Abstract
The Panel on Food Additives and Flavourings added to Food (FAF) provided a scientific opinion re‐evaluating the safety of phosphates (E 338–341, E 343, E 450–452) as food additives. The Panel considered that adequate exposure and toxicity data were available. Phosphates are authorised food additives in the EU in accordance with Annex II and III to Regulation (EC) No 1333/2008. Exposure to phosphates from the whole diet was estimated using mainly analytical data. The values ranged from 251 mg P/person per day in infants to 1,625 mg P/person per day for adults, and the high exposure (95th percentile) from 331 mg P/person per day in infants to 2,728 mg P/person per day for adults. Phosphate is essential for all living organisms, is absorbed at 80–90% as free orthophosphate excreted via the kidney. The Panel considered phosphates to be of low acute oral toxicity and there is no concern with respect to genotoxicity and carcinogenicity. No effects were reported in developmental toxicity studies. The Panel derived a group acceptable daily intake (ADI) for phosphates expressed as phosphorus of 40 mg/kg body weight (bw) per day and concluded that this ADI is protective for the human population. The Panel noted that in the estimated exposure scenario based on analytical data exposure estimates exceeded the proposed ADI for infants, toddlers and other children at the mean level, and for infants, toddlers, children and adolescents at the 95th percentile. The Panel also noted that phosphates exposure by food supplements exceeds the proposed ADI. The Panel concluded that the available data did not give rise to safety concerns in infants below 16 weeks of age consuming formula and food for medical purposes.
Keywords: phosphates, phosphorus, food additive, acceptable daily intake, risk assessment, safety
Short abstract
This publication is linked to the following EFSA Supporting Publications article: http://onlinelibrary.wiley.com/doi/10.2903/sp.efsa.2019.EN-1624/full
Summary
The present opinion document deals with the re‐evaluation of phosphoric acid–phosphates – di‐, tri‐ and polyphosphates (E 338–341, E 343, E 450–452) when used as a food additive.
Phosphates are authorised food additives in the European Union (EU) in accordance with Annex II and III to Regulation (EC) No 1333/2008 on food additives and specific purity criteria have been defined in the Commission Regulation (EU) No 231/2012. E 338, E 339, E 340 and E 341 are also authorised in food category 13.1 foods for infants and young children.
Phosphates have been previously evaluated by the EU Scientific Committee on Food (SCF, 1978, 1991, 1994, 1997) and by the Joint FAO/WHO Expert Committee on Food Additives (JECFA, 1974, 1982a,b, 2002). JECFA concluded that the allocation of an acceptable daily intake (ADI) was not appropriate for phosphates ‘as phosphorus is an essential nutrient and unavoidable constituent of food’ and it was decided, therefore, to assign a ‘maximum tolerable daily intake’ (MTDI) rather than an ADI. The MTDI allocated was 70 mg/kg body weight (bw) per day (expressed as phosphorus) for the sum of phosphates and polyphosphates, both naturally present in food and ingested as food additives (JECFA, 1982a). The SCF subsequently agreed with the JECFA MTDI estimate for phosphates and assigned the cations an ADI ‘not specified’ as they are natural constituents of man, animals and plants (SCF, 1991).
The Expert Group on Vitamins and Minerals (EVM) further concluded that a total intake of 2,400 mg/day (considering 2,110 mg/day inorganic phosphorus from food including food additives and water and 250 mg/day from supplemental phosphorus) does not result in any adverse effects (Expert Group on Vitamins and Minerals, 2003).
In the EFSA NDA Opinion on Tolerable Upper Intake level of phosphorus, the upper level for phosphorus was not established because available data were not sufficient and indicate that normal healthy adults can tolerate phosphorus (phosphates) intake up to at least 3,000 mg/day without adverse systemic effects (EFSA NDA Panel, 2005).
The Panel on Nutrition, Dietetic Products, Novel Food and Allergy of the Norwegian Scientific Committee for Food Safety (VKM) published an assessment of dietary intake of phosphorus in relation to tolerable upper intake levels suggesting 3,000 mg/day as provisional upper level (UL) for total phosphorus intake in adults and 750 mg/day as UL for supplements (VKM, 2017).
Phosphate is essential for all living organisms. Inorganic phosphate used as food additives assessed in this opinion is assumed to dissociate in the gastrointestinal tract. The inorganic phosphorus deriving from food additives is mainly absorbed in the amount of approximately 80–90% as free orthophosphate. Excretion is via the kidney through glomerular filtration and tubular handling.
The Panel considered phosphates to be of low acute oral toxicity and there is no concern with respect to genotoxicity and carcinogenicity.
In standard short‐term, subchronic and chronic toxicity studies, the only significant adverse effect of phosphates is calcification of the kidney and tubular nephropathy. In the chronic rat study with sodium triphosphate, the no‐observable‐adverse‐effect level (NOAEL) was 76 mg/kg bw per day phosphorus (Hodge, 1960). Adding the background dietary phosphorus of 91 mg/kg bw per day to the NOAEL of 76 mg P/kg bw per day gives a total value of 167 mg P/kg bw per day.
In studies performed in mice, rats, rabbits or hamsters, there are no signs of reproductive or developmental toxicity at any dose tested. The Panel thus concluded that exposure to phosphates do not present any risk for reproductive or developmental toxicity.
The epidemiological studies reviewed did not find consistent associations between dietary phosphorous intake and cardiovascular‐related outcomes and do not provide sufficient and reliable data to assess the role of phosphate on bone health.
Clinical interventional trials in which the doses were given on top of the normal diet were performed over several months. No impairment of the renal function was reported with daily doses up to 2,000 mg phosphorus (28.6 mg/kg per day), whereas doses of 4,800 mg/day (68.6 mg/kg per day) elicited renal impairment. Histopathological examinations of human kidney specimens from exposed patients showed similar findings as seen in animals. In several of the studies using phosphorus doses up to 2,000 mg/day, the subjects had soft stools or diarrhoea which is not to be seen as adverse but is classified as discomfort. However, when higher doses are given, such as the doses for bowel cleansing in preparation for colonoscopy (e.g. 11,600 mg/kg or 165.7 mg/kg bw) these doses acted as a cathartic agent and this effect has to be clearly seen as adverse.
Several case reports indicate that a high acute single dose of phosphate (160 mg/kg bw and more) can induce renal impairment.
The evidence from epidemiological and human interventional studies is not suited to derive an ADI. The Panel therefore selected the 167 mg P/kg bw per day NOAEL identified by Hodge (1960) as the basis to derive the ADI. The chemical‐specific adjustment factor for phosphate accounting for interspecies and interindividual differences in toxicokinetics (TK) and toxicodynamics (TD) is 2 × 2 = 4. To this value, the phosphorus‐specific uncertainty factor of 4 is to be applied resulting in an ADI value of 42 mg/kg bw per day, rounded to 40 mg/kg bw per day.
Currently, phosphates (E 338–341, E 343, E 450–452) are authorised food additives in the EU with maximum permitted levels (MPLs) ranging from 500 to 20,000 mg/kg in 104 authorised uses and at quantum satis (QS) in four.
To assess the dietary exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives, the exposure was calculated based on two different sets of concentration data: (1) MPLs as set down in the EU legislation (defined as the regulatory maximum level exposure assessment scenario); and (2) reported use levels (defined as the refined exposure assessment scenario).
While analytical data were used to consider the exposure to phosphorus from all dietary sources.
In the context of this opinion, the Panel was in the special situation to assess the safety of food additives, phosphate salts, which are also nutrients. The Panel based its assessment on the toxicity of phosphorus (phosphate moiety). Since the ADI encompasses the phosphorus intake from natural sources and from food additives sources, the usual exposure assessment using the reported use levels of the food additives was not appropriate to characterise the risk linked to the exposure to phosphorus and the exposure assessment was based on analytical data of the total phosphorus content of foods. In this scenario, the exposure exceeds the ADI of 40 mg/kg bw per day in infants from 12 weeks to 11 months, toddlers and children both at the mean and high level. In adolescents, the high level is also exceeding the ADI of 40 mg/kg bw per day.
Based on the reported use levels, the Panel calculated two refined exposure estimates: a brand‐loyal consumer scenario and a non‐brand‐loyal scenario. The Panel considered that the refined exposure assessment approach resulted in more realistic long‐term exposure estimates and that the refined non‐brand loyal scenario is the most relevant exposure scenario for the safety evaluation of phosphates. In the non‐brand‐loyal exposure assessment scenario, estimated exposure to phosphates ranged between 1 and 48 mg P/kg bw per day at the mean and between 3 and 62 mg P/kg bw per day at the 95th percentile for all population groups.
The derived ADI 40 mg P/kg bw per day results in a exposure to phosphorus of 2,800 mg/person per day for an adult of 70 kg which is within the safety level of exposure of 3,000 mg/person per day set by the EFSA NDA Panel (2005).
The Panel concluded that the group ADI of 40 mg/kg bw per day, expressed as phosphorus, is protective for healthy adults because it is below the doses at which clinically relevant adverse effects were reported in short‐term and long‐term studies in humans. However, this ADI does not apply to humans with moderate to severe reduction in renal function. Ten per cent of general population might have chronic kidney disease with reduced renal function and they may not tolerate the amount of P per day which is at the level of ADI.
The Panel noted that in the exposure estimates based on analytical data exceeded the proposed ADI for infants, toddlers and children at the mean level and for infants, toddlers, children and adolescents at the 95th percentile. The Panel also noted that P exposure from food supplements exceeds the proposed ADI.
The Panel concluded that the available data did not give rise to safety concerns in infants below 16 weeks of age consuming formula and food for medical purposes. When receiving data on the content of contaminants in formula, the Panel noted that the high aluminium content may exceed the tolerable weekly intake (TWI).
The Panel recommends that:
The EC considers setting numerical Maximum Permitted Level for phosphates as food additives in food supplements.
The European Commission considers revising the current limits for toxic elements (Pb, Cd, As and Hg) in the EU specifications for phosphates (E 338–341, E 343, E 450–452) in order to ensure that phosphates (E 338–341, E 343, E 450–452) as a food additive will not be a significant source of exposure to those toxic elements in food.
The European Commission considers revising the current limit for aluminium in the EU specifications for the use of calcium phosphate (E 341).
The European Commission to consider revising the current EU specifications for calcium dihydrogen phosphate (E 341(i)), calcium hydrogen phosphate (E 341(ii)), tricalcium phosphate (E 341(iii)), dimagnesium phosphate (E 343(ii)) and calcium dihydrogen diphosphate (E 450(vii)) to include characterisation of particle size distribution using appropriate statistical descriptors (e.g. range, median, quartiles) as well as the percentage (in number and by mass) of particles in the nanoscale (with at least one dimension < 100 nm) present in calcium dihydrogen phosphate (E 341(i)), calcium hydrogen phosphate (E 341(ii)), tricalcium phosphate (E 341(iii)), dimagnesium phosphate (E 343(ii)) and calcium dihydrogen diphosphate (E 450(vii)) used as a food additive. The measuring methodology applied should comply with the EFSA Guidance document (EFSA Scientific Committee, 2018).
The development of analytical methods for the determination of phosphate additives in the range of foods and beverages permitted to contain them should be considered.
The EFSA Scientific Committee reviews current approaches to the setting of health‐based guidance values for regulated substances which are also nutrients to assess if a coherent harmonised strategy for such risk assessments should be devised.
1. Introduction
The present opinion deals with the re‐evaluation of the following food additives: phosphoric acid (E 338), monocalcium phosphate (E 341(i)), dicalcium phosphate (E 341(ii)), tricalcium phosphate (E 341(iii)), monomagnesium phosphate (E 343(i)), dimagnesium phosphate (E 343(ii)) monosodium phosphate (E 339(i)), disodium phosphate (E 339(ii)), trisodium phosphate (E 339(iii)), monopotassium phosphate (E 340(i)), dipotassium phosphate (E 340(ii)), tripotassium phosphate (E 340(iii)), disodium diphosphate (E 450(i)), trisodium diphosphate (E 450(ii)), tetrasodium diphosphate (E 450(iii)), tetrapotassium diphosphate (E 450(v)), dicalcium diphosphate (E 450(vi)), calcium dihydrogen diphosphate (E 450(vii)), magnesium dihydrogen diphosphate (E 450(ix)), pentasodium triphosphate (E 451(i)), pentapotassium triphosphate (E 451(ii)), sodium polyphosphate (E 452(i)), potassium polyphosphate (E 452(ii)), sodium calcium polyphosphate (E 452(iii)) and calcium polyphosphate (E 452(iv)). For brevity, these food additives will be referred to as phosphates in this document (listed overview of the substances considered in this opinion is available in Appendix A).
As usual in the re‐evaluation of food additives, this opinion addresses the safety of phosphorus intake from the use of the above listed food additives in the general population.
During the drafting of the opinion, a request for extension of use has been received and is included in this opinion. The terms of reference are reported below.
1.1. Background and Terms of Reference as provided by the European Commission
1.1.1. Background to the re‐evaluation of phosphoric acid–phosphates – di‐, tri‐ and polyphosphates (E 338–341, E 343, E 450–452) as food additives
Regulation (EC) No 1333/20081 of the European Parliament and of the Council on food additives requires that food additives are subject to a safety evaluation by the European Food Safety Authority (EFSA) before they are permitted for use in the European Union. In addition, it is foreseen that food additives must be kept under continuous observation and must be re‐evaluated by EFSA.
For this purpose, a programme for the re‐evaluation of food additives that were already permitted in the European Union before 20 January 2009 has been set up under the Regulation (EU) No 257/20102. This Regulation also foresees that food additives are re‐evaluated whenever necessary in the light of changing conditions of use and new scientific information. For efficiency and practical purposes, the re‐evaluation should, as far as possible, be conducted by group of food additives according to the main functional class to which they belong.
The order of priorities for the re‐evaluation of the currently approved food additives should be set on the basis of the following criteria: the time since the last evaluation of a food additive by the Scientific Committee on Food (SCF) or by EFSA, the availability of new scientific evidence, the extent of use of a food additive in food and the human exposure to the food additive taking also into account the outcome of the Report from the Commission on Dietary Food Additive Intake in the EU3 of 2001. The report ‘Food additives in Europe 20004’ submitted by the Nordic Council of Ministers to the Commission, provides additional information for the prioritisation of additives for re‐evaluation. As colours were among the first additives to be evaluated, these food additives should be re‐evaluated with a highest priority.
In 2003, the Commission already requested EFSA to start a systematic re‐evaluation of authorised food additives. However, as a result of adoption of Regulation (EU) 257/2010 the 2003 Terms of References are replaced by those below.
1.1.1.1. Terms of Reference
The Commission asks the European Food Safety Authority to re‐evaluate the safety of food additives already permitted in the Union before 2009 and to issue scientific opinions on these additives, taking especially into account the priorities, procedures and deadlines that are enshrined in the Regulation (EU) No 257/2010 of 25 March 2010 setting up a programme for the re‐evaluation of approved food additives in accordance with the Regulation (EC) No 1333/2008 of the European Parliament and of the Council on food additives.
1.1.2. Background to the request for the extension of use of phosphoric acid–phosphates – di‐, tri‐ and polyphosphates (E 338–341, E 343, E 450–452) as food additives
The Directorate‐General for Health and Food Safety received a request for the extension of use of phosphoric acid–phosphates – di‐, tri‐ and polyphosphates (E 338–341, E 343, E 450–452) by removing the restriction ‘only sugar confectionary’ in the relevant provision in the food category 05.2 ‘Other confectionary including breath refreshing microsweets’.
1.1.2.1. Terms of Reference
The European Commission requested EFSA to provide a scientific opinion on the safety of the proposed extension of use in accordance with Regulation (EC) No 1331/2008 establishing a common authorisation procedure for food additives, food enzymes and food flavourings and proposed that EFSA incorporates in that risk assessment the assessment of the safety of the proposed extension of use.
1.1.3. Interpretation of Terms of Reference
The former ANS Panel described its risk assessment paradigm in its Guidance for submission for food additive evaluations in 2012 (EFSA ANS Panel, 2012). This Guidance states, that in carrying out its risk assessments, the Panel sought to define a health‐based guidance value (HBGV), e.g. an acceptable daily intake (ADI) (IPCS, 2004) applicable to the general population. ADI is defined as ‘an estimate of the amount of a substance in food or drinking water that can be consumed over a lifetime without presenting an appreciable risk to health. It is usually expressed as milligrams of the substance per kilogram of body weight and applies to chemical substances such as food additives, pesticide residues and veterinary drugs’. (EFSA Glossary).
Phosphates are normal constituents in the body and are regular components of the diet. According to the EFSA NDA Panel the available data are not sufficient to establish an upper level (UL) for phosphorus (EFSA NDA Panel, 2005). The EFSA NDA Panel stated in this opinion that ‘The available data indicate that normal healthy individuals can tolerate phosphorus (phosphate) intakes up to at least 3,000 mg/day without adverse systemic effects’. In 2015, the NDA Panel set adequate intakes (AIs) values for various age groups.
Inorganic phosphates authorised as a food additive are efficiently absorbed and used systemically. It is noteworthy that although phosphorus is an essential constituent of the human body and other life forms, the element itself always occurs systemically in the oxidation state (V) as free or combined phosphate. It is absorbed and involved in many structural and functional roles as phosphate (HPO2− 4) (see Section 3.5.1). However, dietary and environmental exposure to phosphorus may come from other forms of phosphorus (V). Whereas the systemic physiologically active moiety is phosphate it has become conventional in nutritional and risk assessment as well as regulatory contexts to use inorganic phosphorus as generic the term (Pi). For the purposes of this opinion, phosphorus will be expressed as P. This is particularly necessary in the context of establishing a group ADI which encompasses phosphorus from all sources including all classes of phosphates as food additives (E 338–341, E 343, E 450–452). The mass conversion factors between phosphate and P2O5 or P are summarised in Appendix B.
The Panel considered that sodium, potassium, calcium and magnesium salts of phosphate and condensed phosphates are expected to dissociate in the gastrointestinal tract into phosphate and their corresponding cations. The resulting sodium, potassium, calcium and magnesium cations will enter their normal physiological processes. The kinetics of the corresponding cations are not assessed in the opinion.
Data were not always available for all the authorised phosphates for all endpoints but for the reason described above the Panel considered that it is possible to perform read‐across between different phosphate additives.
The opinion will also conclude on the proposed extensions of use received during the course of the drafting opinion.
1.2. Information on existing authorisations and evaluations
Phosphates are authorised food additives in the EU in accordance with Annex II and III to Regulation (EC) No 1333/20085. E 338, E 339, E 340, E 341 are also authorised in food category 13.1 foods for infants and young children. Commission Delegated Regulation (EU) 2016/127 and Commission Delegated Regulation (EU) 2016/128, as well as Commission Directive 2006/141/EC and Commission Directive 1999/21/EC, define minimum and maximum levels for phosphorus as well as for the cations of the various phosphate salts (i.e. calcium, potassium and sodium) in the final formula. These statutory requirements are based on the scientific advice by the Scientific Committee on Food (SCF, 1996, 1997, 1998) and EFSA (EFSA NDA Panel, 2013). The minimum and maximum levels of phosphorus for infant formula are set at 25 mg/100 kcal and 90 mg/100 kcal, in the case of infant formula based on soy the maximum level is 100 mg/100 kcal. The minimum and maximum levels for infant formula for special medical purposes are set at 25 mg/100 kcal and 100 mg/100 kcal. In Europe, the phosphates that are permitted as additives in infant formula (category 13.1.1) and foods for infants for special medical purposes (13.1.5.1) are specified in Regulation (EC) No 1333/2008. The permitted level of phosphates used as a food additive, either alone or in combination, is set at a maximum concentration of 1,000 mg/L reconstituted formula. The maximum level is expressed as P2O5.
In addition, tricalcium phosphate is authorised, according to Annex III to Regulation (EC) No 1333/2008, for use as food additives in nutrients in infant formula. The maximum carry‐over of tricalcium phosphate from nutrients is set at 150 mg/kg as P2O5 and within the limit for calcium, phosphorus and calcium:phosphorus ratio as specified in Commission Directive 2006/141/EC. In addition to their use as food additives, calcium, magnesium, potassium and sodium salts of orthophosphoric acid are included in the list of mineral substances which may be used in the manufacture of food supplements reported in the Annex II of Directive 2002/46/EC6 and in the list of mineral substances which may be added to foods reported in the Annex II of Regulation (EC) No 1925/20067.
Calcium, magnesium, potassium and sodium salts of orthophosphoric acid are included in the Union list set out in the Annex to Regulation (EU) No 609/20138 as permitted for use in: infant formula and follow‐on formula, food for special medical purposes and total diet replacement for weight control. Calcium and magnesium sodium salts of orthophosphoric acid are also permitted for use in processed cereal‐based food and baby food.
According to the CODEX STAN 72‐1981 on Infant Formula and Formulas for Special Medical Purposes (FSMP) intended for infants, sodium phosphates (339(i), (ii), (iii)) and potassium phosphates (340(i), (ii), (iii)) may be used as additives in infant formula and infant FSMP. The maximum level is specified at 450 mg/L as phosphorus in the ready‐to‐use product, singly or in combination and within the limits for sodium, potassium and phosphorus (SNE, 2018).
Phosphates have been previously evaluated by the EU SCF (1978, 1991, 1994, 1997) and by the Joint FAO/WHO Expert Committee on Food Additives (JECFA) latest in 1973 and 1982 (JECFA, 1974, 1982a,b).
The toxicology and safety of diphosphates, triphosphates and polyphosphates when used as food additives has previously been evaluated by the Joint FAO/WHO Expert Committee on Food Additives (JECFA) as part of a larger group of phosphate compounds (JECFA, 1964, 1974, 1982a,b, 1986, 2002). At its 26th meeting, JECFA concluded that the allocation of an ADI was not appropriate for phosphates ‘as phosphorus is an essential nutrient and unavoidable constituent of food’ (JECFA, 1982a). It was decided, therefore, to assign a ‘maximum tolerable daily intake’ (MTDI) rather than an ADI. The MTDI allocated was 70 mg/kg bw per day (expressed as phosphorus) for the sum of phosphates and polyphosphates, both naturally present in food and ingested as food additives. ‘The lowest level of phosphate that produced nephrocalcinosis in rat (1% P in the diet) is used as the basis for the evaluation and, by extrapolation based on the daily food intake of 2,800 calories, gives a dose level of 6,600 mg P per day as the best estimate of the lowest level that might conceivably cause nephrocalcinosis in man’. The use of a safety factor was not considered suitable by JECFA with the justification that phosphorous is also a nutrient.
The SCF agreed with the JECFA MTDI estimate for phosphates and assigned the cations an ADI ‘not specified’ as they are natural constituents of man, animals and plants (SCF, 1991).
In 2012, JECFA evaluated magnesium dihydrogen diphosphate (E 450(ix)) for use as food additive (JECFA, 2012a). In its 76th report, JECFA stated the following: ‘The information submitted to the Committee and in the scientific literature did not indicate that the MTDI of 70 mg/kg bw for phosphate salts, expressed as phosphorus, is insufficiently health protective. On the contrary, because the basis for its derivation might not be relevant to humans, it could be overly conservative. Therefore, there is a need to review the toxicological basis of the MTDI for phosphate salts expressed as phosphorus (JECFA, 2012b).
The Expert Group on Vitamins and Minerals (EVM) used as a starting point 750 mg/day; this is the dose that, after oral administration of phosphorus as various phosphate salts, gives osmotic diarrhoea and mild gastrointestinal symptoms in humans. The EVM applied an uncertainty factor of 3 (to allow interindividual variations) to the 750 mg/day and concluded that a supplemental intake of 250 mg/day (3.6 mg/kg bw per day) would not be expected to induce adverse effects (Expert Group on Vitamins and Minerals, 2003). The EVM further concluded that a total intake of 2,400 mg/day (considering 2,110 mg/day inorganic phosphorus from food including food additives and water and 250 mg/day from supplemental phosphorus) does not result in any adverse effects. The exposure calculation in food has been based on a survey from 1986/7 (NDNS 1986/7) which does not include specific estimation of phosphates content in food from food additives.
In the EFSA NDA Opinion on Tolerable Upper Intake level of phosphorus (EFSA NDA Panel, 2005), the upper level for phosphorus was not established because available data were not sufficient, although some adverse gastrointestinal effects have been reported at doses of phosphorus‐containing supplements exceeding 750 mg/day. EFSA reported that the mean dietary and supplemental intake of phosphorus in European countries is approximately 1,000–1,500 mg/day and indicate that normal healthy adults can tolerate phosphorus (phosphates) intake up to at least 3,000 mg/day without adverse systemic effects.
In 2015, EFSA published a Scientific Opinion on Reference Values for phosphorus setting adequate intakes (AIs) for all population groups. The AI recommended is 160 mg/day for infants aged 7–11 months, between 250 and 640 mg/day for children and 550 mg/day for adults. The AI for phosphorus has been derived based on the Dietary Reference Values (DRVs) for calcium by using a molar calcium to phosphorus ratio of 1.4:1 (EFSA NDA Panel, 2015).
In 2006, the National Health and Medical Research Council of Australia and the New Zealand Ministry of Health published AIs for infants between 0 and 6 months (Australian Government, NHMRC). The AI of 100 mg/day was calculated by multiplying the average intake of breast milk (0.78 L/day) by the average concentration of phosphorus in breast milk (124 mg/L) from 10 studies reviewed by Atkinson et al. (1995).
The Panel on Nutrition, Dietetic Products, Novel Food and Allergy of the Norwegian Scientific Committee for Food Safety (VKM) published an assessment of dietary intake of phosphorus in relation to tolerable upper intake levels suggesting 3,000 mg/day as provisional UL for total phosphorus intake in adults and 750 mg/day as UL for supplements (Norwegian Scientific Committee for Food Safety (VKM, 2017)).
2. Data and methodologies
2.1. Data
The Panel on Food Additives and Flavourings (FAF) and its predecessor, the Panel on Food Additives and Nutrient Sources, were not provided with a newly submitted dossier. EFSA, therefore, launched a public call for data9 and a public consultation.10 A technical report has been issued by EFSA collecting the answers received in response to the public consultation. All answers received were considered in the development of this opinion.
For the re‐evaluation, the Panel based its assessment on information submitted to EFSA following the public calls for data, the public consultation, information from previous evaluations and additional available literature up to 18 March 2019. Attempts were made at retrieving relevant original study reports on which previous evaluations or reviews were based however these were not always available to the Panel.
Following the request for additional data on particle size sent by EFSA on 18 September 2018, one of the Interested Parties requested a clarification teleconference, which was held on 4 October 2018.
An applicant has submitted a dossier in support of the application for the extension of use of phosphoric acid–phosphates – di‐, tri‐ and polyphosphates (E 338–341, E 343, E 450–452) as a food additive which is also addressed in this opinion (Documentation provided to EFSA n. 1).
The EFSA Comprehensive European Food Consumption Database (Comprehensive Database11) was used to estimate the dietary exposure.
The Mintel's Global New Products Database (GNPD) is an online resource listing food products and compulsory ingredient information that are included in labelling. This database was used to verify the use of food additive (E 338, E 341(i), E 341(ii), E 341(iii), E 343(i), E 343(ii) E 339(i)), (E 339(ii), E 339(iii), E 340(i), E 340(ii), E 340(iii), E 450(i), E 450(ii), E 450(iii), E 450(v), E 450(vi), E 450(vii), E 450(ix), E 451(i), E 451(ii), E 452(i), E 452(ii), E 452(iii) and E 452(iv) in food products.
2.2. Methodologies
This opinion was formulated following the principles described in the EFSA Guidance on transparency with regard to scientific aspects of risk assessment (EFSA Scientific Committee, 2009) and following the relevant existing guidance documents from the EFSA Scientific Committee.
The FAF Panel assessed the safety of phosphates as food additives in line with the principles laid down in Regulation (EU) 257/2010 and in the relevant guidance documents: Guidance on submission for food additive evaluations by the SCF (2001) and taking into consideration the Guidance for submission for food additive evaluations in 2012 (EFSA ANS Panel, 2012).
On 31 May 2017, EFSA published a guidance document on the risk assessment of substances present in food intended for infants below 16 weeks of age thus enabling EFSA to assess the safety of food additives uses in food for infants below 12 weeks of age (EFSA Scientific Committee, 2017). Therefore, the current evaluation also addresses the safety of use of food additives for all age groups, including the infants below 12 or 16 weeks of age following the principles outlined in that guidance.
When the test substance was administered in the feed or in the drinking water, but doses were not explicitly reported by the authors as mg/kg bw per day based on actual feed or water consumption, the daily intake was calculated by the Panel using the relevant default values as indicated in the EFSA Scientific Committee Guidance document (EFSA Scientific Committee, 2012a) for studies in rodents or, in the case of other animal species, by JECFA (2000). In these cases, the daily intake is expressed as equivalent. When in human studies in adults (aged above 18 years) the dose of the test substance administered was reported in mg/person per day, the dose in mg/kg bw per day was calculated by the Panel using a body weight of 70 kg as default for the adult population as described in the EFSA Scientific Committee Guidance document (EFSA, 2012a).
Dietary exposure to phosphates from their use as food additives was estimated combining food consumption data available within the EFSA Comprehensive European Food Consumption Database with the maximum levels according to Annex II to Regulation (EC) No 1333/200812. Reported use levels and analytical data submitted to EFSA following a call for data were used to assess exposure under different scenarios(see Section 3.3.1). Uncertainties on the exposure assessment were identified and discussed.
Dietary exposure for infants (0–16 weeks) from infant formula and from foods for special medical purposes (FSMP) was calculated based on the minimum and maximum content as defined in the Commission Delegated Regulation (EU) 2016/127 and Commission Delegated Regulation (EU) 2016/128, as well as Commission Directive 2006/141/EC and Commission Directive 1999/21/EC and the reference values on the energy requirements of infants in the first months of life (EFSA NDA Panel, 2013, 2014).
For the assessment of epidemiological studies, a systematic approach has been taken and the protocol is provided in the Appendixes C and D. In addition, the answers received in response to the Public Consultation have been considered for the interpretation of the epidemiology studies. It should be noted that because this opinion is dealing with general population, studies focussing on subpopulations with specific health conditions (e.g. patients with moderate to severe decreased renal function) were not considered.
3. Assessment
3.1. Technical data
3.1.1. Chemistry of phosphates
All phosphorus oxoacids and anions have POH groups in which the hydrogen atom is ionisable (Cotton and Wilkinson, 1972). The principal acid is orthophosphoric acid and its various anions. The phosphate ion carries a −3 formal charge and is the conjugate base of the hydrogen phosphate ion, HPO4 2−, which is the conjugate base of H2PO4 −, the dihydrogen phosphate ion, which in turn is the conjugate base of H3PO4, phosphoric acid. Linear polyphosphates are salts of the anions of general formula [PnO3n+1](n+2)−. Examples are MI 4P2O7, (where M represents the associated cation) diphosphate (also named pyrophosphate), and MI 5P3O10, a tripolyphosphate. Cyclic phosphates are salts of anions of general formula [PnO3n+1]n−. Examples are M3P3O9, a trimetaphosphate, and M4P4O12, a tetrametaphosphate.
The sodium, potassium and ammonium orthophosphates are all water‐soluble. Most other phosphates (including magnesium and calcium) are only slightly soluble or are insoluble in water. As a rule, the hydrogen and dihydrogen phosphates are slightly more soluble than the corresponding non‐hydrogenated phosphates. The pyrophosphates are mostly water‐soluble. Aqueous phosphate exists in four forms: in strongly basic conditions, the phosphate ion (PO4 3−) predominates. Phosphoric acid is tribasic: at 25°C, pK1 = 2.15, pK2 = 7.1 and pK3 ≅ 12.4. In weakly basic conditions, the hydrogen phosphate ion (HPO4 2−) is prevalent. In weakly acidic conditions, the dihydrogen phosphate ion (H2PO4−) is most common. In strongly acidic conditions, trihydrogen phosphate (H3PO4) is the main form. H3PO4, HPO4 2− and H2PO4− behave as separate weak acids because the successive pK values differ by more than 4. The region in which the acid is in equilibrium with its conjugate base is defined by pH ≈ pK ± 2. Thus, the three pH regions are approximately 0–4, 5–9 and 10–14.
A general structural formula of basic structure of ortho and condensed phosphates is given in Figure 1.
Figure 1.
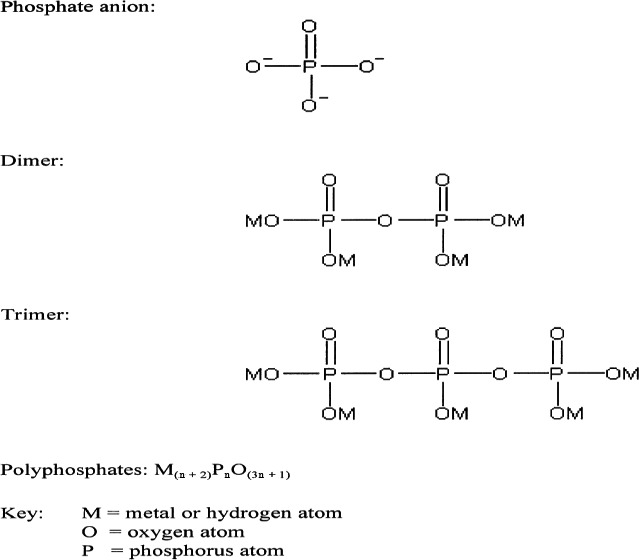
Example of basic structure of ortho‐ and condensed phosphates taken from Weiner et al. (2001)
Annex 1 of EU 1333/2008 describes the range of additive functional classes which have been summarised in Appendix A for phosphates as described in JECFA Monographs (JECFA, 2018).
Organic phosphates in different forms are also present in the diet and differ considerably in the physico‐chemical and physiological properties from inorganic phosphates.
3.1.2. Specifications
The identity of substances description and specifications for phosphates as defined in the Commission Regulation (EU) No 231/2012 and by JECFA are listed in Appendix E.
The Panel noted that, according to the EU specifications for phosphates impurities of elements arsenic, cadmium, lead and mercury are each permitted up to a concentration of 1 mg/kg. Contamination of phosphate additives at such levels could have a significant impact on the exposure to these metals, for which the exposure already are close to the HBGVs or benchmark doses (lower confidence limits) established by EFSA (EFSA CONTAM Panel, 2009a,b, 2010, 2012a,b,c, 2014).
The Panel noted that in EU specifications for E 343(i) the chemical name monomagnesium dihydrogen monophosphate has to be corrected.
When considering the information submitted by the industry on the actual aluminium content in infant formula (final food), the Panel noted that the amount of aluminium may result in an exceedance of the respective tolerable weekly intake (TWI) (Documentation provided to EFSA n. 2,3,4,5).
The Panel noted that the use of calcium phosphate (E 341), for which maximum limits for aluminium have been set in the EU specifications, can contribute to the total aluminium content in infant formula.
3.1.3. Particle size
Industry (Documentation provided to EFSA n. 6) provided information on the particle size distribution (volume‐based (Dv) values) of calcium dihydrogen phosphate (E 341(i)) (n = 3), calcium hydrogen phosphate (E 341(ii)) (n = 6), tricalcium phosphate (E 341(iii)) (n = 7), dimagnesium phosphate (E 343(ii)) (n = 2) and calcium dihydrogen diphosphate (E 450(vii)) (n = 2) analysed by five laboratories using dynamic light scattering (DLS). One of the laboratories indicated that the sample feeding took place by vibrating plate. The lower Dv50 values were reported for six out of the seven samples of E 341(iii) (around 5 μm) while for the other sample the Dv50 value range from 33 to 92 μm (STD = 22). The major difference in the Dv50 value was observed between the two analysed samples for (E 343(ii)), for one was around 7 μm (STD = 0689) and for the other ranged from 152 to 196 μm (STD = 18).
Additional information of the analysis of other samples of calcium dihydrogen phosphate (E 341(i)) (n = 3), calcium hydrogen phosphate (E 341(ii)) (n = 5), tricalcium phosphate (E 341(iii)) (n = 6), dimagnesium phosphate (E 343(ii)) (n = 3) and calcium dihydrogen diphosphate (E 450(vii)) (n = 3) by transmission electron microscopy (TEM), scanning electron microscopy (SEM) and DLS was submitted (Documentation provided to EFSA n. 7). Median minimum Feret diameter values were reported among other parameters for SEM and TEM.
The lower median minimum Feret diameter values were reported for E 341(iii) (ranged from 2 to 7 μm) using SEM. A big variability on the median minimum Feret diameter values was observed between the analysed samples of E 341(i) (ranged from 3 to 150 μm) using SEM. Similar observations were noted for the results reported by TEM. Before the microscopic analyses, the samples were applied at the adhesive carbon tape by gently tapping of the SEM stub with the applied adhesive tape on top of the appropriate sample. According to the authors, this approach allowed them to observe the particles and their aggregates/agglomerates in the native form.
SEM imagines were post‐processed considering a uniform rectangular grid (49–196 nodal points) and only the particles or particles aggregates/agglomerates in the nodal‐points were analysed. The Panel noted that the point counting methodology tends to give biased results since large particles have more chance to be selected for measurement than the small. In addition, for some samples magnification should be higher to allow precise measurement.
As indicated in the report, in the TEM images only the particles with well detectable boundaries were analysed. The Panel noted that the magnification used did not allow to identify if there are or not smaller particles.
The same samples were analysed by DLS and number‐based (Dn) values were reported (Documentation provided to EFSA n. 6). Dn10 values for some of the samples of E 341(ii), E 341(iii), E 343(ii) and E 450(vii) were around 140 nm.
Based on the available information, the Panel cannot exclude that particles in the nanorange can be present in phosphates when used as a food additive.
3.1.4. Manufacturing process
Information was submitted by CEFIC – Phosphoric Acid and Phosphates Producers Association (PAPA) in response to the public call for data.
Phosphoric acid and salts
Phosphoric acid is produced commercially by two main methods, either a wet process or an electrothermal process. In the wet process, phosphate rock is digested with a mineral acid (usually sulfuric acid, but nitric or hydrochloric acids may also be used). A filtration step then separates the ‘wet’ phosphoric acid from the insoluble calcium sulfate slurry. As variable amounts of inorganic impurities may be present depending on the origin of the phosphate rock the phosphoric acid is purified through a solvent extraction purification process to produce the food‐grade additive. In the electrothermal process, the phosphate rock, coke and silica are first heated in an electric resistance furnace to more than 1,100°C to extract elemental phosphorus from the ore. The elemental phosphorus is then oxidised to P4O10 (phosphorus pentoxide) and subsequently hydrated and the mist is collected. This process produces a high‐purity orthophosphoric acid due to the use of pure phosphorous for combustion and only the impurity arsenic needs to be removed in an additional purification step involving treatment with excess hydrogen sulfide and filtration of the precipitate (Documentation provided to EFSA n. 8).
Calcium and magnesium phosphates are produced commercially from phosphoric acid and either calcium oxide or calcium hydroxide, and either magnesium oxide or magnesium hydroxide, respectively. The raw materials are mixed together and the product is separated via centrifugation or filtration. The product is a solid that undergoes further physical treatment (drying, milling, sieving) before being passed through a metal detector and then packaged (Documentation provided to EFSA n. 9,10). No further information on purity requirements for the Ca and Mg containing starting materials were provided.
Both mono‐ and disodium phosphates are prepared commercially by neutralisation of phosphoric acid using sodium carbonate or sodium hydroxide. Crystals of a specific hydrate can then be obtained by evaporation of the resultant solution within the temperature range over which the hydrate is stable. For the preparation of trisodium phosphate, sodium hydroxide must be used to reach the high pH because carbon dioxide cannot be stripped readily from the solution above a pH approaching 8. Similarly, the potassium phosphates are produced by successive replacement of the protons (H+) of phosphoric acid with potassium ions.
Diphosphates
The three sodium diphosphates are produced commercially by the neutralisation of phosphoric acid with sodium hydroxide. Solutions of the two reagents are mixed in the required proportions for the specific product (1:1 sodium hydroxide:phosphoric acid for E 450(i); 3:2 for E 450(ii); and 2:1 for E 450(iii)). After reaction, the solution is filtered to remove insoluble impurities. The solution is spray‐dried or passed through a rotary kiln or drum dryer. Temperatures greater than 200°C are used; as well as evaporating the water, this temperature promotes a condensation reaction between phosphate groups to produce the diphosphate. The solid material produced is milled, sieved or ground, passed through a metal detector and packaged. Information on manufacturing of tetrasodium diphosphate (E 450(iv)) is missing.
Tetrapotassium diphosphate is manufactured in a similar way, using potassium hydroxide and phosphoric acid. A higher temperature of 350–400°C is used to dry the product and promote the condensation of phosphate groups. The solid product is processed in the same way as described above.
Dicalcium diphosphate is produced from anhydrous dicalcium phosphate (calcium hydrogen phosphate, CaHPO4). The dicalcium phosphate is calcined in a drum drier, rotary kiln or kneader drier at 350–400°C, under which conditions a condensation reaction occurs between phosphate groups. The coarse granules formed are milled, sieved, passed through a metal detector and bagged.
Calcium dihydrogen diphosphate is made in a similar way to the above, but the starting material is monocalcium phosphate (Ca(H2PO4)). This is calcined in a drum drier, rotary kiln or kneader drier at 270–350°C, where condensation between phosphate groups occurs. The solid product is treated in the same way as described in the above paragraphs.
Magnesium dihydrogen diphosphate (E 450(ix)) is manufactured by adding an aqueous dispersion of magnesium hydroxide slowly to phosphoric acid, until a molar ratio of approximately 1:2 (Mg:P) is achieved. The temperature is held at 60°C during the reaction. Approximately 0.1% hydrogen peroxide is added and the resulting slurry is heated and milled (Documentation provided to EFSA n. 7).
Triphosphates
Pentasodium triphosphate and pentapotassium triphosphate are produced commercially by the neutralisation of phosphoric acid with sodium or potassium hydroxide, respectively. The neutralised mixture is dried via spray‐drying or by being passed through a drum dryer or rotary kiln at temperatures above 250°C. The phosphate produced (di‐, tri‐ etc) depends on the degree of neutralisation and the temperature and residence time in the dryer or kiln. The coarse granules formed are usually milled, sieved, passed through a metal detector and then bagged.
Polyphosphates
The thermal dehydration of monosodium phosphate can give a number of condensed polyphosphates. The particular products formed depend on the conditions used – temperature, water vapour and tempering. Heating NaH2PO4 to above 620°C and quenching rapidly gives Graham's salt, a water‐soluble polyphosphate glass with a composition of (NaPO3)x (where x = 4–1.1). The glass consists of around 90% high molecular weight polyphosphates, with the rest being made up of various cyclic metaphosphates. In contrast, the dehydration of NaH2PO4 at 260–300°C produces the low temperature form of Maddrell's salt, (NaPO3)n – III, insoluble metaphosphate III. Further heat treatment of this at 360–430°C produces a second form of Maddrell's salt, insoluble metaphosphate II (also (NaPO3)n). The potassium compound, Kurrol's salt, is similarly obtained by thermal dehydration of KH2PO4. No information on manufacturing of E 452(iii) sodium calcium polyphosphate and E 452(iv) calcium polyphosphate.
3.1.5. Methods of analysis in food
Introduction
A variety of analytical methods have been used for the determination of phosphate additives in foods and beverages. So‐called ‘classical’ methods are generally only useful for total phosphate but have been modernised for current applications in some areas. Modern methods such as ion chromatography (IC), capillary zone electrophoresis (CZE) and nuclear magnetic resonance spectroscopy (NMR) can separate, identify and quantify different phosphate types but are not be able to differentiate between added and naturally occurring phosphates. Moreover, most methods suffer from lack of information on natural variation of phosphate levels where only a few useful but limited reviews are available.
Plasma spectrometry is a useful tool for the estimation of the total phosphorus content. Upon comparing IC with direct current plasma spectrometry (DCP), IC can only provide information on ionic phosphates while DCP can allow the determination of all forms of phosphorus. However, a combination of the two techniques can provide a powerful tool for separating, identifying and measuring all forms of phosphorus (Urasa and Ferede, 1986).
The measurement of added phosphates in food products is not straightforward due to the presence of several types of phosphate additives (i.e. poly, tri‐, pyro‐, orthophosphates). The quantification of phosphate alone cannot be used to verify the presence of added phosphates due to the presence of naturally occurring phosphates and other phosphorus‐containing components such as phospholipids and phosphoproteins. For example, there is ca. 0.1–4.8% naturally occurring phosphates in seafood (Campden, 2012); hence, there is a need to distinguish between natural phosphates, which are not well defined, and added phosphates. In addition, there is the issue of stability since polyphosphates are readily hydrolysed to pyrophosphates and (eventually) to orthophosphates due to phosphatase activity (temperature‐dependent), processing conditions and during analysis (Scharpf and Kichline, 1967; Das et al., 2011; Campden 2012).
Extraction procedures for phosphates are sample‐specific and therefore vary across foods and beverages permitted to contain phosphate additives. Certain extraction conditions (e.g. acids) can also promote the degradation of polyphosphates to orthophosphates.
Indirect methods
Indirect methods for estimation phosphate content are essentially restricted to moisture content and protein content. The ratios of moisture:protein and phosphate:protein can provide useful information on added phosphates. However, the moisture contents of foodstuffs vary greatly and protein measurement relies on the use of interim nitrogen factors following Kjeldahl analysis. While these methods can show when phosphates and/or water have been added, their accuracy is questionable due to natural variation in phosphate content of foodstuffs (Campden, 2012).
Direct methods
Phosphate may be determined in meat samples using digestion with a mixture of hydrochloric and nitric acids, followed by filtration and treatment with quimociac reagent to form precipitates of quinolinium phosphomolybdate, which are then filtered, washed, dried and quantified gravimetrically (USDA, 2009).
Spectrophotometric methods
Direct analysis of phosphate in foodstuffs is commonly carried out using spectrophotometric (colorimetric) methods, e.g. by measuring the intensity of colour resulting from the interaction of orthophosphates with reagents such as molybdenum blue, yellow vanamolybdate complex and malachite green (Þórarinsdóttir et al. (2010); Campden, 2012). Colorimetric analysis requires the decomposition of poly‐, tri‐ and other forms to orthophosphates achieved through the use of strong acids such as trichloroacetic acid (TCA) and sulfuric acid (H2SO4). The total phosphate content is usually expressed as P2O5 and therefore does not distinguish between different classes of phosphate additive. A spectrophotometric method has been developed that is able to distinguish between phosphorus due to water‐soluble (i.e. inorganic) from organic phosphorus sources such as phospholipid and phosphoprotein (Cupisti et al., 2012). An adaptation of this method can be used to distinguish between orthophosphate and condensed polyphosphates (Þórarinsdóttir et al., 2010). The condensed forms react much more slowly, so measurements are made at 15 and 90 min and the difference between the results is the amount of the condensed forms. The method described above cannot distinguish between the di‐, tri‐ and polyphosphates.
Modern spectrophotometric methods have good sensitivity and precision, which is important because of the natural variation in total phosphates content in foodstuffs. McKie and McCleary (2016) developed and validated a novel and rapid method for the determination of total phosphorus and phytic acid in foods and animal feeds. The method involves the extraction of phytic acid followed by dephosphorylation with phytase and alkaline phosphatase, and measured colorimetrically using a modified molybdenum blue assay. Such methods are used for determining the phosphate content of fertilisers and for assessing the purity of phosphate food additives (JECFA, 2018; EU, 231/2012). The Association of Official Analytical Chemists (AOAC) method describes a standard colorimetric method for the determination of orthophosphate in water (AOAC, 1997). Method details are summarised in Table 1.
Table 1.
Reference methods listed by BVL (2018) and available standard methods
| E number(s) | Method number, name, origin | Analyte(s) | Analytical technique | Matrices |
|---|---|---|---|---|
| BVL methods | ||||
| 450–452 | L 06.00‐15L 07.00‐20L 08.00‐22 | Condensed phosphates | Thin‐layer chromatography | Meat, meat products, processed meats, bakery wares |
| 450–452 | L 06.00‐9 | Di‐, Tri‐, Poly‐ Phosphate | Spectrophotometry | Foodstuff, e.g. meat products, fish products, dairy, bakery products, grain‐based foods |
| 450(i–vii) | L 06.00‐15ISO‐Norm 5553 | Diphosphate | Thin‐layer chromatography | Dairy, meat products, fish products |
| 451(i, ii) | L 06.00‐15ISO‐Norm 5553 | Triphosphate | Thin‐layer chromatography | Dairy, meat products, fish products |
| 452(i–iv) | L 06.00‐15 mod. Iso‐Norm 5553(qualitative)L 06.00‐09 mod. (quantitative) | Di‐, Tri‐, Poly‐ Phosphate | Thin‐layer chromatography Spectrophotometry | Meat products, dairy (cheese, processed cheese), fish products |
| 338–341, 343,450–452 | Photometric determination of phosphate after acid digestion in drinks | Total phosphate as PO4 | Spectrophotometry | Soft drinks |
| 338–341, 343,450–452 | L 06.00‐9 | Total phosphate as P2O5 | Spectrophotometry | Meat, meat products, cheese, dairy |
| 338–343, 450, 451 | Condensed phosphatesL 06.00‐15 | Condensed phosphates | Qualitative chromatography | Meat and meat products |
| 338–343, 450, 451 | Total phosphorus contentL 06.00‐9 | P2O5 | Spectrophotometry | Meat and meat products |
| 338–343, 450, 451 | Total phosphorus contentL 03.00‐17 | Phosphorous | Spectrophotometry | Cheese, processed cheese, processed cheese preparations |
| 339(i–iii) | L 06.00‐15 mod | Triphosphate | Thin‐layer chromatography | Fish products |
| 340(i–iii) | Not specified | Phosphoric acid | Ion chromatography | Soft drinks |
| 338 | L 31.00‐6 | Phosphate | Spectrophotometry without ashing | Soft drinks |
| Other standard methods/norms | ||||
| BSI 4401‐15:1981/ISO 5553;1981. Methods of test for meat and meat products. Detection of polyphosphates (by spectrophotometry) | ||||
| PD ISO/TS 18083:2013. Processed cheese products. Calculation of content of added phosphate calculated as phosphorus (by spectrophotometry) | ||||
| AOAC, 1997. Standard colorimetric method for the determination of orthophosphate in water (by spectrophotometry) | ||||
Chromatographic methods
Thin‐layer chromatography (TLC) methods for determining phosphates are relatively simple and cheap and can separate poly‐, tri‐, pyro‐ and orthophosphates. Quantitative estimates of phosphates content can be achieved by comparing colour intensities of spots with standard phosphate solutions. The main disadvantage of TLC is the hydrolysis in situ of phosphates during sample extraction and analysis (Campden, 2012). Without additional analysis, TLC is essentially a qualitative technique and it has been shown that false‐negative results can arise. For example, where polyphosphates have completely hydrolysed to orthophosphates and are no longer detectable as a distinct species, while similar observations during the TLC analysis of white shrimp, where the limit of detection was estimated at 0.08% (w/w) sodium triphosphate (Campden 2012).
High‐performance liquid chromatography (HPLC), or more accurately IC, has been shown to be a useful method for the determination of individual polyphosphates and other phosphate species. IC can separate and quantify poly‐, tri‐, pyro‐ and orthophosphates. Post‐column colorimetric and conductivity detection can be used to provide sensitive and selective performance with good linear range. IC methods can be used for the simultaneous determination of condensed phosphates including orthophosphates (P1), diphosphates (P2) and polyphosphates (P3 and greater).
Examples of the application of IC in fish, shellfish and crustacea may be found in Campden (2012). A similar methodology has been used IC has been used to determine phosphate species in sausage (Dionex 2010) and for the determination of polyphosphates in fish, shrimp and cuttlefish, and on commercial products of cooked ham, wurstel, corned beef, processed cheese and fish (Iammarino and Di Taranto, 2012). IC has been used recently for the rapid and automated determination of orthophosphate in carbonated soft drinks (De Borba and Rohrer, 2018). Method details are summarised in Table 1.
Electrophoretic methods
Capillary electrophoresis (CE) is a family of related techniques used to separate charged particles based on their size to charge ratio when an electric current is applied (Campden, 2012). The most commonly used technique is capillary zone electrophoresis (CZE), where separation is based on differences in solute size and charge at a given pH. In capillary isotachophoresis (cITP), samples are loaded into a capillary set between two electrolytes (leading and terminating), whereupon the analytes are separated into discrete zones between the electrolytes according to their electrophoretic mobility. Both techniques, either alone or in combination, have been used to detect added phosphates in foodstuffs. Detection techniques include conductivity, fluorescence or ultraviolet (UV). CZE/cITP with conductivity detection has been used to determine phosphate in meat, canned meat products, ham, smoked ham, sausages, paté, prawns, squid and mixed seafood (Jastrzębska, 2009, 2011; Campden 2012). Method details are summarised in Table 1. The clear advantages of using CZE/cITP methods is that they can determine different phosphate species (ortho, di‐ and tri‐) simultaneously and rapidly, requiring a relatively small amount of sample. While results have been reported to be sensitive, accurate and precise the importance of robust sample preparation is requisite. Sample inhomogeneity and the presence of protein and fat can decrease method precision.
Nuclear magnetic resonance (NMR)
31P NMR has been used generally as a research tool rather than as a routine analytical procedure but this technique is becoming more widely available and affordable. 31P NMR can differentiate simultaneously between different phosphate types and is quantifiable. It has been applied to fish and meat products with adequate sensitivity (Campden, 2012). Method details are summarised in Table 1. The results obtained by 31P NMR are reported to more accurate and precise compared to those obtained using the molybdovanadate yellow spectrophotometric method (Szłyk and Hrynczyszyn, 2011).
The issue of polyphosphate degradation notwithstanding, non‐destructive, simultaneous observation of different phosphate species is clearly an analytical advantage. Moreover, 31P NMR it has been used to measure total phosphates or polyphosphates but cannot be used to distinguish between natural and added compounds.
Ion chromatography
Upon comparing IC with DCP, IC can only provide information on ionic phosphates while DCP can allow the determination of all forms of phosphorus. However, a combination of the two techniques can provide a powerful tool for separating, identifying and measuring all forms of phosphorus (Urasa and Ferede, 1986).
Other methods
Much less widely used techniques for phosphate determination include thermal differential photometry and microwave dielectric spectroscopy, which are essentially research tools that are not readily applicable to routine analysis of foodstuffs. X‐ray fluorescence has also been used (Documentation provided to EFSA n. 7) although is not a widespread technique.
Standard methods and norms
There are few validated official methods available. Those identified to date are summarised with standard methods listed by BVL (2018) in Table 1. The scope of these methods covers ortho‐, condensed and polyphosphate analytes, and most foodstuffs and beverages apart from those for infants (e.g. infant formula). Analytical techniques are essentially limited to TLC and/or spectrophotometry, except for IC which is specified for the analysis of soft drinks. Data provided by CEFIC‐PAPA provide evidence for the accuracy and precision requirements of standard methods for phosphate determination. For example, the total phosphorus is calculated as g/100 g reported to two significant figures (Documentation provided to EFSA n. 11).
The scope of methods for the determination of phosphates in foodstuffs must cover the complete range of foods and beverages permitted to contain phosphate additives and must be readily applicable in laboratories, i.e. not unnecessarily complex or costly.
While quantitative spectrophotometric methods provide sufficient sensitivity and ease of use, they are limited in scope to the detection and measurement of phosphates in the ortho form, i.e. di‐, tri‐ and polyphosphates must be hydrolysed first to orthophosphates. Hydrolysis may be achieved chemically and/or enzymatically but it will not be possible to discriminate between phosphates present naturally and phosphate additives (however, the latter are likely to be present at a much higher concentration relative to natural phosphates). Published spectrophotometric methods therefore require further development to encompass all foodstuffs within the required scope, especially with respect to extraction and isolation techniques.
Since spectrophotometric methods cannot be used qualitatively to identify different phosphate additive species, the use of more sophisticated techniques that can separate, identify and quantify different phosphate species is required. Of the available methods, IC is the most widely used but to date, has not been applied to the full range of foodstuffs permitted to contain phosphate additives. For the simultaneous determination of condensed phosphates using IC, systems employing a mobile phase comprising KOH (or NaOH) and macroporous divinyl benzene/ethylvinyl benzene stationary phase run under gradient elution conditions with suppressed conductivity detection, are the most widely reported. In order to reduce the reporting of false positive and/or false negative results, it is recommended that sample preparation times should be as short as possible and should include steps to deactivate phosphatase enzymes.
Appropriate analytical methods must be developed and validated to recognised international protocols so that they are fit for purpose with respect to expected phosphate concentration ranges (i.e. ranging from ca. 500 to 50,000 mg/kg, as well as quantum satis). Some foodstuffs have ‘no limit defined’. There should also be clear distinction between methods for total phosphate and methods for identifying and quantifying separate phosphate types, i.e. methods must be robust, and the units used for reporting phosphate content should be standardised.
There is a clear inconsistency in the reporting of levels of phosphates in food products (as well as in serum and urine), due largely to the form in which the results are expressed. Historically, phosphorus content has been expressed in terms of mg P2O5/100 g, which is usually applied to determination of total phosphorus and phytic acid in fertilisers, which allows for normalisation of P content across a range of products comprising different mixtures of phosphates. It is also applied to some foods and animal feeds. Other (particularly clinical) studies report phosphorus levels as mg P/kg. Modern analytical methods tend to report P content as mg/kg total phosphate or where possible as mg/kg individual ortho‐, pyro‐ or polyphosphates.
In order to fulfil the requirements of EU regulation EU 1333/2008 with regard to the presence and maximum levels of phosphates, it is recommended that analytical results are expressed as either total phosphates (P3O4 3− irrespective of counter ion), or in terms of the individual phosphate species, as mg/kg.
Literature sources show that spectrophotometry has been established as a reliable technique for the determination of total phosphate in foodstuffs. Similarly, IC has been applied successfully to a limited range of foodstuffs for the simultaneous determination of different phosphate additive species. The Panel noted the need for development of analytical methods since those currently available for total phosphate and phosphate speciation do not cover the entire range of foodstuffs permitted to contain phosphate additives.
3.1.6. Stability of the substance and fate in food
No information was identified in the literature on the reaction and fate of phosphoric acid or its calcium and magnesium salts in food. Phosphoric acid is soluble in water and is expected to dissociate in beverages and fresh food to phosphate and H+ ions. No information was identified in the literature on the reaction and fate of sodium and potassium phosphates in food. Since sodium and potassium phosphates are freely soluble in water they are expected to be dissolved in beverages and fresh food to phosphate and the respective cations.
Phosphoric acid and its sodium and potassium salts dissociate readily after being added to foods and beverages, thereby affecting its technological function as an acidity regulator (Documentation provided to EFSA n. 8), whereas calcium and magnesium phosphates require solubilisation under acidic conditions (Documentation provided to EFSA n. 9,10).
The effects of phosphates in general on the colour and quality of salted fish are summarised by Þórarinsdóttir et al. (2010). Yellowing of the fish due to oxidation reduces the commercial quality. Positive effects of phosphates on colour and the commercial quality of the fish (by maintaining the natural colour of the fish) are thought to be due to reduced oxidation, which is brought about by the sequestering action of the phosphates on metals present in the salt used.
The addition of sodium phosphates to meat has been shown to have antioxidant effects that decrease the rate of oxidation of lipids in meat (Miller, 2010). Di‐, tri‐ and higher phosphates are susceptible to the action of phosphatase enzymes, in particular during extraction from food or biological samples when they can be converted into monophosphates. Das et al. (2011) used Zn(II) and Cd(II)‐based complexes to bind with tetrasodium diphosphate in order to investigate the activity of alkaline phosphatase in physiological conditions. Allen and Cornforth (2009) describe the iron‐binding activity of sodium tripolyphosphate in a lipid‐free model system. At concentrations of 1 and 0.05 mg/mL, 88% and 21%, respectively, of the added iron was bound. This activity was considered to be the basis for the antioxidant effect of sodium tripolyphosphate. Weilmeier and Regenstein (2004) added sodium polyphosphate to mackerel samples and observed an antioxidant effect, although this was not as strong as the effect with propyl gallate, ascorbic acid or erythorbic acid. Jin et al. (2011) purified and characterised the tripolyphosphatase responsible for the hydrolysis of tripolyphosphates in rabbit psoas major muscle tissue.
Polyphosphates
All polyphosphates (also referred to as condensed phosphates) are subject to hydrolytic decomposition (reversion) when in solution. The rate of decomposition is affected by:
Temperature
pH (generally < 7 or > 11)
Multivalent metal ions, e.g. Ca2+, Fe2+
Concentration at mg/L level, since as the concentration increases, the reversion rate decreases
Phosphatase enzymes
Phosphate species.
It is generally accepted that pyrophosphate is the most stable, followed by tripolyphosphates. During hydrolysis of the longer chain phosphates, shorter chains as well as orthophosphates are formed. Among the shorter chains formed are pyrophosphates. Research suggests that when the pyrophosphate concentration increases, due to hydrolysis of higher polyphosphates, the rates of reversion diminish. It may be that an equilibrium is established between the higher condensed phosphates and their hydrolysis products.
Scharpf and Kichline (1967) showed that following the addition of long‐chain sodium polyphosphate to cheese extracts in which the natural alkaline phosphatase activity was high, the concentration and distribution of phosphate species remained unchanged after storage at 3–7°C for 4 weeks. After 4 weeks storage at 20°C, the concentration of the long‐chain species decreased from 89% to 64%, whereas the concentration of the orthophosphate species increased from 4% to 27%.
In a conservative review of polyphosphate breakdown and stability (Campden, 2012) it was reported that:
Most polyphosphates added to food are broken down to orthophosphate units in the stomach and may be significantly hydrolysed to orthophosphates during storage and cooking.
After 2 weeks of frozen storage, only 12% of the total phosphorus in uncooked shrimp muscle corresponded to the tripolyphosphate added. After ten weeks, the phosphorus levels corresponded to 45% orthophosphate. This was considered to be due to natural rather than heat‐induced hydrolysis.
At elevated temperatures, such as in steam cooking, sodium tripolyphosphate will hydrolyse rapidly to orthophosphates.
Samples of three different commercially available cooked shrimp products treated with tripolyphosphate and stored frozen for 11 months, showed that the total polyphosphate was 87%, 89% and 103% of the original levels, indicating that very little hydrolysis occurred.
The stability of polyphosphates in fish and shrimps under various treatment and storage regimen was reported by Campden (2012). Samples were either untreated or treated and analysed after 0, 1, 2 and 3 days storage. The relative level of polyphosphate (expressed as P2O5) in raw shrimps was reduced from 1,500 mg/kg to 0 mg/kg after 4 days due to phosphatase activity. Conversely, no polyphosphate degradation was observed in cooked shrimp treated with polyphosphate (at 2,600 mg/kg) after cooking, indicating heat‐induced phosphatase deactivation during cooking.
The addition of sodium phosphates to meat has been shown to have antioxidant effects that decrease the rate of oxidation of lipids in meat (Miller, 2010). Di‐, tri‐ and higher phosphates are susceptible to the action of phosphatase enzymes, in particular during extraction from food or biological samples when they can be converted into monophosphates. Campden (2012) report that flash heat treatment with a microwave oven can be used to avoid this.
The impact of high temperature treatments of on the composition of polyphosphates with regard to phosphate chain length in aqueous solutions in the presence and absence of calcium ions has been reported by Rulliere et al. (2012). Treatment at 120°C for 10 min led to the hydrolytic degradation of long‐chain polyphosphates into orthophosphate and trimetaphosphate, whereas heating the salts to 100°C in aqueous solutions had little effect on composition. The presence of calcium ions increased the rate of hydrolysis of long‐chain phosphates leading to increased amounts of trimetaphosphate and pyrophosphate end products. The evolution of emulsifying salts composition under heat treatment was reported to lead to modification of their chelating properties since short‐chain phosphates are less efficient at chelating calcium than long‐chain phosphates.
3.2. Authorised uses and use levels
Maximum levels of phosphates (E 338–341, E 343, E 450–452) have been defined in Annex II to Regulation (EC) No 1333/200813 on food additives, as amended. In this document, these levels are named maximum permitted levels (MPLs).
Currently, phosphates (E 338–341, E 343, E 450–452) are authorised food additives in the EU with MPLs ranging from 500 to 20,000 mg/kg expressed as P2O5 in 104 authorised uses and at quantum satis (QS) in four. The 108 different uses and use levels are corresponding to 65 different food categories. Table for converting phosphates into P2O5 and P is in Appendix B.
Table 2 summarises the food categories with their restrictions/exceptions that are permitted to contain added phosphates (E 338–341, E 343, E 450–452) and the corresponding MPLs as set by Annex II to Regulation (EC) No 1333/2008.
Table 2.
