Abstract
Adipose tissue derived mesenchymal stem/stromal cell (ASC)-derived extracellular vesicles (EV) have been reported to be beneficial against dextran sulfate sodium (DSS)-induced colitis in mice. However, the underlying mechanisms have not been fully elucidated. We hypothesize that the tumor necrosis factor-α-stimulated gene/protein 6 (TSG-6) in EVs is a key factor influencing the alleviation of colitis symptoms. DSS-induced colitis mice (C57BL/6, male, Naïve = 6, Sham = 8, PBS = 8 EV = 8, CTL-EV = 8, TSG-6 depleted EV = 8) were intraperitoneally administered EVs (100 ug/mice) on day 1, 3, and 5; colon tissues were collected on day 10 for histopathological, RT-qPCR, western blot and immunofluorescence analyses. In mice injected with EV, inflammation was alleviated. Indeed, EVs regulated the levels of pro- and anti-inflammatory cytokines, such as TNF-α, IL-1β, IFN-γ, IL-6, and IL-10 in inflamed colons. However, when injected with TSG-6 depleted EV, the degree of inflammatory relief was reduced. Furthermore, TSG-6 in EVs plays a key role in increasing regulatory T cells (Tregs) and polarizing macrophage from M1 to M2 in the colon. In conclusion, this study shows that TSG-6 in EVs is a major factor in the relief of DSS-induced colitis, by increasing the number of Tregs and macrophage polarization from M1 to M2 in the colon.
Introduction
Inflammatory bowel disease (IBD) is a chronic debilitating disease that affects both humans and dogs, characterized by abdominal pain and diarrhoea. It may result in significant morbidity and mortality, with compromised quality of life and life expectancy. Clinical signs may be controlled by single or combination therapy, including dietary modifications, antibiotics and immune-suppressants. However, since there is no clear treatment method, clinical recurrence frequently occurs even after treatment, and thus, new therapeutic agents need to be sought [1].
Adipose tissue derived mesenchymal stem/stromal cells (ASCs) are of great interest as novel therapeutics for IBD patients because of their unique ability to regulate immune cells and heal damaged colonic tissue [2]. Particularly, it has been found that extracellular vesicles (EVs, 40–1000 nm sized circular membrane fragments shed from the cell surface) secreted from cells can mediate the delivery of secreted molecules in cell-to-cell communication. Thus, studies on the use of EVs as an alternative to stem cells have been actively conducted [3, 4]. Recently, various studies have been carried out on the application of EVs as therapeutic agents in various pre-clinical models such as acute kidney injury, hepatitis, cystitis and uveitis[5–8]. In addition, injecting EVs into DSS-induced colitis mouse models has shown that not only does it improve activity and appetite, but it also alleviates inflammation in the colon [9]. Although these studies reported that damaged tissues were improved following treatment with EVs, the factors responsible for the protective effects have yet to be elucidated. If stem cell-derived EVs are to be used as therapeutic agents in the future, in-depth mechanistic studies to determine which factors are most highly associated with the ability of EVs to alleviate inflammation must be conducted.
Tumor necrosis factor (TNF)-α stimulated gene/ protein 6 (TSG-6) secreted from stem cells is a major factor responsible for regulation of inflammatory responses [10–12]. Moreover, several studies have shown that TSG-6 plays important roles in attenuating DSS-induced colitis in mice by altering the composition of immune cells in the colon [11, 13]. However, studies on TSG-6 in EVs have not yet been conducted, and, thus, further studies are required.
In particular, IBD is related to an immunological imbalance in the intestinal mucosa, which is primarily associated with cells of the adaptive immune system that respond to self-antigens produced under inflammatory conditions in such patients [14, 15]. Among the intestinal immune cells, regulatory T cells (Tregs) control the balance of immune cell functions and play critical roles in self-tolerance and homeostasis in the colon [16]. Additionally, macrophages of the colon are essential for local homeostasis and play an important role in inflammation and protective immunity[17]. And they are classically divided into two major types: A very basic dichotomous view classified M1 as having an inflammatory phenotype, while M2 was considered an anti-inflammatory macrophage[18]. For this reason, various methods of increasing Tregs and macrophage M2 types in the colon in colitis experimental models have been proposed as treatment options, with stem cell derived EV being one of them[9, 19]. However, there is still a lack of research on mechanisms, and there is a need for further study.
