Abstract
Facilitating mentalization, or the ability to understand mental states and their link to behavior, is increasingly viewed as a common mechanism of action across effective psychotherapies. Here we present an overview of a new set of contemplative psychotherapeutic techniques, Mentalizing Imagery Therapy (MIT), that uses guided imagery and mindfulness practices to facilitate mentalization. MIT aims to reduce negative psychological symptoms by stimulating an understanding of mental states and their links to behavior in self and others, including in challenging interpersonal situations. Case discussions of MIT in personality disordered and depressed patients are used to illustrate theoretical points and the specific practical benefits of MIT. We conclude that there are promising indications that the imagery and mindfulness practices of MIT, that are specifically targeted to facilitate insight in the context of attachment relationship challenges, may help to improve mentalization and reduce symptoms of depression and anxiety. Both in practice and with respect to its articulated goals, MIT promotes a distinct set of capacities from other mindfulness or compassion based therapies. Further research is required to determine the clinical efficacy of MIT in controlled trials.
Keywords: mentalization, mindfulness, meditation, guided imagery, personality disorders, depression
Introduction
Mentalization is the capacity to understand one’s own and others’ internal mental processes, such as thoughts, feelings, needs, desires, and motivations, and their relationship to behavior (Allen, 2003; Bateman & Fonagy, 2004). Mentalization is a key determinant of the ability to represent self, develop a coherent self-organization, distinguish self from others, make others’ behavior intelligible, and is intimately related to capacities for affect regulation, impulse control and the experience of self-agency (Fonagy, Gergely, Jurist, & Target, 2002). Deficits in mentalization are common across many psychiatric conditions, including major depression (Fischer-Kern et al., 2013; Ladegaard, Larsen, Videbech, & Lysaker, 2014), post traumatic stress disorder (Plana, Lavoie, Battaglia, & Achim, 2014), anxiety disorders (Nolte, Guiney, Fonagy, Mayes, & Luyten, 2011), psychotic disorders (Adolphs, 2001; Brune, 2005), eating disorders (Kuipers, van Loenhout, van der Ark, & Bekker, 2016), pervasive developmental disorders (Chung, Barch, & Strube, 2014; Frith, 2001), and personality disorders such as borderline personality disorder (BPD) (Bateman & Fonagy, 2012) and antisocial personality disorder (Bateman, O’Connell, Lorenzini, Gardner, & Fonagy, 2016). Moreover, an emerging consensus suggests that a common mechanism of effective psychotherapies is the stimulation of the capacity for mentalization (Allen, 2008; Allen & Fonagy, 2014; Choi-Kain & Gunderson, 2008).
Mentalization Based Therapy (MBT), which focuses on enhancing mentalization through a dynamic psychotherapy approach, has demonstrated efficacy for BPD (Bateman & Fonagy, 1999, 2009) and adolescents who self-harm (Rossouw & Fonagy, 2012). Mentalizing Imagery Therapy (MIT) seeks to encode principles of mentalization into a set of contemplative practices in order to facilitate reduction of psychological symptoms, such as depression and anxiety, and promote greater interpersonal understanding and effectiveness (Morgan, Zamaria, Lavretsky, & Jain, 2018). MIT practices focus on mindfulness of mental phenomena from the outset, and rapidly proceed to contemplate the minds of others, the influence of others on self and that of self on others (Jain, 2014).
“Mentalizing” (the preferred verb form of mentalization) refers to an active process that may be implicit (unconscious) or explicit (conscious) of considering one’s own and others mental states and their intersection. It is closely related to a higher level of cognition (or metacognition) whereby more elaborated and often categorical mental representations are created of lower-level (or second-order) mental representations of primary percepts (Flavell & Miller, 1998). The relationship between mentalizing and other intersecting concepts such as empathy, mindfulness and theory of mind is summarized in Table 1.
Table 1.
Psychological Concepts Related to Mentalizing
| Psychological Concept | Relationship to Mentalizing |
|---|---|
| Empathy | The ability to understand another’s emotions (Singer & Klimecki, 2014). Related to two dimensions of mentalizing: emotion and others. |
| Compassion | A feeling of caring for and desire to alleviate suffering in self and others (Gilbert, 2014; Dalai Lama, 2001; Neff, 2003). At minimum with regards to mentalization, implies an ability to explicitly identify the negative emotional states of oneself and others. |
| Metacognition | Refers to the ability to know and regulate one’s cognitive processes (Metcalfe & Shimamura, 1994). Focuses on the cognitive pole of mentalizing self. |
| Mindfulness | Attention to present moment experience, coupled with a nonjudgmental attitude (Kabat-Zinn, 1990). Mindfulness of mental states may facilitate mentalizing (Allen, 2013). |
| Psychological Mindedness | Disposition to reflect on one’s own and others mental life (Appelbaum, 1973; Farber, 1985). Refers to the explicit, conscious and deliberate aspects of mentalizing (Choi-Kain & Gunderson, 2008). |
| Theory of Mind | The understanding that self and others have mental states (Premack & Woodruff, 1978). Theory of mind is necessary but not sufficient for mentalizing. |
The capacity to mentalize is maturational (similar to linguistic ability) and normally arises within the context of childhood attachment relationships, which facilitate identification of self-states as well as those of caregivers in the context of interpersonal interactions, sometimes in emotionally charged situations (Fonagy et al., 2002). Good mentalizing involves understanding human behavior as ‘agentive’ and motivated by internal states of mind that are always at least partially opaque to others. Characteristics of poor mentalizing include rigidity, claims of all-knowingness about states of mind, lack of curiosity, and black-and-white thinking (Bateman & Fonagy, 2016, pp. 116-120).
On the basis of functional brain imaging studies, mentalizing has been deconstructed into four attributes, each of which is dimensional in nature and can be defined by its extreme poles: cognition–emotion, implicit– explicit, internal–external, self–other (Fonagy & Luyten, 2009). These poles have to be in balance if mentalization is to be adaptive and robust. Imbalances across the poles of mentalization result in phenomenologically observed, non-mentalizing modes of thought. Non-mentalizing modes normally developmentally antedate fully mentalizing modes of thinking and may be more likely to be retained when the emotional environment of the child includes neglect or other adversity (Ensink et al., 2015). In this context, inadequate mentalizing is likely to recur repeatedly within complex interpersonal situations throughout life (Fonagy et al., 1996). Dominant modes of non-mentalizing (which can be directed towards oneself or others) include teleological thinking, psychic equivalence, and pretend mode (Fonagy & Bateman, 2008).
Teleological thinking involves inferring another person’s (or one’s own) state of mind based on actions that have been performed, e.g., “He didn’t call me; therefore, he doesn’t like me.” It reflects the domination of observed (external) processes of mentalizing over inferred (internal) mentalizing (i.e. the loss of the balance between the two) (Bateman & Fonagy, 2016, p. 18).
Psychic equivalence is a mode of functioning characterized by equating internal states with reality, resulting in unwarranted yet deeply held beliefs, such as that others think and feel in exactly the same way as the subject does; e.g., “I am sure she disapproved of me – I could just see it in her eyes”. The narrative is characterized by certainty, the suspension of doubt, an absolute view of reality defined by self-experience, and a sense of finality that bucks any attempt at presenting alternative views of reality – “It just is”. Psychic equivalence reflects the domination of emotion, which is normally experienced with a sense of certainty, over cognition, which is characterized by a sense of doubt (Baron-Cohen, Golan, Chakrabarti, & Belmonte, 2008; Bateman & Fonagy, 2016, p. 17). Psychic equivalence is distinct from thought-action fusion (Shafran, Thordarson, & Rachman, 1996), or the belief that thoughts are the moral equivalent of behaviors or that thinking about unacceptable or disturbing events makes them more likely to happen, in that in psychic equivalence there is an immediate isomorphism between internal mental states and perceptions of others’ mental states in the external world.