MPLs of phosphates (E 338–341, E 343, E 450–452) in foods according to the Annex II to Regulation (EC) No 1333/2008
| Food category code | Food category name | Restrictions/exceptions | E‐number | Name | MPL (mg/L or mg/kg as appropriate) | Footnotes (as in Reg (EC) No 1333/2008 |
|---|---|---|---|---|---|---|
| 0 | Food additives permitted in all categories of foods | Only foods in dried powdered form (i.e. foods dried during the production process, and mixtures thereof), excluding foods listed in table 1 of Part A of this Annex | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 10,000 | 1 , 4 , 57 |
| 01.1 | Unflavoured pasteurised and sterilised (including UHT) milk | Only sterilised and UHT milk | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 1,000 | 1 , 4 |
| 01.4 | Flavoured fermented milk products including heat‐treated products | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 3,000 | 1 , 4 | |
| 01.5 | Dehydrated milk as defined by Directive 2001/114/EC | Only partly dehydrated milk with less than 28% solids | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 1,000 | 1 , 4 |
| 01.5 | Dehydrated milk as defined by Directive 2001/114/EC | Only partly dehydrated milk with more than 28% solids | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 1,500 | 1 , 4 |
| 01.5 | Dehydrated milk as defined by Directive 2001/114/EC | Only dried milk and dried skimmed milk | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 2,500 | 1 , 4 |
| 01.6.3 | Other creams | Only sterilised, pasteurised, UHT cream and whipped cream | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 |
| 01.7.1 | Unripened cheese excluding products falling in category 16 | Except mozzarella | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 2,000 | 1 , 4 |
| 01.7.5 | Processed cheese | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 20,000 | 1 , 4 | |
| 01.7.6 | Cheese products (excluding products falling in category 16) | Only unripened products | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 2,000 | 1 , 4 |
| 01.8 | Dairy analogues, including beverage whiteners | Only whipped cream analogues | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 |
| 01.8 | Dairy analogues, including beverage whiteners | Only processed cheese analogues | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 20,000 | 1 , 4 |
| 01.8 | Dairy analogues, including beverage whiteners | Only beverage whiteners | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 30,000 | 1 , 4 |
| 01.8 | Dairy analogues, including beverage whiteners | Only beverage whiteners for vending machines | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 50,000 | 1 , 4 |
| 02.2.1 | Butter and concentrated butter and butter oil and anhydrous milkfat | Only soured cream butter | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 2,000 | 1 , 4 |
| 02.2.2 | Other fat and oil emulsions including spreads as defined by Council Regulation (EC) No 1234/2007 and liquid emulsions | Only spreadable fats | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 |
| 02.3 | Vegetable oil pan spray | Only water‐based emulsion sprays for coating baking tins | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 30,000 | 1 , 4 |
| 03 | Edible ices | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 1,000 | 1 , 4 | |
| 04.2.4.1 | Fruit and vegetable preparations excluding compote | Only fruit preparations | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 800 | 1 , 4 |
| 04.2.4.1 | Fruit and vegetable preparations excluding compote | Only seaweed based fish roe analogues | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 1,000 | 1 , 4 |
| 04.2.4.1 | Fruit and vegetable preparations excluding compote | Only glazings for vegetable products | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 4,000 | 1 , 4 |
| 04.2.5.4 | Nut butters and nut spreads | Only spreadable fats excluding butter | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 |
| 04.2.6 | Processed potato products | Including prefried frozen en deep frozen potatoes | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 |
| 05.2 | Other confectionery including breath refreshening microsweets | Only candied fruit | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 800 | 1 , 4 |
| 05.2 | Other confectionery including breath refreshening microsweets | Only sugar confectionery, except candied fruit | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 |
| 05.3 | Chewing gum | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | Quantum satis | 1 , 4 | |
| 05.4 | Decorations, coatings and fillings, except fruit based fillings covered by category 4.2.4 | Only toppings (syrups for pancakes, flavoured syrups for milkshakes and ice cream; similar products) | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 3,000 | 1 , 4 |
| 05.4 | Decorations, coatings and fillings, except fruit based fillings covered by category 4.2.4 | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 | |
| 06.2.1 | Flours | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 2,500 | 1 , 4 | |
| 06.2.1 | Flours | Only self‐raising flour | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 20,000 | 1 , 4 |
| 06.2.1 | Flours | Only self‐raising flour | E 450(ix) | Magnesium dihydrogen diphosphate | 15,000 | 4 , 81 |
| 06.3 | Breakfast cereals | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 | |
| 06.5 | Noodles | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 2,000 | 1 , 4 | |
| 06.5 | Noodles | E 450(ix) | Magnesium dihydrogen diphosphate | 2,000 | 4 , 81 | |
| 06.6 | Batters | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 12,000 | 1 , 4 | |
| 06.6 | Batters | E 450(ix) | Magnesium dihydrogen diphosphate | 12,000 | 4 , 81 | |
| 07.1 | Bread and rolls | Only soda bread | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 20,000 | 1 , 4 |
| 07.1 | Bread and rolls | Only refrigerated, prepacked yeast based doughs used as basis for pizzas, quiches, tarts and similar products | E 450 | Diphosphates | 12,000 | 4 |
| 07.1 | Bread and rolls | Only pizza dough (frozen or chilled) and ‘tortilla’ | E 450(ix) | Magnesium dihydrogen diphosphate | 15,000 | 4 , 81 |
| 07.2 | Fine bakery wares | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 20,000 | 1 , 4 | |
| 07.2 | Fine bakery wares | E 450(ix) | Magnesium dihydrogen diphosphate | 15,000 | 4 , 81 | |
| 08.2 | Meat preparations as defined by Regulation (EC) No 853/2004 | Only breakfast sausages: in this product, the meat is minced in such a way so that the muscle and fat tissue are completely dispersed, so that fibre makes an emulsion with the fat, giving the product its typical appearance; Finnish grey‐salted Christmas ham, burger meat with a minimum vegetable and/or cereal content of 4% mixed within the meat, Kasseler, Bräte, Surfleisch, toorvorst, šašlõkk, ahjupraad, Bílá klobása, Vinná klobása, Sváteční klobása, Syrová klobása and frozen vertical rotating meat spits made of sheep, lamb, veal and/or beef treated with liquid seasoning or from poultry meat treated with or without liquid seasoning used alone and/or combined as well as sliced and/or minced and designed to be roasted by a food business operator and then consumed by the final consumer | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 |
| 08.3.1 | Non‐heat‐treated meat products | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 | |
| 08.3.2 | Heat–treated meat products | Except foie gras, foie gras entier, blocs de foie gras, Libamáj, libamáj egészben, libamáj tömbben | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 |
| 08.3.3 | Casings and coatings and decorations for meat | Only glazings for meat | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 4,000 | 1 , 4 |
| 09.1.1 | Unprocessed fish | Only frozen and deep‐frozen fish fillets | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 |
| 09.1.2 | Unprocessed molluscs and crustaceans | Only frozen and deep‐frozen molluscs and crustaceans | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 |
| 09.2 | Processed fish and fishery products including molluscs and crustaceans | Only canned crustaceans products; surimi and similar products | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 1,000 | 1 , 4 |
| 09.2 | Processed fish and fishery products including molluscs and crustaceans | Only fish and crustacean paste and in processed frozen and deep‐frozen molluscs and crustaceans | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 |
| 09.2 | Processed fish and fishery products including molluscs and crustaceans | Only salted fish of the Gadidae family that have been pre‐salted by injecting and/or brine salting with an at least 18% salt solution and often followed by dry salting | E 450 | Diphosphates | 5,000 | 1 , 79 |
| 09.2 | Processed fish and fishery products including molluscs and crustaceans | Only salted fish of the Gadidae family that have been pre‐salted by injecting and/or brine salting with an at least 18% salt solution and often followed by dry salting | E 451 | Triphosphates | 5,000 | 1 , 79 |
| 09.2 | Processed fish and fishery products including molluscs and crustaceans | Only salted fish of the Gadidae family that have been pre‐salted by injecting and/or brine salting with an at least 18% salt solution and often followed by dry salting | E 452 | Polyphosphates | 5,000 | 1 , 79 |
| 10.2 | Processed eggs and egg products | Only liquid egg (white, yolk or whole egg) | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 10,000 | 1 , 4 |
| 11.1 | Sugars and syrups as defined by Directive 2001/111/EC | Only dried powdered foods | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 10,000 | 4 |
| 11.4.2 | Table‐top sweeteners in powder form | E 341 | Calcium phosphates | Quantum satis | ||
| 12.1.1 | Salt | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 10,000 | 1 , 4 | |
| 12.1.2 | Salt substitutes | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 10,000 | 1 , 4 | |
| 12.5 | Soups and broths | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 3,000 | 1 , 4 | |
| 12.6 | Sauces | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 | |
| 12.9 | Protein products, excluding products covered in category 1.8 | Only vegetable protein drinks | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 20,000 | 1 , 4 |
| 13.1.1 | Infant formulae as defined by Directive 2006/141/EC | E 338 | Phosphoric acid | 1,000* | 4 , 44 | |
| 13.1.1 | Infant formulae as defined by Directive 2006/141/EC | E 339 | Sodium phosphates | 1,000* | 4 , 15 | |
| 13.1.1 | Infant formulae as defined by Directive 2006/141/EC | E 340 | Potassium phosphates | 4 , 15 | ||
| 13.1.2 | Follow‐on formulae as defined by Directive 2006/141/EC | E 338 | Phosphoric acid | 4 , 44 | ||
| 13.1.2 | Follow‐on formulae as defined by Directive 2006/141/EC | E 339 | Sodium phosphates | 1,000* | 4 , 15 | |
| 13.1.2 | Follow‐on formulae as defined by Directive 2006/141/EC | E 340 | Potassium phosphates | 4 , 15 | ||
| 13.1.3 | Processed cereal‐based foods and baby foods for infants and young children as defined by Directive 2006/125/EC | Only processed cereal based foods and baby foods, only for pH adjustment | E 338 | Phosphoric acid | 1,000* | 4 |
| 13.1.3 | Processed cereal‐based foods and baby foods for infants and young children as defined by Directive 2006/125/EC | Only cereals | E 339 | Sodium phosphates | 1,000* | 4 , 20 |
| 13.1.3 | Processed cereal‐based foods and baby foods for infants and young children as defined by Directive 2006/125/EC | Only cereals | E 340 | Potassium phosphates | 1,000* | 4 , 20 |
| 13.1.3 | Processed cereal‐based foods and baby foods for infants and young children as defined by Directive 2006/125/EC | Only cereals | E 341 | Calcium phosphates | 1,000* | 4 , 20 |
| 13.1.3 | Processed cereal‐based foods and baby foods for infants and young children as defined by Directive 2006/125/EC | Only in fruit‐based desserts | E 341 | Calcium phosphates | 1,000* | 4 |
| 13.1.3 | Processed cereal‐based foods and baby foods for infants and young children as defined by Directive 2006/125/EC | Only biscuits and rusks | E 450 | Diphosphates | 5,000* | 4 , 15 |
| 13.1.4 | Other foods for young children | E 338 | Phosphoric acid | 1 , 4 , 44 | ||
| 13.1.4 | Other foods for young children | E 339 | Sodium phosphates | 1,000* | 1 , 4 , 15 | |
| 13.1.4 | Other foods for young children | E 340 | Potassium phosphates | 1,000* | 1 , 4 , 15 | |
| 13.1.5.1 | Dietary foods for infants for special medical purposes and special formulae for infants | Only for pH adjustment | E 338 | Phosphoric acid | 1,000* | 1 , 4 |
| 13.1.5.1 | Dietary foods for infants for special medical purposes and special formulae for infants | E 339 | Sodium phosphates | 1,000* | 1 , 4 , 20 | |
| 13.1.5.1 | Dietary foods for infants for special medical purposes and special formulae for infants | E 340 | Potassium phosphates | 1,000* | 1 , 4 , 20 | |
| 13.1.5.1 | Dietary foods for infants for special medical purposes and special formulae for infants | E 341 | Calcium phosphates | 1,000* | 1 , 4 , 20 | |
| 13.1.5.2 | Dietary foods for babies and young children for special medical purposed as defined in Directive 1999/21/EC | E 338 | Phosphoric acid | 1,000* | 4 , 44 | |
| 13.1.5.2 | Dietary foods for babies and young children for special medical purposed as defined in Directive 1999/21/EC | E 339 | Sodium phosphates | 1,000* | 4 , 15 | |
| 13.1.5.2 | Dietary foods for babies and young children for special medical purposed as defined in Directive 1999/21/EC | E 340 | Potassium phosphates | 1,000* | 4 , 15 | |
| 13.1.5.2 | Dietary foods for babies and young children for special medical purposed as defined in Directive 1999/21/EC | E 341 | Calcium phosphates | 1,000* | 4 , 20 | |
| 13.1.5.2 | Dietary foods for babies and young children for special medical purposed as defined in Directive 1999/21/EC | Only biscuits and rusks | E 450 | Diphosphates | 5,000* | 4 , 15 |
| 13.2 | Dietary foods for special medical purposes defined in Directive 1999/21/EC (excluding products from food category 13.1.5) | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 | |
| 13.3 | Dietary foods for weight control diets intended to replace total daily food intake or an individual meal (the whole or part of the total daily diet) | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 | |
| 13.4 | Foods suitable for people intolerant to gluten as defined by Regulation (EC) No 41/2009 | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 | |
| 14.1.1 | Water, including natural mineral water as defined in Directive 2009/54/EC and spring water and all other bottled or packed waters | Only prepared table waters | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 500 | 1 , 4 |
| 14.1.4 | Flavoured drinks | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 700 | 1 , 4 | |
| 14.1.4 | Flavoured drinks | Only sport drinks | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 500 | 1 , 4 |
| 14.1.4 | Flavoured drinks | Only chocolate and malt dairy‐based drinks | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 2,000 | 1 , 4 |
| 14.1.4 | Flavoured drinks | Only whey protein containing sport drinks | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 4,000 | 1 , 4 |
| 14.1.4 | Flavoured drinks | Only vegetable protein drinks | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 20,000 | 1 , 4 |
| 14.1.5.2 | Other | Only coffee‐based drinks for vending machines; Instant tea and instant herbal infusions | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 2,000 | 1 , 4 |
| 14.2.3 | Cider and perry | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 1,000 | 1 , 4 | |
| 14.2.4 | Fruit wine and made wine | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 1,000 | 1 , 4 | |
| 14.2.5 | Mead | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 1,000 | 1 , 4 | |
| 14.2.6 | Spirit drinks as defined in Regulation (EC) No 110/2008 | Except: whisky, whiskey | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 1,000 | 1 , 4 |
| 14.2.7.1 | Aromatised wines | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 1,000 | 1 , 4 | |
| 14.2.7.2 | Aromatised wine‐based drinks | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 1,000 | 1 , 4 | |
| 14.2.7.3 | Aromatised wine‐product cocktails | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 1,000 | 1 , 4 | |
| 14.2.8 | Other alcoholic drinks including mixtures of alcoholic drinks with non‐alcoholic drinks and spirits with less than 15% of alcohol | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 1,000 | 1 , 4 | |
| 15.1 | Potato‐, cereal‐, flour‐ or starch‐based snacks | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 | |
| 15.2 | Processed nuts | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 | |
| 16 | Desserts excluding products covered in category 1, 3 and 4 | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 3,000 | 1 , 4 | |
| 16 | Desserts excluding products covered in category 1, 3 and 4 | Only dry powdered dessert mixes | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 7,000 | 1 , 4 |
| 17.1 | Food supplements supplied in a solid form, excluding food supplements for infants and young children | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | Quantum satis | ||
| 17.2 | Food supplements supplied in a liquid form, excluding food supplements for infants and young children | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | Quantum satis |
MPL: maximum permitted level; UHT: Ultra High Temperature.
The additives may be added individually or in combination.
The maximum level is expressed as P2O5.
E 339 and E 340 are authorised individually or in combination and in conformity with the limits set in Directives 2006/141/EC, 2006/125/EC, 1999/21/EC.
E 339, E 340 and E 341 are authorised individually or in combination.
In conformity with the limits set in Directives 2006/141/EC, 2006/125/EC, 1999/21/EC.
The maximum level shall apply unless a different maximum level is specified in points 01 to 18 of this Annex in relation to individual foods or categories of foods.
The maximum level applies to the sum of E 450, E 451 and E 452 used individually or in a combination.
The total amount of phosphates shall not exceed the maximum level for E 338–452.
The maximum levels of use indicated refer to foods ready for consumption prepared following manufacturer's’ instructions, for all subcategories under 13.1 Foods for infants and young children.
The Panel noted that for three food categories, no number for the maximum level is provided for certain provisions (see above for FC 13.1.1 for food additive E 340, FC 13.1.2 for food additive E 338 and E 340 and for FC 13.1.4 for food additive E 338). However, the footnotes associated with the provisions refer to the limits set in Directives 2006/141/EC, 2006/125/EC and 1999/21/EC which shall be respected. In addition, for E 340 in FC 13.1.1 and 13.1.2 the use level is set up individually or in combination with E 339 by the footnote (15).
The directives considered in the footnotes (15) or (44) prescribe that the maximum level of 1,000 mg/kg in the FC 13.1.1 for instance are applicable to all the phosphates additives authorised in the same food category. In the MPL scenario, the Panel agreed to use a MPL of 1,000 mg/kg for the food categories that for which MPLs were not provided (FCs 13.1.1, 13.1.2 and 13.1.4).
According to Annex III, Part 1 of Regulation (EC) No 1333/2008, calcium phosphates (E 341) is authorised as a carrier in all food additives at QS.
According to Annex III, Part 2 of Regulation (EC) No 1333/2008, E 338, E 339, E 340, E 343, E 450, E 451 are also authorised as food additive in preparations of the colour E 163 anthocyanins with a maximum level in the preparations of 40,000 mg/kg singly or in combination (expressed as P2O5). E 341 is also authorised, according to Part 2, as food additive:
-
–
in colour and emulsifier preparations with a maximum level in the preparations of 40,000 mg/kg (expressed as P2O5);
-
–
in polyol preparations and E 412 guar gum preparations with a maximum level in the preparation of 10,000 mg/kg (expressed as P2O5).
According to Annex III, Part 3 of Regulation (EC) No 1333/2008, phosphoric acid (E 338) is also authorised as a food additive in food enzymes with a maximum level in the enzymes preparation of 10,000 mg/kg (expressed as P2O5) and at QS in the final products (food or beverages).
According to Annex III, Part 3 of Regulation (EC) No 1333/2008, E 339, E 340, E 341, E 343 are also authorised as a food additive in food enzymes with a maximum level in the enzymes preparation of 50,000 mg/kg (expressed as P2O5) and at QS in the final products (food or beverages). These food additives are also authorised to be used as carriers.
According to Annex III, Part 3 of Regulation (EC) No 1333/2008, E 450, E 451, E 452 are also authorised as a food additive in food enzymes with a maximum level in the enzymes preparation of 50,000 mg/kg (expressed as P2O5) and at QS in the final products (food or beverages).These food additives are not authorised to be used as carriers.
According to Annex III, Part 4, phosphates (E 338–341, E 343, E 450–452) are authorised at the maximum level of 40,000 mg/kg (singly or in combination expressed as P2O5) in all flavourings.
In addition, according to Annex III, Part 5, Section A of Regulation (EC) No 1333/2008, phosphates (E 338–341, E 343, E 450–452) are also authorised at the maximum level of 40,000 mg/kg expressed as P2O5 in the nutrient preparation, in all nutrients.
According to Annex III, Part 5, Section B of Regulation (EC) No 1333/2008, tricalcium phosphate (E 341(iii) is also authorised at the maximum carry‐over of 150 mg/kg as P2O5 and within the limit for calcium, phosphorus and calcium:phosphorus ratio as set in Directive 2006/141/EC in all nutrients in infant formulae and follow‐on formulae as defined by Directive 2006/141/EC; and at the maximum level of 1,000 mg/kg expressed as P2O5 from all uses in final food mentioned in point 13.1.3 of Part E of Annex II is respected in all nutrients in processed cereal based foods and baby foods for infants and young children as defined by Directive 2006/141/EC.
3.2.1. Proposed extension of use
One request for extension of use was also considered in the exposure estimates. The request referred to the removal of the restriction ‘only sugar confectionary’ in the food category 05.2 ‘Other confectionary including breath refreshing microsweets’. This request would change the Regulation (EC) No 1333/2008 as reported in Table 3.
Table 3.
Proposed uses and maximum use levels for phosphates (E 338–341, E 343, E 450–452) in food category 05.2 following the requested extension of use
| Food category code | Food category name | Restrictions/exceptions | E‐number | Name | MPL (mg/L or mg/kg as appropriate) | Footnotes (as in Reg (EC) No 1333/2008) |
|---|---|---|---|---|---|---|
| 05.2 | Other confectionery including breath refreshening microsweets | Only candied fruit | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 800 | 1 , 4 |
| 05.2 | Other confectionery including breath refreshening microsweets | Except candied fruit | E 338–452 | Phosphoric acid–phosphates – di‐, tri‐ and polyphosphates | 5,000 | 1 , 4 |
MPL: maximum permitted level.
The additives may be added individually or in combination.
The maximum level is expressed as P2O5.
3.3. Exposure data
3.3.1. Reported use levels or data on analytical levels of phosphates (E 338–341, E 343, E 450–452)
Most food additives in the EU are authorised at a specific MPL. However, a food additive may be used at a lower level than the MPL. Therefore, information on actual use levels is required for performing a more realistic exposure assessment, especially for those food additives for which no MPL is set and which are authorised according to QS. In the case of phosphates additives, only chewing‐gum and food supplements were authorised at QS.
In the framework of Regulation (EC) No 1333/2008 on food additives and of Commission Regulation (EU) No 257/2010 regarding the re‐evaluation of approved food additives, EFSA issued a public call14 for occurrence data (usage level and/or concentration data) on phosphates (E 338–341, E 343, E 450–452). In response to this call, both types of data on phosphates (E 338–341, E 343, E 450–452) were submitted to EFSA by industry and Member States, respectively.
Summarised data on reported use levels in foods provided by industry
Industry provided EFSA with data on use levels (n = 1,298) of phosphates (E 338–341, E 343, E 450–452) in foods for 89 out of the 108 authorised uses in which phosphates (E 338–341, E 343, E 450–452) are authorised.
Updated information on the actual use levels of phosphates (E 338–341, E 343, E 450–452) in foods was made available to EFSA by the Association des Entreprises Produits Alimentaires Elabores (ADEPALE), Association of the European Self‐Medication Industry (AESGP), Comité Européen des Fabricants de Sucre (CEFS), Dr Loges Naturheilkunde neu entdecken, European Chemical Industry Council (CEFIC), European Dairy Association (EDA), European Fish Processors and Traders Association & European Federation of National Organisations of Importers and Exporters of Fish (AIPCE‐CEP), European Potato Processors’ Association (EUPPA), Food Drink Europe (FDE), Food Supplement Europe (FSE), IMACE, International Chewing Gum Association (ICGA), Intersnack, L'ALLIANCE 7, Nathura, Specialised Nutrition Europe (SNE).
The Panel noted that a data provider (namely CEFIC) is not a food industry using phosphates in its food products but is an association representing food additive producers/chemical suppliers and not directly using these substances as additives in foods. Usage levels reported by food additive producers are not considered at the same level as those provided by food industry. Food additive producers may recommend usage levels to the food industry but the final levels might, ultimately, be different. Therefore, unless food additive producers confirm that the recommended levels are used by food industry, they are not considered in the refined exposure scenario. In this opinion, data coming from CEFIC were not considered in the refined assessment. These data are nevertheless presented in the Appendix F.
Data provided by Nathura (n = 3) were also discarded from the current exposure estimates. These data were initially checked with the provider but the levels submitted were found not to be correct as these levels would results in a phosphates content which is higher than 100%.
The Panel noted that 325 usage levels referred to niche products. When other usage levels were available for the same authorised uses, the Panel decided to exclude them from further analysis. Levels from niche products were used for unflavoured pasteurised and sterilised (including UHT) milk (FC 01.1), chewing‐gum (FC 05.3) and processed cereal‐based foods and baby foods for infants and young children (FC 13.1.3) in the absence of other levels.
The Panel also noted that levels provided for the use of phosphates as nutrient sources (e.g. phosphates in formulae) and not as food additives. These levels were not taken into account for estimating exposure of phosphates (E 338–341, E 343, E 450–452) as food additives.
Some data (n = 190) were provided as phosphates (‘E 338–452’) or as mixture of different E‐numbers.
Most of the data submitted to EFSA were expressed directly in P2O5, the other in the food additive added. In the latter, thanks to the availability of the specific E‐number, the use levels were converted into P2O5, based on the conversion factors (see Appendix B). However, some data providers are using phosphates in a subcomponent of their final product. In these instances, the E number subcategories (i, ii, iii) were not specified. Thus, the levels could not be expressed as P2O5, which is the case for all data on snacks (n = 7) and 73 levels on food supplements. Food supplements and snacks use levels not expressed as P2O5, were converted using the converting factors reported in Appendix B. In case the salt is not specified, the factor used to convert this level in P2O5 is the one of the anhydrous form and this could lead to an overestimation. The use levels not expressed as P2O5 are indicated in Appendix F.
Some levels were submitted for food categories not listed in Table 1. However, phosphates could be used in those as these foods are in dried powdered form and can contain phosphates. This is the case for:
-
–
icing sugar (belonging to FC 11.2)
-
–
pasta (FC 06.4.2) with seasonings.
Some levels were also submitted for FC 07.1 Bread and rolls. Foods belonging to this category can contain phosphates from their authorisation and uses in their ingredients [e.g. flour (FC 06.2.1), decorations, coatings and fillings (FC 05.4)]. After considering all the data, the Panel agreed that for FC 07.1 maximum uses reported by industry were used in the regulatory maximum exposure assessment scenario.
Appendix F provides data on the use levels of phosphates (E 338–341, E 343, E 450–452) in foods as reported by industry.
Summarised data on analytical results in food submitted by Member States
In total, 2,418 analytical results were reported to EFSA by 10 countries: Belgium (n = 379), the Czech Republic (n = 674), Germany (n = 310), Hungary (n = 302), Ireland (n = 42), Italy (n = 18), Lithuania (n = 66), Portugal (n = 6), Spain (n = 325) and the UK (n = 296). Substances analysed were expressed either as phosphorus (P), phosphoric acid or sum of phosphates expressed as P2O5. For this evaluation all results were converted to P.
Some of the analytical results were left‐censored (LC): either not quantified (< LOQ) in 824 samples or not detected (< LOD) in 14 samples. To consider left‐censored analytical data (i.e. analytical results < LOD or < LOQ), the substitution method as recommended in the ‘Principles and Methods for the Risk Assessment of Chemicals in Food’ (WHO, 2009) and the EFSA scientific report ‘Management of left‐censored data in dietary exposure assessment of chemical substances’ (EFSA, 2010) was used. In the present opinion, analytical data below LOD or LOQ were assigned half of LOD or LOQ, respectively. Therefore, it should be noted that the use of middle‐bound (MB) LOD/LOQ values (half of LOD or LOQ) in the exposure assessment, may have resulted in either an overestimation, where phosphates were not present, or underestimation, where the concentration was between the MB and LOQ/LOD value, but the analytical method was not able to detect or quantify it. The higher percentage of left‐censored data was observed for the food categories confectionary (FC 05.2, 96.7% of LC data), water (FC 14.1.1, 81.8% LC data), flavoured drinks (FC 14.1.4, 72.6% of LC data). Some left‐censored samples were identified with a very high LOQ. While checking LOQ with the data provider, it appears that there was an error in the reporting of the LOQ. Therefore, these samples were discarded.
Complete information on the methods of analysis (e.g. validation) was not made available to EFSA, but all samples were analysed by accredited laboratories. Data were sampled between 2009 and 2016 and analysed between 2009 and 2017. The Panel noted that the methods of analysis applied are generally not able to differentiate between phosphates added as food additives and naturally present in foods.
The majority of the data (n = 2,252) were expressed as μg/kg and were converted to mg/kg as were levels expressed in percent (n = 66) whereas the levels expressed in kcal (n = 1) or per 100 kcal (n = 99) were discarded since no information on the food energy content was available.
The food categories with the most data were FC 15.1 snacks (n = 507), FC 14.1.4 flavoured drinks (n = 500), confectionery FC 05.2 (n = 212), unprocessed fruits and vegetables FC 04.1 (n = 159).
Almost all food categories according to the food additives nomenclature (Part D to Regulation No 1333/2008) are covered by the analytical data available. Data on chewing‐gums, processed eggs, some sugars and syrups, salts, FSMP for infants and young children, some alcoholic beverages and food supplements were not available.
Overall, 2,271 analytical results reported for phosphates in foods were used by the Panel in the exposure assessment.
Appendix G shows the analytical results of phosphates in foods as reported by Member States.
3.3.2. Summarised data extracted from the Mintel's Global New Products Database
The Mintel's GNPD is an online database which monitors new introductions of packaged goods in the market worldwide. It contains information of more than 1,000,000 food and beverage products that are or have been available on the European food market. Mintel started covering EU's food markets in 1996, currently having 20 out of its 28 member countries and Norway presented in the Mintel's GNPD.15
For the purpose of this Scientific Opinion, the Mintel's GNPD16 was used for checking the labelling of food and beverages products and food supplements for phosphates (E 338–341, E 343, E 450–452) within the EU's food market as the database contains the compulsory ingredient information on the label.
According to the Mintel's GNPD, phosphates (E 338–341, E 343, E 450–452) was labelled on many products (n = 44178) between January 2014 and March 2019 (more than 84,000 since 1996).
Appendix H lists the percentage of the food products labelled with phosphates (E 338–341, E 343, E 450–452) out of the total number of food products per food subcategories according to the Mintel's GNPD food classification. The percentages ranged from less than 0.1% in many food subcategories to 73% for evaporated milk (up to 100% in the Mintel's GNPD food subcategory ‘Growing Up Milk (4+ years)’ but this category contains only 3 products). Infants and toddlers formulae contain quite largely phosphates in their ingredients (more than 50% of products). Bread and bread products as well as fine bakery wares are also labelled with phosphates for more than 10% of the products on the European market.
The average percentage of foods labelled to contain phosphates (E 338–341, E 343, E 450–452) was 9.6%.
No data were provided to EFSA for certain products labelled as containing phosphates in which phosphates are authorised. These include:
-
–
alcoholic beverages,
-
–
white milk: the few milks found in Mintel are mainly enriched with calcium, or white milk other than from cow, e.g. goat, sheep. Levels of phosphates were provided for goat milk only, while phosphates (E 338–341, E 343, E 450–452) are authorised in all sterilised and UHT milk.
-
–
eggs & egg products,
-
–
nuts,
-
–
hard cheese & semi‐hard cheese: it is not clear whether these food items are part of FC 01.7.5 Processed cheeses or contain phosphates because are seasoned cheeses or cheese with other ingredients (such as chorizo),
-
–
vegetables.
Phosphates (E 338–341, E 343, E 450–452) were found to be labelled in Mintel food categories of nectar and juices. FCs 14.1.2 and 14.1.3 are not authorised to contain phosphates. However, it is not clear whether nectars and juices as coded in the Mintel GNPD completely match with fruit juices and fruit nectars as defined in the legislation.
In most of these subcategories, the percentage of foods labelled with phosphates was low.
Approximately one‐third of the products are labelled as containing diphosphates (E 450).
3.3.3. Food consumption data used for exposure assessment
EFSA Comprehensive European Food Consumption Database
Since 2010, the EFSA Comprehensive European Food Consumption Database (Comprehensive Database) has been populated with national data on food consumption at a detailed level. Competent authorities in the European countries provide EFSA with data on the level of food consumption by the individual consumer from the most recent national dietary survey in their country (cf. Guidance of EFSA on the ‘Use of the EFSA Comprehensive European Food Consumption Database in Exposure Assessment’ (EFSA, 2011a). Consumption surveys added in the Comprehensive database in 2015 were also taken into account in this assessment.17
The food consumption data gathered by EFSA were collected by different methodologies and thus direct country‐to‐country comparisons should be interpreted with caution. Depending on the food category and the level of detail used for exposure calculations, uncertainties could be introduced owing to possible subjects’ underreporting and/or misreporting of the consumption amounts. Nevertheless, the EFSA Comprehensive Database includes the currently best available food consumption data across Europe.
Food consumption data from the following population groups were used for the exposure assessment: infants, toddlers, children, adolescents, adults and the elderly. For the present assessment, food consumption data were available from 33 different dietary surveys carried out in 19 European countries (Table 4).
Table 4.
Population groups considered for the exposure estimates of phosphates (E 338–341, E 343, E 450–452)
| Population | Age range | Countries with food consumption surveys covering more than 1 day |
|---|---|---|
| Infants < 16 weeks | From birth up to and including 16 weeks of age | Not applicablec |
| Infants | From more than 12 weeks up to and including 11 months of age | Bulgaria, Denmark, Finland, Germany, Italy, UK |
| Toddlersa | From 12 months up to and including 35 months of age | Belgium, Bulgaria, Denmark, Finland, Germany, Italy, Netherlands, Spain, UK |
| Childrenb | From 36 months up to and including 9 years of age | Austria, Belgium, Bulgaria, Czech Republic, Denmark, Finland, France, Germany, Greece, Italy, Latvia, Netherlands, Spain, Sweden, UK |
| Adolescents | From 10 years up to and including 17 years of age | Austria, Belgium, Cyprus, Czech Republic, Denmark, Finland, France, Germany, Italy, Latvia, Netherlands, Spain, Sweden, UK |
| Adults | From 18 years up to and including 64 years of age | Austria, Belgium, Czech Republic, Denmark, Finland, France, Germany, Hungary, Ireland, Italy, Latvia, Netherlands, Romania, Spain, Sweden, UK |
| The elderlyb | From 65 years of age and older | Austria, Belgium, Denmark, Finland, France, Germany, Hungary, Ireland, Italy, Romania, Netherlands, Sweden, UK |
The term ‘toddlers’ in the EFSA Comprehensive Database corresponds to ‘young children’ in Regulations (EC) No 1333/2008 and (EU) No 609/2013.
The terms ‘children’ and ‘the elderly’ correspond, respectively, to ‘other children’ and the merge of ‘elderly’ and ‘very elderly’ in the Guidance of EFSA on the ‘Use of the EFSA Comprehensive European Food Consumption Database in Exposure Assessment’ (EFSA, 2011a).
Recommended values of 200 and 260 mL/kg bw per day as conservative mean and high level consumption values were used (EFSA Scientific Committee, 2017).
Consumption records were codified according to the FoodEx classification system (EFSA, 2011b). Nomenclature from the FoodEx classification system has been linked to the food categorisation system (FCS) as presented in Annex II of Regulation (EC) No 1333/2008, part D, to perform exposure estimates. In practice, the FoodEx food codes were matched to the FCS food categories.
Food categories considered for the exposure assessment of phosphates (E 338–341, E 343, E 450–452)
The food categories in which the use of phosphates (E 338–341, E 343, E 450–452) is authorised were selected from the nomenclature of the EFSA Comprehensive Database (FoodEx classification system), at the most detailed level possible (up to FoodEx Level 4) (EFSA, 2011b).
Some food categories or their restrictions/exceptions are not referenced in the EFSA Comprehensive Database and could therefore not be taken into account in the present estimate. This was the case for 15 authorised uses (Appendix I) and may have resulted in an underestimation of the exposure. The authorised uses which were not taken into account are described below (in ascending order of the FCS codes):
01.7.6 Cheese products (excluding products falling in category 16), only unripened products
02.3 Vegetable oil pan spray, only water‐based emulsion sprays for coating baking tins
04.2.4.1 Fruit and vegetable preparations excluding compote, only seaweed based fish roe analogues
04.2.4.1 Fruit and vegetable preparations excluding compote, only glazing for vegetable products
06.2.1 Flours, only self‐raising flour. Self‐raising flour is not a food item available in the FoodEx nomenclature and only flour (with no restrictions) was used at the MPL of 2,500 mg/kg.
06.6 Batters
07.1 Bread and rolls, only soda bread
08.2 Meat preparations as defined by Regulations (EC) No 853/2004, only breakfast sausages: in this product, the meat is minced in such a way so that the muscle and fat tissue are completely dispersed, so that fibre makes an emulsion with the fat, giving the product its typical appearance; Finnish grey salted Christmas ham, burger meat with a minimum vegetable and/or cereal content of 4% mixed within the meat, Kasseler, Bräte, Surfleisch, toorvorst, šašlõkk, ahjupraad, Bílá klobása, Vinná klobása, Sváteční klobása, Syrová klobása and frozen vertical rotating meat spits made of sheep, lamb, veal and/or beef treated with liquid seasoning or from poultry meat treated with or without liquid seasoning used alone and/or combined as well as sliced and/or minced and designed to be roasted by a food business operator and then consumed by the final consumer.
08.3.3 Casings and coatings and decorations for meat, only glazings for meat
10.2 Processed eggs and egg products, only liquid egg (white, yolk or whole egg)
12.1.2 Salt substitutes
14.1.1 Water, including natural mineral water as defined in Directive 2009/54/EC and spring water and all other bottled or packed waters, only prepared table waters
14.1.4 Flavoured drinks, the restriction only whey protein containing sport drinks cannot be differentiated from the sport drinks, therefore all sport drinks were taken into account at MPL of 500 mg/kg, while MPL for whey protein containing sport drinks equals 20,000 mg/kg.
14.2.4 Fruit wine and made wine
14.2.5 Mead
For the following authorised uses, the restrictions/exceptions which apply to the use of phosphates (E 338–341, E 343, E 450–452) could not be taken into account, and therefore, the whole food category was considered in the exposure assessment. This applies to seven food categories (Appendix I) and may have resulted in an overestimation of the exposure:
01.5 Dehydrated milk as defined by Directive 2001/114/EC, the two restrictions (only partly dehydrated milk with less than 28% solids/only partly dehydrated milk with more than 28% solids) cannot be differentiated. Foods from the FC 01.5 were divided into two subcategories: dehydrated milk at the MPL of 1,500 mg/kg and dried milk at the MPL of 2,500 mg/kg.
01.8 Dairy analogues, including beverage whiteners, only beverage whiteners for vending machines. All beverages whiteners (for vending machines or not) were taken into account at the same MPL of 30,000 mg/kg.
05.4 Decorations, coatings and fillings, except fruit based fillings covered by category 4.2.4, the restriction ‘only toppings (syrups for pancakes, flavoured syrups for milkshakes and ice cream; similar products’ cannot be differentiated from the whole food category. Therefore the whole FC 05.4 was taken into account at the MPL of 5,000 mg/kg.
08.3.2 Heat–treated meat products, except foie gras, foie gras entier, blocs de foie gras, Libamáj, libamáj egészben, libamáj tömbben.
09.2 Processed fish and fishery products including molluscs and crustaceans, only salted fish of the Gadidae family that have been pre‐salted by injecting and/or brine salting with an at least 18% salt solution and often followed by dry salting: fishes from the Gadidae family (i.e. cod and whiting) were taken into account as the restriction cannot be applied.
14.1.5.2 Other, only coffee‐based drinks for vending machines
16 Desserts, only dry powdered mixes.
The FCs 17.1/17.2 Food supplements, in solid, liquid form, the form cannot be differentiated and the same use level was applied to the whole FC 17. This would lead to an overestimate if use levels of food supplements supplied in solid form are higher than use levels of food supplements supplied in liquid form.
Phosphates (E 338–341, E 343, E 450–452) are authorised in the sterilised and UHT milk of the FC 01.1 unflavoured pasteurised and sterilised milk. Use levels were reported from food industry only on goat milk. Considering that information retrieved from Mintel shows few cow milks (mainly enriched ones), goat or sheet milk labelled with phosphates (E 338–341, E 343, E 450–452), only goat milk available in the FoodEx nomenclature were considered.
Phosphates (E 338–341, E 343, E 450–452) are also allowed in FC 13.2, 13.3 and 13.4. Food items under food categories 13.2, 13.3 and 13.4 consumed by population groups – children, adolescents, adults and the elderly – may be very diverse and, in addition, there is very limited information on their consumption. Therefore, eating occasions belonging to the food categories 13.2, 13.3 and 13.4 were reclassified under food categories in accordance to their main component.
The use levels available for food categories 13.2, 13.3 and 13.4 were not considered for the exposure assessment.
3.4. Exposure estimates
3.4.1. Exposure to phosphates (E 338–341, E 343, E 450–452) from its use as food additives
The Panel estimated the chronic dietary exposure to phosphates (E 338–341, E 343, E 450–452) for the following population groups: infants, toddlers, children, adolescents, adults and the elderly. Dietary exposure to phosphates (E 338–341, E 343, E 450–452) was calculated by multiplying concentrations of phosphates (E 338–341, E 343, E 450–452) expressed as P2O5 per food category (Appendix I) with their respective consumption amount per kilogram body weight for each individual in the Comprehensive Database. The exposure per food category was subsequently added to derive an individual total exposure per day. These exposure estimates were averaged over the number of survey days, resulting in an individual average exposure per day for the survey period. Dietary surveys with only 1 day per subject were excluded as they are considered as not adequate to assess repeated exposure.
This was carried out for all individuals per survey and per population group, resulting in distributions of individual exposure per survey and population group (Table 4). On the basis of these distributions, the mean and 95th percentile of exposure were calculated per survey and per population group. The 95th percentile of exposure was only calculated for those population groups with a sufficiently large sample size (EFSA, 2011a). Therefore, in the present assessment, the 95th percentile of exposure for infants from Italy and for toddlers from Belgium, Italy and Spain were not estimated.
Reported use levels from industry give information on the amount of the food additive added to food.
Exposure assessment to phosphates (E 338–341, E 343, E 450–452) was carried out by the FAF Panel based on two different sets of concentration data: (1) MPLs as set down in the EU legislation (defined as the regulatory maximum level exposure assessment scenario); and (2) reported use levels (defined as the refined exposure assessment scenario). These two scenarios are discussed in detail below.
These scenarios do not consider the consumption of food supplements and FSMP. These exposure sources are covered in two additional scenarios detailed below (foods for special medical purposes consumer only scenario and food supplements consumers only scenario).
A possible additional exposure from the use of phosphates (E 338–341, E 343, E 450–452) as food additives as carriers in food additives, in food colours, food enzymes, food flavourings and in nutrients in accordance with Annex III to Regulation (EC) No 1333/2008 (Parts 1, 2, 3, 4, 5 Sections A and B) was not considered in exposure assessment scenarios.
Regulatory maximum level exposure assessment scenario
The regulatory maximum level exposure assessment scenario is based on the MPLs as set in Annex II to Regulation (EC) No 1333/2008 and listed in Table 2. For the four uses authorised according to QS, the maximum of the reported use levels was used (Appendix I).
The Panel considers the exposure estimates derived following this scenario as the most conservative since it is assumed that that the population will be exposed to the food additives present in food at the MPL/maximum reported use levels over a lifetime.
Refined exposure assessment scenario
The refined exposure assessment scenario is based on use levels reported by food industry. This exposure scenario can consider only authorised uses for which these data were available to the Panel.
Appendix I summarises the concentration levels of phosphates (E 338–341, E 343, E 450–452) used in the refined exposure assessment scenario. Based on the available data set, the Panel calculated two refined exposure estimates based on two model populations:
-
The brand‐loyal consumer scenario: It was assumed that a consumer is exposed long‐term to phosphates (E 338–341, E 343, E 450–452) present at the maximum reported use level for one food category. This exposure estimate is calculated as follows:
-
–
Combining food consumption with the maximum of the reported use levels for the main contributing food category at the individual level.
-
–
Using the mean of the typical reported use levels for the remaining authorised uses.
-
–
The non‐brand‐loyal consumer scenario: It was assumed that a consumer is exposed long‐term to phosphates (E 338–341, E 343, E 450–452) present at the mean reported use levels in food. This exposure estimate is calculated using the mean of the typical reported use levels for all authorised uses.
Exposure assessment for specific population groups
Infants below 16 weeks:
Exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives for infants below 16 weeks was also estimated. This scenario is based on the recommended consumption levels from Scientific Committee Guidance (EFSA Scientific Committee, 2017). This guidance ‘recommends values of 200 and 260 mL/kg bw per day as conservative mean and high level consumption values to be used for performing the risk assessments of substances which do not accumulate in the body present in food intended for infants below 16 weeks of age’. These recommended consumption levels correspond to 14‐ to 27‐day‐old infants consumption. For regulatory maximum level exposure assessment scenario, MPL for infant formulae of 1,000 mg/kg was used and for the refined scenario, reported use levels (typical and maximum) were considered.
Exposure on a body weight basis is the metric used to compare exposure with the ADI value but exposure per person is also provided in the Tables for ease of reference. A body weight of 4 kg (EFSA NDA Panel, 2018) was used for this specific assessment of infants below 16 weeks of age. This body weight is the median weight of 4 weeks girl infants according to the report from Van Buuren et al. (2012).
Some carers use bottled water rather than tap water to reconstitute formulae powder and make it ready to feed. Phosphates are permitted to be added to bottled waters (Table 2, food category 14.1.1) but only for ‘prepared table waters’. Inspection of the Mintel database revealed no incidences of still (uncarbonated) bottled water containing phosphate additives being recorded. There were a few entries (n = 14) covered by this general food code but they were for flavoured water beverages. The scenario of using bottled water containing phosphate additives to reconstitute formulae power was therefore not used.
‘Food supplement consumers only’:
Phosphates (E 338–341, E 343, E 450–452) are authorised in the food category 17 Food supplements as defined in Directive 2002/46/EC excluding food supplements for infants and young children. As exposure via food supplements may deviate largely from the one via food, and that the number of food supplement consumers may be low depending on populations and surveys, an additional estimate was calculated in order to reflect additional exposure to food additives from food supplements compared to exposure to food additives excluding these sources. This will be estimated as follow:
-
–
Consumers only of food supplements will be assumed to be exposed to phosphates (E 338–341, E 343, E 450–452) present at the maximum reported use levels on a daily basis via consumption of food supplements.
-
–
For the remaining authorised uses, the mean of the typical reported use levels is used.
As food category 17 do not consider food supplements for infants and toddlers as defined in the legislation, exposure to phosphates (E 338–341, E 343, E 450–452) from food supplements are not estimated for these two population groups.
This exposure assessment included all authorised uses for general population and food supplements (Appendix I).
FSMP consumers only:
As phosphates (E 338–341, E 343, E 450–452) are also authorised in the food categories 13.1.5.1 and 13.1.5.2, an additional exposure assessment taking into account these two food categories was performed to estimate the exposure of infants and toddlers who may eat and drink these FSMP.
The consumption of these foods is not reported in the EFSA Comprehensive database. To consider potential exposure to phosphates (E 338–341, E 343, E 450–452) via these foods, the Panel assumes that the amount consumed of FSMP in infants and toddlers resembles that of comparable foods in infants and toddlers from the general population. Thus, the consumption of FSMP categorised as food category 13.1.5 is assumed to equal that of formulae and food products categorised as food categories 13.1.1, 13.1.2, 13.1.3 and 13.1.4.
Phosphates (E 338–341, E 343, E 450–452) are also allowed in FSMP consumed in other population groups (FC 13.2, 13.3 and 13.4). Food items under food categories 13.2, 13.3 and 13.4 consumed by population groups – children, adolescents, adults and the elderly – may be very diverse and, in addition, there is very limited information on their consumption. Therefore, eating occasions belonging to the food categories 13.2, 13.3 and 13.4 were reclassified under food categories in accordance to their main component. The use levels available for food categories 13.2, 13.3 and 13.4 were not considered for the exposure assessment and no exposure estimates were calculated for these population groups.
This exposure assessment was estimated as follows:
-
–
Consumers only of FSMP were assumed to be exposed to phosphates (E 338–341, E 343, E 450–452) present at the maximum reported use level on a daily basis via consumption of food categories 13.1.5.1 and 13.1.5.2 (infant formulae, follow‐on formulas and processed cereal‐based foods and baby foods for infants and young children as defined by Commission Directive 2006/125/EC).
-
–
For the remaining authorised uses, the mean of the typical reported use levels was used.
This estimate included 50 authorised uses (Appendix I).
Dietary exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives
Tables 5a,b summarise the estimated exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives in seven population groups (Table 4) according to the different exposure scenarios. Results are presented in mg phosphorus (P) per person and per day and in mg P/kg bw per day. Results expressed mg P2O5 per person and per day and mg P2O5/kg bw per day are available in the appendixes to the opinion (Appendix J). Detailed results per population group and survey (in mg P2O5/kg bw per day) are also presented in Appendix K.
Table 5a.
Summary of dietary exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives in the regulatory maximum level exposure assessment scenario and in the refined exposure assessment scenarios, in seven population groups (minimum–maximum across the dietary surveys in mg P/person per day)
| Infants below 16 weeks | Infants (12 weeks–11 months) | Toddlers (12–35 months) | Children (3–9 years) | Adolescents (10–17 years) | Adults (18–64 years) | The elderly (≥ 65 years) | |
|---|---|---|---|---|---|---|---|
| Regulatory maximum level exposure assessment scenario | |||||||
| • Mean | 349 | 198–998 | 446–1,554 | 725–1,751 | 857–1,945 | 850–1,867 | 890–1,848 |
| • 95th percentile | 454 | 419–1,714 | 753–2,052 | 1,070–2,959 | 1,461–3,462 | 1,530–3,638 | 1,510–3,551 |
| Refined estimated exposure assessment scenario | |||||||
| Brand‐loyal scenario | |||||||
| • Mean | 213 | 96–309 | 101–372 | 108–620 | 130–733 | 319–722 | 337–747 |
| • 95th percentile | 278 | 222–570 | 203–745 | 215–1,291 | 287–1,603 | 658–1,600 | 683–1,559 |
| Non‐brand‐loyal scenario | |||||||
| • Mean | 192 | 81–141 | 78–152 | 69–237 | 74–298 | 126–278 | 121–241 |
| • 95th percentile | 250 | 191–253 | 153–266 | 135–613 | 155–749 | 253–636 | 212–480 |
Table 5b.
Summary of dietary exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives in the regulatory maximum level exposure assessment scenario and in the refined exposure assessment scenarios, in seven population groups (minimum–maximum across the dietary surveys in mg P/kg bw per day)
| Infants below 16 weeks | Infants (12 weeks–11 months) | Toddlers (12–35 months) | Children (3–9 years) | Adolescents (10–17 years) | Adults (18–64 years) | The elderly (≥ 65 years) | |
|---|---|---|---|---|---|---|---|
| Regulatory maximum level exposure assessment scenario | |||||||
| • Mean | 87 | 25–113 | 45–113 | 39–82 | 16–40 | 12–27 | 12–24 |
| • 95th percentile | 113 | 53–196 | 73–145 | 61–148 | 29–84 | 22–58 | 21–48 |
| Refined estimated exposure assessment scenario | |||||||
| Brand‐loyal scenario | |||||||
| • Mean | 53 | 12.0–35.0 | 10.1–27.2 | 5.9–25.6 | 2.4–16.6 | 4.4–10.6 | 4.7–9.9 |
| • 95th percentile | 69 | 27.4–65.7 | 20.6–53.6 | 11.4–55.9 | 5.1–37.0 | 9.1–25.2 | 9.4–20.2 |
| Non‐brand‐loyal scenario | |||||||
| • Mean | 48 | 10.2–15.8 | 5.5–11.1 | 3.7–9.9 | 1.4–6.8 | 1.8–3.7 | 1.7–3.2 |
| • 95th percentile | 62 | 21.5–38.9 | 12.6–21.2 | 7.3–26.5 | 3.0–17.1 | 3.6–8.2 | 3.1–7.1 |
bw: body weight.
In the regulatory maximum level exposure assessment scenario, the mean exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives ranged from 198 mg P/person per day in infants (> 12 weeks) to 1,945 mg P/person per day in adolescents. The high (95th percentile) exposure ranged from 419 mg/person per day in infants (> 12 weeks) to 3,638 mg/person per day in adults.
In the brand‐loyal refined estimated exposure scenario, the mean exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives ranged from 96 mg P/person per day in infants (> 12 weeks) to 747 mg P/person per day for the elderly, and the high exposure (95th percentile) from 203 mg P/person per day in toddlers to 1,600 mg P/person per day for adolescents, adults and the elderly. In the non‐brand‐loyal scenario, mean exposure ranged from 69 mg P/person per day in children to 298 mg P/person per day in adolescents, and the high exposure from 135 mg P/person per day in children to 749 mg P/person per day in adolescents.
Exposure estimated for infants below 16 weeks of age was between 349 mg P/person per day at the mean and 454 mg P/person per day at the high level (95th percentile) when using the MPLs (regulatory maximum level exposure assessment scenario). In the refined estimated exposure scenario, the mean exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives was estimated at 213 mg P/person per day at the mean and 278 mg P/person per day at the high level for the brand‐loyal scenario while for the non‐brand‐loyal scenario, the estimates were 192 mg P/person per day at the mean and 250 mg P/person per day at the high level.
In the refined estimated exposure scenario taking into account the foods for special medical purposes (FSMP) for infants and toddlers, mean exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives ranged for infants between 111 and 209 mg P/person per day and between 66 and 157 mg P/person per day for toddlers. The 95th percentile of exposure to phosphates (E 338–341, E 343, E 450–452) ranged for infants between 199 and 463 mg/person per day and for toddlers between 201 and 217 mg/person per day. Results of infants and toddlers exposure expressed per kg bw are presented in the table below (Table 6).
Table 6.
Summary of dietary exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives for FSMP consumers only, in infants and toddlers (minimum–maximum across the dietary surveys in mg P/kg bw per day)
| Infants (< 16 weeks) | Infants (12 weeks–11 months) | Toddlers (12–35 months) | |
|---|---|---|---|
| • Mean | 87 | 13–29 | 4–14 |
| • 95th percentile | 113 | 26–76 | 17–20 |
bw: body weight.
For the food supplements consumers only, mean exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives ranged from 275 mg P/person per day for children to 1,541 mg P/person per day for the elderly. The 95th percentile of exposure to phosphates (E 338–341, E 343, E 450–452) ranged from 753 mg P/person per day for adolescents to 7,292 mg P/person per day for adults. The Panel noted the high levels for food supplements compared to therapeutic use (see Section 3.8.1). According to data providers, in a number of cases, the phosphates are added principally as nutrient substance and not as additives. However, in other cases, the addition of phosphates (e.g. higher reported use levels) is due to their technical requirements as food additives rather than an intended use as nutrient sources. The Panel noted the high intakes resulting from such levels and the potential risk for people who might consume food supplements regularly.
Results of children, adolescents, adults and the elderly exposure expressed per kg bw are presented in the table below (Table 7).
Table 7.
Summary of dietary exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives for food supplements consumers only, in children, adolescents, adults and the elderly (minimum–maximum across the dietary surveys in mg P/kg bw per day)
| Children (3–9 years) | Adolescents (10–17 years) | Adults (18–64 years) | The elderly (≥ 65 years) | |
|---|---|---|---|---|
| • Mean | 15–89 | 8–23 | 6–22 | 10–24 |
| • 95th percentile | 38–112 | 21–26 | 20–99 | 24–83 |
bw: body weight.
Main food categories contributing to exposure to phosphates (E 338–341, E 343, E 450–452)
The main food categories contributing to the total exposure to phosphates (E 338–341, E 343, E 450–452) as food additives presented below are extracted from the results expressed in mg P2O5/kg bw per day (Appendix L).
Main food categories contributing to exposure to phosphates (E 338–341, E 343, E 450–452) using the regulatory maximum level exposure assessment scenario
In the regulatory maximum level exposure assessment scenario, the main contributing food categories to the total mean exposure estimates for infants were infant formulae and processed cereal‐based foods and baby foods. For toddlers, fine bakery wares are the main contributing food category, while for children, fine bakery wares and Unflavoured pasteurised and sterilised (including UHT) milk are the main contributing food categories. For all other populations, the main contributing food categories are bread and rolls and fine bakery wares.
Main food categories contributing to exposure to phosphates (E 338–341, E 343, E 450–452) using the refined exposure assessment scenario
In the brand‐loyal refined estimated exposure scenario, the main contributing food categories to the total mean exposure estimates for infants were infant formulae and processed cereal‐based foods and baby foods. For the other populations – toddlers, children, adolescents, adults, the elderly – the main contributing food categories are bread and rolls and fine bakery wares. Meat products are the third contributing food categories for adults and the elderly.
In the non‐brand‐loyal refined estimated exposure scenario, the main contributing food categories to the total mean exposure estimates for infants were infant formulae and processed cereal‐based foods and baby foods. As for the brand‐loyal scenario, for the other populations – toddlers, children, adolescents, adults, the elderly – the main contributing food categories are bread and rolls and fine bakery wares. Added to these, processed cheese is also an important food contributing category for toddlers; and for children, adults and the elderly, meat products and sugars and syrups (as defined by Directive 2001/111/EC) are also important food contributing categories.
Dietary exposure to phosphates (E 338–341, E 343, E 450–452) considering the proposed extension of use
Tables 8a,b summarises the estimated exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives in six population groups (Table 4) taken into account the proposed extension of use on the FC 05.2 ‘Other confectionary including breath refreshing microsweets’ according to the different exposure scenarios. Results are presented in mg phosphorus (P)/person and per day and mg P/kg bw per day. Results in mg P2O5/person and per day and mg P2O5/kg bw per day are available in the appendixes to the opinion (Appendix M.1). Detailed results per population group and survey are also presented in Appendix M.2.
Table 8a.
Summary of dietary exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives in the regulatory maximum level exposure assessment scenario and in the refined exposure assessment scenarios, in six population groups (minimum–maximum across the dietary surveys in mg P/person per day) considering the proposed extension of use
| Infants (12 weeks–11 months) | Toddlers (12–35 months) | Children (3–9 years) | Adolescents (10–17 years) | Adults (18–64 years) | The elderly (≥ 65 years) | |
|---|---|---|---|---|---|---|
| Regulatory maximum level exposure assessment scenario considering the extension of use in FC 05.2 only | ||||||
| • Mean | 198–998 | 446–1,555 | 725–1,751 | 857–1,945 | 850–1,867 | 890–1,848 |
| • 95th percentile | 419–1,714 | 754–2,052 | 1,070–2,959 | 1,461–3,462 | 1,530–3,638 | 1,510–3,551 |
| Refined estimated exposure assessment scenario considering extension of use in FC 05.2 | ||||||
| Brand‐loyal scenario | ||||||
| • Mean | 96–309 | 101–372 | 108–620 | 130–733 | 319–722 | 337–747 |
| • 95th percentile | 222–570 | 203–745 | 215–1,291 | 287–1,603 | 658–1,600 | 683–1,559 |
| Non‐brand‐loyal scenario | ||||||
| • Mean | 81–141 | 78–152 | 69–237 | 74–298 | 126–278 | 121–241 |
| • 95th percentile | 191–253 | 153–266 | 135–613 | 155–749 | 253–636 | 212–480 |
Table 8b.
Summary of dietary exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives in the regulatory maximum level exposure assessment scenario and in the refined exposure assessment scenarios, in six population groups (minimum–maximum across the dietary surveys in mg P/kg bw per day) considering the proposed extension of use
| Infants (12 weeks–11 months) | Toddlers (12–35 months) | Children (3–9 years) | Adolescents (10–17 years) | Adults (18–64 years) | The elderly (≥ 65 years) | |
|---|---|---|---|---|---|---|
| Regulatory maximum level exposure assessment scenario considering the extension of use in FC 05.2 only | ||||||
| • Mean | 25–113 | 45–113 | 39–82 | 16–40 | 12–27 | 12–24 |
| • 95th percentile | 53–196 | 73–145 | 61–148 | 29–84 | 22–58 | 21–48 |
| Refined estimated exposure assessment scenario considering extension of use in FC 05.2 | ||||||
| Brand‐loyal scenario | ||||||
| • Mean | 12.0–35.0 | 10.1–27.2 | 5.9–25.6 | 2.4–16.6 | 4.4–10.6 | 4.7–9.9 |
| • 95th percentile | 27.4–65.7 | 20.6–53.6 | 11.4–55.9 | 5.1–37.0 | 9.1–25.2 | 9.4–20.2 |
| Non‐brand‐loyal scenario | ||||||
| • Mean | 10.2–15.8 | 5.5–11.1 | 3.7–9.9 | 1.4–6.8 | 1.8–3.7 | 1.7–3.2 |
| • 95th percentile | 21.5–38.9 | 12.6–21.2 | 7.3–26.5 | 3.0–17.1 | 3.6–8.2 | 3.1–7.1 |
bw: body weight.
While for the current authorisation, confectionery with added sugar were included, the proposed extension of use was considered by including the FC 05.2 confectionery without added sugar. The latter category represents a small consumption level. Added to the low use level for the food category 05.2 of confectionary and the high number of authorised uses taken into account in the assessment, it should explain the fact that no difference is noticed in the exposure estimates with the proposed extension of use.
Uncertainty analysis
Uncertainties in the exposure assessment of phosphates (E 338–341, E 343, E 450–452) have been discussed above. In accordance with the guidance provided in the EFSA opinion related to uncertainties in dietary exposure assessment (EFSA, 2007), the following sources of uncertainties have been considered and summarised in Table 9.
Table 9.
Qualitative evaluation of influence of uncertainties on the dietary exposure estimate
| Sources of uncertainties | Directiona |
|---|---|
| Consumption data: different methodologies/representativeness/underreporting/misreporting / no portion size standard | +/− |
| Methodology used to estimate high percentiles (95th) long‐term (chronic) exposure based on data from food consumption surveys covering only a few days | + |
| Correspondence of reported use levels to the food items in the EFSA Comprehensive Food Consumption Database: uncertainties to which types of food the levels refer to | +/− |
| Uncertainty in possible national differences in use levels of authorised uses | +/− |
Reported use levels:
|
++ |
| The 57 authorised uses which were taken into account in the refined exposure assessment scenarios out of all authorised uses (N = 108), corresponded to 30% to 93% of the amount (g of foods by body weight) of food consumption documented in the EFSA Consumption Database | − |
| Foods selected for the exposure assessment: exclusion of authorised uses due to missing FoodEx linkage (n = 15/total number of authorised uses) | − |
| Foods selected for the exposure assessment: inclusion of authorised uses without considering the restriction/exception (n = 7/total number of authorised uses) | + |
| Foods included in the exposure assessment: no data for certain authorised uses which were therefore not considered in the refined exposure estimates (n = 11/total number of authorised uses) | − |
| Foods which may contain the food additive according to Annex III to Regulation (EC) No 1333/2008 not taken into account | − |
Regulatory maximum level exposure assessment scenario:
|
+ |
Refined exposure assessment scenarios:
|
+/− |
+, uncertainty with potential to cause overestimation of exposure; −, uncertainty with potential to cause underestimation of exposure.
Phosphates (E 338–341, E 343, E 450–452) are authorised for 108 uses. The Panel calculated that out of the foods authorised to contain phosphates (E 338–341, E 343, E 450–452) according to Annex II to Regulation (EC) No 1333/2008, 30% (for children) to 93% (for infants) of the amount of food consumed (by weight) per population group was reported to potentially contain phosphates (E 338–341, E 343, E 450–452) as a food additive.
Data were received on most of the food categories in which the food additives are authorised to be added (no data for unprocessed fish, molluscs and crustaceans, alcoholic beverages, breakfast cereals, butter, salts).
The Panel noted that information from the Mintel GNPD (Appendix H) indicated that phosphates (E 338–341, E 343, E 450–452) were labelled on 134 food subcategories, categorised according to the Mintel GNPD nomenclature. Most of these food subcategories were included in the current exposure assessment, as only approximately 1.5% of the foods (from 10 different food subcategories) labelled with phosphates from Mintel were not taken into account in the assessment.
The percentage of foods per Mintel subcategory labelled to contain phosphates (E 338–341, E 343, E 450–452) was on average of 9.6%. For eight subcategories, the percentage of foods labelled with phosphates (E 338–341, E 343, E 450–452) was above 45%. In the assessment, it was assumed that 100% of the foods belonging to an authorised food category contained the additive. The Panel noted that the information from the Mintel GNPD indicated that phosphates (E 338–341, E 343, E 450–452) are used in a large range of foods. Therefore, an exposure assessment based on the premise that all of the foods contain phosphates would probably lead to an overestimation of the dietary exposure which represents the largest uncertainty.
The Panel noted that foods which may contain phosphates (E 338–341, E 343, E 450–452) due to carry‐over (Annex III, Parts 1, 2, 3, 4, 5) were not considered in the current exposure assessment.
Overall, the Panel considered that the uncertainties identified would, in general, result in an overestimation of the exposure to phosphates (E 338–341, E 343, E 450–452) from their use as food additives according to Annex II in European countries considered in the EFSA European database for the regulatory maximum level exposure scenario. For the refined estimated exposure scenario, uncertainties would also lead to an overestimation of exposure to phosphates (E 338–341, E 343, E 450–452).
3.4.2. Exposure to total phosphorus via the diet
Exposure to total phosphorus from the diet was estimated using analytical data. This exposure estimate is calculated using the mean/median, whichever is higher, of analytical levels for all food categories. This scenario was chosen to be representative of wider range of samples taken from the market as well as the long‐term intake. This calculation covers all dietary intake of phosphorus including that emanating from other food additives containing phosphorus, as well as the use of phosphates (E 338–341, E 343, E 450–452) according to Annex III of Regulation No 1333/2008 (carry‐over).
Analytical levels provided by the Member States reflect the levels of phosphorus in foods whatever the origin (from natural and other dietary sources). Therefore, the exposure estimated with analytical data should reflect more closely what is ingested through the diet including phosphorus‐containing food additives added for other technological reasons. While these limited analytical data covered most of food categories from the diet, they were provided only by 10 Member States. Nonetheless the Panel assumed that these estimates were indicative of dietary exposure to phosphorus in European countries considered in the EFSA European database via the whole diet (from natural and other dietary sources).
For some food categories for which no analytical data were available, reported use levels were used in order to cover in a more exhaustive way foods in which phosphates can be present. This is the case for chewing gum (FC 05.3) and sugars and syrups as defined by Directive 2001/11/EC (FC 11.1).
Tables 10a,b summarise the estimated exposure to phosphates from the diet in seven population groups (Table 4). Results are presented in mg phosphorus (P)/person and per day and in mg P/kg bw per day. Detailed results per population group and survey (in mg P/kg bw per day and mg P/person per day) are also presented in Appendixes N.1 and N.2.
Table 10a.
Summary of dietary exposure to phosphorus from the diet,* in seven population groups (minimum–maximum across the dietary surveys in mg P/person per day)
| Infants (< 16 weeks) | Infants (12 weeks–11 months) | Toddlers (12–35 months) | Children (3–9 years) | Adolescents (10–17 years) | Adults (18–64 years) | The elderly (≥ 65 years) | |
|---|---|---|---|---|---|---|---|
| • Mean | 254 | 251–577 | 693–1,032 | 798–1,363 | 986–1,573 | 1,204–1,625 | 1,185–1,561 |
| • 95th percentile | 331 | 451–964 | 1,069–1,388 | 1,169–2,008 | 1,505–2,427 | 1,829–2,728 | 1,743–2,619 |
Using analytical data except for chewing‐gum (FC 05.3) and sugars and syrups (FC 11.1).
Table 10b.
Summary of dietary exposure to phosphorus from the diet,* in seven population groups (minimum–maximum across the dietary surveys in mg P/kg bw per day)
| Infants (< 16 weeks) | Infants (12 weeks–11 months) | Toddlers (12–35 months) | Children (3–9 years) | Adolescents (10–17 years) | Adults (18–64 years) | The elderly (≥ 65 years) | |
|---|---|---|---|---|---|---|---|
| • Mean | 64 | 32–85 | 55–74 | 33–62 | 18–33 | 16–22 | 16–20 |
| • 95th percentile | 83 | 56–106 | 85–123 | 55–92 | 31–56 | 25–36 | 24–35 |
bw: body weight.