Therefore, this study focused on elucidating the role of TSG-6 in EVs in mitigating colitis and as well as to describe potential mechanisms responsible for any protective effects observed in DSS-induced mouse models of colitis. We also investigated the effect that EVs have on Treg and M2 within the colon and how TSG-6 in EVs affects the Treg and M2 population in inflamed colons.
Materials and methods
All animal experimental procedures were approved by the Institutional Animal Care and Use Committee of Seoul National University (SNU), Republic of Korea, and all protocols were in accordance with approved guidelines (SNU; protocol no. SNU-180829-2-1).
Isolation, culture, and characterization of cASCs
The adipose tissue was obtained from a healthy adult female dog during ovariohysterectomy at the SNU Veterinary Medicine Teaching Hospital, with the owner’s consent. ASCs were isolated from tissues and cultures as previous described [11, 20]. The cells were characterized for the expression of several stem cell markers by flow cytometry before they were used in the experiments. Additionally, the differentiation ability of cells was confirmed for cASCs at passages 3 and 4, and these cells were used in subsequent experiments. The methods used for isolating, culturing, and characterizing stem cells are described in detail in S1 File, and corresponding results were described in detail in S1 Fig. This experiment was repeated a minimum of three times to confirm reproducibility.
Small interfering RNA (siRNA) transfection of cASCs
To obtained TSG-6 depleted EV, when cASCs reached approximately 70% confluence, they were transfected for 48 h with TSG-6 siRNA or control siRNA (sc-39819 and sc-27007, respectively, Santa Cruz Biotechnology, Dallas, TX, USA) using Lipofectamine RNAiMAX (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s instructions [11, 20, 21]. TSG-6 knockdown was confirmed by gel PCR and RT-qPCR. The cells were washed twice with PBS, and the media was exchanged with DMEM containing exosome-depleted FBS for an additional 48 h before collecting TSG-6-depleted EVs. EVs were obtained using an ultracentrifuge as above described, and the relative TSG-6 protein levels in EVs were measured by western blot analysis. Protein concentrations were determined by performing BCA assays. The total protein content (20 μg) of each sample was subjected to sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and immunoblotting with antibodies against CD63 (NBP2-42225; Novus Inc., Littleton, CO, USA)) and TSG-6 (sc-30140; Santa Cruz Biotechnology). These results were described in S2 Fig. This experiment was repeated a minimum of three times to confirm reproducibility.