Pretend mode, a particularly problematic mode of non-mentalizing for psychological therapy, is a process by which a person’s experience of thoughts and feelings are not based on evidence and are poorly linked to external (or physical) reality. Most commonly, such descriptions of internal states in self and others are overly elaborated, loosely connected to actual events, far more easily modified than might be expected, and carry little emotional conviction. This kind of behavior reflects the dominance of implicit/automatic cognition coupled with an internal hyper-reflective focus unbalanced by observable reality (Bateman & Fonagy, 2016, p. 18).
Certain aspects of mindfulness indicate potential utility for mentalizing. Common to most definitions of mindfulness is an attentional component that involves a focus on present moment experience along with an attitude that is open, nonjudgmental or curious (Anālayo, 2003; Bishop et al., 2004; Van Dam et al., 2017), and this includes attention to mental phenomena. For example, during a mindfulness of breathing exercise in Mindfulness Based Stress Reduction (MBSR) or Mindfulness Based Cognitive Therapy (MBCT), if thoughts occur, one may register them, meta-cognitively categorize them (for example as “judging”, and then return attention to the breath) (Kabat-Zinn, 1990; Segal, Williams, & Teasdale, 2002).
Because mindfulness practices in the clinical setting (such as mindfulness of breathing or the body scan within MBSR and MBCT) most frequently involve attention to self, mindfulness has been categorized in the domain of explicit mentalization of self (Choi-Kain & Gunderson, 2008). However, early Buddhist thought (Anālayo, 2003) and many contemporary mindfulness practices also encourage practitioners to maintain a mindful attitude during interactions with others (for examples of instructions related to mindfulness in relationships, please refer to Stahl and Goldstein (2010, pp. 157-173).
Cognitively, maintaining a mindful attitude facilitates the creation of second-order experience of mental life, i.e., the abstract conceptualization of a thought or emotion as a state of mind being experienced (Fonagy et al., 2002). By doing so, mindfulness provides a frame in which mentalizing becomes possible in contexts where adequate mentalizing would otherwise be hard to achieve. For example, a person who is not maintaining a mindful state of mind, e.g. constantly internally ruminating about how terrible her or his spouse’s past actions have been, may be unable to process and benefit from the spouse’s current more subtle expressions of caring. On the other hand, mindful attention toward ruminative thoughts as thoughts that are a partial description of reality allows for a greater openness to pay attention to present-moment experience of how the spouse is acting with curiosity, and flexible integration of the new information about the spouse into a coherent internal working model that includes past activities (Bretherton & Munholland, 2008; Fresco, Segal, Buis, & Kennedy, 2007). It could be that such thought decentering is most beneficial for mentalization when it helps to place one’s internal reactions and those of others in a specific cause-and-effect narrative. However, this may not necessarily occur, particularly if sustained attention to present-moment experience is rigidly enforced and inhibits reflection on the recent (and remote) past.
Reductions in emotional arousal may also mediate the benefits of mindfulness for mentalization. The capacity for mentalization is inversely related to the level of emotional arousal that a person experiences (Fonagy & Bateman, 2008), particularly in terms of emotional activation of attachment-related experience (Nolte et al., 2013). To the extent that meditative practices or daily mindfulness practices facilitate stress reduction and relaxation that continues outside of the meditation period, they may help to provide a more optimal internal environment for mentalization during daily life. There is preliminary evidence to suggest that mindfulness facilitates mentalization in the immediate aftermath of practice: healthy subjects in a randomized study who engaged in a brief period of breath-focused mindfulness meditation evinced more accurate mental state attribution on the “Reading the Mind in the Eyes” test than a control group which was invited to immerse themselves in their thoughts and feelings (Tan, Lo, & Macrae, 2014). Mindfulness may also impact the implicit pole of mentalizing, as participants randomized to a brief mindfulness exercise showed less in-group preference on the implicit attitudes test than those listening to a natural history recording (Lueke & Gibson, 2015).
To develop meditative practices that might directly promote mentalizing in attachment relationships, Jain (2014) created a set of syncretic meditation and imagery practices that lead to a focus on interpersonally complex situations. The body of MIT practices includes elements of several meditation traditions: mindfulness, tantra, and Upanishadic/Vedantic. These techniques are informed by mentalization theory and therapy (Bateman & Fonagy, 2004; Fonagy et al., 2002), object relations theory (Klein, 1946), and imagery rehearsal techniques (Krakow et al., 2001; Oettingen et al., 2009). MIT practices seek to promote several facets of mentalizing: self from within (the experience of one’s internal mental life), self from outside (how one imagines one comes across to others), others from within (i.e. how others may experience their own emotions, thoughts, etc.) and, most traditionally, others from outside (what others are thinking and feeling). It targets both affective and cognitive poles of mentalization. The practices involve a combination of implicit mentalization (an internal knowing that arises when contemplating the self and others) and explicit mentalization (psychoeducation regarding the mentalizing aspects of the intervention/consciously simulating mental states).
MIT techniques have been taught within different practice settings. These include individual psychotherapy sessions, and four and six week long programs in which participants meet once per week. These practices represent a refinement of those first presented in the context of a feasibility study for stressed dementia caregivers by Jain, Nazarian, & Lavretsky (2014). In the case series below, we provide a brief overview of the practice components of the main MIT techniques, address theoretical foundations of the components, and illustrate how mentalization may be facilitated using brief case examples. Although some cases were drawn from pilot feasibility research studies, it is not our intent in this article to provide formal hypothesis testing of MIT techniques, but rather to provide theoretical background and narrative examples of how the practices facilitate mentalizing as part of a therapeutic process. Individual cases were selected based on the clarity with which participants articulated their experiences and to illustrate the range of conditions in which MIT techniques have been used.
Method
Participants
Cases 1 and 7 were drawn from a 4-week MIT group taught as part of a pilot clinical trial for depressed family dementia caregivers. All procedures were carried out in accordance with University of California, Los Angeles (UCLA), Institutional Review Board #13-001877. Subjects were over 35 years of age, relatives of a patient with dementia and the primary caregiver, and Patient Health Questionnaire 9 score >= 10 (indicating moderate depression symptoms) (Kroenke, Spitzer, & Williams, 2001). Subjects were excluded for active suicidality, primary psychiatric illness other than depression, ongoing substance abuse, unstable medical illness. Case 4 was obtained from a feasibility study of a 6-week MIT group as augmentation for BPD, under the auspices of UCLA Institutional Review Board #14-000150. Subjects in this trial had a DSM-IV diagnosis of BPD and were in ongoing psychotherapy or actively seeking psychotherapy. Exclusion criteria included having made a suicide attempt in the past month or having active suicidal intent. In both studies, the Mini-International Neuropsychiatric Interview (Sheehan et al., 1998) was used to identify cases of depression. Cases 2, 3, 5 and 6 were acquired from the psychotherapy and psychopharmacology practice of the first author. Diagnoses were made according to DSM-IV criteria. Case 8 conveys the experience of a participant in an MIT teacher training program and was utilized with written permission.
Procedure
In reporting the cases, efforts were made to mask individual subject identities by omitting personally identifying details. Ethical treatment of subjects in research studies was made in accordance with the Belmont Report (National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, 1978).