Using analytical data except for chewing‐gum (FC 05.3) and sugars and syrups (FC 11.1).
In the estimated exposure scenario based on analytical data, the mean exposure to phosphates ranged from 16 mg P/kg bw per day for adults and the elderly to 85 mg P/kg bw per day for infants, and the high exposure (95th percentile) from 24 mg P/kg bw per day for the elderly to 123 mg P/kg bw per day for toddlers (Table 10b). For infants below 16 weeks of age exposure was estimated to be 64 mg P/kg bw per day at the mean and 83 mg P/kg bw per day at the high level (95th percentile).
Main food categories contributing to exposure to phosphates using analytical data
In this scenario, the main contributing food categories to the total mean exposure estimates for infants were unflavoured pasteurised and sterilised (including UHT) milk, infant and follow‐on formulae. For the other populations – toddlers, children, adolescents, adults, the elderly – the main contributing food categories are unflavoured pasteurised and sterilised (including UHT) milk, bread and rolls and meat products (Appendix O).
Specific scenarios
The specific scenarios on food supplements and FSMP were also performed. As no analytical data for food supplements and foods for special medical purposes for infants and toddlers (FCs 13.1.5.1 and 13.1.5.2) were available, maximum levels for these food categories were taken from the reported use levels from industry for estimating exposure of FSMP consumers only and food supplements consumers only.
For the FSMP food categories (i.e. FCs 13.1.5.1 and 13.1.5.2), reported use levels were submitted by industry when phosphates are added as food additives but also as nutrients. For the FSMP scenario performed with the reported use levels only (Section 3.4.1), only the levels provided for the need of phosphates as food additives were used. In the current FSMP scenario, also the use levels reported for the addition of phosphates as nutrients were considered.
Estimates for the infants and toddlers consumers only of foods for special medical purposes ranged at the mean from 35 mg P/kg bw per day for infants (12 weeks–11 months) to 154 mg P/kg bw per day for infants below 16 weeks (Table 11). At the high level, exposure ranged from 65 mg P/kg bw per day for toddlers to 200 mg P/kg bw per day for the infants below 16 weeks. As mentioned above, this scenario is related to the infants and toddlers consumers only of FSMP, eating foods at mean concentration of phosphorus except for the FCs 13.1.5.1 and 13.1.5.2 for which the maximum reported use levels were used instead.
Table 11.
Summary of dietary exposure to phosphorus for FSMP consumers only from the diet,* in infants and toddlers (minimum–maximum across the dietary surveys in mg P/kg bw per day)
| Infants (< 16 weeks) | Infants (12 weeks–11 months) | Toddlers (12–35 months) | |
|---|---|---|---|
| • Mean | 154 | 35–75 | 55–78 |
| • 95th percentile | 200 | 65–133 | 81–112 |
bw: body weight.
Phosphorus is also present in other sources (e.g. milk).
Table 12.
Summary of dietary exposure to phosphorus for food supplements consumers only from the diet, in children, adolescents, adults and the elderly (minimum–maximum across the dietary surveys in mg P/kg bw per day)
| Children (3–9 years) | Adolescents (10–17 years) | Adults (18–64 years) | The elderly (≥ 65 years) | |
|---|---|---|---|---|
| • Mean | 53–138 | 31–48 | 25–40 | 25–42 |
| • 95th percentile | 84–153 | 58–62 | 44–121 | 41–97 |
bw: body weight.
This scenario focused on the specific population of food supplement consumers only. Estimates ranged from 1,280 mg P/person per day for children to 2,839 mg P/person per day for elderly, at the mean; and from 1,958 mg P/person per day for the children to 8,923 mg P/person per day for adults, at the high level. The mean concentration of phosphorus from the diet was considered background. Dietary exposure is estimated from food supplements intake, assuming all food supplements contain phosphates, at the maximum reported use level combined with the background. Uncertainty linked to the lack of knowledge on the form of calcium phosphates as mentioned in the food supplements' consumers only scenario (page 35) also apply to the above estimates. For these reasons, this scenario reflects a conservative exposure estimate to phosphorus.
Uncertainty analysis for the general analytical data
Exposure intakes of phosphorus through the whole diet are subject to the same uncertainties concerning the food consumption data than the exposure estimates of phosphates (E 338–341, E 343, E 450–452) as food additives (as mentioned in Table 9). Uncertainties to which types of food the analytical levels refer to is another uncertainty which applies to intakes of phosphorus through the whole diet. Apart for the methodology used to estimate high percentiles (95th) long‐term (chronic) exposure based on data from food consumption surveys covering only a few days which should result in an overestimation of the exposure intakes, the other uncertainties linked to consumption data could results in both under or overestimation of the true exposure to phosphates though the whole diet.
Finally, some food categories were not taken into account as no data were available (processed eggs, salts and some alcoholic beverages). This would lead to an underestimate of the total intake; however, considering the food categories missing, the underestimation in that case of the general population should be low.
3.4.3. Exposure via other sources
Phosphates are also used in cosmetic products and in medications as an active pharmaceutical ingredient, or as a counter‐ion for drugs or mostly as an excipient. Quantification of exposure via all these sources is not precisely known and could therefore not be taken into account in this opinion.
3.5. Biological and toxicological data
Phosphorus only occurs in the body as its pentavalent form bound to oxygen as phosphate. As such it occurs in organic and inorganic forms. Phosphate is essential for all living organisms. The intracellular activity of phosphate ions participates in acid base balance. Phosphate is intrinsically involved with regulation of metabolic processes via phosphorylation of proteins and supplying energy by means of nucleotides triphosphates (e.g. ATP, GTP, CTP and UTP) which serve as energy depots supporting protein and polysaccharide synthesis, ion pumps, cell signalling, muscle contractility. Phosphate is also component of second messengers such as cyclic adenosine monophosphate (cAMP), inositol polyphosphates (IP3) and cyclic guanine monophosphate (cGMP). Phosphate is fundamental for the structure and function of DNA and ribonucleic acid (RNA). Phospholipids are part of cell membrane structure where they affect the membrane fluidity and function. In erythrocytes, 2–3 diphosphoglycerate modulates the release of oxygen from haemoglobin in tissues (Frausto da Silva and Williams, 2001).
The whole human body P content is 500–700 g; it varies with skeletal mass which is higher in men. Fifteen percent of the phosphate in the body is involved in the above‐mentioned metabolic function and control, whereas the largest pool of phosphates (approximately 85%) is found together with calcium in the skeleton.
Free phosphate is found in both intracellular and extracellular fluid (ECF). Approximately 85% of P in the ECF is present as HPO4 2− and H2PO4 − (4:1 ratio). These anions are important for acid‐base regulation and their relative amounts and association with cations are pH dependent. The ratio between the two ionised phosphate forms is integral to the control of P and of Ca absorption, distribution, excretion and bone deposition. In some instances, inappropriate mineralisation can occur in soft tissues such as the kidneys and cardiovascular structures. This pathological process is called biomineralisation.
Biomineralisation is sensitive to the saturation of ECF (plasma and interstitial fluid) with hydroxyapatite (Ca5(PO4)3OH) and its precipitation at foci for crystallisation, however the process and its regulation are not fully understood (Tavafoghi and Cerruti, 2016). Hydroxyapatite is the predominant salt in the ECF at physiological pH and pCO2 and the activity product (Ca X P) of ionised calcium (1.1–1.3 mmol/L) and P (0.9–1.4 mmol/L) approximates to 1.3 mmol2/L2. It has been suggested that when this value exceeds by approximately twofold the solubility constant of hydroxyapatite, the salt precipitates at crystallisation foci. This may occur when serum phosphate exceeds 2.4–2.5 mmol/L. The higher serum levels of P and Ca in early life compared with those of adulthood are seen to be consistent with the concept that they support physiological skeletal mineralisation (Heaney, 2012). It has been proposed that carbonated hydroxyapatite is the form involved in mineralisation and that charged amino acids in non‐collagen proteins, via binding of Ca2− and PO4 3−, and possibly localised supersaturation of hydroxyapatite, induce nucleation and crystal precipitation, leading to tissue mineralisation (Tavafoghi and Cerruti, 2016). High phosphorus intake (3,000 mg phosphorus per person per day on top of the diet) may disrupt the hormonal regulation of phosphorus, calcium and vitamin D (Calvo and Uribarri, 2013). This imbalance may contribute to bone loss and consequently the increased risk of osteoporosis and bone fractures (Calvo and Lamberg‐Allardt, 2017). Further discussion on interaction between phosphorus and other minerals can be found in EFSA 2013.
Phosphates which occur naturally in food are absorbed throughout the duodenum and jejunum, but principally in the duodenum and jejunum with an efficiency of between 55 and 90% of the amount and source of dietary phosphate and vitamin D status (Sabbagh et al., 2011). In the intestinal lumen, inorganic phosphate is released from the food by phosphatases at a rate that depends on the chemical complexity of the organic phosphates. Phosphate from phytates (myoinositol esaphosphate) is poorly released. The formation of complexes between dietary phytates, calcium, magnesium and some amino acids mutually reduce their availability for intestinal uptake (Cheryan, 1980). The bioavailability of phosphate from phytates is poor (20–30%) due to the lack of the enzyme phytase in humans. Generally, the availability for net phosphate absorption might be limited by the calcium content of the diet (Heaney and Nordin, 2002; Sabbagh et al., 2011; Heaney, 2012; O'Brien et al., 2014; Scanni et al., 2014). Other factors including epidermal growth factor, glucocorticoids, oestrogens, acid base balance and phosphatonins potentially influence the absorption of phosphates either directly or indirectly (Penido and Alon, 2012).
It has been proposed that since dietary phosphates arising from food additives are in an inorganic forms they do not require release by luminal phosphatases and could be taken up and absorbed more efficiently than organic phosphate from animal or plant foods (Kalantar‐Zadeh et al., 2010). The major determinant of systemic phosphate homeostasis is renal handling of phosphate, namely the amount of phosphate ultrafiltered by the glomerulus and the amount that is reabsorbed at tubular level. Urinary loss of phosphate is the major route of phosphate excretion and under normal physiologic conditions the renal phosphate transporter threshold is the main determinant of phosphate plasma levels.
Factors influencing renal loss of phosphate are parathyroid hormone (PTH), Klotho and fibroblast growth factor‐23 (FGF‐23) while calcitriol is the major factor regulating intestinal phosphate absorption.
Under normal conditions, serum phosphate levels show the highest values in the first months of age (2.38 ± 0.54 mmol/L corresponding to 7.4 ± 1.7 mg/dL at 1 month, 2.21 ± 0.43 mmol/L corresponding to 6.9 ± 1.3 mg/dL at 3 month of age) while it significantly decreased at 6 month (1.80 ± 0.41 mmol/L corresponding to 5.6 ± 1.3 mg/dL) (Bistarakis, 1986). Subsequently, serum levels progressively decrease during childhood to achieve the average adult reference values of approximately 1.0 mmol/L (corresponding to 3.2 mg/dL) by the age of 16 years (Alon, 1994). This pattern has been attributed to higher renal tubular phosphate reabsorption in infants and children occurring to maintain the rapid body growth and calcification of the skeleton.
3.5.1. Absorption, distribution, metabolism and excretion
Human studies
Absorption
Inorganic phosphate used as food additives assessed in this opinion is assumed to dissociate in the gastrointestinal lumen. The released phosphate is well absorbed mainly as free orthophosphate in the small intestine with amounts ranging between 55 and 90% of the dose (Sabbagh et al., 2011; Heaney, 2012; O'Brien et al., 2014; Scanni et al., 2014). Several factors regulate the phosphate absorption among them calcitriol, PTH epidermal growth factor, glucocorticoids, oestrogens, metabolic acidosis, phosphatonins and secreted frizzled‐related protein 4 (sFRP‐4) (Penido and Alon, 2012). Intestinal phosphate absorption occurs by passive diffusion (McHardy and Parsons, 1956) and sodium‐dependent active transport (Walton and Gray, 1979; Eto et al., 2006). There are different sodium transporters in the body [NaPi‐IIa (SLC34A1), NaPi‐IIb (SLC34A2 or NPT2b) and NaPi‐IIc (SLC34A3)]. NaPi‐IIb is predominant in the intestine (Penido and Alon, 2012; Biber et al., 2013) and its activity is modulated by active vitamin D and by a low phosphorus diet (Segawa et al., 2005; Forster et al., 2011; Sabbagh et al., 2011).
Phosphorus availability for intestinal absorption may be limited by the calcium content of the diet (Sabbagh et al., 2011; Heaney, 2012; O'Brien et al., 2014; Scanni et al., 2014).
Atkinson et al. (1995) reviewed data on the P content of human breast milk and reported this to be between 160 mg/L at 14 days, 140 mg/L at 30 and 90 days and 120 mg/L at 180 days post‐partum. Neonatal absorption of phosphorus is between 86% and 97% irrespective of calcium or phosphorus intakes (Loughead and Tsang, 1998; Kovacs, 2015).
Distribution
Phosphorus is distributed throughout the body with the largest pool (approximately 85% of body content) together with calcium in the skeleton as hydroxyapatite.
Excretion
About 200 mmol of P is filtered daily by the glomerulus of which 80% or more is reabsorbed in proximal tubules. The tubular uptake of P is mediated via sodium phosphate co‐transporters, in particular NaPi‐IIa, characterised by a threshold known as the tubular maximum for P (TmP) (Tenenhouse, 2005). PTH and FGF‐23 with Klotho influence the re‐absorption rate of the ultrafiltrated P. In steady‐state conditions, the amount of phosphorus excreted in the urine equals or is close to the amount of dietary phosphorus absorbed by gut (Berndt and Kumar, 2009; Scanni et al., 2014). However, in the real practice, a single urinary P measurement is not believed as a validated marker of dietary exposures in free living populations (Cupisti and Gallieni, 2018; Stremke et al., 2018). Osgood and Ivey reported that the concentration of P32 in plasma after intravenous injection had a mean half‐life of 8.5 days in patients with leukaemia (Osgood et al., 1950). Faecal losses of P result from non‐absorbed dietary phosphorus, mostly represented by phytate (Greger et al., 1978; Anderson, 2005; Delgado‐Andrade et al., 2011), and from digestive secretions (0.9–4 mg/kg bw per day) (O'Brien et al., 2014).
In summary, the inorganic phosphorus deriving from food additives is mainly absorbed as free orthophosphate. The amount of orthophosphate absorbed is about 80–90%. Excretion is via the kidney through glomerular filtration and tubular handling. Data are available on the kinetics of disodium diphosphate, trisodium diphosphate, tetrasodium diphosphate and tetrapotassium diphosphate but not on dicalcium diphosphate and calcium dihydrogen diphosphate.
Animal studies
The absorption of P32‐radiolabelled tetrasodium diphosphate, sodium tripolyphosphate, sodium polyphosphate and sodium hexametaphosphate was investigated in rats by measuring the blood, liver, stomach, brain, intestine and bones concentration of P32 by radiochromatography (Schreier and Noller, 1955). The lower molar mass compounds were absorbed more rapidly than those with a higher molar mass. At 18 h, more than 60% of the sodium hexametaphosphate was still found in the intestinal tract. Radioactive orthophosphate and a small amount of diphosphate were present in the blood. The authors stated that high polymeric phosphates do not penetrate the intestinal wall readily; however, the diphosphate is hydrolysed into orthophosphate at neutral pH.
Tetrasodium diphosphate absorption was measured in the rats after 3 weeks continuous treatment via diet. Food consumption was determined and the faeces and urine collected in the 5% tetrasodium diphosphate group over a 6‐day period from five male animals (Datta et al., 1962). In another study part, faeces and urine were collected over a 3‐day period from five male animals having treated for 8 weeks with 5% tetrasodium diphosphate and from five male animals having treated for 8 weeks with 5% sodium orthophosphate in the diet. Food, urine and faeces were analysed for calcium and diphosphate. Diphosphate was not detected in rat faeces or urine; however, orthophosphate was found in the urine so that it can be concluded that diphosphate was almost completely hydrolysed to orthophosphate in the rat gut and the resulting orthophosphate was well absorbed (approximately 85%) from the gastrointestinal tract.
There are no data on the toxicokinetics (TK) of dicalcium diphosphate and calcium dihydrogen diphosphate.
3.5.2. Measurements of intake and exposure in humans
Markers of exposure in humans need to be evaluated in the context of the risk assessment of phosphates. There are several indicators used to characterise the exposure in epidemiological studies all of which have considerable limitations.
Dietary intake
Different dietary assessment methods have been used in the epidemiological studies to measure phosphorus intake from diet. Three studies (Alonso et al., 2010; Yamamoto et al., 2013; Kwak et al., 2014) have used food frequency questionnaires (FFQ) to measure the phosphorous intake while one study also used 3 days food record (Itkonen et al., 2013).
All the dietary assessment methods rely on food composition tables to give the amount of phosphorus in each food item. The food composition tables give most often one value for each food item, and thereby do not distinguish between naturally occurring phosphorus and that from food additives. There can be large variation in the phosphorus level in the same type of food (Benini et al., 2011; Trautvetter et al., 2018). Total phosphorus concentrations have been shown to be up to twofold higher in food items with phosphorus additives, compared with additive free products (Karalis and Murphy‐Gutekunst, 2006; Benini et al., 2011).
Dietary records and 24‐h dietary recalls are open‐ended dietary assessment methods and single 24‐h dietary recalls are not sufficient to estimate chronic phosphate intake reliably (Cupisti and Gallieni, 2018; Stremke et al., 2018). More than one 24‐h dietary recall is needed to assess exposure (EFSA, 2014).
FFQ are closed methods. To be able to capture phosphorus rich foods, the questionnaires have to be design considering this specific goal. Only one of the studies using FFQ gives an energy‐adjusted correlation coefficient of 0.51 for phosphorus compared with several 24‐h recalls (Kwak et al., 2014). Both methods used the same food composition table.
Serum/plasma phosphorus concentration
The reference range for serum phosphorus is 0.8–1.5 mmol/L (2.7–4.5 mg/dL) in adults and 1.3–2.3 mmol/L (4.0–7.0 mg/dL) in children (more details in introduction to Section 3.5).
In the NHANES III study (1988–1994) dietary intake of phosphorus, encompassing 15,513 participants, was assessed by 24‐h dietary recall and in addition a questionnaire for 1‐month food frequency was used (NHANES III, 1988–1994). The data were used by de Boer et al. (2009) to investigate the relationship between dietary phosphorus intake and single measurement of serum phosphorus concentration. A statistically significant relationship was found between the two parameters, with each 500‐mg/day increment in phosphorus intake being associated with an increase of 0.03 mg/dL in serum phosphorus (p < 0.001), after adjustment for age, sex, race, time of measurement and fasting status. A further study with fewer participants (N = 3,421) did not find any relationship between phosphorus intake and serum phosphorus concentration (Mataix et al., 2006). Serial measurements throughout the day and subsequent averaging the values would result in a better estimate of phosphorus exposure (Portale et al., 1987; Calvo and Heat, 1988; Kemi et al., 2006).
Moore et al. (2015) conducted a cross‐sectional study using data from the NHANES to investigate the association between food sources rich in organic phosphorus and foods rich in inorganic phosphate from additives and serum phosphorus levels. A total of 7,895 subjects, aged 20–85 years (mean 46.7, SD = 0.5 years), not pregnant and with no missing data on laboratory values for serum phosphorus, urine creatinine and albuminuria as well as dietary data were included in the study. Demographic, clinical and dietary data (24‐h food recall) was obtained for all participants. Population mean age and the mean serum phosphorus was 46.7 years (SD = 0.5) and 3.81 mg /dL (SD = 0.01), respectively. Phosphorus content of foods was categorised as organic and inorganic. High serum phosphorus was associated with high consumption of dairy foods categorised as containing inorganic phosphates (p = 0.0097) after controlling for estimated glomerular filtration rate (eGFR), body mass index (BMI; in kg/m2) and albumin‐to‐creatinine ratio. High serum phosphate was also observed in high consumers of dairy food categorised as not containing inorganic phosphate.
Trautvetter et al. (2016) investigated the association between serum phosphate and dietary phosphorous and calcium in a double‐blind, placebo‐controlled study of 32 women and 30 men. Participants received dietary phosphorous (1,000 mg/day) with different amounts calcium (0, 500, 1,000 mg/day) for 8 weeks. The study did not show any association between dietary phosphate intake and fasting serum phosphorous. A high intake of phosphorous without adequate calcium did affect plasma FGF‐23, although with a large interindividual variability which makes it unsuitable as a surrogate marker of intake.
Karp et al. (2013) investigated the effect of dietary phosphorous on calcium phosphorous metabolism in an acute (24‐h), placebo‐controlled cross‐over study on 14 women (mean age 23 years). Participants received 1,500 mg/day phosphorous as monophosphate or polyphosphate. The results showed an acute increase in serum and urinary phosphorous following the ingestion of the phosphorous supplement, although serum phosphorous concentration returned to baseline concentrations after 24 h.
Kemi et al. (2006) investigated the acute effect of high dietary phosphorous and bone metabolism in 14 women (mean age 24 years). In a randomised, placebo‐controlled cross‐over study, participants received either 0, 250, 750 or 1,500 mg phosphorous, and concentrations of serum phosphate, ionised calcium and PTH were measured for 24 h. The results suggest a dose–response relationship between phosphorous intake and serum phosphorous concentration and PTH, and an inverse relationship with ionised calcium concentration. These results confirm findings from other studies that serum phosphorous concentration can be affected in the short‐term by dietary intake, but do not provide information on the association with chronic or habitual intake.
At dietary phosphate intake below 20 mmol/day (619 mg/day), there is a correlation between dietary intakes and serum or plasma phosphate concentrations. However, at intakes above this, corresponding to customary intakes, the relationship is much weaker and is not indicative of intakes (Heaney, 1997).
All the studies on the association between measurements of phosphate intake by dietary assessment and serum P showed only a weak correlation in subjects with normal renal functions.
The poor relationship between phosphate intake and serum/plasma level might be partially explained by the different bioavailability of phosphate from different sources. For example, the poor release of phosphate from phytates, as well as the interaction between phytates and inorganic phosphorous (see Section 3.5.1), reduce the bioavailability of dietary phosphorous from plant foods (Schlemmer et al., 2009). Vegetarian diets with the same phosphorous content as animal‐based diets therefore appear to result in a lower absorption of phosphorous and subsequently a lower serum P and urinary excretion (Moe et al., 2011). The relationship between dietary and serum phosphorous is therefore confounded not only by homoeostatic regulation of serum phosphorous, but also the dietary source and form of phosphorous.
Another factor could be underestimation of phosphate content in food due to insufficient information in food composition tables and limitations of the methods of some dietary intake measurements (EFSA, 2014).
The EFSA NDA Panel considered that single serum phosphorus concentration measurements cannot serve as surrogate for phosphorus intake (EFSA NDA Panel, 2015). The FAF Panel agreed with this position.
Urinary phosphorus excretion
The main route of phosphorus elimination is excretion in the urine the mechanisms being glomerular filtration and tubular reabsorption in the kidney. Hence, urinary phosphorus excretion is a surrogate for phosphorus intake. A 24‐h collection of the urine will give a more precise estimate than measuring the concentration in a spot urine even if normalised by urine creatinine.
Urinary excretion of phosphorous has been considered to be a surrogate marker of phosphorous intake (Morimoto et al., 2014), although this is based on the assumption of a uniform and constant absorption of dietary phosphorous and its complete renal excretion (Hruska et al., 2008). However, Brixen et al. (1992) has shown that urinary phosphorous is affected by short‐term changes in dietary phosphorous intake, and both Morimoto et al. (2014) and Trautvetter et al. (2018) show only weak associations between dietary phosphorous and urinary phosphorous. The study reviewed here did not show an association between urinary phosphorous excretion and increased risk of cardiovascular diseases (CVDs), but this might only reflect short‐term phosphorous intake and is therefore not suitable to assess the risks associated with habitual phosphorous intake.
According to Sun et al. (2017) who evaluated the variability of a variety of urinary makers in three major surveys, it is necessary to have three times within 1 year 24‐h collection of urine to provide a reasonably strong correlation with the true long‐term average urinary excretion of phosphate.
The Panel considered that single spot urinary phosphorus excretion, and single 24‐h urinary excretion are not valid markers for long‐term dietary exposure which is in agreement with the conclusion from the NDA Panel in 2015.
FGF‐23 – Marker of exposure and effect
FGF‐23 is a hormone produced by osteocytes which regulates phosphate excretion by influencing the phosphate reabsorption in the kidney mediated via alpha‐Klotho as a cofactor.
Some publications showed that dietary intake of phosphorus was related to the FGF‐23 plasma concentration (Antoniucci et al., 2006). However, others did not find this association (Larsson et al., 2003).
FGF‐23 is elevated in relation to the decline of kidney function in patients with chronic kidney disease (CKD; Larsson et al., 2003; Faul et al., 2011). Elevated FGF‐23 was linked predominantly to left ventricular dysfunction and consequently to related morbidity and mortality; it likely occurs nearly exclusively in subjects with CKD in whom the FGF‐23 system is strongly stimulated (reviewed in Stöhr et al., 2018). Only few studies investigated the association in subjects without renal disease and mostly in elderly patient which raises the question of the generalisability of the findings (Arnlöv et al., 2013; Brandenburg et al., 2014).
Whereas the group of Faul et al. (2011) interpreted their results obtained in patients with CKD as demonstrating that elevated FGF‐23 activity/levels caused left ventricular hypertrophy (Grabner et al., 2015; Leifheit‐Nestler et al., 2016) novel findings challenges this interpretation. Recent data allow the interpretation that FGF‐23 is locally produced and released by myocytes in the event of (acute) myocardial damage.
When considering whether FGF‐23 could be used as a marker to determine the safe level of phosphate intake it has to be considered that the role of FGF‐23 for negative influences on cardiac function is not yet established as in a recent review (Stöhr et al., 2018) the authors concluded: ‘Prior to any therapeutic intervention with the aim to minimize potentially negative FGF‐23 effects upon cardiac structure and function, research needs to focus on and clarify relevant unsolved issues. Just to name a few, the community needs to prove how cardiac disease induces (rather than follows) FGF‐23 secretion, to what degree cardiomyocytes may themselves produce FGF‐23 in health and disease, whether such locally produced FGF‐23 has a physiological role in (acute) myocardial damage; and whether or not (systemic) FGF‐23 excess itself directly drives the development of myocardial damage’.
Furthermore, a clear dose–response relationship between phosphate intake and plasma concentration of FGF‐23 has not been established. This does not allow to estimate the phosphate intake when FGF‐23 levels were measured in clinical studies with cardiac endpoints.
Hence, the Panel decided that FGF‐23 levels could not be used as an endpoint to assess the adverse health effects of phosphate.
3.5.3. Toxicology
There are numerous toxicology studies available with most of the phosphates used as food additives. However, the studies are generally quite old and not performed according to current guidelines. Furthermore, cations of the phosphates are constituents of human tissues that occur naturally in food stuffs, and intake of them does not cause adverse human health effects, providing that the intake isn't so high as to disturb the homeostatic mechanisms controlling the electrolyte balance of the body. Therefore, the toxicity of the cations is not discussed in this opinion.
Furthermore, in all animal studies, the phosphates were added in addition to any phosphate present in the diet. In order to calculate the doses administered over time (mg/kg bw per day) relevant conversion factors from the EFSA guidance on selected default values were used (EFSA, 2012).
The Panel recognise that where the purity details of the test material(s) used in the studies below are not stated, there will be an uncertainty associated with the true amount of phosphate used in test dosages. The exact amount of phosphate was unknown because in some toxicological studies it was not stated whether the test material used was in the anhydrous form or one of the several hydrated forms. The EU (and JECFA) additive specifications for phosphates (Appendix E) prescribe a range for the purity assay expressed as P2O5, which provides an indication of the purity limits. Moreover, the specifications for certain phosphates reveal several synonyms for the materials, which appear to be historically interchangeable through these and other studies. In the light of this, dosage levels have been recalculated on an anhydrous basis.
3.5.4. Acute toxicity
There are acute oral toxicity studies with all phosphates under evaluation. Available data are summarised below.
Phosphoric acid
Phosphoric acid was administered to Sprague–Dawley rats at doses between 2,510 and 6,310 mg/kg. The LD50 value was estimated to be more than 3,500 mg/kg (Randall and Robinson, 1990).
Magnesium phosphates
In an unpublished report from Food and Drug Research Laboratories (1973), cited in (JECFA, 1982b), a LD50 value of 4,600 mg/kg was reported when monocalcium phosphate was administered orally to mice and 2,170 mg/kg when administered to rats.
When tricalcium phosphate was tested for acute oral toxicity in female Wistar rats the LD50 value was estimated to be greater than 2,000 mg/kg bw (Harlan‐Laboratories‐Ltd, 2010a)
Sodium and potassium phosphates
A LD50 value of 3,700 mg/kg bw was reported when monosodium phosphate was administered orally to mice, and 4,100 mg/kg bw when administered orally to rats (unpublished report from Food and Drug Research Laboratories (1975), cited in (JECFA, 1982b).
A LD50 value for the guinea pig was reported to be 2,000 mg/kg bw when monosodium phosphate was administered orally (Eichler, 1950), cited in (JECFA, 1982b).
A LD50 value of 3,200 mg/kg bw was reported when monopotassium phosphate was administered orally to mice and 2,820 mg/kg bw when administered to rats (unpublished report from Food and Drug Research Laboratories (1975), cited in (JECFA, 1982b).
Diphosphates
In an acute oral toxicity study where disodium diphosphate was administered to fasted adult male Swiss Webster mice and adult male Sprague–Dawley rats LD50 values of 2,300 mg/kg bw in mice and 1,800 mg/kg were reported (Newell et al., 1974).
In another acute oral toxicity study, Sprague–Dawley rats were administered tetrasodium diphosphate at a dose of 2,000 mg/kg bw (Seo et al., 2011). No deaths or clinical signs of toxicity were observed up to 14 days after dosing. Thus, the LD50 for tetrasodium diphosphate was greater than 2,000 mg/kg bw in this study.
Triphosphates
The JECFA evaluation of 1982 reports the following oral LD50 values for sodium triphosphate; 2,380 mg/kg bw in mouse, 1,700 mg/kg bw in rat and 2,500 mg/kg bw in rabbit, referencing Food and Drug Research Lab (1973); however, the original report which was available for review does not include the information reported by JECFA (1982b). No further detail is available for review.
Sodium triphosphate is reported to have an oral LD50 value of 3,210 mg/kg in mouse (Zipf, 1957). The report is a summary, with no further detail available.
Polyphosphates
The JECFA monograph (unpublished report from Food and Drug Research Laboratories 1974 cited in JECFA, 1982) reported an acute oral LD50 value for sodium hexametaphosphate in mice of 3,700 mg/kg bw and in rat of 2,400 mg/kg bw.
An acute oral LD50 of 7,250 mg/kg bw in mice has been reported for sodium hexametaphosphate (Zipf, 1957).
According to the REACH registrant, in an unpublished acute oral toxicity study, sodium metaphosphate (OECD, 2001) and sodium hexametaphosphate were administered to female Wistar rats at dose of 2,000 mg/kg bw by oral gavage. There were no deaths and no adverse findings. The LD50 value was concluded to be greater than 2,000 mg/kg bw.
Overall the acute oral toxicity of all evaluated phosphates is very low with LD50 values generally exceeding 2,000 mg/kg bw.
3.5.5. Short‐term and subchronic toxicity
There are short‐term and subchronic toxicology studies with most of the phosphates under evaluation. Most of the studies are quite old and of variable quality and not performed according to current guidelines.
Calcium and magnesium phosphates
A study investigated nephrocalcinosis in weanling female Wistar rats fed diets varying in concentrations of Ca and P supplied as inorganic salts (Hitchman et al., 1979). Higher phosphate and calcium percentages were obtained by adding: calcium carbonate and calcium dihydrogen phosphate or a mixture of calcium dihydrogen phosphate and monosodium phosphate to the semisynthetic diet for periods of 4–6 weeks. Treated groups were compared with control rats fed laboratory chow for the same period of time. Nephrocalcinosis was produced by semisynthetic diets with inorganic phosphate concentrations as low as 0.5% (equivalent to 600 mg/kg bw per day) on a weight basis; in contrast, rats fed regular laboratory chow showed no evidence of nephrocalcinosis. The severity of the nephrocalcinosis was proportional to dietary phosphate concentrations from 0.5 to 1.0% but other dietary constituents also altered the severity of the lesion. With a lower dietary phosphate content of 0.5%, increasing dietary Ca from 0.5 to 1.0% resulted in a decrease in the severity of the renal calcification. Decreasing protein concentrations from 25 to 15% casein increased the severity of the renal lesions (p < 0.01). Other dietary factors also seemed to modify the phosphate‐induced nephrocalcinosis since no lesions occurred in rats on laboratory chow. The authors suggested that the availability of dietary phosphate may be a factor. The phosphate in the semisynthetic diets was totally inorganic while the natural foods of laboratory chow contain, at least in part, organic phosphate (Hitchman et al., 1979).
Sodium and potassium phosphate
Rat
Sprague–Dawley rats (weight: 60–150 g) were placed on a chow diet containing 10% disodium phosphate (equivalent to 12,000 mg/kg bw per day) for periods of 24–72 h (Craig, 1957). Some animals were killed at the end of the feeding period while other animals were placed on a control diet for 2–7 days. Animals on the experimental diet did not lose weight but developed polydipsia and high urine volume which persisted after returning to a normal diet. Kidneys were enlarged with the degree of enlargement correlated intake of food containing phosphate. Histological changes were found in the inner cortex, outer medulla and less frequently in the outer cortex of the kidneys. Histochemical changes in the form of marked deposition of minerals in the kidneys of rats kept on the diet containing an excess of inorganic phosphate were observed.
In a study by Dymsza et al. (1959), three groups with 12 male Wistar rats in each group were fed diets containing added dipotassium phosphate so that the calcium and phosphorus concentrations in the experimental diets were as detailed below.
| Diet | Calcium % (mg/kg bw per day) | Phosphorus % (mg/kg bw per day) |
|---|---|---|
| Control | 0.56 (504) | 0.42 (378) |
| ‘Normal orthophosphate’ | 0.47 (423) | 0.43 (387) |
| ‘High orthophosphate’ | 0.50 (450) | 1.30 (1170) |
bw: body weight.
The study was conducted in three stages, with experimental observations after animals had consumed the test diets for 50, 60 or 150 days. No adverse physiological effects were observed clinically at autopsy or on histological examination, including absence of nephrocalcinosis in the group of rats receiving ‘high orthophosphate’ within a period of 150 days, even though the weight of the kidneys was increased in this group.
Groups of 26‐day old female albino rats were fed either a basal diet (control) or diets containing phosphoric acid, monosodium phosphate, disodium phosphate or trisodium phosphate at doses between 2,556 and 7,836 mg/kg bw (Mackay and Oliver, 1934). The rats were killed 44 days later. Addition of inorganic phosphate in any form led to increase of the kidney weights and gross examination revealed that kidneys were enlarged and firm with a pebbled surface produced by numerous scars in all dosed groups. Renal lesions in the form of cells necrosis of the convoluted tubules, regeneration of atypical epithelium and calcification of the necrotic debris were found in rats from all groups that had received phosphate in the diet while the kidneys from control animals were normal.
Female Wistar rats were fed a basal diet or a basal diet containing various concentrations of calcium, magnesium and phosphorus in the form of calcium oxide, magnesium oxide and monosodium phosphate (Chow et al., 1980). The experiments lasted for either 7 or 11 weeks. The concentrations of calcium and phosphorus were 0.4, 0.5, 0.8, 1.0, 1.5 and 2% of the diet dry matter (equivalent to 360, 450, 720, 900, 1,350 and 1,800 mg/kg bw per day) while the concentrations of magnesium were 0.2%, 0.4%, 0.8% and 1% of diet dry matter (equivalent to 180, 360, 720 and 900 mg/kg bw per day). The low levels of the minerals met or exceeded the requirements for rats. Magnesium phosphate uroliths developed in the renal pelvis, bladder and/or ureter of rats fed diets containing 1% magnesium (900 mg/kg bw per day) with either 1.0% or 0.5% phosphorus (900 or 720 mg/kg bw per day). Calcium phosphate uroliths formed in the renal tubules of the corticomedullary junction of rats fed a diet containing phosphorus ≥ 0.8% (720 mg/kg bw per day) and magnesium ≤ 0.8% of diet dry matter (≤ 720 mg/kg bw per day). The incidence and severity of the uroliths were reduced by increasing the magnesium content from 0.2 (180 mg/kg bw per day) to 0.8% (720 mg/kg bw per day) and by increasing the calcium to phosphorus ratio to > 1. The results indicated that interactions among the dietary content of calcium, magnesium and phosphorus affects incidence, severity and type of uroliths in rats.
Three‐week‐old female (RIV:TOX) rats were allowed to acclimate for 13 days on a diet containing 0.4% phosphorus and 0.04% Mg (Mars et al., 1988). Phosphorus was added in the form of monosodium phosphate dihydrate. The rats were transferred to four groups (6 animals per group) and fed diets varying in phosphorus and magnesium content only. These diets consisted of either 0.2% or 0.6% P and 0.02% or 0.04% Mg; another four groups were fed 0.4% or 0.8% P and 0.02% or 0.04% magnesium (the 0.2, 0.4, 0.6 and 0.8% P doses were calculated to 240, 480, 720 or 960 mg/kg bw per day, respectively (EFSA, 2012). The study lasted for 28 days. Groups fed a diet containing 0.4%, 0.6% and 0.8% P showed a statistically significant decrease in urinary calcium levels but faecal excretion was not systematically affected. Dietary content of 0.4%, 0.6% and 0.8% P increased faecal excretion of Mg (p < 0.01) and decreased urinary excretion of Mg (p < 0.01). Increased dietary P intake was positively correlated with urinary excretion of P (r = 0.99). Kidney weights were statistically significantly increased by dietary P (p < 0.01) and so were kidney levels of Ca (p < 0.01) and P (p < 0.01). Calcification was only investigated in the groups fed on a diet of 0.2% and 0.6% P. Calcification of the kidney was only found in the group receiving 0.6% (720 mg/kg bw per day) P and all the animals showed some degree of nephrocalcinosis in that group.
Ritskes‐Hoitinga et al. (1989) studied the effects of a control diet containing 0.4% phosphorus (1.51 g monosodium phosphate dihydrate/100 g diet) and a diet containing 0.6% phosphorus (2.52 g monosodium phosphate dihydrate/100 g diet) (equivalent to approximately 480 and 720 mg/kg P bw per day) fed to female SPF‐derived outbred Wistar rats for 28 days. The treatment with 0.6% phosphorus resulted in statistically significant increase in marked kidney calcification. In rats fed the 0.6% phosphorus diet, phosphorus retention and urinary excretion were greater compared with rats fed the 0.4% phosphorus diet. The following indicators of kidney function were examined: urinary volume, urine and plasma osmolality, urine and plasma creatinine, urine and plasma urea, urea and creatinine clearance and urinary albumin excretion. Of these indicators, only urinary albumin excretion was significantly increased in rats fed the diet containing 0.6% phosphorus. Urinary pH was also decreased in the group fed the high phosphorus diet. A statistically significant increase in calcium, phosphorus and magnesium content in the kidney was observed (p < 0.01, for all).
Body weight and feed intake was not affected. No no‐observable‐adverse‐effect level (NOAEL) could be derived from this study.
Female Wistar rats were fed a diet of monopotassium phosphate in levels corresponding to either a normal phosphorus diet or high phosphorus diet (Matsuzaki et al., 2001). The content of monopotassium phosphate in normal phosphorus diet was 6,848 g/kg and 46,361 g/kg (corresponding to 822 and 5,563 mg/kg bw per day) in the high phosphorus diet. The experiment was ended after 21 days. A statistically significant increase in phosphorus intake was observed in animals in on the high phosphorus diet as well as a decrease in magnesium intake. Calcium, magnesium and phosphorus concentrations in the kidney were significantly increased and kidney dry weight was also increased in the group fed the high phosphorus diet compared with the group fed the normal phosphorus diet. Nephrocalcinosis was observed in all the rats fed on the high phosphorus diet and was not observed in the kidneys of the animals fed the normal phosphors diet. Serum urea nitrogen concentration as well as creatinine, albumin, N‐acetyl‐β‐d‐glucosaminidase activity and β2‐microglobulin in urine were not affected. Calcium and magnesium concentration in urine showed a statistically significant decrease in the rats fed high phosphorus compared with rats fed normal phosphorus diet. The phosphorus content in urine was statistically significantly increased in the rats fed high phosphorus. Calcium absorption was unaffected whereas magnesium absorption was decreased and phosphorus absorption was increased in the high phosphorus group. The NOAEL of this study was 187 mg P/kg bw per day.
Dog
Male Beagle dogs were given equimolar amounts of dipotassium phosphate (trihydrate) or disodium phosphate (dihydrate) daily by gavage; the control group was given the vehicle (water) (Schneider et al., 1981. In the first week, the doses were 2,080 mg/kg bw per day dipotassium phosphate and 1,625 mg/kg bw per day disodium phosphate and the animals were dosed prior to their food. Because vomiting occurred the doses were halved, and food was given prior to the test solutions. In weeks 2–9, the animals received 1,040 mg/kg bw per day dipotassium phosphate and 812.5 mg/kg bw per day per day disodium phosphate. The doses in weeks 10–22 were as in the first week, i.e. 2,080 mg/kg bw per day dipotassium phosphate and 1,625 mg/kg bw per day disodium phosphate. At the end of the 9th week, two animals from each group were killed and the remaining animals were killed at the end of the 22nd week. The kidneys from all the animals were examined by light microscopy and kidneys from 2 animals in each group were examined by electron microscopy. Nephrocalcinosis with disseminated atrophy of the proximal tubule was found in animals treated with dipotassium phosphate or disodium phosphate and the changes were more marked after 22 weeks than after 9 weeks.
Diphosphate
Rat
Sprague–Dawley rats were administered tetrasodium diphosphate by oral gavage for 90 days (5 doses per week) according to OECD test guideline 408 (OECD, 1998) at doses of 250, 500 and 1,000 mg/kg bw per day (Seo et al., 2011). Control animals received filtered tap water only. There were no treatment‐related deaths in any of the groups. The only clinical finding was hair loss in female rats at 500‐ and 1,000‐mg/kg bw per day groups. Body weight gains were lower in males of the 1,000‐mg/kg bw per day group compared with controls. Urinalysis results were normal for all groups. Total white blood cell counts were statistically significantly increased compared with controls in males and females of the highest dose group. In the 1,000‐mg/kg bw per day group, neutrophil counts were statistically increased in females and lymphocyte counts statistically significantly decreased. Total red blood cell, haemoglobin, haematocrit, prothrombin time and activated partial thromboplastin time were statistically significantly reduced in males of the 1,000‐mg/kg bw per day group compared with controls. Prothrombin time was also statistically significantly reduced in males of the 500‐mg/kg bw per day group. Numerous changes to serum chemistry where also detected in treated animals. Serum total protein was statistically significantly reduced in males and females in the 500‐ and 1,000‐mg/kg bw per day groups. Albumin was statistically significantly decreased in males of the 500‐ and 1,000‐mg/kg bw per day groups. This reduction in albumin was also observed in females of the 1,000‐mg/kg bw per day group. The albumin/globulin ratio was statistically significantly increased in the 500‐ and 1,000‐mg/kg bw per day females, and the 1,000 mg/kg bw per day males. Serum aspartate aminotransferase (AST) was statistically significantly increased in high‐dose males, and alanine aminotransferase (ALT) was statistically significantly decreased in high‐dose females. Serum calcium (males and females p < 0.01), phosphorus (males p < 0.01; females p < 0.05), sodium (females only p < 0.01), potassium (males only p < 0.05) and chloride (males only p < 0.05) were statistically significantly reduced in the high‐dose groups. Serum phosphate and sodium were also statistically significantly reduced in the 500‐mg/kg bw per day males and females. In comparison to control values, relative (not absolute) liver weights in males of the 500‐ and 1,000‐mg/kg bw per day groups were statistically significantly increased (p < 0.05). The absolute and relative liver weights of the 1,000‐mg/kg bw per day females, and the relative liver weights of the 500‐ and 1,000‐mg/kg bw per day females were statistically significantly increased (all p < 0.01). There were no gross pathological findings. The only histopathological findings were kidney lesions; cortical tubular basophilia of the renal tubule was more evident in males of the 1000‐mg/kg bw per day group. Mineralisation of the kidney was also observed in females of the 1000‐mg/kg bw per day group.
The authors of the study considered the findings regarding haematological parameters most likely not be toxicologically relevant and they concluded that the NOAEL for this study is 500 mg/kg bw per day tetrasodium diphosphate (corresponding to 116 mg/kg P bw per day).
The Panel agrees with this NOAEL for calcification and lesions of the kidney.
Tetrasodium diphosphate was administered to rats (10 animals/sex per group) via their diet at concentrations of 1.0%, 2.5% and 5% (approximately 900, 2,250 and 4,500 mg/kg bw per day) for 16 weeks (Datta et al., 1962) A control group received untreated diet only. After the end of treatment liver and kidney function tests as well as haematology, organ weights, macroscopic and microscopic examinations were conducted. There was no effect on liver function or haematology. However, the kidney function (measured by specific gravity of urine between 8 and 24 h of water deprivation) of males in the 2.5% and 5% groups and females of the 5% group was impaired. Animals of the 5% group had statistically significant increases in relative weights of the heart, stomach (p < 0.01), intestines (females only; p < 0.01), kidneys (male: p < 0.05; females: p < 0.01) and testes (p < 0.05). The relative kidney weights were also statistically significantly increased (p < 0.01) in females of the 2.5% group. Macroscopic examinations revealed pale, pitted kidneys, calcification of kidneys, and hypertrophy and haemorrhages of the cardiac/pyloric border of stomach in male and female animals of the 5% group and females of the 2.5% group. The kidney was the only organ/tissue to show microscopic changes. At all doses, there was 95–100% of the group affected by microscopic changes, which were primarily in the cortex for the 1.0% and 2.5% groups. The main observations in the cortex were cortical atrophy and cortical hyaline degeneration, whereas the medullary zone was more affected in the rats treated with 5% tetrasodium diphosphate. The main findings in the medullary zone were medullary calcification and medullary necrosis. Tubular casts and chronic inflammatory changes were also observed in the 2.5 and 5% groups. Haemorrhages and exudates were observed in all groups in a dose‐dependent manner. The Panel concluded that the NOAEL for this study was less than 1.0% (the lowest dose tested; approximately 900 mg/kg bw per day tetrasodium diphosphate). This corresponds to 209 mg/kg bw per day P assuming that the anhydrous form has been used.
Triphosphates
Rat
Rats (14 males/group) were administered 0.2%, 2% and 10% (equivalent to 180, 1,800 and 9,000 mg/kg bw per day) of sodium triphosphate (corresponding to pentasodium triphosphate) in diet for 28 days (Hodge, 1956). A control group receiving 9,000 mg/kg sodium chloride was also included. Three rats were sacrificed from each dose level on the 3rd, 7th and 14th day of the experiment and the remaining 5 rats on day 28. Early kidney changes compatible with phosphate nephritis were evident on the 3rd day in rats receiving 9,000 mg/kg bw per day sodium triphosphate, including nuclear pyknosis, coagulative necrosis and early breakdown of cells of the broad limb of Henle. These changes had become more pronounced by day 7, with tubular necrosis having spread from its origin near the junction of the outer zone of the medulla to the inner cortex. By day 14, the 9,000 mg/kg group had further severe changes in the tubules, including tubular necrosis with dilatation of the proximal convoluted tubules and subcapsular spaces of glomeruli. Clinical signs included growth retardation and increased kidney weight at the 9,000 mg/kg bw per day. Sodium chloride at 9,000 mg/kg bw per day also resulted in an increase in average kidney weight with dilated tubules and acute pyelitis. The rats that received 1,800 mg/kg triphosphate in diet had inflammatory changes in the kidney which were not characteristic of tubular necrosis as such but were likely to be due to the phosphate in the diet (as stated by the study authors). The animals administered 180 mg/kg bw per day had no test material‐related kidney abnormalities. The Panel therefore concluded 180 mg/kg bw per day (corresponding to 45 mg/kg P bw per day) to be the NOAEL in this study.
Dog
Dogs (4 animals) were administered 100 mg/kg bw per day of sodium triphosphate (corresponding to pentasodium triphosphate) in diet for 28 days (Hodge, 1956). The tissues of the dogs receiving 100 mg/kg bw per day were normal, with no apparent histological changes. A second group of dogs (4 animals) were fed sodium triphosphate on a program of increasing dose, starting at 1,000 mg/kg and ending at 4,000 mg/kg 5 months later as follows: 1,000 mg/kg bw per day for 2 weeks, 1,500 mg/kg for 3.5 weeks, 2,000 mg/kg bw per day for 2.5 weeks, 2,500 mg/kg bw per day for 6.5 weeks, 3,000 mg/kg bw per day for 1 week, 3,500 mg/kg bw per day for 2 weeks and 4,000 mg/kg bw per day for 4 weeks. One dog began to lose weight on the 2,500 mg/kg bw per day dose, whereas the three other dogs only lost weight once on the 4,000 mg/kg bw per day diet. Blood samples were taken at the beginning and the end of the studies, which gave normal haematological values. Organ weights were normal. At necropsy, hypertrophy of the left ventricle and tubular damage in the kidney was evident in dogs receiving the high dose. The kidneys showed focal areas of granulomatous response with associated multinucleated giant cells. A NOAEL for this study is difficult to determine due to the varying dose that was administered, and necropsy was only performed at the end of the dosing period with the highest dose.
Polyphosphates
Rat
Rats (14 males/group) were administered 0.2%, 2% and 10% of sodium hexametaphosphate (corresponding to soluble sodium polyphosphate) in their diet for 28 days equivalent to 180, 1,800 and 9,000 mg/kg bw per day sodium hexametaphosphate, respectively (Hodge, 1956). Sodium triphosphate (corresponding to pentasodium triphosphate) was also tested in this study (see above under triphosphate). Since the results with sodium hexametaphosphate are identical with those found with sodium triphosphate with a NOAEL of 180 mg/kg bw per day (corresponding to 55 mg/kg P bw per day), no review of the results with hexametaphosphate is made here.
In a limited 28‐day study, male weanling rats (5 animals/group) were given a diet supplemented with sodium hexametaphosphate at a concentration of 0.2%, 2%, 5% or 10% equivalent to 180, 1,800, 4,500 and 9,000 mg/kg bw per day sodium hexametaphosphate, respectively (Franklin Institute Research Laboratories, 1973). At sacrifice on days 3, 7, 15 and 28 relative splenomegaly was observed. The kidneys were pale and swollen and renal tubular necrosis was ‘remarkable’ (no information on the time points at which these observations were made). Following administration of a diet containing 2% sodium hexametaphosphate, acute pelvic inflammation was observed on day 28. There were no adverse effects following administration of a diet containing 0.2%, equivalent to 180 mg/kg bw per day sodium hexametaphosphate (corresponding to 55 mg/kg bw per day P) which was thus derived as the NOAEL.
Groups of Wistar rats (12 animals/group) were given a diet containing sodium hexametaphosphate at 0.93% and 3.5% for 50, 60 or 150 days equivalent to 837 and 3,150 mg/kg bw per day sodium hexametaphosphate, respectively (Dymsza et al., 1959). There were no adverse physiological effects observed in clinical tests (determination of haemoglobin and blood serum calcium and phosphorus content after 60 days, and red blood cell counts, haemoglobin, and blood serum calcium and phosphorus after 150 days), necropsies (organ weights after 60 days) or microscopic examinations (heart and kidney after 150 days) at either dose. The Panel concludes that due to the limited nature of this study it is difficult to derive a NOAEL.
Summary
In summary, results of multiple studies in rats and dogs ranging from 28 to 150 days have demonstrated that kidney is a target organ to phosphates at high doses. At high phosphate loads, excess phosphate causes increased bone demineralisation and release of calcium. This mechanism is part of a physiological regulatory mechanism leading to calcification of the kidney and tubular nephropathy.
The Panel noted that the highest reliable NOAEL for kidney effects, 500 mg/kg bw per day corresponding to 116 mg/kg bw per day phosphorus, was identified in a 90‐day rat study with tetrasodium diphosphates performed according to OECD guidelines (Seo et al., 2011). In the same study, a dose of 1,000 mg/kg bw per day corresponding 233 mg/kg bw per day phosphorus was demonstrated to induce effects in the kidney.
3.5.6. Genotoxicity
Phosphoric acid, phosphates, diphosphates, triphosphates and polyphosphates have been tested for genotoxicity in a variety of in vitro and in vivo assays. In neither in vitro nor in vivo assays did any of the tested phosphates produce a positive response.
In vitro tests included Salmonella Typhimurium mutagenicity assay (unpublished report from Litton‐Litton Bionetics cited in JECFA 1982b, Haworth et al., 1983; Cipollaro et al., 1986; Newell et al., 1974; Ishidate et al., 1984; Kim et al., 2010; Fujita and Sasaki, 1990), Saccharomyces cerevisiae mutagenicity assay (unpublished report from Litton Bionetics cited in JECFA 1982b), Escherichia coli mutagenicity assays (Demerec et al., 1951; Olivier and Marzin, 1987), chromosomal aberration test in Chinese hamster fibroblasts (Ishidate et al., 1984) and in human embryonic lung cells (unpublished report from Litton Bionetics cited in JECFA 1982b).
In vivo tests included chromosomal aberration test in rats (unpublished report from Litton Bionetics cited in JECFA 1982b), dominant lethal assay in rats (Newell et al., 1974), host‐mediated assay in mice (Newell et al., 1974) and mouse translocation test (Newell et al., 1974).
There is one reported study where the authors claimed that phosphoric acid (E 338) increased the mean tail length and mean tail intensity in Comet assay in human lymphocytes in vitro (25, 50, 100, 200 μg/mL) (Yilmaz et al., 2014). However, the relevance of the findings reported in this study for risk assessment is questionable.
The Panel concluded that available data clearly show that phosphate is not genotoxic in standard test systems.
3.5.7. Chronic toxicity and carcinogenicity
There are few chronic toxicity or carcinogenicity studies available for the phosphates under evaluation. Only data on tetrasodium diphosphate, sodium triphosphate and sodium metaphosphate (also referred as sodium hexametaphosphate or Graham's salt) are available. Furthermore, the studies are relatively old, of variable quality and not performed according to current guidelines.
Diphosphates
Rat
Tetrasodium diphosphate was administered to groups of rats (24–36 animals/group; strain, age and numbers per sex not stated) in their diets at concentrations of 1.8%, 3% or 5% (approximately 810, 1,350 and 2,250 mg/kg bw per day) for 6 months (Hahn et al., 1958; Hahn and Seifen, 1959). Control animals received basic control diet. Nephrocalcinosis was observed in animals administered 1,350 or 2,250 mg/kg bw per day tetrasodium diphosphate. In the group at 1,620 mg/kg bw per day, a slight, but statistically significant increase in kidney weights was recorded and microscopic examination revealed renal calcification in some animals (number not stated). The study authors noted that slight renal calcification was also observed in the control animals but as stated by JECFA (1982b) was much less extensive than in the treated animals. No other adverse effects were reported. Therefore, the NOAEL under the conditions of this study can be concluded to be less than 810 mg/kg bw per day (corresponding to 189 mg/kg P bw per day) tetrasodium diphosphate in the diet. A lower concentration of 1.1% (approximately 495 mg/kg bw per day) of tetrasodium diphosphate was later tested under the same conditions for 6 months (Hahn, 1961; JECFA, 1982b). There was slight growth retardation initially, but this did not persist throughout the exposure period. After 39 weeks, slight kidney calcification was observed.
Triphosphates
Rat
Groups of weanling albino rats (50 animals/sex per group) were maintained on diets containing 0%, 0.05%, 0.5% and 5% (equivalent to 0, 25, 250 and 2,500 mg/kg bw per day) sodium triphosphate (corresponding to pentasodium triphosphate) for 2 years (Hodge, 1959). Body weights of the animals were recorded, blood samples taken, and urine analysis performed during the study. At the end of the experimental period, surviving rats were terminated and the tissues and organs fixed and sectioned and studied for histopathology. Bone samples were collected at termination to detect any abnormalities or calcification. At the 2,500 mg/kg dose, a clear growth depression was evident in male rats, which was less pronounced in female rats during both the first and second year. The mortality was high but the majority of the deaths (8–28 rats per group) were due to respiratory infection and pericarditis‐peritonitis. The number of deaths from tumours was very small (≤ 2 animals per group) and did not differ between the different dose levels and controls, presenting no evidence for the carcinogenicity of sodium triphosphate. There was no indication of the treatment having an effect percentage of sugar and protein in urine. Haematology data indicated that male rats at the 1‐year time point receiving the 2,500 mg/kg diet may have been slightly anaemic. The red blood cell count, haematocrit percentages and haemoglobin values were lower compared to other groups. A similar trend was not established for female animals. No other changes in haematological values were reported. In the high dose male rats, kidney weights, measured as the kidney to body ratio were higher than in other groups. A similar effect was also noted in the liver, brain, testes, stomach and heart weights. For female rats receiving the 2,500 mg/kg diet, an increase in liver and kidney weights was also seen in the 2,500 mg/kg group. Bone analysis revealed shorter femur length in both sexes receiving the 2,500 mg/kg diet, an indication that the rats had failed to grow as stated by study authors. All calcium–phosphorus bone ratios were reported to be within normal range. At the end of the 2‐year study period, the surviving animals were sacrificed, and tissues gathered for histological examination. The main finding was enlarged, granular kidneys in rats of both sexes receiving the 2,500 mg/kg diet. Convoluted renal tubules were found to be dilated, especially in the loop of Henle. Hyaline casts were present in most cases. Associated changes were interstitial fibrosis and hyalinised, fibrotic glomeruli. The collective term to describe the condition was ‘chronic tubular nephropathy’, which was present in all rats receiving the high dose. However, control rats, and rats receiving 25 mg/kg bw per day and 250 mg/kg bw per day showed similar changes and therefore establishing definitive treatment‐related causality was not possible. Furthermore, chronic pyelonephritis is stated by the study authors to be frequently present in older rats. However, the study authors conclude that the chronic tubular nephropathy appears to be phosphate‐specific in the high dose group due to scarcity of inflammatory cell infiltrate, gross enlargement of the kidneys, extreme dilation of tubules of loop of Henle and calcification. Tumour incidence in the control and treatment groups was comparable and not considered to be treatment related. Based on the test article‐specific kidney effects which were seen only at the high dose. The panel concluded that 250 mg/kg bw per day (corresponding to 63 mg/kg P bw per day) was the NOAEL in this study.
Polyphosphates
Rat
The carcinogenicity of sodium metaphosphate (corresponding to soluble sodium polyphosphate) was investigated in F344 rats (50 animals/sex per dose; 6 weeks old) (Kitahori et al., 1998). Sodium metaphosphate was administered in the diet at concentrations of 1.5% or 3.0%. (approximately 750 and 1,500 mg/kg bw per day) for 108 weeks. There was also a control group that received untreated diet. Blood samples were taken from all surviving animals in week 108 for haematology and clinical chemistry investigations. Urinalysis was also conducted. Macroscopic and microscopic examinations were conducted on all animals in the study. There were no treatment‐related effects on survival, body weight gains, haematology, clinical chemistry or urinalysis. Many tumours developed in all groups, including the controls. However, the organ distribution and histological characteristics were comparable to those reported to occur spontaneously in this strain of rat. The authors of the study concluded that sodium metaphosphate does not induce tumours in rats, when given orally in the diet for 108 weeks. With regard to non‐neoplastic effects, mineralisation (marked calcium deposition in the pars intermedia of the kidney in the 3% group), cast formation and basophilic tubular cell proliferation was observed in the kidneys of the treated female animals. The panel concluded that the NOAEL for carcinogenicity in this study was 1,500 mg/kg bw per day (corresponding to 456 mg/kg P bw per day), the highest dose tested whereas the NOAEL for microscopic effects observed in the kidneys was < 750 mg/kg bw per day (corresponding to 229 mg/kg P bw per day).
Groups of albino Rochester rats (50 animals/sex per group; described as weanling) were administered a diet containing 0.05%, 0.5% and 5% sodium hexametaphosphate (corresponding to soluble sodium polyphosphate) (approximately 25, 250 and 2,500 mg/kg bw per day) for 2 years (Hodge, 1960). Body weights were recorded weekly for the first 3 months and then every 2 weeks thereafter. Blood samples were taken from 5 animals/sex once before treatment began, monthly for the first 6 months, every 2 months for the rest of the first year, and then every 3 months for the second year. Haemoglobin values, red blood cell characteristics, red blood cell counts, white blood cell counts and differential counts were recorded for all blood samples. Pooled urine samples were collected three times per year to determine sugar and protein content. At termination, tissues and organs from 10 animals/sex per group were collected and studied microscopically. Mortality rates were high (64–78%) and were primarily due to respiratory infections. Tumour incidence increased with age in almost all groups, but there was no dose relationship with sodium hexametaphosphate. Kidney weights were increased in animals in the 5% group and microscopic examinations revealed increased calcification in the tubules of the kidneys. The authors of the study stated that the calcification is believed to be an intensification of the severity of naturally occurring processes of infection and degeneration. However, some of the rats in the 5% group had normal kidneys. Therefore, the NOAEL in this study is approximately 250 mg/kg bw per day (corresponding to 76 mg/kg P bw per day) hexametaphosphate based on treatment‐related effects on the kidney and reduced body weight gain. There was no evidence of increased tumour incidence in any group.
Graham's salt (sodium hexametaphosphate) was administered to groups of rats (24–36 animals/group; strain, age and numbers per sex not stated) in their diets at concentrations of 1.8%, 3% or 5% (approximately 1,620, 2,700 and 4,500 mg/kg bw per day) for 6 months (Hahn et al., 1958; Hahn and Seifen, 1959). Control animals received untreated diets. In the 3% and 5% groups, body weight gain was statistically significantly reduced (p value not stated). In the 3% group, the reduction was transient, whereas in the 5% group the reduction persisted through the 6‐month exposure period. No such effect on body weight gain was observed in the 1.8% group. Nephrocalcinosis was observed in animals administered 3% or 5% sodium hexametaphosphate. The renal calcification was less marked in animals treated with Graham's salt than with other phosphates, such as sodium tripolyphosphate. No other adverse effects were reported.
In summary, there are three 2‐year carcinogenicity studies in rats available, one with sodium triphosphate and two with sodium polyphosphate. In none of the studies were there any relationship between treatment with the phosphates and tumour development. The Panel thus concluded that phosphates do not have any carcinogenic potential. The key adverse effects in these three life time studies as well as in two chronic toxicity studies of 6 months duration were calcification in the kidneys and tubular nephropathy. The lowest tested level of phosphate causing an effect in the kidney was approximatively 750 mg/kg bw (corresponding to 229 mg P/kg bw per day) in a 2‐year study with sodium metaphosphate (Kitahori et al., 1998). Two reliable NOAELs could be identified, 250 mg/kg bw per day (corresponding to 63 mg/kg P bw per day) and 250 mg/kg bw per day (corresponding to 76 mg/kg P bw per day) with sodium triphosphate and sodium hexametaphosphate, respectively (Hodge, 1959, 1960).
In conclusion, the only significant adverse effect of phosphates in standard short‐term, subchronic and chronic toxicity studies is calcification of the kidney and tubular nephropathy. These kidney effects are observed in all species investigated and the onset of the effects are apparently quite rapid with marked effects seen already after a few weeks of treatment.
3.5.8. Reproductive and developmental toxicity
Phosphoric acid, calcium and magnesium phosphate
Mouse
Female albino CD‐1 outbred mice (23–26 mated animals/group) were administered monocalcium phosphate monohydrate (corresponding to calcium dihydrogen phosphate) by gavage in doses of 0, 4.65, 21.6, 100 or 465 mg/kg bw per day through gestation days (GD) 6–15. All animals were observed daily for appearance and behaviour, and body weights were recorded on GD 0, 6, 11, 15 and 17. On GD 17, all dams were subjected to caesarean section and the number of implantation sites, resorption sites and live and dead fetuses were documented. The body weight of the live fetuses was measured. All fetuses were examined for the presence of external congenital abnormalities. Furthermore, one‐third of the fetuses were examined for visceral abnormalities and the remaining two‐thirds for skeletal abnormalities. Treatment with monocalcium phosphate monophosphate induced no maternal toxicity or developmental effects at dose levels up to 465 mg/kg bw per day in mice, the highest dose tested (FDRL 1974, cited in (JECFA, 1982b)].
Rat
In a study with rats given 0.4% or 0.75% (equivalent to 200 or 375 mg/kg bw per day) dietary phosphoric acid over the whole life span and with successive generations no adverse effect on the growth of three successive generations was observed. The animals were mated when they were 32‐week‐old as well as 11 weeks later (only the 0.4% group); no adverse effects were noted as evaluated by the body weight of the dams, the number of living pups and stillborn per litter, the average pup weight at birth and the number of pups at weaning. No significant differences were noted in haematological parameters in comparison with control rats. The histological examination (liver, spleen, adrenals, testes, skeletal muscle, femur and kidney) revealed no pathological changes. Teeth were examined in a number of rats following dietary administration for 3–16 months (both 0.4% and 0.75% groups); no extensive lesions were observed except for dental attrition of the molars which was slightly more marked in the treated group compared to the control group. According to the authors the dental attrition was not to be regarded as a harmful effect (Bonting and Jansen, 1956).
Female albino rats (Wistar derived stock) (25–29 mated animals per group) were administered monocalcium phosphate monohydrate by gavage (vehicle: water) at doses of 0, 4.1, 19.1, 88.5 or 410 mg/kg bw per day through GD 6–15. All animals were observed daily for appearance and behaviour, and body weights were recorded on GD 0, 6, 11, 15 and 20. On GD 20, all dams were subjected to caesarean section and the numbers of implantation sites, resorption sites, and live and dead fetuses were recorded. The body weights of live pups were recorded and all fetuses were examined grossly for the presence of external abnormalities. One‐third of the fetuses of each litter underwent detailed visceral examinations and the remaining two‐thirds were examined for skeletal defects. Treatment with monocalcium phosphate monophosphate induced no maternal toxicity or developmental effects at dose levels up to 415 mg/kg bw per day in rats, the highest dose tested (FDRL 1974, cited in (JECFA, 1982b)).
