch‐to‐batch analysis for five batches of NF
| Parameters | Batches | |||||
|---|---|---|---|---|---|---|
| CPN4215 1000216 FD | CPN4215 1000316 FD | CPN4215 1000416 FD | CPN4215 1000516 FD | CPN4215 1000616 FD | Mean ± SD | |
| Physiochemical properties | ||||||
| Appearance | Powder or agglomerates | |||||
| Colour | White to off white | |||||
| pH (20°C, 5% solution) | 4.6 | 4.0 | 4.3 | 4.5 | 4.4 | 4.4 ± 0.2 |
| Composition | ||||||
| HiMS [w/w % dry matter] | 94.7 | 92.4 | 92.2 | 92.0 | 92.0 | 92.7 ± 1.2 |
| LNT [w/w % dry matter] | 80.1 | 80.2 | 77.0 | 76.2 | 78.9 | 78.5 ± 1.8 |
| d‐Lactose [w/w %] | 6.27 | 6.28 | 8.94 | 9.33 | 7.18 | 7.6 ± 1.5 |
| Lacto‐N‐triose II [w/w %] | 8.15 | 6.28 | 5.95 | 6.24 | 5.55 | 6.4 ± 1.0 |
| para‐LNH‐2 [w/w %] | 2.38 | 2.85 | 2.48 | 2.93 | 3.21 | 2.8 ± 0.3 |
| LNT fructose isomer [w/w %] | 0.53 | 0.69 | 0.60 | 0.73 | 0.71 | 0.65 ± 0.1 |
| Sum of other carbohydrates [w/w %] | 1.1 | 1.3 | 1.4 | 1.4 | 1.2 | 1.3 ± 0.1 |
| Total specified carbohydrates (dry matter) [w/w %] | 98.8 | 97.9 | 96.7 | 97.1 | 97.2 | 97.5 ± 0.8 |
| Water [w/w %] | 1.5 | 1.9 | 2.0 | 1.6 | 2.7 | 1.9 ± 0.5 |
| Ash, sulfated [w/w %] | 0.15 | 0.11 | 0.08 | 0.07 | 0.09 | 0.1 ± 0.03 |
| Microbiological parameters | ||||||
| Aerobic mesophilic total plate count [CFU/g] | < 10 | < 10 | < 10 | < 10 | < 10 | < 10 |
| Enterobacteriaceae [in 10 g] | Absent | Absent | Absent | Absent | Absent | Absent |
| Salmonella spp.[in 25 g] | Absent | Absent | Absent | Absent | Absent | Absent |
| Cronobacter (Enterobacter) sakazakii [in 10 g] | Absent | Absent | Absent | Absent | Absent | Absent |
| Listeria monocytogenes[in 25 g] | Absent | Absent | Absent | Absent | Absent | Absent |
| Bacillus cereus [CFU/g] | < 10 | < 10 | < 10 | < 10 | < 10 | < 10 |
| Yeasts [CFU/g] | < 10 | < 10 | < 10 | < 10 | < 10 | < 10 |
| Moulds [CFU/g] | < 10 | < 10 | < 10 | < 10 | < 10 | < 10 |
HiMS: human identical milk saccharides; CFU: colony forming units; LNT: lacto‐N‐tetraose; ±SD: standard deviation.
The microbiological purity of batches of the NF has been assessed for non‐pathogenic microorganisms (bacteria, yeasts and moulds) as general hygiene indicators as well as for selected food‐borne pathogens.
The Panel considers that the information provided on the composition of the NF is sufficient and does not raise safety concerns.
3.4.1. Stability
Stability of NF
The bulk stability of the powdered NF produced by fermentation has been investigated in two representative batches, in an ongoing 5‐year study under real‐time conditions (25°C, 60% relative humidity (RH)) and an ongoing 2‐year study under accelerated conditions (40°C, 75% RH).
Upon EFSA's request for additional information, the applicant provided interim results of two batches of the NF. Results on composition, sensory testing, physical and microbiological parameters have been provided for the two batches up to 24 and 36 months for the real time stability and up to 18 and 24 months for accelerated stability studies. The results indicate that there is no appreciable degradation of NF ingredients, no changes in impurity profile, and no alterations in the microbiological quality of the ingredient.
Based on the data available, the Panel considers that the NF is expected to be stable for at least 24 months when stored at room temperature.
Stability of NF under the intended conditions of use
The stability of the LNT ingredients in powdered IF has also been investigated. Long‐term storage (up to 12 months) at various temperatures (4, 20, 30 and 37°C) showed that LNT in the IF (containing other HiMOs, long‐chain polyunsaturated fatty acids (LC‐PUFA), vitamins and minerals to mimic the intended conditions of use) is stable under the tested conditions since no appreciable variations of the HiMO levels over time were observed.
No stability data for LNT in other food matrices have been provided. LNnT, the constitutional isomer of LNT has been demonstrated to be stable in various food matrices, including yoghurts, ready‐to‐drink flavoured milk and citrus fruit beverages. All stability studies on LNnT were conducted using formulations representative of commercial food products on the market and under typical processing (i.e., pasteurisation and/or UHT heating) and typical storage conditions (e.g. temperature and shelf‐life) for such products.
Based on the highly similar structure, the applicant assumes that the stability properties of LNnT and LNT are comparable.
The Panel considers that the available data provide sufficient information with respect to the stability of the NF in the food matrices.
3.5. Specifications
The specifications of the NF as proposed by the applicant are presented in Table 2. The parameters include the main components of the mixture of HiMS (predominantly LNT), the principal raw material D‐lactose and lacto‐N‐triose II and also two other oligosaccharides, para‐lacto‐N‐hexaose‐2 and ‘LNT fructose isomer’.
Table 2.
Specifications of the NF
| Description: the NF is a purified, white to off‐white powder that is produced by a microbial process and contains lacto‐N‐tetraose (LNT) and limited levels of lactose, lacto‐N‐triose II and lacto‐N‐hexaose‐2. | ||
|---|---|---|
| Source: A genetically modified strain of Escherichia coli K‐12 DH1 MDO | ||
| Parameter | Specification | Method |
| Identification (LNT) | RT of standard ± 3% | HPLC/UV |
| Sum of HiMS1 (dry matter) | ≥ 90.0 w/w % | HPLC/UV and HPLC/PAD |
| LNT (dry matter) | ≥ 70.0 w/w % | HPLC/UV and HPLC/PAD |
| d‐Lactose | ≤ 12.0 w/w % | HPAEC/PAD |
| Lacto‐N‐triose II | ≤ 10.0 w/w % | HPAEC/PAD |
| para‐LNH‐2 | ≤ 3.5 w/w % | HPAEC/PAD |
| LNT fructose isomer | ≤ 1.0 w/w % | HPLC/CAD |
| Sum of other carbohydrates | ≤ 5.0 w/w % | HPLC/CAD and HPAEC/PAD |
| pH (20°C, 5% solution) | 4.0–6.0 | Eur. Ph. 9.2 2.2.3 (07/2016:20203) |
| Water | ≤ 6.0 w/w % | Karl‐Fisher |
| Ash, sulfated | ≤ 0.5 w/w % | Eur. Ph. 9.2 2.4.14 (04/2010:20414) |
| Residual protein | ≤ 0.01 w/w % | Bradford assay (UV spectroscopy) (2) |
| Microbiological Parameters | ||
| Aerobic mesophilic total plate count | ≤ 1,000 CFU/g | ISO 4833‐1:2014 |
| Enterobacteriaceae | ≤ 10 CFU/g | ISO 21528‐1:2004, MSZ ISO 21528‐2:2004 |
| Salmonella spp. | Absent in 25 g | ISO 6579:2006 |
| Yeasts | ≤ 100 CFU/g | ISO 7954:1999 |
| Moulds | ≤ 100 CFU/g | ISO 7954:1999 |
| Residual endotoxins | ≤ 10 EU/mg | Eur. Ph. 2.6.14 |
LNT: lacto‐N‐tetraose; CFU: colony forming units; EU: endotoxin units; Eur. Ph.: European Pharmacopoeia; HiMS: Human identical Milk Saccharides; HPLC: high‐performance liquid chromatography; CAD: charged aerosol detection; PAD: pulsed amperometric detection KF: Karl–Fischer; RT: retention time; ISO: International Organization for Standardization; UV: ultraviolet.
Sum of carbohydrates LNT, lactose and Lacto‐N‐triose II; (2) LOR (reporting limit) = 17 mg/kg.
The sum of relevant HiMS (LNT, lactose and lacto‐N‐triose II) has been introduced by the applicant as a parameter with a minimum level set at 90% to ensure a highly consistent product quality. The LNT content is specifically set with a minimum of 70% (dry matter).
The Panel noted that the efficiency of the production process when compared to the one of its constitutional isomer LNnT produced by fermentation, is relatively low (lacto‐N‐triose II and d‐lactose levels up to 10 and 12%, respectively). This fact has been explained by the applicant as a change in the production process to reduce the use of solvents, while maintaining a high (≥90% w/w dry matter) sum of HiMS.
Another parameter called ‘sum of other carbohydrates’ has been introduced, to include other carbohydrates individually present in low concentration, up to a total amount of 5%.
Microbiological parameters for Listeria monocytogenes, Cronobacter (Enterobacter) sakazakii and Bacillus cereus are monitored through internal specifications.
Analyses were performed using internationally recognised methods or newly developed and validated analytical protocols at Glycom's Research & Development Department and confirmed by accredited laboratories.
The Panel considers that the information provided on the specification of the NF is sufficient and does not raise safety concerns.
3.6. History of use of the NF and/or of its source
3.6.1. History of use of the NF
The applicant states that the NF does not have a history of use.
Two other HiMOs (i.e. the constitutional isomer LNnT and 2’‐FL) produced by the same applicant by chemical synthesis and by fermentation with E. coli K‐12 have been included in the European novel food list ((EU) 2018/1023) as well as granted GRAS status in the US (FDA, 2016) and considered novel food ingredients in Israel and Singapore. The HiMO produced by fermentation was considered substantially identical to the one obtained by chemical synthesis. LNnT can be added in several food categories alone or in combination with 2’‐FL at a dose up to 0.6 g L or kg ((EU) 2017/2470).3
3.6.2. Consumption of oligosaccharides constituent of the NF in breast milk
Human breast milk contains a family of structurally related oligosaccharides, known as HMOs, as the third largest solid components. The highest concentrations of HMOs occur in human colostrum (20 to 25 g/L), and concentrations between 5 to 20 g/L occur in mature human milk (Thurl et al., 2010; Bode, 2012; Urashima et al., 2018). HMOs amount and composition vary among mothers and over the course of lactation. LNT belongs to the subfraction of ‘neutral core’ HMOs, characterised by the presence of N‐acetyl‐d‐glucosamine (GlcNAc) and that accounts for 10–20% of the total HMO (Thurl et al., 2010; Rijnierse et al., 2011; Bode, 2012). In addition, LNT is one of the most abundant HMOs along with 2’‐FL, 6’‐sialyllactose, lacto‐N‐fucopentaose I and LNnT.