Intervention
For cases drawn from the pilot trials of MIT (Cases 1, 4, and 7), group sessions met once per week for two hours. Participants were provided with an intervention manual and 15 to 30 minute audio recordings of MIT practices for home practice. Each class began with breathing and stretching exercises that emphasized facets of mindfulness, particularly awareness of and attention to physical and mental experience, and then discussed specific MIT practices, one per week in the four week program: “Eye in the Center”, “Nesting Doll”, “Situation Solver”, “Life Globe”). (In the 6 week program for Case 4, two weeks were allocated to “Situation Solver” and two weeks to “Life Globe” practice.) Within the first author’s clinical practice (Cases 3, 5, and 6), MIT techniques were offered in the context of longitudinal treatment that also involved psychodynamic therapy and psychopharmacological treatment, and in this setting a treatment manual was not followed but techniques were proffered per clinical judgment. The teacher training program for MIT (Case 8) lasted 4 weeks and consisted of once weekly instructional meetings and home practice of the techniques with audio recordings.
MIT practices
“Eye in the Center” meditation practice
In this practice, the participants first focus on their natural experience of observing sensations such as the breath. They then attend to a sense of observing awareness. Next, they note their sense of presence in the body using a brief body scan, and finally focus attention particularly at a location in the lower chest, midway between the top of the head and the base of the spine, along the spinal column. The participants “map out” their sensations of breathing, posture and muscular tension, feelings and thoughts, all in relation to this inner central location.
This practice explicitly focuses on recognizing mental experience within the body, and thus serves to promote rudimentary mentalization of self. It moves attention to the lower chest, a region that was associated with self-reflective awareness in ancient Upanishadic thought (Olivelle, 1996, pp. 122-124), and continues to be used in both loving kindness/compassion-based meditation practices (Dalai Lama, 2001) and other relaxation techniques (Childre & Rozman, 2006). This region is consistently topographically mapped in experiences of several primary emotions, including anger, fear, love, happiness, sadness, and anxiety (Nummenmaa, Glerean, Hari, & Hietanen, 2014). Enhancing attention within this region might result in heightened awareness of these constitutional self-states, enhancing their second-order representations and triggering images embodying these emotional states. The connection created by the symbolic representation of embodied affect often triggers memories and thoughts which can serve to elaborate and clarify current concerns.
“Nesting Doll” meditation practice
Following localization of a sense of awareness or perceiving, a participant makes a small imaginal model of self that focuses on her or his mental life and locates this model within the center of the body. The participant does not overly focus on external appearance, but rather directs attention to internal experience and how the body contains it. This may include any surface mental content, including sensations, feelings, thoughts, or daydreams. The participant brings both negative and positive thoughts and emotions into the model, including those he or she would rather avoid. In addition to mental content that spontaneously draws attention, participants also include “lost” elements of self that were reflected upon prior to the meditation: motivations surrounding the desire to learn meditation, present-moment sensations (such as the breathing and that of awareness itself) that are not a part of experience when the mind is fully dominated by feelings and discursive thoughts, and (according to subject-specific beliefs) a sense of spirituality or connection to the divine or the great natural mystery regarding existence.
In this practice, the participant learns to observe their experience of self and hold the various labels for it that may arise in their mind as phenomena worthy of inspection and continued observation. Creating a physical reality for the experience in an object improves identification of self-experience and helps move the experience out of the domain of psychic equivalence, while ensuring that the pendulum does not swing into pretend mode. The creation of a model of the feeling and thinking self is an unambiguous attempt to create a representation of both explicit and implicit mental states and ‘hold’ them in a particular reflective place as a part of physical reality. This practice further stimulates mentalization of self by helping participants observe, without undue avoidance, their thoughts, feelings, and motivations, and to consider these in a neutral-to-positive frame (experience of awareness, sensations of breathing, spirituality/mystery). Towards the end of the practice, mentalization of self is balanced with that of another person by creating a “nesting doll” of the other, grounding it within the physical center, and imagining the other’s self-experience. Implicit mentalizing may be further enhanced outside of the practice when interacting with others; participants are also encouraged to remember the internal world of the other, such as others’ motivations and feelings, during challenging interpersonal situations when there are failures of interpersonal understanding. Ensuring that not only explicit and implicit mentalizing but also self and other mentalizing are balanced may serve to particularly stimulate mentalization of others (Bateman & Fonagy, 2016).
The Nesting Doll meditation adapts tantric practices in which the body was used as a grounding to gain increased insight and benefit from practices. Within Buddhist and Hindu tantric traditions, mental images of spiritual phenomena such as mantras or deities were localized within the body (Dalai Lama, Tsong-ka-pa, & Hopkins, 1987; Kripananda, 1995). Practitioners thus hoped to “absorb” the divine content of the visualization and experience it with greater intensity. In the Nesting Doll meditation, MIT coupled the idea of bringing a visualization into the body with an object relations perspective on the self: that recognition of the self as a “whole” would help to facilitate entry into a “depressive position”, in which a person has the capacity to maintain a realistic view of negative and positive parts of self (Klein, 1946). Unlike classical mindfulness or Upanishadic traditions, there is a reification of an individual, narrative sense of self – not self as an ineffable, empty, or present-moment experience that lacks underlying reality or is a manifestation of “illusion”. There is also an implicit value placed on the narrative self, including that mental elaborations are objects worthy of attention. This differs from most MBSR or MBCT practices, in which attention is shifted from discursive thought to focus largely on present-moment sensory experiences (Kabat-Zinn, 1990; Segal et al., 2002). Towards the end of each part of the visualization (on self or other), the participant is invited to send loving or caring wishes to themselves or the other person of focus “if they wish”. This is not the central focus as in compassion meditation (Jazaieri et al., 2013; Neff & Germer, 2013), but rather a suggestion that the participant may advantage themselves of if they feel ready to do so.
“Situation Solver” imagery practice
In this imagery practice, participants first identify and write about a challenging interpersonal situation that triggered an emotional reaction and a negative behavioral response. They then sit for the imagery practice and engage in a sequence of steps meant to create a context where mentalizing is possible by addressing imbalances of the mentalizing poles: balancing affect with cognition, others’ perspectives with that of the self, an internal perspective with an external/teleological one, and explicit mentalizing with non-reflective implicit mentalizing. To achieve this, the participant is asked to:
Imagine the challenging situation and embody it within the center (reducing arousal).
Imagine the situation occurring from their perspective, including their thoughts and feelings (balancing the mere describing of actions with mentalization of self from the inside).
Switch perspectives to imagine how they came across to the interlocutor (balancing self from inside with mentalization of self from the outside).
Imagine what it would be like to experience the feelings and thoughts the interlocutor might have been having as the other acted back towards them (balancing self with mentalization of other from the inside).
Imagine how their interlocutor would have felt or acted had the participants’ own feelings been fully known or accessible to the interlocutor (further balancing self and other but demanding higher level of cognition to balance emotion).
Take into account the impact of the broader environment in which the situation occurred (e.g. enclosed space, crowd, class, etc.) on the participant’s and the other person’s mental state (technique to loosen rigid schematic thinking and maximize potential for mentalizing).
Remember what “deeper” motivations, reflecting their larger life goals, they would like to bring to the situation if they were in it again, and reflect on their interconnectedness with the other person (with full mentalizing established and narrative coherence and mnemonic access improved, the participant can, by this stage, address and solve the social problem, which will help reintegrate the person into their social context).