Three groups (groups I–III) of pregnant Wistar rats (10 weeks old) were treated during GD 0–20 either with the standard diet (group I), corn oil vehicle on standard diet (group II) or on standard diet supplemented with 175 mg/kg bw per day tricalcium phosphate (group III) (Güngörmüș et al., 2010). In a second study, the dose was 350 mg/kg bw per day (Kiliç et al., 2012). Vehicle and tricalcium phosphate were administered orally by gavage. Caesarean section was performed on GD 20. No signs of illness or abnormal behaviour were observed in the dams during the treatment. There were no statistically significant effects on fetal mortality, fetal body lengths and weights. No resorptions, short or absent tail, fore or hind limbs were observed in this study. The placental weights, but not placental index (weight of placenta/weight of fetus), of the tricalcium phosphate group (Group III) were found to be statistically decreased compared to group I (standard diet) (p ≤ 0.05). At skeletal examination, there were no gross skeletal anomalies, incomplete ossification, reduced sternebrae number, misshaped sternebrae, rib or other bones. Moreover, the ossification in fore‐ and hind‐limbs, sacral and caudal bones was complete, there were no extra or missing bones observed in any of the groups. According to morphometric measurements of fetuses, the following parameters were significantly decreased; lengths of left ulna (28.3%, p ≤ 0.05), right femur (29.8%, p ≤ 0.05), left femur (34.9%, p ≤ 0.05) and diameter of the skull of y‐axis (12.3%, p ≤ 0.05) in the tricalcium phosphate treatment groups when compared with control (group I). However, only ulna and left femur were statistically significant different from the vehicle control (group II, p ≤ 0.05). Fetal body lengths and weights were not affected by treatment. Furthermore, there was an increase in transumbilical diameter in the treatment group (group III) both compared to the control (group I) (p ≤ 0.05) and oil control groups (Group II) (p ≤ 0.05) (Güngörmüș et al., 2010).
The study from Güngörmüș et al. (2010) has, however, several shortcomings and inconclusive results. There were only five pregnant rats per group in the study which had two control groups, but only one dose group. The number of fetuses is 11 in the untreated control group, 6.6 in the control group fed with vehicle and 10.5 in the calcium phosphate groups indicating poor performance of the study. Inconsistencies were observed between the results section where the authors conclude ‘no gross structural anomalies or malformations’ and in the discussion where the sentence is found ‘We observed several foetuses with malformations such as: reduced skull development and shorter forelimb and hindlimb formation’. The findings of a reduction in length of left ulna and bilateral femurs are thus most probably artefacts.
In the second study (Kiliç et al., 2010), histopathological changes in maternal liver, kidney, heart, brain, placenta and fetal liver and kidney were reported. In the fetuses, the absolute liver weight increased whereas the relative liver weight decreased which is inconsistent.
Given the inconsistencies and the uncertainty about the causing agent, the Panel considered the studies as inappropriate for risk assessment.
Rabbit
Virgin adult Dutch‐belted female rabbits (15–27 artificially inseminated animals per group) were administered with monocalcium phosphate monohydrate by gavage (vehicle: water) at doses of 0, 2.17, 10.10, 46.7 or 217.0 mg/kg bw per day through GD 6–18. All animals were observed daily for appearance and behaviour, and body weights were recorded on GD 0, 6, 12, 18 and 29. On GD 29, all dams were subjected to caesarean section and the numbers of corpora lutea, implantation sites, resorption sites, and live and dead fetuses were recorded. The body weights of live fetuses were recorded and all fetuses were examined grossly for the presence of external congenital abnormalities. Live fetuses were then placed in an incubator for 24 h for an evaluation of neonatal survival. All pups were then sacrificed and examined for visceral abnormalities and skeletal defects. Treatment with monocalcium phosphate monophosphate induced no maternal toxicity or developmental effects at dose levels up to 217 mg/kg bw per day in rabbits, the highest dose tested (FDRL 1974, cited in (JECFA, 1982b)).
Sodium and potassium phosphate
Mouse
Female albino CD‐1 outbred mice (19–22 pregnant animals per group) were administered with monosodium phosphate by gavage at doses of 0, 3.7, 17.2, 79.7 or 370.0 mg/kg bw per day from GD 6 to 15. The vehicle used was water. Body weights were recorded on GD 0, 6, 11, 15 and 17. All animals were observed daily for appearance and behaviour. On GD 17, all dams were subjected to caesarean section and the sex, numbers of corpora lutea, implantation sites, resorption sites, and live and dead fetuses were recorded. The body weight of the live pups was also measured. All fetuses were examined grossly for the presence of external congenital abnormalities. Furthermore, one‐third of the fetuses were examined for visceral abnormalities and the remaining two‐thirds for skeletal defects. No maternal toxicity or developmental effects were noted at dose levels up to 370 mg/kg bw, the highest dose tested (FDRL 1975, cited in (JECFA, 1982b)).
Groups of pregnant albino CD‐1 mice were dosed by gavage with monopotassium phosphate from GD 6 through 16. Body weights were recorded on GD 0, 6, 11, 15 and 17 of gestation. On GD 17, all dams were subjected to caesarean section and the number of implantation sites, resorption sites and live and dead fetuses were recorded. The body weight of the live fetuses was also measured. All fetuses were examined for the presence of external congenital abnormalities. Furthermore, one‐third of the foetuses were examined for visceral abnormalities and the remaining two‐thirds for skeletal abnormalities. No maternal toxicity or developmental effects were noted for monopotassium phosphate at dose levels up to 320 mg/kg bw (FDRL 1975, cited in (JECFA, 1982b)).
Rat
Groups of 20 pregnant albino Wistar derived rats were dosed by gavage with monosodium phosphate (anhydrous) at dose level of 0, 4.1, 19.0, 88.3 or 410.0 mg/kg bw per day from GD 6 to 15. The vehicle used was water. Body weights were recorded on days 0, 6, 11, 15 and 20 of gestation. All animals were observed daily for appearance and behaviour. On GD 20, all dams were subjected to caesarean section and the sex, numbers of corpora lutea, implantation sites, resorption sites, and live and dead fetuses were recorded. The body weight of the live pups was also measured. The urogenital tract of each dam was examined for anatomical normality. All fetuses were examined grossly for the presence of external congenital abnormalities. Furthermore, one‐third of the foetuses were examined for visceral abnormalities and the remaining two‐thirds for skeletal defects. No maternal toxicity or developmental effects were noted at dose levels up to 410 mg/kg bw, the highest dose tested (FDRL 1975, cited in (JECFA, 1982b)).
Diphosphates
Mouse
Female albino CD‐1 mice (25 mated animals/group) were administered from GD 6 to 15 with 0, 3.35, 15.6, 72.3 or 335 mg/kg bw per day disodium diphosphate by oral gavage (FDRL 1973, cited in (JECFA, 1982b)). Maternal body weights were measured on GD 0, 6, 11, 15 and 17, and all animals were observed for clinical signs of toxicity. Food consumption was also measured. On GD 17, a caesarean section was conducted on all dams. The number of implantation sites, resorption sites, and live and dead fetuses was recorded. All fetuses were examined macroscopically for external congenital abnormalities. One‐third of the fetuses were examined for visceral abnormalities and two‐thirds for skeletal abnormalities. No maternal toxicity or developmental effects were noted at dose levels up to 335 mg/kg bw, the highest dose tested.
Female albino CD‐1 mice (25 mated animals/group) were with administered 0, 1.3, 6.0, 28 or 130 mg/kg bw per day tetrasodium diphosphate by gavage from GD 6 to 15 (FDRL 1975, cited in (JECFA, 1982b)). Maternal body weights were measured on GD 0, 6, 11, 15 and 17, and all animals were observed for clinical signs of toxicity. Food consumption was also measured. On gestation day 17 a caesarean section was conducted on all dams. The sex, numbers of corpora lutea, implantation sites, resorption sites, and live and dead fetuses was recorded. The body weights of the live fetuses were recorded. All fetuses were examined macroscopically for external congenital abnormalities. One‐third of the fetuses were examined for visceral abnormalities and two‐thirds for skeletal abnormalities. No maternal toxicity or developmental effects were noted at dose levels up to 130 mg/kg bw, the highest dose tested.
Hamster
Female golden hamsters (25 mated animals/group) were administered with 0, 1.66, 7.71, 35.8 or 166 mg/kg bw per day disodium diphosphate by gavage from GD 6 to 10 (FDRL 1973, cited in (JECFA, 1982b)). Maternal body weights were measured on GD 0, 6, 8, 10 and 14, and all animals were observed for clinical signs of toxicity. On GD 14 a caesarean section was conducted on all dams. The number of implantation sites, resorption sites, and live and dead foetuses was recorded. The body weights of the live fetuses were measured. All fetuses were examined macroscopically for external congenital abnormalities. One‐third of the fetuses were examined for visceral abnormalities and two‐thirds for skeletal abnormalities. No maternal toxicity or developmental effects were noted at dose levels up to 166 mg/kg bw, the highest dose tested.
Rat
Female albino Wistar‐derived rats (25 mated animals/group) were administered with 0, 1.69, 9.24, 42.95 or 169 mg/kg bw per day disodium diphosphate by gavage from GD 6 to 15 (FDRL 1973, cited in (JECFA, 1982b)). Maternal body weights were measured on GD 0, 6, 11, 15 and 20, and all animals were observed for clinical signs of toxicity. Food consumption was also measured. On GD 20 a caesarean section was conducted on all dams. The number of implantation sites, resorption sites, and live and dead fetuses recorded. The body weights of the live fetuses were measured. All fetuses were examined macroscopically for external congenital abnormalities. One‐third of the fetuses were examined for visceral abnormalities and two‐thirds for skeletal abnormalities. No maternal toxicity or developmental effects were noted at dose levels up to 169 mg/kg bw, the highest dose tested.
Female albino Wistar‐derived rats (25 mated animals/group) were administered with 0, 1.38, 6.41, 29.7 or 138 mg/kg bw per day tetrasodium diphosphate by gavage from GD 6 to 15 (FDRL 1975, cited in (JECFA, 1982b)). Maternal body weights were measured on GD 0, 6, 11, 15 and 20, and all animals were observed for clinical signs of toxicity. Food consumption was also measured. On GD 20 a caesarean section was conducted on all dams. The sex, numbers of corpora lutea, implantation sites, resorption sites, and live and dead fetuses were recorded. The body weights of the live fetuses were measured. All fetuses were examined macroscopically for external congenital abnormalities. One‐third of the foetuses were examined for visceral abnormalities and two‐thirds for skeletal abnormalities. No maternal toxicity or developmental effects were noted at dose levels up to 138 mg/kg bw, the highest dose tested.
Rabbit
Female Dutch‐belted rabbits (15 artificially inseminated animals/group) were artificially inseminated (were administered with 0, 1.28, 5.95, 27.6 or 128 mg/kg bw per day disodium diphosphate by gavage from GD 6 to 18 (FDRL 1973, cited in (JECFA, 1982b)). Maternal body weights were measured on GD 0, 6, 12, 18 and 29, and all animals were observed for clinical signs of toxicity. Food consumption was also measured. On GD 29 a caesarean section was conducted on all dams. The number of corpora lutea, implantation sites, resorption sites, and live and dead foetuses was recorded. The body weights of the live fetuses were measured. All foetuses were examined macroscopically for external congenital abnormalities. The live fetuses of each litter were then placed in an incubator for 24 h to evaluate neonatal survival. All surviving pups were sacrificed and examined for visceral and skeletal abnormalities. No maternal toxicity or developmental effects were noted at dose levels up to 128 mg/kg bw, the highest dose tested.
Triphosphates
Rat
A study previously described by Hodge (1959) combined a chronic toxicity and a reproductive study in rat. The reproductive study was carried out with the 250 mg/kg dose group and the control group. Sixteen females and 8 males were mated. They were mated again at 10 days after weaning of the first litter. Thereafter, 16 females and 8 males were selected from the control and 250 mg/kg group at weaning and continued on their respective diets. When the animals were 100 days old they were mated and they were thereafter mated again 10 days after weaning the first litter, and the whole procedure was repeated with the rats to produce a second litter of the third generation. Parameters of reproductive behaviour which were evaluated included number of females mated, number of pregnancies, mortalities and number of live births, organ weights and pathology. When 21 days old, 10 males and 10 females from each group were necropsied, and the test material‐related abnormalities recorded. The initial mating (first generation, first litter) resulted in 14 pregnancies in the control group and 15 pregnancies in the test group receiving 250 mg/kg sodium triphosphate. No differences in performance were noted between the control and test animals. The second mating (first generation, second litter) resulted in 12 pregnancies in both test and control groups. No significant difference was reported between rats receiving the 250 mg/kg diet and the control rats. The first generation rats were raised to reach 100 days. They were then mated to produce the first litter of the second generation. By performance, the test and control rats were identical. The first litter of the second generation resulted in 12 pregnancies, with no difference in reproductive performance between test and control rats. Similarly, the second litter of the second generation was raised with no complications or difference in survival, growth and fertility. The rats were raised to 100 days of age and mated. The first or second litter of the third generation were not affected in treatment‐related effects when test and control rats were compared. All animals investigated revealed no remarkable pathological findings at necropsy, with no abnormalities in tissues of young animals. The authors of the study concluded that there was no evidence of reproductive toxicity associated with administration of 250 mg/kg sodium triphosphate. The report is lacking in detail, but it adds weight of evidence to the lack of reproductive and developmental effects of the triphosphates.
Rabbit
Dutch‐belted rabbits (17 to 20 females artificially inseminated animals/group) were dosed by gavage with 0, 2.5, 11.6, 54 or 250 mg/kg sodium triphosphate (corresponding to pentasodium triphosphate) from GD 6 to 18 (FDRL 1973, cited in (JECFA, 1982b)). Between 13 and 16 mated rabbits became pregnant out of the 17 to 20 animals per group. Body weights were recorded on GD 0, 6, 12, 18 and 29. Clinical signs, behaviour and food consumption were monitored throughout the study. On GD 29, the animals were subjected to caesarean section and the numbers of corpora lutea, implantation sites, resorption sites and live and dead fetuses were recorded. External abnormalities assessed and body weights were recorded. The live fetuses were maintained in an incubator and observed for neonatal survival for 24 h, after which surviving pups sacrificed and examined for visceral abnormalities and skeletal defects. No maternal toxicity or developmental effects were noted at dose levels up to 250 mg/kg bw, the highest dose tested.
Polyphosphates
Mouse
Female albino CD‐1 mice (25 mated animals/group) were administered with 0 3.7, 17.2, 79.7 or 370 mg/kg bw per day sodium hexametaphosphate (corresponding to soluble sodium polyphosphate) by gavage from GD 6 to 15 (FDRL, 1974). Maternal body weights were measured on GD 0, 6, 11, 15 and 17, and all animals were observed daily for clinical signs of toxicity. Food consumption was also measured. On GD 17 a caesarean section was conducted on all dams. The sex, number of corpora lutea, implantation sites, resorption sites, and live and dead fetuses were recorded. The body weights of the live fetuses were recorded. All fetuses were examined macroscopically for external congenital abnormalities. One‐third of the fetuses were examined for visceral abnormalities and two‐thirds for skeletal abnormalities. No maternal toxicity or developmental effects were noted at dose levels up to 370 mg/kg bw, the highest dose tested.
Rat
Groups of albino Rochester rats (50 weanling animals/sex/group) were administered a diet containing 0.05%, 0.5% and 5% (equal to 26, 260 and 2,600 mg/kg bw per day), sodium hexametaphosphate for 2 years (Hodge, 1960). Animals (16 females and 8 males, 100 days old) from the 0.5% hexametaphosphate group and the untreated control group were selected for a reproductive toxicity study (P1 generation). These animals were bred to produce three F1 generations (F1a, F1b and F1c). The F1a generation were sacrificed on postnatal day 30. Adults from the F1b generation (P2) were mated at 100 days of age to produce the F2a generation, which was sacrificed on postnatal day 30. A second mating of the P2 animals produced the F2b generation, which at 100 days of age (P3) were mated to produce the F3a and F3b generations. The F3a animals were sacrificed on postnatal day 30. The F3b animals were sacrificed on postnatal day 21 and a microscopic examination conducted. Diet containing hexametaphosphate at a concentration of 0.5% and the control diet were available to the animals throughout the study depending on the test group. The study authors concluded that the average number of pups per litter was comparable between the control and treated groups, as was pup mortality, and pup organ weights (F3b only). The microscopic examination did not reveal any abnormal findings in treated animals. Therefore, there were no adverse effects observed under the conditions of this non‐standard study. Although this is a non‐standard study conducted pre‐Good Laboratory Practice (GLP), in the absence of other more reliable studies it provides some reassurance that sodium polyphosphate, and other polyphosphates, do not have an adverse effect on reproduction up to a dose of approximately 260 mg/kg bw per day.
Female albino Wistar‐derived rats (25 mated animals/group) were administered with 0, 2.4, 11.1, 51.7 or 240 mg/kg bw per day sodium hexametaphosphate by gavage from GD 6 to 15 (FDRL, 1974). Maternal body weights were measured on GD 0, 6, 11, 15 and 20, and all animals were observed daily for clinical signs of toxicity. Food consumption was also measured. On GD 20 a caesarean section was conducted on all dams. The sex, number of corpora lutea, implantation sites, resorption sites, and live and dead fetuses were recorded. The body weights of the live pups were measured. The urogenital tract of each dam was also examined. All fetuses were examined macroscopically for external congenital abnormalities. One‐third of the foetuses were examined for visceral abnormalities and two‐thirds for skeletal abnormalities. No maternal toxicity or developmental effects were noted at dose levels up to 240 mg/kg bw, the highest dose tested.
Summary
In summary, there are a number of studies, although generally not conducted to current OECD guidelines, evaluating reproductive and developmental toxicity of the phosphates under evaluation. In studies performed in mice, rats, rabbits or hamsters, there are no signs of reproductive or developmental toxicity at any dose tested. The Panel thus concluded that exposure to phosphates do not present any risk for reproductive or developmental toxicity.
3.5.9. Other animal and in vitro studies
There are a large number of experimental in vivo and in vitro studies, many of which are quite recent, investigating the association of phosphates at high concentrations with pathologies other than kidney calcification and tubular nephropathy (Razzaque, 2012; Uribarri and Calvo, 2018).
Generally, in vitro systems, genetically modified animals and other animal models are used in these studies. It was difficult to establish underlining mechanisms and dose response for the observed effects. Nevertheless, findings in some of the studies (e.g. activation of metabolic pathways that promote cell transformation and cancer, regulation of osteopontin, induction of endothelial dysfunction, alterations of FGF‐23 levels and the Wnt pathway balance, etc.) may indicate potential adverse effects of phosphates.
The Panel did not consider these sufficiently robust nor validated to be used in the risk assessment of phosphate as food additives.
Bone
Several studies in animals report that high phosphorus intake causes bone reabsorption or decreased bone formation.
Effect of high phosphorus intake on bone metabolism‐related gene expression was demonstrated young and aged mice measuring PTH and mediators of osteoclastic bone resorption. Young (12 week old) and aged (80 week old) male mice (12 animals/group) were fed with control diet (0.3% P) or high P content diet (1.2% P) for 4 weeks. The high P content diet increased serum PTH in both young and aged mice and increased receptor activator of NF‐kB ligand (RANK)/osteoprotegerin (OPG)mRNA ratio in the femur of aged mice (Katsumata et al., 2014).
Male Wistar rats (20 animals/group) were fed with control diet (0.6% phosphate) or high phosphate diet (1.2%) for 8 weeks. Bone mineral density (BMD) of femur and lumbar spine was investigated and high‐phosphate intake diet did not appear to negatively impact BMD value (Huttunen et al., 2006).
Abnormal bone mineralisation occurred also when rats were given phosphoric‐acid containing soft drinks instead of water. Young adult (30 days) and immature (30 days) Sprague–Dawley male rats (14 animals/group) has access to tap water (control) or cola‐containing drink ad libitum for one week. Both adult and immature animals receiving cola‐containing drink developed hypercalciuria and hyperphosphaturia. Immature rats developed significant reduction in calcium regulatory hormones such as 1α,25(OH)2D3 and 25‐OHD3 but only adult rats showed developed significant hyperparathyroidism (Amato et al., 1998).
Four groups (9 animals/group) of male Wistar rats (5 week old) were fed with semi‐purified diet non‐supplemented or supplemented with 1%, 1.4%, or 2,2% calcium hydrogen phosphate (Hardwick et al., 1987). Rats receiving diet supplemented with calcium hydrogen phosphate did not show effect on whole blood or plasma ionised Ca, plasma, total Ca, or plasma inorganic P levels. Femur dry weight and length was not affected by the different diets, nor did bone Ca content increase with supplementation.
Anderson et al. (1977), investigated the effect of diets supplied by high phosphorus in monkeys. Nineteen (male and female) juvenile cinnamon ringtail monkeys were fed diets with Ca:P ratio of 1:4, 1:2.1, 1:0.4, 1:0.5 (corresponding to 1.20%, 2%, 0.40% and 0.47% P) up to approximately 7 years. The results did not show any short or long‐term effect in the skeleton in both young growing and adult monkey. The authors reported that those results are in contrast to studies in other species although the Ca:P tested were very similar.
The Panel concluded that effects observed on bone metabolism and bone mineralisation in animals are not well characterised enough to derive an association with dietary high phosphate intake.
3.6. Epidemiology on cardiovascular diseases
3.6.1. Studies on dietary phosphorus and cardiovascular diseases‐related outcomes
Cardiovascular mortality
Chang et al. (2014) conducted a cohort study among healthy US subjects aged 20–80 years (NHANES III; 1998–1994, n = 12,366) to investigate the association between phosphorus intake and all‐cause mortality and cardiovascular‐specific mortality. Among those initially enrolled, 2,680 subjects were excluded from the analysis because of the presence of diabetes, self‐reported history of myocardial infarction and/or congestive heart failure (HF) and/or stroke and/or cancer as well as subjects with extreme energy intakes and with eGFR of 60 mL/min*1.73 m2 or lower. Out of the 12,366 initially enrolled individuals, 9,686 subjects were included in the analysis. Vital stats and cause of death was obtained by using The NHANES III mortality file from the study participation to 31 December 2006 (median follow‐up time: 14.7 years, Interquartile Range (IQR): 13.1–16.2 years). Dietary intake data was assessed by a 24‐h dietary recall. The median phosphorus intake was 1,166 mg/day (IQR: 823–1,610 mg/day); median phosphorus density was 0.58 mg/kcal (0.48–0.70 mg/kcal). Median values of phosphorus consumption in the lowest to highest quartiles were 629, 993, 1,356 and 1,992 mg/day, respectively. Estimated glomerular filtration rate values (mL/min*1.73 m2) in the first, second, third and fourth quartile were as following: 102.6 SD = 0.7; 101.6, SD = 0.7; 102.1, SD = 0.6, 104.4, SD = 0.6. In the multivariate analysis, adjusted for age, sex, race, ethnicity, poverty income ratio, BMI, blood pressure (BP), smoking, physical activity, cholesterol, urine albumin/creatinine ratio, glomerular filtration rate and vitamin D, high absolute phosphorus intake (1,400 mg/day or more) was associated with high overall mortality (HR: 1.89, 95% confidence intervals (CI): (1.03–3.46) while phosphorus density was not (HR: 1.05; 95% CI: 1.01–1.10). For cardiovascular mortality neither absolute intake of phosphorus (HR: 1.02, 95% CI: 0.29–3.58) or phosphorus density (HR: 1.02, 95% CI: 0.93–1.12) were associated with an increased risk. When serum phosphorus was introduced in the models, the risk estimates for both absolute and density phosphorus intake and overall mortality did not change. Serum phosphorus was associated with overall mortality (HR: 1.37, 95% CI: 1.13, 1.67) per each 1 mg/dL increase in serum phosphorus (p = 0.002). The strength of the study was the long follow‐up, the size of the study and the good control of confounding factors. The main limitation of the study was the use of a single 24‐h recall assessing dietary intake, in particular, phosphorus intake. A single day is unlikely to be representative of usual individual intake, especially for phosphorus. The number of days necessary for assessing nutrients and energy intake seems to be at least 5 days. Non‐differential misclassification error leads to HR biases towards the null.
Blood pressure
Alonso et al. (2010) investigated in two US multicentre cohort studies the association between phosphorus intake and hypertension. The study population consisted in 8,208 subjects (age range 45–65 years) from the Atherosclerosis Risk in Communities Study (ARIC) and 2,901 subjects (age range 45–84 years) from the Multi‐Ethnic study of Atherosclerosis (MESA). Subjects with hypertension at baseline and with prevalent CVDs and diabetes were excluded from the analysis. Subjects with missing data were also excluded. Demographic, clinical and dietary data were collected at baseline. Dietary habits were assessed using a 66‐item FFQ in the ARIC study and a 120‐item FFQ in the MESA study. Three measurements were averaged to estimate systolic and diastolic BP. After an average follow‐up of 7.1 years in the ARIC study and 3.8 years in the MESA study, 2,400 and 945 cases of hypertension were identified. The average phosphorus intake was 1,084 mg daily in the ARIC study and 1,103 mg daily in the MESA study. In the multivariate analysis, controlling for age, race, sex BMI, waist circumference, eGFR, education, income, physical activity, cigarette smoking, study site, alcohol intake, energy intake, calcium, vitamin D (only in ARIC), sodium, potassium, magnesium, fruits and vegetables and whole grains intake, no increased risk was found for phosphorus intake and hypertension in the pooled analysis of the two studies (HR: 1.01, 95% CI: 0.82–1.23). When the analysis was conducted separately, no increased risk was found for both ARIC study (Q5, 1,472 mg phosphorus; HR: 0.97, 95% CI: 0.77–1.24) and MESA study (Q5, 1,526 mg phosphorus; HR: 1.10, 95% CI: 0.75; 1.61). The strength of the study was the pooled analysis of two cohort studies and the good control for confounding factors. The limitation of the study was the high number of excluded subjects mainly because of missing data, the lack of data comparing, for some important characteristics the study base and the subjects included in the study (selection bias).
Mazidi et al. (2017) conducted a cross‐sectional study in Iran to investigate the association between diet, in particular phosphorus intake, and BP in individuals aged 35–64 years. Subjects with history of unstable angina, myocardial infarction, stroke, HF, peripheral vascular disease including transient ischaemic attack or amaurosis fugax, cardiovascular interventions or surgery, cancer, autoimmune, infectious and inflammatory diseases were excluded from the analysis. Participants were in total 5,670 subjects (2,179 males, mean age 50.1 years, SD = 8.1) and 3,491 females (mean age 48.2 years, SD = 7.8). Demographic information, clinical, anthropometric (weight, height, waist circumference) and dietary data (24‐h recall) were collected for all participants. Weight and height, total cholesterol, triglycerides and high‐density lipoprotein (HDL) cholesterol were also measured. A significant inverse correlation between phosphorus intake and systolic BP (p = 0.04) and diastolic BP (p = 0.03) was found. The limitation of the study was the cross‐sectional design that impedes drawing conclusions of a possible causality and the lack of a proper statistical method.
Left ventricular mass
Yamamoto et al. (2013), within the MESA, investigated, using a cross‐sectional design, the association between dietary phosphorus with left ventricular mass (LVM) in 4,494 subjects free of known CVD (mean age 61.6 years) and with completed dietary data. Demographic, clinical and lifestyle data were collected at baseline. Dietary phosphorus intake was assessed by a 120‐item FFQ. Mean dietary phosphorus intake was 1,167 mg/day in men and 1,017 mg/day in women. The mean and standard deviation LVM for men and women were 168.6 ± 36.8 g and 123.8 ± 27.4 g, respectively. In the multivariate analysis, after controlling for age, race, height and weight, total dietary calories, dietary sodium, smoking, alcohol use, education, moderate‐vigorous physical activity, diabetes status, systolic BP, antihypertensive medication use, urinary albumin to creatinine ratio, C‐reactive protein and eGFR, each 20% greater estimated dietary phosphorus consumption was associated with 1.06 g greater LVM (p < 0.001). The strength of the study was the good control for confounding factors. The limitation of the study was the cross‐sectional design.
Intima‐media thickness
Itkonen et al. (2013) conducted a cross‐sectional study to investigate the relationship between dietary phosphorus intake, in particular food additive phosphate, and intima‐media thickness (IMT). A randomly sample of 1,920 subjects living in Helsinki, aged 37–47 years (females, n = 370; males, n = 176) was derived from the Population Register Centre in Finland. Out of the 1,920 initially enrolled subjects, 678 participated in the study. Subjects with renal dysfunction, post‐menopausal females and with subjects with missing data were excluded from the analysis. Data on smoking status, information on dietary habits (3‐day food records and FFQ) focusing on phosphorus, calcium and vitamin D, was obtained for all participants. Fasting blood samples and spot urine samples, weight and height, BP, and information on smoking habits and physical activity were also collected at the time of the visit. Common carotid artery IMT was measured using high‐resolution ultrasonography. Mean phosphorus intake from diet (natural occurring phosphate) was 1 617 mg/day (SD = 428). Exposure estimate for phosphates as food additives (FAP) were derived from maximum EU regulation FAP content from the following foodstuffs: marinated meat, sausages, cold meat cuts, cola beverages and processed cheeses. A FAP score (1–6) was created by dividing subjects into tertiles of intake for each FAP group (meat products, cola beverages, processed cheeses), with score 0 indicating the lowest intake tertile, score 1 the middle tertile and score 2 the highest tertile. Then, the scores from different FAP sources were summed and each subject had a score of one to six. No significant association was observed between TP intake or FAP score and IMT after adjusting for sex, age, low‐density/high‐density lipoprotein cholesterol ratio, smoking status and IMT sonographer class. The strength of the study was the attempt to separate total phosphorus and FAP intake. The main limitation of the study was the cross‐sectional design that impedes drawing conclusions of a possible causality. Moreover, the FAP score is not very easily interpreted.
Coronary artery calcification
Kwak et al. (2014) conducted a cross‐sectional study (n = 23,652) to study the relationship between phosphorus intake and phosphorus serum levels and coronary artery calcification (CAC). Eligible participants had no CKD (estimated glomerular filtration rate ≥ 60 mL/min*1.73 m2) and/or CVD. Participants (40.8 ± 7.3 years) were mainly (males 83%), who underwent, as part of health check‐ups, cardiac computed tomographic estimation of CAC (scores, 1–100 and > 100). Dietary habits, including alcohol intake was assessed by a FFQ. Clinical data and information on physical activity and smoking were collected for all participants. In the multivariate analysis, adjusted for adjusted for age, sex, smoking status, alcohol intake, physical activity, body mass index, educational level, family history of CVD, medication for dyslipidaemia, diabetes mellitus, hypertension, glomerular filtration rate, albumin, ferritin, total calorie intake, calcium intake, phosphorus intake and calcium supplements, high serum phosphorus (≥ 3.9 mg/dL) was associated with high CAC scores, (OR: 3.33, 95% CI: 2.55–4.35, p‐trend < 0.001). No association was found for high intake of phosphorus (≥ 965 mg/daily. The strength of the study is the large sample size and the good control of confounding factors. The limitation of the study was the cross‐sectional design that impedes drawing conclusions of a possible causality.
Summary of the results of the studies on dietary phosphorus/phosphates and cardiovascular‐related outcomes
Two cohort studies (Alonso et al., 2010; Chang et al., 2014) and four cross‐sectional studies; (Itkonen et al., 2013; Yamamoto et al., 2013; Kwak et al., 2014; Mazidi et al., 2017) investigated the relationship between dietary phosphorus and cardiovascular‐related outcomes. Alonso et al. (2010) pooled the data of two cohort studies (7.1‐year and 3.2‐year cohort studies, n = 8,208) and found no association between phosphorus intake and hypertension. Chang et al. (2014) conducted a 3.4‐year cohort study (n = 7,705) and found no association between high phosphorus intake (> 1,400 mg/day) estimated from a single 24‐h recall, and cardiovascular specific mortality. The study of Yamamoto et al. (2013) studied the association between dietary phosphorus with LVM in 4,494 subjects and showed that each 20% greater estimated dietary phosphorus consumption was associated with 1.06 g greater LVM and it was statistically significant. Itkonen et al. (2013) studied the relationship between dietary phosphorus intake, in particular food additive phosphate, and IMT and found no association. Kwak et al. (2014) the relationship between phosphorus intake and coronary artery calcification and found no association. Mazidi et al. (2017) investigated the association between phosphorus intake and BP and found a statistically significant inverse correlation between phosphorus intake and BP. In conclusion, there is insufficient data in the cohort studies to link dietary phosphates intake to cardiovascular risk. Inconsistent results have been reported from cross‐sectional studies.
One of the limitations of the epidemiological studies that assessed dietary phosphorus and CVDs outcomes was the use of food composition databases which might not include data on all phosphates used as food additives leading to underestimation of the total phosphate intake. Another limitation was the use the 24‐h recall assessing food intake. It is known that a single day is unlikely to be representative of usual individual intake, especially for phosphorus. The number of days necessary for assessing micronutrients and energy intake seems to be at least 5 days. Thus, this misclassification error may have led risk estimates towards null.
Overall, there is insufficient evidence to link dietary phosphates intake to cardiovascular outcome.
3.6.2. Studies on serum phosphorus/phosphate and cardiovascular diseases‐related outcomes18
Cardiovascular disease incidence and cardiovascular mortality
Chang et al. (2014) investigated associations between serum phosphorous and all‐cause and cardiovascular mortality prospectively in 12,984 participants of NHANES III (mean age 44 years, 52% women, after excluding 181 participants with more than 24 h fasting times or inconsistent venepuncture times). Serum phosphorous was measured at baseline using the reaction of inorganic phosphorous with ammonium molybdate, measured by spectrophotometry. Age, sex, race, ethnicity, cigarette smoking (never, former or current), physical activity, and family income were self‐reported, height, weight at baseline were measured using standardised methods. Participants were stratified by fasting‐duration before venepuncture (≥ 12 h, 6,633 participants; < 12 h, 6,351 participants). Mortality data were obtained from the NHANES III Mortality File, and cardiovascular mortality was defined as International Classification of Diseases (ICD)‐10 I00–178, and after a median follow‐up of 14.3 years, 2,993 deaths had occurred. After adjusting the multivariable model for examination session (morning vs afternoon/evening), age, sex, African American race, Mexican ethnicity, poverty, inactivity, body mass index, smoking status, systolic BP, diabetes, non‐HDL cholesterol level, ACR, eGFR and vitamin D status, high serum phosphorous was significantly associated with all‐cause [HR Q1 vs Q4: HR: 1.74 (95% CI: 1.38; 2.20)] and cardiovascular (HR: 2.00; 95% CI: 1.36; 2.96) mortality in those with 12 h or more fasting before venepuncture, but not those with shorter fasting duration (HR: 1.08; 95% CI: 0.98, 1.32 and HR: 1.21; 95% CI: 0.88,1.67], respectively). A continuous analysis using linear splines shows a significant increase in all cause mortality (HR: 1.35; 95% CI: 1.05, 1.74) per mg/dL) and cardiovascular mortality (HR: 1.45; 95% CI: 1.05, 2.00 per mg/dL). The strength of the study was the large sample size and the long follow‐up. The main limitation of the study was the lack of adjustment for diet.
Larsson et al. (2010) investigated associations between serum phosphorous and all‐cause and cardiovascular mortality in 2,176 men of the Uppsala Longitudinal Study of Adult Men [mean age 50 years, after excluding participants lacking data on creatinine, Ca or Pi measurements (n = 139), or with eGFRCG of 60 mL/min* 1.73 m2 or below (n = 7)]. Serum phosphorous (fasting blood samples, fasting from midnight) was measured at baseline using the reaction of inorganic phosphorous with ammonium molybdate, measured by spectrophotometry. Data on lifestyle, e.g. smoking habits and medical history, were obtained by questionnaire at baseline. Cardiovascular death (ICD‐8 and ICD‐9, codes 390–459; ICD‐10 codes I00–I99) was established using the Swedish national cause‐of‐death register, and after a median follow‐up of 29.8 years, 1,009 participants had died, of which 466 were due to CVDs. After adjusting for age, body mass index, smoking, high serum phosphorous (T3, >2.8 mg/dL vs T1, <2.5 mg/dL) was associated with cardiovascular mortality (HR 1.31; 95% CI: 1.06, 1.63) but not all‐cause mortality (HR: 1.16; 95% CI: 1.00, 1.35). In a continuous model, all cause (HR 1.06; 95% CI: 1.01, 1.12 and cardiovascular mortality (HR 1.10; 95% CI: 1.02, 1.18) per SD increase) were both associated with serum phosphorus. This did not change materially by including only participants with eGFRCG > 90 mL/min* 1.73 m2 (n = 1,777). Strengths of the study was the long follow‐up time and the main limitation was the lack of adjustment for diet and physical activity.
Onufrak et al. (2009) investigated associations between serum phosphorous, all‐cause mortality and coronary artery disease (CAD) incidence in 13,998 participants (7,923 women, mean age 54 years, after excluding those with missing serum phosphorous data (n = 150), self‐reported history of stroke or CAD (n = 1,010), and those with eGFR below 60 mL/min* 1.73 m2 (n = 392) or above 150 mL/min* 1.73 m2 (n = 182) of the ARIC who were free from CAD at baseline. Serum phosphorous was measured in fasting blood samples using the DART method at baseline. Deaths were ascertained using a variety of methods, including official records, obituaries, hospital records and interviews with next of kin, and after a median of 13.2 years of follow‐up, 1,546 participants had died. After adjusting for age, sex, black race, body mass index, diabetes, hypertension, total cholesterol, HDL cholesterol, triglycerides, current smoking, eGFR (by CKD‐EPI formula), serum fibrinogen, post‐menopausal status and hormone replace therapy (HRT), high serum phosphorous (> 3.8 mg/dL vs < 3.1 mg/dL) was associated with an increased risk of CVDs (HR: 1.45; 95% CI: 1.04, 2.01) and all‐cause mortality (HR. 1.45; 95% CI: 1.12, 1.88) was found for men but not for women. Strengths of the study were the long‐term follow‐up time and the sample size; the limitations were the self‐report assessment of the outcomes in some cases and the lack of adjustment for diet and physical activity.
Dhingra et al. (2007) conducted a cohort study on 3,368 subjects within the Framingham Offspring study (mean age, 44 years; 51% of women) to investigate the association between serum levels of phosphorus and calcium and CVD incidence. All subjects with CKD and/or CVD were not included in the study. Information on smoking habits and alcohol consumption was obtained from all participants. Weight, height, BP, total cholesterol, HDL cholesterol, serum albumin, blood glucose, haemoglobin, C‐reactive protein and triglycerides were all measured at baseline and every 4 years. Subjects with eGFR of less than 60 mL/min* 1.73 m2 were excluded from the study. After a follow‐up of 16.1 years, 524 incident CVD cases (159 events in women) were identified through reviewing hospital records, physician office visit notes, and pathology reports. CVD was defined as fatal or nonfatal myocardial infarction, angina pectoris (stable or unstable), cerebrovascular events (stroke or transient ischaemic attacks), peripheral vascular disease, or congestive HF. After adjusting in the multivariate model for age, sex, BMI, diabetes, BP, hypertensive drug use, smoking, alcohol consumption, total high‐density cholesterol ratio, haemoglobin, serum albumin, eGFR, proteinuria and protein C‐reactive protein, high levels of serum phosphorus was associated with an increased CVD risk in a dose response manner (Q4 = 3.5–6.2 mg/dL; HR: 1.55, 95% CI: 1.16–2.07, p trend = 0.04). The increased risk remained statistically significant in the model in which up‐dated CVD risk factors every 4 years were included and in the model that excluded subjects with proteinuria and with an eGFR of 90 mL/min* 1.73 m2 or lower. The strength of the study was the long follow‐up time. The limitation of this study was the lack of control for diet and physical activity.
Foley et al. (2008) conducted a US multicentre cohort study (Atherosclerosis Risk in Communities) to investigate the relationship between calcium phosphate levels and coronary heart disease, stroke and death. Out of 15,732 subjects (mean age 54.2 years, SD = 5.7) initially enrolled, a total of 13,816 subjects were included in the analysis. Demographic and clinical data was collected at baseline for all participants. Information on smoking habits, alcohol consumption and dietary habits was obtained for all participants. FFQ (61‐item instrument) was used to assess dietary habits. Population phosphorus and calcium intake was 14.2 mg/kg (SD = 6.2) and 8.7 mg/kg (SD = 5.3), respectively. Serum phosphate and calcium was also measured at baseline. Mean serum levels of phosphate and calcium was 3.4 (SD = 0.5) mg/dL and 9.8 (SD = 0.4) mg/dL, respectively. The mean level of eGFR was 93.1 (SD = 21.5) per mL/min* 1.73 m2. After 12.6 years of follow‐up, 141 cases of coronary heart diseases and 44 cases of stroke were identified. In this study, dietary intake of phosphorus was associated with serum phosphate (p < 0.0001). In the multivariate analysis, adjusting for age, demographic characteristics, comorbid conditions, serum albumin and eGFR, serum phosphorous (per 0.5 mg/dL) was associated with both stroke (HR: 1.11, 95% CI: 1.02–1.21) and death (HR: 1.14, 95% CI: 1.09–1.20). No association was found for serum phosphate and coronary heart disease (HR: 1.03, 95% CI: 0.98–1.08). For calcium‐phosphate product (per 5.5 mg2/dL2) risk estimates for coronary heart diseases, stroke and death were as following: HR: 1.03, 95% CI: 0.98–1.08; HR: 1.15, 95% CI: 1.05–1.26; and HR: 1.15, 95% CI: 1.09–1.20. The strength of the study was the large sample size and the good follow‐up time. The limitation of the study was the lack of data on the number of people lost in the follow‐up, many missing values in the exposure variables; people with CVDs were not excluded from the study; lack of adjustments for dietary variables, BMI, BP and physical activity.
Onufrak et al. (2009) investigated associations between serum phosphorous all‐cause mortality and CAD incidence in 13,998 participants [7,923 women, mean age 54 years, after excluding those with missing serum phosphorous data (n = 150), self‐reported history of stroke or CAD (n = 1,010), and those with eGFR below 60 mL/min* 1.73 m2 (n = 392) or above 150 mL/min* 1.73 m2 (n = 182)] of the ARIC who were free from CAD at baseline. Serum phosphorous was measured in fasting blood samples using the DART method at baseline. Incident CAD was defined as definite or probably myocardial infarction (fatal or non‐fatal) or death due to CAD. CAD events were detected through annual interviews and surveys of hospital records, and after a median of 13.2 years of follow‐up, 992 participants experienced incident CAD. After adjusting for age, sex, black race, body mass index, diabetes, hypertension, total cholesterol, HDL cholesterol, triglycerides, current smoking, eGFR (by CKD‐EPI formula), serum fibrinogen, post‐menopausal status and HRT, high serum phosphorous (> 3.8 mg/dL vs < 2.9 mg/dL) was associated with CAD incidence in men (HR: 1.45; 95% CI: 1.04; 2.01) but not in women (HR: 0.95; 95% 0.63; 1.41). Strengths of the study were the long‐term follow‐up time and the sample size. The limitations were the self‐report assessment of the outcomes and the lack of adjustment for diet and physical activity.
Dhingra et al. (2010) investigated, within a cohort study (Framingham Offspring study), the association between serum phosphorus and incidence of HF (n = 3,666). It was also studied, using a cross‐sectional design, the relationship between serum phosphorus and echocardiographic left ventricular mass, dimensions and systolic function. Subjects with previous myocardial infarction and/or atrial fibrillation (AF) and/or eGFR < 60 mL/min* 1.73 m2 were excluded from the analysis. In total, 3,300 participants [1,616 men, mean age 44.7 years (SD = 10.3); 1,684 women, mean age 44.0 years (SD = 9.9 years)] were included in the analysis. Clinical data and information on smoking and alcohol were obtained for all participants. The mean eGFR (mL/min* 1.73 m2) was 106 (SD = 43) for men and 114 (SD = 76) for women. After a mean of 17.4 years of follow‐up, 157 cases of HF were identified. After pooling sex‐specific quartiles and controlling for age, sex, BMI, diabetes mellitus, systolic BP, treatment for hypertension, smoking, total cholesterol/HDL cholesterol ratio, valve disease, albumin, haemoglobin, eGFR and proteinuria, subjects in the fourth quartile of serum phosphorus (mean: 3.8 mg/dL for women and 3.6 mg/dL for men) had twice the risk of having a HF in comparison to subjects in the first quartile (HR: 2.09; 95% CI: 1.28–3.40, p‐trend = 0.02). In a subgroup analysis that included 1,850 individuals with eGFR > 90 mL/min* 1.73 m2 and no proteinuria and with phosphorus lower than 4.5 mg/dL, the risk increased even more (HR: 3.11; 95% CI: 1.04–1.69, p‐trend = 0.02). In the same model, using serum phosphorus as a continuous variable the risk remained (HR: 2.40; 95% CI: 1.29–4.46). After adjusting for LVM, dimensions and left ventricular systolic function the risk associated with high phosphorus levels and incidence of HF remained in all models. The strength of the study was the long follow‐up time. The limitation of the study was the lack of control for diet and physical activity.
McGovern et al. (2013) investigated the association between serum phosphate and cardiovascular events within the ‘Quality Improvement in Chronic Kidney Disease’ (QICKD) cluster randomised trial. Subjects with CKDs (n = 33,648, mean age 72.8 years, SD = 16.1 years) and subjects without CKDs (n = 24.184, mean age 52.8 years, SD = 17 years) were included in the study and were followed over a period of 2.5 years. Normal renal function was defined as an eGFR of 90 mL/min* 1.73 m2 or more and absence of significant proteinuria. In the group with normal renal function, 133 strokes, 120 TIAs, 84 MIs, 110 coronary artery procedures, 45 other advanced CAD events, 77 new cases of HF and 521 deaths were identified during the 30 months of follow‐up while in the group with CKD subjects, 291 strokes, 254 TIAs, 199 MIs, 222 coronary artery procedures, 77 other advanced coronary artery, 222 new cases of HF and 1,401 deaths were identified. After adjusting for sex, age, smoking, hypertension, diabetes and cholesterol, subjects with normal renal function and high serum phosphate (1.25–1.50 mmol/L) had an increased risk of cardiovascular events (OR: 1.36, 95% CI 1.06–1.74) in comparison to subjects with normal renal function and serum phosphate levels from 0.75 to 1.00 mmol/L. The risk was even higher for subjects with phosphate levels of 1.50 mmol/L or more, but it did not reach statistical significance (OR: 1.80, 95% CI: 0.89–3.63). In people with CKD, a statistically significant increased risk for cardiovascular events was found for phosphate levels above 1.25 mmol/L. Limitations of the study was the short time of follow‐up the broad definition of cardiovascular events and the lack of control for dietary and physical activity.
Lutsey et al. (2014) within a US multicentre cohort study (ARIC) studied the relationship between serum magnesium, phosphorus and calcium and incidence of HF. Subjects who had a previous HF and/or missing information on the outcome and/or ethnic minorities were excluded from the analysis. A total of 14,709 (aged 45–64 years in the period from 1987 to 1989) were included in the analysis. Demographic information, medical history and medication use, dietary habits including alcohol consumption and lifestyle information such as smoking and physical activity were collected at baseline. After a median follow‐up of 20.6 years, 2,250 incident HF events (ICD‐9 codes from 428.0 to 428.9) were identified through calling by phone participants to ask information on hospitalisation, by reviewing local hospital discharges and by retrieving death certificates. Mean phosphorus levels were 3.43 (SD = 0.49 mg/dL). In the multivariate model, after adjusting for age, sex, race, centre, education, physical activity, smoking status, BMI, diabetes, systolic BP, hypertension medication use, lipid‐lowering medication use, prevalent coronary heart disease (CHD), eGFR, low‐density lipoprotein (LDL) cholesterol, HDL cholesterol, triglycerides and albumin, subjects with high serum phosphorus (median 4.1 mg/dL) had an increased risk for HF (median 4.1 mg/dL) (Q5 vs Q1, HR: 1.36; 95% CI: 1.18, 1.56, p‐trend = 0.0005). After including magnesium and calcium in the models, the risk estimates did not change. The strength of the study was the large sample size. Limitations of the study were the inclusion of subjects also with eGFR below 60 mL/min* 1.73 m2 and lack of control for dietary habits.
Hayward et al. (2017) conducted a retrospective cohort study within sentinel primary care networks of the Royal College of General Practitioners Research and Surveillance Centre to investigate if serum phosphate was a predictor of primary cardiac events. The study included 121,605 patients (18–90 years) free from CVDs. The serum phosphate level was the mean of up to five phosphate measurements before any cardiovascular event. The outcome was defined as any primary cardiac event of myocardial infarction, acute coronary syndrome or revascularisation procedures. After 5 and 9 years of follow‐up (from the initial phosphate measurement), there were 1,595 and 2,268 events, respectively. Demographic data, smoking habits and biochemical and clinical data such as systolic BP, HDL cholesterol, LDL cholesterol, eGFR, diabetes status and blood markers HbA1c, corrected calcium, sodium, potassium and albumin data was obtained for all patients. In the 9‐year review, subjects with phosphate levels of 0.75 mmol/L or less (OR: 1.89, 95% CI: 1.23–2.81) and subjects with phosphate levels above 1.25 mmol/L (OR: 1.83, 95% CI: 1.44–2.31), in comparison to subjects with phosphate levels between 1.0 and 1.25 mmol/L, had an increased risk of a cardiovascular event. The strength of the study was the large sample size and the limitation of the study was the use of administrative data, no clear indication of the confounding factors included in the models.
Lopez et al.(2013) investigated associations between serum phosphorous and AF in 14,998 participants [8,071 women, mean age 54 years, after excluding those who were of a racial group other than white or black (n = 103), those with prevalent AF at visit 1 (n = 37), low‐quality or missing electrocardiograms (n = 242), missing phosphorus levels (n = 124), non‐fasting blood samples (n = 485), missing covariates (n = 108) and eGFR < 15 mL/min* 1.73 m2 (n = 18)] of the ARIC who were free from AF at baseline. Serum phosphorous was measured in frozen fasting blood samples using a method based on ammonium molybdate at baseline. AF diagnoses were ascertained using electrocardiograms performed at study visits, hospital discharge codes and death certificates. During a median follow‐up of 19.7 years, 1,656 incident AF occurred, and after adjusting for age, sex, race, study site, education, height, smoking, alcohol drinking, body mass index, diabetes, serum calcium (adjusted for albumin), systolic BP, diastolic BP, use of antihypertensive medications, eGFR (modelled as a spline), prevalent stroke, prevalent HF and prevalent coronary heart disease, high serum phosphorous (≥ 3.9 mg/dL vs ≤ 3.0 mg/dL) was not associated with increased risk of AF (HR: 1.15; 95% 0.98; 1.36). After stratification by eGFR, a significant association was only found in those participants with eGFR ≥ 90 mL/min* 1.73 m2 (n = 10,149; 1,022 cases; (HR: 1.34; 95% CI: 1.09; 1.65), but not those with eGFR 60–90 mL/min* 1.73 m2 (n = 4297; 587 cases; HR 0.91 [0.68; 1.21]) or eGFR < 60 mL/min* 1.73 m2 (n = 243; 47 cases; HR 1.24; 95% CI: 0.44; 3.46). Strengths of this study are the sample size and duration; the limitations were the lack of adjustment for diet and physical activity.
Foley et al.(2009) investigated the association between serum phosphorous and coronary artery calcification in 3,015 out of 5,115 participants of the Coronary Artery Risk Development in Young Adults (CARDIA) study for whom data on serum phosphorous concentration at baseline and coronary artery calcium level after 15 years of follow‐up were available (mean age at baseline 25.2 years, 54% women; 1,444 participants were lost at follow‐up, 629 did not have data on coronary artery calcium and a further 27 did not have data on serum phosphorous). Serum phosphorous was measured in fasting (12 h) blood samples using a SMAC 12 continuous flow analyser, coronary artery calcification was assessed by different methods in different study centres, i.e. Imatron C‐150 electron beam scanner, GE Lightspeed multidetector scanner or Siemens (Berlin, Germany) VZ multidetector scanner to calculate a calcification score. 9.6% of the study population had some artery calcification, but only 1.6% had moderate or severe calcification. After adjusting for age, sex, ethnicity, education, smoking status, prevalent diabetes, family history of MI, BMI, blood lipids and glucose, BP, eGFR, exercise, medication and diet (e.g. alcohol, calcium and phosphorous), serum phosphorous was significantly associated with calcification score category (0, 0–10, 10–100, 101–300 or 300 units, OR 1.17 (1.01; 1.34) per 0.5 mg/dL, and a calcification score above 10 (OR: 1.20; 95% CI: 1.01; 1.43). In categorical analyses, using quantiles, high serum phosphorous (> 3.9 mg/dL vs ≤ 3.3 mg/dL) was significantly associated with a calcification score above 10 (OR 1.60; 95% CI: 1.01; 2.55). These associations did not change materially after excluding participants with an eGFR below 60 mL/min* 1.73 m2. The strength of the study was the long follow‐up period and the limitations were the use of a logistic model and the use of a single 24‐h dietary recall.
In summary, nine cohort studies on CVD incidence (Dhingra et al., 2007, 2010; Foley et al., 2008; Onufrak et al., 2009; Lopez et al., 2013; McGovern et al., 2013; Lutsey et al., 2014; Hayward et al., 2017) and two cohort studies on cardiovascular mortality (Larsson et al., 2010; Chang et al., 2014) were reviewed. Dhingra et al. (2007) conducted a cohort study on 3,368 subjects and observed that high serum phosphorus was associated with an increased CVD risk in a dose response manner. Foley et al. (2008) conducted a multicentre cohort study in 13,816 subjects and showed a positive association between serum phosphates and stroke incidence but not for serum phosphorus and coronary heart disease incidence. Onufrak et al. (2009) conducted a cohort study in 13,998 participants and showed that high serum phosphorous was associated with an increased risk for CAD incidence among men but not among women. Dhingra et al. (2010) in cohort study of 3,666 subjects showed that serum phosphorus was associated, in a dose‐response manner, with an increased risk of HF. McGovern et al. (2013) in a cohort study of 24,184 subjects showed that high phosphorus levels were associated with an increased risk for cardiovascular events. Lutsey et al. (2014) within a US multicentre cohort study (n = 14,709) showed that high serum phosphorus was associated with an increased risk of HF. Hayward et al. (2017) conducted a retrospective cohort study on 121,605 subjects and showed an increased risk of cardiovascular events among subjects with both low (0.75 mmol/L or less) and high serum phosphorus levels (1.25 mmol/L or more). Lopez et al. (2013) in a cohort of 14,998 subjects showed that high serum phosphorous was not associated with the incidence of AF. Foley et al. (2009) investigated in a cohort study of 3,015 subjects the association between serum phosphorous and coronary artery calcification level and found a statistically significant association. Chang et al. (2014) in a cohort study of 12,984 subjects showed that high levels of phosphorus was associated with an increased risk of cardiovascular mortality. Larsson et al. (2010) in cohort study of 2,176 men showed an increased risk of cardiovascular mortality for those in the highest category of phosphorus.
Overall, there is evidence for a link between serum phosphorus and incidence of CVDs and some evidence to link serum phosphorus and cardiovascular mortality.
Coronary artery calcification
Kwak et al. (2014) conducted a cross‐sectional study (n = 23,652) to study the relationship between phosphorus intake and phosphorus serum levels and CAC. Eligible participants had no CKD (eGFRrate ≥ 60 mL/min* 1.73 m2) and/or CVD. Participants (40.8 ± 7.3 years) were mainly (males 83%), who underwent, as part of health check‐ups, cardiac computed tomographic (CT) estimation of CAC (scores, 1–100 and > 100). Dietary habits, including alcohol intake was assessed by a FFQ. Clinical data and information on physical activity and smoking were collected for all participants. In the multivariate analysis, adjusted for adjusted for age, sex, smoking status, alcohol intake, physical activity, body mass index, educational level, family history of CVD, medication for dyslipidaemia, diabetes mellitus, hypertension, glomerular filtration rate, albumin, ferritin, total calorie intake, calcium intake, phosphorus intake and calcium supplements, high serum phosphorus (≥ 3.9 mg/dL) was associated with high CAC scores, (OR: 3.33, 95% CI: 2.55–4.35, p‐trend < 0.001). No association was found for high intake of phosphorus (≥ 965 mg/daily). The strength of the study is the large sample size and the good control of confounding factors. The limitation of the study was the cross‐sectional design that impedes drawing conclusions of a possible causality.
Linefsky et al. (2011) in a cross‐sectional study investigated the association between serum phosphorous and calcific aortic valve disease (n = 1,938) (70% women, mean age 73 years) participants of the cardiovascular health study (after excluding 1,428 participants with prevalent CVDs, 948 with insufficient amounts of serum and 378 with missing echocardiogram). Serum phosphorous was measured in fasting serum using time‐rated colorimetric reaction with ammonium molybdate. Outcomes were aortic annulus calcitication (AAC) and aortic valve calcification (AVC), and mitral annular calcification (MAC). AVS was identified as aortic cusp thickening with normal aortic cusp, MAC was defined by an intense echocardiograph‐producing structure located at the junction of the atrioventricular groove and posterior mitral leaflet on the parasternal long‐axis, short‐axis or apical four‐chamber view. The presence of AAC was similarly defined as increased echodensity of the aortic root at the insertions of the aortic cusps. Following adjustment for age, sex, race, eGFR, hypertension, diabetes, smoking, body mass index, LDL cholesterol, HDL cholesterol, statin use, serum calcium levels and clinic site, high serum phosphorous (> 4.0 mg/dL vs < 3.0 mg/dL) was significantly associated with aortic valve sclerosis (OR: 1.64; 95% CI: 1.10, 2.43) and mitral annular calcification (OR: 1.62; 95% CI: 1.10; 2.38), but not aortic annual calcification (OR: 1.32; 95% 0.90; 1.92). Analyses using serum phosphorous as a continuous variable showed a significant association only for aortic valve sclerosis (OR: 1.17; 95% CI: 1.04; 1.31) per 0.5 mg/dL increase). Strengths of this study is the number of confounders included. The limitation of this study is the cross‐sectional nature as well as limited methodological information.
Park et al. (2016) investigated the association between serum phosphorous and coronary artery calcification in 2,509 (37% women, mean age 54 years old) patients undergoing coronary CT screening (after excluding those with eGFR below 60 mL/min* 1.73 m2, albuminuria and previous history of overt vascular events. Serum phosphorous was measured using a clinical analyser, coronary artery calcification was quantified as the Agatston Score on coronary CT. Following adjustment for age, sex, diabetes, hypertension, body mass index, systolic BP, corrected serum calcium, albumin, haemoglobin A1c, LDL cholesterol and HDL cholesterol, high serum phosphorous (> 4 mg/dL vs < 3.2 mg/dL) was associated with a higher risk of an Agatston score above 100 [OR 2.11 (1.34; 3.32)]. The main limitation of the study was the cross‐sectional design that impedes drawing conclusions of a possible causality.
Criqui et al. (2010) investigated risk factors of artery calcification in 1,974 out of 6,814 participants of the MESA (mean age 58 years old). Patients without complete CT scan and free of CVD at base‐line were excluded. Serum phosphorous was one risk factor and measured in 1,125 participants as part of an ancillary study, but no information about analytical methods or collection date were available, nor data on the composition of this subcohort, including calcification scores. Abdominal artery calcification was determined by electron‐beam CT scan, whereas coronary artery calcification was measured by either electron‐beam CT scan or multidetector CT, and the results used to calculate the Agatston score. At follow‐up, 552 participants had developed abdominal artery calcification, 813 coronary artery calcification and 997 had both. After adjustment for age, sex, ethnicity, smoking status, blood‐pressure, antihypertensive drug use, glycaemic status, HDL, LDL, lipid‐lowering drug use and calcium, there were no statistically significant associations between serum phosphorous and abdominal artery calcification (OR: 0.96; 95% CI: 0.79, 1.17] per SD [0.52 mg/mL] increase) or coronary artery calcification (OR: 1.11; 95% CI: 0.95; 1.31), although there was a statistically significant association between serum phosphorous and coronary Agatston score in a continuous model (ln(CAC + 1), β = 0.21; p < 0.01, per SD increase). The main limitation of this study was the lack of information on follow‐up time and the lack of information on the subcohort for whom serum phosphorous data were available. Results were also not adjusted for diet or physical activity.
Linefsky et al. (2014) within the US Multi‐Ethnic Study of Atherosclerosis (ARIC), a study was conducted (n = 6,814) to examine the association between phosphate metabolism biomarkers (serum phosphate, urine phosphate, PTH and FGF‐23) and aortic valve calcification (AVC). Eligible criteria for participating in the study was aged 45–84 years and being free from clinical CVD. Out of the 6,814 subjects initially enrolled, 5,145 subjects were free of AVC aortic valve calcification. Demographic data, medical history, smoking status and medication history and fasting blood and urine samples were collected from all subjects. BP, eGFR, total and HDL were also measured at baseline. Mean serum phosphate levels was 3.67 (SD = 0.52 mg/dL) and median urine phosphate level was 44.1 mg/dL (IQR: 24.9–67.7 mg/dL). During the follow‐up time (mean 2.4 years), 211 subjects developed AVC (4.1%). The mean eGFR was 99.81 (SD = 25.8) mL/min* 1.73 m2 in subjects free from AVC (n = 5899) and 86.33 (SD = 24.5) mL/min* 1.73 m2 in subjects with AVC at baseline. AVC prevalence was 13.2% and it was associated with higher phosphate levels (> 3.5 mg/dL). In the multivariate model, controlling for age, gender, ethnicity, study site, scanner type, BMI, BP, diabetes, smoking, LDL‐cholesterol, HDL‐cholesterol, 25‐hydroxyvitamin D, eGFR, albumin to creatinine ratio and serum calcium, an increased risk, although not statistically significant, was found between high serum phosphate levels (> 4.0 mg/dL) and incident of AVC (HR: 1.25; 95% CI: 0.90–1.72) and high urine phosphate levels (67.9 mg/dL) and incident of AVC (HR: 1.18; 95% CI: 0.94–1.49). No association between PTH (HR: 1.10; 95% CI: 0.95–1.08) and serum FGF‐23 pg/mL (HR: 1.10; 95% CI: 0.92–1.31, p‐trend = 0.29) and incidence of aortic valve calcification was found. The strength of the study was the prospective design and relatively large sample size and the limitations were the short follow‐up time, the inclusion of subjects not free of AVC at baseline and the lack of control in the models for diet and physical activity.
Arterial stiffness
Ix et al. (2009) within the MESA (Multi‐Ethnic Study of Atherosclerosis) study investigated the association between serum phosphorus and ankle‐brachial index in men and women (n = 1,370) In order to maximise the range of kidney function in the study sample., they selected all participants (n = 641) with an eGFR < 60 mL/min* 1.73 m2 and randomly selected 1,000 participants from the remainder of the cohort with higher GFR. Serum phosphorous was measured in morning serum obtained after an overnight fast using reflectance spectrophotometry. Arterial stiffness was assessed using ankle brachial index (ABI, calculated as ratio of leg and arm systolic BP), pulse pressure and large and small artery elasticity (using pulse wave analysis). After adjusting for age, sex, race/ethnicity, diabetes, smoking (ever), BMI, LDL, HDL, log triglycerides, eGFR, log CRP and log albuminuria, high serum phosphorous (> 4.0 mg/dL vs < 3.0 mg/dL) was significantly associated with high ABI (ABI > 1.3; OR: 4.6, 95% CI: 1.6; 13.2), but no statistically significant associations were found for other measured of arterial stiffness. The limitation of the study was the cross‐sectional design that impedes drawing conclusions of a possible causality.
Carotid artery intima‐media thickness
Onufrak et al. (2008) investigated the association between serum phosphorous and carotid IMT (cIMT) in 13,340 participants (57% women) of the community‐based ARIC. Participants were without known coronary heart disease, stroke or renal disease. Participants with eGFR above 150 mL/min* 1.73 m2 (n = 165) or below 45 mL/min* 1.73 m2 (n = 47) were excluded from the analysis. Dietary data (FFQ) were available for 10,688 participants. Serum phosphorous was measured in fasting blood samples. cIMT was determined by measuring the far wall of the common carotid artery, the bulb and the internal carotid artery bilaterally. Following adjustment for age, sex, race, diabetes, hypertension, total cholesterol, HDL and smoking status and eGFR, cIMT was significantly associated with serum phosphorous in a dose‐response manner (p‐trend = 0.003). The limitation of the study was the cross‐sectional design that impedes drawing conclusions of a possible causality.
Summary of the results of studies on serum phosphorus and other related outcomes
Kwak et al. (2014) conducted a cross‐sectional study (n = 23,652) to study the relationship between phosphorus intake and phosphorus serum levels and CAC and found that high serum phosphorus was associated with high CAC scores. Linefsky et al. (2011), in a cross‐sectional study investigated the association between serum phosphorous and calcific aortic valve disease and found that high serum phosphorous was significantly associated with aortic valve sclerosis and mitral anular calcification but not aortic anular calcification. Park et al. (2016) in a cross‐sectional study investigated the association between serum phosphorous and coronary artery calcification in 2,509 and found a higher risk of an Agatston score above 100 for those with high serum phosphorus levels. Criqui et al. (2010) in a cross‐sectional study investigated risk factors of artery calcification in 1,974 and found no statistically significant associations between serum phosphorous and abdominal artery calcification or coronary artery calcification, although there was a statistically significant association between serum phosphorous and coronary Agatston score. Linefsky et al. (2014) in a cross‐sectional study (n = 6,814) examined the association between phosphate biomarkers (serum phosphate, urine phosphate, PTH and serum FGF‐23 and AVC and found no statistically significant association between high serum phosphate and urine phosphate levels and incident of AVC. Arterial stiffness was assessed using ABI, calculated as ratio of leg and arm systolic BP), pulse pressure and large and small artery elasticity (using pulse wave analysis and found that high serum phosphorous was significantly associated with high ABI‐IX 2009 (Onufrak et al., 2008) investigated in a cross‐sectional study the association between serum phosphorous and cIMT and found a statistically significant association, with a dose–response, between serum phosphorus and cIMT, with a dose‐response.
Overall, because of the cross‐sectional nature of all studies, the results finding an association between phosphorus serum levels and vascular calcification are uncertain and firm conclusion cannot be drawn.