Although the HMO pattern depends on the genetic background of the mother, core HMOs such as LNT and LNnT, are present in all types of milks from all mothers’ phenotypes (Erney et al., 2000; Kunz et al., 2016). The biological relevance of the structural difference between LNT and LNnT, i.e. type 1 vs type 2 linkage between the terminal Gal and next to GlcNAc (and the respective ratio between the 2 forms) is not clear.
Several publications on HMO and LNT in human milk have been provided by the applicant. The amount of LNT in human milk, as for other HMOs, is genetically determined and also depending on the lactation period, with higher levels reported in colostrum (Coppa et al., 1999, 2001; Erney et al., 2000; Asakuma et al., 2008, 2011; Thurl et al., 2010, 2017; De Leoz et al., 2012; Galeotti et al., 2012, 2014; Spevacek et al., 2015; Austin et al., 2016; McGuire et al., 2017). Thurl et al. (2017) summarised the findings from 21 studies and reported that the content of LNT in milk from mothers who delivered at the end of gestation period ranged from 0.59 to 0.98 g/L (average 0.79 g/L). It was noted that the amount of LNT was slightly more abundant (ranging from 0.39 to 1.68 g/L, average 1.04 g/L) in mothers who delivered pre‐terms. Erney et al. (2001) reported an average concentration of 0.76 g/L (with a maximum of 2.74 g/L) in pooled milk samples from different lactating phases. LNT was found in all samples collected from 264 mothers.
Based on the mean and the highest reported occurrence levels of LNT in human milk as reported by Erney et al. (2001) and considering the average and high daily intake of breast milk (800 mL and 1200 mL, respectively) for infants from 0 to 6 months (EFSA NDA Panel, 2013), the daily intake levels of LNT from human milk for a 6.7 kg body weight (bw) infant (EFSA Scientific Committee, 2012) have been calculated (Table 3). This default bw used by the NDA Panel is for an infant of 3–6 months of age, who is more likely to consume such amount of human milk.
Table 3.
Estimated daily intake levels of LNT from human milk (800 mL and 1,200 mL) for infants of 6.7 kg bw, based on mean and high concentration of 0.76 g/L and 2.74 g/L, respectively, of LNT measured in human milk
| Daily intake levels (mg/kg bw) from 800 mL of human milk | Daily intake levels (mg/kg bw) from 1200 mL of human milk | |||
|---|---|---|---|---|
| Mean concentration | High concentration | Mean concentration | High concentration | |
| LNT | 91 | 327 | 136 | 491 |
bw: body weight.
Oligosaccharides have also been detected in domestic farm animal milk, however at lower concentrations as compared to human milk (Urashima et al., 2012, 2013; Aldredge et al., 2013; Albrecht et al., 2014).
The Panel noted that although the main component of the NF is LNT, other fractions such as lactose, lacto‐N‐triose II and para‐LNH‐2 are present in different amounts. While lactose is the most represented molecule in human breast milk, less is known for the other two fractions.
Lacto‐N‐triose II is a metabolic intermediate of LNT and also produced from the catabolism of LNT and LNnT (Miwa et al., 2010; Honda et al., 2013; Bidart et al., 2016; Thongaram et al., 2017) by gut microbiota fermentation. para‐LNH‐2 is an isomer of LNH, present in human milk mainly as mono‐ and difucosyl‐ derivatives (Yamashita et al., 1977; Albrecht et al., 2011; Thurl et al., 2017).
The presence of these oligosaccharides in human milk has not been quantified.
3.7. Proposed uses and use levels and anticipated intake
3.7.1. Target population
The target population proposed by the applicant is the general population, except for food supplements for which the target population is individuals above 1 year of age.
3.7.2. Proposed uses and use levels
The NF is intended to be added to a variety of foods, at the maximum use levels as indicated in Table 4. The Panel notes that for ‘Food for special medical purposes’ the applicant did not propose either maximum use levels or maximum intake levels.
Table 4.
Proposed Food Uses and maximum use Levels for LNT
| EU food category number | Food category name | Proposed Maximum use level |
|---|---|---|
| 1 | Dairy products and analogues | |
| 1.1 | Unflavoured pasteurised and unflavoured sterilised (including UHT) milk | 1.0 g/L |
| 1.2/1.3 | Unflavoured fermented milk‐based products | 1.0 g/L beverages |
| 10 g/kg products other than beverages | ||
| 1.4 | Flavoured fermented milk‐based products including heat‐treated products | 1.0 g/L beverages |
| 10 g/kg products other than beverages | ||
| 7 | Bakery wares | |
| 7.2 | Fine bakery wares. Cereal bars only | 10 g/kg |
| 13 | Foods for special groups (FSG) | |
| 13.1 | Foods for infants and young children | |
| 13.1.1 | Infant formula as defined in Regulation (EU) No 609/2013 | 0.8 g/L in the final product ready for use, marketed as such or reconstituted as instructed by the manufacturer |
| 13.1.2 | Follow‐on formula as defined in Regulation (EU) No 609/2013 | 0.6 g/L in the final product ready for use, marketed as such or reconstituted as instructed by the manufacturer |
| 13.1.3 | Processed cereal‐based food and baby food for infants and young children as defined in Regulation (EU) No 609/2013 | 0.6 g/L in the final product ready for use, marketed as such or reconstituted as instructed by the manufacturer |
| 5 g/kg for products other than beverages | ||
| 13.1.4 | Milk‐based drinks and similar products intended for young children | 0.6 g/L in the final product ready for use, marketed as such or reconstituted as instructed by the manufacturer |
| 5 g/kg for products other than beverages | ||
| 13.2 | Foods for special medical purposes as defined in Regulation (EU) No 609/2013 | |
| 13.2 | Foods for special medical purposes as defined in Regulation (EU) No 609/2013 | On case‐by‐case basis |
| 13.3 | Total diet replacement for weight control as defined in Regulation (EU) No 609/2013 | |
| 13.3 | Total diet replacement for weight control as defined in Regulation (EU) No 609/2013 | 2.0 g/L beverages |
| 20 g/kg products other than beverages | ||
| 14 | Beverages | |
| 14.1.4 | Flavoured drinks | 1.0 g/L |
UHT: ultra‐high temperature.
The applicant also intends to market the NF as food supplement, at the maximum daily intake of 2 g, for individuals above 1 year of age. Food supplements are not intended to be used if other foods with added LNT are consumed the same day.
3.7.3. Anticipated intake of the NF
Anticipated intake of the NF from the consumption of infant formula in infants up to 16 weeks of age
IF is expected to be the only food consumed by infants aged 0–16 weeks who are not breastfed. The high consumption of IF has been estimated to be 260 mL/kg bw per day for infants aged 0–16 weeks (EFSA Scientific Committee, 2017). Based on the maximum proposed use level of the NF (0.8 g/L in IF), the high intake of the NF from IF alone is estimated to be 208 mg/kg bw per day.
Considering the mean content of 78% for LNT in the NF (as indicated in Table 1), the daily intake of LNT from the consumption of IF added with the NF corresponds to approximately 162 mg/kg bw for LNT. The Panel notes that the anticipated daily intake of the NF from the consumption of IF (only) does not exceed the estimated high daily intake of LNT in breastfed infants per kg/bw (Table 3).
Anticipated intake of LNT from the proposed uses and use levels of the NF
The applicant estimated the daily intake of the NF by using the EFSA Food Additive Intake model (FAIM) tool (FAIM 2.0, 2017) and compared the intake to surveys conducted in UK (NDNS and its complement DNSIYC (Diet and Nutrition Survey of Infants and Young Children)). However, considering that the food categories in the FAIM tool, which are based on Regulation (EC) 1333/2008, do not allow a precise matching with the food categories proposed for the NF, the intake estimations performed by the applicant resulted in high and uncertain estimated intakes. Thus, EFSA performed a refined estimate of the anticipated daily intake of the NF, at the maximum proposed use levels of the NF, using individual data from EU dietary surveys (EFSA, 2011) and by applying the FoodEx2 classification (Table 5). The lowest and highest mean and 95th percentile anticipated daily intake of the NF for all subjects, among the EU dietary surveys, are presented in Table 6.
Table 5.
FoodEx2 categories and maximum use levels of the NF used in the refined estimate of the anticipated daily intake of the NF using individual data from EU dietary surveys
| CODE | FoodEx2 Level | Food category | Maximum use level of the NF mg/100 g |
|---|---|---|---|
| A02LV | 5 | Cow milk | 100 |
| A0CXA | 5 | European buffalo milk | 100 |
| A02MC | 5 | Sheep milk | 100 |
| A02 MB | 4 | Goat milk | 100 |
| A02MV | 3 | Butter milk | 100 |
| A02NQ | 4 | Yoghurt drinks | 100 |
| A02NR | 4 | Probiotic milk‐like drinks | 100 |
| A02NV | 5 | Kefir | 100 |
| A02NE | 4 | Yoghurt | 1,000 |
| A00EY | 4 | Cereal bars | 1,000 |
| A00EZ | 4 | Cereal bars plain | 1,000 |
| A00FA | 4 | Cereal bars mixed | 1,000 |
| A03PZ | 4 | Infant formulae, powder | 650 |
| A03QE | 4 | Infant formulae, liquid | 80 |
| A03QK | 4 | Follow‐on formulae, powder | 485 |
| A03QQ | 4 | Follow‐on formulae, liquid | 60 |
| A03QZ | 3 | Cereals with an added high protein food which have to be reconstituted | 300 |
| A03QY | 3 | Simple cereals which have to be reconstituted | 300 |
| A0BZF | 3 | Cereals with added high protein food reconstituted | 60 |
| A0BZE | 3 | Simple cereals for infants and children reconstituted | 60 |
| A03RA | 3 | Biscuits, rusks and cookies for children | 500 |
| A03RC | 2 | Ready‐to‐eat meal for infants and young children | 500 |
| A03RB | 3 | Pasta for children | 500 |
| A03RN | 3 | Fruit and vegetable juices and nectars specific for infants and young children | 60 |
| A03RP | 3 | Special food for children's growth | 60 |
| A03RT | 4 | Total daily diet replacement for weight reduction | 2,000 |
| A0EQN | 5 | Soft drinks with minor amounts of fruits or flavours | 100 |
| A03EA | 5 | Soft drink with fruit juice (fruit content below the minimum for nectars) | 100 |
| A03EX | 5 | Soft‐drink, flavoured, no fruit | 100 |
| A03FQ | 4 | Cola Type drinks | 100 |
Table 6.