This practice helps participants reflect on interpersonal situations that were over-arousing and caused mentalizing deficits. Because the meditative setting reduces emotional arousal and promotes relaxation, it helps them to think more clearly about what happened in their own mind, and that of others, during the situation. The practice invites participants to bring their mental representation of another person, which is often fixed in non-mentalizing modes of thought, into the body. By incorporating the image of the interlocutor into the subject’s own body and including somatic sensations such as breathing and awareness into the fictive image, participants have a firmer base to perceive the other as a whole person. They may emerge from fixed pre-mentalizing modes (such as psychic equivalence or teleology) and experience others from a more grounded and realistic viewpoint. This is consistent with a computational neuroscience approach that suggests that embodied simulation facilitates mentalization, and that therapies engaging the body may help patients with mentalizing deficits (Fineberg, Steinfeld, Brewer, & Corlett, 2014). As in the Nesting Doll practice, there are similarities of this practice with deity visualization techniques, but as opposed to focusing on a deity, the practitioner considers another person and that person’s mind in a particular situation to be a worthy focus of attention.
“Life Globe” meditation practice
In this practice, participants create an image of their world as a whole, and bring parts of the image sequentially into the center. To stimulate their thoughts, a diagram is provided (Figure 1) that illustrates components of their world, including self, family, friends, society, nature, and source. The bottom half of the diagram contains solid lines, which reflect the boundaries they normally perceive through the five senses. The solid lines end in the upper half of the diagram, to represent the unification of physical objects within quantum physics.
Figure 1.
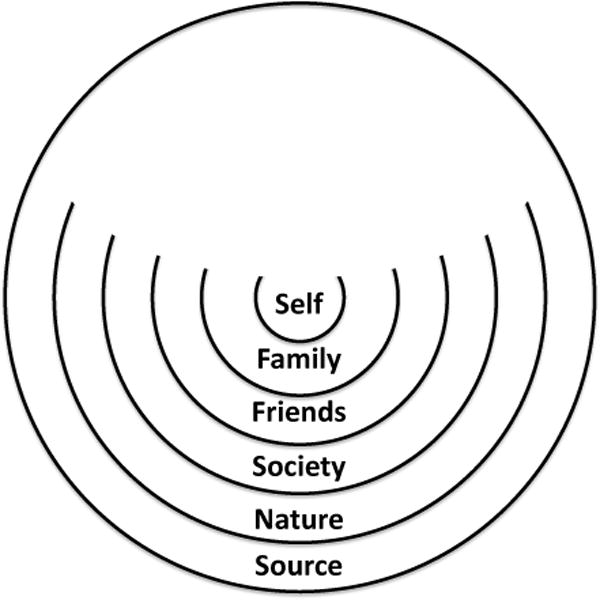
Life Globe diagram
The participant identifies specific family members, friends, communities such as work or school, nature, source as they understand it (i.e. mystery of nature/‘Big Bang’ if they are agnostic or atheist, or God/deity if religious/spiritual). After an image of each person or element is brought into the center (e.g. a family member), the participant shifts perspectives to imagine (1) what that other person feels and thinks about when he or she is sitting at rest without other activities (internal, explicit mentalization of others), and (2) what the person thinks or feels towards the participant (mentalization of self from the outside, as seen by another). For each community or environmental aspect, the participant contemplates how they fit into it and what effect they personally have upon it (furthering a mentalization of self from the outside). With each element, the participant is encouraged to embrace and nurture the fundamental unity within nature that connects them. At the end of the practice, the participant sits with focused awareness of the whole “Life Globe” that they have created, and observes it along with any thoughts or feelings that arise.
This practice aims to create links between the self and different levels of social function. These often become collapsed in the context of intense or disrupted personal attachments and the person is left in a state of psychic equivalence: that the feeling of being alone or isolated with unique challenges means the individual actually is alone. The practice directly departs from a classical Western dualistic framework, notably promoted by Freud (1929/2000), who insisted that experiences of oceanic merging were regressions to a primitive narcissism: “…another way taken by the ego of denying the dangers it sees threatening it in the external world” (p. 5).
However, it equally departs from classical Vedantic or Buddhist mindfulness meditation traditions in which personal feelings, thoughts, and perspectives are often considered to be unreal manifestations (Olivelle, 1996) or fundamentally empty (Anālayo, 2003); MIT instead validates them as part and parcel of the universe. In contrast to meditative stances in which an experience of unity might emerge from recursive observation of internal states or mantra repetition, the Life Globe meditation challenges participants to construct a mental representation of other people’s internal being, and then to contemplate how this is fundamentally connected to their own internal reality. It thus makes explicit an implicit assumption of mentalization: that the mind of another can lead to behavior that then affects one’s own internal world implies a deep and fundamental connectedness.
The instructions for the Life Globe quote Einstein as saying that the notion that one is separated from the rest results from an “optical delusion” of consciousness (Sullivan, 1972). However, there is no insistence that the narrative self is unreal, but rather that a lack of perception of how the self and others are linked results in a tendency towards experiences of loneliness and extreme individuality. By extending the boundaries of self, the practice counters the tendency to experience isolation in the non-mentalizing physical world of social organizations (e.g. work, school, neighborhood) or to use stereotyping and prejudice to dilute self-blame (e.g. ‘women cannot be trusted’; ‘Mexicans are drug dealers and rapists’). Psychodynamic formulation of the Life Globe might be in terms of countering the projection of negative parts of the self into others (paranoid/schizoid tendencies) that may dominate the participants’ relationships (particularly those with severe personality disorders.)
Measures
In the pilot trial cases (Cases 1, 4, and 7) and Case 3, the Quick Inventory of Depression Symptoms – Self Report (QIDS) (Rush et al., 2003) was obtained before and after MIT to measure changes in depression symptoms. Narrative descriptions were drawn from the clinical and research records of the first author.
Data Analyses
The QIDS-SR total score and percentage change was calculated for relevant cases. Depression symptom remission was defined as QIDS-SR score < 6. Narratives were assessed thematically for their relevance to MIT theory.
Results
Case 1
Eye in the Center
During home practice, A 38-year-old female with major depression described first feeling “sadness”, and hen having “images of shadows come back in the shape of girls” into her mind. When contemplating these images and later discussing them with a friend, she realized that they might be related to recent difficulties she had had with a childhood friend. She recognized that this might contribute to her depression. In this case, the “Eye in the Center” meditation helped the participant place her feelings of depression in a narrative context in the setting of an attachment relationship, facilitating mentalization of self and emotion. Quantitatively, she experienced remission of depression symptoms over the course of her 4 week group MIT intervention: QIDS 14 at baseline to 3 at follow up (80% reduction).
Case 2
Eye in the Center
A 58-year-old patient with Major Depression and Parkinson’s disease during practice described an image coming to her mind of a “turtle, with its hard shell but soft interior, rising into the sky.” With further discussion, she realized that the turtle shell was like the rigid encasing of her Parkinsonian body, but that inside there was still an inner mental “softness” of being that she could experience as having a sense of somatic lightness. In this case, the “Eye in the Center practice” helped the patient delineate between experiences of mind and those of body, recognizing the characteristics of each (mentalization of self).
Case 3
Nesting Doll
A 28-year-old female with major depression and generalized anxiety disorder, who had been extremely self-critical since childhood (and felt that her mother had been quite critical of her), experienced an exacerbation of anxiety and depression symptoms during medical school, and tried to numb her symptoms by abusing alcohol and stimulants. Ultimately, she had to withdraw from her training program. She ruminated on ideas of failure and worthlessness. Although she tried to push the thoughts out of her mind, this only helped temporarily, and when something “even a little bad” happened, the thoughts “resurfaced crushingly”.