3.6.3. Studies on urinary phosphorus/phosphate and cardiovascular‐related outcomes19
Cardiovascular diseases and mortality
In 880 patients with stable CVD and normal kidney functions, serum phosphorus excretion were measured and the participants were followed for 7.4 years. Cardiovascular events and all‐cause mortality were recorded (Palomino et al., 2013).
Urinary phosphorous excretion has been investigated as surrogate marker of phosphorous intake (Trautvetter et al., 2018), and it has been suggested that it can be used to estimate actual intake (Morimoto et al., 2014), but the data available are very limited. Human intervention studies (see below) suggest that urinary phosphorous excretion mainly reflects acute changes in intake and not long term, habitual intake.
The results of the study by Palomino are therefore not suitable to assess the risk of phosphorous intake.
3.6.4. Overall conclusion
there is insufficient evidence to link dietary phosphates intake to cardiovascular outcome.
there is some evidence to link serum phosphorus and CVDs incidence and some evidence to link serum phosphorus and cardiovascular mortality. However, serum phosphorus cannot serve as surrogate for phosphorus intake and studies did not control for important confounding factors.
the link between phosphorus serum levels and vascular calcification seen in cross sectional studies does not allow drawing conclusions of a possible causality due the limitation of the study design.
3.7. Epidemiology studies on bone health
Few epidemiological studies investigated the role of phosphate on bone health in the general healthy population. Cross‐sectional studies were not included in the evaluation.
Tucker et al. (2006) within the Framingham Osteoporosis study (1,413 women and 1,125 men) showed that cola‐flavoured carbonated beverages containing phosphate were associated, in a dose response manner, with BMD in women but not in men. BMD was measured using dual‐energy X‐ray absorptiometry (DXA) at the right hip and the lumbar spine. After controlling for confounders such as BMI, smoking, alcohol use, age, physical activity, calcium, vitamin D, caffeine intake from other sources other than cola and oestrogen use, negative linear associations were seen for cola consumption and BMD at each hip site femoral neck, ward's area trochanter, but not the spine, in women (p < 0.001). After stratifying the consumption of colas by caffeine content (caffeinated/decaffeinated), the effect remained only for ward's area but not for other hip. No association was seen between non cola‐flavoured carbonated beverage consumption and BMD. In this study, total dietary phosphorus intake was not different from daily cola‐flavoured carbonated beverage consumers and no cola‐flavoured carbonated beverage consumers but the calcium‐to‐phosphorus ratio was lower.
Campos‐Obando et al. (2017) combined data (n = 23,412) from two cohorts studies (Dutch Rotterdam study and the US Osteoporotic Fractures in Men study) to investigate the relation between serum phosphorus and incidence of fractures (self‐reported in the US study and measured by X‐ray in the Dutch Rotterdam study). In the pool analysis, serum phosphate was inversely associated with lumbar BMD measured by DXA in men (β = −0.06; 95% CI: −0.11 to −0.02) but not in women, after controlling for age, BMI, smoking and race. In the combined data analysis, after 6.6 years of follow‐up a total of 1,825 fractures were recorded. In the multivariate analysis, adjusting for age, body mass index, smoking, serum levels of calcium, potassium, 25‐hydroxyvitamin D, eGFR, phosphate intake, PTH, FGF‐23 levels and phosphate levels (1 mg/dL increase), an elevated risk of fractures was observed for both women and men (HR: 1.47; 1.31–1.65) When the analysis was conducted using phosphate in quintiles (Q5 = 3.8 mg/dL), a dose–response was observed between serum phosphate and all types of fractures. Limitations of the studies were the outcome variable used in the US study (self‐report) and the lack of control in both studies for physical activity and other potential confounders.
In summary, in the study of Tucker et al. (2006) the effect of phosphate on BMD was seen only in women, but not in man, consuming cola‐flavoured carbonated beverages containing phosphate, while in the study of Campos‐Obando et al. (2017) the effect of serum phosphorus on BMD was observed only in men and for lumbar spine BMD but not femoral neck BMD. In the study of Campos‐Obano that investigated also the effect of serum phosphorus on the incidence of fractures, an increased risk of fractures was observed for both sex in a dose‐response manner.
It is important to note that phosphate serum level is not considered to be appropriate to estimates phosphates intake. Therefore, more data on actual intake to assess the impact of phosphate intake on bone density and fractures are needed, in agreement with Vorland et al. (2017).
In conclusion, despite the effect of a high phosphorus intake on the activity of calcium‐phosphate metabolism regulating hormones, there is insufficient evidence for an association between dietary phosphate intake and pathologically reduced BMD which is in accordance with evaluation from the NDA Panel (EFSA NDA Panel, 2005). There is also insufficient evidence for an association between serum phosphate and incidence of fractures.
3.8. Human studies
The Panel noted that in all human case reports and interventional studies the customary dietary phosphate intake was not reported and therefore the dose estimate only relates to supplementary phosphates intake observed in case reports or given in the clinical interventional studies.
3.8.1. Effects on kidney
Case series and case reports after acute administration
Publications were identified by a systematic literature search in which nineteen case of acutely severely impaired renal function are described after administration of phosphate as a treatment for bowel cleansing in preparation for colonoscopy (Fine and Patterson, 1997; Vukasin et al., 1997; Orias et al., 1999; Markowitz et al., 2004; Gonlusen et al., 2006; Santos et al., 2010; Cakar et al., 2012; Arikan et al., 2013).
For 15 of the patients, the dose was reported and the lowest dose which was causally related to an impairment of renal function was reported as 11,600 mg/day, in most cases consisting of two 5,800 mg doses taken 12–24 h apart (see Appendix P). In some of the cases, the patients recovered but, in several cases, renal impairment persisted and leading to CKD. One patient died. It is to be noted that many patients had an advanced age and pre‐existing pathological conditions, e.g. hypertension. However, when baseline creatinine values have been measured, they resulted in the normal range (Aasebø et al., 2007).
The Panel noted that acute doses of phosphorus of 11,600 mg (165.7 mg/kg bw) given within 12–24 h can have deleterious effects on the kidney in some patients, in particular in the elderly (Study n. 2 in Appendix F; all but one patient were older than 55 years).
Histopathological evaluations of kidney specimens were published from patients with acute phosphate nephropathy after intake of phosphate salts as a treatment for bowel cleansing. The histological findings clearly showed calcium‐phosphate crystals deposits within the cytoplasm of tubular epithelial cells and within tubular lumina (Aasebø et al., 2007; Vervaet et al., 2009; Markowitz and Perazella, 2009).
Interventional studies with short–term exposure
In seven clinical intervention studies with short‐term exposure towards phosphorus, no impaired renal function was mentioned (see Appendix Q). The doses varied between 660 mg phosphorus and 2,500 mg phosphorus daily (11–40 mg P/kg bw/day) and the duration of the treatment was between 1 day and 14 days. The number of study participants encompassed 6–20 subjects.
Interventional studies with long‐term exposure
Fifteen clinical studies were identified by a literature search in which subjects were exposed at least 1 month up to 2 years to phosphate (see Appendix R). The number of included subjects was small (between 5 and 13 subjects) with the exception of two studies in which 25 subjects (Ettinger, 1976) and 47 subjects (Miller et al., 1991) were treated. Doses between 350 and 7,200 mg/day phosphorus were given, mostly by the oral route with the exception of two studies where phosphorus was given by the intravenous route. The doses were an add‐on to the phosphorus intake by the normal diet. In 14 of the 16 studies, the daily dose was at or below 2,000 mg phosphorus/day (28.6 mg/kg bw per day) and no influence on the renal function was described. The number of patients from all studies was 200.
In the clinical interventional trial of Dudley and Blackburn (1970), nine patients, age 35–71 years, were studied in a variety of conditions [hyperparathyroidism (4 patients); multiple myeloma (1 patient); renal calculi (4 patients)]. The patients received daily doses between 2,250 (32.1 mg/kg per day) and 4,500 mg daily (64.2 mg/kg per day) (one patient 2,250 mg/day, 7 patients 3,375 mg/day and 1 patient 4,500 mg/day) over a period of 9–87 months. In this study, creatinine clearance decreased in 2 patients (dose 4,500 mg/day for 78 months and 3,375 mg/day for 42 months). In all, but two patients (dose 2,250 mg daily for 16 months and 87 months, respectively) calcification in tissues were noted.
In the clinical interventional trial of Bernstein and Newton (1966), 10 patients, 16–69 years old, received phosphorus for studying its effect on kidney stone formation. 4 patients received 2,400 mg, 5 patients 4,800 mg and 1 patient 7,200 mg phosphorus daily for 4–24 weeks. At the end of the treatment period, in the dose group of 2,400 mg phosphorus daily, one patient had slightly reduced renal function; in the dose group of 4,800 mg phosphorus daily two patients had a reduced renal function and in the highest dose individual (7,200 mg phosphorus daily) creatinine clearance reduced to 50% of the pre‐treatment value.
The Panel noted that in clinical trials daily doses up to 2,000 mg phosphorus (28.6 mg/kg bw per day) given over several months up to 2 years were tolerated without impairment of the renal function, whereas doses of 4,800 mg/day (68.6 mg/kg bw per day) and higher elicited renal impairment.
A meta‐analysis of the studies with the aim to construct a dose–response relationship is hampered by the differing design, the differing duration, the low number of subjects per dose group and the insufficient reporting of study details. Nevertheless, these studies can give valuable information on the tolerability of phosphate doses in humans.
3.8.2. Effects on the gastrointestinal tract
In several of the clinical studies, it was noted that the subjects had soft stools or diarrhoea. In the study of Brixen et al. (1992) which was a short‐term study of 7 days duration, 2 of 19 patients receiving 750 mg/day (10.7 mg/kg bw per day), 3 of 19 patients receiving 1,500 mg/day (21.4 mg/kg bw per day) and 7 of 20 patients receiving 2,250 mg/day (32.1 mg/kg bw per day) complained of gastrointestinal side effects. The Panel noted that the described effect is not to be seen as adverse but is classified as discomfort. However, when higher doses are given, such as the doses for bowel cleansing in preparation for colonoscopy (11,600 mg/day or 165.7 mg/kg bw) these doses acted as a cathartic agent and this effect has to be clearly seen as adverse.
3.8.3. Effects on PTH
Studies showing that phosphates intake induce PTH elevation are available (Reiss et al., 1970; Bell et al., 1977; Silverberg et al., 1986; Calvo and Heat, 1988; Calvo, et al. 1988; Calvo et al., 1990; Brixen et al., 1992; Kärkkäinen and Lamberg‐Allardt, 1996). The studies were of short duration, mainly in young adults, and long‐term studies measuring fractures incidence or bone density changes are lacking.
3.8.4. Effects on blood pressure
In an experimental interventional study in healthy subjects, Mohammad et al. (2018) investigated the influence of 6 weeks phosphorus intake in a dose of 17.15 mg/kg bw per day on top of the normal diet compared to a control group without additional phosphorus intake on a plethora of endpoints. Further treatment of 5 weeks was administered after a single intramuscular injection of vitamin D3 (600,000 U). An increase in P in serum was observed from 1.1 mmol/L to 1.3 mmol/L (week 6) and 1.4 mmol/L (week 11) in the group loaded with phosphorus with a corresponding elevation of urinary excretion of P. From further endpoints studied, FGF‐23, Klotho and PTH were increased at week 6 as was urinary Klotho the values returning to normal within the next 5 weeks under treatment. Related to the administration of vitamin D3 serum 25(OH)D and serum 1,25(OH)D were elevated in both groups.
Mean 24‐h systolic and diastolic BP as well as heart rate were increased in the phosphorus exposed group. The mean increase was 4 mm Hg (systolic) and 3 mm Hg (diastolic) and the pulse rate increased from 68 to 72 beats/min. Metanephrine and normetanephrine excretion in the urine was increased but within the reference range.
Further 41 parameters were measured and only the sodium excretion in both groups in urine was elevated due to the administration of phosphorus as sodium salt and of sodium in the control group. It is to be noted that none of the three parameters of endothelial function and arterial elasticity were changed by the phosphorus treatment.
The authors claim that the elevations of BP and pulse rate are caused by an elevated adrenergic activity. However, there is no physiological explanation and basis by which mechanism phosphorus intake may act on BP and pulse rate. Unfortunately, the authors did investigate only one single dose level of phosphorus which precludes drawing conclusions on the influence of higher and lower doses of phosphorus on the BP. A further shortcoming of the study is that the intake of phosphorus by the diet was not controlled by a dietary questionnaire and although some information can be drawn from the urinary concentration of phosphorus the amount of phosphorus excreted is not given in the publication. Although this publication is of interest, further confirmation of the findings is necessary and further dose levels have to be investigated.
3.9. Special populations – Infants below the age of 16 weeks
Sometimes in addition to natural phosphate content phosphates are added to infant formulas food for special medical purposes (FSMP) either for technological reasons and/or for its nutritional role (see Section 1.2). Special physiology and relevant toxicological and clinical studies are reviewed in the SNE publication (https://www.specialisednutritioneurope.eu/sne-literature-review-on-phosphates). A summary based on this document is given here.
Several clinical studies in infants consuming infant formula or FSMP with added phosphate have been performed. The outcomes investigated in these studies are generally effects on growth and/or on serum inorganic phosphate levels.
Most of these studies have investigated the effect of added phosphate (phosphoric acid, sodium phosphate, potassium phosphate or calcium phosphate) on growth parameters (including body weight, length and head circumference). These studies involved more than 2,600 infants and ranged in duration between 16 weeks and 1 year. In all studies, there were no statistical differences in the growth of the infant cohorts fed the various formulae from those of breast‐fed infants and their growth matched the WHO growth standards.
There are a limited number of studies that assess the effect of formulas with or without added phosphate on serum inorganic phosphate concentration. Most of the studies have investigated the effects of formula not containing any added phosphate but where the phosphorus comes from natural presence in the milk ingredients. These studies indicate that infants fed formula have somewhat higher serum inorganic phosphate concentration than breastfed infants. However, the average serum inorganic phosphate concentration in formula‐fed infants is within the normal reference range for serum inorganic phosphate laboratory values for infants.
Few studies have been performed where the effect on serum inorganic phosphate concentrations of infant formula with added phosphate has been investigated. Despite high phosphorus concentration in the supplemented formula the infants receiving this formula did not have higher serum inorganic phosphate concentrations
In conclusion, clinical studies in infants who consume either standard infant formula or FSMP with added phosphates demonstrate that the important clinical outcome, growth, is similar to WHO growth standard. This observation demonstrates that the addition of phosphates within the regulatory limits is of no concern. Furthermore, any adverse effect contributed to added phosphates would be through increased serum inorganic phosphate concentration. As demonstrated in a clinical study with high phosphorus, content in infant formula did not result in any significant increase of serum inorganic phosphate, which still fell within the normal range.
3.10. Mode of action, derivation of a phosphate‐specific adjustment factor and derivation of ADI
3.10.1. Mode of action
Since nephrocalcinosis and/or tubular‐interstitial nephropathy were identified as common endpoints in human and animal studies whereas bone and cardiovascular endpoints could not be confirmed as relevant for healthy human population in epidemiology studies, the only mode of action of interest concerns the effects on kidney.
Key events: In the process of renal excretion, phosphate is freely ultrafiltrated through glomerular barrier and reabsorbed in the proximal tubule by sodium‐dependent transporters. When phosphate ultrafiltrate load exceeds the reabsorption capacity of the proximal tubule, the delivery of phosphate to the distal renal tubule increases disproportionately. As a consequence, calcium‐phosphate concentration increases within the distal tubular lumen, up to formation of Ca‐P crystals. It is important to note that this can occur in the distal tubule and in the collecting ducts, and that calcium‐phosphate solubility is also a function of luminal fluid pH. In normal conditions, the pH values changes from 7.4 in the Bowman capsule to 6.6 in the distal tubule, a difference which does not strongly influence the solubility of calcium phosphate (see Section 3.1.1). Concerning the tubular fluid volume, another factor influencing phosphate solubility, it reduces along the tubular transit. When we compare the processes in man and rat, it can be assumed that the production of the urine is guided by the same principles. However, quantitative differences are evident. The estimated median volume of primary urine is 4.4 L /kg bw per day in the rat (Pestel et al., 2007) and 2.16 L/kg bw per day in man (range 1.60–2.8 L/kg bw per day; 5th to 95th percentile) (Poggio et al., 2009). The volume of urine excreted from the bladder is 67.8 ± 16 mL/kg bw per day in rats (Shevock et al., 1993) and 33.5 mL/kg bw per day in man (ICRP, 2002). According to these data, the rat produces twice the volume of the primary urine than a human and excretion of the urine volume from the bladder is similarly twice in rat compared to man. Hence, it can be assumed that along the lumen in the tubule and in the collecting duct of the kidney the volume in rat is twice of that in man. The volume of urine plays a deciding role as the concentration of calcium phosphate and its solubility depends on its volume. At the rat NOAEL for added phosphate with a daily dose of 76 mg/kg bw, the concentration in the primary urine and along the renal tubules is twice in humans compared to rat because the volume of the urine in humans is a factor 2 lower than the urine volume in rats.
Concordance of the key events in man and animal: In several short‐term and subchronic rat studies, the endpoint calcification in the kidney has been observed in a dose‐dependent manner with different phosphates (Chow et al., 1980; Mars et al., 1988; Ritskes‐Hoitinga et al., 1989; Seo et al., 2011). The effect has also been observed in dogs (Schneider et al., 1981). The most reliable NOAEL from the short‐term and subchronic studies was 500 mg/kg bw per day, corresponding to 116 mg/kg bw per day phosphorus in a 90‐day study (Seo et al., 2011). In chronic rat studies, calcifications in the kidneys and tubular nephropathy was observed with NOAELs of 250 mg/kg bw per day with sodium triphosphate, corresponding to 63 mg/kg bw per day phosphorus and 250 mg/kg be per day sodium hexametaphosphate, corresponding to 76 mg/kg bw per day phosphorus (Hodge, 1959, 1960). The human interventional studies indicate that a dose of 2,000 mg/day (corresponding to 28.5 mg/kg bw per day) may be without an effect on the kidney function (references see Appendix Q). The mechanism and its key events are confirmed to be also relevant for humans by comparison of the histopathological changes described in the animal studies and in some publications describing the histopathology in human renal specimens. In these specimens, calcium phosphate crystals precipitate predominantly in the distal tubule and collecting duct in patients with renal damage due to high intake of phosphate (Aasebø et al., 2007; Markowitz and Perazella, 2009; Vervaet et al., 2009). In addition, following high acute phosphate exposure renal tissue histology shows tubular atrophy and interstitial fibrosis that are signs of an irreversible chronic damage. It is likely that the persistence of crystal deposition within tubules prevents recovery of the acute damage leading to fibrosis (Markowitz et al., 2004). Vervaet et al. (2009) have investigated the fate of the crystal deposits in the renal tubule and observed overgrowth of the crystal deposits in the tubule, translocation into the interstitium and followed by inflammation and fibrosis. These histopathological changes are described in the Section 3.10.2 (derivation of ADI).
Temporal association: The key events, calcium‐phosphate crystal formations in the distal tubules in the kidneys and impaired kidney function, are observed in humans with a temporal relationship to the intake of phosphate which depends on the dose. There are case reports indicating that acute renal failure was elicited with a single extremely high dose (160 mg/kg bw and more) whereas up to 2,500 mg/day (35.7 mg/kg bw per day) phosphorus (short‐term exposure of up to 2 weeks) had no effect and calcifications were noted with a dose of 32.1 mg/kg bw per day in a long‐term administration. As pointed out in Section 3.8, the dose of phosphorus is in addition to that found in the normal diet.
Strength, consistency and specificity of association of toxicological response with key events: There are no alternative mechanisms explaining the observed calcifications in the kidney and kidney impairment after phosphate exposure.
Biological plausibility and coherence: The observed effect is the consequence of the exposure of the kidney as it is the only excretory organ for phosphate with a salt that will deposit in the event of saturation. The effect is plausible and explained by physicochemical properties and the biology of the urine production in mammalia.
Uncertainties, inconsistencies and data gaps: The induction of precipitates in the kidney following exposure to calcium phosphate is well established. Clear dose responses have been reported in rats exposed to phosphates and in some human studies. In all the studies the dose of phosphorus is in addition to that found in the normal diet. Solid information on the phosphorus content of the feed could be retrieved for one of the rat studies (personal communication, Purina Korea, January 2019). Uncertainty and inconsistencies are very low concerning mode of action.
3.10.2. Derivation of a chemical‐specific adjustment factor for phosphate
The evidence from epidemiological and human interventional studies is not suited to derive an ADI. In the epidemiological studies in which effects were seen concentrations of phosphorus in plasma/blood were related to the effects. However, plasma/blood phosphorus levels cannot be converted into dietary phosphorus exposure rendering the information on concentration–effect relationship unsuitable for the derivation of an ADI. The human interventional studies had major deficiencies as explained in Section 3.8.1. Therefore, evidence provided in the animal models has to be the basis for derivation of the ADI.
In this respect, it is important to note that the effects on kidney are consistent between humans and animals. The Panel considered which uncertainties factor would be appropriate and the Panel decided that the data are sufficient to derive and apply a chemical‐specific adjustment factor for phosphate instead of the default factor of 100. Whereas the term uncertainty factor is used when the default value of 100 is used to convert the NOAEL into an ADI value, the term ‘adjustment factor’ is appropriate in cases where a substance specific factor (here: phosphate specific factor) is derived and used.
The default uncertainty factor of 100 is composed of a factor of 10 accounting for the interspecies differences between test species and humans and a second factor of 10 accounting for the interindividual differences in the human population. The two factors allow for interspecies differences and human variability in TK differences and toxicodynamics (TD). For the TK component of the interspecies factor, a value of 4 is then used when the extrapolation is made from the rat to the human (EFSA SC 2012 guidance on default value reference). This factor of 4 is based on allometric scaling from rat to humans. The remaining factor of 2.5 is attributed to the interspecies differences in TD. The uncertainty factor for interindividual differences has been further subdivided into two factors of 3.2 to allow to account for TK and TD differences. Whereas the factor of 10 describes the variability in the human population well as can be taken from an analysis of variability of doses of drugs, the subdivision into the two factors of 3.2 is not well supported by data.
In 2005, the IPCS/WHO proposed a framework indicating how chemical‐specific TK and/or TD data can be used to replace the default factors or its subfactors. In line with the suggestions and following the extended approach as described in the IPCS/WHO document (2014), the quantitative analysis of the mode of action can aid to develop chemical‐specific adjustment factors allowing for (interspecies and interindividual differences in TK and TD processes and their applications in chemical risk assessment has been recently reviewed (Bhat et al., 2017). The adverse effect of phosphate is due to the physico‐chemical properties of calcium phosphate, the solubility, which is a substance property and is not species‐specific. Hence, the TD part of the interspecies factor can be reduced to 1. With regard to the ‘kinetic’ part of the interspecies factor the renal handling of phosphate has to be considered. Phosphate is excreted by glomerular filtration and tubular reabsorption occurs, in both rats and humans. The solubility depends on the concentration of calcium phosphate which depends on the phosphate dose and the volume of the urine.
A chemical‐specific adjustment factor for phosphate for interspecies differences in TK: the difference of the volume of the primary urine is the main determinant for the volume of urine in the tubule where calcium phosphate precipitation occurs and can be calculated for rat and humans. The estimated median primary volume is 4.4 L/kg bw per day ± 0.88 in the rat (Pestel et al., 2007) and 2.16 L/kg bw per day in man with a range of 1.60–2.8 L/kg bw per day (5th–95th percentile) in healthy kidney donors (Poggio et al., 2009). The ratio of the median glomerular filtration rate between rat and human (4.4 L/kg per day divided by 2.16 L/kg bw per day) equals 2. A ratio of 2 between rat and man results also from the volume of urine excreted from the bladder which is 67.8 ± 16 mL/kg bw per day in rats (Shevock et al., 1993) and 33.5 mL/kg bw per day in man (International Commission on Radiological Protection (ICRP), 2002).
From these data, we derived a phosphate‐specific adjustment factor allowing for interspecies differences in TK of 2 giving phosphate‐specific adjustment factors for interspecies differences of 2 (2(TK) × 1(TD)) (see Figure 2).
Figure 2.
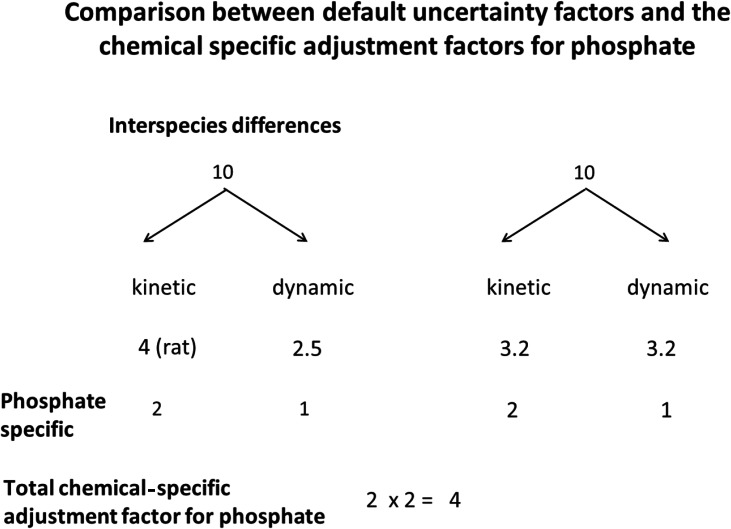
Comparison between default uncertainty factors and the chemical specific adjustment factors for phosphate
A chemical‐specific adjustment factor for phosphate for interindividual differences in TK: the same argument as for the TD interspecies subfactor is applicable for TD subfactor in humans which therefore is 1. For TK processes, creatinine clearance reflects the physiology of renal filtration of endogenous substances and xenobiotics and the normal range of healthy clinical values for adults and elderly are between 60 and 120 mL/min, with 90 mL/min often considered as the reference for creatinine clearance. Taking the ratio between the mean creatinine clearance (90 mL/min) and the lower end of the range (60 mL/min) gives a value of 1.5 (giving a ratio of 1.5 The Panel decided to increase this factor allowing for interindividual differences in TK to a value of 2 to provide a conservative estimate particularly to further take into consideration the healthy elderly population Hence, the phosphate specific adjustment factor for interindividual differences in TK was set a value of 2.
The composite phosphate specific adjustment factor accounting for interspecies and interindividual differences in TK and TD is then 2 × 2 = 4.
3.10.3. Minimum and maximum levels of phosphorus for infant formula (infants below the age of 16 weeks) and for infant formula for special medical purposes
For the age group of the infants below the age of 16 weeks, the special physiology of phosphate has to be considered. As pointed out in the introduction part of Section 3.5 the plasma levels of phosphate are twofold higher in the first 6 months of life compared with the adult plasma level indicating that the regulation of the plasma level is different in this age group compared to the adult man.
By regulation, the minimum and maximum total levels of phosphorus for infant formula are set at 25 mg/100 kcal and 90 mg/100 kcal, in the case of infant formula based on soy the maximum level is 100 mg/100 kcal. The minimum and maximum levels for infant formula for special medical purposes are set at 25 and 100 mg/100 kcal (Commission Delegated Regulation (EU) 2016/127 and Commission Delegated Regulation (EU) 2016/128, as well as Commission Directive 2006/141/EC and Commission Directive 1999/21/EC). These limits mean that at the high level consumption of 260 mL/kg bw per day by infant formula and by FSMP for infants (as calculated by EFSA, 2017) the exposure would be approximately between 44 and 175 mg/kg bw per day for phosphorus irrespective of whether phosphorus is delivered from the formula as nutrient or as food additive.
4. Discussion
Phosphates are normal constituents in the body and are regular components of the diet; however, no Tolerable Upper Intake Level (UL) (EFSA NDA Panel, 2005) has been established but in 2015 the NDA Panel set Adequate Intakes (AIs) values for various age groups.
In the context of this opinion, the Panel was in the special situation to derive an ADI for a substance which at the same time is a nutrient and a food additive. The ADI is the acceptable daily intake of a substance by exposure to phosphates from all sources including those naturally occurring in the diet, food additives and water.
4.1. Technical data
According to Commission Regulation (EU) No 231/2012, calcium dihydrogen phosphate (E 341(i)), calcium hydrogen phosphate (E 341(ii)), tricalcium phosphate (E 341(iii)), dimagnesium phosphate (E 343(ii)) and dicalcium dihydrogen diphosphate (E 450(vii)) are described as ‘insoluble in water’ or ‘sparingly soluble’. However, information from other sources indicates that tricalcium phosphate (E 341(iii)) is soluble in water at 25°C (2.5 mg/100 g H2O), and calcium dihydrogen phosphate (E 341(i)) is soluble in dilute hydrochloric acid (US National Library of Medicine, https://pubchem.ncbi.nim.nih.gov). Their solubilities in the gastrointestinal tract are not known especially given the presence of other dissolved ions and differences in pH that may be encountered. Thus, insoluble particles of these phosphate salts could theoretically be present within the gastrointestinal tract. It is conceivable that a small proportion of these particles may be in the nanorange. Based on the information received on the particle size of these phosphates, the Panel cannot exclude that particles in the nanorange can be present in phosphates when used as a food additive and, therefore, identified the need for additional information.
There are few validated official methods available for the determination of phosphates in foodstuffs permitted to contain phosphate additives in the EU. Those identified to date are summarised with standard methods listed by BVL (BVL, 2018) in Table 2. The scope of these methods covers ortho‐, condensed and polyphosphate analytes, and most foodstuffs and beverages apart from those for infants (e.g. infant formula). The analytical techniques described in these methods are essentially limited to TLC and/or spectrophotometry, except for IC which is specified for the analysis of soft drinks. Data provided by CEFIC‐PAPA provide evidence for the accuracy and precision requirements of standard methods for phosphate determination. For example, the total phosphorus is calculated as g/100 g reported to two significant figures (Documentation provided to EFSA n. 11). The Panel therefore identified the need for the development of analytical methods for phosphates in the range of foods permitted to contain them.
When considering the information submitted by the industry on the actual aluminium content in infant formula (final food), the Panel noted that the amount of aluminium may result in an exceedance of the respective TWI.
The Panel noted that the use of calcium phosphate (E 341), for which maximum limits for aluminium have been set in the EU specifications, can contribute to the total aluminium content in infant formula.
4.2. Kinetics
In humans, phosphorus deriving from food additives is mainly absorbed as free orthophosphate. The amount of orthophosphate absorbed from food additives is about 80–90%. No metabolism takes place and excretion is via the kidney through glomerular filtration and tubular handling. Data are available on the kinetics of disodium diphosphate, trisodium diphosphate, tetrasodium diphosphate and tetrapotassium diphosphate but not on dicalcium diphosphate and calcium dihydrogen diphosphate.
In animal models, the kinetics of phosphate are generally the same as in humans.
4.3. Animal toxicity data
There is a large number of toxicity studies on phosphates primarily in rats and mice but also in other species such as dogs, guinea pigs and hamsters
Data were not always available for all the authorised phosphates for all endpoints but the Panel considered possible to perform read‐across between different phosphate additives.
Most studies are not performed according to the current guidelines and standard (OECD). The available data is however robust enough to be used to assess the safety of phosphates in animals and for NOAEL estimation.
For certain phosphate species added to feed, the number of water molecules were not specified. In these cases, the calculation of P content has been based on the anhydrous form.
It is clear from the available data that none of the phosphates are genotoxic in vitro or in vivo and that they are not carcinogenic. Furthermore, they do not present any risk for reproductive or developmental toxicity.
The only significant adverse effect observed with phosphates in standard toxicity studies is related to calcification of the kidneys and tubular nephropathy. These adverse effects are observed in acute, short‐term, subchronic and chronic toxicity studies and in all species tested. The underlying mechanism behind these effects has been described in the mode of action (Section 3.9). As the renal effects are due to excess phosphate load and not to a direct effect of the cation and since all phosphate additives (E 338–341, E 343, E 450–542) are converted to orthophosphate, it is expected that all classes and structures of the phosphate additives would produce the same critical effects at high doses. Therefore, a single NOAEL can be established for all phosphates used as food additives. The NOAELs varied between the studies and phosphates tested but the reason for this variation is probably primarily due to doses of phosphates chosen and to spacing of the doses. Dietary factors, such as calcium and phosphate levels in the diet, may also contribute to the variability. Information regarding phosphate and calcium levels in the diets used are lacking in a most studies.
NOAELs and lowest‐observed‐adverse‐effect‐levels (LOAELs) could be identified from short‐term, subchronic and chronic toxicity studies in rats. In subchronic studies, the highest reliable NOAEL relating to effects in the kidney was 500 mg/kg bw per day (corresponding to 116 mg P/kg bw per day), derived from a 90‐day rat study with tetrasodium diphosphates performed according to OECD guidelines. The lowest phosphate level leading to effects on the kidney can be estimated to be approximately 1,000 mg/kg bw per day (corresponding to 233 mg P/kg bw per day) in the same study. In chronic toxicity studies, reliable NOAELs could be identified from two 2‐year studies, 250 mg/kg bw per day (corresponding to 63 mg P/kg bw per day) and 250 mg/kg bw per day (corresponding to 76 mg P/kg bw per day) with sodium triphosphate (corresponding to pentasodium triphosphate) and sodium hexametaphosphate (corresponding to soluble sodium polyphosphate), respectively. The lowest level of phosphate causing an effect in the kidney was approximatively 750 mg/kg bw per day (corresponding to 229 mg P/kg bw per day) in a 2‐year study with sodium metaphosphate.
In conclusion, the only significant adverse effect of phosphates in animals is nephrocalcinosis and tubule‐interstitial nephropathy. The onset and progression of these effects appears quite rapid and the NOAELs and LOAELs for derived from subchronic and chronic studies are in the same range.
Although studies in animals report that high phosphorus intake causes bone reabsorption or decreased bone formation, the Panel considered that effects observed on bone metabolism and bone mineralisation in animals are not well characterised enough to derive an association with dietary high phosphate intake.
4.4. Epidemiology
The epidemiological studies reviewed here did not find consistent associations between dietary phosphorous intake and cardiovascular‐related outcomes; all studies had important limitations such as the lack of control for important confounding factors (e.g. diet and physical activity). In addition, the use of food composition databases which might not include data on all phosphates used as food additives might lead to underestimation of the total phosphate intake. A further limitation is the considerable variability of phosphorus content in many foods depending on a number of factors such as food seasonality (Poulsen et al., 2015) and bioavailability of phosphorous from different sources (Karp et al., 2012). These factors make an accurate assessment of internal exposure from dietary sources unreliable.
Moreover, a single‐day dietary record is unlikely to be representative of usual individual intake, especially for phosphorus. Multiple dietary records are necessary for assessing micronutrients. The misclassification of food intake can attenuate observed associations between intake and disease risk, and therefore risk estimates are biased towards the null.
Most studies reviewed using serum phosphorus concentration as a measure for exposure found an increase in risk for CVDs with high serum phosphorous concentrations (3.4–4.5 mg/dL). However, the concentrations observed were generally within the reference range (2.7–4.5 mg/dL). It is however important to be aware of the fact that serum phosphorus levels are influenced not only by diet but also by various metabolic factors. Although Moore et al. (2015) suggested that serum phosphorous concentrations are more sensitive to phosphate additives, the association between dietary intake and serum phosphorous is weak (R2=0.03 in multivariable model including kidney function, BMI and albumin‐to‐creatinine ratio). In contrast, serum phosphorous concentrations change considerably throughout the day and follow a circadian rhythm (Ix et al., 2014), and these changes are affected by diet in a non‐dose‐response way. For example, phosphorous supplementation can affect the 24‐h mean phosphorous concentration but it does not affect the serum concentration after an overnight fast (Portale et al., 1987). Moreover, serum phosphorous cannot be used to distinguish between different dietary phosphorous sources. Serum phosphorous concentration is therefore not a suitable surrogate marker of phosphorous intake, but rather a marker of other physiological processes. In summary, the results from epidemiological studies reviewed do not provide reliable information to assess the impact of phosphorous on CVDs.
Only two epidemiological studies investigated the role of phosphate on bone health in the general healthy population.
In the study of Tucker et al. (2006) the effect of phosphate on BMD was seen only in women, but not in man, consuming cola‐flavoured carbonated beverages containing phosphate while in the study of Campos‐Obando et al. (2017) the effect of serum phosphorus on BMD was observed only in men and for lumbar spine BMD but not femoral neck BMD. In the study of Campos‐Obano that investigated also the effect of serum phosphorus and incidence of fractures, an increased risk of fractures was observed for both sexes, in a dose‐response manner.
In summary, the results of these two studies do not provide sufficient and reliable data to assess the role of phosphate on bone health. More data on actual intake to assess the impact of phosphate intake on bone density and fractures are needed.
Studies showing that high phosphates intake induces PTH elevation are available (see Vorland et al., 2017). The studies were of short duration, mainly in young adults, and long‐term studies measuring fractures incidence or bone density changes are lacking.
4.5. Case reports and clinical data in humans
Several case reports indicate that a high acute single dose of phosphate (160 mg/kg bw and more) can induce renal impairment.
Clinical interventional trials in which the doses were given on top of the normal diet were performed over several months. No impairment of the renal function was reported with daily doses up to 2,000 mg phosphorus (28.6 mg/kg per day) whereas doses of 4,800 mg/day (68.6 mg/kg per day) elicited renal impairment. Histopathological examinations of human kidney specimens from exposed patients showed similar findings as seen in animals. In several of the studies using phosphorus doses up to 2,000 mg/day, the subjects had soft stools or diarrhoea which is not to be seen as adverse but is classified as discomfort. However, when higher doses are given, such as the doses for bowel cleansing in preparation for colonoscopy (e.g. 11,600 mg per person or 165.7 mg/kg bw) these doses acted as a cathartic agent and this effect has to be clearly seen as adverse.
In conclusion, in a chronic exposure setting the clinical data indicate that adverse effects on the kidney have been reported in human at added phosphates doses threefold lower than that causing adverse renal effects in animals.
4.6. Mode of action and discussion of uncertainty
The mode of action for the kidney impairment is precipitation of calcium phosphate which occurs in the kidney, the only organ for phosphate excretion, when the solubility is exceeded. Thus, the mechanism of action is related to a physicochemical property of calcium phosphate. From the identified mechanism of action which is species independent and independent from individual factors, the Panel derived a TD inter‐ and intraspecies factor of 1.
The maximum limit of solubility depends on the volume in which a certain amount of calcium phosphate is dissolved. Concerning the solubility of calcium phosphate in the primary urine, the urinary volume is relevant. The interspecies difference (rat vs man) in the volume of primary urine is 4.4 L/kg bw per day in rat vs 2.16 L/kg bw per day in man (see Section 3.10.2) resulting in a factor of 2. In other words, when a certain amount of phosphorus/kg bw per day would not exceed the solubility in rat with a urine volume of twice that in humans, the daily dose in humans not exceeding the solubility would be half of that amount.
For the variability of the urinary volume in humans, the Panel used information on the variability of the glomerular filtration rate in healthy subjects (between 60 and 120 mL/min). In order to account for the potentially lower glomerular filtration in subjects of the general population with a higher age and slightly impaired renal function, the Panel decided to consider the lower level of glomerular filtration rate resulting in an intraspecies factor for TK to 2. In other words, when a certain amount of phosphorus/kg bw per day which would not exceed the solubility in humans with a normal urine volume, the daily dose in humans with slight to moderate renal impairment not exceeding the solubility would be half of that amount.
Uncertainty:
-
1
The first aspect is the application of the read across approach. Phosphates have been studied for all relevant endpoints required to assess the safety of a food additive. However, toxicological studies do not exist for all salts of phosphates authorised as food additives and the Panel applied a read across approach. Whereas no arguments point to the fact that the endpoints for toxicity of the various phosphates would differ it has to be assumed that the bioavailability and hence the dose for eliciting toxicity would differ with the solubility of the salts. In this respect as the calcium salts are only sparingly soluble or even insoluble in water, their bioavailability may be lower than that of other salts. Experimental data directly comparing the bioavailability of the various phosphate salts are lacking.
However, the lowest phosphate dose leading to effects in the kidney in short‐term studies with monosodium phosphate dehydrate, the phosphorus dose is 123.8 mg/kg bw per day (Mars et al., 1988). The corresponding dose of the mixture of calcium dihydrogen phosphate and monosodium phosphate is 149.1 mg/kg bw per day. The comparison the two dose levels leading to effects on the kidney shows that the dose of the water‐soluble and hence highly bioavailable monosodium phosphate dehydrate is only slightly lower (20%) than the dose of the sparingly soluble calcium dihydrogen phosphate and the water‐soluble monosodium phosphate as a mixture. This indicates that phosphate is also available from calcium dihydrogen phosphate. The study from which the reference point is derived was a study with sodium metaphosphate which is water‐soluble. Hence, the selected reference point overestimates the toxicity of the sparingly water‐soluble and ‐insoluble calcium salts of phosphate, the extent might be around 20%.
-
2
The second aspect is the selection of the key toxicity endpoint. Calcifications in the kidney have been identified as the most relevant endpoint for phosphorus which is observed in several species and also in man. Based on available data the selection of the key toxicity is unlikely to contribute to the uncertainty.
-
3
The third aspect is the selection of the NOAEL. The highest reliable NOAEL from the short‐term and subchronic studies was 500 mg/kg bw per day, corresponding to 116 mg/kg bw per day phosphorus in a 90‐day study (Seo et al., 2011). In chronic rat studies calcifications in the kidneys and tubular nephropathy was observed and the NOAELs of 250 mg/kg bw per day with sodium triphosphate (corresponding to pentasodium triphosphate) (63 mg/kg be per day phosphorus) and 250 mg/kg bw per day sodium hexametaphosphate (corresponding to soluble sodium polyphosphate) (76 mg/kg bw per day phosphorus) were identified (Hodge, 1959, 1960).
-
4
The forth aspect is the derivation of the chemical specific adjustment factor for phosphorus. The derivation of the TD factor is based on the physicochemical property of the causing agent, calcium phosphate and this is applicable to the situation in rat and in humans as demonstrated by comparison of histopathology in both species. The TK interspecies factor of 2 is based on the species‐specific different volumes of urine (see Section 3.10.2) and the TK intraspecies factor was set at 2 (see Section 3.10.2). For the interspecies TK factor of 2, the uncertainty could be estimated from the standard deviation of the measurements which would result in values between 1.44 and 2.85 indicating a relatively low uncertainty in the estimate of 2. The intraspecies TK factor was estimated from a study in healthy subjects and resulted in a factor of 1.5. The Panel decided to enlarge this factor to 2 to reduce the uncertainty in the extrapolation from the healthy subjects to the general population. The resulting total compound specific adjustment factor is then 4.
Considering all aspects which have to be discussed to characterise the uncertainty surrounding the ADI it can be stated that the uncertainty is low although a firm numerical number for the magnitude of the uncertainties cannot be given.
An ADI did not exist until now, and in 1982, JECFA concluded that the allocation of an ADI was not appropriate for phosphates ‘as phosphorus is an essential nutrient and unavoidable constituent of food’ (JECFA, 1982a). Therefore, JECFA assigned a ‘maximum tolerable daily intake’ (MTDI) of 70 mg/kg bw per day (expressed as phosphorus) for the sum of phosphates and polyphosphates, both naturally present in food and ingested as food additives. The rationale for the MTDI was that ‘The lowest level of phosphate that produced nephrocalcinosis in rat (1% P in the diet) is used as the basis for the evaluation and, by extrapolation based on the daily food intake of 2,800 calories, gives a dose level of 6,600 mg P per day as the best estimate of the lowest level that might conceivably cause nephrocalcinosis in man’. In the evaluation, JECFA justified not to apply a safety factor with the argument that phosphorous was also a nutrient.
The solubility of calcium phosphate was identified as the relevant mechanism of action causing nephrocalcinosis in animals and man. In contrast to JECFA the Panel identified the urinary volume as relevant biological difference between rat and humans which influences the solubility of calcium phosphate. Taking also into account the variability of the urinary volume expressed as glomerular filtration rate in the human population the Panel derived a chemical specific adjustment factor of 4 for phosphorus.
4.7. Derivation of the ADI
In the context of this opinion, the Panel was in the special situation to derive an ADI for a substance which at the same time is a nutrient and a food additive. The ADI is the acceptable daily intake of a substance and includes exposure by food additives in addition to the exposure to the substance naturally occurring in the diet.
As explained in the discussion above the derivation of the ADI for phosphorus has to be based on the results of studies in animals. Three studies, one subchronic study and two chronic studies are available from which NOAELs could be derived. In the two chronic studies, the NOAELs were 63 mg/kg P bw per day and 76 mg/kg P bw per day (Hodge, 1959, 1960). However, the content of phosphorus in the background diet could not be identified. In the subchronic 90‐day rat study performed according to OECD guidelines the NOAEL was 116 mg/kg bw per day phosphorus (Seo et al., 2011). The content of phosphorus in the diet could be retrieved (personal communication, Cargill Agri Purina Korea, 29 January 2019) and was calculated to result in a daily intake of 91 mg P/kg bw per day.
The Panel noted that the most appropriate reference point for derivation the ADI would be a NOAEL from a chronic study. Among the present two chronic studies, the higher NOAEL of 76 mg P/kg bw per day has been selected. Considering that ADI includes exposure by food additives in addition to the substance naturally occurring in the diet, the content of the phosphorus in the animal diet has to be taken into account. The Panel considered the content of phosphorus retrieved for Seo et al. study as an appropriate estimate of a standard animal diet which is also in conformity with phosphorus content in laboratory animal diets from different sources (Ritskes‐Hoitinga et al., 1991; Nutrient Requirements of Laboratory Animals, 1995).
Adding the dietary P of 91 mg/kg bw per day to the NOAEL of 76 mg P/kg bw per day gives a value of 167 mg P/kg bw per day. To this value, the chemical‐specific adjustment factor for phosphate of 4 is to be applied resulting in an ADI value of 42 mg/kg bw per day, rounded to 40 mg/kg bw per day.
The Panel noted that this ADI would be the same if derived from the 90‐day study. Since this is a subchronic study an adjustment factor of 2 should be applied (EFSA guidance 2012) resulting in a NOAEL of 58 mg P/kg bw per day. Adding the dietary P of 91 mg/kg bw per day to the adjusted NOAEL of 58 mg P/kg bw per day gives a value of 149 mg P/kg bw per day. Following the application of the phosphorus‐specific adjustment factor of 4, this would result in an ADI of 37 mg/kg bw per day.
The Panel noted that the ADI of 40 mg P/bw per day does not apply to humans with moderate to severe reduction in renal function since the adjustment factor for intraspecies variability covers only individual with slight renal impairment.
The EFSA NDA Panel has not set an upper level for phosphorus but a ‘safety’ level of intake. The ADI of 40 mg/kg bw per day would result in an intake level of 2,800 mg P per person per day for a 70 kg adult person which is within the limits of the safety intake level of 3,000 mg P/person per day set by the EFSA NDA Panel (2005).
The newly derived ADI value for P compares well with consumption data from epidemiological studies. The mean dietary consumption was 1,373 mg phosphorus per day in adult subjects in the NHANES studies 2001 to 2014, the mean intake of phosphorus in adults from the diet alone was 1,725 mg/day with a P95 intake of 2,855 mg/day in a recent Norwegian survey (VKM Report 2017: 18) and the highest phosphorus dietary intake in the epidemiological studies reviewed (see Appendix S) was 3,600 mg/day. In contrast, the MTDI of JECFA (1982a) of 70 mg phosphorus/kg bw per day (equally to 4,900 mg phosphorus per adult person per day, assuming 70 kg body weight) is higher that the exposure reported in the cited epidemiological studies.
4.8. Exposure assessment
Phosphates (E 338–341, E 343, E 450–452) are authorised for 108 different uses (corresponding to 65 different food categories) according to Annex II to Regulation (EC) No 1333/2008 and data were received for most of the uses in which the food additives are authorised to be added.
To assess the dietary exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives, the exposure was calculated based on two different sets of concentration data: (1) MPLs as set down in the EU legislation (defined as the regulatory maximum level exposure assessment scenario); and (2) reported use levels (defined as the refined exposure assessment scenario).
While analytical data were used to consider the exposure to phosphorus from all dietary sources.
As mentioned above, in the context of this opinion, the Panel was in the special situation to assess the safety of food additives, phosphate salts, which are also nutrients. The Panel based its assessment on the toxicity of phosphorus (phosphate moiety). Since the ADI encompasses the phosphorus intake from natural sources and from food additives sources, the usual exposure assessment using the reported use levels of the food additives was not appropriate to characterise the risk linked to the exposure to phosphorus and the exposure assessment was based on analytical data of the total phosphorus content of foods. In other contexts, the evaluation of the adverse effects of nutrients serve as a basis to set ULs (EFSA NDA Panel, 2006). The Panel noted the lack of a harmonised procedure to assess the safety and set HBGVs for substances that are at the same time food additives and nutrients. The Panel considered that there is a need for developing a general approach to be followed in the case a food additive is also a nutrient.
Based on the reported use levels, the Panel calculated two refined exposure estimates based on different assumptions as described in Section 3.4.1: a brand‐loyal consumer scenario and a non‐brand‐loyal scenario. The Panel considered that the refined exposure assessment approach resulted in more realistic long‐term exposure estimates compared to the regulatory maximum level exposure assessment scenario.
The exposure estimates in the regulatory maximum level exposure assessment scenario were between 12 and 113 mg P/kg bw per day at the mean and between 21 and 196 mg P/kg bw per day at the 95th percentile for all population groups (Table 5b). The Panel noted that the estimated long‐term exposures based on this scenario are very likely conservative, as this scenario assumes that all foods and beverages listed under the Annex II to Regulation No 1333/2008 contain phosphates (E 338–341, E 343, E 450–452) as food additives at the MPL.
Considering the refined brand‐loyal exposure assessment scenario, estimated exposure to phosphates (E 338–341, E 343, E 450–452) was between 2 and 53 mg P/kg bw per day at the mean and between 9 and 69 mg P/kg bw per day at the 95th percentile for all population groups.
For the refined non‐brand‐loyal exposure assessment scenario, estimated exposure to phosphates (E 338–341, E 343, E 450–452) ranged between 1 and 48 mg P/kg bw per day at the mean and between 3 and 62 mg P/kg bw per day at the 95th percentile for all population groups (Table 5b).
The Panel considered that for the main food category (bread and rolls) contributing to the exposure estimates, brand‐loyalty would not be expected and therefore selected the refined non‐brand loyal scenario as the most relevant exposure scenario for the safety evaluation of phosphates (E 338–341, E 343, E 450–452) for toddlers, children, adolescents, adults and the elderly. Dietary exposure to phosphates (E 338–341, E 343, E 450–452) according to this exposure scenario was maximally 11 mg/kg bw per day at the mean level and 26 mg/kg bw per day at the high (P95) level. For infants, infant formulae were the main contributing food category, and the brand‐loyal scenario should be considered.
For the food supplements consumers only, mean exposure to phosphates (E 338–341, E 343, E 450–452) from their uses as food additives ranged from 275 mg P/person per day for children to 1,541 mg P/person per day for the elderly. The 95th percentile of exposure to phosphates (E 338–341, E 343, E 450–452) ranged from 753 mg P/person per day for adolescents to 7,292 mg P/person per day for adults. The Panel noted the high levels for food supplements compared to therapeutic use (see Section 3.8.1). According to data providers, in a number of cases, the phosphates are added principally as nutrient substance and not as additives. However, in other cases, the addition of phosphates (e.g. higher reported use levels) is due to their technical requirements as food additives rather than an intended use as nutrient sources. The Panel noted the high intakes resulting from such levels and the potential risk for people who might consume food supplements regularly.
The Panel calculated that out of the foods authorised to contain phosphates (E 338–341, E 343, E 450–452) according to Annex II to Regulation (EC) No 1333/2008, a minimum of 30 (for children) to a maximum of 93% (for infants) of the amount of food consumed (by weight) per population group was reported to potentially contain phosphates (E 338–341, E 343, E 450–452) as food additives.
The exposure assessments were influenced by several uncertainties (Table 8a). The Panel noted that most of Mintel subcategories were included in the current exposure assessment (missing food categories are alcoholic beverages, some vegetables, see Section 3.3.2). The percentage of foods per subcategory labelled to contain phosphates (E 338–341, E 343, E 450–452) was on average of 9.6% whereas in the assessment, it was assumed that 100% of the foods belonging to an authorised food category contained the additive. The Panel noted that an exposure assessment based on the premise that all of the foods contain phosphates would probably lead to an overestimation of the dietary exposure which represents the largest uncertainty.
Overall, the Panel considered that the uncertainties identified would, in general, result in an overestimation of the exposure to phosphates (E 338–341, E 343, E 450–452) from their use as food additives according to Annex II in European countries considered in the EFSA European database for the regulatory maximum level exposure scenario. For the refined estimated exposure scenario, uncertainties would also lead to an overestimation of exposure to phosphates (E 338–341, E 343, E 450–452).
The Panel also noted that the refined exposure estimates are based on information provided on the reported level of use of phosphates (E 338–341, E 343, E 450–452). If actual practice changes, these refined estimates may no longer be representative and should be updated.
Scenarios based on uses and use levels estimating exposure including the proposed extension of use were performed. The proposed extension of use did not show any change in the total estimated exposure probably because the proposed change in the authorised use of the FC 05.2 does not add a large number of foods compared to the current authorisation.
Exposure to phosphates from the whole diet was estimated using mainly analytical data (estimated exposure scenario based on analytical data). Not all available data could be included in the assessment but most of the foods consumed were taken into account in this estimate.
In this scenario, the exposure exceeds the ADI of 40 mg/kg bw per day in infants from 12 weeks to 11 months, toddlers and children both at the mean and high level. In adolescents, the high level is also exceeding the ADI of 40 mg/kg bw per day.
Both estimates using reported use levels and analytical data are limited by several uncertainties described in exposure section. Although caveats related to these estimates, exposure from food additives for all population groups except infants would indicatively contribute between 6 and 21% of the total mean intakes. For infants from 12 weeks to 11 months, the percentages would range between 12 and 30%.
To compare the estimated exposure scenario based on analytical data, with the exposure published in other opinions and surveys the mean exposure to phosphorus was calculated as the exposure per person per day and compared to exposure data from surveys. The values ranged from 254 mg P/person per day in infants to 1,625 mg P/person per day for adults, and the high exposure (95th percentile) from 331 mg P/person per day in infants to 2,728 mg P/person per day for adults.
Exposure estimates of phosphorus using the same methodology (consumption data from national dietary surveys and levels of phosphorus in food from analytical measurement) was also performed in the NDA Panel opinion (EFSA NDA Panel, 2015). Intake estimates from the 2015 opinion and the current estimates are very much similar per population groups. Foods in both opinion are not classified under the same categories but food categories contributing the most to the mean exposure are also the same: milk and dairy products, grains and grain‐based products and meat and meat products in EFSA, 2015; unflavoured pasteurised and sterilised (including UHT) milk, bread and rolls and meat products for EFSA, 2018 (this opinion).
The high level of exposure to phosphorus coming from food supplements is reflected also in the dietary exposure in the food supplements consumers only scenario using analytical data.
Direct comparison of exposure based on analytical data with exposure reported in the epidemiological studies is not readily achieved due to differences in methodologies applied. Whereas comparison between such data is indicative only, the exposure levels are reasonably similar.
4.9. Infants and young children
By regulation, the minimum and maximum total levels of phosphorus for infant formula are set at 25 and 90 mg/100 kcal, in the case of infant formula based on soy the maximum level is 100 mg/100 kcal. The minimum and maximum levels for infant formula for special medical purposes are set at 25 and 100 mg/100 kcal (Commission Delegated Regulation (EU) 2016/127 and Commission Delegated Regulation (EU) 2016/128, as well as Commission Directive 2006/141/EC and Commission Directive 1999/21/EC). These limits mean that at the high level consumption of 260 mL/kg bw per day by infant formula and by FSMP for infants (as calculated by EFSA, 2017), the exposure would be approximately between 44 and 175 mg/kg bw per day for phosphorus irrespective of whether phosphorus is delivered from the formula as nutrient or as food additive. Given the limits set by existing regulation, it seems not appropriate to use the ADI set for food additives only for infants formulae, nor is necessary to derive a numerical ADI applicable for this age group.
5. Conclusions
Considering the overall database relevant for phosphoric acid–phosphates – di‐, tri‐ and polyphosphates, the Panel derived a group ADI for phosphates expressed as phosphorus of 40 mg/kg bw per day from a chronic study. This ADI corresponds to an acceptable intake of phosphorus of 2,800 mg/day for an adult of 70 kg. This is within the level of 3,000 mg/day indicated by the EFSA NDA Panel (2005) as being tolerated by healthy individuals.
The Panel considers that the group ADI of 40 mg/kg bw per day, expressed as phosphorus, is protective for healthy adults because it is below the doses at which clinically relevant adverse effects were reported in short‐term and long‐term studies in humans. However, this ADI does not apply to humans with moderate to severe reduction in renal function. Ten per cent of general population might have CKD with reduced renal function and they may not tolerate the amount of P per day which is at the level of ADI. The total phosphorus content of foods (naturally occurring and added as additives) is not mandatory to be reported on food labels.
The Panel noted that the exposure estimates based on analytical data exceeded the proposed ADI for infants, toddlers and children at the mean level and for infants, toddlers, children and adolescents at the 95th percentile. The Panel also noted that P exposure from food supplements exceeds the proposed ADI.
The Panel concluded that the available data did not give rise to safety concerns in infants below 16 weeks of age consuming formula and food for medical purposes. When receiving data on the content of contaminants in formula, the Panel noted that the high aluminium content may exceed the TWI.
6. Recommendations
The Panel recommends that:
The EC considers setting numerical Maximum Permitted Level for phosphates as food additives in food supplements.
The European Commission considers revising the current limits for toxic elements (Pb, Cd, As and Hg) in the EU specifications for phosphates (E 338–341, E 343, E 450–452) in order to ensure that phosphates (E 338–341, E 343, E 450–452) as a food additive will not be a significant source of exposure to those toxic elements in food.
The European Commission considers revising the current limit for aluminium in the EU specifications for the use of calcium phosphate (E 341).
The European Commission to consider revising the current EU specifications for calcium dihydrogen phosphate (E 341(i)), calcium hydrogen phosphate (E 341(ii)), tricalcium phosphate (E 341(iii)), dimagnesium phosphate (E 343(ii)) and calcium dihydrogen diphosphate (E 450(vii)) to include characterisation of particle size distribution using appropriate statistical descriptors (e.g. range, median, quartiles) as well as the percentage (in number and by mass) of particles in the nanoscale (with at least one dimension < 100 nm) present in calcium dihydrogen phosphate (E 341(i)), calcium hydrogen phosphate (E 341(ii)), tricalcium phosphate (E 341(iii)), dimagnesium phosphate (E 343(ii)) and calcium dihydrogen diphosphate (E 450(vii)) used as a food additive. The measuring methodology applied should comply with the EFSA Guidance document (EFSA Scientific Committee, 2018).
The development of analytical methods for the determination of phosphate additives in the range of foods and beverages permitted to contain them should be considered.
The EFSA Scientific Committee reviews current approaches to the setting of HBGVs for regulated substances which are also nutrients to assess if a coherent harmonised strategy for such risk assessments should be devised.
7. Documentation provided to EFSA
Application dossier for the extension of use of phosphoric acid–phosphates – di‐, tri‐ and polyphosphates (E 338‐452) in the food category 05.2 ‘Other confectionary including breath refreshing microsweets’. Submitted by Perfetti Van Melle SpA, April 2018.
CEFIC‐PAPA, 2018. PAPA Contribution to EFSA request for additional information – EFSA re‐evaluation of phosphates (EFSA‐Q‐2017‐00492). Analytical data on impurities for phosphate additives used in “food for infants below 16 weeks of age. Submitted to EFSA on June 2018.
Mead Johnson Nutrition/Reckitt Benckiser, 2018. Submission of information to the EFSA call for technical and toxicological data on phosphates authorised as food additives in the EU (EFSA‐Q‐2017‐00492). Submitted to EFSA on June 2018.
Hipp, 2018. Contribution to EFSA request for additional information – EFSA re‐evaluation of phosphates (EFSA‐Q‐2017‐00492). Submitted to EFSA June 2018.
Abbott Nutrition, 2018. Contribution to EFSA request for additional information – EFSA re‐evaluation of phosphates. Submitted to EFSA June 2018.
CEFIC‐PAPA, 2017. PAPA contribution to EFSA call for data – EFSA ‐Q‐number : EFSA‐Q‐2017‐00492. Submitted to EFSA on December 2017.
CEFIC‐PAPA, 2018. Contribution to EFSA call for data – EFSA ‐Q‐number: EFSA‐Q‐2017‐00492. Submitted to EFSA on November 2018.
CEFIC‐PAPA, 2012. Reply to EFSA: Re‐evaluation of food additives: call for data (15.2.2012). E 338 Phosphoric acid. Submitted to EFSA on August 2012.
CEFIC‐PAPA, 2012. Reply to EFSA: Re‐evaluation of food additives: call for data (15.2.2012). E 341 Calcium phosphates. Submitted to EFSA on August 2012.
CEFIC‐PAPA, 2012. Reply to EFSA: Re‐evaluation of food additives: call for data (15.2.2012). E 343 Magnesium phosphates. Submitted to EFSA on August 2012.
CEFIC‐PAPA, 2012. Reply to EFSA: Re‐evaluation of food additives: call for data (15.2.2012). E 451 Triphosphates. Annex 12 on the determination of total phosphorus in cheese and cheese products by interlaboratory study. Submitted to EFSA on August 2012.
CEFIC‐PAPA, 2012. Reply to EFSA: Re‐evaluation of food additives: call for data (15.2.2012). E 340 Potassium phosphates. Submitted to EFSA on August 2012.
CEFIC‐PAPA, 2012. Reply to EFSA: Re‐evaluation of food additives: call for data (15.2.2012). E 339 Sodium phosphates. Submitted to EFSA on August 2012.
CEFIC‐PAPA, 2012. Reply to EFSA: Re‐evaluation of food additives: call for data (15.2.2012). E 450 Diphosphates. Submitted to EFSA on 13 August 2012.
CEFIC‐PAPA, 2012. Reply to EFSA: Re‐evaluation of food additives: call for data (15.2.2012). E 451 Triphosphates. Submitted to EFSA on 13 August 2012.
CEFIC‐PAPA, 2012. Reply to EFSA: Re‐evaluation of food additives: call for data (15.2.2012). E 452 Polyphosphates. Submitted to EFSA on 13 August 2012.
CEFIC‐PAPA, 2013. Reply to EFSA: EFSA call for scientific data on miscellaneous food additives –phosphate compounds listed under the category “acidity regulators. Submitted to EFSA on 18 January 2013.
CEFIC‐PAPA, 2014. Additional data for eight phosphates. Submitted to EFSA on 23 July 2014.
CEFIC‐PAPA, 2016. Additional particle size data for phosphates. Submitted to EFSA on 05 February 2016.
BVfL, 2012. Aufruf der EFSA‐052/2012 zur Neubewertung diverser in der EU zugelassener Lebensmittelzusatzstoffe unterschiedlicher Funktionsklassen im Kontext der Verordnung (EG) Nr. 1333/2008 des Europäischen Parlaments und des Rates vom 16. Dezember 2008 über Lebensmittelzusatzstoffe. Submitted to EFSA on August 2012.
Ludwig Maximilians Universität München, 2018. Reply to EFSA: Call for data on phosphates authorised as food additives in the EU. Submitted to EFSA on 29 January 2018.
ERA‐EDTA, 2018. Reply to EFSA: Call for technical and toxicological data on phosphates authorised as food additives in the EU. Submitted to EFSA on 3 January 2018.
Dr. Paul Lohmann, 2018. Reply to EFSA: EFSA‐Q‐2017‐00492 call for dat/E343(ii) Dimagnesium phosphate. Submitted to EFSA on 3 January 2018.
Renal Nutrition Group of the British Dietetic Association (BDA), 2018. Reply to EFSA: EFSA‐Q‐2017‐00492. Submitted to EFSA on 3 January 2018.
Specialised Nutrition Europe (SNE), 2018. SNE submission of information to the EFSA Call for technical and toxicological data on phosphates authorised as food additives in the EU. Submitted to EFSA on 8 June 2018.
Pre‐evaluation document “The sodium and potassium salts of phosphoric acid (E 339(i), 339(ii), 339(iii), 340(i), 340(ii) and 340(iii))” prepared by DTU Food (Contractor) 13 November 2014.
Pre‐evaluation document “Phosphoric acid and its calcium and magnesium salts (E 338, 341(i), 341(ii), 341(iii), 343(i) and 343(ii))” prepared by DTU Food (Contractor) 13 November 2014.
Pre‐evaluation document “Re‐evaluation of disodium diphosphate (E 450(i)), trisodium diphosphate (E 450(ii)), tetrasodium diphosphate (E 450(iii)), tetrapotassium diphosphate (E 450(v)), dicalcium diphosphate (E 450(vi)) and calcium dihydrogen diphosphate (E 450(vii)) as food additives” prepared by DTU Food (Contractor) on 25 November 2013
Pre‐evaluation document “Re‐evaluation of pentasodium triphosphate and pentapotassium triphosphate (E 451) as food additives” prepared by Peter Fisk Associates Ltd on 27 November 2014.
Pre‐evaluation document “Re‐evaluation of sodium polyphosphate (E 452(i)), potassium polyphosphate (E 452(ii)), sodium calcium polyphosphate (E 452(iii)) and calcium polyphosphate (E 452(iv)) as food additives” prepared by Peter Fisk Associates Ltd 25 November 2013.
Association des Entreprises Produits Alimentaires Elabores (ADEPALE), 2017. Data on use levels of phosphates (E 338‐341, E 343, E 450‐452) in foods in response to the EFSA call for food additives usage level and/or concentration data in food and beverages intended for human consumption (2017). Submitted to EFSA on 16 November 2017.
Association of the European Self‐Medication Industry (AESGP), 2017. Data on use levels of phosphates (E 338‐341, E 343, E 450‐452) in foods in response to the EFSA call for food additives usage level and/or concentration data in food and beverages intended for human consumption (2017). Submitted to EFSA on 16 November 2017.