Ranges among EU surveys of the estimated daily intake of the NF (mg/kg bw), based on the individual data from the EFSA Comprehensive Food Consumption Database
| Age groups | Number of EU dietary surveys | Estimated daily intake of the NF – all subjects (mg/kg bw) | |
|---|---|---|---|
| Range of means (lowest and highest) among EU dietary surveys | Range of 95th percentile (lowest and highest) among EU dietary surveys | ||
|
Infants (up to 11 months) |
11 | 33–209 | 82–685 |
|
Young children or toddlers (12–35 months) |
14 | 38–154 | 119–430 |
|
Other children (3–9 years) |
19 | 18–93 | 47–234 |
|
Adolescents (10–17 years) |
18 | 7–24 | 19–61 |
|
Adults (18–64 years) |
19 | 4–15 | 17–45 |
|
Elderly (≥ 65 years) |
18 | 4–13 | 16–38 |
| Pregnant women | 2 | 3–13 | 8–39 |
| Lactating women | 2 | 10–14 | 37–38 |
NF: novel food; bw: body weight.
The refined anticipated daily intake of the NF for each population group from each EU dietary survey is available in the excel file annexed to this scientific opinion (under ‘Supporting information’).
Based on 78% mean LNT content in the NF (Table 1), the refined anticipated daily intake of LNT is calculated from the highest 95th percentile anticipated daily intake of the NF (Table 7).
Table 7.
Estimated daily intake of LNT (mg/kg bw) from the highest 95th percentile of intake of the NF, based on 78% purity (mean content as per compositional data)
| Estimated daily intake (mg/kg bw) | ||
|---|---|---|
| Age groups | For the NF Highest 95th percentile among EU dietary surveys (as reported in table 6) | For LNT Highest 95th percentile among EU dietary surveys |
|
Infants (up to 11 months) |
685 | 534 |
|
Young children or toddlers (12–35 months) |
430 | 335 |
|
Other children (3–9 years) |
234 | 182 |
|
Adolescents (10–17 years) |
61 | 48 |
|
Adults (18–64 years) |
45 | 35 |
|
Elderly (≥ 65 years) |
38 | 29 |
| Pregnant women | 39 | 30 |
| Lactating women | 38 | 30 |
bw: body weight.
The Panel notes that the highest estimated 95th percentile intake considering 78% LNT content (i.e. 534 mg/kg bw corresponding to 78% of 685 mg/kg bw) on the basis of 11 dietary surveys covered by the EFSA Food Consumption Database, is approximately 10% above the high estimate for LNT from human milk (i.e. 491 mg/kg bw) in infants (up to 11 months).
Considering that the exposure of LNT from human milk is only exceeded in one out of 11 dietary surveys included in the EFSA Food Consumption Database (Table 6 and excel file annexed under ‘Supporting information’) and the conservative assumption underlying this type of intake assessment, in particular, assuming that all foods of the proposed food categories consumed by infants are added with the NF at the maximum proposed use levels, the Panel considers it unlikely that infants (up to 11 months) would exceed high intake levels estimated for LNT intake from human milk.
Anticipated intake of LNT from food supplements
The applicant has proposed a maximum daily intake of 2 g of the NF as food supplements for individuals above 1 year of age. Food supplements are not intended to be used if other foods with added LNT are consumed the same day. For toddlers (aged 12–35 months), food supplements are not intended to be used if breast milk or other foods with added NF or LNT are consumed the same day.
Considering the mean content of 78% for LNT in the NF the maximum daily intake from food supplements of the NF (i.e. 2 g/day) results in a maximum daily intake of 131 mg/kg bw, for toddlers with bw of 11.9 kg (default bw value for toddlers (EFSA Scientific Committee, 2012)). For individuals above 3 years of age, the maximum daily intake of the NF from food supplements on a bw basis would be lower than that for toddlers.
The Panel notes that the maximum daily intake of LNT from the use of NF as food supplements (i.e. 2 g/day) for individuals above 1 year of age does not exceed the estimated high daily intake of LNT from human milk calculated for infants on a bw basis (Table 3).
3.7.4. Combined intake from the NF and other sources
The Panel noted that the NF, LNT and related minor fractions (mainly lacto‐N‐triose II and para‐LNH‐2), is not authorised for use in food categories other than those proposed for the NF under assessment. Therefore, the only additional source for these oligosaccharides is human milk.
Food supplements are not intended to be used if other foods with added LNT or breast milk are consumed the same day.
3.8. Absorption, distribution, metabolism and excretion (ADME)
There are no data submitted for the NF or LNT.
HMOs, including LNT, are considered ‘non‐digestible oligosaccharides’ (EFSA NDA Panel, 2014) since they do not undergo any significant digestion in the upper gastrointestinal tract (Brand‐Miller et al., 1995, 1998; Engfer et al., 2000; Chaturvedi et al., 2001; Gnoth et al., 2001; Rudloff and Kunz, 2012).
Brand‐Miller et al. (1995, 1998) reported that HMOs, consumed as a load (a purified oligosaccharide fraction from human milk), are fermented in the colon by intestinal microbiota. Chaturvedi et al. (2001) and Coppa et al. (2001) reported that 97% and 40‐50%, respectively, of the ingested HMOs are excreted unchanged in faeces of breastfed infants. Furthermore, approximately 1–2% of the ingested amounts of HMOs is excreted unchanged in the infants’ urine (Rudloff et al., 1996; Gnoth et al., 2000; Goehring et al., 2014; Vazquez et al., 2017; EFSA, NDA Panel 2019).
Specifically, for LNT, it has been observed that an infant breastfed may receive approximately 50‐100 mg for each suckling and that an amount up to 3 mg in a day is found in the urine (Rudloff and Kunz, 2012; Rudloff et al., 2012), therefore confirming the trend of HMOs family.
Based on information available on HMOs the Panel considers that limited digestion of the NF occurs in the upper gastrointestinal tract and that only small amounts are expected to be absorbed. Moreover, there are no indications that the absorption of LNT, which is the main constituent of the NF, or other components may differ from that of equivalent components in the human milk.
3.9. Nutritional information
The NF is mainly composed by the non‐digestible oligosaccharide LNT. The Panel considers that consumption of the NF at the proposed use levels is not nutritionally disadvantageous.
3.10. Toxicological information
The list of toxicological studies, which were provided and claimed proprietary by the applicant, is reported in Table 8. These studies were conducted with the NF (batch CPN4215 1000416FD), which was constituted by 77% w/w dry matter of LNT (6% of lacto‐N‐triose II and 2.5% para‐LNH‐2; total of 96.7% specified carbohydrates, 9% lactose included).
Table 8.
List of toxicological studies with the NF provided by the applicant
| Test material | Reference | Type of study |
|---|---|---|
|
NF (77% LNT) |
Unpublished study report, 2018a Phipps et al., 2018; |
Bacterial reverse mutation test (Ames test) |
|
Unpublished study report, 2018b, 2019 Phipps et al., 2018; |
In vitro mammalian Cell Micronucleus Test | |
|
Unpublished study report, 2018c Phipps et al., 2018; |
14‐day DRF repeated dose oral toxicity study in neonatal rats | |
|
Unpublished study report, 2018d Phipps et al., 2018 |
90‐day GLP repeated dose oral toxicity study in neonatal rats |
LNT: lacto‐N‐tetraose; DRF: dose range finding; GLP: Good Laboratory Practice.
The applicant also provided toxicological studies on LNnT, the isomer of LNT, which was obtained by chemical synthesis and microbial fermentation using genetically modified strains of E. coli K‐12. The Panel considers that these toxicological studies on LNnT can provide supporting evidence for the safety assessment of the NF.
3.10.1. Genotoxicity
The potential genotoxicity of the NF was investigated in a bacterial reverse mutation test and an in vitro mammalian cell micronucleus test (Phipps et al., 2018, unpublished study reports, 2018a,b, 2019). These studies were conducted in compliance with Organisation for Economic Co‐operation and Development (OECD) principles of Good Laboratory Practice (GLP) (OECD, 1998a) and in accordance with the OECD test guidelines No 471 (OECD, 1997) and 487 (OECD, 2016).
The in vitro assessment of the mutagenic potential of the NF was performed with histidine‐dependent auxotrophic mutants of Salmonella Typhimurium, strains TA1535, TA1537, TA98 and TA100, and a tryptophan‐dependent mutant of E. coli, strain WP2 uvrA (pKM101), that were exposed to the NF diluted in water at concentrations up to 5,106.1 μg/plate either in the presence or absence of liver microsomal fractions (S9). No substantial, reproducible or dose‐related increases in revertant colony numbers over control counts were observed with any of the strains following exposure to LNT at any concentration (irrespective of the presence or absence of S9). No evidence of toxicity was obtained following exposure to the NF. Therefore, the NF showed to be non‐mutagenic at concentrations up to 5106.1 μg/plate, in the absence or presence of metabolic activation.
In the in vitro mammalian cell micronucleus test, concentrations of LNT up to 2,042.44 μg/mL were tested to assess the potential of LNT to cause an increase in the induction of micronuclei in in vitro cultured human peripheral blood lymphocytes in the presence or absence of metabolic activation (S9 fraction). No statistically significant increases in the number of binucleate cells containing micronuclei both after 3‐hour treatment in the presence of S9 mix or following 20‐hour treatment in the absence of S9 were recorded. However, as also reported by Phipps et al. (2018) ‘following short‐term exposure in the absence of S9, a statistically significant increase (p < 0.05) in the percentage of micronucleated cells was observed at the highest LNT concentration (2,042.44 μg/mL) compared with vehicle controls, which was also associated with a statistically significant linear trend (p < 0.05). However, as the mean value (10.5) was below the laboratory historical vehicle control upper limit (11.1), the increase at this concentration was considered biologically irrelevant and the results were considered negative overall’. Since according to OECD TG487, these data should be considered ‘neither clearly negative nor clearly positive’ the NDA Panel decided to request further tests. At the repetition of the in vitro test applying the same experimental conditions clear negative results were obtained (unpublished study report, 2019). The NF did not show any evidence of clastogenicity or aneugenicity in the absence and presence of metabolic activation.