She was referred to the first author for brief clinical intervention as augmentation for ongoing medication management with another psychiatrist. Previously, she had undergone 12 step programs and yoga teacher training, in which she had received exposure to yogic mindfulness exercises. She was taught the Nesting Doll practice without any other preparatory exercises. As she imagined the model of her having these self-critical thoughts, she noticed how much they contributed to her feeling depressed and anxious, and how much they reflected a part of her – her external failures. However, she noticed that they did not acknowledge her internal qualities, such as empathy and kindness. She learned to observe the thoughts and not push them away but incorporate them into an image that included more parts of her mind, including the motivation she was generating to meditate, to do therapy and to heal. The effort to create a physical reality for her self-critical feelings (of which she had been well aware previously, albeit in a pretend mode) enabled her to avoid getting caught up in the negative thoughts, or (in a psychic equivalence mode) feeling as if they were so real they actually controlled her. She was able to remember more of her goodness, and began to feel more compassion for herself.
In the second part of the meditation focused on an important other, the participant chose to bring a representation of her mother inside her chest and initially experienced this as aversive. She found her mother to be highly critical and “did not want her inside there”. She experienced a physical pain in her chest as she underwent the process and tension in her facial muscles. However, as she continued to look through her mother’s eyes and feel as if within her mother’s body during the session, she experienced not only the criticisms leveled at her but also her mother’s fears and anxieties which prompted them. As she put it, “when I saw her vulnerability, I could also see that I don’t have to take what she says so personally.” After a few sessions, the practice no longer felt aversive or painful and she felt increased compassion for her mother, along with reduced sensitivity to the criticisms leveled at her.
Over the course of three weeks, her depression symptoms reduced by 75% on the QIDS, and anxiety symptoms substantially but not fully resolved on clinical exam. At this point, she was referred back to her psychiatrist for ongoing treatment. Regarding the Nesting Doll focus on self, it may be that non-mentalizing modes of thinking (that she was worthless due to her life failures) were reduced by remembering internal aspects of her mind. In this case, self-compassion emerged as a result of an increased coherence of self-representation (self-understanding). Regarding the Nesting Doll focus on other, embodying the representation of her mother enabled for increased explicit mentalizing of her mother from the inside, and this reduced the extent to which her mother’s criticisms made her feel badly about herself.
Case 4
Situation Solver
A 24-year-old female with BPD and major depression underwent a group MIT program for six weeks as part of a feasibility study while also engaging in Mentalization Based Therapy. She described having had a “screaming match” with her officemate, whom she described in foul language and as an “instigator”. Now she felt anxious about seeing her officemate, to the point of avoiding going to work. During the imaginal part of the Situation Solver exercise, her memory for the event was enhanced, and she realized that she yelled first at her officemate, and wondered whether, if had she not yelled first, her officemate might not have yelled back. She was able to describe the feelings that led to her yelling (particularly, an intense feeling of being disrespected), but was able also to look from her officemate’s perspective, and realize her actions may have generated similar feelings in her officemate as well. She imaginally rehearsed taking her officemate’s feelings into account and acting more calmly in the situation. We suggest that the practice reduced non-mentalizing modes of thinking whereby the experience of being yelled at unequivocally implied that the officemate was “a cold-hearted selfish instigator” (teleological stance) and meant a total lack of respect (psychic equivalence), to a mentalizing construction where affect was less overwhelming and sufficient cognition was available to support the assumption of alternative perspectives. She continued to use some of the MIT practices after the group ended while continuing MBT. Although she was noted to have a 40% reduction in QIDS, she had also made an antidepressant medication addition in the second week that precluded attribution of this effect to MIT.
Case 5
Situation Solver
A 31-year-old male with narcissistic personality disorder and obsessive–compulsive disorder, who previously had engaged in therapy with two providers whom he devalued and who was unwilling to take medications, described in individual psychotherapy that his girlfriend’s past sexual encounters were “personal attacks on him” – despite the fact that these had occurred prior to them having met – because they triggered his anxiety and obsessional thoughts regarding her “purity”. At times, he wanted to hurt and punish her by calling her names like “slut” and “whore” and by shaming her about her inability to live up to their shared religious values. After doing the Situation Solver, he felt he no longer wanted to hurt his girlfriend because he realized “how hurt she would be if she knew that (his) intention was to cause her pain, and (he) felt ashamed about this.” The patient’s ruminations about his girlfriend’s sexual history prior to their meeting – as being some form of direct attack on him – were in the pretend mode completely disconnected from the reality of what had occurred. The Situation Solver brought a balance of internal and external perspectives, reduced ruminations (at least temporarily), and brought forward a state in which he could mentalize and envision the impact of his actions on his girlfriend. After some symptomatic improvement and relative stabilization of his relationship, he ended therapy.
Case 6
Situation Solver
A 39 year-old male with BPD, dissociative identity disorder, chronic methamphetamine abuse, and minor neurocognitive disorder secondary to HIV encephalopathy was seen by the first author for twice-weekly individual mentalization based psychotherapy coupled with MIT techniques. At times when he became very angry, he engaged in self-harming behaviors including swallowing damaging objects such as batteries, coins and razor blades. Prior to therapy, he averaged over 26 emergency room visits and over 45 days of hospitalization on general medical and psychiatric units each year, despite medication management with antidepressant, antipsychotic and mood stabilizing drugs and intensive outpatient community treatment provided by a county case worker. Often, his impulsivity was triggered by interactions with his mother, who served as his legal conservator. In these situations, he felt simultaneously abandoned, alone, humiliated, and misunderstood. For example, his mother attempted to establish a contingency management approach to promote positive behavior. He presented to the following session with an angry and suspicious outburst that she had done so “just because she liked to lord it over him, and wanted him to be disabled so that she could control every aspect of his life”.
Compassion-based and loving kindness meditative practices failed because he experienced them as dismissive of his immediate and pressing concerns – his mother in reality was wrong and controlling – and he automatically dismissed them. Breath-focused mindful awareness exercises sometimes temporarily soothed his mood, but his overall negative judgments – and his automatic thought errors regarding her motives – remained. The Situation Solver meditation led to his developing a representation of his own thoughts and feelings (mentalizing his own reaction) as well as adopting (embodying) her perspective, his level of arousal decreased and he was able to explicitly understand that from his mother’s perspective, the controlling behavior was an indication of her care for his well-being. The change of perspective led to a reduction of hostility, enabled him to feel more connected to his mother, and helped him understand the situation better. His complaints about her lessened, as did his level of agitation. Over the course of a year of therapy that integrated MIT practices coupled with mood stabilizing medication, his emergency room visits, hospitalizations and swallowing episodes declined by more than 80%. Despite this progress, eventual relapse on methamphetamines led to a new cycle of hospitalizations and ultimately his demise via cardiac arrest.
Case 7
Life Globe
A 52-year-old male patient with major depression, caring for his grandmother with dementia, felt isolated due to overwhelming caregiving responsibilities and believed that “no one really cared about [him].” He participated in a 4 week MIT group. During Life Globe practice, after imaginally bringing others into his center and looking from their perspectives, he described remembering “that there are actually a lot of other people out there who care about me,” with whom he interacted on a regular basis. In this case, a teleological mode of thought, that no-one was there for him because they didn’t share his burden of caregiving, was replaced by a deeper understanding of others’ feelings of caring toward him. After the group, the patient reported increased mindfulness and less reactivity to stressors such as his girlfriend leaving him, and his depression symptoms reduced by 37% over the group.
Case 8
Life Globe
It is also useful to consider the potential effects of the Life Globe practice in someone with strong psychological defenses, no diagnosed psychiatric illness, and intact functioning. A nurse learning the practice as part of a teacher training program reported that when contemplating connectedness with family she felt “love, understanding, belonging, and kindness.” With her co-workers, she felt “respected, a leader, quiet, organized, know what to do, professional and maybe on reflection not easy to know me because of my professional personality.” With community she looked “smart, clean, quiet, but a woman with a mission”. With nature, that she was “a part of the problem but am trying with biodegradable products in my home, gardening, recycling”. She also felt that she experienced a sense of connectedness with all things, that “the ‘I’ is not a speck in the universe or world but is melted into all of the source.” The Life Globe practice promoted a sense of connectedness, but importantly did not foster characteristics such as feelings of omnipotence that would suggest regression to a primitive narcissistic state. Rather, it enabled her to gain a more realistic sense of (1) how others regarded her that was tinged with both positive and negative elements, (2) how she affected the world around her, and (3) how she was deeply linked with it. She continued to practice MIT practices on a regular basis.