Comité Européen des Fabricants de Sucre (CEFS), 2017. Data on use levels of phosphates (E 338‐341, E 343, E 450‐452) in foods in response to the EFSA call for food additives usage level and/or concentration data in food and beverages intended for human consumption (2017). Submitted to EFSA on 29 November 2017.
Dr Loges Naturheilkunde neu entdecken, 2017. Data on use levels of phosphates (E 338‐341, E 343, E 450‐452) in foods in response to the EFSA call for food additives usage level and/or concentration data in food and beverages intended for human consumption (2017). Submitted to EFSA on 9 June 2017.
European Chemical Industry Council (CEFIC), 2017. Data on use levels of phosphates (E 338‐341, E 343, E 450‐452) in foods in response to the EFSA call for food additives usage level and/or concentration data in food and beverages intended for human consumption (2017). Submitted to EFSA on 30 November 2017.
European Dairy Association (EDA), 2017. Data on use levels of phosphates (E 338‐341, E 343, E 450‐452) in foods in response to the EFSA call for food additives usage level and/or concentration data in food and beverages intended for human consumption (2017). Submitted to EFSA on 30 November 2017.
European Fish Processors and Traders Association & European Federation of National Organisations of Importers and Exporters of Fish (AIPCE‐CEP), 2017. Data on use levels of phosphates (E 338‐341, E 343, E 450‐452) in foods in response to the EFSA call for food additives usage level and/or concentration data in food and beverages intended for human consumption (2017). Submitted to EFSA on 30 November 2017.
European Potato Processors’ Association (EUPPA), 2017. Data on use levels of phosphates (E 338‐341, E 343, E 450‐452) in foods in response to the EFSA call for food additives usage level and/or concentration data in food and beverages intended for human consumption (2017). Submitted to EFSA on 30 November 2017.
FDE (FoodDrinkEurope), 2017. Data on use levels of phosphates (E 338‐341, E 343, E 450‐452) in foods in response to the EFSA call for food additives usage level and/or concentration data in food and beverages intended for human consumption (2017). Submitted to EFSA on 29 November 2017.
Food Supplement Europe (FSE), 2017. Data on use levels of phosphates (E 338‐341, E 343, E 450‐452) in foods in response to the EFSA call for food additives usage level and/or concentration data in food and beverages intended for human consumption (2017). Submitted to EFSA on 30 November 2017.
IMACE, 2017. Data on use levels of phosphates (E 338‐341, E 343, E 450‐452) in foods in response to the EFSA call for food additives usage level and/or concentration data in food and beverages intended for human consumption (2017). Submitted to EFSA on 29 November 2017.
International Chewing Gum Association (ICGA), 2017. Data on use levels of phosphates (E 338‐341, E 343, E 450‐452) in foods in response to the EFSA call for food additives usage level and/or concentration data in food and beverages intended for human consumption (2017). Submitted to EFSA on 30 November 2017.
Intersnack, 2017. Data on use levels of phosphates (E 338‐341, E 343, E 450‐452) in foods in response to the EFSA call for food additives usage level and/or concentration data in food and beverages intended for human consumption (2017). Submitted to EFSA on 29 November 2017.
L'ALLIANCE 7, 2017. Data on use levels of phosphates (E 338‐341, E 343, E 450‐452) in foods in response to the EFSA call for food additives usage level and/or concentration data in food and beverages intended for human consumption (2017). Submitted to EFSA on 30 November 2017.
Nathura, 2017. Data on use levels of phosphates (E 338‐341, E 343, E 450‐452) in foods in response to the EFSA call for food additives usage level and/or concentration data in food and beverages intended for human consumption (2017). Submitted to EFSA on 7 March 2017.
Specialised Nutrition Europe (SNE), 2017. Data on use levels of phosphates (E 338‐341, E 343, E 450‐452) in foods in response to the EFSA call for food additives usage level and/or concentration data in food and beverages intended for human consumption (2017). Submitted to EFSA on 8 December 2017.
Abbreviations
- AAC
aortic annulus calcification
- ABI
ankle brachial index
- ACR
Albumin‐to‐creatinine ratio
- ADEPALE
Association des Entreprises Produits Alimentaires Elabores
- ADI
acceptable daily intake
- AF
atrial fibrillation
- AI
adequate intake
- AIPCE‐CEP
European Fish Processors and Traders Association & European Federation of National Organisations of Importers and Exporters of Fish
- ALP
alkaline phosphatase
- ALT
alanine aminotransferase
- AMP
adenosine monophosphate
- ANS
EFSA Panel on Food Additives and Nutrient Sources
- AOAC
Association of Official Analytical Chemists
- ARIC
Atherosclerosis Risk in Communities study
- AST
aspartate aminotransferase
- ATP
adenosine triphosphate
- AVC
aortic valve calcification
- BMD
bone mineral density
- BMI
body mass index
- BP
blood pressure
- BVL
German Federal Office for Consumer Protection and Safety
- bw
body weight
- CAC
coronary artery calcification
- CAD
coronary artery disease
- cAMP
adenosine monophosphate
- CARDIA
Coronary Artery Risk Development in Young Adults
- CAS
Chemical Abstract Service
- CE
capillary electrophoresis
- CEFIC
European Chemical Industry Council
- CEFS
Comité Européen des Fabricants de Sucre
- cGMP
cyclic guanine monophosphate
- CHD
coronary heart disease
- CI
confidence interval
- CIR
Cosmetic Ingredient Review Expert Panel
- cITP
capillary isotachophoresis
- CKD
chronic kidney disease
- CRF
corticotropin‐releasing factor
- CTP
cytidine triphosphate
- CVD
cardiovascular disease
- CZE
capillary zone electrophoresis
- DCP
direct current plasma spectrometry
- DLS
dynamic light scattering
- Dn
number‐based
- DRV
Dietary Reference Value
- Dv
volume‐based
- DXA
dual X‐ray absorptiometry
- ECF
extracellular fluid
- ECHA
European Chemicals Agency
- EDA
European Dairy Association
- eGFR
estimated glomerular filtration rate
- EINECS
European Inventory of Existing Commercial chemical Substances
- EUPPA
European Potato Processors’ Association
- EVM
Expert Group on Vitamins and Minerals
- F1
first‐generation pups
- F2
second‐generation pups
- FAF
Food Additives and Flavourings
- FAP
phosphates as food additives
- FC
food category
- FCS
food categorisation system
- FDA
US Food and Drug Administration
- FDE
Food Drink Europe
- FDRL
Food and Drink Research Laboratories
- FGF‐23
fibroblast growth factor 23
- FFQ
food frequency questionnaires
- FSE
Food Supplement Europe
- FSMP
food for special medical purposes
- GD
gestation days
- GLP
Good Laboratory Practice
- GNPD
Global New Products Database
- GTP
guanosine‐5’‐triphosphate
- HBGV
health‐based guidance value
- HCT
hychlorothiazide
- HDL
high‐density lipoprotein
- HF
heart failure
- HPLC
high‐performance liquid chromatography
- HR
hazard ratio
- HRT
hormone replace therapy
- HTA
Hypertonia arterialis
- IC
ion chromatography
- ICD
International Classification of Diseases
- ICGA
International Chewing Gum Association
- IMT
intima‐media thickness
- IPCS
International Program on Chemical Safety
- IQR
Interquartile Range
- IUCLID
International Uniform Chemical Information Database
- JECFA
Joint FAO/WHO Expert Committee on Food Additives
- KCl
Potassium chloride
- LC
left‐censored
- LD50
lethal dose, 50%, i.e. dose that causes death among 50 % of treated animals
- LDL
low‐density lipoprotein
- LOAEL
lowest‐observed‐adverse‐effect‐level
- LOD
limit of detection
- LOQ
limit of quantification
- LVM
left ventricular mass
- MB
middle‐bound
- MESA
Multi‐Ethnic study of Atherosclerosis
- MI
myocardial infarction
- MPL
maximum permitted level
- MTDI
maximum tolerable daily intake
- NDA
Nutrition, Novel Food and Food Allergens
- NHANES III
Third National Health and Nutrition Examination Survey
- NMR
nuclear magnetic resonance
- NOAEL
no‐observable‐adverse‐effect level
- NOEL
no‐observed‐effect level
- NOS
Newcastle–Ottawa Scale
- OECD
Organisation for Economic Co‐operation and Development
- OPG
osteoprotegerin
- P
phosphorus
- Pi
inorganic phosphorus
- P1
first‐generation adults
- P2
second‐generation adults
- P3
third‐generation adults
- PAPA
Phosphoric Acid and Phosphates Producers Association
- PTH
parathyroid hormone
- QICKD
Quality Improvement in Chronic Kidney Disease
- QS
quantum satis
- RANK
receptor activator of NF‐kB ligand
- REACH
Registration, Evaluation, Authorisation and restriction of CHemicals
- RNA
ribonucleic acid
- SCF
Scientific Committee for Food
- SDP
plasma spectrometry
- SEM
scanning electron microscopy
- sFRP‐4
secreted frizzled‐related protein 4
- SNE
Specialised Nutrition Europe
- TCA
trichloroacetic acid
- TD
toxicodynamics
- TEM
transmission electron microscopy
- TemaNord
Nordic Council of Ministers
- TIA
Transient Ischemic Attack
- TK
toxicokinetics
- TLC
thin‐layer chromatography
- TmP
tubular maximum for P
- TWI
tolerable weekly intake
- UHT
Ultra High Temperature
- UL
upper level
- UTP
uridine‐5’‐triphosphate
- UV
ultraviolet
- VKM
Norwegian Scientific Committee for Food Safety
- WHO
World Health Organization
Appendix A – Summary of range of phosphates functional classes according to JECFA
1.
| E No. | Phosphate name | Acidulant | Sequestrant | Synergist antioxidant | Emulsifier | Emulsion stabiliser | Texturiser | Buffer1 | Neutralising agent | Raising agent2 | Firming agent | Anti caking agent |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 338 | Phosphoric acid | + | + | + | ||||||||
| 339(i) | Monosodium | + | + | |||||||||
| 339(ii) | Disodium | + | + | + | ||||||||
| 339(iii) | Trisodium | + | + | + | ||||||||
| 340(i) | Monopotassium | + | + | + | + | |||||||
| 340(ii) | Dipotassium | + | + | + | ||||||||
| 340(iii) | Tripotassium | + | + | + | ||||||||
| 341(i) | Monocalcium | + | + | + | + | |||||||
| 341(ii) | Dicalcium | + | + | + | ||||||||
| 341(iii) | Tricalcium | + | ||||||||||
| 343(i) | Monomagnesium | + | ||||||||||
| 343(ii) | Dimagnesium | |||||||||||
| 450(i) | Disodium di | + | + | + | ||||||||
| 450(ii) | Trisodium di | + | + | + | ||||||||
| 450(iii) | Tetrasodium di | + | + | + | ||||||||
| 450(v) | Tetrapotassium di | + | + | |||||||||
| 450(vi) | Dicalcium di | + | + | + | ||||||||
| 450(vii) | Calcium dihydrogen | + | + | + | ||||||||
| 450(ix) | Magnesium dihydrogen | + | + | + | ||||||||
| 451(i) | Pentasodium tri | + | + | |||||||||
| 451(ii) | Pentapotassium tri | + | ||||||||||
| 452(i) | Sodium poly | + | + | + | ||||||||
| 452(ii) | Potassium poly | + | + | + | ||||||||
| 452(iii) | Sodium calcium poly | + | + | + | ||||||||
| 452(iv) | Calcium poly | + | + | + |
Including acidity regulator.
Including leavening agent/dough conditioner/yeast food.
Appendix B – Table for converting phosphates into phosphorus pentoxide (P2O5) and phosphorus (P)
1.
| E number | Formula | MW | 1 g substance = g P2O5 | 1 g P2O5 = g P |
|---|---|---|---|---|
| E 338 | H3PO4 | 98.00 | 0.724 | 0.315 |
| E 339(i) | NaH2PO4 | 119.98 | 0.592 | 0.258 |
| “ | NaH2PO4, H2O | 138.00 | 0.514 | 0.224 |
| “ | NaH2PO4, 2H2O | 156.01 | 0.455 | 0.198 |
| E 339(ii) | Na2HPO4 | 141.96 | 0.500 | 0.218 |
| “ | Na2HPO4, 2H2O | 177.99 | 0.399 | 0.174 |
| “ | Na2HPO4, 7H2O | 268.06 | 0.265 | 0.115 |
| “ | Na2HPO4, 12H2O | 358.14 | 0.198 | 0.086 |
| E 339(iii) | Na3PO4 | 163.94 | 0.433 | 0.188 |
| “ | Na3PO4, 2H2O | 181.96 | 0.390 | 0.170 |
| “ | Na3PO4, 12H2O | 380.12 | 0.187 | 0.081 |
| E 340(i) | KH2PO4 | 136.09 | 0.522 | 0.227 |
| E 340(ii) | K2H2PO4 | 174.17 | 0.407 | 0.177 |
| E 340(iii) | K3PO4 | 212.28 | 0.334 | 0.145 |
| E 341(i) | Ca(H2PO4)2 | 234.05 | 0.606 | 0.264 |
| E 341(ii) | CaH2PO4, 2H2O | 172.09 | 0.412 | 0.179 |
| E 341(iii) | 10CaO, 3P2O5, H2O | 1,004.67 | 0.424 | 0.185 |
| E 343(i) | Mg(H2PO4)2, 4H2O | 290.34 | 0.489 | 0.213 |
| E 343(ii) | MgHPO4, n H2O (n = 0–3) | 120.28* | 0.590 | 0.257 |
| E450(i) | Na2H2P2O7 | 221.94 | 0.640 | 0.279 |
| E450(ii) | Na3HP2O7 | 243.92 | 0.582 | 0.253 |
| “ | Na3HP2O7, H2O | 261.94 | 0.542 | 0.236 |
| E 450(iii) | Na4P2O7 | 265.90 | 0.534 | 0.233 |
| “ | Na4P2O7, 10H2O | 446.05 | 0.318 | 0.138 |
| E 450(v) | K4P2O7 | 330.34 | 0.430 | 0.187 |
| “ | K4P2O7, 3H2O | 383.39 | 0.369 | 0.161 |
| E 450(vi) | Ca2P2O7 | 254.10 | 0.559 | 0.243 |
| E 450(vii) | CaH2P2O7 | 216.04 | 0.657 | 0.286 |
| E 451(i) | Na5P3O10 | 367.86 | 0.579 | 0.252 |
| “ | Na5P3O10, 6H2O | 475.95 | 0.447 | 0.195 |
| E 451(ii) | K5P3O10 | 448.41 | 0.475 | 0.207 |
| E 452(i) | (NaPO3)n (n > 3) | 102*n | 0.696*n | 0.303*n |
| E 452(ii) | (KPO3)n | 118*n | 0.601*n | 0.262*n |
| E 452(iv) | (CaP2O6)n (n ≥ 2) | 198*n | 0.717*n | 0.312*n |
Anhydrous form.
Appendix C – The link between phosphates and cardiovascular diseases: epidemiology search protocol
Objective
To assess, if any, the association between phosphates/phosphorus intake and cardiovascular diseases and serum phosphorus level and cardiovascular diseases, including cardiovascular specific mortality.
To assess, if any, the association between phosphates/phosphorus intake and stroke and serum phosphorus level and stroke, including stroke specific mortality.
To assess, if any, the association between phosphates intake and serum phosphorus levels and intermediate outcomes of cardiovascular events, such as coronary artery calcification.
To assess, if any, the association between phosphate‐responsive hormones (fibroblast growth factor‐23, parathyroid hormone) and cardiovascular diseases and/or stroke.
Methods
Types of studies and participants
Observational studies (cohort, case–control and cross‐sectional studies) will be included, that investigated the association between: phosphates in diet and/or serum phosphorus and cardiovascular diseases; phosphates in diet and/or serum phosphorus and stroke; phosphates in diet and/or serum phosphorus and cardiovascular specific mortality; phosphates in diet and/or serum phosphorus and stroke specific mortality; phosphates in diet and serum phosphorus levels and intermediate outcomes of cardiovascular events such as coronary artery calcification; phosphate‐responsive hormones (fibroblast growth factor‐23, parathyroid hormone) and cardiovascular events.
Study participants will be adults of either sex or age. Studies that evaluated phosphates/phosphorus from other sources other than diet (medicine, environmental/occupational exposure) will be excluded. Studies that were included in the EFSA report (2013) that are considered informative will be also included in the report.
Types of outcome measures to be included
Primary outcome:
Incidence of cardiovascular diseases and incidence of stroke.
Secondary outcome:
Intermediate outcomes for cardiovascular diseases and cardiovascular mortality.
Phosphate‐responsive hormones (fibroblast growth factor‐23, parathyroid hormone and calcitriol) and cardiovascular events.
Search Strategy and Data Extraction
Electronic searches
Relevant studies were located by searching PubMed. PRISMA flow diagram (Moher et al., 2009) helped managing search strategy and data extraction.
((“phosphates”[MeSH Terms] OR “phosphates”[All Fields] OR “phosphate”[All Fields]) AND intake[All Fields]) AND (“cardiovascular system”[MeSH Terms] OR (“cardiovascular”[All Fields] AND “system”[All Fields]) OR “cardiovascular system”[All Fields] OR “cardiovascular”[All Fields]) AND (“epidemiology”[Subheading] OR “epidemiology”[All Fields] OR “epidemiology”[MeSH Terms])
AND
((“phosphorus”[MeSH Terms] OR “phosphorus”[All Fields] OR “phosphorus”[All Fields]) AND intake[All Fields]) AND (“cardiovascular system”[MeSH Terms] OR (“cardiovascular”[All Fields] AND “system”[All Fields]) OR “cardiovascular system”[All Fields] OR “cardiovascular”[All Fields]) AND (“epidemiology”[Subheading] OR “epidemiology”[All Fields] OR “epidemiology”[MeSH Terms])
AND
(“phosphates”[MeSH Terms] OR “phosphates”[All Fields]) AND (“atherosclerosis”[MeSH Terms] OR “atherosclerosis”[All Fields] OR “atherogenesis”[All Fields]) AND (“cohort studies”[MeSH Terms] OR (“cohort”[All Fields] AND “studies”[All Fields]) OR “cohort studies”[All Fields] OR “cohort”[All Fields])
AND
(“phosphorus, dietary”[MeSH Terms] OR (“phosphorus”[All Fields] AND “dietary”[All Fields]) OR “dietary phosphorus”[All Fields] OR “phosphorus”[All Fields] OR “phosphorus”[MeSH Terms]) AND (“atherosclerosis”[MeSH Terms] OR “atherosclerosis”[All Fields] OR “atherogenesis”[All Fields]) AND (“cohort studies”[MeSH Terms] OR (“cohort”[All Fields] AND “studies”[All Fields]) OR “cohort studies”[All Fields] OR “cohort”[All Fields])
AND
(“phosphates”[MeSH Terms] OR “phosphates”[All Fields]) AND (“atherosclerosis”[MeSH Terms] OR “atherosclerosis”[All Fields] OR “atherogenesis”[All Fields]) AND (“case‐control studies”[MeSH Terms] OR (“case‐control”[All Fields] AND “studies”[All Fields]) OR “case‐control studies”[All Fields] OR (“case”[All Fields] AND “control”[All Fields]) OR “case control”[All Fields])
AND
(“phosphorus, dietary”[MeSH Terms] OR (“phosphorus”[All Fields] AND “dietary”[All Fields]) OR “dietary phosphorus”[All Fields] OR “phosphorus”[All Fields] OR “phosphorus”[MeSH Terms]) AND (“atherosclerosis”[MeSH Terms] OR “atherosclerosis”[All Fields] OR “atherogenesis”[All Fields]) AND (“case‐control studies”[MeSH Terms] OR (“case‐control”[All Fields] AND “studies”[All Fields]) OR “case‐control studies”[All Fields] OR (“case”[All Fields] AND “control”[All Fields]) OR “case control”[All Fields])
AND
(“phosphates”[MeSH Terms] OR “phosphates”[All Fields]) AND (“cardiovascular system”[MeSH Terms] OR (“cardiovascular”[All Fields] AND “system”[All Fields]) OR “cardiovascular system”[All Fields] OR “cardiovascular”[All Fields]) AND (“case‐control studies”[MeSH Terms] OR (“case‐control”[All Fields] AND “studies”[All Fields]) OR “case‐control studies”[All Fields] OR (“case”[All Fields] AND “control”[All Fields] AND “studies”[All Fields]) OR “case control studies”[All Fields])
AND
(“parathyroid hormone”[MeSH Terms] OR (“parathyroid”[All Fields] AND “hormone”[All Fields]) OR “parathyroid hormone”[All Fields]) AND (“phosphates”[MeSH Terms] OR “phosphates”[All Fields]) AND (“cardiovascular system”[MeSH Terms] OR (“cardiovascular”[All Fields] AND “system”[All Fields]) OR “cardiovascular system”[All Fields] OR “cardiovascular”[All Fields]) AND (“cohort studies”[MeSH Terms] OR (“cohort”[All Fields] AND “studies”[All Fields]) OR “cohort studies”[All Fields] OR “cohort”[All Fields])
AND
(“parathyroid hormone”[MeSH Terms] OR (“parathyroid”[All Fields] AND “hormone”[All Fields]) OR “parathyroid hormone”[All Fields]) AND (“phosphates”[MeSH Terms] OR “phosphates”[All Fields]) AND (“cardiovascular system”[MeSH Terms] OR (“cardiovascular”[All Fields] AND “system”[All Fields]) OR “cardiovascular system”[All Fields] OR “cardiovascular”[All Fields]) AND (“case‐control studies”[MeSH Terms] OR (“case‐control”[All Fields] AND “studies”[All Fields]) OR “case‐control studies”[All Fields] OR (“case”[All Fields] AND “control”[All Fields]) OR “case control”[All Fields])
AND
(“fibroblast growth factors”[MeSH Terms] OR (“fibroblast”[All Fields] AND “growth”[All Fields] AND “factors”[All Fields]) OR “fibroblast growth factors”[All Fields] OR (“fibroblast”[All Fields] AND “growth”[All Fields] AND “factor”[All Fields]) OR “fibroblast growth factor”[All Fields]) AND (“phosphates”[MeSH Terms] OR “phosphates”[All Fields]) AND (“cardiovascular system”[MeSH Terms] OR (“cardiovascular”[All Fields] AND “system”[All Fields]) OR “cardiovascular system”[All Fields] OR “cardiovascular”[All Fields]) AND (“cohort studies”[MeSH Terms] OR (“cohort”[All Fields] AND “studies”[All Fields]) OR “cohort studies”[All Fields] OR “cohort”[All Fields])
AND
(“fibroblast growth factors”[MeSH Terms] OR (“fibroblast”[All Fields] AND “growth”[All Fields] AND “factors”[All Fields]) OR “fibroblast growth factors”[All Fields] OR (“fibroblast”[All Fields] AND “growth”[All Fields] AND “factor”[All Fields]) OR “fibroblast growth factor”[All Fields]) AND (“phosphates”[MeSH Terms] OR “phosphates”[All Fields]) AND (“cardiovascular system”[MeSH Terms] OR (“cardiovascular”[All Fields] AND “system”[All Fields]) OR “cardiovascular system”[All Fields] OR “cardiovascular”[All Fields]) AND (“case‐control studies”[MeSH Terms] OR (“case‐control”[All Fields] AND “studies”[All Fields]) OR “case‐control studies”[All Fields] OR (“case”[All Fields] AND “control”[All Fields]) OR “case control”[All Fields])
No language restriction was applied. Previous review articles will be hand searched for other relevant studies.
Study selection, data extraction and assessment of methodology quality (bias)
Working Group experts in epidemiology will identify potential studies to be added in the draft review provided by EFSA. These experts will screen the full‐texts and identify studies for inclusion and identify and record reasons for exclusion of the ineligible studies. Disagreement will be solved through discussion or, if required, the working group will be consulted. Duplicate records will be identified and excluded and multiple reports that relate to the same study will collated so that each study rather than each report is the unit of interest in the evaluation.
Sources of bias in observational studies can be due to the study design and analytic methods. Using statistical adjustments in the models or matching procedures, may decrease the risk of bias, which can increase confidence in the results. The Newcastle–Ottawa Scale (NOS) will be used as a guideline for describing and interpreting studies. The latter scale for judging the quality of the studies will be used if a meta‐analysis is envisaged, as recommended by the Cochrane Collaboration (Higgins et al., 2008). This scale uses a star system to assess the quality of a study in three domains: selection, comparability and outcome (cohort studies) or exposure (case–control studies). The NOS assigns a maximum of four stars for selection, two stars for comparability and three stars for exposure/outcome. Therefore, nine stars reflect the highest quality. Any discrepancies will be addressed by a joint re‐evaluation of the original article by the epidemiology group. Studies in which mortality/and intermediate outcomes are the outcome will be given a different weight. Cross‐sectional studies are of limited value in assessing whether there is a true exposure‐outcome relationship, nonetheless they will be described in the opinion for completeness.
The following items will be included while describing each study:
Type of study (case–control/cohort/cross‐sectional)
Characteristics of the population and setting (e.g. age, sex, sample size, sources and methods of selection of participants, eligibility criteria, methods of case ascertainment and control selection, matching criteria and the number of controls per case)
Objective of the study
Exposure (e.g. type of dietary questionnaire and mode of assessment)
Type of outcome (incidence/mortality/intermediate outcomes)
Number of cases identified during the follow‐up (cohort)
Time of follow‐up and number of lost to follow‐up
-
Results of the main findings:
-
8.1
ORs or hazard ratios, with their 95% confidence intervals and p for trend if present and cut‐off values associated with the risk of cardiovascular diseases and/or stroke and/or intermediate outcomes and/or cardiovascular and/or stroke mortality
-
8.2
Confounding factors considered by the authors (main risk factors for the specific outcomes) and included in the multivariate analysis (e.g. age, sex, socioeconomic status and/or education, smoking, BMI, calcium, alcohol, vitamin D, total energy intake)
-
8.1
Subgroup analysis if conducted (e.g. sex and factors that may potentially affect phosphorus’ metabolism such as renal dysfunction)
Strength and limitation of each study.
Appendix D – The link between phosphates, bone metabolism and osteoporosis: epidemiology search protocol
Search 1
| Database | Coverage | Access |
|---|---|---|
| Embase | Inception‐present | http://www.embase.com |
| Pubmed | Inception‐present | http://www.ncbi.nlm.nih.gov/pubmed |
Search strategies
Embase
| No. | Query |
|---|---|
| #13 | #11 NOT #12 |
| #12 | ‘osteoporosis’/exp OR osteoporosis:ti,ab |
| #11 | #10 AND ([english]/lim OR [german]/lim) |
| #10 | #8 NOT #9 |
| #9 | (‘animal’/exp OR ‘nonhuman’/exp) NOT ‘human’/exp |
| #8 | #1 AND #7 |
| #7 | #2 OR #3 OR #4 OR #5 OR #6 |
| #6 | (broken NEAR/5 bone*):ti,ab |
| #5 | fracture*:ti,ab OR bmc:ti,ab OR bmd:ti,ab |
| #4 | bone*:ti,ab AND mineral:ti,ab AND concentration:ti,ab |
| #3 | (bone* NEAR/5 (content OR densit* OR health OR mass OR volume OR loss* OR metabolism OR mineral* OR disease*)):ti,ab |
| #2 | ‘bone health’/exp OR ‘bone density’/exp OR ‘bone disease’/de OR ‘bone mass’/exp OR ‘bone mineral’/exp OR ‘fracture’/exp OR ‘bone metabolism’/exp |
| #1 | ‘phosphate’/exp AND ‘dietary intake’/de OR (((phosphate OR phosphates) NEAR/15 intak*):ti,ab) |
PubMed
| No. | Query |
|---|---|
| #13 | #11 NOT #12 |
| #12 | ‘osteoporosis’/exp OR osteoporosis:ti,ab |
| #11 | #10 AND ([english]/lim OR [german]/lim) |
| #10 | #8 NOT #9 |
| #9 | (‘animal’/exp OR ‘nonhuman’/exp) NOT ‘human’/exp |
| #8 | #1 AND #7 |
| #7 | #2 OR #3 OR #4 OR #5 OR #6 |
| #6 | (broken NEAR/5 bone*):ti,ab |
| #5 | fracture*:ti,ab OR bmc:ti,ab OR bmd:ti,ab |
| #4 | bone*:ti,ab AND mineral:ti,ab AND concentration:ti,ab |
| #3 | (bone* NEAR/5 (content OR densit* OR health OR mass OR volume OR loss* OR metabolism OR mineral* OR disease*)):ti,ab |
| #2 | ‘bone health’/exp OR ‘bone density’/exp OR ‘bone disease’/de OR ‘bone mass’/exp OR ‘bone mineral’/exp OR ‘fracture’/exp OR ‘bone metabolism’/exp |
| #1 | ‘phosphate’/exp AND ‘dietary intake’/de OR (((phosphate OR phosphates) NEAR/15 intak*):ti,ab) |
Search 2
(“phosphates”[MeSH Terms] OR “phosphates”[All Fields]) AND ((“fractures, bone”[MeSH Terms] OR (“fractures”[All Fields] AND “bone”[All Fields]) OR “bone fractures”[All Fields] OR “fractures”[All Fields]) AND (“epidemiology”[Subheading] OR “epidemiology”[All Fields] OR “epidemiology”[MeSH Terms]))
(“phosphates”[MeSH Terms] OR “phosphates”[All Fields]) AND ((“fractures, bone”[MeSH Terms] OR (“fractures”[All Fields] AND “bone”[All Fields]) OR “bone fractures”[All Fields] OR “fracture”[All Fields]) AND (“cohort studies”[MeSH Terms] OR (“cohort”[All Fields] AND “studies”[All Fields]) OR “cohort studies”[All Fields] OR “cohort”[All Fields]))
((“phosphorus, dietary”[MeSH Terms] OR (“phosphorus”[All Fields] AND “dietary”[All Fields]) OR “dietary phosphorus”[All Fields] OR “phosphorus”[All Fields] OR “phosphorus”[MeSH Terms]) AND intake[All Fields]) AND ((“fractures, bone”[MeSH Terms] OR (“fractures”[All Fields] AND “bone”[All Fields]) OR “bone fractures”[All Fields] OR “fracture”[All Fields]) AND (“cohort studies”[MeSH Terms] OR (“cohort”[All Fields] AND “studies”[All Fields]) OR “cohort studies”[All Fields] OR “cohort”[All Fields]))
(“phosphorus, dietary”[MeSH Terms] OR (“phosphorus”[All Fields] AND “dietary”[All Fields]) OR “dietary phosphorus”[All Fields] OR “phosphorus”[All Fields] OR “phosphorus”[MeSH Terms]) AND (“fractures, bone”[MeSH Terms] OR (“fractures”[All Fields] AND “bone”[All Fields]) OR “bone fractures”[All Fields] OR “fractures”[All Fields]) AND (“case‐control studies”[MeSH Terms] OR (“case‐control”[All Fields] AND “studies”[All Fields]) OR “case‐control studies”[All Fields] OR (“case”[All Fields] AND “control”[All Fields] AND “study”[All Fields]) OR “case control study”[All Fields])
Phosphate [All Fields] AND (“fractures, bone”[MeSH Terms] OR (“fractures”[All Fields] AND “bone”[All Fields]) OR “bone fractures”[All Fields] OR “fractures”[All Fields]) AND (“case‐control studies”[MeSH Terms] OR (“case‐control”[All Fields] AND “studies”[All Fields]) OR “case‐control studies”[All Fields] OR (“case”[All Fields] AND “control”[All Fields] AND “study”[All Fields]) OR “case control study”[All Fields])
(“phosphoric acid”[Supplementary Concept] OR “phosphoric acid”[All Fields] OR “phosphoric acids”[MeSH Terms] OR (“phosphoric”[All Fields] AND “acids”[All Fields]) OR “phosphoric acids”[All Fields] OR (“phosphoric”[All Fields] AND “acid”[All Fields])) AND (“fractures, bone”[MeSH Terms] OR (“fractures”[All Fields] AND “bone”[All Fields]) OR “bone fractures”[All Fields] OR “fractures”[All Fields]) AND (“cohort studies”[MeSH Terms] OR (“cohort”[All Fields] AND “studies”[All Fields]) OR “cohort studies”[All Fields] OR “cohort”[All Fields])
Appendix E – Identity of the substances and specifications
Phosphoric acid
According to Commission Regulation (EU) No 231/2012, the food additive E 338 is identified as
Chemical name: Phosphoric acid
EINECS Number: 231‐633‐2
Chemical formula: H3PO4
Molecular weight: 98.00
Physical description: Clear, colourless, odourless, viscous liquid
CAS number: 7664‐38‐20
Solubility: Miscible with water and with ethanol
Phosphoric acid has a melting point of 42.4°C and a boiling point of 407°C (CRC, 2012a). Regarding acidity, the dissociation constants are pKa1 2.12, pKa2 7.21 and pKa3 12.67 (EFSA‐FEEDAP‐Panel, 2013). The partition coefficient (log p value) is −1.644 ± 0.350 (at a temperature of 25°C) (Calculated using Advanced Chemistry Development (ACD/Labs) Software V11.02 (© 1994–2013 ACD/Labs) (SciFinder, 2013a).
Synonyms include: Orthophosphoric acid and monophosphoric acid.
Monosodium phosphate
According to Commission Regulation (EU) No 231/201220), the food additive E 339(i) is identified as
Chemical name: Sodium dihydrogen monophosphate
EINECS Number: 231‐449‐2
Chemical formula: NaH2PO4 (anhydrous form), NaH2PO4 ∙ H2O (monohydrate form) or NaH2PO4 ∙ 2H2O (dehydrate form)
Molecular weight: 119.98 (anhydrous form), 138.00 (monohydrate form) or 156.01 (dehydrate form)
Physical description: White odourless, slightly deliquescent powder, crystals or granules
CAS number: 7558‐80‐7
Solubility: Freely soluble in water and insoluble in ethanol or ether
Monosodium phosphate (anhydrous) has a melting point of 200°C, at which temperature it decomposes (CRC, 2012a).
No information on log p value has been retrieved.
Synonyms include: Monosodium monophosphate; acid monosodium monophosphate; monosodium orthophosphate; monobasic sodium phosphate and sodium dihydrogen monophosphate.
Disodium phosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 339(ii) is identified as
Chemical name: Disodium hydrogen monophosphate and disodium hydrogen orthophosphate
EINECS Number: 231‐448‐7
Chemical formula: Na2H2PO4 (anhydrous form), Na2H2PO4 ∙ nH2O (n = 2,7 or 12) (hydrates form)
Molecular weight: 141.98 (anhydrous form)
Physical description: Anhydrous disodium phosphate occurs as a white, hygroscopic, odourless powder. The dihydrate occurs as a white crystalline, odourless solid. The heptahydrate occurs as white, odourless, efflorescent crystals or granular powder. The dodecahydrate occurs as a white, efflorescent, odourless powder or crystals
CAS number: 7558‐79‐4
Solubility: Disodium phosphate is freely soluble in water and insoluble in ethanol
No information on melting point or log p value has been retrieved.
Synonyms include: Disodium monophosphate; secondary sodium phosphate; disodium orthophosphate; dibasic sodium phosphate and disodium acid phosphate.
Trisodium phosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 339(iii) is identified as
Chemical name: Trisodium monophosphate, trisodium phosphate and trisodium orthophosphate
EINECS Number: 231‐509‐8
Chemical formula: Na3PO4 (anhydrous form), Na3PO4 ∙ nH2O (n = 1/2,1,6,8 or 12) (hydrates form)
Molecular weight: 163.94 (anhydrous form)
Physical description: White odourless crystals, granules or a crystalline powder
CAS number: 7601‐54‐9
Solubility|: Freely soluble in water and insoluble in ethanol
Trisodium phosphate (anhydrous) has a melting point of 1,583°C (CRC, 2012b).
No information on log p value has been retrieved.
Synonyms include: Tribasic sodium phosphate and sodium phosphate.
Monopotassium phosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 340(i) is identified as
Chemical name: Potassium dihydrogen phosphate, monopotassium dihydrogen orthophosphate and monopotassium dihydrogen monophosphate
EINECS Number: 231‐913‐4
Chemical formula: KH2PO4
Molecular weight: 136.09
Physical description: Odourless, colourless crystals or a white granular or crystalline powder
CAS number: 7778‐77‐0
Solubility: Freely soluble in water and insoluble in ethanol
Monopotassium phosphate has a melting point of 253°C (CRC, 2012e; SciFinder, 2013c).
No information on log p value has been retrieved.
Synonyms include: Monobasic potassium phosphate; monopotassium monophosphate and mono potassium orthophosphate.
Dipotassium phosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 340(ii) is identified as
Chemical name: Dipotassium hydrogen monophosphate, dipotassium hydrogen phosphate and dipotassium hydrogen orthophosphate
EINECS Number: 231‐834‐5
Chemical formula: K2HPO4
Molecular weight: 174.18
Physical description: Colourless or white granular powder, crystals or masses and is a deliquescent and hygroscopic substance
CAS number: 7758‐11‐4
Solubility: Freely soluble in water and insoluble in ethanol
Dipotassium phosphate has a melting point of 151.5–154.0°C where it decomposes (CRC, 2012c).
No information on log p value has been retrieved.
Synonyms include: Dipotassium monophosphate; secondary potassium phosphate; dipotassium orthophospahte and dibasic potassium phosphate.
Tripotassium phosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 340(i) is identified as
Chemical name: Tripotassium monophosphate, tripotassium phosphate and tripotassium orthophosphate
EINECS Number: 231‐907‐1
Chemical formula: K3PO4 (anhydrous form), K3PO4 ∙ nH2O (n = 1 or 3) (hydrates form)
Molecular weight: 212.27 (anhydrous form)
Physical description: Colourless or white, odourless hygroscopic crystals or granules
CAS number: 7778‐53‐2
Solubility: Freely soluble in water and insoluble in ethanol
Tripotassium phosphate (anhydrous) has a melting point of 1,340°C (CRC, 2012d).
No information on log p value has been retrieved.
Synonyms include: Tribasic potassium phosphate; potassium phosphate and tripotassium orthophosphate.
Calcium dihydrogen phosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 341 (i) is identified as
Chemical name: Calcium dihydrogen phosphate
EINECS Number: 231‐837‐1
Chemical formula: Ca(H2PO4)2 anhydrous or Ca(H2PO4)2 ∙ H2O monohydrate
Molecular weight: Anhydrous 234.05; monohydrate 252.07
Physical description: Hygroscopic white crystals or granules or granular powder
CAS number: anhydrous 7758‐23‐8; monohydrate 10031‐30‐8
Solubility: Sparingly soluble in water, insoluble in ethanol
Calcium dihydrogen phosphate monohydrate has a melting point of 100°C where it decomposes (CRC, 2012d).
No information on log p value has been retrieved.
Synonyms include: Monobasic calcium phosphate; monocalcium orthophosphate; monocalcium phosphate; calcium biphosphate and acid calcium phosphate.
Calcium hydrogen phosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 341(ii) is identified as
Chemical name: Calcium monohydrogen phosphate, calcium hydrogen orthophosphate and secondary calcium phosphate
EINECS Number: 231‐826‐1
Chemical formula: CaHPO4 anhydrous or Ca(HPO4) ∙ 2H2O dihydrate
Molecular weight: anhydrous 136.06; dihydrate 172.09
Physical description: Hygroscopic white crystals or granules or granular powder
CAS number: anhydrous 7757‐9309
Solubility: Sparingly soluble in water, insoluble in ethanol
No information on melting point or log p value has been retrieved.
Synonyms include: Dibasic calcium phosphate and dicalcium phosphate
Tricalcium phosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 341(iii) is identified as
Chemical name: Pentacalcium hydroxy monophosphate and tricalcium monophosphate
EINECS Number: 235‐330‐6
Chemical formula: Ca5(PO4)3 ∙ OH or Ca3(PO4)2
Molecular weight: 502 Ca5(PO4)3; 310 Ca3(PO4)2
Physical description: White, odourless powder which is stable in air
CAS number: 7758‐87‐4
Solubility: Practically insoluble in water; insoluble in ethanol, soluble in dilute hydrochloric and nitric acid
Tricalcium phosphate has a melting point of 1,670°C (CRC, 2012c; SciFinder, 2013b).
No information on log p value has been retrieved.
Synonyms include: Calcium phosphate, tribasic; calcium orthophosphate; pentacalcium hydroxy monophosphate and calcium hydroxyapatite.
Monomagnesium phosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 343(i) is identified as
Chemical name: Monomagnesium dihydrogen monophosphate
EINECS Number: 236‐004‐6
Chemical formula: Mg(H2PO4)2 ∙ nH2O (n = 0–4)
Molecular weight: 218.3 (anhydrous), 254.3 (dihydrate), 290.3 (tetrahydrate)
Physical description: White, odourless, crystalline powder
CAS number: 13092‐66‐5 (anhydrous),15609‐87‐7 (dehydrate)
Solubility: Slightly soluble in water
No information on melting point or log p value has been retrieved.
Synonyms include: Magnesium dihydrogen phosphate; magnesium phosphate, monobasic; monomagnesium orthophosphate.
Dimagnesium phosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 343(ii) is identified as
Chemical name: dimagnesium monohydrogen monophosphate
EINECS Number: 231‐823‐5
Chemical formula: MgHPO4 ∙ nH2O (n = 0–3)
Molecular weight: 120.30 (anhydrous)
Physical description: white, odourless, crystalline powder
CAS number: 7757‐86‐0
Solubility: Slightly soluble in water, soluble in dilute acids, but insoluble in ethanol
Dimagnesium phosphate has a melting point of 550°C where it decomposes (CRC, 2012b).
No information on log p value has been retrieved.
Synonyms include: Magnesium hydrogen phosphate; magnesium phosphate, dibasic; dimagnesium orthophosphate and secondary magnesium phosphate.
Disodium diphosphate
According to Commission Regulation (EU) No 231/201220), the food additive E 450(i) is identified as
Chemical name: Disodium dihydrogen diphosphate
EINECS Number: 231‐972‐6
Chemical formula: Na2H2P2O7
Molecular weight: 221.94
Physical description: White powder or grains
CAS number: 7758‐16‐9
Solubility: Soluble in water
The melting point is reported as > 450°C (Haynes, 2010).
Synonyms include: disodium dihydrogen diphosphate, disodium pyrophosphate, disodium dihydrogen pyrophosphate and acid sodium pyrophosphate.
Trisodium diphosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 450(ii) is identified as
Chemical name:
EINECS Number: 238‐735‐6
Chemical formula: Na3HP2O7 (anhydrous form) or Na3HP2O7 ∙ H2O (monohydrate form)
Molecular weight: 243.93 (anhydrous form), 261.95 (monohydrate form)
Physical description: White powder or grains
CAS number: 14691‐80‐6 (anhydrous form), 26573‐04‐6 (monohydrate form)
Solubility: Soluble in water
Synonyms include: trisodium monohydrogen diphosphate, trisodium monohydrogen pyrophosphate, trisodium hydrogen phosphate, trisodium pyrophosphate and acid trisodium pyrophosphate.
Tetrasodium diphosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 450(iii) is identified as
Chemical name: Tetrasodium phosphate
EINECS Number: 231‐767‐1
Chemical formula: Na4P2O7 (anhydrous form) or Na4P2O7 ∙ 10H2O (decahydrate form)
Molecular weight: 265.94 (anhydrous form), 446.09 (decahydrate form)
Physical description: Colourless or white crystals or a white crystalline or granular powder
CAS number: 7722‐88‐5
Solubility: Soluble in water
The melting point is reported as 988°C (Haynes, 2010).
Synonyms include: include tetrasodium pyrophosphate, tetrasodium disphosphate, tetrasodium phosphate and sodium pyrophosphate.
Tetrapotassium diphosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 450(v) is identified as
Chemical name: Tetrapotassium diphosphate
EINECS Number: 230‐785‐7
Chemical formula: K4P2O7
Molecular weight: 330.34 (anhydrous form)
Physical description: Colourless crystals or a white, very hygroscopic powder
CAS number: 7320‐34‐5
Solubility: Soluble in water
The substance is reported to decompose at 1,300°C (Haynes, 2010).
Synonyms include: Tetrapotassium pyrophosphate, potassium pyrophosphate and tetrapotassium salt of diphosphoric acid.
Dicalcium diphosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 450(vi) is identified as
Chemical name: Dicalcium diphosphate, dicalcium pyrophosphate
EINECS Number: 232‐221‐5
Chemical formula: Ca2P2O7
Molecular weight: 254.12
Physical description: Fine, white, odourless powder
CAS number: 7790‐76‐3
Solubility: Insoluble in water
Synonyms include: Calcium pyrophosphate and dicalcium pyrophosphate.
Calcium dihydrogen diphosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 450(vii) is identified as
Chemical name: Calcium dihydrogen diphosphate
EINECS Number: 238‐933‐3
Chemical formula: CaH2P2O7
Molecular weight: 215.97
Physical description: White crystals or powder
CAS number: 14866‐19‐4
Solubility: Not specified in Commission Regulation (EU) No 231/2012
Synonyms include: Acid calcium pyrophosphate, monocalcium dihydrogen pyrophosphate, calcium dihydrogen pyrophosphate and monocalcium dihydrogen diphosphate.
Magnesium dihydrogen diphosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 450(ix) is identified as
Chemical name: Monomagnesium dihydrogen diphosphate
EINECS Number: 244‐016‐8
Chemical formula: MgH2P2O7
Molecular weight: 200.25
Physical description: White crystals or powder
CAS number: 13446‐24‐7
Solubility: Slightly soluble in water, practically insoluble in ethanol
Synonyms include: Acid magnesium pyrophosphate, monomagnesium dihydrogen pyrophosphate; magnesium diphosphate, magnesium pyrophosphate.
Pentasodium triphosphate
According to Commission Regulation (EU) No 231/201220), the food additive E 451(i) is identified as
Chemical name: Pentasodium triphosphate
EINECS Number: 231‐838‐7
Chemical formula: Na5P3O10 ∙ nH2O (n = 0 or 6)
Molecular weight: 367.86 (anhydrous form), 475.94 (hexahydrate form)
Physical description: White, slightly hygroscopic granules or powder
CAS number: 7758‐29‐4
Solubility: Freely soluble in water and insoluble in ethanol
The melting point is reported as 622°C (Haynes, 2010).
Synonyms include: pentasodium tripolyphosphate and sodium tripolyphosphate.
Pentapotassium triphosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 451(ii) is identified as
Chemical name: Pentapotassium triphosphate, pentapotassium tripolyphosphate
EINECS Number: 237‐574‐9
Chemical formula: K5P3O10
Molecular weight: 448.82
Physical description: White, very hygroscopic powder or granules
CAS number: 13845‐36‐8
Solubility: Very soluble in water
Synonyms include: potassium triphosphate and potassium tripolyphosphate.
Sodium polyphosphate
According to Commission Regulation (EU) No 231/201220), the food additive E 452(i) is identified as
Chemical name: Sodium polyphosphate
Commission Regulation (EU) No 231/2012 is laying down specifications for E 452(i), in two forms.
Soluble sodium polyphosphate
EINECS Number: 272‐808‐3
Chemical formula: H(n+2)PnO(3n+1) where ‘n’ is not less than 2
Molecular weight: (102)n
Physical description: Colourless or white, transparent platelets, granules or powders
CAS number: 68915‐31‐1, 10124‐56‐8 and 10362‐03‐2
Solubility: Very soluble in water
Synonyms include: sodium hexametaphosphate; sodium tetrapolyphosphate; Graham's salt; sodium polyphosphates, glassy; sodium polymetaphosphate; sodium metaphosphate.
Soluble sodium polyphosphate is described in Commission Regulation (EU) No 231/2012 as follows:
‘Soluble sodium polyphosphates are obtained by fusion and subsequent chilling of sodium orthophosphates. These compounds are a class consisting of several amorphous, water‐soluble polyphosphates composed of linear chains of metaphosphate units, (NaPO3)x where x ≥ 2, terminated by Na2PO4 groups. These substances are usually identified by their Na2O/P2O5 ratio or their P2O5 content. The Na2O/P2O5 ratios vary from about 1.3 for sodium tetrapolyphosphate, where x = approximately 4; to about 1.1 for Graham's salt, commonly called sodium hexametaphosphate, where x = 13 to 18; and to about 1.0 for the higher molecular weight sodium polyphosphates, where x = 20 to 100 or more. The pH of their solutions varies from 3.0 to 9.0’.
JECFA specification describes the chain structure as ‘metaphosphate units, (NaPO3)x where x = 2’; this is at odds with this point in the definition above and also with the comments in JECFA on the composition of various forms, which are the same as those in the definition above.
The REACH Registration Dossier on sodium metaphosphate (REACH Registration Dossier, online) submitted to the European Chemicals Agency (ECHA) includes a melting point of > 723 K, and a solubility of 54.8–59.7% (w/w).
Insoluble sodium polyphosphate
EINECS Number: 272‐808‐3
Chemical formula: H(n+2)PnO(3n+1) where ‘n’ is not less than 2
Molecular weight: (102)n
Physical description: A white crystalline powder
CAS number: No CAS registry number is included in Commission Regulation (EU) No 231/2012 for this form
Solubility: Insoluble in water, soluble in mineral acids and in solutions of potassium and ammonium (but not sodium) chlorides
Synonyms include: Insoluble sodium metaphosphate; Maddrell's salt; insoluble sodium polyphosphate; IMP
This form of sodium polyphosphate is not included in the JECFA specifications.
Potassium polyphosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 452 (ii) is identified as
Chemical name: Potassium polyphosphate
EINECS Number: 232‐212‐6
Chemical formula: (KPO3)n
Molecular weight: (102)n
Physical description: Fine white powder or crystals or colourless glassy platelets
CAS number: 7790‐53‐6
Synonyms include: One gram dissolves in 100 mL of a 1 in 25 solution of sodium acetate
Synonyms include: Include potassium metaphosphate, potassium polymetaphosphate and Kurrol salt.
Sodium calcium polyphosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 452 (iii) is identified as
Chemical name: sodium calcium polyphosphate
EINECS Number: 233‐782‐921
Chemical formula: (NaPO3)n CaO where n is typically 5
Molecular weight: No molecular weight is included in Commission Regulation (EU) No 231/2012 and in JECFA specifications
Physical description: White glassy crystals or spheres
CAS number: No CAS registry number is included in either Commission Regulation (EU) No 231/2012 or the JECFA specifications for this substance.
Solubility: Not included in either Commission Regulation (EU) No 231/2012 or the JECFA specifications for this substance
Synonyms include: Sodium calcium polyphosphate, glassy.
Calcium polyphosphate
According to Commission Regulation (EU) No 231/2012, the food additive E 452 (iv) is identified as
Chemical name: calcium polyphosphate
EINECS Number: 236‐769‐6
Chemical formula: (CaP2O6)n
Molecular weight: (198)n
Physical description: Odourless, colourless crystals or white powder
CAS number: No CAS registry number is included in either Commission Regulation (EU) No 231/2012 or the JECFA specifications for this substance, entering the EINECS number in the ESIS database and the ECHA public database gives a CAS registry number of 13477‐39‐9
Solubility: Usually sparingly soluble in water, soluble in acid medium
Synonyms include: Calcium metaphosphate and calcium polymetaphosphate.
The specifications for phosphoric acid (E 338), monocalcium phosphate (E 341(i)), dicalcium phosphate (E 341(ii)), tricalcium phosphate (E 341(iii)), monomagnesium phosphate (E 343(i)), dimagnesium phosphate (E 343(ii)) monosodium phosphate (E 339(i)), disodium phosphate (E 339(ii)), trisodium phosphate (E 339(iii)), monopotassium phosphate (E 340(i)), dipotassium phosphate (E 340(ii)), tripotassium phosphate (E 340(iii)), disodium diphosphate (E 450(i)), trisodium diphosphate (E 450(ii)), tetrasodium diphosphate (E 450(iii)), tetrapotassium diphosphate (E 450(v)), dicalcium diphosphate (E 450(vi)), calcium dihydrogen diphosphate (E 450(vii)), pentasodium triphosphate (E 451(i)), pentapotassium triphosphate (E 451(ii)), sodium polyphosphate (E 452(i)), potassium polyphosphate (E 452(ii)), sodium calcium polyphosphate (E 452(iii)) and calcium polyphosphate (E 452(iv)) as defined in the Commission Regulation (EU) No 231/2012 and by JECFA are listed in Tables E.1–10b.
Table E.1.
Specifications for phosphoric acid (E 338) according to Commission Regulation (EU) No 231/2012 and JECFA (2002)
| Commission Regulation (EU) No 231/2012 | JECFA (2002) | |
|---|---|---|
| Definition | Phosphoric acid | Phosphoric acid, orthophosphoric acid |
| Assay | Content not less than 67.0% and not more than 85.7%. Phosphoric acid is commercially available as an aqueous solution at variable concentrations | Not less than 75% and not less than the minimum or within the range of percent claimed by the vendor |
| Description | Clear, colourless, viscous liquid | Clear, colourless, odourless, viscous liquid |
| Identification |
Test for acid: Passes test Test for phosphate: Passes test |
Solubility: Miscible with water and with ethanol Test for acid: Strongly acid, even at high dilution Test for phosphate: Neutralise a few millilitres of phosphoric acid and add dilute nitric acid TS. Then, add an equal volume of ammonium molybdate TS and warm. A bright canary‐yellow precipitate is obtained which is soluble in dilute ammonia TS |
| Puritya |
Volatile acids: not more than 10 mg/kg (as acetic acid) Chlorides: not more than 200 mg/kg (expressed as chlorine) Nitrates: not more than 5 mg/kg (as NaNO3) Sulfates: not more than 1,500 mg/kg (as CaSO4) Fluoride: not more than 10 mg/kg (expressed as fluorine) Arsenic: not more than 1 mg/kg Cadmium: not more than 1 mg/kg Lead: not more than 1 mg/kg Mercury: not more than 1 mg/kg |
Nitrates: not more than 5 mg/kg Volatile acids: not more than 10 mg/kg as acetic acid Chlorides (Vol. 4): not more than 200 mg/kg as chlorine Sulfates (Vol. 4): not more than 0.15% Fluoride (Vol. 4): not more than 10 mg/kg Arsenic (Vol. 4): not more than 3 mg/kg Lead (Vol. 4): not more than 4 mg/kg |
This specification refers to a 75% aqueous solution.
Table E.2.
Specifications for monosodium phosphate (E 339(i)) according to Commission Regulation (EU) No 231/2012 and JECFA (2006b,c,d,e,f)
| Commission Regulation No 231/2012 | JECFA (2006b,c,d,e,f) | |
|---|---|---|
| Assay |
After drying at 60°C for 1 h and then at 105°C for 4 h, contains not less than 97% of NaH2PO4 P2O5 content between 58.0% and 60.0% on the anhydrous basis |
Not less than 97% after drying |
| Description | A white odourless, slightly deliquescent powder, crystals or granules | White odourless, slightly deliquescent powder, crystals, or granules |
| Identification | ||
| Test for sodium | Passes test | Passes test |
| Test for phosphate | Passes test | Passes test |
| Solubility | Freely soluble in water. Insoluble in ethanol or ether | Freely soluble in water; insoluble in ethanol, ether or chloroform |
| pH | Between 4.1 and 5.0 (1% solution) | 4.2–4.6 (1 in 100 solution) |
| Test for orthophosphate | – | To a 1% solution of the sample add silver nitrate TS; the yellow precipitate formed is soluble in dilute nitric acid TS |
| Purity | ||
| Loss on drying | The anhydrous salt loses not more than 2.0%, the monohydrate not more than 15.0%, the dihydrate not more than 25% (60°C, 1 h then 105°C, 4 h) |
Anhydrous: Not more than 2% (60°C, 1 h, then 105°C, 4 h) Monohydrate: Not more than 15% (60°C, 1 h, then 105°C, 4 h) Dihydrate: Not more than 25% (60°C, 1 h, then 105°C, 4 h) |
| Water‐insoluble matter | Not more than 0.2% on the anhydrous basis | – |
| Free acid and disodium phosphate | – | 2.00 g of the sample dissolved in 40 mL of water require for neutralisation not more than 0.3 mL of either N sodium hydroxide or N sulfuric acid, using methyl orange TS as indicator |
| Fluoride | Not more than 10 mg/kg (expressed as fluorine) | Not more than 10 mg/kg |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg (Method II) |
| Cadmium | Not more than 1 mg/kg | |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
Table E.3.
Specifications established for disodium phosphate (E 339(ii)) according to Commission Regulation (EU) No 231/2012 and JECFA (2006a)
| Commission Regulation No 231/2012 | JECFA (2006b,c,d,e,f) | |
|---|---|---|
| Assay |
After drying at 40°C for 3 h and subsequently at 105°C for 5 h, contains not less than 98% of Na2HPO4 P2O5 content between 49% and 51% on the anhydrous basis |
Not less than 98.0% after drying |
| Description | Anhydrous disodium hydrogen phosphate is a white, hygroscopic, odourless powder. Hydrated forms available include the dihydrate: a white crystalline, odourless solid; the heptahydrate: white, odourless, efflorescent crystals or granular powder; and the dodecahydrate: white, efflorescent, odourless powder or crystals |
Anhydrous: White, hygroscopic, odourless powder Dihydrate: White crystalline, odourless solid Heptahydrate: White, odourless, efflorescent crystals or granular powder Dodecahydrate: White, efflorescent, odourless powder or crystals |
| Identification | ||
| Test for sodium | Passes test | Passes test |
| Test for phosphate | Passes test | Passes test |
| Solubility | Freely soluble in water. Insoluble in ethanol | Freely soluble in water; insoluble in ethanol |
| pH | Between 8.4 and 9.6 (1% solution) | 9.0–9.6 (1 in 100 solution) |
| Test for orthophosphate | – | Dissolve 0.1 g of the sample in 10 mL water, acidify slightly with dilute acetic acid TS and add 1 mL of silver nitrate TS. A yellow precipitate is formed |
| Purity | ||
| Loss on drying | The anhydrous salt loses not more than 5.0%, the dihydrate not more than 22.0%, the heptahydrate not more than 50.0%, the dodecahydrate not more than 61.0% (40°C, 3 h then 105°C, 5 h) |
Anhydrous: Not more than 5.0% (40°C, 3 h, then 105°C, 5 h). Dihydrate: Not more than 22.0% (40°C, 3 h, then 105°C, 5 h) Heptahydrate: Not more than 50.0% (40°C, 3 h, then 105°C, 5 h) Dodecahydrate: Not more than 61.0% (40°C, 3 h, then 105°C, 5 h) |
| Water‐insoluble matter/substances | Not more than 0.2% on the anhydrous basis | Not more than 0.2% |
| Fluoride | Not more than 10 mg/kg (expressed as fluorine) | Not more than 50 mg/kg (Method I or III) |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg (Method II) |
| Cadmium | Not more than 1 mg/kg | |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
Table E.4.
Specifications established for trisodium phosphate (E 339(iii)) according to Commission Regulation (EU) No 231/2012 and JECFA (2006a)
| Commission Regulation No 231/2012 | JECFA (2006b,c,d,e,f) | |
|---|---|---|
| Assay |
Sodium phosphate anhydrous and the hydrated forms, with the exception of the dodecahydrate, contain not less than 97.0% of Na3PO4 calculated on the dried basis Sodium phosphate dodecahydrate contains not less than 92.0% of Na3PO4 calculated on the ignited basis P2O5 content between 40.5% and 43.5% on the anhydrous basis |
Anhydrous, hemihydrate and monohydrate: Not less than 97.0% calculated on the dried basis Dodecahydrate: Not less than 92.0% calculated on the ignited basis |
| Description | White odourless crystals, granules or crystalline powder | White odourless crystals, granules or a crystalline powder; hydrated forms available include hemi‐ and monohydrates, hexahydrate, octahydrate, decahydrate and dodecahydrate; the dodecahydrate contains 1/4 mol of sodium hydroxide |
| Identification | ||
| Test for sodium | Passes test | To 5 mL of a 1 in 20 solution of the sample add 1 mL of acetic acid TS and 1 mL of uranyl zinc acetate TS. A yellow crystalline precipitate is formed within a few min |
| Test for phosphate | Passes test | To 5 mL of a 1 in 100 solution of the sample add 1 mL of concentrated nitric acid and 5 mL of ammonium molybdate TS and warm. A bright canary‐yellow precipitate is obtained |
| Solubility | Freely soluble in water. Insoluble in ethanol | Freely soluble in water; insoluble in ethanol |
| pH | Between 11.5 and 12.5 (1% solution) | 11.5–12.5 (1 in 100 solution) |
| Test for orthophosphate | – | Dissolve 0.1 g of the sample in 10 mL water, acidify slightly with dilute acetic acid TS and add 1 mL of silver nitrate TS. A yellow precipitate is formed |
| Purity | ||
| Loss on ignition | When dried at 120°C for 2 h and then ignited at about 800°C for 30 min, the losses in weight are as follows: anhydrous not more than 2.0%, monohydrate not more than 11.0%, dodecahydrate: between 45.0% and 58.0% |
Anhydrous: Not more than 2% (120°C, 2 h, then 800°C, 30 min) Monohydrate: Not more than 11% (120°C, 2 h, then 800°C, 30 min) Dodecahydrate: 45–58% (120°C, 2 h, then 800°C, 30 min) |
| Water‐insoluble matter/substances | Not more than 0.2% on the anhydrous basis | Not more than 0.2% |
| Fluoride | Not more than 10 mg/kg (expressed as fluorine) | Not more than 50 mg/kg (Method I or III) |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg (Method II) |
| Cadmium | Not more than 1 mg/kg | |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
Table E.5.
Specifications established for monopotassium phosphate (E 340(i)) according to Commission Regulation (EU) No 231/2012 and JECFA (2006a)
| Commission Regulation No 231/2012 | JECFA (2006b,c,d,e,f) | |
|---|---|---|
| Assay |
Content not less than 98.0% after drying at 105°C for 4 h P2O5 content between 51.0% and 53.0% on the anhydrous basis |
Not less than 98.0% after drying |
| Description | Odourless, colourless crystals or white granular or crystalline powder | Odourless, colourless crystals or white granular or crystalline powder |
| Identification | ||
| Test for potassium | Passes test | Passes test |
| Test for phosphate | Passes test | Passes test |
| Solubility | Freely soluble in water. Insoluble in ethanol | Freely soluble in water; insoluble in ethanol |
| pH | Between 4.2 and 4.8 (1% solution) | 4.2–4.7 (1 in 100 solution) |
| Test for orthophosphate | – | To 5 mL of a 1 in 100 solution of the sample, add silver nitrate TS. A yellow precipitate is obtained |
| Purity | ||
| Loss on drying | Not more than 2.0% (105°C, 4 h) | Not more than 2% (105°C, 4 h) |
| Water‐insoluble matter/substances | Not more than 0.2% on the anhydrous basis | Not more than 0.2% |
| Fluoride | Not more than 10 mg/kg (expressed as fluorine) |
Not more than 10 mg/kg See description under TESTS |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg (Method II) |
| Cadmium | Not more than 1 mg/kg | – |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
Table E.6.
Specifications established for dipotassium phosphate (E 340(ii)) according to Commission Regulation (EU) No 231/2012 and JECFA (2006a)
| Commission Regulation No 231/2012 | JECFA (2006b,c,d,e,f) | |
|---|---|---|
| Assay |
Content not less than 98% after drying at 105°C for 4 h P2O5 content between 40.3% and 41.5% on the anhydrous basis |
Not less than 98.0% after drying |
| Description | Colourless or white granular powder, crystals or masses; deliquescent substance, hygroscopic | Colourless or white granular powder, crystals or masses; deliquescent |
| Identification | ||
| Test for potassium | Passes test | Passes test |
| Test for phosphate | Passes test | Passes test |
| Solubility | Freely soluble in water. Insoluble in ethanol | Freely soluble in water, insoluble in ethanol |
| pH | Between 8.7 and 9.4 (1% solution) | 8.7–9.3 (1 in 100 solution) |
| Test for orthophosphate | Dissolve 0.1 g of the sample in 10 mL water, acidify slightly with dilute acetic acid TS and add 1 mL of silver nitrate TS. A yellow precipitate is formed | |
| Purity | ||
| Loss on drying | Not more than 2.0% (105°C, 4 h) | Not more than 5% (105°C, 4 h) |
| Water‐insoluble matter/substances | Not more than 0.2% (on the anhydrous basis) | Not more than 0.2% |
| Fluoride | Not more than 10 mg/kg (expressed as fluorine) |
Not more than 10 mg/kg See description under TESTS |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
Table E.7.
Specifications established for tripotassium phosphate (E 340(iii)) according to Commission Regulation (EU) No 231/2012 and JECFA (2006a)
| Commission Regulation 231/2012 | JECFA (2006b,c,d,e,f) | |
|---|---|---|
| Assay |
Content not less than 97% calculated on the ignited basis P2O5 content between 30.5% and 34.0% on the ignited basis |
Not less than 97.0% of K3PO4, calculated on the ignited basis |
| Description | Colourless or white, odourless hygroscopic crystals or granules. Hydrated forms available include the monohydrate and trihydrate | Colourless or white, odourless hygroscopic crystals or granules; hydrated forms available include the monohydrate and trihydrate |
| Identification | ||
| Test for potassium | Passes test | To a 1 in 100 solution of the sample add 1 volume of saturated sodium hydrogen tartrate solution and 1 volume of ethanol and shake. A white crystalline precipitate is formed |
| Test for phosphate | Passes test | To 5 mL of a 1 in 100 solution of the sample add 1 mL of concentrated nitric acid and 5 mL of ammonium molybdate TS and warm. A bright canary‐yellow precipitate is obtained |
| Solubility | Freely soluble in water. Insoluble in ethanol | Freely soluble in water; insoluble in ethanol |
| pH | Between 11.5 and 12.3 (1% solution) | 11.5–12.5 (1 in 100 solution) |
| Test for orthophosphate | – | Dissolve 0.1 g of the sample in 10 mL water, acidify slightly with dilute acetic acid TS and add 1 mL of silver nitrate TS. A yellow precipitate is formed |
| Purity | ||
| Loss on ignition | Anhydrous: not more than 3.0%; hydrated: not more than 23.0% (determined by drying at 105°C for 1 h and then ignite at about 800 ± 25°C for 30 min) |
Anhydrous: Not more than 3% (120°C, 2 h, then 800°C, 30 min) Hydrated: Not more than 23% (120°C, 2 h, then 800°C, 30 min) |
| Water‐insoluble matter/substances | Not more than 0.2% (on the anhydrous basis) | Not more than 0.2% |
| Fluoride | Not more than 10 mg/kg (expressed as fluorine) |
Not more than 10 mg/kg See description under TESTS |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg (Method II) |
| Cadmium | Not more than 1 mg/kg | – |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
Table E.8.