Based on the results of these studies, the Panel considers that there are no concerns regarding genotoxicity of the NF.
3.10.2. Repeated dose toxicity studies
The applicant provided a 14‐day DRF (dose range finding) repeated dose oral toxicity study where groups of eight Crl:CD(SD) neonatal rats/sex were given water (control), 3,250 and 4,000 mg/kg bw per day of LNT by oral gavage starting from day 7 of age (unpublished study report, 2018c). The highest dose is considered by the author to be close to the maximum feasible dose due to limited solubility in water and high viscosity of the prepared formulation and aligned with the doses selected for the assessment of its isomer LNnT (up to 5,000 mg/kg bw per day, Coulet et al., 2013, EFSA NDA Panel, 2015). There were no deaths or any variations in clinical signs, body weight or macroscopic pathology attributable to LNT. Clinical pathology parameters were not assessed. Since the NF up to the highest tested dose of 4,000 mg/kg day did not cause any adverse effect, the highest dose was considered a suitable high dose for the subsequent 90‐day study in neonatal rats.
In the 90‐day study groups of 10 Crl:CD(SD) neonatal rats/sex group were given water (control), 1,000, 2,500 or 4,000 mg/kg bw per day of LNT by oral gavage starting from day 7 of age once daily for at least 90 days, until the day before necropsy (Phipps et al., 2018; unpublished study reports, 2018d). An additional control group was treated with oligofructose powder (a non‐digestible oligosaccharide permitted in infant nutrition) at 4,000 mg/kg bw per day, to compare any effects related to the general fibre‐like characteristics at the same high dose.
This study has been designed based upon the OECD TG408 (OECD, 1998b), but has been adapted (i.e. use of juvenile animals) to consider the requirements for toxicity testing of new chemical entities for use in the paediatric population (as was suggested by US FDA, 2006 and EMEA, 2008). There were no deaths or any variations in clinical signs, functional observation battery tests, macroscopic and microscopic examinations attributable to LNT. Variations in food consumption (decreased in males at top dose in the last month of treatment) and in body weight (transient increase in the first two weeks of treatment at intermediate and high dose, mainly in females and similar to the reference control) were recorded. In addition variations in some haematological (i.e. levels of some red blood cells (RBC)‐, white blood cells (WBC)‐related parameters and platelets at top dose in males or females) and blood chemistry parameters (fluctuations in transaminases, urea, creatinine, cholesterol and electrolytes levels), increase in body weight of females at the time of vaginal opening and increase in absolute organ weights in females (i.e. kidneys, liver, ovary and spleen) and males (i.e. pituitary and testes) were also recorded (Appendix A). The findings observed were of low magnitude, without dose correlation, sometimes occurring only in one gender or at the end of recovery period and are considered by the Panel as unlikely to be treatment‐related.
Statistically significant differences that have been observed in groups treated with the NF are reported in Appendix A.
The author of the study concluded that under the experimental condition applied, the dose of 4,000 mg/kg bw per day of LNT is considered as the no‐observed‐adverse‐effect‐level (NOAEL). The Panel notes that this specific experimental design, with treatment of animals by gavage prior to weaning, may result in high variability in several parameters. However, considering the absence of variations of toxicological relevance, the Panel agrees with the conclusion.
3.10.3. Toxicological studies conducted with lacto‐N‐neotetraose
In addition to the technical reports of the toxicological studies conducted with LNT, the applicant also provided information about studies conducted with the constitutional isomer LNnT when produced by fermentation using the same E. coli K‐12 DH1. The Panel assessed this NF obtained by chemical synthesis (EFSA, NDA Panel, 2015) and these two new studies from 2016 were not assessed. Considering the very high similarity between the two constitutional isomers the Panel is of the view that such studies can be considered as supportive evidence for the assessment of LNT.
The applicant reported that in studies conducted following OECD guidelines and in accordance with GLP principles, LNnT (purity 94.4%) did not elicit adverse effects in any of the tested doses or concentrations. No signs of mutagenicity, clastogenicity or aneugenicity in genotoxicity studies were noted. In the 90‐day oral study in the rat the highest dose of 5,000 mg/kg bw per day was identified as NOAEL.
Table 9.
List of toxicological studies conducted with LNnT produced by fermentation
| Test material | Reference | Type of study | Experimental details |
|---|---|---|---|
| LNnT | Unpublished study report, 2016a | In vitro mammalian Cell Micronucleus Test | 512, 1,600, 2,000 μg LNnT/mL; ± S9 |
| Unpublished study report, 2016b | 90‐day GLP repeated dose oral toxicity study (neonatal rat) | 10 Wistar rats sex/group; 1,000, 2,500, 5,000 mg/kg bw per day |
LNnT: lacto‐N‐neotetraose; GLP: Good Laboratory Practice; bw: body weight.
3.10.4. Human data
No human intervention studies with LNT have been provided by the applicant and no reference to human data was made. The Panel noted that studies with the constitutional isomer LNnT obtained by chemical synthesis have been conducted in adults and infants, and that data were overall sufficient to conclude about the safety of its use under the proposed conditions (EFSA NDA Panel, 2015).
The Panel considers the information as supportive for the assessment of LNT.
3.11. Allergenicity
The protein content in the NF is very low with a level that is below 0.01% (w/w) (limit of reporting 17 mg/kg) as indicated in the specifications (Table 2). The applicant provided evidence for the absence of microorganisms in the NF.
In addition, the applicant has assessed the allergenic potential of introduced proteins as a result of the genetic modification of the E. coli K‐12 host (which itself is recognised as non‐allergenic) using the search algorithms provided by the Allergen Online tool (version 17) of the University of Nebraska (FARRP, 2017). No sequence alerts for potential allergenicity were identified.
The Panel considers that the likelihood of allergenic reactions to the NF is very low.
4. Discussion
The NF is a powdered mixture mainly composed by LNT, but also containing d‐lactose and other oligosaccharides such as para‐lacto‐N‐hexaose‐2 (para‐LNH‐2), lacto‐N‐triose II and a small fraction of other carbohydrates. The NF is obtained by microbial fermentation with a genetically modified strain of E. coli K‐12. The information provided on the manufacturing process, composition and specifications of the NF, including absence of DNA from the producing microorganisms, does not raise safety concerns.
The applicant intends to add the NF to a variety of foods, including IF and follow‐on formula, foods for infants and young children, foods for special medical purposes and food supplements. The target population is the general population except for food supplements, for which the target population is individuals above 1 year of age.
Considering that LNT is a naturally occurring oligosaccharide present in human milk, the history of human exposure to LNT concerns breastfed infants. LNT is one of the most abundant HMO along with 2’‐FL, 6’‐SL, lacto‐N‐fucopentaose I and LNnT. The Panel notes that a safety assessment of its constitutional isomer (LNnT) when chemically synthesised has been carried out by EFSA (EFSA NDA Panel, 2015). The Panel also noted that LNnT when obtained by fermentation (E. coli K‐12 DH1) has been included in the European novel food list. A mixture of other HiMOs (2’‐FL and DFL) produced by fermentation using the same E. coli strain and genotype has been recently assessed (EFSA NDA Panel, 2019).
The Panel considers that there are no concerns regarding genotoxicity of the NF. The highest dose of 4,000 mg/kg bw per day used in the 90‐day oral toxicity study conducted in neonatal rats was considered as the NOAEL.
The Panel notes that the anticipated daily intake of LNT in the NF from the consumption of IF (only), in infants up to 16 weeks of age, does not exceed the highest intake level of LNT in breastfed infants on a bw basis. The anticipated daily intake of the NF for the proposed uses at their respective maximum use levels in the other population categories is unlikely to exceed the highest intake level of LNT in breastfed infants on a bw basis. Thus, since the intake in breastfed infants on a bw basis is expected to be safe also for other population groups, and taking into account supportive evidence provided by human intervention studies that involved the isomer LNnT and were conducted with adults and infants, the Panel considers that the intake of the NF for the proposed uses at their respective maximum use levels can be considered safe.
The maximum daily intake of the NF as food supplement (i.e. 2 g/day) for individuals above one year of age does not exceed the highest intake level of LNT in breastfed infants per kg bw. Food supplements are not intended to be used if other foods with added LNT (as well as breast milk for young children) are consumed on the same day.
The Panel notes that for other oligosaccharides present as a small fraction in the NF (i.e. lacto‐N‐triose II and para‐LNH‐2) a comparison with exposures from human milk cannot be performed.
When comparing the NOAEL from the 90‐day toxicity study with the estimated exposure per population category (at 95th percentile; Table 7) the margins of exposure are ranging from 7 to 138. It is also noted that with substances of this nature the maximum feasible doses that can be used in subchronic studies (because of viscosity and risk of nutritional imbalance) are only able to ensure a relatively low safety margin with respect to the highest estimated daily intakes in the intended population.
However, taking into account the intrinsic nature of HMOs with their limited absorption, the low levels in the NF, the absence of toxicologically relevant effects in the subchronic study up to the highest dose tested and considering that infants are naturally exposed to these substances, the Panel considers that no safety concerns arise.
For foods for special medical purposes, the applicant did not propose maximum use levels and the Panel considers that the maximum use levels of the NF should not be higher than the maximum levels specified for the proposed food uses or the maximum daily intake proposed for food supplements.
5. Conclusions
The Panel concludes that the NF, composed of LNT and other structurally related oligosaccharides, is safe under the proposed conditions of use. The target population is the general population, except for food supplement for which the target population is limited to individuals above 1 year of age.
Food supplements are not intended to be used if other foods with added LNT or breast milk are consumed the same day.
The Panel could not have reached the conclusions on the safety of the NF under the proposed conditions of use without the following data claimed as proprietary by the applicant:
annexes to the dossier which relate to the identity, the production process, composition and specifications of the NF (see annexes indicated in section 2.1).
bacterial reverse mutation test (unpublished study report, 2018a), in vitro micronucleus test (unpublished study report, 2018b, 2019), and 90‐day oral toxicity study with the NF (Unpublished study report, 2018d) including the summary table of the statistically significant observations in the 90‐day study (Appendix B.3 to the dossier). The results of these studies have been published by Phipps et al. (2018).