Discussion
In the eight cases above, MIT practices promoted mentalizing consistent with the practical elements of each guided imagery and mindfulness technique. Those practices focused on the self resulted in varying degrees of self mentalization in the affective, cognitive and explicit domains. Those practices with an element focusing on others resulted in enhanced mentalizing of self from the outside, and others from the inside. This suggests that MIT may have utility in promoting self and other mentalizing.
Comparison of MIT to mindfulness and compassion based therapies
Similarities between MIT and mindfulness and compassion based therapies include increasing awareness of present-moment sensations, and approaching mental experience with a curious and open attitude. There are several differences between the mentalization elements of MIT and the principle mindfulness practices used within MBCT or MBSR. Whereas MIT seeks to achieve a balance across the mentalizing polarities – self-other, internal-external, implicit-explicit, cognitive-affective (Luyten & Fonagy, 2015), – the practices of MBCT and MBSR tend towards a self, internal, implicit focus. Thus, in MBCT and MBSR, attention to discursive thought (explicit) outside of the present moment (external) in the context of relationships (other) is not encouraged within the meditative practices (Kabat-Zinn, 1990; Segal et al., 2002). Self-perception through others’ eyes (another aspect of external mentalizing) is not emphasized. Outside of the meditative practices, daily mindfulness within MBCT and MBSR continues towards an implicit, internal focus on experience, although this may be directed either to self or others, affect or cognition. On the basis of these differences, we hypothesize that participants may experience more relaxation and greater stress reduction through the practices of MBCT and MBSR relative to MIT, but less improvement in the ability to mentalize in complex interpersonal relationships, which requires attention to explicit and external dimensions of mentalizing.
Compassionate Mind Training seeks to reduce self-criticism and shame while increasing acceptance and self-compassion (Gilbert, 2014). This program offers a sophisticated approach to making explicit the psychological defenses that lead to the perpetuation of self-criticism and shame within an evolutionary framework, and then introduces imagery exercises to help the participant form idealized images of caring that the participant may use as a source of self-compassion. CMT has shown some promise for symptom alleviation in patients with symptoms among subjects with chronic mood and personality problems (Gilbert & Procter, 2006), and eating disorders (Kelly, Wisniewski, Martin-Wagar, & Hoffman, 2017). Relative to MIT, CMT focuses more on combatting internal negative feelings with idealized images of caring, and less on external and other focused dimensions of mentalizing.
Similar to MIT, Buddhist-derived compassion meditation and loving kindness (CMLK) therapies (Fredrickson, Cohn, Coffey, Pek, & Finkel, 2008; Jazaieri et al., 2013; Ozawa-de Silva, Dodson-Lavelle, Raison, & Negi, 2012) involve practices that may facilitate self and other mentalizing. CMLK therapies take two major approaches to generating compassionate feelings towards self and others: (1) focusing on an image for which one has immense gratitude or love (such as a relative) and then extending the feelings one has for the loved one to the self and others (Fredrickson et al., 2008; Jazaieri et al., 2013; Neff & Germer, 2013), and (2) engendering a meta-cognitive awareness that others wish for happiness and to avoid suffering just like oneself (Jazaieri et al., 2013; Ozawa-de Silva et al., 2012). In contrast, MIT takes a “bottom up” approach by asking participants to focus on simulating another’s mental states in complex relationship situations without providing a meta-cognitive overlay (consistent with an MBT approach), and focuses more on the external dimension of mentalizing.
Limitations and Future Research
As an experiential intervention that aims to promote mentalizing and reduce negative psychological symptoms, MIT may be studied as a primary or augmentation treatment for other therapies, such as MBT, that aim to stimulate mentalizing in patients, for example those with BPD, as well as to reduce depression and anxiety symptoms. MIT may also benefit caregivers of patients with mental illness. Caregivers often have poor insight into their relatives’ conditions because their relatives’ minds operate in different ways that are experience-distant from the caregiver. Pilot studies suggest that MIT practices are feasible for stressed family dementia caregivers, who described greater understanding and insight into loved ones’ conditions, as well as lasting reductions in depression and anxiety, and improved ability to provide care (Jain et al., 2014; Morgan et al., 2018). We also suggest that MIT may be studied to enhance mentalizing in healthy populations of individuals who would like to enhance self and other mentalizing and their effectiveness in interpersonal relationships. Limitations of this study are intrinsic to those of a case series: namely, lack of control for expectation and non-specific effects.
Acknowledgments
Funding: Felipe A. Jain was supported by grants from the National Institute on Aging #1R21AG051970, the Morris A. Hazan Memorial Foundation, the Friends of the Semel Institute, and an institutional Ruth L. Kirschtein National Research Service Award #5T32MH017140. Peter Fonagy is in receipt of a U.K National Institute for Health Research Senior Investigator Award # NF-SI-0514-10157.
Mentalizing Imagery Therapy: Theory and case series of imagery and mindfulness practices to help understand self and others
Footnotes
Author Contributions. FJ: designed and executed the study, conducted the data analyses, and wrote the paper. PF: collaborated in the writing and editing of the manuscript. All authors approved the final version of the manuscript for submission.
Conflict of Interest. The authors report no conflicts of interest.
Ethics Statement. The University of California, Los Angeles, provided Institutional Review Board approval for the pilot trial cases. Cases drawn from clinical practice were reported in compliance with procedures of the Massachusetts General Hospital Institutional Review Board for case reporting limited to medical records.
Informed Consent. Written informed consent was obtained from all subjects enrolled in research pilot trials.