Specifications established for calcium dihydrogen phosphate (E 341 (i)) according to Commission Regulation (EU) No 231/2012 and JECFA (2006a)
| Commission Regulation No 231/2012 | JECFA (2006b,c,d,e,f) | |
|---|---|---|
| Assay |
Content not less than 95% on the dried basis P2O5 content between 55.5% and 61.1% on the anhydrous basis |
Anhydrous: Not less than 16.8% and not more than 18.3% of Ca Monohydrate: Not less than 15.9% and not more than 17.7% of Ca |
| Description | Granular powder or white, deliquescent crystals or granules | Hygroscopic white crystals or granules, or granular powder |
| Identification | ||
| Solubility | – | Sparingly soluble in water, insoluble in ethanol |
| Test for calcium | Passes test | Passes test |
| Test for phosphate | Passes test | Passes test |
| CaO content |
Between 23.0% and 27.5% (anhydrous) Between 19.0% and 24.8% (monohydrate) |
|
| Purity | ||
| Loss on drying |
Anhydrous: not more than 14% (105°C, 4 h) Monohydrate: not more than 17.5% (105°C, 4 h) |
Monohydrate: Not more than 1% (60°C, 3 h) |
| Loss on ignition |
Anhydrous: not more than 17.5% (after ignition at 800 ± 25°C for 30 min) Monohydrate: not more than 25.0% (determined by drying at 105°C for 1 h, then ignite at 800 ± 25°C for 30 min) |
Anhydrous: Between 14.0% and 15.5% (800°C, 30 min) |
| Fluoride | Not more than 30 mg/kg (expressed as fluorine) |
Not more than 50 mg/kg Anhydrous: Determine as directed in Method II Monohydrate: Proceed as directed under Method IV |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg (Method II) |
| Cadmium | Not more than 1 mg/kg | |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
| Aluminium |
Not more than 70 mg/kg (only if added to food for infants and young children) Not more than 200 mg/kg (for all uses except food for infants and young children) |
– |
Table E.9.
Specifications established for calcium hydrogen phosphate (E 341(ii)) according to Commission Regulation (EU) No 231/2012 and JECFA (2006a)
| Commission Regulation No 231/2012 | JECFA (2006b,c,d,e,f) | |
|---|---|---|
| Assay |
Dicalcium phosphate, after drying at 200°C for 3 h, contains not less than 98% and not more than the equivalent of 102% of CaHPO4 P2O5 content between 50.0% and 52.5% on the anhydrous basis |
Not less than 98.0% and not more than the equivalent of 102.0% after drying |
| Description | White crystals or granules, granular powder or powder | White crystals or granules, granular powder or powder |
| Identification | ||
| Solubility | Sparingly soluble in water. Insoluble in ethanol | Sparingly soluble in water; insoluble in ethanol |
| Test for calcium | Passes test | Passes test |
| Test for phosphate | Passes test | Passes test |
| Purity | ||
| Loss on drying | – |
Anhydrous: Not more than 2% (200°C, 3 h) Dihydrate: Not less than 18% and not more than 22% (200°C, 3 h) |
| Loss on ignition | Not more than 8.5% (anhydrous), or 26.5% (dihydrate) after ignition at 800 ± 25°C for 30 min | – |
| Fluoride | Not more than 50 mg/kg (expressed as fluorine) | Not more than 50 mg/kg (Method I or III) |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg (Method II) |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Mercury | Not more than 1 mg/kg | – |
| Aluminium |
Not more than 100 mg/kg for the anhydrous form and not more than 80 mg/kg for the dihydrated form (only if added to food for infants and young children) Not more than 600 mg/kg for the anhydrous form and not more than 500 mg/kg for the dihydrated form (for all uses except food for infants and young children). This applies until 31 March 2015 Not more than 200 mg/kg for the anhydrous form and the dihydrated form (for all uses except food for infants and young children). This applies from 1 April 2015 |
– |
Table E.10.
Specifications established for tricalcium phosphate (E 341(iii)) according to Commission Regulation (EU) No 231/2012 and JECFA (2006a)
| Commission Regulation No 231/2012 | JECFA (2006b,c,d,e,f) | |
|---|---|---|
| Assay |
Content not less than 90% calculated on the ignited basis P2O5 content between 38.5% and 48.0% on the anhydrous basis |
Not less than the equivalent of 90% of Ca3(PO4)2, calculated on the ignited basis |
| Description | A white, odourless powder which is stable in air | White, odourless powder which is stable in air |
| Identification | ||
| Solubility | Practically insoluble in water; insoluble in ethanol, soluble in dilute hydrochloric and nitric acid | Practically insoluble in water; insoluble in ethanol, soluble in dilute hydrochloric and nitric acid |
| Test for calcium | Passes test | Dissolve about 100 mg of the sample by warming with 5 mL of dilute hydrochloric acid TS and 5 mL of water. Add 1 mL of ammonia TS, dropwise, with shaking and then add 5 mL of ammonium oxalate TS. A white precipitate forms |
| Test for phosphate | Passes test | To a warm solution of the sample in a slight excess of nitric acid add ammonium molybdate TS. A yellow precipitate forms |
| Purity | ||
| Loss on ignition | Not more than 8% after ignition at 800 ± 25°C for 0.5 h | Not more than 10% after ignition at 825°C to constant weight |
| Fluoride | Not more than 50 mg/kg (expressed as fluorine) | Not more than 50 mg/kg (Method I or III) |
| Arsenic | Not more than 1 mg/kg | |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Mercury | Not more than 1 mg/kg | – |
| Aluminium |
Not more than 150 mg/kg (only if added to food for infants and young children) Not more than 500 mg/kg (for all uses except food for infants and young children). This applies until 31 March 2015 Not more than 200 mg/kg (for all uses except food for infants and young children). This applies from 1 April 2015 |
– |
Table E.11.
Specifications established for monomagnesium phosphate (E 343(i)) according to Commission Regulation (EU) No 231/2012 and JECFA (2008)
| Commission Regulation No 231/2012 | JECFA (2008) | |
|---|---|---|
| Assay | Not less than 51.0% after ignition calculated as P2O5 at the ignited basis (800 ± 25°C for 30 min) | Not less than 96% and not more than 102% as Mg2P2O7 on the ignited basis |
| Description | White, odourless, crystalline powder | White, odourless, crystalline powder |
| Identification | ||
| Solubility | Slightly soluble in water | Slightly soluble in water |
| Test for magnesium | Passes test | Passes test |
| Test for phosphate | Passes test | Passes test |
| Purity | ||
| Loss on drying | Anhydrous: Not more than 1.5% (105°C, 4 h) | |
| Loss on ignition |
Anhydrous: Not more than 18.5% Dihydrate: Not more than 33% Tetrahydrate: Not more than 43% |
|
| MgO content | Not less than 21.5% after ignition or at an anhydrous basis (105°C, 4 h) | – |
| Fluoride | Not more than 10 mg/kg (as fluorine) |
Not more than 10 mg/kg See description under TESTS |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Mercury | Not more than 1 mg/kg | – |
Table E.12.
Specifications established for dimagnesium phosphate (E 343(ii)) according to Commission Regulation (EU) No 231/2012 and JECFA (2006a)
| Commission Regulation No 231/2012 | JECFA (2006b,c,d,e,f) | |
|---|---|---|
| Assay | Not less than 96% after ignition (800 ± 25°C for 30 min) | Not less than 96.0% on the ignited basis |
| Description | White, odourless, crystalline powder | Odourless white crystalline powder |
| Identification | ||
| Solubility | Slightly soluble in water | Slightly soluble in water, soluble in dilute acids, but insoluble in ethanol |
| Test for magnesium | Passes test | Dissolve 100 mg in 0.5 mL of diluted acetic acid TS and 20 mL of water. Add 1 mL of ferric chloride TS, let stand for 5 min and filter. The filtrate gives a positive test for magnesium |
| Test for phosphate | Passes test | Passes test |
| Purity | ||
| Loss on ignition | Not less than 29% and not more than 36% (800 ± 25°C to constant weight) | |
| MgO content | Not less than 21.5% after ignition or at an anhydrous basis (105°C, 4 h) | – |
| Fluoride | Not more than 10 mg/kg (as fluorine) | Not more than 10 mg/kg (Method III) |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Mercury | Not more than 1 mg/kg | – |
Table E.13.
Specifications for disodium diphosphate (E 450(i)) according to Commission Regulation (EU) No 231/2012 and as INS 450(i) according to JECFA (2012a,b)
| Commission Regulation (EU) No 231/2012 | JECFA (2012a,b) | |
|---|---|---|
| Assay | Content not less than 95% of disodium diphosphate. P2O5 content not less than 63.0% and not more than 64.5% | Not less than 95.0% |
| Description | White powder or grains | White, crystalline powder or granules |
| Identification | ||
| Test for sodium | Passes test | Passes test |
| Test for phosphate | Passes test | Passes test |
| Solubility | Soluble in water | Soluble in water |
| pH | Between 3.7 and 5.0 (1% solution) | 3.7–5.0 (1 in 100 solution) |
| Purity | ||
| Loss on drying | Not more than 0.5% (105°C, 4 h) | Not more than 0.5% (105°, 4 h) |
| Water‐insoluble matter | Not more than 1% | Not more than 1% |
| Fluoride | Not more than 10 mg/kg (expressed as fluorine) | Not more than 10 mg/kg |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
| Aluminium | No more than 200 mg/kg | – |
Table E.14.
Specifications for trisodium diphosphate (E 450(ii)) according to Commission Regulation (EU) No 231/2012 and as INS 450(ii) according to JECFA (2012a,b)
| Commission Regulation (EU) No 231/2012 | JECFA (2012a,b) | |
|---|---|---|
| Assay | Content not less than 95% on the dried basis. P2O5 content not less than 57% and not more than 59% | Not less than 57% and not more than 59% expressed as P2O5 on the dried basis |
| Description | White powder or grains, occurs anhydrous or as a monohydrate | White powder or grains |
| Identification | ||
| Test for sodium | Passes test | Passes test |
| Test for phosphate | Passes test | Passes test |
| Solubility | Soluble in water | Soluble in water |
| pH | Between 6.7 and 7.5 (1% solution) | – |
| Purity | ||
| Loss on ignition | Not more than 4.5% on the anhydrous compound (450–550°C). Not more than 11.5% on the monohydrate basis |
Anhydrous: not more than 4.5 Monohydrate: not more than 11.5% |
| Loss on drying |
Not more than 0.5% (105°C, 4 h) for anhydrous Not more than 1.0% (105°C, 4 h) for monohydrate |
Anhydrous: not more than 0.5% (105°, 4 h) Monohydrate: not more than 1.0% (105°, 4 h) |
| Water‐insoluble matter | Not more than 0.2% | Not more than 0.2% |
| Fluoride | Not more than 10 mg/kg (expressed as fluorine) | Not more than 10 mg/kg |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
Table E.15.
Specifications for tetrasodium diphosphate (E 450(iii)) according to Commission Regulation (EU) No 231/2012 and as INS 450(iii) according to JECFA (2012a,b)
| Commission Regulation (EU) No 231/2012 | JECFA (2012a,b) | |
|---|---|---|
| Assay | Content not less than 95% of Na4P2O7 on the ignited basis. P2O5 content not less than 52.5% and not more than 54.0% | Not less than 95.0% on the ignited basis |
| Description | Colourless or white crystals, or a white crystalline or granular powder. The decahydrate effloresces slightly in dry air | Colourless or white crystals, or a white crystalline or granular powder; the decahydrate effloresces slightly in dry air |
| Identification | ||
| Test for sodium | Passes test | Passes test |
| Test for phosphate | Passes test | Passes test |
| Solubility | Soluble in water. Insoluble in ethanol | Soluble in water. Insoluble in ethanol |
| pH | Between 9.8 and 10.8 (1% solution) | 9.9–10.8 (1 in 100 solution) |
| Purity | ||
| Loss on ignition | Not more than 0.5% for the anhydrous salt, not less than 38% and not more than 42% for the decahydrate (105°C, 4 h then 550°C, 30 min |
Not more than 0.5% for anhydrous, 38–42% for decahydrate (105°, 4 h then 550°, 30 min) |
| Water‐insoluble matter | Not more than 0.2% | Not more than 0.2% |
| Fluoride | Not more than 10 mg/kg (expressed as fluorine) | Not more than 10 mg/kg |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
Table E.16.
Specifications for tetrapotassium diphosphate (E 450(v)) according to Commission Regulation (EU) No 231/2012 and as INS 450(v) according to JECFA (2012a,b)
| Commission Regulation (EU) No 231/2012 | JECFA (2012a,b) | |
|---|---|---|
| Assay | Content not less than 95% (800°C for 0.5 h). P2O5 content not less than 42.0% and not more than 43.7% | Not less than 95% on the ignited basis |
| Description | Colourless crystals or white, very hygroscopic powder | Colourless or white crystals, or a white crystalline or granular powder, powder of granular solid; hygroscopic |
| Identification | ||
| Test for potassium | Passes test | Passes test |
| Test for phosphate | Passes test | Passes test |
| Solubility |
Soluble in water Insoluble in ethanol |
Soluble in water Insoluble in ethanol |
| pH | Between 10.0 and 10.8 (1% solution) | 10.0–10.7 (1 in 100 solution) |
| Purity | ||
| Loss on ignition | Not more than 2% (105°C, 4 h then 550°C, 30 min | Not more than 2% (105°, 4 h; then 550°, 30 min) |
| Water‐insoluble matter | Not more than 0.2% | Not more than 0.2% |
| Fluoride | Not more than 10 mg/kg (expressed as fluorine) | Not more than 10 mg/kg |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
Table E.17.
Specifications for dicalcium diphosphate (E 450(vi)) according to Commission Regulation (EU) No 231/2012 and as INS 450(vi) according to JECFA (2012a,b)
| Commission Regulation (EU) No 231/2012 | JECFA (2012a,b) | |
|---|---|---|
| Assay | Content not less than 96%. P2O5 content not less than 55% and not more than 56% | Not less than 96% |
| Description | A fine, white, odourless powder | Fine, white, odourless powder |
| Identification | ||
| Test for calcium | Passes test | Passes test |
| Test for phosphate | Passes test | Passes test |
| Solubility |
Insoluble in water Soluble in dilute hydrochloric and nitric acids |
Insoluble in water Soluble in dilute hydrochloric and nitric acids |
| pH | Between 5.5 and 7.0 (10% suspension in water) | 5.5–7.0 (1 in 10 slurry) |
| Purity | ||
| Loss on ignition | Not more than 1.5% (800 ± 25 °C, 30 min) | Not more than 1.5% |
| Fluoride | Not more than 50 mg/kg (expressed as fluorine) | Not more than 50 mg/kg |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
Table E.18.
Specifications for calcium dihydrogen diphosphate (E 450(vii)) according to Commission Regulation (EU) No 231/2012 and as INS 450(vii) according to JECFA (2012a,b)
| Commission Regulation (EU) No 231/2012 | JECFA (2012a,b) | |
|---|---|---|
| Assay | Content not less than 90% on the anhydrous basis. P2O5 content not less than 61% and not more than 66% | Not more than 64% expressed as P2O5 on dried basis |
| Description | White crystals or powder | White crystals or powder |
| Identification | ||
| Test for calcium | Passes test | Passes test |
| Test for phosphate | Passes test | Passes test |
| Purity | ||
| Loss on drying | – | Anhydrous: not more than 1% (105°, 4 h) |
| Acid‐insoluble matter | Not more than 0.4% | Not more than 0.4% |
| Fluoride | Not more than 30 mg/kg (expressed as fluorine) | Not more than 30 mg/kg |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
| Aluminium |
Not more than 800 mg/kg This applies until 31 March 2015 Not more than 200 mg/kg This applies from 1 April 2015 |
– |
Table E.19.
Specifications for magnesium dihydrogen diphosphate (E 450(ix)) according to Commission Regulation (EU) No 231/2012 and as INS 450(ix) according to JECFA (2012a,b)
| Commission Regulation (EU) No 231/2012 | JECFA (2012a,b) | |
|---|---|---|
| Assay | P2O5 content not less than 68.0% and not more than 70.5% expressed as P2O5MgO content not less than 18.0% and not more than 20.5% expressed as MgO | |
| Description | White crystals or powder | |
| Identification | ||
| Solubility | Slightly soluble in water, practically insoluble in ethanol | |
| Particle size | The average particle size will deviate between 10 and 50 μm | |
| Test for magnesium | Passes test | |
| Purity | ||
| Loss on ignition | Not more than 12% (800°C, 0.5 h) | Not more than 12% (800°C, 0.5 h) |
| Orthophosphate | Not more than 4% as (PO4)3− | |
| Calcium | Not more than 4% | |
| Fluoride | Not more than 20 mg/kg (expressed as fluorine) | Not more than 20 mg/kg |
| Arsenic | Not more than 1 mg/kg | Not more than 1 mg/kg |
| Cadmium | Not more than 1 mg/kg | Not more than 1 mg/kg |
| Lead | Not more than 1 mg/kg | Not more than 1 mg/kg |
| Aluminium | Not more than 50 mg/kg | Not more than 50 mg/kg |
Table E.20.
Specifications for pentasodium triphosphate (E 451(i)) according to Commission Regulation (EU) No 231/2012 and as INS 451(i) according to JECFA (2012a,b)
| Commission Regulation (EU) No 231/2012 | JECFA (2012a,b) | |
|---|---|---|
| Assay |
Content not less than 85.0% (anhydrous) or 65.0% (hexahydrate) P2O5 content not less than 56% and not more than 59% (anhydrous) or not less than 43% and not more than 45% (hexahydrate) |
Anhydrous: not less than 85.0% of Na5O10P3 and not less than 56.0% and not more than 58.0% of P2O5 Hexahydrate: not less than 65.0% of Na5O10P3 and not less than 43.0% and not more than 45.0% of P2O5 |
| Description | White, slightly hygroscopic granules or powder | White, slightly hygroscopic granules or powder |
| Identification | ||
| Test for sodium | Passes test | Passes test |
| Test for phosphate | Passes test | Passes test |
| Solubility | Freely soluble in water. Insoluble in ethanol | Freely soluble in water. Insoluble in ethanol |
| pH | Between 9.1 and 10.2 (1% solution) | Between 9.1 and 10.1 (1% solution) |
| Purity | ||
| Loss on drying |
Anhydrous: not more than 0.7% (105°C, 1 h) Hexahydrate: not more than 23.5% (60°C, 1 h, then 105°C, 4 h) |
Anhydrous: not more than 0.7% (105°, 1 h) Hexahydrate: not more than 23.5% (60°, 1 h, followed by 105°, 4 h) |
| Water‐insoluble matter | Not more than 0.1% | Not more than 0.1% |
| Higher polyphosphates | Not more than 1% | Not detectable |
| Fluoride | Not more than 10 mg/kg (expressed as fluorine) | Not more than 50 mg/kg |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
Table E.21.
Table 2 Specifications for pentapotassium triphosphate (E 451(ii)) according to Commission Regulation (EU) No 231/2012 and as INS 451(i) according to JECFA (2012a,b)
| Commission Regulation (EU) No 231/2012 | JECFA (2012a,b) | |
|---|---|---|
| Assay | Content not less than 85% on the anhydrous basis | Not less than 85% of K5O10P3 on the dried basis, the remainder being principally other potassium phosphates |
| Description | White, very hygroscopic powder or granules | Hygroscopic white granules or powder |
| Identification | ||
| Test for potassium | Passes test | Passes test |
| Test for phosphate | Passes test | Passes test |
| Solubility | Very soluble in water | Very soluble in water |
| pH | Between 9.2 and 10.5 (1% solution) | Between 9.2 and 10.1 (1% solution) |
| Purity | ||
| Loss on ignition | Not more than 0.4% (105°C, 4 h, then 550°C, 30 min) | Not more than 0.4% after drying (105°, 4 h) followed by ignition at 550° for 30 min) |
| Water‐insoluble matter | Not more than 2% | Not more than 2% |
| P2O5 content | P2O5 content not less than 46.5% and not more than 48% | Not less than 46.5% and not more than 48.0% |
| Fluoride | Not more than 10 mg/kg (expressed as fluorine) | Not more than 10 mg/kg |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
Table E.22.
Specifications for sodium polyphosphate (E 452(i) I. Soluble polyphosphate) according to Commission Regulation (EU) No 231/2012 and as INS 452(i) according to JECFA (2012a,b)
| Commission Regulation (EU) No 231/2012 | JECFA (2012a,b) | |
|---|---|---|
| Assay | P2O5 content not less than 60% and not more than 71% on the ignited basis | Not less than 60.0% and not more than 71.0% of P2O5 |
| Description | Colourless or white, transparent platelets, granules or powders | Colourless or white, transparent platelets, granules or powders |
| Identification | ||
| Test for sodium | Passes test | A 1 in 20 solution passes test |
| Test for phosphate | Passes test | Dissolve 0.1 g of the sample in 5 mL of hot dilute nitric acid TS. Warm on a steam bath for 10 min and cool. Neutralise to litmus with sodium hydroxide TS, and add silver nitrate TS. A yellow precipitate is formed which is soluble in dilute nitric acid TS |
| Solubility | Very soluble in water | Very soluble in water |
| pH | Between 3.0 and 9.0 (1% solution) | – |
| Purity | ||
| Loss on ignition | Not more than 1% | Not more than 1.0% |
| Water‐insoluble matter | Not more than 0.1% | Not more than 0.1% |
| Fluoride | Not more than 10 mg/kg (expressed as fluorine) | Not more than 10 mg/kg |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
Table E.23.
Specifications for sodium polyphosphate (E 452(i) II. insoluble polyphosphate) according to Commission Regulation (EU) No 231/2012 and as INS 452(i) according to JECFA (2012a,b)
| Commission Regulation (EU) No 231/2012 | |
|---|---|
| Assay | P2O5 content not less than 68.7% and not more than 70.0% |
| Description | White crystalline powder |
| Identification | |
| Test for sodium | Passes test |
| Test for phosphate | Passes test |
| Solubility | Insoluble in water, soluble in mineral acids and in solutions of potassium and ammonium (but not sodium) chlorides |
| pH | About 6.5 (1 in 3 suspension in water) |
| Purity | |
| Fluoride | Not more than 10 mg/kg (expressed as fluorine) |
| Arsenic | Not more than 1 mg/kg |
| Cadmium | Not more than 1 mg/kg |
| Lead | Not more than 1 mg/kg |
| Mercury | Not more than 1 mg/kg |
Table E.24.
Specifications for potassium polyphosphate (E 452(ii)) according to Commission Regulation (EU) No 231/2012 and as INS 452(ii) according to JECFA (2012a,b)
| Commission Regulation (EU) No 231/2012 | JECFA (2012a,b) | |
|---|---|---|
| Assay | P2O5 content not less than 53.5% and not more than 61.5% on the ignited basis | Not less than 53.5% and not more than 61.5% of P2O5 on the ignited basis |
| Description | Fine white powder or crystals or colourless glassy platelets | Odourless, colourless or white glassy masses, fragments, crystals or powder |
| Identification | ||
| Test for potassium | Passes test | Mix 0.5 g of the sample with 10 mL of nitric acid and 50 mL of water, boil for about 30 min and cool. The resulting solution is used for the test |
| Test for phosphate | Passes test | Mix 0.5 g of the sample with 10 mL of nitric acid and 50 mL of water, boil for about 30 min and cool. The resulting solution is used for the test |
| Solubility | 1 g dissolves in 100 mL of a 1 in 25 solution of sodium acetate | 1 g dissolves in 100 mL of a 1 in 25 solution of sodium acetate |
| pH | Not more than 7.8 (1% suspension) | – |
| Purity | ||
| Loss on ignition | Not more than 2% (105°C, 4 h then 550°C, 30 min) | Not more than 2% after drying (105°, 4 h) followed by ignition at 550°C for 30 min |
| Cyclic phosphate | Not more than 8% on P2O5 content | Not more than 8.0% |
| Fluoride | Not more than 10 mg/kg (expressed as fluorine) | Not more than 10 mg/kg |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
Table E.25.
Specifications for sodium calcium polyphosphate (E 452(iii)) according to Commission Regulation (EU) No 231/2012 and as INS 452(iii) according to JECFA (2012a,b)
| Commission Regulation (EU) No 231/2012 | JECFA (2012a,b) | |
|---|---|---|
| Assay | P2O5 content not less than 61% and not more than 69% on the ignited basis | Not less than 61% and not more than 69% expressed as P2O5 on dried basis |
| Description | White glassy crystals, spheres | White glassy crystals, spheres |
| Identification | ||
| Test for sodium | – | Passes test |
| Test for calcium | – | Passes test |
| Test for phosphate | – | Passes test |
| pH | Approximately 5–7 (1% m/m slurry) | – |
| CaO content | 7–15% m/m | – |
| Purity | ||
| Fluoride | Not more than 10 mg/kg | Not more than 10 mg/kg |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
Table E.26.
Specifications for calcium polyphosphate (E 452(iv)) according to Commission Regulation (EU) No 231/2012 and as INS 452(iv) according to JECFA (2012a,b)
| Commission Regulation (EU) No 231/2012 | JECFA (2012a,b) | |
|---|---|---|
| Assay | P2O5 content not less than 71% and not more than 73% on the ignited basis | Not less than 50.0 and not more than 71.0% of P2O5 on the ignited basis |
| Description | Odourless, colourless crystals or white powder | Odourless, colourless crystals or powder |
| Identification | ||
| Test for calcium | Passes test | The solution of the test for phosphate gives positive tests for calcium |
| Test for phosphate | Passes test | Mix 0.5 g of the sample with 10 mL of nitric acid and 50 mL of water, boil for about 30 min and cool. The resulting solution is used for the test |
| Solubility | Usually sparingly soluble in water. Soluble in acid medium | Usually incompletely soluble in water; soluble in acid medium |
| CaO content | 27–29.5% | – |
| Purity | ||
| Loss on ignition | Not more than 2% (105°C, 4 h than 550°C, 30 min) | Not more than 2% after drying (105°C, 4 h) followed by ignition (550°C, 30 min) |
| Cyclic phosphate | Not more than 8% (on P2O5 content) | Not more than 8% calculated on P2O5 content |
| Fluoride | Not more than 30 mg/kg (expressed as fluorine) | Not more than 10 mg/kg |
| Arsenic | Not more than 1 mg/kg | Not more than 3 mg/kg |
| Cadmium | Not more than 1 mg/kg | – |
| Lead | Not more than 1 mg/kg | Not more than 4 mg/kg |
| Mercury | Not more than 1 mg/kg | – |
Appendix F – Summary of the reported use levels (mg/kg or mg/L as appropriate) of phosphates (E 338–341, E 343, E 450–452) provided by industry
Appendix G – Summary of analytical results (mg P/kg or mg P/L as appropriate) of phosphorus provided by Member States
Appendix H – Number and percentage of food products labelled with phosphates (E 338‐341, E 343, E 450‐452) out of the total number of food products present in the Mintel GNPD per food subcategory between 2014 and 2019
Appendix I – Concentration levels of phosphates (E 338–341, E 343, E 450–452) used in the regulatory maximum level exposure assessment scenario and in the refined exposure assessment scenarios (mg/kg or mL/kg as appropriate)
Appendix J – Summary of total estimated exposure of phosphates (E 338–341, E 343, E 450–452) from their use as food additives for the regulatory maximum level exposure assessment scenario and the refined exposure assessment scenarios, in seven population groups (min‐max across the dietary surveys in mg P2O5/kg bw per day and in mg P2O5/person per day)
Appendix K – Total estimated exposure of phosphates (E 338–341, E 343, E 450–452) from their use as food additives for the regulatory maximum level exposure assessment scenario and the refined exposure assessment scenarios per population group and survey: mean and 95th percentile (mg P2O5/kg bw per day)
Appendix L – Main food categories contributing to exposure to phosphates (E 338–341, E 343, E 450–452) using the regulatory maximum level exposure assessment scenario and the refined exposure assessment scenarios, based on the results expressed in mg P2O5/kg bw per day (> 5% to the total mean exposure)
Appendix M
M1: Summary of total estimated exposure of phosphates (E 338–341, E 343, E 450–452) from their use as food additives and the proposed extension of uses for the regulatory maximum level exposure assessment scenario and the refined exposure assessment scenarios (min–max across the dietary surveys in mg P2O5/kg bw per day and in mg P2O5/person per day)
M2: Total estimated exposure of phosphates (E 338–341, E 343, E 450–452) from their use as food additives and the proposed extension of use for the regulatory maximum level exposure assessment scenario and the refined exposure assessment scenarios per population group and survey: mean and 95th percentile (mg P2O5/kg bw per day)
Appendix N
N1: Summary of exposure to total phosphorus via the diet (using analytical data) per population group and survey: mean and 95th percentile (mg P/kg bw per day)
N2: Summary of exposure to total phosphorus via the diet (using analytical data) per population group and survey: mean and 95th percentile (mg P/person per day)
Appendix O – Main food categories contributing to exposure to total phosphorus via the diet (using analytical data, based on exposure in mg P/kg bw per day) (> 5% to the total mean exposure)
1.
Appendices F–O can be found in the online version of this output (‘Supporting information’ section): https://efsa.onlinelibrary.wiley.com/doi/10.2903/j.efsa.2019.5674
Appendix P – Case series and case reports after acute administration
1.
| Case series and case reports after acute administration | |||||||
|---|---|---|---|---|---|---|---|
| No. | Author | Age/sex | History |
Dose given in mg of phosphorus Oral Solution |
Outcome | Serum creatinine levels (mg/dL) | Clinical/pathological observation |
| 1 | Aasebø et al. (2007) | 69/F | Breast cancer. Hypertension | 11,600 (2 × 5,800 within 12 h) | Remission |
Baseline: 0.79 Onset: 4.32–5.97 Follow‐up: 1.60 |
Baseline: diagnosis of membranous glomerulonephritis (?) after the increase of creatinine > 5.97, in a second biopsy calcium phosphate deposits |
| 2 | Arikan et al. (2013) | 18/F | Ileus | 11,600 (2 × 5,800 within 12 h) | Haemodialysis remission |
Baseline: 0.41 Onset: 0.87–1.08 Follow‐up: 0.60 |
|
| 3 | Cakar et al. (2012) | 65/M | Hypertension | 11,600 (2 × 5,800 within 12 h) | CKD. Patient started haemodialysis treatment |
Baseline: 1.14 Onset: 1.82 Follow‐up: 3.14 |
Kidney biopsy showed mild focal tubulointerstitial inflammation, tubular atrophy, sclerosis |
| 4 | Fine and Patterson (1997) | 84/F | Hypertension, mild cardiac insufficiency. | 34,800 (6 × 5,800) over 4 days | Death |
Baseline: 0.7 Onset: 2.5 – |
|
| 5 | Gonlusen et al. (2006) | 56/F | Gastroesophageal reflux, mild Crohn's disease | 11,600 (2 × 5,800 within 12 h) | Remission |
Baseline: 0.8 Onset: 3.8 Follow‐up: 1.6 |
Renal biopsy (44 days after colonoscopy) nephrocalcinosis |
| 6 | Markowitz et al. (2004) | 69/M | HTA (losartan), carcinoma, mild hyperparathyroidism. Folic acid | 11,600 (2 × 5,800 within 12 h) | Unknown |
Baseline: 1.2 Onset: 6.7–8.5 Follow‐up: – |
After the colonoscopy, the patient presented with an episode of gross haematuria |
| 7 | Markowitz et al. (2004) | 82/M | Hypertension. Surgical intervention with hemicolectomy | 15,500 (2 × 5,800 = 11,600 within 12 h) + 3,900 | Unknown |
Baseline: 0.9 Onset: 5.2–4.9 Follow‐up: 4.3 |
|
| 8 | Markowitz et al. (2004) | 55/F | Diabetes mellitus, Hypertension, coronary heart disease | 11,600 (2 × 5,800 within 12 h) | Unknown |
Baseline: 0.6 Onset: 4.5 Follow‐up: 3.5 |
|
| 9 | Markowitz et al. (2004) | 64/F | hypertonia arterialis (enalapril, HCT, aspirin) diabetes mellitus (glipizide, rosiglitazone), obesity. Use of KCL. Adenomatous rectal polyp | 11,600 (2 × 5,800 within 12 h) | Unknown |
Baseline: 0.9 Onset: 2.3 Follow‐up: 3.3 |
|
| 10 | Markowitz et al. (2004) | 76/F | Hypertension), | 11,600 (2 × 5,800 within 12 h) | Unknown |
Baseline: 0.9 Onset: 6.0–8.0 Follow‐up: 3.7 |
Patient needed haemodialysis |
| 11 | Orias et al. (1999) | 76/M | Hypertension | 29,000 (5 × 5,800 within 2 days) | Remission, without further haemodialysis |
Baseline: 1.1 Onset: 2.5–3.7 Follow‐up: 1.3 |
Haemodialysis was initiated |
| 12 | Santos et al. (2010) | 84/M | History of stage 3 obstructive CRF | 11,600 (2 × 5,800 10–12 h apart) | Regular haemodialysis |
Baseline: – Onset: 9.2 Follow‐up: – |
Kidney biopsy showed tubules were mildly dilated and nephrocalcinosis |
| 13 | Santos et al. (2010) | 88/M | B‐cell lymphoma IV‐B stage | 11,600 (2 × 5,800 10–12 h apart) | Phosphate nephropathy. No clinical improvement Death |
Baseline: – Onset: 3.45 – |
Renal ultrasound showed kidneys with enhanced echogenicity |
| 14 | Slee et al. (2008) | 62/F | Hypertension | 11,600 (2 × 5,800 within 12 h) | CKD stage 4 |
Baseline: 0.83 Onset: 1.97–4.95 Follow‐up: 1.8 |
Kidney biopsy (on day 10) nephrocalcinosis with diffuse non‐polarising tubular deposits in the tubulointerstitium |
| 15 | Vukasin et al. (1997) | 69/F | Unknown | 23,200 (2 × 5,800 12 h apart) + 5,800 × 2 (5 h apart) | Remission |
Baseline: – Onset: 1.7–2.3 Follow‐up: Normal |
|
CKD: chronic kidney disease.; HTA: Hypertonia arterialis; HCT: hychlorothiazide; KCl: Potassium chloride; CRF: corticotropin‐releasing factor.
Appendix Q – Interventional studies – short‐term exposure
1.
| Interventional studies – short–term exposure | |||||||
|---|---|---|---|---|---|---|---|
| Authors (publication year) | Title | Number of patients | Phosphorus dose (mg/day) | Duration of exposure (days) | Renal function | Bowel complaints | |
| 1 | Brixen et al. (1992) | Effects of a Short Course of Oral Phosphate Treatment on Serum Parathyroid Hormone(I‐84) and Biochemical Markers of Bone Turnover: A Dose‐Response Study |
19 19 20 |
750 1,500 2,250 |
7 7 7 |
No change in serum creatinine mentioned |
2 patients 3 patients 7 patients |
| 2 | Ittner et al. (1986) | Reduced parathyroid hormone response to peroral phosphate in osteoporotic patients | 7 | 1,500 | 1 | No change in serum creatinine | Not mentioned |
| 3 | Portale et al. (1987) | Dietary intake of phosphorus modulates the circadian rhythm in serum concentration of phosphorus. Implications for renal production of 1,25‐dihydroxyvitamin D | 6 |
1,000 2,500 |
9 10 |
No change in serum creatinine | Not mentioned |
| 4 | Silverberg et al. (1986) | The effect of oral phosphate administration on major indices of skeletal metabolism in normal subjects | 13 | 660 | 5 | Not mentioned | Not mentioned |
| 5 | Smith and Nordin (1964) | The effect of a high phosphorus intake on total and ultrafiltrable plasma calcium and phosphate clearance. | 8 | 1,500 | 7–10 | Not mentioned | Not mentioned |
| 6 | Van Den Berg et al. (1980) | Orthophosphate therapy decreases urinary calcium excretion and 1,25(OH)2D concentration in idiopathic hypercalciuria | 11 | 2,000 | 14 | Not mentioned | Not mentioned |
| 7 | Yamaoka et al. (1989) | Effect of single oral phosphate loading on vitamin D metabolites in normal subjects and in X‐linked hypophosphatemic rickets | 7 | 2,000 | 1 | No change in serum creatinine | Not mentioned |
Appendix R – Interventional studies – long‐term exposure
1.
| Interventional studies – long‐term exposure | |||||||
|---|---|---|---|---|---|---|---|
| Authors (publication year) | Title | Number of patients | Phosphorus dose (mg/day) | Duration of exposure (months) | Renal function | Bowel complaints | |
| 1 | Alexandre et al. (1988) | Effects of a one‐year administration of phosphate and intermittent calcitonin on bone‐forming and bone‐resorbing cells in involutional osteoporosis: a histomorphometric study | 15 | 500 | 12 | Not mentioned as reduced | Not mentioned |
| 2 | Bernstein and Newton (1966) | The effect of oral sodium phosphate on the formation of renal calculi and on idiopathic hypercalcuria | 10 |
2,400 (4 patients) 4,800 (5 patients) 7,200 (1 patient) |
6–24 4–24 24 |
Slightly reduced (1 patient) reduced (2 patients) 50% reduction |
Not mentioned |
| 3 | Calvo et al. (1990) | Persistently Elevated Parathyroid Hormone Secretion and Action in Young Women after Four Weeks of Ingesting High Phosphorus, Low Calcium Diets. | 10 | 807 (1,723 (phosphate‐rich diet)– 916 (basal diet)) | 1 | Not mentioned | Not mentioned |
| 4 | Dudley and Blackburn (1970) | Extraskeletal calcification complicating oral neutral phosphate therapy | 9 |
2,250 (1) 3,375 (7) 4,500 (1) |
9–87 | Renal function decreased (2 patients: 3,375 and 4,500) | Not mentioned |
| 5 | Ettinger (1976) | Recurrent Nephrolithiasis: Natural History and Effect of Phosphate Therapy. | 25 | 1,400 | 36 | No changes in renal function, or creatinine mentioned | Stool softness |
| 6 | Goldsmith et al. (1968) | Phosphate supplementation as an adjunct in the therapy of multiple myeloma. | 10 |
Nine patients 1,000 one patient 2,000 |
0.75–9 | No deterioration of renal function | Not mentioned |
| 7 | Goldsmith et al. (1976) | Hormone and bone morphology in osteoporosis effects of phosphorus supplementation on serum parathyroid | 7 | 1,000 | 3–20 | Inulin clearance and PAH clearance not changed | Not mentioned |
| 8 | Hulley et al. (1971) | The effect of supplemental oral phosphate on the bone mineral changes during prolonged bed rest | 5 | 1,327 | 4 | No changes of creatinine clearance | Not mentioned |
| 9 | Kuntz et al. (1986) | Treatment of post‐menopausal osteoporosis with phosphate and intermittent calcitonin | 10 | 535 (1,500 mg/day for 5 days every third week for 6 months) | 6 | No changes in renal function, or creatinine mentioned | Not mentioned |
| 10 | Miller et al. (1991) | Effect of cyclical therapy with phosphorus and etidronate on axial bone mineral density in postmenopausal osteoporotic women | 47 | 65.75 (for 3 days a dose of 2,000 mg, 8 times over 2 years) | 24 | No changes in renal function, or creatinine mentioned | Not mentioned |
| 12 | Popovtzer et al. (1976) | Effects of alternating phosphorus and calcium infusions on osteoporosis | 5 | 150–300 (5–10 mg/kg bw per day: 3 days per week) | 10–12 | No change in creatinine clearance (pre vs. post) | Not mentioned |
| 13 | Bell et al. (1977) | Physiological responses of human adults to foods containing phosphate additives | 8 | 1,100 | 1 | Not mentioned | Not mentioned |
| 14 | Shapiro et al. (1975) | Osteoporosis | 10 | 2,200 | 12–24 | No changes in serum creatinine mentioned | Not mentioned |
| 15 | Ulmann et al. (1984) | Fréquence des récifdives lithiasiques après une curre de diurèse simple ou assiciée à un traitement par un duirétique thiazidique ou le phophore | 13 | 1,500 | 24 (median) | No change in serum creatinine mentioned | Not mentioned |
| 16 | Whybro et al. (1998) | Phosphate supplementation in young men: lack of effect on calcium homeostasis and bone turnover | 12 | 1,000, 1,500 and 2,000 (escalating) | 3 | No change in serum creatinine | Not mentioned |
Appendix S – Phosphorus intake, middle and high intakes (mg/day), reported in human studies referenced in the present opinion
1.
| Author (year) | Middle phosphate intake (mg/day) | Highest expressed phosphate intake (mg/day) | Country | Dietary assessment method |
|---|---|---|---|---|
| Alonso et al. (2010) | 1,084 (ARIC‐study) mean | 2,856 (highest) | USA | FFQ (66 items) |
| 1,103 (MESA‐study) | 3,570 (highest) | USA | FFQ (120 items) | |
| Yamamoto et al. (2013) |
1,167 (men) 1,017 (women) |
5,032 (men) 4,069 (women) maximum intake |
USA | FFQ (120 items) |
| Kwak et al. (2014) |
759 median |
976 75th percentile |
Korea | FFQ (103 items) |
| Mazidi et al. (2017) |
1,222 median |
1,641 highest 75th percentile |
Iran | Single 24‐h recall |
| Chang et al. (2014) |
1,166 median |
2,355 (75th percentile in highest quartile) | USA | Single 24‐h recall |
| Itkonen et al. (2013) | 1,617 |
1,795 ± 469 (SD) males |
Finland | 3 day food record + FFQ |
| Tucker et al. (2006) |
1,198–1,206 (categorised by cola consumption) adjusted for age and energy intake |
1,206 ± 10 mean ± SD adjusted for age and energy intake |
USA | FFQ (126 items) |
FFQ: food frequency questionnaires.
Annex 1 – Newcastle–Ottawa quality assessment scale case control studies
1.
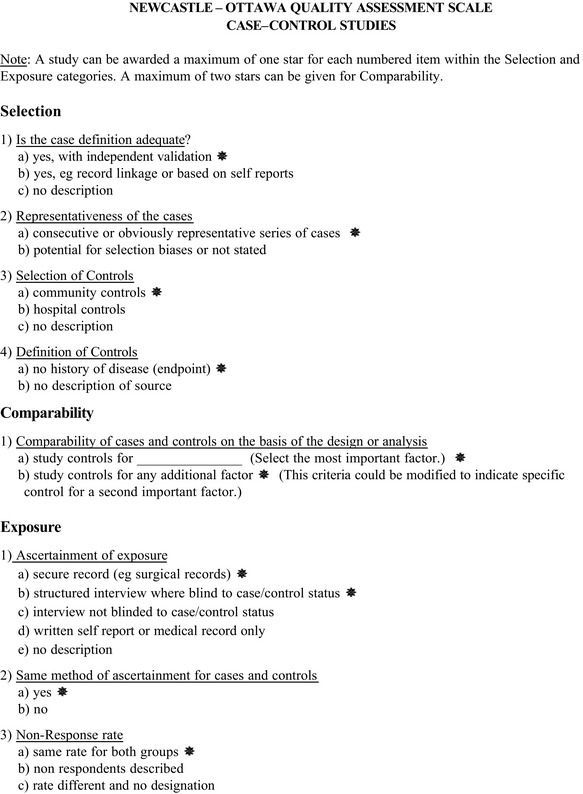
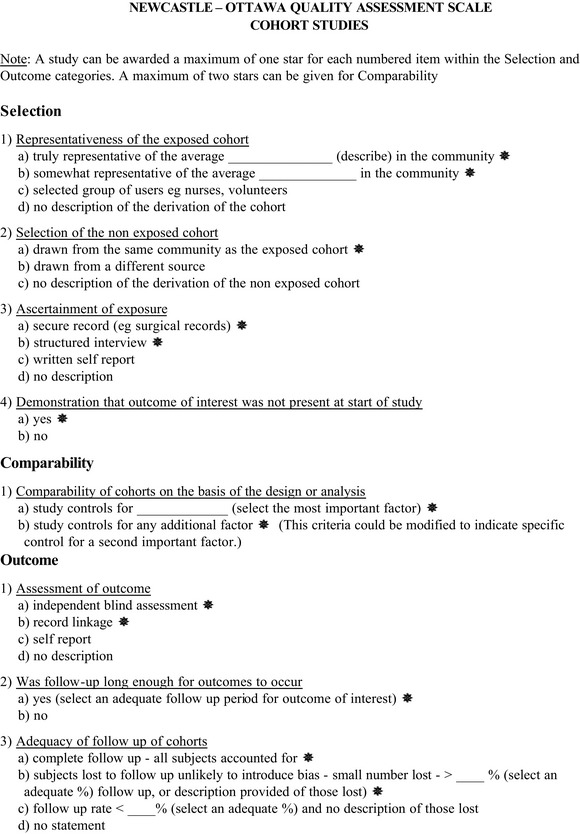
Annex 2 – Coding manual for case control and cohort studies
1.
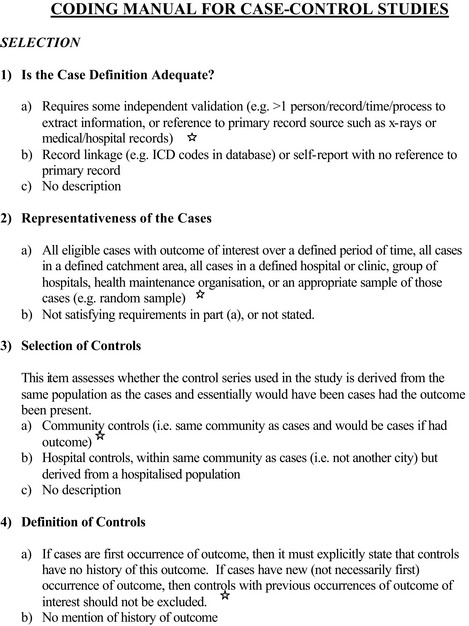
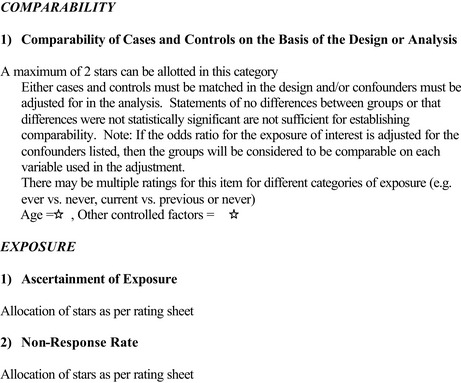
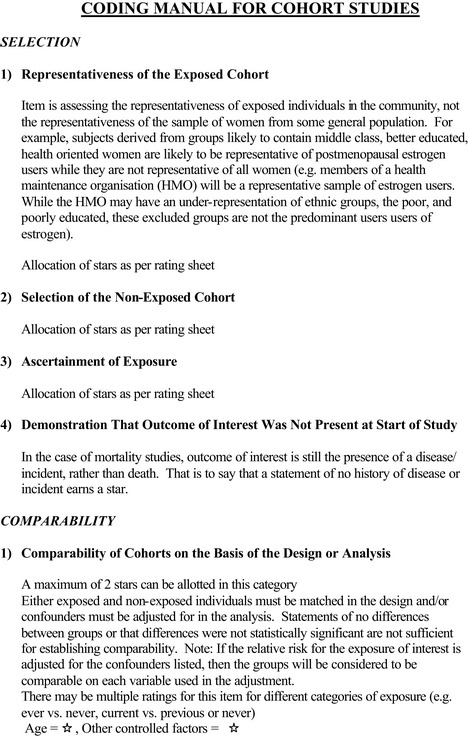
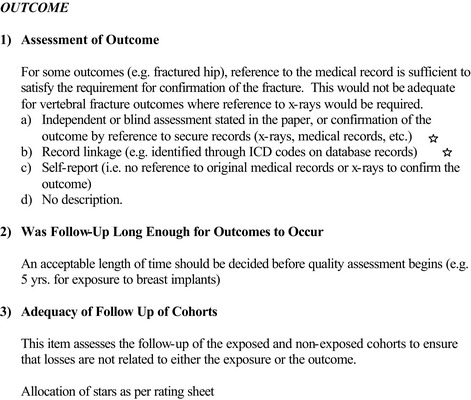
Annex 3 – STROBE Statement—Checklist of items that should be included in reports of cross‐sectional studies
1.
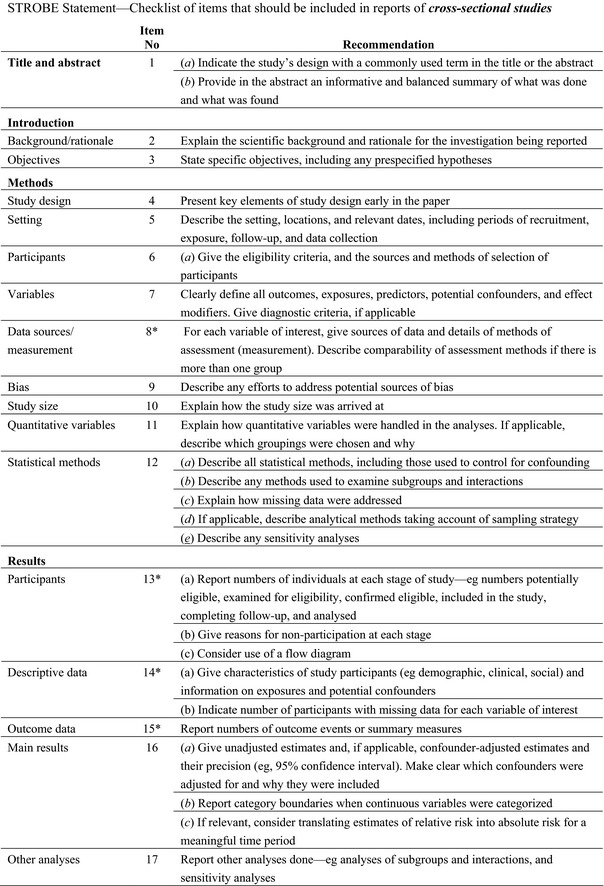
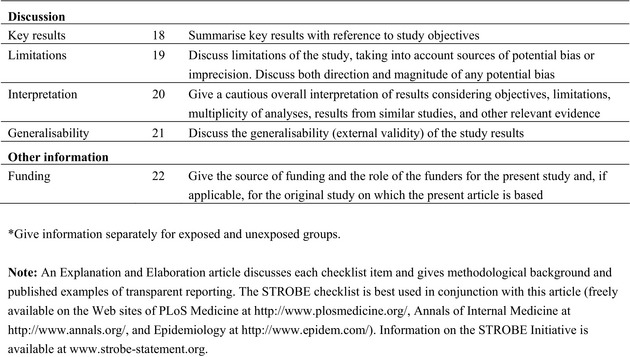
Supporting information
Summary of the reported use levels (mg/kg or mg/L as appropriate) of phosphates (E 338–341, E 343, E 450–452) provided by industry
Summary of analytical results (mg P/kg or mg P/L as appropriate) of phosphorus provided by Member States
Number and percentage of food products labelled with phosphates (E 338‐341, E 343, E 450‐452) out of the total number of food products present in the Mintel GNPD per food subcategory between 2014 and 2019
Concentration levels of phosphates (E 338–341, E 343, E 450–452) used in the regulatory maximum level exposure assessment scenario and in the refined exposure assessment scenarios (mg/kg or mL/kg as appropriate)
Summary of total estimated exposure of phosphates (E 338–341, E 343, E 450–452) from their use as food additives for the regulatory maximum level exposure assessment scenario and the refined exposure assessment scenarios, in seven population groups (min‐max across the dietary surveys in mg P2O5/kg bw per day and in mg P2O5/person per day)
Total estimated exposure of phosphates (E 338–341, E 343, E 450–452) from their use as food additives for the regulatory maximum level exposure assessment scenario and the refined exposure assessment scenarios per population group and survey: mean and 95th percentile (mg P2O5/kg bw per day)
Main food categories contributing to exposure to phosphates (E 338–341, E 343, E 450–452) using the regulatory maximum level exposure assessment scenario and the refined exposure assessment scenarios, based on the results expressed in mg P2O5/kg bw per day (> 5% to the total mean exposure)
M1: Summary of total estimated exposure of phosphates (E 338–341, E 343, E 450–452) from their use as food additives and the proposed extension of uses for the regulatory maximum level exposure assessment scenario and the refined exposure assessment scenarios (min–max across the dietary surveys in mg P2O5/kg bw per day and in mg P2O5/person per day)
M2: Total estimated exposure of phosphates (E 338–341, E 343, E 450–452) from their use as food additives and the proposed extension of use for the regulatory maximum level exposure assessment scenario and the refined exposure assessment scenarios per population group and survey: mean and 95th percentile (mg P2O5/kg bw per day)
N1: Summary of exposure to total phosphorus via the diet (using analytical data) per population group and survey: mean and 95th percentile (mg P/kg bw per day)
N2: Summary of exposure to total phosphorus via the diet (using analytical data) per population group and survey: mean and 95th percentile (mg P/person per day)
Main food categories contributing to exposure to total phosphorus via the diet (using analytical data, based on exposure in mg P/kg bw per day) (> 5% to the total mean exposure)
Suggested citation: EFSA FAF Panel (EFSA Panel on Food Additives and Flavourings) , Younes M, Aquilina G, Castle L, Engel K‐H, Fowler P, Frutos Fernandez MJ, Fürst P, Gürtler R, Husøy T, Mennes W, Moldeus P, Oskarsson A, Shah R, Waalkens‐Berendsen I, Wölfle D, Aggett P, Cupisti A, Fortes C, Kuhnle G, Lillegaard IT, Scotter M, Giarola A, Rincon A, Tard A and Gundert‐Remy U, 2019. Scientific Opinion on the re‐evaluation of phosphoric acid–phosphates – di‐, tri‐ and polyphosphates (E 338–341, E 343, E 450–452) as food additives and the safety of proposed extension of use. EFSA Journal 2019;17(6):5674, 156 pp. 10.2903/j.efsa.2019.5674
Requestor: European Commission
Question numbers: EFSA‐Q‐2011‐00532; EFSA‐Q‐2011‐00533; EFSA‐Q‐2011‐00534; EFSA‐Q‐2011‐00535; EFSA‐Q‐2011‐00536; EFSA‐Q‐2011‐00537; EFSA‐Q‐2011‐00538; EFSA‐Q‐2011‐00539; EFSA‐Q‐2011‐00540; EFSA‐Q‐2011‐00541; EFSA‐Q‐2011‐00542; EFSA‐Q‐2011‐00543; EFSA‐Q‐2011‐00618; EFSA‐Q‐2011‐00619; EFSA‐Q‐2011‐00620; EFSA‐Q‐2011‐00621; EFSA‐Q‐2011‐00622; EFSA‐Q‐2011‐00623; EFSA‐Q‐2011‐00624; EFSA‐Q‐2011‐00625; EFSA‐Q‐2011‐00626; EFSA‐Q‐2011‐00628; EFSA‐Q‐2011‐00629; EFSA‐Q‐2011‐00630; EFSA‐Q‐2018‐00597.
Panel members: Gabriele Aquilina, Laurence Castle, Karl‐Heinz Engel, Paul Fowler, Maria Jose Frutos Fernandez, Peter Fürst, Rainer Gürtler, Ursula Gundert‐Remy, Trine Husøy, Wim Mennes, Peter Moldeus, Agneta Oskarsson, Romina Shah, Ine Waalkens‐Berendsen, Detlef Wölfle and Maged Younes.
Acknowledgements: The Panel wishes to thank Dominique Turck, Agnès de Sesmaisons‐Lecarré and Valeriu Curtui for the support provided to this scientific output. The ANS Panel wishes to acknowledge all European competent institutions, Member State bodies and other organisations that provided data for this scientific output.
Adopted: 4 June 2019*
Reproduction of the images listed below is prohibited and permission must be sought directly from the copyright holder: Figure 1: © Elsevier Science Ltd.
* This opinion was first adopted by the FAF Panel on 27 March 2019, as reflected in the minutes of the FAF Panel Plenary Meeting of 27–29 March 2019: http://www.efsa.europa.eu/sites/default/files/event/190326-m.pdf. However, the adopted version was withdrawn prior to publication and the current version was adopted by the FAF Panel on 4 June 2019.
This publication is linked to the following EFSA Supporting Publications article: http://onlinelibrary.wiley.com/doi/10.2903/sp.efsa.2019.EN-1624/full
Notes
Regulation (EC) No 1333/2008 of the European Parliament and of the Council of 16 December 2008 on food additives. OJ L 354, 31.12.2008, p. 16–33.
Commission Regulation (EU) No 257/2010 of 25 March 2010 setting up a programme for the re‐evaluation of approved food additives in accordance with Regulation (EC) No 1333/2008 of the European Parliament and of the Council on food additives. OJ L 80, 26.3.2010, p. 19–27.
COM(2001) 542 final.
Food Additives in Europe 2000, Status of safety assessments of food additives presently permitted in the EU, Nordic Council of Ministers, TemaNord 2002, 560.
Regulation (EC) No 1333/2008 of the European Parliament and of the Council of 16 December 2008 on food additives. OJ L 354, 31.12.2008.
Directive 2002/46/EC of the European Parliament and of the Council of 10 June 2002 on the approximation of the laws of the Member States relating to food supplements. OJ L 183, 12.7.2002, p. 51–57.
Regulation (EC) No 1925/2006 of the European Parliament and of the Council of 20 December 2006 on the addition of vitamins and minerals and of certain other substances to foods. OJ L 404, 30.12.2006, p. 26–38.
Regulation (EU) No 609/2013 of the European Parliament and of the Council of 12 June 2013 on food intended for infants and young children, food for special medical purposes, and total diet replacement for weight control and repealing Council Directive 92/52/EEC, Commission Directives 96/8/EC, 1999/21/EC, 2006/125/EC and 2006/141/EC, Directive 2009/39/EC of the European Parliament and of the Council and Commission Regulations (EC) No 41/2009 and (EC) No 953/2009. OJ L 181, 29.6.2013, p. 35–56.
Call for technical and toxicological data on phosphates authorised as food additives in the EU. Published: 14 July 2017. Available online: https://www.efsa.europa.eu/en/data/call/170615
Questions for health professionals in the fields of nephrology, mineral metabolism, cardiovascular and nutrition medicine on phosphates food additives re‐evaluation. Published: 1 June 2018. Available online: https://www.efsa.europa.eu/en/consultations/call/180601
Available online: http://www.efsa.europa.eu/en/food-consumption/comprehensive-database
Commission Regulation (EC) No 1333/2008 of the European Parliament and of the Council of 16 December 2008 on food additives. OJ L 354, 31.12.2008, p. 16.
Regulation (EC) No 1333/2008 of the European Parliament and of the Council of 16 December 2008 on food additives. OJ L 354, 31.12.2008, p. 16.
Missing Bulgaria, Cyprus, Estonia, Latvia, Lithuania, Luxembourg, Malta and Slovenia.
http://www.gnpd.com/sinatra/home/ accessed on 18/3/2019.
Available online: http://www.efsa.europa.eu/en/datexfoodcdb/datexfooddb.htm
Due regard has been given to the convention in epidemiological studies for expression of the results as (serum/urine) phosphorus rather than phosphate. In this section we regard serum phosphorus to mean phosphate.
Due regard has been given to the convention in epidemiological studies for expression of the results as (serum/urine) phosphorus rather than phosphate. In this section, we regard serum phosphorus to mean phosphate.
Commission Regulation (EU) No 231/2012 of 9 March 2012 laying down specifications for food additives listed in Annexes II and III to Regulation (EC) No 1333/2008 of the European Parliament and of the Council. OJ L 83, 22.3.2012, p. 1–295.
There is a lack of clarity in relation to the EINECS number. Entering 233‐782‐9 into the ESIS database or the ECHA public database returns the substance sodium metaphosphate with a CAS registry number 10361‐03‐2; this name and number are included under sodium polyphosphate I: soluble polyphosphate in Commission Regulation (EU) No 231/2012 and the number is included in the JECFA specification for INS No. 452(i). The same name and/or CAS registry number are associated with EINECS number 233‐782‐9 on some chemical supplier web‐sites, for example Guidechem (http://www.guidechem.com/products/10361-03-2.html), Carlo Erba (http://www.carloerbareagenti.com/Repository/DIR199/CH1213_GB.pdf).
References
- Aasebø W, Scott H and Ganss R, 2007. Kidney biopsies taken before and after oral sodium phosphate bowel cleansing. Nephrology, Dialysis, Transplantation, 22, 920–922. [DOI] [PubMed] [Google Scholar]
- Alexandre C, Chappard D, Caulin F, Bertrand A, Palle S and Riffat G, 1988. Effects of a one‐year administration of phosphate and intermittent calcitonin on bone‐forming and bone‐resorbing cells in involutional osteoporosis: a histomorphometric study. Calcified Tissue International, 42, 345–350. [DOI] [PubMed] [Google Scholar]
- Allen K and Cornforth D, 2009. Effect of chelating agents and spice‐derived antioxidants on myoglobin oxidation in a lipid‐free model system. Journal of Food Science, 74, C375–C379. [DOI] [PubMed] [Google Scholar]
- Alon US, 1994. Treatment of IgA nephropathy in children. Pediatric Nephrology, 8, 394–395. [DOI] [PubMed] [Google Scholar]
- Alonso A, Nettleton JA, Ix JH, de Boer IH, Folsom AR, Bidulescu A, Kestenbaum BR, Chambless LE and Jacobs DR Jr, 2010. Dietary phosphorus, blood pressure, and incidence of hypertension in the atherosclerosis risk in communities study and the multi‐ethnic study of atherosclerosis. Hypertension, 55, 776–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amato D, Maravilla A, Montoya C, Gaja O, Revilla C, Guerra R and Paniagua R, 1998. Acute effects of soft drink intake on calcium and phosphate metabolism in immature and adult rats. Revista de Investigacion Clinica, 50, 185–189. [PubMed] [Google Scholar]
- Anderson J, 2005. Phosphorus In: Caballero B, Allen L. and Prentice A. (eds.). Encyclopedia of Human Nutrition. Elsevier, Oxford, UK: pp. 486–490. [Google Scholar]
- Anderson MP, Hunt RD, Griffiths HJ, Mcintyre KW and Zimmerman RE, 1977. Long‐term effect of low dietary calcium‐phosphate ratio on skeleton of Cebus albifrons monkeys. Journal of Nutrition, 107, 834–839. [DOI] [PubMed] [Google Scholar]
- Antoniucci DM, Yamashita T and Portale AA, 2006. Dietary phosphorus regulates serum fibroblast growth factor‐23 concentrations in healthy men. Journal of Clinical Endocrinology and Metabolism, 91, 3144–3149. [DOI] [PubMed] [Google Scholar]
- AOAC (Association of Official Analytical Chemists), 1997. Phosphorus in Water: Photometric Method. Method 973.55, Gaithersburg, MD, USA. [Google Scholar]
- Arikan H, Guler D, Birdal G, Nalcaci S, Aykut E, Ozcan C, Irmak R, Banzragch M and Arzu V, 2013. Massive hyperphosphatemia in a patient with neuronal intestinal dysplasia after bowel preparation with oral sodium phosphate. Renal Failure, 35, 875–878. 10.3109/0886022x.2013.794704 [DOI] [PubMed] [Google Scholar]
- Arnlöv J, Carlsson AC, Sundstrom J, Ingelsson E, Larsson A, Lind L and Larsson TE, 2013. Serum FGF23 and risk of cardiovascular events in relation to mineral metabolism and cardiovascular pathology. Clinical Journal of the American Society of Nephrology, 8, 781–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkinson SA, Chappell JE and Clandinin MT, 1995. Calcium supplementation of mother's milk for low birth weight infants: problems related to absorption and excretion. Nutrition Research, 7, 813–823. [Google Scholar]
- Australian Government National Health and Medical Research Council , 2006. Nutrient Reference Values for Australia and New Zealand Including Recommended Dietary Intakes. Available online: https://www.nhmrc.gov.au/guidelines-publications/n35-n36-n37
- Bell RR, Draper HH, Tzeng DY, Shin HK and Schmidt GR, 1977. Physiological responses of human adults to foods containing phosphate additives. Journal of Nutrition, 107, 42–50. [DOI] [PubMed] [Google Scholar]
- Benini O, D'Alessandro C, Gianfaldoni D and Cupisti A, 2011. Extra‐phosphate load from food additives in commonly eaten foods: a real and insidious danger for renal patients. Journal of Renal Nutrition, 21, 303–308. 10.1053/j.jrn.2010.06.021 [DOI] [PubMed] [Google Scholar]
- Berndt T and Kumar R, 2009. Novel mechanisms in the regulation of phosphorus homeostasis. Physiology, 24, 17–25. 10.1152/physiol.00034.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DS and Newton R, 1966. The effect of oral sodium phosphate on the formation of renal calculi and on idiopathic hypercalcuria. Lancet, 2, 1105–1107. [DOI] [PubMed] [Google Scholar]
- Bhat VS, Meek MEB, Valcke M, English C, Boobis A and Brown R, 2017. Evolution of chemical‐specific adjustment factors (CSAF) based on recent international experience; increasing utility and facilitating regulatory acceptance. Critical Reviews in Toxicology, 47, 729–749. 10.1080/10408444.2017.1303818 [DOI] [PubMed] [Google Scholar]
- Biber J, Hernando N and Forster I, 2013. Phosphate transporters and their function. Annual Review of Physiology, 75, 535–550. 10.1146/annurev-physiol-030212-183748 [DOI] [PubMed] [Google Scholar]
- Bistarakis I, 1986. Renal handling of phosphate in the first six months of life. Archives of Disease in Childhood, 61, 677–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Boer IH, Rue TC and Kestenbaum B, 2009. Serum phosphorus concentrations in the third National Health and Nutrition Examination Survey (NHANES III). American Journal of Kidney Diseases, 53, 399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonting SL and Jansen BCP, 1956. The effect of a prolonged intake of phosphoric acid and citric acid in rats. Voeding, 17, 137–148. [Google Scholar]
- Brandenburg VM, Kleber ME, Vervloet MG, Tomaschitz A, Pilz S, Stojakovic T, Delgado G, Grammer TB, Marx N, März W and Scharnagl H, 2014. Fibroblast growth factor 23 (FGF23) and mortality: the Ludwigshafen Risk and Cardiovascular Health Study. Atherosclerosis, 237, 53–59. [DOI] [PubMed] [Google Scholar]
- Brixen K, Nielsen HK, Charles P and Mosekilde L, 1992. Effects of a short course of oral phosphate treatment on serum parathyroid hormone (1‐84) and biochemical markers of bone turnover: a dose‐response study. Calcified Tissue International, 51, 276–281. [DOI] [PubMed] [Google Scholar]
- BVL , 2018. German Federal Office for Consumer Protection and Safety. Response to EFSA call for data. Available online: http://www.bvl.bund.de/EN/homepage_node.html. Accessed 15/02/2018
- Cakar M, Kanbay M, Sarlak H, Akhan M, Gok M, Unal HU, Demirbas S and Yilmaz MI, 2012. Findings of biopsy‐proven chronicity and end‐stage renal failure associated with oral sodium phosphate solution. Renal Failure, 34, 499–501. 10.3109/0886022X.2011.654145 [DOI] [PubMed] [Google Scholar]
- Calvo MS and Heat H III, 1988. Acute effects of oral phosphate‐salt ingestion on serum phosphorus, serum ionized calcium and parathyroid hormone in young adults. American Journal of Clinical Nutrition, 47, 1025–1029. [DOI] [PubMed] [Google Scholar]
- Calvo MS and Lamberg‐Allardt CJ, 2017. Vitamin D research and public health nutrition: a current perspective. Public Health Nutrition, 20, 1713–1717. 10.1017/S1368980017001835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvo MS and Uribarri J, 2013. Public health impact of dietary phosphorus excess on bone and cardiovascular health in the general population. American Journal of Clinical Nutrition, 98, 6–15. [DOI] [PubMed] [Google Scholar]
- Calvo MS, Kumar R and Heat H III, 1988. Elevated secretion and action of serum parathyroid hormone in young adults consuming high phosphorus, low calcium diets assembled from common foods. Journal of Clinical Endocrinology and Metabolism, 66, 823–829. [DOI] [PubMed] [Google Scholar]
- Calvo MS, Kumar R and Heat H III, 1990. Persistently elevated parathyroid hormone secretion and action in young women after four weeks of ingesting high phosphorus, low calcium diets. Journal of Clinical Endocrinology and Metabolism, 70, 1334–1340. [DOI] [PubMed] [Google Scholar]
- Campden , 2012. Review of polyphosphates as additives and testing methods for them in scallops and prawns. Report No. SR654. Campden BRI, ISBN No. 978‐1‐906634‐60‐5.