Steps taken by EFSA
Letter from the European Commission to the European Food Safety Authority with the request for a scientific opinion on the safety of lacto‐N‐tetraose as a novel food. Ref. Ares (2018)4459745, dated 30/08/2018.
On 30/08/2018, a valid application from the European Commission on lacto‐N‐tetraose as NF, which was submitted by Glycom A/S, was made available to EFSA by the European Commission through Commission e‐submission portal (NF 2018/0524) and the scientific evaluation procedure started.
On 28/02/2019 and 27/05/2019, EFSA requested the applicant to provide additional information to accompany the application and the scientific evaluation was suspended.
On 10/05/2019 and 21/08/2019, additional information was provided by the applicant and the scientific evaluation was restarted.
During its meeting on 30/10/2019, the NDA Panel, having evaluated the data, adopted a scientific opinion on the safety of lacto‐N‐tetraose as a NF pursuant to Regulation (EU) 2015/2283.
Abbreviations
- 2’‐FL
2’ fucosyllactose
- ADME
absorption, distribution, metabolism and excretion
- ALT
alanine aminotransferase
- AST
aspartate aminotransferase
- bw
body weight
- CFU
colony forming units
- DFL
difucosyllactose
- DRF
dose range finding
- DSMZ
German Collection of Microorganisms and Cell Cultures (Deutsche Sammlung von Mikroorganismen und Zellkulturen)
- EU
endotoxin units
- Eur.Ph.
European pharmacopeia
- FAIM
Food Additive Intake Model
- FL
fucosyllactose
- FOF
follow‐on formula
- Gal
galactose
- GlcNAc
N‐acetylglucosamine
- GLP
Good Laboratory Practice
- GMP
Good Manufacturing Practice
- GRAS
generally recognized as safe
- HACCP
Hazard Analysis Critical Control Points
- HiMO
human identical milk oligosaccharides
- HiMS
human identical milk saccharides
- HMO
human milk oligosaccharide
- HPAEC‐PAD
high‐performance anion exchange chromatography/pulsed amperometric detection
- HPLC/CAD
high‐performance liquid chromatography/charged aerosol detection
- HMBC
heteronuclear multiple bond correlation
- HSQC
heteronuclear single quantum coherence
- IF
infant formula
- ISO
International Organization for Standardization
- KF
Karl–Fischer
- LC‐PUFA
long‐chain polyunsaturated fatty acids
- LNH
lacto‐N‐hexaose
- LNT
lacto‐N‐tetraose
- LNnT
lacto‐N‐neotetraose
- LOQ
limit of quantification
- LOR
limit of reporting
- LUC
large unstained cells
- MCH
mean cell haemoglobin
- MCHC
mean cell haemoglobin concentration
- MCV
mean cell volume
- MS
mass spectrometry
- GlcNAc
N‐acetylglucosamine
- NF
novel food
- NOAEL
no observed adverse effect level
- NOESY
nuclear overhauser effect spectroscopy
- NMR
1H‐nuclear magnetic resonance spectroscopy
- OECD
Organisation for Economic Co‐operation and Development
- PAD
pulsed amperometric detection
- para‐LNH‐2
para‐lacto‐N‐hexaose‐2
- PCR
polymerase chain reaction
- QPS
qualified presumption of safety
- RBC
red blood cells
- RDW
red cell distribution width
- RH
relative humidity
- RT
retention time
- SL
sialyllactose
- UHT
ultra‐high temperature
- UV
ultraviolet
- WBC
white blood cells
- zqTOCSY
zero quantum total correlation spectroscopy
Appendix A – Summary results of the 90‐day repeated dose toxicity study with the NF
Summary results of parameters with statistically significant differences in the 90‐day repeated dose toxicity study with the NF (unpublished study report, 2018d)
| Parameters | Exposure (day) | Sex | Control | Oligofructose control (4,000 mg/kg bw) |
Low dose (1,000 mg/kg bw) |
Mid dose (2,500 mg/kg bw) |
High dose (4,000 mg/kg bw) |
|---|---|---|---|---|---|---|---|
| Body weight (g) | 4 | F | 20.3 ± 1.33 | 21.9 ± 2.89* | 20.7 ± 1.96 | 22.1 ± 1.33* | 21.9 ± 2.19* |
| 5 | M | 23.1 ± 1.58 | 24.7 ± 2.32* | 24.2 ± 2.03 | 25.0 ± 1.94* | 24.3 ± 2.34* | |
| 5 | F | 22.3 ± 1.41 | 24.2 ± 3.21** | 22.6 ± 2.02 | 24.6 ± 1.29** | 23.8 ± 2.39** | |
| 6 | M | 24.8 ± 1.49 | 27.3 ± 2.53** | 26.5 ± 2.42* | 27.3 ± 1.84** | 26.7 ± 2.57** | |
| 6 | F | 23.8 ± 1.46 | 26.7 ± 3.53** | 24.7 ± 2.20 | 26.9 ± 1.66** | 26.3 ± 2.71** | |
| 7 | M | 26.5 ± 1.95 | 30.0 ± 2.70** | 29.0 ± 2.82** | 29.8 ± 2.14** | 29.2 ± 2.99** | |
| 7 | F | 25.4 ± 1.75 | 29.4 ± 3.76** | 27.3 ± 2.67 | 29.4 ± 1.86** | 28.8 ± 3.06** | |
| 8 | M | 28.7 ± 2.51 | 32.1 ± 3.16** | 30.8 ± 3.06* | 31.7 ± 2.03* | 31.1 ± 2.93* | |
| 8 | F | 27.7 ± 2.20 | 31.5 ± 4.08** | 29.2 ± 2.58 | 31.2 ± 1.82** | 30.6 ± 3.07** | |
| 9 | M | 31.5 ± 2.78 | 33.9 ± 3.59* | 33.0 ± 3.77 | 34.1 ± 2.48* | 34.1 ± 3.55* | |
| 9 | F | 30.3 ± 2.45 | 33.7 ± 4.52** | 31.0 ± 2.96 | 33.4 ± 2.14* | 33.6 ± 3.33** | |
| 10 | M | 33.5 ± 2.79 | 36.4 ± 4.91* | 35.1 ± 4.24 | 37.2 ± 3.13* | 36.4 ± 3.64* | |
| 10 | F | 32.2 ± 2.96 | 35.9 ± 5.53** | 32.9 ± 3.33 | 36.1 ± 2.34** | 36.0 ± 3.45** | |
| 11 | F | 34.2 ± 3.85 | 37.5 ± 5.73* | 35.4 ± 3.78 | 39.0 ± 2.46** | 37.7 ± 3.37** | |
| 12 | F | 36.6 ± 4.49 | 39.6 ± 5.98 | 37.2 ± 4.34 | 41.5 ± 2.72** | 40.7 ± 3.95** | |
| 13 | F | 40.3 ± 4.93 | 43.2 ± 6.55 | 39.1 ± 5.06 | 45.2 ± 3.73* | 43.9 ± 3.93* | |
| 15 | F | 47.6 ± 5.79 | 50.7 ± 7.54 | 47.5 ± 5.39 | 53.2 ± 3.96* | 50.8 ± 4.20* | |
| 18 | F | 60.0 ± 6.3 | 64 ± 8.6 | 61 ± 6.3 | 67 ± 4.1* | 64 ± 5.4* | |
| 22 | F | 80.0 ± 7.3 | 83 ± 10.4 | 81 ± 7.1 | 88 ± 4.8* | 84 ± 7.3* | |
| Food consumption | 29‐32 | M | 22.0 ± 2.0 | 20.0 ± 1.4 | 21.0 ± 0.7 | 22.0 ± 0.6 | 20.0 ± 0.7* |
| (g/animal/day) | 57‐60 | M | 30.0 ± 1.0 | 28.0 ± 3.1 | 29.0 ± 0.9 | 30.0 ± 1.9 | 27.0 ± 0.8* |
| 60‐64 | M | 29.0 ± 1.1 | 27.0 ± 2.0 | 27.0 ± 0.3 | 29.0 ± 1.5 | 27.0 ± 0.7* | |
| 74‐78 | M | 28.0 ± 1.0 | 27.0 ± 1.9 | 27.0 ± 0.2 | 28.0 ± 0.9 | 26.0 ± 1.1* | |
| 78‐81 | M | 29.0 ± 0.5 | 27.0 ± 3.0 | 28.0 ± 0.3 | 29.0 ± 1.0 | 27.0 ± 0.2** | |
|
Ulna length (mm) |
22 | F | 25.4 ± 0.48 | 25.3 ± 0.85 | 25.0 ± 0.81 | 25.3 ± 0.56 | 25.9 ± 0.51* |
| 78 | M | 40.1 ± 1.15 | 39.4 ± 1.00 | 39.8 ± 1.08 | 39.9 ± 1.12 | 39.0 ± 0.85** | |
| 78 | F | 37.3 ± 0.88 | 36.0 ± 0.82** | 36.8 ± 1.00 | 36.4 ± 0.93* | 36.3 ± 0.85** | |
| Sexual maturation | |||||||
| Body weight (g) at vaginal opening | F | 111 ± 13.5 | 123 ± 22.2 | 117 ± 11.7 | 128 ± 14.4* | 121 ± 13.8* | |
| Haematology | |||||||
| Haematocrit (L/L) | 90 | F | 0.417 ± 0.03 | 0.388 ± 0.02** | 0.419 ± 0.02 | 0.419 ± 0.03 | 0.388 ± 0.01* |
| week 4 rec | F | 0.405 ± 0.02 | 0.391 ± 0.01 | 0.401 ± 0.01 | 0.389 ± 0.02 | 0.378 ± 0.01* | |