References
- Adolphs R. The neurobiology of social cognition. Current Opinion in Neurobiology. 2001;11(2):231–239. doi: 10.1016/j.conb.2008.06.003. [DOI] [PubMed] [Google Scholar]
- Allen JG. Mentalizing. Bulletin of the Menninger Clinic. 2003;67(2):91–112. doi: 10.1521/bumc.67.2.91.23440. [DOI] [PubMed] [Google Scholar]
- Allen JG. Mentalizing as a conceptual bridge from psychodynamic to cognitive-behavioral therapy. European Psychotherapy. 2008;8:103–121. doi: 10.1177/0011000008330830. [DOI] [Google Scholar]
- Allen JG. Psychotherapy is an ethical endeavor: Balancing science and humanism in clinical practice. Bulletin of the Menninger Clinic. 2013;77(2):103–131. doi: 10.1521/bumc.2013.77.2.103. [DOI] [PubMed] [Google Scholar]
- Allen JG, Fonagy P. Mentalizing in psychotherapy. In: Hales RE, Yudofsky SC, Roberts LW, editors. The American Psychiatric Publishing textbook of psychiatry. 6th. Washington, DC: American Psychiatric Publishing; 2014. pp. 1095–1118. [Google Scholar]
- Anālayo. Satipaṭṭhāna: The direct path to realization. Birmingham, UK: Windhorse Publications; 2003. [Google Scholar]
- Appelbaum SA. Psychological-mindedness: word, concept and essence. The International Journal of Psycho-Analysis. 1973;54(1):35–46. [PubMed] [Google Scholar]
- Baron-Cohen S, Golan O, Chakrabarti B, Belmonte MK. Social cognition and autism spectrum conditions. In: Sharp C, Fonagy P, Goodyer I, editors. Social cognition and developmental psychopathology. Oxford, UK: Oxford University Press; 2008. pp. 29–56. [Google Scholar]
- Bateman A, Fonagy P. Effectiveness of partial hospitalization in the treatment of borderline personality disorder: A randomized controlled trial. American Journal of Psychiatry. 1999;156(10):1563–1569. doi: 10.1176/ajp.156.10.1563. [DOI] [PubMed] [Google Scholar]
- Bateman A, Fonagy P. Psychotherapy for borderline personality disorder: Mentalization-based treatment. Oxford, UK: Oxford University Press; 2004. [Google Scholar]
- Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. American Journal of Psychiatry. 2009;166(12):1355–1364. doi: 10.1176/appi.ajp.2009.09040539. [DOI] [PubMed] [Google Scholar]
- Bateman A, Fonagy P. Handbook of mentalizing in mental health practice. Washington, DC: American Psychiatric Association Publishing; 2012. [Google Scholar]
- Bateman A, Fonagy P. Mentalization-based treatment for personality disorders: A practical guide. Oxford, UK: Oxford University Press; 2016. [Google Scholar]
- Bateman A, O’Connell J, Lorenzini N, Gardner T, Fonagy P. A randomised controlled trial of mentalization-based treatment versus structured clinical management for patients with comorbid borderline personality disorder and antisocial personality disorder. BMC Psychiatry. 2016;16:1–12. doi: 10.1186/s12888-016-1000-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bateman AW, Fonagy P. The development of an attachment-based treatment program for borderline personality disorder. Bulletin of the Menninger Clinic. 2003;67(3):187–211. doi: 10.1521/bumc.67.3.187.23439. [DOI] [PubMed] [Google Scholar]
- Bateman AW, Fonagy P. Mentalization-based treatment of BPD. Journal of Personality Disorders. 2004;18(1):36–51. doi: 10.1521/pedi.18.1.36.32772. [DOI] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Devins G. Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice. 2004;11(3):230–241. doi: 10.1093/clipsy/bph077. [DOI] [Google Scholar]
- Bretherton K, Munholland KA. Internal working models in attachment relationships: A construct revisited. In: Cassidy J, Shaver PR, editors. Handbook of attachment: Theory, research and clinical applications. 2nd. New York, NY: Guilford Press; 2008. pp. 89–111. [Google Scholar]
- Brune M. “Theory of mind” in schizophrenia: A review of the literature. Schizophrenia Bulletin. 2005;31(1):21–42. doi: 10.1093/schbul/sbi002. [DOI] [PubMed] [Google Scholar]
- Childre DL, Rozman D. Transforming anxiety: The HeartMath solution for overcoming fear and worry and creating serenity. Oakland, CA: New Harbinger Publications, Inc.; 2006. [Google Scholar]
- Choi-Kain LW, Gunderson JG. Mentalization: Ontogeny, assessment, and application in the treatment of borderline personality disorder. American Journal of Psychiatry. 2008;165(9):1127–1135. doi: 10.1176/appi.ajp.2008.07081360. [DOI] [PubMed] [Google Scholar]
- Chung YS, Barch D, Strube M. A meta-analysis of mentalizing impairments in adults with schizophrenia and autism spectrum disorder. Schizophrenia Bulletin. 2014;40(3):602–616. doi: 10.1093/schbul/sbt048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lama Dalai. An open heart: Practicing compassion in everyday life. Boston, MA: Little Brown & Co.; 2001. [Google Scholar]
- Dalai Lama Tsong-ka-pa, Hopkins J. Deity Yoga: In action and performance tantra. Ithaca, NY: Snow Lion Publications; 1987. [Google Scholar]
- Ensink K, Normandin L, Target M, Fonagy P, Sabourin S, Berthelot N. Mentalization in children and mothers in the context of trauma: An initial study of the validity of the Child Reflective Functioning Scale. British Journal of Developmental Psychology. 2015;33(2):203–217. doi: 10.1111/bjdp.12074. [DOI] [PubMed] [Google Scholar]
- Farber BA. The genesis, development, and implications of psychological-mindedness in psychotherapists. Psychotherapy: Theory, Research, Practice, Training. 1985;22(2):170–177. doi: 10.1037/h0085490. [DOI] [Google Scholar]
- Fineberg SK, Steinfeld M, Brewer JA, Corlett PR. A computational account of borderline personality disorder: Impaired predictive learning about self and others through bodily simulation. Frontiers in Psychiatry. 2014;5:111. doi: 10.3389/fpsyt.2014.00111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer-Kern M, Fonagy P, Kapusta ND, Luyten P, Boss S, Naderer A, Leithner K. Mentalizing in female inpatients with major depressive disorder. Journal of Nervous and Mental Disease. 2013;201(3):202–207. doi: 10.1097/NMD.0b013e3182845c0a. [DOI] [PubMed] [Google Scholar]
- Flavell JH, Miller PH. Social cognition. In: Damon W, Kuhn D, Siegler RS, editors. Handbook of child psychology. 5th. New York, NY: Wiley; 1998. pp. 851–898. [Google Scholar]
- Fonagy P, Bateman A. The development of borderline personality disorder–a mentalizing model. Journal of Personality Disorders. 2008;22(1):4–21. doi: 10.1521/pedi.2008.22.1.4. [DOI] [PubMed] [Google Scholar]
- Fonagy P, Gergely G, Jurist EL, Target M. Affect regulation, mentalization, and the development of the self. New York, NY: Other Press; 2002. [Google Scholar]
- Fonagy P, Leigh T, Steele M, Steele H, Kennedy R, Mattoon G, Gerber A. The relation of attachment status, psychiatric classification, and response to psychotherapy. Journal of Consulting and Clinical Psychology. 1996;64(1):22–31. doi: 10.1037/0022-006X.64.1.22. [DOI] [PubMed] [Google Scholar]
- Fonagy P, Luyten P. A developmental, mentalization-based approach to the understanding and treatment of borderline personality disorder. Development and Psychopathology. 2009;21(4):1355–1381. doi: 10.1017/S0954579409990198. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL, Cohn MA, Coffey KA, Pek J, Finkel SM. Open hearts build lives: Positive emotions, induced through loving-kindness meditation, build consequential personal resources. Journal of Personality and Social Psychology. 2008;95(5):1045–1062. doi: 10.1037/a0013262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fresco DM, Segal ZV, Buis T, Kennedy S. Relationship of posttreatment decentering and cognitive reactivity to relapse in major depression. Journal of Consulting and Clinical Psychology. 2007;75(3):447–455. doi: 10.1037/0022-006X.75.3.447. [DOI] [PubMed] [Google Scholar]
- Freud S. Civilization and its discontents. Aylesbury, UK: Chrysoma Associates Ltd; 2000. Original work published 1929. [Google Scholar]