- Campos‐Obando N, Koek WNH, Hooker ER, van der Eerden BC, Pols HA, Hofman A, van Leeuwen JP, Uitterlinden AG, Nielson CM and Zillikens MC, 2017. Serum phosphate is associated with fracture risk: The Rotterdam Study and MrOS. Journal of Bone and Mineral Research, 32, 1182–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang AR and Anderson C, 2017. Dietary phosphorus intake and the kidney. Annual Review of Nutrition, 37, 321–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang AR, Lazo M, Appel LJ, Gutierrez OM and Grams ME, 2014. High dietary phosphorus intake is associated with all‐cause mortality: results from NHANES III. American Journal of Clinical Nutrition, 99, 320–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheryan M, 1980. Phytic acid interactions in food systems. Critical Reviews in Food Science and Nutrition, 13, 297–335. [DOI] [PubMed] [Google Scholar]
- Chow FH, Taton GF, Boulay JP, Lewis LD, Remmenga EE and Hamar DW, 1980. Effect of dietary calcium, magnesium, and phosphorus on phosphate urolithiasis in rats. Investigative Urology, 17, 273–276. Available online: http://www.ncbi.nlm.nih.gov/pubmed/7351360 [PubMed] [Google Scholar]
- Cipollaro M, Corsale G, Esposito A, Ragucci E, Staiano N, Giordano GG and Pagano G, 1986. Sublethal pH decrease may cause genetic damage to eukaryotic cell: a study on sea urchins and Salmonella typhimurium . Teratogenesis, Carcinogenesis, and Mutagenesis, 6, 275–287. Available online: http://www.ncbi.nlm.nih.gov/pubmed/2875539 [DOI] [PubMed] [Google Scholar]
- Cotton FA and Wilkinson G, 1972. Advanced Inorganic Chemistry. 3rd edition Interscience Publishers, London: pp. 394–402. [Google Scholar]
- Craig JM, 1957. Histological and histochemical changes in the kidneys of rats fed a diet with an excess of inorganic phosphate. American Journal of Pathology, 33, 621. [Google Scholar]
- CRC , 2012a. CRC Handbook of Chemistry and Physics, CASrn 7664‐38‐2. CRC Press LLC, Boca Raton, FL. [Google Scholar]
- CRC , 2012b. CRC Handbook of Chemistry and Physics, CASrn 7757‐86‐0. CRC Press LLC, Boca Raton, FL. [Google Scholar]
- CRC , 2012c. CRC Handbook of Chemistry and Physics, CASrn 7758‐87‐4. CRC Press LLC, Boca Raton, FL. [Google Scholar]
- CRC , 2012d. CRC Handbook of Chemistry and Physics, CASrn 10031‐30‐8. CRC Press LLC, Boca Raton, FL. [Google Scholar]
- CRC , 2012e. CRC Handbook of Chemistry and Physics, CASrn 7778‐77‐0. CRC Press LLC, Boca Raton, FL. [Google Scholar]
- Criqui MH, Kamineni A, Allison MA, Ix JH, Carr JJ, Cushman M, Detrano R, Post W and Wong ND, 2010. Risk factor differences for aortic versus coronary calcified atherosclerosis: the multiethnic study of atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology, 30, 2289–2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cupisti A and Gallieni M, 2018. Urinary phosphorus excretion: not what we have believed it to be? Clinical Journal of the American Society of Nephrology, 13, 973–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cupisti A, Benini O, Ferretti V, Gianfaldoni D and Kalantar‐Zadeh K, 2012. Novel differential measurement of natural and added phosphorus in cooked ham with or without preservatives. Journal of Renal Nutrition, 22, 533–540. Available online: http://www.ncbi.nlm.nih.gov/pubmed/22406120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das P, Bhattacharya S, Mishra S and Das A, 2011. Zn(II) and Cd(II)‐based complexes for probing the enzymatic hydrolysis of Na4P2O7 by alkaline phosphatase in physiological conditions. Chemical Communications, 47, 8118–8120. [DOI] [PubMed] [Google Scholar]
- Datta PK, Frazer AC, Sharratt M and Sammons HG, 1962. Biological effects of food additives. II. Sodium pyrophosphate. Journal of the Science of Food and Agriculture, 13, 556–566. [Google Scholar]
- De Borba B and Rohrer J, 2018. Application note 169. Rapid determination of phosphate and citrate in carbonated soft drinks using a reagent‐free ion chromatography system. Thermo Fisher Scientific. Available online: https://tools.thermofisher.com/content/sfs/brochures/AN-169-IC-Phosphate-Citrate-Soft-Drinks-AN71409-EN.pdf. Accessed 09 April 2018.
- Delgado‐Andrade C, Seiquer I, García MM, Galdó G and Navarro MP, 2011. Increased Maillard reaction products intake reduces phosphorus digestibility in male adolescents. Nutrition, 27, 86–91. 10.1016/j.nut.2009.10.009 [DOI] [PubMed] [Google Scholar]
- Demerec M, Bertani G and Flint J, 1951. A survey of chemicals for mutagenic action on E. coli . American Naturalist, 85, 119–136. [Google Scholar]
- Dhingra R, Sullivan LM, Fox CS, Wang TJ, D'Agostino RB Sr, Gaziano JM and Vasan RS, 2007. Relations of serum phosphorus and calcium levels to the incidence of cardiovascular disease in the community. Archives of Internal Medicine, 167, 879–885. [DOI] [PubMed] [Google Scholar]
- Dhingra R, Gona P, Benjamin EJ, Wang TJ, Aragam J, D'Agostino RB Sr, Kannel WB and Vasan RS, 2010. Relations of serum phosphorus levels to echocardiographic left ventricular mass and incidence of heart failure in the community. European Journal of Heart Failure, 12, 812–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dionex , 2010. Application Update 172: Determination of Polyphosphates Using Ion Chromatography. Dionex Corporation, Sunnyvale, CA, USA. [Google Scholar]
- Dudley FJ and Blackburn CRB, 1970. Extraskeletal calcification complicating oral neutral‐phosphate therapy. Lancet, 2, 628–630. [DOI] [PubMed] [Google Scholar]
- Dymsza HA, Reussner G Jr and Thiessen R Jr, 1959. Effect of normal and high intakes of orthophosphate and metaphosphate in rats. Journal of Nutrition, 69, 419–428. Available online: http://www.ncbi.nlm.nih.gov/pubmed/13819016 [DOI] [PubMed] [Google Scholar]
- EFSA (European Food Safety Authority), 2007. Scientific opinion of the Scientific Committee related to uncertainties in dietary exposure assessment. EFSA Journal 2007;5(1):438, 54 pp. 10.2903/j.efsa.2007.438 [DOI] [Google Scholar]
- EFSA (European Food Safety Authority), 2010. Management of left‐censored data in dietary exposure assessment of chemical substances. EFSA Journal 2010;8(3):1557, 96 pp. 10.2903/j.efsa.2010.1557 [DOI] [Google Scholar]
- EFSA (European Food Safety Authority), 2011a. Use of the EFSA Comprehensive European Food Consumption Database in exposure assessment. EFSA Journal 2011;9(3):2097, 34 pp. 10.2903/j.efsa.2011.2097 [DOI] [Google Scholar]
- EFSA (European Food Safety Authority), 2011b. Evaluation of the FoodEx, the food classification system applied to the development of the EFSA Comprehensive European Food Consumption Database. EFSA Journal 2011;9(3):1970, 27 pp. 10.2903/j.efsa.2011.1970 [DOI] [Google Scholar]
- EFSA (European Food Safety Authority), 2014. Guidance on the EU Menu methodology. EFSA Journal 2014;12(12):3944, 77 pp. 10.2903/j.efsa.2014.3944 [DOI] [Google Scholar]
- EFSA ANS Panel (EFSA Panel on Food Additives and Nutrient Sources Added to Food), 2012. Guidance for submission for food additive evaluations. EFSA Journal 2012;10(7):2760, 60 pp. 10.2903/j.efsa.2012.2760 [DOI] [Google Scholar]
- EFSA CONTAM Panel (EFSA Panel on Contaminants in the Food Chain), 2009a. Scientific opinion on cadmium in food. EFSA Journal 2009;7(10):980, 139 pp. 10.2903/j.efsa.2009.98 [DOI] [Google Scholar]
- EFSA CONTAM Panel (EFSA Panel on Contaminants in the Food Chain), 2009b. Scientific Opinion on arsenic in food. EFSA Journal 2009;7(10):1351, 199 pp. 10.2903/j.efsa.2009.1351 [DOI] [Google Scholar]
- EFSA CONTAM Panel (EFSA Panel on Contaminants in the Food Chain), 2010. Scientific Opinion on lead in food. EFSA Journal 2010;8(4):1570, 151 pp. 10.2903/j.efsa.2010.1570 [DOI] [Google Scholar]
- EFSA CONTAM Panel (EFSA Panel on Contaminants in the Food Chain), 2012a. Scientific Opinion on the risk for public health related to the presence of mercury and methylmercury in food. EFSA Journal 2012;10(12):2985, 241 pp. 10.2903/j.efsa.2012.2985 [DOI] [Google Scholar]
- EFSA CONTAM Panel (EFSA Panel on Contaminants in the Food Chain), 2012b. Scientific Opinion on lead dietary exposure in the European population. EFSA Journal 2012;10(7):2831, 59 pp. 10.2903/j.efsa.2012.2831 [DOI] [Google Scholar]
- EFSA CONTAM Panel (EFSA Panel on Contaminants in the Food Chain), 2012c. Scientific Opinion on cadmium dietary exposure in the European population. EFSA Journal 2012;10(1):2551, 59 pp. 10.2903/j.efsa.2012.2831 [DOI] [Google Scholar]
- EFSA CONTAM Panel (EFSA Panel on Contaminants in the Food Chain), 2014. Scientific Opinion on dietary exposure to inorganic arsenic in the European population. EFSA Journal 2014;12(3):3597, 68 pp. 10.2903/j.efsa.2014.3597 [DOI] [Google Scholar]
- EFSA FEEDAP Panel (EFSA Panel on Additives and Products or Substances used in Animal Feed), 2013. Scientific Opinion on the safety and efficacy of orthophosphoric acid for all animal species. EFSA Journal 2013;11(1):3043, 11 pp. 10.2903/j.efsa.2013.3043 [DOI] [Google Scholar]
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies), 2005. Opinion of the Scientific Panel on Dietetic products, nutrition and allergies [NDA] related to the tolerable upper intake level of phosphorus. EFSA Journal 2005;3(8):233, 19 pp. 10.2903/j.efsa.2005.233 [DOI] [Google Scholar]
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies), 2006. Tolerable upper intake levels for vitamins and minerals. Available online: https://www.efsa.europa.eu/sites/default/files/efsa_rep/blobserver_assets/ndatolerableuil.pdf
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies), 2013. Scientific Opinion on nutrient requirements and dietary intakes of infants and young children in the European Union. EFSA Journal 2013;11(10):3408, 103 pp. 10.2903/j.efsa.2013.3408 [DOI] [Google Scholar]
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies), 2014. Scientific Opinion on the essential composition of infant and follow‐on formulae. EFSA Journal 2014;12(7):3760, 106 pp. 10.2903/j.efsa.2014.3760 [DOI] [Google Scholar]
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies), 2015. Scientific Opinion on Dietary Reference Values for phosphorus. EFSA Journal 2015;13(7):4185, 54 pp. 10.2903/j.efsa.2015.4185 [DOI] [Google Scholar]
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies), 2018. Scientific opinion on the update of the tolerable upper intake level for vitamin D for infants. EFSA Journal 2018;16(8):5365, 118 pp. 10.2903/j.efsa.2018.5365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- EFSA Scientific Committee , 2009. Guidance of the Scientific Committee on transparency in the scientific aspects of risk assessments carried out by EFSA. Part 2: general principles. EFSA Journal 2009;7(7):1051, 22 pp. 10.2903/j.efsa.2009.1051 [DOI] [Google Scholar]
- EFSA Scientific Committee , 2017. Guidance on Guidance on the risk assessment of substances present in food intended for infants below 16 weeks of age. EFSA Journal 2017;15(5):4849, 58 pp. 10.2903/j.efsa.2017.4849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- EFSA Scientific Committee , 2018. Guidance on risk assessment of the application of nanoscience and nanotechnologies in the food and feed chain: Part 1, human and animal health. EFSA Journal 2018;16(7):5327, 95 pp. 10.2903/j.efsa.2018.5327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eto N, Tomita M and Hayashi M, 2006. NaPi‐mediated transcellular permeation is the dominant route in intestinal inorganic phosphate absorption in rats. Drug Metab Pharmacokinet, 21, 217–221. [DOI] [PubMed] [Google Scholar]
- Ettinger B, 1976. Recurrent nephrolithiasis: natural history and effect of phosphate therapy. A double‐blind controlled study. American Journal of Medicine, 61, 200–206. [DOI] [PubMed] [Google Scholar]
- EU 231/2012 . Commission Regulation (EU) No. 231/2012 of 9 March 2012 laying down specifications for food additives listed in Annexes II and III to Regulation (EC) No. 1333/2008 of the European Parliament and of the Council. Official Journal of the European Union, 22.3.2012, L83/1‐L83/295.
- Expert Group on Vitamins and Minerals , 2003. Safe Upper Levels for Vitamins and Minerals. Available online: https://cot.food.gov.uk/sites/default/files/vitmin2003.pdf
- Faul C, Amaral AP, Oskouei B, Hu MC, Sloan A, Isakova T, Gutiérrez OM, Aguillon‐Prada R, Lincoln J, Hare JM, Mundel P, Morales A, Scialla J, Fischer M, Soliman EZ, Chen J, Go AS, Rosas SE, Nessel L, Townsend RR, Feldman HI, St John Sutton M, Ojo A, Gadegbeku C, Di Marco GS, Reuter S, Kentrup D, Tiemann K, Brand M, Hill JA, Moe OW, Kuro‐O M, Kusek JW, Keane MG and Wolf M, 2011. FGF23 induces left ventricular hypertrophy. The Journal of Clinical Investigation, 121, 4393–4408. 10.1172/jci46122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fine A and Patterson J, 1997. Severe hyperphosphatemia following phosphate administration for bowel preparation in patients with renal failure: two cases and a review of the literature. American Journal of Kidney Diseases, 29, 103–105. [DOI] [PubMed] [Google Scholar]
- Foley RN, Collins AJ, Ishani A and Kalra PA, 2008. Calcium‐phosphate levels and cardiovascular disease in community‐dwelling adults: the Atherosclerosis Risk in Communities (ARIC) Study. American Heart Journal, 156, 556–563. [DOI] [PubMed] [Google Scholar]
- Foley RN, Collins AJ, Herzog CA, Ishani A and Kalra PA, 2009. Serum phosphorus levels associate with coronary atherosclerosis in young adults. Journal of the American Society of Nephrology, 20, 397–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forster I, Hernando N, Sorribas V and Werner A, 2011. Phosphate transporters in renal, gastrointestinal, and other tissues. Advances in Chronic Kidney Disease, 18, 63–76. 10.1053/j.ackd.2011.01.006 [DOI] [PubMed] [Google Scholar]
- Franklin Institute Research Laboratories , 1973. Food Ingredients – phosphates. Report PB 221224.
- Frausto da Silva JJR and Williams RJP, 2001. The Biological Chemistry of the Elements. 2nd Edition, Chapter 18; (Phosphate, silica, and chloride: acid‐base non‐metals). Oxford University Press, New York: 481 pp. Available online http://www.efsa.europa.eu/en/efsajournal/pub/3043.htm?utm_source=alerts&utm_medium=email&utm_content=all&utm_campaign=aih [Google Scholar]
- Fujita H and Sasaki M, 1990. Mutagenicity test of food additives with Salmonella typhimurium TA 97 and TA 102(V). Annual Report of the Tokyo Metropolitan Research Laboratory of Public Health, 41, 315–322. [Google Scholar]
- Goldsmith RS, Bartos H, Hulley SB, Ingbar SH and Moloney WC, 1968. Phosphate supplementation as an adjunct in the therapy of multiple myeloma. Archives of Internal Medicine, 122, 128–133. [PubMed] [Google Scholar]
- Goldsmith RS, Jowsey J, Dubé WJ, Riggs BL, Arnaud CD and Kelly PJ, 1976. Effects of phosphorus supplementation on serum parathyroid hormone and bone morphology in osteoporosis. Journal of Clinical Endocrinology and Metabolism, 43, 523–532. [DOI] [PubMed] [Google Scholar]
- Gonlusen G, Akgun H, Ertan A, Olivero J and Truong LD, 2006. Renal failure and nephrocalcinosis associated with oral sodium phosphate bowel cleansing: clinical patterns and renal biopsy findings. Archives of Pathology and Laboratory Medicine, 130, 101–106. [DOI] [PubMed] [Google Scholar]
- Grabner A, Amaral AP, Schramm K, Singh S, Sloan A, Yanucil C, Li J, Shehadeh LA, Hare JM, David V, Martin A, Fornoni A, Di Marco GS, Kentrup D, Reuter S, Mayer AB, Pavenstädt H, Stypmann J, Kuhn C, Hille S, Frey N, Leifheit‐Nestler M, Richter B, Haffner D, Abraham R, Bange J and Sperl B, 2015. Activation of cardiac fibroblast growth factor receptor 4 causes left ventricular hypertrophy. Cell Metabolism, 22, 1020–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greger JL, Baligar P, Abernathy RP, Bennett OA and Peterson T, 1978. Calcium, magnesium, phosphorus, copper, and manganese balance in adolescent females. American Journal of Clinical Nutrition, 31, 117–121. [DOI] [PubMed] [Google Scholar]
- Güngörmüș C, Kiliç Akay MT and Kolankaya D, 2010. The effects of maternal exposure to food additive E341 (tricalcium phosphate) on foetal development of rats. Environmental Toxicology and Pharmacology, 29, 111–116. [DOI] [PubMed] [Google Scholar]
- Hahn F, 1961. Toxikologie der polyphosphate. Ernahrungsw, Supplement 1, 55–64. [Google Scholar]
- Hahn F and Seifen E, 1959. Weitere untersuchungen zur frage der chronischen verträglichkeit von phosphaten. Arzneimittel‐Forsch, Naturwissenschaften, 9, 501–503.14398844 [Google Scholar]
- Hahn F, Jacobi H and Seifen E, 1958. Do ortho‐ and polyphosphates show variable compatibilities on chronic feeding? Arzneimittel‐Forschung, 8, 286–289. [PubMed] [Google Scholar]
- Hardwick LL, Clemens RA and Jones MR, 1987. Effects of calcium‐phosphate supplementation on calcium, phosphorus, and magnesium‐metabolism in the Wistar Rat. Nutrition Research, 7, 787–796. [Google Scholar]
- Harlan‐Laboratories‐Ltd , 2010a. Tricalcium bis(orthophosphate): Acute oral toxicity in the rat – fixed dose method. Project number 2920/0015. Study sponsor: Inorganic phosphate consortium c/o. Unpublished report.
- Haworth S, Lawlor T, Mortelmans K, Speck W and Zeiger E, 1983. Salmonella mutagenicity test‐results for 250 chemicals. Environmental Mutagenesis, 5, 1–142. [PubMed] [Google Scholar]
- Hayward N, McGovern A, de Lusignan S, Cole N, Hinton W and Jones S, 2017. U‐shaped relationship between serum phosphate and cardiovascular risk: A retrospective cohort study. PLoS ONE, 12, e0184774 10.1371/journal.pone.0184774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaney RP, 1997. Phosphorus. National Academy of Sciences, 146–189. Available online: http://www.nap.edu/catalog/5776.html [Google Scholar]
- Heaney RP, 2012. Phosphorus In: Erdman JW, Jr, MacDonald IA. and Zeisel SH. (eds.). Present Knowledge in Nutrition. 10th edition John Wiley & Sons, Washington, DC, pp. 447–458. [Google Scholar]
- Heaney RP and Nordin BE, 2002. Calcium effects on phosphorus absorption: implications for the prevention and co‐therapy of osteoporosis. Journal of the American College of Nutrition, 21, 239–244. [DOI] [PubMed] [Google Scholar]
- Higgins J, Green S, and Cochrane Collaboration , 2008. Cochrane Handbook for Systematic Reviews of Interventions. Wiley‐Blackwell, Chichester, England; Hoboken, NJ. [Google Scholar]
- Hitchman AJ, Hasany SA, Hitchman A, Harrison JE and Tam C, 1979. Phosphate‐induced renal calcification in the rat. Canadian Journal of Physiology and Pharmacology, 57, 92–97. [DOI] [PubMed] [Google Scholar]
- Hodge HC, 1956. Short term Oral Toxicity Tests of Condensed Phosphates in Rats and Dogs. The University of Rochester School of Medicine and Dentistry and Strong Memorial Hospital, New York. [Google Scholar]
- Hodge HC, 1959. Chronic Oral Toxicity Studies in Rats of Sodium Tripolyphosphate. The University of Rochester School of Medicine and Dentistry, New York. [Google Scholar]
- Hodge HC, 1960. Unpublished report. Chronic oral Toxicity Studies in Rats of Sodium Hexametaphosphate. Department of Pharmacology, University of Rochester School of Medicine and Dentistry, Rochester, New York. [Google Scholar]
- Hruska KA, Mathew S, Lund R, Qiu P and Pratt R, 2008. Hyperphosphatemia of chronic kidney disease. Kidney International, 74, 148–157. 10.1038/ki.2008.130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulley SB, Vogel JM, Donaldson CL, Bayers JH, Friedman RJ and Rosen SN, 1971. The effect of supplemental oral phosphate on the bone mineral changes during prolonged bed rest. The Journal of Clinical Investigation, 50, 2506–2518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huttunen MM, Pietilä PE, Viljakainen HT and Lamberg‐Allardt CJ, 2006. Prolonged increase in dietary phosphate intake alters bone mineralization in adult male rats. Journal of Nutritional Biochemistry, 17, 479–484. [DOI] [PubMed] [Google Scholar]
- Iammarino M and Di Taranto A, 2012. Determination of polyphosphates in products of animal origin: application of a validated ion chromatography method for commercial samples analyses. European Food Research and Technology, 235, 409–417. [Google Scholar]
- International Commission on Radiological Protection (ICRP) , 2002. Basic anatomical and physiological data for use in radiological protection: reference values In: Valentin J. (ed.). Annals of the ICRP. ICRP Publication, Oxford, 89 pp. [Google Scholar]
- IPCS , 2004. IPCS Risk Assessment Terminology(Part 1: IPCS/OECD Key Generic terms used in Chemical Hazard/Risk Assessment (http://www.inchem.org/documents/harmproj/harmproj/harmproj1.pdf)
- Ishidate MJ, Sofuni T, Yoshikawa K, Hayashi M, Nohmi T, Sawada M and Matsuoka A, 1984. Primary mutagenicity screening of food additives currently used in Japan. Food and Chemical Toxicology, 22, 623–636. [DOI] [PubMed] [Google Scholar]
- Itkonen ST, Karp HJ, Kemi VE, Kokkonen EM, Saarnio EM, Pekkinen MH, Kärkkäinen MU, Laitinen EK, Turanlahti MI and Lamberg‐Allardt CJ, 2013. Associations among total and food additive phosphorus intake and carotid intima‐media thickness – a cross‐sectional study in a middle‐aged population in Southern Finland. Nutrition Journal, 12, 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ittner J, Dambacher MA, Muff R, Rüegsegger P, Trechsel U and Fischer JA, 1986. Reduced parathyroid hormone response to peroral phosphate in osteoporotic patients. Mineral and Electrolyte Metabolism, 12, 199–203. [PubMed] [Google Scholar]
- Ix JH, De Boer IH, Peralta CA, Adeney KL, Duprez DA, Jenny NS, Siscovick DS and Kestenbaum BR, 2009. Serum phosphorus concentrations and arterial stiffness among individuals with normal kidney function to moderate kidney disease in MESA. Clinical Journal of the American Society of Nephrology, 4, 609–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ix JH, Anderson CA, Smits G, Persky MS and Block GA, 2014. Effect of dietary phosphate intake on the circadian rhythm of serum phosphate concentrations in chronic kidney disease: a crossover study. American Journal of Clinical Nutrition, 100, 1392–1397. 10.3945/ajcn.114.085498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jastrzębska A, 2009. Modifications of spectrophotometric methods for total phosphorus determination in meat samples. Chemical Papers, 63, 47–54. [Google Scholar]
- Jastrzębska A, 2011. Capillary isotachophoresis as rapid method for determination of orthophosphates, pyrophosphates, tripolyphosphates and nitrites in food samples. Journal of Food Composition and Analysis, 24, 1049–1056. [Google Scholar]
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 1964. Specifications for the identity and purity of food additives and their toxicological evaluation: emulsifiers, stabilizers, bleaching and maturing agents. Seventh report of the Joint FAO/WHO Expert Committee on Food Additives. WHO Technical report series No. 281. [PubMed]
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 1974. Toxicological evaluation of some food additives including anticaking agents, antimicrobials, antioxidants, emulsifiers and thickening agents. Seventeenth Report. Available online: http://www.inchem.org/documents/jecfa/jecmono/v05je88.htm [PubMed]
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 1982a. Evaluation of certain food additives and contaminants. Twenty‐sixth report of the Joint FAO/WHO Expert Committee on Food Additives. Geneva. WHO Technical report series TRS 683.
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 1982b. Phosphoric acid and phosphate salts. In: Toxicological evaluation of certain food additives. Twenty‐sixth meeting of the Joint FAO/WHO Expert Committee on Food Additives. Geneva. WHO Food Additive Series, FAS 17.
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 1986. Evaluation of certain food additives and contaminants. Twenty‐ninth report of the Joint FAO/WHO Expert Committee on Food Additives. Geneva. WHO Technical report series TRS 733. [PubMed]
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 2000. Guidelines for the Preparation of Toxicological Working Papers for the Joint FAO/WHO Expert Committee on Food Additives. Geneva, Switzerland. [Google Scholar]
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 2002. Evaluation of certain food additives and contaminants. Fifty‐seventh report of the Joint FAO/WHO Expert Committee on Food Additives. WHO Technical report series TRS. 909.
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 2006a. Monograph 1. Combined compendium of food additive specifications. Available online: http://www.fao.org/food/food-safety-quality/scientific-advice/jecfa/jecfa-additives/en/
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 2006b. Monograph 1. Combined compendium of food additive specifications. All specifications monographs from the 1st to the 65th meeting (1956‐2005). Volume 4, Available online: http://www.fao.org/food/food-safety-quality/scientific-advice/jecfa/jecfa-additives/en/
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 2006c. Monograph 1. Combined compendium of food additive specifications. All specifications monographs from the 1st to the 65th meeting (1956‐2005). Volume 4, Available online: http://www.fao.org/food/food-safety-quality/scientific-advice/jecfa/jecfa-additives/en/
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 2006d. Monograph 1. Combined compendium of food additive specifications. All specifications monographs from the 1st to the 65th meeting (1956‐2005). Volume 4, Available online: http://www.fao.org/food/food-safety-quality/scientific-advice/jecfa/jecfa-additives/en/
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 2006e. Monograph 1. Combined compendium of food additive specifications. All specifications monographs from the 1st to the 65th meeting (1956‐2005). Volume 4, Available online: http://www.fao.org/food/food-safety-quality/scientific-advice/jecfa/jecfa-additives/en/
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 2006f. Monograph 1. Combined compendium of food additive specifications. All specifications monographs from the 1st to the 65th meeting (1956‐2005). Volume 4, Available online: http://www.fao.org/food/food-safety-quality/scientific-advice/jecfa/jecfa-additives/en/
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 2008. Monograph 5. JECFA specification Volume 4, Available online: http://www.fao.org/food/food-safety-quality/scientific-advice/jecfa/jecfa-additives/en/
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 2012a. Summary report of the seventy‐sixth meeting of JECFA. Available online: http://www.fao.org/fileadmin/user_upload/agns/pdf/76th_JECFA_summary_report.pdf
- JECFA (Joint FAO/WHO Expert Committee on Food Additives), 2012b. Seventy‐sixth report of the Joint FAO/WHO Expert Committee on Food Additives. Available online: https://apps.who.int/iris/bitstream/handle/10665/77752/WHO_TRS_974_eng.pdf;jsessionid=ABF458C5FEFBAE145B4A00A32CFBC6EA?sequence=1
- JECFA , 2018. Available online: http://www.fao.org/food/food-safety-quality/scientific-advice/jecfa/jecfa-additives/en/ [Accessed 10 January 2018]
- Jin H, Xiong Y, Peng Z, He Y, Wang R and Zhou G, 2011. Purification and characterization of myosin‐tripolyphosphatase from rabbit Psoas major muscle: research note. Meat Science, 89, 372–376. [DOI] [PubMed] [Google Scholar]
- Kalantar‐Zadeh K, Gutekunst L, Mehrotra R, Kovesdy CP, Bross R, Shinaberger CS, Noori N, Hirschberg R, Benner D, Nissenson AR and Kopple JD, 2010. Understanding sources of dietary phosphorus in the treatment of patients with chronic kidney disease. Clinical Journal of the American Society of Nephrology, 5, 519–530. 10.2215/cjn.06080809 [DOI] [PubMed] [Google Scholar]
- Karalis M and Murphy‐Gutekunst L, 2006. Patient education. Enhanced foods: hidden phosphorus and sodium in foods commonly eaten. Journal of Renal Nutrition, 16, 79–81. [DOI] [PubMed] [Google Scholar]
- Kärkkäinen M and Lamberg‐Allardt C, 1996. An acute intake of phosphate increases parathyroid hormone secretion and inhibits bone formation in young women. Journal of Bone and Mineral Research, 11, 1905–1912. 10.1002/jbmr.5650111211 [DOI] [PubMed] [Google Scholar]
- Karp H, Ekholm P, Kemi V, Hirvonen T and Lamberg‐Allardt C, 2012. Differences among total and in vitro digestible phosphorus content of meat and milk products. Journal of Renal Nutrition, 22, 344–349. 10.1053/j.jrn.2011.07.004 [DOI] [PubMed] [Google Scholar]
- Karp HJ, Kemi VE, Lamberg‐Allardt CJ and Kärkkäinen MU, 2013. Mono‐ and polyphosphates have similar effects on calcium and phosphorus metabolism in healthy young women. European Journal of Nutrition, 52, 991–996. 10.1007/s00394-012-0406-5 [DOI] [PubMed] [Google Scholar]
- Katsumata S, Matsuzaki H, Katsumata‐Tsuboi R, Uehara M and Suzuki K, 2014. Effects of high phosphorus diet on bone metabolism‐related gene expression in young and aged mice. Journal of Nutrition and Metabolism, 2014, 575932 10.1155/2014/575932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemi VE, Kärkkäinen MU and Lamberg‐Allardt CJ, 2006. High phosphorus intakes acutely and negatively affect Ca and bone metabolism in a dose‐dependent manner in healthy young females. British Journal of Nutrition, 96, 545–552. [PubMed] [Google Scholar]
- Kiliç A, Güngörmüs C, Kolankaya D and Akay MT, 2010. Histopathological, haematological and biochemical effects of E341 (food additive) induced maternal toxicity in rats. Toxicology, 196(Supplement), S330. [Google Scholar]
- Kiliç A, Güngörmüs C, Koçkaya EA, Kolankaya D and Akay MT, 2012. Are there any toxic effects of food additive tricalcium phosphate on pregnant rats and their foetuses? Journal Biological & Chemistry, 40, 171–181. [Google Scholar]
- Kim SJ, Rim KT, Kim HY and Yang JS, 2010. Mutagenicity of octane and tetrasodium pyrophosphate in bacterial reverse mutation (Ames) test. Journal of Toxicological Sciences, 35, 555–562. [DOI] [PubMed] [Google Scholar]
- Kitahori Y, Konishi N, Cho M, Yamamoto K, Nakagawa Y, Matsui E and Hiasa Y, 1998. Lack of carcinogenicity of sodium metaphosphate in Fischer 344 rats. Journal of Pathology, 11, 41–47. [Google Scholar]
- Kovacs CS, 2015. Calcium, phosphorus, and bone metabolism in the fetus and newborn. Early Human Development, 91, 623–628. 10.1016/j.earlhumdev.2015.08.007 [DOI] [PubMed] [Google Scholar]
- Kwak SM, Kim JS, Choi Y, Chang Y, Kwon MJ, Jung JG, Jeong C, Ahn J, Kim HS, Shin H and Ryu S, 2014. Dietary intake of calcium and phosphorus and serum concentration in relation to the risk of coronary artery calcification in asymptomatic adults. Arteriosclerosis, Thrombosis, and Vascular Biology, 34, 1763–1769. [DOI] [PubMed] [Google Scholar]
- Larsson T, Nisbeth U, Ljunggren O, Jüppner H and Jonsson KB, 2003. Circulating concentration of FGF‐23 increases as renal function declines in patients with chronic kidney disease, but does not change in response to variation in phosphate intake in healthy volunteers. Kidney International, 64, 2272–2279. [DOI] [PubMed] [Google Scholar]
- Larsson TE, Olauson H, Hagstrom E, Ingelsson E, Arnlov J, Lind L and Sundström J, 2010. Conjoint effects of serum calcium and phosphate on risk of total, cardiovascular, and noncardiovascular mortality in the community. Arteriosclerosis, Thrombosis, and Vascular Biology, 30, 333–339. [DOI] [PubMed] [Google Scholar]
- Leifheit‐Nestler M, Grosse Siemer R, Flasbart K, Richter B, Kirchhoff F, Ziegler WH, Klintschar M, Becker JU, Erbersdobler A, Aufricht C, Seeman T, Fischer DC, Faul C and Haffner D, 2016. Induction of cardiac FGF23/FGFR4 expression is associated with left ventricular hypertrophy in patients with chronic kidney disease. Nephrology, Dialysis, Transplantation, 31, 1088–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linefsky JP, O'Brien KD, Katz R, de Boer IH, Barasch E, Jenny NS, Siscovick DS and Kestenbaum B, 2011. Association of serum phosphate levels with aortic valve sclerosis and annular calcification: the cardiovascular health study. Journal of the American College of Cardiology, 58, 291–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linefsky JP, O'Brien KD, Sachs M, Katz R, Eng J, Michos ED, Budoff MJ, de Boer I and Kestenbaum B, 2014. Serum phosphate is associated with aortic valve calcification in the Multi‐ethnic Study of Atherosclerosis (MESA). Atherosclerosis, 233, 331–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez FL, Agarwal SK, Grams ME, Loehr LR, Soliman EZ, Lutsey PL, Chen LY, Huxley RR and Alonso A, 2013. Relation of serum phosphorus levels to the incidence of atrial fibrillation (from the Atherosclerosis Risk In Communities [ARIC] study). American Journal of Cardiology, 111, 857–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loughead J and Tsang RC, 1998. Neonatal calcium and phosphorus metabolism In: Cowett RM. (ed.). Principles of Perinatal‐Neonatal Metabolism. 2nd Edition, Springer, Berlin, London, Paris, Milan: pp. 879–908. [Google Scholar]
- Lutsey PL, Alonso A, Michos ED, Loehr LR, Astor BC, Coresh J and Folsom AR, 2014. Serum magnesium, phosphorus, and calcium are associated with risk of incident heart failure: the Atherosclerosis Risk in Communities (ARIC) Study. American Journal of Clinical Nutrition, 100, 756–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackay EM and Oliver J, 1934. Renal damage following the ingestion of a diet containing an excess of inorganic phosphate. Journal of Experimental Medicine, 61, 319–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markowitz GS, Nasr SH, Klein P, Anderson H, Stack JI, Alterman L, Price B, Radhakrishnan J and D'Agati VD, 2004. Renal failure and acute nephrocalcinosis following oral sodium phosphate bowel cleansing. Human Pathology, 35, 675–684. [DOI] [PubMed] [Google Scholar]
- Markowitz GS and Perazella MA, 2009. Acute phosphate nephropathy. Kidney International, 76, 1027–1034. [DOI] [PubMed] [Google Scholar]
- Mars YWHM, Lemmens AG and Beynen AC, 1988. Dietary phosphorus and nephrocalcinosis in female rats. Nutrition Reports International, 38, 249–258. [Google Scholar]
- Mataix J, Aranda P, López‐Jurado M, Sánchez C, Planells E and Llopis J, 2006. Factors influencing the intake and plasma levels of calcium, phosphorus and magnesium in southern Spain. European Journal of Nutrition, 45, 349–354. [DOI] [PubMed] [Google Scholar]
- Matsuzaki H, Masuyama R, Uehara M, Nakamura K and Suzuki K, 2001. Greater effect of dietary potassium tripolyphosphate than of potassium dihydrogenphosphate on the nephrocalcinosis and proximal tubular function in female rats from the intake of a high‐phosphorus diet. Bioscience, Biotechnology, and Biochemistry, 65, 928–934. Available online: http://www.ncbi.nlm.nih.gov/pubmed/11388474 [DOI] [PubMed] [Google Scholar]
- Mazidi M, Nematy M, Heidari‐Bakavoli AR, Namadchian Z, Ghayour‐Mobarhan M and Ferns GA, 2017. The relationship between dietary intake and other cardiovascular risk factors with blood pressure in individuals without a history of a cardiovascular event: Evidence based study with 5670 subjects. Diabetes and Metabolic Syndrome, 11(Suppl 1), S65–S71. 10.1016/j.dsx.2016.12.005 [DOI] [PubMed] [Google Scholar]
- McGovern AP, de Lusignan S, van Vlymen J, Liyanage H, Tomson CR, Gallagher H, Rafiq M and Jones S, 2013. Serum phosphate as a risk factor for cardiovascular events in people with and without chronic kidney disease: a large community based cohort study. PLoS ONE, 8, e74996 10.1371/journal.pone.0074996. eCollection 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHardy GJR and Parsons DS, 1956. The absorption of inorganic phosphate from the small intestine of the rat. Quarterly Journal of Experimental Physiology, 41, 339–409. [Google Scholar]
- McKie VA and McCleary BV, 2016. A novel and rapid colorimetric method for measuring total phosphorus and phytic acid in foods and animal feeds. Journal of AOAC International, 99, 738–743. [DOI] [PubMed] [Google Scholar]
- Miller R, 2010. Functionality of non‐meat ingredients used in enhanced pork. Originally published as a National Pork Board/ American Meat Science Association Fact Sheet, 1998. Updated 2010, Available online: http://www.extension.org/pages/27340/functionality-of-non-meat-ingredients-used-in-enhanced-pork [Accessed: 13 December 2012]
- Miller PD, Neal BJ, McIntyre DO, Yanover MJ, Anger MS and Kowalski L, 1991. Effect of cyclical therapy with phosphorus and etidronate on axial bone mineral density in postmenopausal osteoporotic women. Osteoporosis International, 1, 171–176. [DOI] [PubMed] [Google Scholar]
- Moe SM, Zidehsarai MP, Chambers MA, Jackman LA, Radcliffe JS, Trevino LL, Donahue SE and Asplin JR, 2011. Vegetarian compared with meat dietary protein source and phosphorus homeostasis in chronic kidney disease. Clinical Journal of the American Society of Nephrology, 6, 257–264. 10.2215/cjn.05040610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammad J, Scanni R, Bestmann L, Hulter HN and Krapf R, 2018. A controlled increase in dietary phosphate elevates bp in healthy human subjects. Journal of the American Society of Nephrology, 29, 2089–2098. 10.1681/asn.2017121254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG and Group P, 2009. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. BMJ, 339, b2535 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore LW, Nolte JV, Gaber AO and Suki WN, 2015. Association of dietary phosphate and serum phosphorus concentration by levels of kidney function. American Journal of Clinical Nutrition, 102, 444–453. [DOI] [PubMed] [Google Scholar]
- Morimoto Y, Sakuma M, Ohta H, Suzuki A, Matsushita A, Umeda M, Ishikawa M, Taketani Y, Takeda E and Arai H, 2014. Estimate of dietary phosphorus intake using 24‐h urine collection. Journal of Clinical Biochemistry and Nutrition, 55, 62–66. 10.3164/jcbn.14-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health and Nutrition Examination Survey (NHANES III 1988‐1994) . Available online: https://wwwn.cdc.gov/nchs/nhanes/nhanes3/default.aspx
- Newell GW, Jorgenson TA and Simmon VF, 1974. Unpublished report. Study of mutagenic effects of sodium acid pyrophosphate (FDA No. 71‐61).
- Norwegian Scientific Committee for Food Safety (VKM) , 2017. Suggests upper intake levels on phosphorus. Availble online: https://vkm.no/download/18.2994e95b15cc545071611db/1497967962933/Assessment%20of%20dietary%20intake%20ofphosphorusin%20relation%20to%20tolerable%20upper%20intake%20levels.pdf
- O'Brien KO, Kerstetter JE and Insogna KL, 2014. Phosphorus In: Ross AC, Caballero B, Cousins RJ, Tucker KL. and Ziegler TR. (eds.). Modern Nutrition in Health and Disease. Lippincott Williams & Wilkins, Philadelphia, PA, USA: pp. 150–158. [Google Scholar]
- OECD (Organisation for Economic Co‐operation and Development), 1998. OECD Guidelines for Testing of Chemicals. Repeated Dose 90‐day Oral Toxicity Study in Rodents.
- OECD (Organisation for Economic Co‐operation and Development), 2001. OECD Guidelines for Testing of Chemicals. Acute Oral Toxicity – Fixed Dose Procedure.
- Olivier P and Marzin D, 1987. Study of the genotoxic potential of 48 inorganic derivatives with the SOS chromotest. Mutation Research, 189, 263–269. [DOI] [PubMed] [Google Scholar]
- Onufrak SJ, Bellasi A, Shaw LJ, Herzog CA, Cardarelli F, Wilson PW, Vaccarino V and Raggi P, 2008. Phosphorus levels are associated with subclinical atherosclerosis in the general population. Atherosclerosis, 199, 424–431. [DOI] [PubMed] [Google Scholar]
- Onufrak SJ, Bellasi A, Cardarelli F, Vaccarino V, Muntner P, Shaw LJ and Raggi P, 2009. Investigation of gender heterogeneity in the associations of serum phosphorus with incident coronary artery disease and all‐cause mortality. American Journal of Epidemiology, 169, 67–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orias M, Mahnensmith RL and Perazella MA, 1999. Extreme hyperphosphatemia and acute renal failure after a phosphorus‐containing bowel regimen. American Journal of Nephrology, 19, 60–63. [DOI] [PubMed] [Google Scholar]
- Osgood EE, Tivey H, Klink E, McKenzie M, Hughes ME, Ort J, Gustafson I, Fuller M, Klobucher V and Stoddard H, 1950. The biological half‐life of radioactive phosphorus in the blood of patients. II. Plasma; with deviations of observations from predicted values and an estimate of total‐phosphorus turnover rate. Cancer, 3, 1003–1009. [DOI] [PubMed] [Google Scholar]
- Palomino HL, Rifkin DE, Anderson C, Criqui MH, Whooley MA and Ix JH, 2013. 24‐hour urine phosphorus excretion and mortality and cardiovascular events. Clinical Journal of the American Society of Nephrology, 8, 1202–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park KS, Park J, Choi SH, Ann SH, Singh GB, Shin ES, Lee JS and Chung HC, 2016. Serum phosphorus concentration and coronary artery calcification in subjects without renal dysfunction. PLoS ONE, 11, e0151007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penido MG and Alon US, 2012. Phosphate homeostasis and its role in bone health. Pediatric Nephrology, 27, 2039–2048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pestel S, Krzykalla V and Weckesser G, 2007. Measurement of glomerular filtration rate in the conscious rat. Journal of Pharmacological and Toxicological Methods, 56, 277–289. [DOI] [PubMed] [Google Scholar]
- Poggio ED, Rule AD, Tanchanco R, Arrigain S, Butler RS, Srinivas T, Stephany BR, Meyer KH, Nurko S, Fatica RA, Shoskes DA, Krishnamurthi V, Goldfarb DA, Gill I and Schreiber MJ Jr, 2009. Demographic and clinical characteristics associated with glomerular filtration rates in living kidney donors. Kidney International, 75, 1079–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popovtzer MM, Stjernholm M and Huffer WE, 1976. Effects of alternating phosphorus and calcium infusions on osteoporosis. American Journal of Medicine, 61, 478–484. [DOI] [PubMed] [Google Scholar]
- Portale AA, Halloran BP and Morris RC Jr, 1987. Dietary intake of phosphorus modulates the circadian rhythm in serum concentration of phosphorus. Implications for the renal production of 1,25‐dihydroxyvitamin D. The Journal of Clinical Investigation, 80, 1147–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulsen NA, Rybicka I, Poulsen HD, Larsen LB, Andersen KK and Larsen MK, 2015. Seasonal variation in content of riboflavin and major minerals in bulk milk from three Danish dairies. International Dairy Journal, 42, 6–11. 10.1016/j.idairyj.2014.10.010 [DOI] [Google Scholar]
- Randall DJ and Robinson EC, 1990. Acute toxicological evaluation of various concentrations of phosphoric acid. Journal of American College of Toxicology B, 69–70. [Google Scholar]
- Razzaque MS, 2012. FGF23, klotho and vitamin D interactions: what have we learned from in vivo mouse genetics studies? Advances in Experimental Medicine and Biology, 728, 84–91. [DOI] [PubMed] [Google Scholar]
- REACH (Registration, Evaluation, Authorisation and restriction of Chemicals) Registration Dossier, online. Sodium Metaphosphate. Available online: https://ec.europa.eu/growth/sectors/chemicals/reach_en [Accessed March 2013].
- Reiss E, Canterbury JM, Bercovitz MA and Kaplan EL, 1970. The role of phosphate in the secretion of parathyroid hormone in man. The Journal of Clinical Investigation, 49, 2146–2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritskes‐Hoitinga J, Lemmens AG, Danse LH and Beynen AC, 1989. Phosphorus‐induced nephrocalcinosis and kidney function in female rats. Journal of Nutrition, 119, 1423–1431. [DOI] [PubMed] [Google Scholar]
- Ritskes‐Hoitinga J, Mathot JNJJ, Danse LHJC and Beynen AC, 1991. Commercial rodent diets and nephrocalcinosis in weanling female rats. Laboratory Animals, 25, 126–132. [DOI] [PubMed] [Google Scholar]
- Rulliere C, Perenes L, Senocq D, Dodi A and Marchesseau S, 2012. Heat treatment effect on polyphosphate chain length in aqueous and calcium solutions. Food Chemistry, 134, 712–716. [DOI] [PubMed] [Google Scholar]
- Sabbagh Y, Giral H, Caldas Y, Levi M and Schiavi SC, 2011. Intestinal phosphate transport. Advances in Chronic Kidney Disease, 18, 85–90. 10.1053/j.ackd.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos P, Branco A, Silva S, Paiva A, Baldaia J, Maximino J, Loureiro A and Henrique R, 2010. Acute phosphate nephropathy after bowel cleansing: still a menace. Nefrologia, 30, 702–704. 10.3265/Nefrologia.pre2010.Jul.10544. [DOI] [PubMed] [Google Scholar]
- Scanni R, vonRotz M, Jehle S, Hulter HN and Krapf R, 2014. The human response to acute enteral and parenteral phosphate loads. Journal of the American Society of Nephrology, 25, 2730–2739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SCF (Scientific Committee for Food), 1978. Report of the Scientific Committee for Food on the provisions relating to additives and processing aids in the draft proposal for a council directive concerning the approximation of the laws of Member States relating to fine bakers’ wares, rusks, pastries and biscuits. (Opinion expressed on 1 May 1978). Available online: https://ec.europa.eu/food/sites/food/files/safety/docs/sci-com_scf_reports_05.pdf
- SCF (Scientific Committee for Food), 1991. First series of food additives of various technological functions. (Opinion expressed on 18 May 1990). Available online: https://ec.europa.eu/food/sites/food/files/safety/docs/sci-com_scf_reports_25.pdf
- SCF (Scientific Committee for Food), 1994. Opinion on certain additives for use in infant formulae, follow‐on formulae and weaning foods (Opinion expressed on 11 December 1992). Available online: http://ec.europa.eu/food/fs/sc/scf/reports/scf_reports_32.pdf
- SCF (Scientific Committee for Food), 1996. Opinion on additives in nutrient preparations for use in infant formulae, follow‐on formulae and weaning foods. 7 June 1996. http://ec.europa.eu/food/fs/sc/scf/reports/scf_reports_40.pdf
- SCF (Scientific Committee for Food), 1997. Opinion on additives in nutrient preparations for use in infant formulae, follow‐on formulae and weaning foods (Opinion expressed on 7 June 1996). Available online: http://ec.europa.eu/food/fs/sc/scf/reports/scf_reports_40.pdf.
- SCF (Scientific Committee for Food), 1998. Opinion of the Scientific Committee of Food on the applicability of the ADI (Acceptable Daily Intake) for food additives to infants. 17 September 1998. http://ec.europa.eu/food/fs/sc/scf/out13_en.html
- SCF (Scientific Committee for Food), 2001. Guidance on Submissions for Food Additive Evaluations by the Scientific Committee on Food, opinion expressed on 11 July 2001, SCF/CS/ADD/GEN/26 Final.
- Scharpf LG and Kichline TP, 1967. Stability of long chain polyphosphate in aqueous cheese extracts. Journal of Agricultural and Food Chemistry, 15, 787–789. [Google Scholar]
- Schlemmer U, Frølich W, Prieto RM and Grases F, 2009. Phytate in foods and significance for humans: food sources, intake, processing, bioavailability, protective role and analysis. Molecular Nutrition & Food Research, 53(Suppl 2), S330–S375. 10.1002/mnfr.200900099. [DOI] [PubMed] [Google Scholar]
- Schneider P, Ober KM and Ueberberg H, 1981. Contribution to the phosphate‐induced nephropathy in the dog. Comparative light and electron microscopic investigations on the proximal tubule after oral application of K2HPO4, Na2HPO4, KCl and NaCl. Experimental Pathology, 19, 53–65. Available online: http://www.ncbi.nlm.nih.gov/pubmed/7262273 [DOI] [PubMed] [Google Scholar]
- Schreier K and Noller HG, 1955. Stoffmechselversuche mit venschiedenen markierten Polyphosphaten. Naunyn‐Schmiedebergs Archiv für Experimentelle Pathologie und Pharmakologie, 227, 199–209. [PubMed] [Google Scholar]
- SciFinder , 2013a. Search on CAS Registry Number 7664‐38‐2.
- SciFinder , 2013b. Search on CAS Registry Number 7758‐87‐4.
- SciFinder , 2013c. Search on CAS Registry Number 7778‐77‐0.
- Segawa H, Yamanaka S, Ito M, Kuwahata M, Shono M, Yamamoto T and Miyamoto K, 2005. Internalization of renal type IIc Na‐Pi cotransporter in response to a high‐phosphate diet. American Journal of Physiology Renal Physiology, 288, F587–F596. [DOI] [PubMed] [Google Scholar]
- Seo DS, Kwon M, Sung HJ and Park CB, 2011. Acute oral or dermal and repeated dose 90‐day oral toxicity of tetrasodium pyrophosphate in Sprague Dawley (SD) Rats. Environmental Health and Toxicology, 26, e2011014 10.5620/eht.2011.26.e2011014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro JR, Moore WT, Jorgensen H, Reid J, Epps CH and Whedon D, 1975. Osteoporosis: evaluation of diagnosis and therapy. Archives of Internal Medicine, 135, 563–567. [DOI] [PubMed] [Google Scholar]
- Shevock PN, Khan SR and Hackett RL, 1993. Urinary chemistry of the normal Sprague‐Dawley rat. Urological Research, 21, 309–312. [DOI] [PubMed] [Google Scholar]
- Shin S, Kim KJ, Chang HJ, Cho I, Kim YJ, Choi BW, Rhee Y, Lim SK, Yang WI, Shim CY, Ha JW, Jang Y and Chung N, 2012. Impact of serum calcium and phosphate on coronary atherosclerosis detected by cardiac computed tomography. European Heart Journal, 33, 2873–2881. [DOI] [PubMed] [Google Scholar]
- Silverberg SJ, Shane E, Clemens TL, Dempster DW, Segre GV, Lindsay R and Bilezikian JP, 1986. The effect of oral phosphate administration on major indices of skeletal metabolism in normal subjects. Journal of Bone and Mineral Research, 1, 383–388. [DOI] [PubMed] [Google Scholar]
- Slee TM, Vleming LJ and Valentijn RM, 2008. Renal failure due to acute phosphate nephropathy. The Netherlands Journal of Medicine, 66, 438–441. [PubMed] [Google Scholar]
- Smith DA and Nordin BE, 1964. The effect of a high phosphorus intake on total and ultrafiltrable plasma calcium and on phosphate clearance. Clinical Science, 26, 479–486. [PubMed] [Google Scholar]
- Specialised Nutrition Europe (SNE) , 2018. SNE literature review of phosphate homeostasis, expert body risk assessment opinions and safety studies in response to EFSA request for technical and toxicological data on phosphates for uses as food additives in foods for infants below 16 weeks of age. Available online: http://www.specialisednutritioneurope.eu/sne-literature-review-on-phosphates
- Stöhr R, Schuh A, Heine GH and Brandenburg V, 2018. FGF23 in cardiovascular disease: innocent bystander or active mediator? Frontiers in Endocrinology, 9, 351 10.3389/fendo.2018.00351. eCollection 2018. Review. Erratum in: Front Endocrinol (Lausanne). 2018 Jul 18;9:422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stremke ER, McCabe LD, McCabe GP, Martin BR, Moe SM, Weaver CM, Peacock M and Hill Gallant KM, 2018. Twenty‐four‐hour urine phosphorus as a biomarker of dietary phosphorus intake and absorption in CKD: A secondary analysis from a controlled diet balance study. Clinical Journal of the American Society of Nephrology, 13, 1002–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Q, Bertrand KA, Franke AA, Rosner B, Curhan GC and Willett WC, 2017. Reproducibility of urinary biomarkers in multiple 24‐h urine samples. American Journal of Clinical Nutrition, 105, 159–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szłyk E and Hrynczyszyn P, 2011. Phosphate additives determination in meat products by 31‐phosphorus nuclear magnetic resonance using new internal reference standard: Hexamethylphosphoroamide. Talanta, 84, 199–203. [DOI] [PubMed] [Google Scholar]
- Tavafoghi M and Cerruti M, 2016. The role of amino acids in hydroxyapatite mineralization. Journal of the Royal Society Interface, 13, 20160462 10.1098/rsif.2016.0462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- TemaNord , 2002. Food Additives in Europe 2000 – Status of safety assessments of food additives presently permitted in the EU. Nordic Council of Ministers Food, Copenhagen 2002.
- Tenenhouse HS, 2005. Regulation of phosphorus homeostasis by the type iia na/phosphate cotransporter. Annual Review of Nutrition, 25, 197–214. [DOI] [PubMed] [Google Scholar]
- Þórarinsdóttir KA, Arason S and Þorkelsson G (Skýrsluágrip Matís ohf (Icelandic Food and Biotech R&D), 2010. The role and fate of added phosphates in salted cod products.
- Trautvetter U, Jahreis G, Kiehntopf M and Glei M, 2016. Consequences of a high phosphorus intake on mineral metabolism and bone remodeling in dependence of calcium intake in healthy subjects – a randomized placebo‐controlled human intervention study. Nutrition Journal, 15, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trautvetter U, Ditscheid B, Jahreis G and Glei M, 2018. Habitual intakes, food sources and excretions of phosphorus and calcium in three German study collectives. Nutrients, 10, 171 10.3390/nu10020171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker KL, Morita K, Qiao N, Hannan MT, Cupples LA and Kiel DP, 2006. Colas, but not other carbonated beverages, are associated with low bone mineral density in older women: the Framingham Osteoporosis Study. American Journal of Clinical Nutrition, 84, 936–942. [DOI] [PubMed] [Google Scholar]
- Ulmann A, Sayegh F, Clavel J and Lacour B, 1984. Incidence of lithiasic recurrence after a diuretic therapy, alone or combined with treatment by a thiazide diuretic or phosphorus. Presse Medicale, 13, 1257–1260. [Article in French] [PubMed] [Google Scholar]
- Urasa IT and Ferede F, 1986. The determination of phosphates using ion chromatography: an evaluation of influential factors. International Journal of Environmental Analytical Chemistry, 23, 189–206. [Google Scholar]
- Uribarri J and Calvo MS, 2018. Dietary Phosphorus: Health, Nutrition, and Regulatory Aspects. CRC Press, Taylor & Francis Group. [Google Scholar]
- USDA , 2009. United States Department of Agriculture, Food Safety and Inspection Service, Office of Public Health Science, Method CLG‐PHS1.01, Determination of phosphate.
- Van Buuren S, Schönbeck Y and van Dommelen P, 2012. Collection, collation and analysis of data in relation to reference heights and reference weights for female and male children and adolescents (0‐18 years) in the EU, as well as in relation to the age of onset of puberty and the age at which different stages of puberty are reached in adolescents in the EU. Project developed on the procurement project CT/EFSA/NDA/2010/01. EFSA Supporting Publication 2012;9(3):EN‐255, 59 pp. 10.2903/sp.efsa.2012.en-2255 [DOI] [Google Scholar]
- Van Den Berg CJ, Kumar R, Wilson DM, Heath H 3rd and Smith LH, 1980. Orthophosphate therapy decreases urinary calcium excretion and serum 1,25‐dihydroxyvitamin D concentrations in idiopathic hypercalciuria. Journal of Clinical Endocrinology and Metabolism, 51, 998–1001. [DOI] [PubMed] [Google Scholar]
- Vervaet BA, Verhulst A, Dauwe SE, De Broe ME and D'Haese PC, 2009. An active renal crystal clearance mechanism in rat and man. Kidney International, 75, 41–51. [DOI] [PubMed] [Google Scholar]
- Vorland CJ, Stremke ER, Moorthi RN and Hill Gallant KM, 2017. Effects of excessive dietary phosphorus intake on bone health. Current Osteoporosis Reports, 15, 473–482. 10.1007/s11914-017-0398-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vukasin P, Weston LA and Beart RW, 1997. Oral Fleet Phospho‐Soda laxative‐induced hyperphosphatemia and hypocalcemic tetany in an adult: report of a case. Diseases of the Colon and Rectum, 40, 497–499. [DOI] [PubMed] [Google Scholar]
- Walton J and Gray TK, 1979. Absorption of inorganic phosphate in the human small intestine. Clinical Science (London, England:1979), 01 May 1979, 56, 407–412. 10.1042/cs0560407 [DOI] [PubMed] [Google Scholar]
- Weilmeier DM and Regenstein JM, 2004. Antioxidant properties of phosphates and other additives during the storage of raw mackerel and Lake Trout. Journal of Food Science, 69, fct102–fct108. [Google Scholar]
- Weiner ML, Salminen WF, Larson PR, Barter RA, Kranetz JL and Simon GS, 2001. Toxicological review of inorganic phosphates. Food and Chemical Toxicology, 39, 759–786. [DOI] [PubMed] [Google Scholar]
- WHO (World Health Organization), 2009. Principles and Methods for the Risk Assessment of Chemicals in Food. Environment Health Criteria 240. Available online: http://www.who.int/foodsafety/publications/chemical-food/en/
- WHO/IPCS (World Health Organization/International Programme on Chemical Safety). 2005. Chemical‐Specific Adjustment Factors (CSAF) for interspecies differences and human variability: guidance document for the use of data in dose/concentration‐response assessment. (IPCS harmonization project document no. 2). WHO/IPCS/01.4, 1‐96. Geneva, Switzerland. Available online: http://apps.who.int/iris/bitstream/handle/10665/43294/9241546786_eng.pdf;jsessionid=66218AD59C80969F46FF7F6FD3178CD4?sequence=1
- WHO/IPCS (World Health Organization/International Programme on Chemical Safety), 2014. Guidance document on evaluating and expressing uncertainty in hazard characterization. (IPCS harmonization project document no. 11). Geneva, Switzerland. Available online: http://www.who.int/ipcs/methods/harmonization/uncertainty_in_hazard_characterization.pdf
- Whybro A, Jagger H, Barker M and Eastell R, 1998. Phosphate supplementation in young men: lack of effect on calcium homeostasis and bone turnover. European Journal of Clinical Nutrition, 52, 29–33. [DOI] [PubMed] [Google Scholar]
- Yamamoto KT, Robinson‐Cohen C, de Oliveira MC, Kostina A, Nettleton JA, Ix JH, Nguyen H, Eng J, Lima JA, Siscovick DS, Weiss NS and Kestenbaum B, 2013. Dietary phosphorus is associated with greater left ventricular mass. Kidney International, 83, 707–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamaoka K, Tanaka H, Kurose H, Shima M, Ozono K, Nakajima S and Seino Y, 1989. Effect of single oral phosphate loading on vitamin D metabolites in normal subjects and in X‐linked hypophosphatemic rickets. Bone and Mineral, 7, 159–169. [DOI] [PubMed] [Google Scholar]
- Yilmaz S, Unal F, Yüzbaşıoğlu D and Celik M, 2014. DNA damage in human lymphocytes exposed to four food additives in vitro. Toxicology and Industrial Health, 30, 926–937. 10.1177/0748233712466132 [DOI] [PubMed] [Google Scholar]
- Zipf K, 1957. Toxicology of polyphosphates. Arzneimittel‐Forschung, 7, 445–446. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Summary of the reported use levels (mg/kg or mg/L as appropriate) of phosphates (E 338–341, E 343, E 450–452) provided by industry
Summary of analytical results (mg P/kg or mg P/L as appropriate) of phosphorus provided by Member States
Number and percentage of food products labelled with phosphates (E 338‐341, E 343, E 450‐452) out of the total number of food products present in the Mintel GNPD per food subcategory between 2014 and 2019
Concentration levels of phosphates (E 338–341, E 343, E 450–452) used in the regulatory maximum level exposure assessment scenario and in the refined exposure assessment scenarios (mg/kg or mL/kg as appropriate)
Summary of total estimated exposure of phosphates (E 338–341, E 343, E 450–452) from their use as food additives for the regulatory maximum level exposure assessment scenario and the refined exposure assessment scenarios, in seven population groups (min‐max across the dietary surveys in mg P2O5/kg bw per day and in mg P2O5/person per day)
Total estimated exposure of phosphates (E 338–341, E 343, E 450–452) from their use as food additives for the regulatory maximum level exposure assessment scenario and the refined exposure assessment scenarios per population group and survey: mean and 95th percentile (mg P2O5/kg bw per day)
Main food categories contributing to exposure to phosphates (E 338–341, E 343, E 450–452) using the regulatory maximum level exposure assessment scenario and the refined exposure assessment scenarios, based on the results expressed in mg P2O5/kg bw per day (> 5% to the total mean exposure)
M1: Summary of total estimated exposure of phosphates (E 338–341, E 343, E 450–452) from their use as food additives and the proposed extension of uses for the regulatory maximum level exposure assessment scenario and the refined exposure assessment scenarios (min–max across the dietary surveys in mg P2O5/kg bw per day and in mg P2O5/person per day)
M2: Total estimated exposure of phosphates (E 338–341, E 343, E 450–452) from their use as food additives and the proposed extension of use for the regulatory maximum level exposure assessment scenario and the refined exposure assessment scenarios per population group and survey: mean and 95th percentile (mg P2O5/kg bw per day)
N1: Summary of exposure to total phosphorus via the diet (using analytical data) per population group and survey: mean and 95th percentile (mg P/kg bw per day)
N2: Summary of exposure to total phosphorus via the diet (using analytical data) per population group and survey: mean and 95th percentile (mg P/person per day)
Main food categories contributing to exposure to total phosphorus via the diet (using analytical data, based on exposure in mg P/kg bw per day) (> 5% to the total mean exposure)