| Haemoglobin (g/dL) | week 4 rec | F | 15.5 ± 0.66 | 14.9 ± 0.34* | 15.3 ± 0.33 | 14.8 ± 0.51* | 14.5 ± 0.32** |
| Erythrocytes (x1012/L) | week 4 rec | F | 7.57 ± 0.26 | 7.39 ± 0.26* | 7.50 ± 0.14 | 7.35 ± 0.32 | 6.86 ± 0.17** |
| MCH (pg) | 90 | M | 19.3 ± 0.75 | 19.8 ± 0.56* | 19.3 ± 0.59* | 19.8 ± 0.85 | 20.1 ± 0.48* |
| week 4 rec | F | 20.5 ± 0.50 | 20.1 ± 0.56 | 20.3 ± 0.56 | 20.1 ± 0.30 | 21.2 ± 0.45* | |
| MCHC (g/dL) | 90 | M | 35.0 ± 1.69 | 36.7 ± 0.44* | 34.9 ± 1.55 | 35.3 ± 2.05 | 37.0 ± 0.79** |
| F | 35.2 ± 1.73 | 36.5 ± 0.74 | 35.5 ± 1.73 | 35.7 ± 1.75 | 36.9 ± 0.75* | ||
| MCV | 90 | F | 56.7 ± 2.24 | 55.0 ± 1.11* | 56.4 ± 1.42 | 56.7 ± 1.97 | 54.9 ± 1.77* |
| week 4 rec | F | 53.5 ± 1.03 | 52.9 ± 1.31 | 53.4 ± 1.54 | 52.9 ± 1.16 | 55.1 ± 0.69* | |
| Red cell distribution width (%) | 90 | F | 11.7 ± 0.32 | 11.4 ± 0.40 | 11.5 ± 0.53 | 11.3 ± 0.31* | 11.1 ± 0.39** |
| week 4 rec | F | 11.2 ± 0.23 | 11.3 ± 0.13 | 11.3 ± 0.53 | 11.2 ± 0.19 | 11.9 ± 0.78* | |
| Leukocytes (X109/L) | 90 | M | 8.70 ± 1.62 | 9.39 ± 1.50 | 10.07 ± 2.13 | 10.39 ± 1.97 | 12.67 ± 3.28** |
| Lymphocytes (X109/L) | 90 | M | 7.13 ± 1.35 | 8.01 ± 1.33 | 8.37 ± 1.95 | 8.51 ± 1.58 | 10.81 ± 2.85 |
| Eosinophils (X109/L) | 90 | M | 0.08 ± 0.02 | 0.09 ± 0.04 | 0.10 ± 0.04* | 0.07 ± 0.03 | 0.12 ± 0.05* |
| LUC (X109/L) | 90 | M | 0.05 ± 0.02 | 0.06 ± 0.02 | 0.06 ± 0.03 | 0.06 ± 0.03 | 0.08 ± 0.04* |
| Platelet count (X109/L) | 90 | M | 886 ± 75.7 | 959 ± 77.4* | 961 ± 57.5 | 918 ± 57.0 | 969 ± 97.7* |
| Clinical chemistry parameters | |||||||
| ALT (U/L) | 90 | M | 31 ± 4.5 | 34 ± 2.4 | 30 ± 3.6 | 36 ± 6.4* | 36 ± 5.6 |
| AST (U/L) | 90 | F | 90 ± 9.3 | 84 ± 12.2 | 79 ± 8.3 | 72 ± 7.1* | 101 ± 64.6* |
| Urea (mmol/L) | 90 | M | 6.01 ± 0.98 | 4.38 ± 0.35** | 6.05 ± 0.74 | 7.06 ± 0.68** | 5.21 ± 0.54* |
| 90 | F | 7.13 ± 0.98 | 5.74 ± 0.69** | 7.03 ± 0.80 | 7.14 ± 0.94 | 6.22 ± 0.38* | |
| Creatinine (μmol/L) | 90 | F | 33 ± 4.4 | 28 ± 2.4* | 30 ± 2.5 | 29 ± 4.0** | 28 ± 3.2** |
| week 4 rec | F | 37 ± 4.7 | 31 ± 2.6** | 29 ± 2.9 | 35 ± 2.7* | 31 ± 3.0* | |
| Cholesterol (mmol/L) | 90 | M | 1.31 ± 0.22 | 1.44 ± 0.23 | 1.28 ± 0.25 | 1.24 ± 0.22 | 1.60 ± 0.32* |
| Potassium (mmol/L) | 90 | M | 4.7 ± 0.30 | 4.5 ± 0.27 | 4.7 ± 0.13 | 4.7 ± 0.31 | 4.4 ± 0.27* |
| Chloride (mmol/L) | 90 | F | 98 ± 1.4 | 99 ± 2.1 | 98 ± 0.8 | 98 ± 0.9 | 100 ± 2.3** |
| week 4 rec | M | 99 ± 1.2 | 100 ± 1.0 | 100 ± 0.8 | 100 ± 1.2 | 101 ± 0.5* | |
| Calcium (mmol/L) | 90 | M | 2.53 ± 0.03 | 2.59 ± 0.07* | 2.60 ± 0.06 | 2.55 ± 0.1 | 2.64 ± 0.06** |
| Inorganic phosphorus (mmol/L) | 90 | M | 2.06 ± 0.24 | 2.31 ± 0.24 | 2.15 ± 0.27 | 2.17 ± 0.30 | 2.42 ± 0.19 |
| A/G (Ratio) | week 4 rec | M | 1.01 ± 0.09 | 1.02 ± 0.09 | 1.06 ± 0.09 | 1.03 ± 0.09 | 1.14 ± 0.10* |
| Urinalysis | |||||||
| Volume (mL) | 90 | F | 4.8 ± 1.78 | 5.8 ± 2.45 | 5.5 ± 1.06 | 6.4 ± 2.58 | 7.5 ± 2.92* |
| pH | 90 | F | 6.7 ± 0.24 | 7.1 ± 0.72 | 7.2 ± 0.30 | 7.2 ± 0.41 | 7.6 ± 0.61** |
| Specific gravity (g/L) | 90 | M | 1029 ± 5.3 | 1024 ± 3.9 | 1028 ± 4.8 | 1024 ± 3.9* | 1024 ± 5.9* |
| 90 | F | 1037 ± 6.9 | 1028 ± 10.6 | 1030 ± 2.9 | 1029 ± 8.3* | 1024 ± 4.7** | |
| Total proteins (mg) | 90 | M | 6.77 ± 3.22 | 5.89 ± 2.16 | 6.11 ± 1.54* | 7.61 ± 3.21* | 6.68 ± 2.35** |
| Organ weight (adjusted mean values) | – | ||||||
| Kidneys (g) | week 4 rec | F | 1.97 | 2.05 | 2.08 | 2.12 | 2.17*3 |
| Liver (g) | week 4 rec | F | 10.57 | 10.92 | 11.19 | 11.04 | 12.48* |
| Ovaries (g) | week 4 rec | F | 0.088 | 0.104* | 0.089 | 0.098 | 0.108** |
| Pituitary (g) | week 4 rec | M | 0.016 | 0.015 | 0.015 | 0.014* | 0.013* |
| Spleen (g) | week 4 rec | F | 0.566 | 0.605 | 0.536 | 0.538 | 0.725* |
| Testes (g) | 90 | M | 3.380 | 3.548* | 3.465 | 3.723* | 3.580* |
MCH: mean cell haemoglobin; MCHC: mean cell haemoglobin concentration; MCV: mean cell volume; RDW: red cell distribution width; LUC: large unstained cells; ALT: alanine aminotransferase; AST: aspartate aminotransferase; A/G: albumin/globulin ratio.
Significantly different from control (p < 0.05) (Vehicle control vs LNT‐treated groups or reference control);
Significantly different from control (p < 0.01) (control vs LNT‐treated groups or reference control).
Supporting information
Contribution of each survey to the estimated intake of the NF (LNT and related fractions) for each population group
Suggested citation: EFSA NDA Panel (EFSA Panel on Nutrition, Novel Foods and Food Allergens) , Turck D, Castenmiller J, De Henauw S, Hirsch‐Ernst KI, Kearney J, Maciuk A, Mangelsdorf I, McArdle HJ, Naska A, Pelaez C, Pentieva K, Siani A, Thies F, Tsabouri S, Vinceti M, Cubadda F, Engel KH, Frenzel T, Heinonen M, Marchelli R, Neuhäuser‐Berthold M, Poulsen M, Sanz Y, Schlatter JR, van Loveren H, Colombo P and Knutsen HK, 2019. Scientific Opinion on the safety of lacto‐N‐tetraose (LNT) as a novel food pursuant to Regulation (EU) 2015/2283. EFSA Journal 2019;17(12):5907, 27 pp. 10.2903/j.efsa.2019.5907
Requestor: European Commission following an application by Glycom A/S
Question number: EFSA‐Q‐2018‐00589
Panel members: Dominique Turck, Jacqueline Castenmiller, Stefaan De Henauw, Karen Ildico Hirsch‐Ernst, John Kearney, Helle Katrine Knutsen, Alexandre Maciuk, Inge Mangelsdorf, Harry J McArdle, Androniki Naska, Carmen Pelaez, Kristina Pentieva, Alfonso Siani, Frank Thies, Sophia Tsabouri and Marco Vinceti.
Acknowledgements: The Panel wishes to thank Davide Arcella for the support provided to this scientific opinion.
Adopted: 30 October 2019
Notes
Regulation (EU) 2015/2283 of the European Parliament and of the Council on novel foods, amending Regulation (EU) No 1169/2011 of the European Parliament and of the Council and repealing Regulation (EC) N0 258/97 of the European Parliament and of the Council and Commission Regulation (EC) No 1852/2001 (2013/0435 (COD). OJ L 327, 11.12.2015, pp. 1–22.
Commission Implementing Regulation (EU) 2017/2469 of 20 December 2017 laying down administrative and scientific requirements for applications referred to in Article 10 of Regulation (EU) 2015/2283 of the European Parliament and of the Council on novel foods. OJ L 351, 30.12.2017, pp. 64–71.
Commission Implementing Regulation (EU) 2017/2470 of 20 December 2017 establishing the Union list of novel foods in accordance with Regulation (EU) 2015/2283 of the European Parliament and of the Council on novel foods (Text with EEA relevance).