- Frith U. Mind blindness and the brain in autism. Neuron. 2001;32(6):969–979. doi: 10.1016/S0896-6273(01)00552-9. [DOI] [PubMed] [Google Scholar]
- Gilbert P. The origins and nature of compassion focused therapy. British Journal of Clinical Psychology. 2014;53(1):6–41. doi: 10.1111/bjc.12043. [DOI] [PubMed] [Google Scholar]
- Gilbert P, Procter S. Compassionate mind training for people with high shame and self-criticism: Overview and pilot study of a group therapy approach. Clinical Psychology & Psychotherapy. 2006;13(6):353–379. doi: 10.1002/cpp.507. [DOI] [Google Scholar]
- Jain FA. Mentalizing Imagery Therapy for Dementia Caregivers: Instructor Manual. 2014 Unpublished manuscript. [Google Scholar]
- Jain FA, Nazarian N, Lavretsky H. Feasibility of central meditation and imagery therapy for dementia caregivers. International Journal of Geriatric Psychiatry. 2014;29(8):870–876. doi: 10.1002/gps.4076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jazaieri H, Jinpa GT, McGonigal K, Rosenberg EL, Finkelstein J, Simon-Thomas E, Goldin PR. Enhancing compassion: A randomized controlled trial of a compassion cultivation training program. Journal of Happiness Studies. 2013;14(4):1113–1126. doi: 10.1007/s10902-012-9373-z. [DOI] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Delacorte Press; 1990. [Google Scholar]
- Kelly AC, Wisniewski L, Martin-Wagar C, Hoffman E. Group-based Compassion-Focused Therapy as an adjunct to outpatient treatment for eating disorders: A pilot randomized controlled trial. Clinical Psychology & Psychotherapy. 2017;24(2):475–487. doi: 10.1002/cpp.2018. [DOI] [PubMed] [Google Scholar]
- Klein M. Notes on some schizoid mechanisms. International Journal of Psychoanalysis. 1946;27:99–110. [PubMed] [Google Scholar]
- Krakow B, Hollifield M, Johnston L, Koss M, Schrader R, Warner TD, Prince H. Imagery rehearsal therapy for chronic nightmares in sexual assault survivors with posttraumatic stress disorder: a randomized controlled trial. JAMA. 2001;286(5):537–545. doi: 10.1001/jama.286.5.537. [DOI] [PubMed] [Google Scholar]
- Kripananda S. The sacred power: A seeker’s guide to Kundalini. South Fallsburg, NY: SYDA Foundation; 1995. [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuipers GS, van Loenhout Z, van der Ark LA, Bekker MH. Attachment insecurity, mentalization and their relation to symptoms in eating disorder patients. Attachment and Human Development. 2016;18(3):250–272. doi: 10.1080/14616734.2015.1136660. [DOI] [PubMed] [Google Scholar]
- Ladegaard N, Larsen ER, Videbech P, Lysaker PH. Higher-order social cognition in first-episode major depression. Psychiatry Research. 2014;216(1):37–43. doi: 10.1016/j.psychres.2013.12.010. [DOI] [PubMed] [Google Scholar]
- Lueke A, Gibson B. Mindfulness meditation reduces implicit age and race bias: The role of reduced automaticity of responding. Social Psychological and Personality Science. 2015;6(3):284–291. doi: 10.1177/1948550614559651. [DOI] [Google Scholar]
- Luyten P, Fonagy P. The neurobiology of mentalizing. Personality Disorders: Theory, Research, and Treatment. 2015;6(4):366–379. doi: 10.1037/per0000117. [DOI] [PubMed] [Google Scholar]
- Metcalfe J, Shimamura AP. Metacognition: Knowing about knowing. Cambridge, MA: MIT Press; 1994. [Google Scholar]
- Morgan S, Zamaria J, Lavretsky H, Jain F. Mentalizing Imagery Therapy for depressed family dementia caregivers: Neural mechanisms underlying changes in mindfulness, self-compassion and grief. American Journal of Geriatric Psychiatry. 2018;26(3):S80–S81. doi: 10.1016/J.JAGP.2018.01.098. [DOI] [Google Scholar]
- National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. The Belmont report: Ethical principles and guidelines for the protection of human subjects of research. Washington, DC: U.S. Government Printing Office; 1978. [PubMed] [Google Scholar]
- Neff KD. The Development and Validation of a Scale to Measure Self-Compassion. Self and Identity. 2003;2(3):223–250. doi: 10.1080/15298860390209035. [DOI] [Google Scholar]
- Neff KD, Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. Journal of Clinical Psychology. 2013;69(1):28–44. doi: 10.1002/jclp.21923. [DOI] [PubMed] [Google Scholar]
- Nolte T, Bolling DZ, Hudac CM, Fonagy P, Mayes L, Pelphrey KA. Brain mechanisms underlying the impact of attachment-related stress on social cognition. Frontiers in Human Neurosciences. 2013;7:816. doi: 10.3389/fnhum.2013.00816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolte T, Guiney J, Fonagy P, Mayes LC, Luyten P. Interpersonal stress regulation and the development of anxiety disorders: An attachment-based developmental framework. Frontiers in Behavioral Neuroscience. 2011;5:55. doi: 10.3389/fnbeh.2011.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nummenmaa L, Glerean E, Hari R, Hietanen JK. Bodily maps of emotions. Proceedings of the National Academy of Sciences. 2014;111(2):646–651. doi: 10.1073/pnas.1321664111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oettingen G, Mayer D, Timur Sevincer A, Stephens EJ, Pak HJ, Hagenah M. Mental contrasting and goal commitment: the mediating role of energization. Personality and Social Psychology Bulletin. 2009;35(5):608–622. doi: 10.1177/0146167208330856. [DOI] [PubMed] [Google Scholar]
- Olivelle P. Upaniṣads. Oxford, UK: Oxford University Press; 1996. [Google Scholar]
- Ozawa-de Silva B, Dodson-Lavelle B, Raison CL, Negi LT. Compassion and ethics: Scientific and practical approaches to the cultivation of compassion as a foundation for ethical subjectivity and well-being. Journal of Healthcare, Science, and the Humanities. 2012;II(1):145–161. [Google Scholar]
- Plana I, Lavoie MA, Battaglia M, Achim AM. A meta-analysis and scoping review of social cognition performance in social phobia, posttraumatic stress disorder and other anxiety disorders. Journal of Anxiety Disorders. 2014;28(2):169–177. doi: 10.1016/j.janxdis.2013.09.005. [DOI] [PubMed] [Google Scholar]
- Premack D, Woodruff G. Does the chimpanzee have a theory of mind? Behavioral and Brain Sciences. 1978;1(4):515–526. doi: 10.1017/S0140525x00076512. [DOI] [Google Scholar]
- Rossouw TI, Fonagy P. Mentalization-based treatment for self-harm in adolescents: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51(12):1304–1313. doi: 10.1016/j.jaac.2012.09.018. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, Keller MB. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry. 2003;54(5):573–583. doi: 10.1016/S0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. New York, NY: Guilford Press; 2002. [Google Scholar]
- Shafran R, Thordarson DS, Rachman S. Thought-action fusion in obsessive compulsive disorder. Journal of Anxiety Disorders. 1996;10(5):379–391. doi: 10.1016/0887-6185(96)00018-7. [DOI] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar JC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(Suppl 20):22–33. doi: 10.1016/S0924-9338(99)80239-9. [DOI] [PubMed] [Google Scholar]
- Singer T, Klimecki OM. Empathy and compassion. Current Biology. 2014;24(18):R875–R878. doi: 10.1016/j.cub.2014.06.054. [DOI] [PubMed] [Google Scholar]
- Stahl B, Goldstein E. A mindfulness-based stress reduction workbook. Oakland, CA: New Harbinger Publications; 2010. [Google Scholar]
- Sullivan W. The Einstein papers. A man of many parts. New York Times. 1972 Mar 29;:20. [Google Scholar]
- Tan LB, Lo BC, Macrae CN. Brief mindfulness meditation improves mental state attribution and empathizing. PLoS ONE. 2014;9(10):e110510. doi: 10.1371/journal.pone.0110510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Dam NT, van Vugt MK, Vago DR, Schmalzl L, Saron CD, Olendzki A, Meyer DE. Mind the hype: A critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspectives on Psychological Science. 2017;13(1):36–61. doi: 10.1177/1745691617709589. [DOI] [PMC free article] [PubMed] [Google Scholar]