References
- Albrecht S, Schols HA, van den Heuvel EGHM, Voragen AGJ and Gruppen H, 2011. Occurrence of oligosaccharides in feces of breast‐fed babies in their first six months of life and the corresponding breast milk. Carbohydrate Research, 346, 2540–2550. [DOI] [PubMed] [Google Scholar]
- Albrecht S, Lane JA, Marino K, Al Busadah KA, Carrington SD, Hickey RM and Rudd PM, 2014. A comparative study of free oligosaccharides in the milk of domestic animals. British Journal of Nutrition, 111, 1313–1328. [DOI] [PubMed] [Google Scholar]
- Aldredge DL, Geronimo MR, Hua S, Nwosu CC, Lebrilla CB and Barile D, 2013. Annotation and structural elucidation of bovine milk oligosaccharides and determination of novel fucosylated structures. Glycobiology, 23, 664–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asakuma S, Urashima T, Akahori M, Obayashi H, Nakamura T, Kimura K, Watanabe Y, Arai I and Sanai Y, 2008. Variation of major neutral oligosaccharides levels in human colostrum. European Journal of Clinical Nutrition, 62, 488–494. [DOI] [PubMed] [Google Scholar]
- Asakuma S, Hatakeyama E, Urashima T, Yoshida E, Katayama T, Yamamoto K, Kumagai H, Ashida H, Hirose J and Kitaoka M, 2011. Physiology of consumption of human milk oligosaccharides by infant gut‐associated Bifidobacteria. Journal of Biological Chemistry, 286, 34583–34592 [plus supplementary data]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin S, De Castro CA, Benet T, Hou Y, Sun H, Thakkar SK, Vinyes‐Pares G, Zhang Y and Wang P, 2016. Temporal change of the content of 10 oligosaccharides in the milk of Chinese urban mothers. Nutrients, 8, 346, 22 pp. 10.3390/nu8060346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bidart GN, Rodriguez‐Diaz J and Yebra MJ, 2016. Extracellular Wall‐Bound‐N‐Acetylglucosaminidase from Lactobacillus casei Is Involved in the Metabolism of the Human Milk Oligosaccharide Lacto‐N‐Triose. Applied and Environmental Microbiology, 82, 570–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blattner FR, Plunkett G 3rd, Bloch CA, Perna NT, Burland V, Riley M, Collado‐Vides J, Glasner JD, Rode CK, Mayhew GF, Gregor J, Davis NW, Kirkpatrick HA, Goeden MA, Rose DJ, Mau B and Shao Y, 1997. The complete genome sequence of Escherichia coli K‐12. Science, 277, 1453–1462. [DOI] [PubMed] [Google Scholar]
- Bode L, 2012. Human milk oligosaccharides: every baby needs a sugar mama. Glycobiology, 22, 1147–1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand‐Miller JC, McVeagh P, McNeil Y and Gillard B, 1995. Human milk oligosaccharides are not digested and absorbed in the small intestine of young infants. Proceedings of the Nutrition Society of Australia, 19, 44. [Google Scholar]
- Brand‐Miller JC, McVeagh P, McNeil Y and Messer M, 1998. Digestion of human milk oligosaccharides by healthy infants evaluated by the lactulose hydrogen breath test. The Journal of Pediatrics, 133, 95–98. [DOI] [PubMed] [Google Scholar]
- Chai W, Piskarev V and Lawson AM, 2001. Negative‐ion electrospray mass spectrometry of neutral underivatized oligosaccharides. Analytical Chemistry, 73, 651–657. [DOI] [PubMed] [Google Scholar]
- Chaturvedi P, Warren CD, Buescher CR, Pickering LK and Newburg DS, 2001. Survival of human milk oligosaccharides in the intestine of infants. In: Bioactive components of human milk. (Advances in experimental medicine and biology, volume 501) Ed Newberg DS, Springer Science+Business Media, New York, 315–323. [DOI] [PubMed]
- Coppa GV, Pierani P, Zampini L, Carloni I, Carlucci A and Gabrielli O, 1999. Oligosaccharides in human milk during different phases of lactation. Acta Paediatrica, Suppl, 430, 89–94. [DOI] [PubMed] [Google Scholar]
- Coppa GV, Pierani P, Zampini L, Bruni S, Carloni I and Gabrielli O, 2001. Characterization of oligosaccharides in milk and faeces of breast‐fed infants by high‐performance anion‐exchange chromatography. Advances in Experimental Medicine and Biology, 501, 307–314. [DOI] [PubMed] [Google Scholar]
- Coulet M, Phothirath P, Constable A, Mardsen E and Schilter B, 2013. Pre‐clinical safety assessment of the synthetic human milk, nature‐identical, oligosaccharide Lacto‐N‐neotetraose (LNnT). Food and Chemical Toxicology, 62, 528–537. [DOI] [PubMed] [Google Scholar]
- Dabrowski U, Egge H and Dabroswki J, 1983. Proton‐nuclear magnetic resonance study of peracetylated derivatives of ten oligosaccharides isolated from human milk. Archives of Biochemistry and Biophysics., 224, 254–260. [DOI] [PubMed] [Google Scholar]
- De Leoz MLA, Gaerlan SC, Strum JS, Dimapasoc LM, Mirmiran M, Tancredi DJ, Smilowitzc JT, Kalanetra KM, Mills DA, German JB, Lebrilla CB and Underwood MA, 2012. Lacto N Tetraose, Fucosylation, and Secretor Status are Highly Variable in Human Milk Oligosaccharides From Women Delivering Preterm. Journal Proteome Research, 11, 4662–4672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EFSA (European Food Safety Authority), 2011. Use of the EFSA Comprehensive European Food Consumption Database in Exposure Assessment. EFSA Journal 2011;9(3):2097, 34 pp. 10.2903/j.efsa.2011.2097 [DOI] [Google Scholar]
- EFSA BIOHAZ Panel (EFSA Panel on Biological Hazards), 2018. Statement on the update of the list of QPS‐recommended biological agents intentionally added to food or feed as notified to EFSA 7: suitability of taxonomic units notified to EFSA until September 2017. EFSA Journal 2018;16(1):5131, 43 pp. 10.2903/j.efsa.2018.5131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- EFSA FEEDAP Panel (EFSA Panel on Additives and Products or Substances used in Animal Feed), 2018. Guidance on the characterisation of microorganisms used as feed additives or as production organisms. EFSA Journal 2018;16(3):5206, 24 pp. 10.2903/j.efsa.2018.5206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies), 2013. Scientific Opinion on nutrient requirements and dietary intakes of infants and young children in the European Union. EFSA Journal 2013;11(10):3408, 103 pp. 10.2903/j.efsa.2013.3408 [DOI] [Google Scholar]
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies), 2014. Scientific Opinion on the essential composition of infant and follow‐on formulae. EFSA Journal 2014;12(7):3760, 106 pp. 10.2903/j.efsa.2014.3760 [DOI] [Google Scholar]
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies), 2015. Scientific opinion on the safety of lacto‐N‐neotetraose as a novel food ingredient pursuant to Regulation (EC) No 258/97. EFSA Journal 2015;13(7):4183, 32 pp. 10.2903/j.efsa.2015.4183 [DOI] [Google Scholar]
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies), 2016. Guidance on the preparation of an application for authorisation of a novel food in the context of Regulaton (EU) 2015/2283. EFSA Journal 2016;14(11):4594, 24 pp. 10.2903/j.efsa.2016.4594 [DOI] [Google Scholar]
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies), 2019. Safety of 2’‐fucosyllactose/difucosyllactose mixture as a novel food pursuant to Regulation (EU) 2015/2283. EFSA Journal 2019;17(6):5717, 23 pp. 10.2903/j.efsa.2019.5717 [DOI] [Google Scholar]
- EFSA Scientific Committee , 2012. Guidance on selected default values to be used by the EFSA Scientific Committee, Scientific Panels and Units in the absence of actual measured data. EFSA Journal 2012;10(3):2579, 32 pp. 10.2903/j.efsa.2012.2579 [DOI] [Google Scholar]
- EFSA Scientific Committee , 2017. Guidance on the risk assessment of substances present in food intended for infants below 16 weeks of age. EFSA Journal 2017;15(5):4849, 58 pp. 10.2903/j.efsa.2017.4849. Available online: https://www.efsa.europa.eu/en/efsajournal/pub/4849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- EMEA , 2008. Guideline on the need for non‐clinical testing in juvenile animals of pharmaceuticals for paediatric indications. Ref. EMEA/CHMP/SWP/169215/2005
- Engfer MB, Stahl B, Finke B, Sawatzki G and Daniel H, 2000. Human milk oligosaccharides are resistant to enzymatic hydrolysis in the upper gastrointestinal tract. The American Journal of Clinical Nutrition, 71, 1589–1596. [DOI] [PubMed] [Google Scholar]
- Erney RM, Malone WT, Skelding MB, Marcon AA, Kleman‐Leyer KM, O'Ryan ML, Ruiz‐Palacios G, Hilty MD, Pickering LK and Prieto PA, 2000. Variability of human milk neutral oligosaccharides in a diverse population. Journal of Pediatric Gastroenterology and Nutrition, 30, 181–192. [DOI] [PubMed] [Google Scholar]
- Erney R, Hilty M, Pickering L, Ruiz‐Palacios G and Prieto P, 2001. Human milk oligosaccharides: a novel method provides insight into human genetics. In: Bioactive components of human milk. 8th International Conference of the International Society for Research on Human Milk and Lactation, Oct. 25‐29, 1997, Plymouth, Mass. Ed., Newburg DS. Kluwer Academic/Plenum Publishers, New York. Advances in Experimental Medicine and Biology, vol 501, 285–297 [PubMed]
- FAIM (Food Additives Intake Model) 2.0, 2017. Available online http://www.efsa.europa.eu/en/applications/foodingredients/tools
- FARRP (Food Allergy Research and Resource Program), 2017. AllergenOnline version 17: home of the FARRP allergen protein database. University of Nebraska‐Lincoln, Food Allergy Research and resource Program (FARRP), Lincoln, NE. Available online: http://www.allergenonline.org/[Accessed: 18 January 2017).
- Galeotti F, Coppa GV, Zampini L, Maccari F, Galeazzi T, Padella L, Santoro L, Gabrielli O and Volpi N, 2012. On‐line high‐performance liquid chromatography‐fluorescence detection‐electrospray ionization‐mass spectrometry profiling of human milk oligosaccharides derivatized with 2‐aminoacridone. Analytical Biochemistry, 430, 97–104 [plus supplementary Appendix A]. [DOI] [PubMed]
- Galeotti F, Coppa GV, Zampini L, Maccari F, Galeazzi T, Padella L, Santoro L, Gabrielli O and Volpi N, 2014. Capillary electrophoresis separation of human milk neutral and acidic oligosaccharides derivatized with 2‐aminoacridone. Electrophoresis, 36, 811–818. [DOI] [PubMed] [Google Scholar]
- Gnoth MJ, Kunz C, Kinne‐Saffran E and Rudloff S, 2000. Human milk oligosaccharides are minimally digested in vitro. The Journal of Nutrition, 130, 3014–3020. [DOI] [PubMed] [Google Scholar]
- Gnoth MJ, Rudloff S, Kunz C and Kinne RK, 2001. Investigations of the in vitro transport of human milk oligosaccharides by a Caco‐2 monolayer using a novel high‐performance liquid chromatography‐mass spectrometry technique. Journal of Biological Chemistry, 276, 34363–34370. [DOI] [PubMed] [Google Scholar]
- Goehring KC, Kennedy AD, Prieto PA and Buck RH, 2014. Direct evidence for the presence of human milk oligosaccharides in the circulation of breastfed infants. PLoS ONE, 9, e101692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorbach SL, 1978. Recombinant DNA: an infectious disease perspective. Journal of Infectious Diseases, 137, 615–623. [DOI] [PubMed] [Google Scholar]
- Honda Y, Nischimoto M, Katayama T and Kitaoka M, 2013. Characterization of the Cytosolic β‐N‐Acetylglucosaminidase from Bifidobacterium longum subsp. longum . Journal of Applied Glycosciences, 60, 141–146. [Google Scholar]
- Hosomi O and Takeya A, 1988. The relationship between the (β1‐3) N‐acetylglucosaminytransferase and the presence of oligosaccharides containing lacto‐N‐triose II structure in bovine and human milk. Japanese Journal of Veterinary Sciences, 51, 1–6. [DOI] [PubMed] [Google Scholar]
- Kuhn R, Baer HH and Gauhe A, 1956. Kristallisierte fucoside‐lactose. Chemische Berichte, 88, 1135. [Google Scholar]
- Kunz C, Meyer C, Collado MC, Geiger L, Garcıa‐Mantrana I, Bertua‐Rıos B, Martınez‐Costa C, Borsch C and Rudloff S, 2016. Influence of Gestational Age, Secretor, and Lewis Blood Group Status on the Oligosaccharide Content of Human Milk. JPGN, 64, 789–798. [DOI] [PubMed] [Google Scholar]
- Lukjancenko O, Wassenaar TM and Ussery DW, 2010. Comparison of 61 sequenced Escherichia coli genomes. Microbial Ecology, 60, 708–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire MK, Meehan CL, McGuire MA, Williams JE, Foster J, Sellen DW, Kamau‐Mbuthia EW, Kamundia EW, Mbugua S, Moore SE, Prentice AM, Kvist LJ, Otoo GE, Brooker SL, Price WJ, Shafii B, Placek C, Lackey KA, Robertson B, Manzano S, Ruız L, Rodrıguez JM, Pareja RG and Bode L, 2017. What's normal? Oligosaccharide concentrations and profiles in milk produced by healthy women vary eographically. The American Journal of Clinical Nutrition, 105, 1086–1100 [plus supplementary data]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miwa M, Horimoto T, Kiyohara M, Katayama T, Kitaoka M, Ashida H and Yamamoto K, 2010. Cooperation of β‐galactosidase and β‐N‐acethylhexosaminidase from bifidobacterial in assimilation of human milk oligosaccharides with type 2 structure. Glycobiology, 20, 1402–1409. [DOI] [PubMed] [Google Scholar]
- Muhldorfer I and Hacker J, 1994. Genetic aspects of Escherichia coli virulence. Microbial Pathogenesis, 16, 171–181. [DOI] [PubMed] [Google Scholar]
- OECD (Organisation for Economic Co‐operation and Development), 1986. Recombinant DNA safety considerations [“Blue Book”]. Available online: https://www.oecd.org/sti/biotech/40986855.pdf
- OECD (Organisation for Economic Co‐operation and Development), 1997. Test No. 471: Bacterial reverse mutation test. In: OECD guidelines for the testing of chemicals, Section 4: Health effects, 11 pp.
- OECD (Organisation for Economic Co‐operation and Development), 1998a. OECD Principles of good laboratory practice (as revised in 1997). OECD series on principles of good laboratory practice and compliance monitoring, number 1, ENV/MC/CHEM(98)17, 41 pp.
- OECD (Organisation for Economic Co‐operation and Development), 1998b. Test No. 408: Repeated dose 90‐day oral toxicity study in rodents. In: OECD guidelines for the testing of chemicals, Section 4: Health effects, 10 pp.
- OECD (Organisation for Economic Co‐operation and Development), 2016. Test No. 487: In vitro mammalian cell micronucleus test. In: OECD guidelines for the testing of chemicals, Section 4: Health effects, 29 pp.
- Pfenniger A, Karas M, Finke B and Stahl B, 2002. Structural analysis of underivatized neutral human milk oligosaccharides in the negative ion mode by nano‐electrospray MSn. Journal of the American Society for Mass Spectrometry, 11, 1331–1340. [DOI] [PubMed] [Google Scholar]
- Phipps KR, Baldwin N, Lynch B, Stannard DR, Soltesova A, Gilby B, Miks MH and Rohrig CH, 2018. Safety evaluation of the human‐identical milk oligosaccharide lacto‐N‐tetraose. Regulatory Toxicology and Pharmacology, 99, 260–273. [DOI] [PubMed] [Google Scholar]
- Rijnierse A, Jeurink PV, van Esch BCAM, Garssen J and Knippels LMJ, 2011. Food‐derived oligosaccharides exhibit pharmaceutical properties. European Journal of Pharmacology, 668, S117–S123. [DOI] [PubMed] [Google Scholar]
- Rudloff S and Kunz C, 2012. Milk oligosaccharides and metabolism in infants. American Society for Nutrition. Advances in Nutrition, 3, 398S–405S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudloff S, Pohlentz G, Diekmann L, Egge H and Kunz C, 1996. Urinary excretion of lactose and oligosaccharides in preterm infants fed human milk or infant formula. Acta Paediatrica, 1996, 598–603. [DOI] [PubMed] [Google Scholar]
- Rudloff S, Pohlentz G, Borsch C, Lentze M and Kunz C, 2012. Urinary excretion of in vivo 13C‐labelled milk oligosaccharides in breastfed infants. British Journal on Nutrition., 107, 957–963. [DOI] [PubMed] [Google Scholar]
- Spevacek AR, Smilowitz JT, Chin EL, Underwood MA, German JB and Slupsky CM, 2015. Infant maturity at birth reveals minor differences in the maternal milk metabolome in the first month of lactation. Journal of Nutrition, 145, 1698–1708[plus supplemental tables] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strecker G, Wieruszki JM, Michalscki JC and Montreuil J, 1989. Assignment of the 1H‐ and 13C‐NMR spectra of eight oligosaccharides of the lacto‐N‐tetraose and neotetraose series. Glycoconiugate Journal, 6, 67–83. [DOI] [PubMed] [Google Scholar]
- Thongaram T, Hoeflinger J, Chow JM and Miller MJ, 2017. Human milk oligosaccharide consumption by probiotic and human‐associated bifidobacterial and lactobacilli. Journal of Dairy Sciences, 100, 7825–7833. [DOI] [PubMed] [Google Scholar]
- Thurl S, Munzert M, Henker J, Boehm G, Muller‐Werner B, Jelinek J and Stahl B, 2010. Variation of human milk oligosaccharides in relation to milk groups and lactational periods. British Journal of Nutrition, 104, 1261–1271. [DOI] [PubMed] [Google Scholar]
- Thurl S, Munzert M, Boehm G, Matthews C and Stahl B, 2017. Systematic review of the concentrations of oligosaccharides in human milk. Nutrition Reviews, 75, 920–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unpublished study report , 2016a. An in vitro micronucleus assay with lacto‐N‐neotetraose (LNnT) in cultured peripheral human lymphocytes. Project 507474.
- Unpublished study report , 2016b. LNnT ‐ 13‐week oral (gavage) juvenile toxicity study in the rat followed by a 4‐week treatment‐free period. Study Number: AB20758.
- Unpublished study report , 2018a. Lacto‐N‐tetraose (amended): Bacterial Reverse Mutation Test. Study Number: SR10LR.
- Unpublished study report , 2018b. (amended). Lacto‐N‐tetraose: In Vitro Micronucleus Test in Human Lymphocytes. Study Number: QR50QW
- Unpublished study report , 2018c. (amended). Lacto‐N‐tetraose (LNT) and 3’‐O‐Sialyllactose (3’‐SL): 14‐Day Dose Range Finding Study in the Neonatal Crl:CD(SD) Rat by Oral (Gavage) Administration. Study Number: LQ48WR
- Unpublished study report , 2018d. Lacto‐N‐tetraose (LNT): 90‐Day Toxicity Study in the Neonatal Crl:CD(SD) Rat by Oral (Gavage) Administration Followed by a 4‐Week Recovery Period. Study Number: TC10BY.
- Unpublished study report , 2019. Lacto‐N‐tetraose: In Vitro Micronucleus Test in Human Lymphocytes. Study Number: QX01WX
- Urashima T, Asakuma S, Leo F, Fukuda K, Messer M and Oftedal OT, 2012. The Predominance of Type I Oligosaccharides Is a Feature Specific to Human Breast Milk. American Society for Nutrition. Adv. Nutr., 3, 473S–482S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urashima T, Taufik E, Fukuda K and Asakuma S, 2013. Recent advances in studies on milk oligosaccharides of cows and other domestic farm animals. Bioscience, Biotechnology, and Biochemistry, 77, 455–466. [DOI] [PubMed] [Google Scholar]
- Urashima T, Yamaguchi E, Ohshima T, Fukuda K and Saito T, 2018. Chemical structures of oligosaccharides in milk of the raccoon (Procyon lotor). Glycoconjugate Journal, 35, 275–286. [DOI] [PubMed] [Google Scholar]
- US EPA (U.S. Environmental Protection Agency), 1997. Escherichia coli K‐12 final risk assessment: attachment I–final risk assessment of Escherichia coli K‐12 derivatives. Available online:(Last updated on September 27, 2012).
- US FDA (Food and Drug Administration), 2006. Guidance for industry: nonclinical safety evaluation of paediatric drug products. CDER February 2006
- US FDA (Food and Drug Administration), 2016. GRAS (Generally Recognized as Safe) for lacto‐N‐neotetraose. GNR 000650. Available on: GRAS Notice (GRN) No. 659. Available online: http://www.fda.gov/Food/IngredientsPackagingLabeling/GRAS/NoticeInventory/default.htm
- Vazquez E, Santos‐Fandila A, Buck R, Rueda R and Ramirez M, 2017. Major human milk oligosaccharides are absorbed inro the systemic circulation after oral administration in rats. British Journal of Nutrition, 117, 237–247. [DOI] [PubMed] [Google Scholar]
- Yamashita K, Tachibana Y and Kobata A, 1977. Oligosaccharides of human milk. The Journal of Biological Chemistry, 252, 5408–5411. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Contribution of each survey to the estimated intake of the NF (LNT and related fractions) for each population group