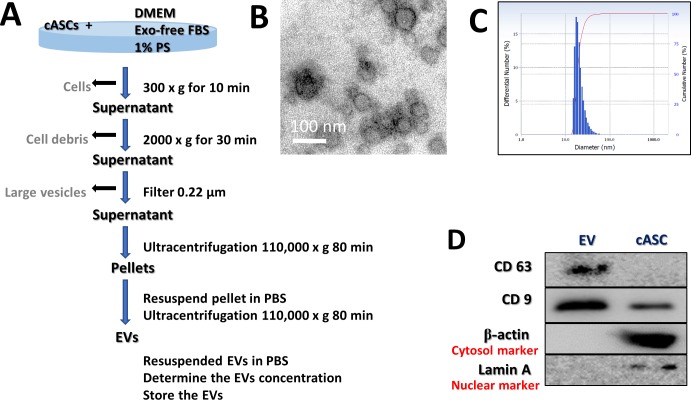
Isolation and characterization of EVs
cASCs were cultured for 48 h in Dulbecco's Modified Eagle's Medium (DMEM; PAN-Biotech, Aidenbach, Germany) supplemented with 10% Exosome-depleted Fetal bovine serum (FBS; Systembio, CA, USA) and 1% penicillin-streptomycin (PS; PAN-Biotech). The supernatant from each cultured cASC sample was collected on ice and centrifuged at 300 × g for 10 min to remove the cells. Each supernatant was transferred to a fresh tube, centrifuged at 2000 × g for 30 min to remove cellular debris, and then passed through a 0.22-μm filter (Millipore, Billerica, MA, USA) to remove the large vesicles. Each supernatant was transferred to a fresh tube and centrifuged at 110,000 × g (Beckman Avanti Centrifuge J-26XP with 70Ti rotor, Brea, CA, USA) for 80 min, washed with Dulbecco’s phosphate-buffered saline (DPBS), and purified by centrifugation at 110,000 × g for 80 min. All centrifugation steps were performed at 4°C. Each pellet was resuspended in DPBS and sterilized by filtration through a 0.22-μm filter (Fig 1C). The total protein concentration in each EV preparation was quantified by performing bicinchoninic acid (BCA) assays, and the samples were stored at −80°C until use. Protein markers of purified EVs were determined by western blotting with antibodies against CD63 (Novus Inc.) and CD9 (GTX76185; GeneTex, Irivine, CA, USA). The EV morphology was characterized by transmission electron microscopy. Briefly, 10 μL of an EV suspension was placed on clean parafilm. A 300-mesh formvar/carbon-coated electron microscopy grid was floated on the drop, with the coated side facing the suspension, and allowed to adsorb for 20 min at 23 ± 2ଌ. The grid was transferred to a 100 μL drop of distilled water and left to stand for 2 min. The grid was then transferred to a 50 μL drop of 2% uranyl acetate for negative staining for 10 min, followed by observation under a TEM (LIBRA 120, Carl Zeiss, Germany) at 120 kV. The size distribution of the particles was measured using a Zeta-potential & Particle size Analyzer (ELSZ-1000ZS, Otsuka Electronics, Osaka, Japan). This experiment was repeated a minimum of three times to confirm reproducibility.
Fig 1. Characterization of cASC-EVs.
(A) Schematic overview of the UC-based purification protocol (B) Scanning electron microscopy micrographs of cASC-EV showed spheroid shaped vesicles with diameters of approximately 20–100 nm. Scale bar, 50 nm. (C) Size-distribution analysis of purified cASC-EVs showed that the vesicle diameters were approximately 20–100 nm. (D) Immunoblotting analysis of common EV markers, where 10 μg of total protein was loaded in each lane. cASCs-EVs expressed CD63 and CD9, while beta actin and lamin A showed lower expression. The displayed data represent at least three repeated experiments with consistent results.
Isolation of peripheral blood mononuclear cells (PBMCs) and non-adherent cells
Using citrate phosphate dextrose adenine-containing tubes, we collected blood samples (30 mL) from three healthy dogs. The blood samples were diluted with an equal volume of phosphate-buffered saline (PBS) and then layered over Ficoll-Plaque PLUS (GE Healthcare Life Sciences, Little Chalfont, UK) in a conical tube. After centrifugation at 400 × g for 30 min, the buffy coat layer was carefully collected. The collected samples were incubated with red blood cell-lysis buffer at room temperature for 10 min. After adding PBS, each sample was centrifuged at 400 × g for 10 min, and the washing and centrifugation steps were repeated. Canine PBMCs (cPBMCs) were resuspended in Roswell Park Memorial Institute (RPMI) medium (Pan-Biotech, Dorset, Germany) supplemented with 10% EV-free FBS and 1% PS. Non-adherent cells were obtained after 24 hours.
Co-culture experiments
DH82 cells, a canine macrophage-like cell line, were purchased from the Korean Cell Line Bank (Seoul, Korea). DH82 cells were seeded in 6-well plates (1×106 cells/well), then incubated for 24 h. After adherence to the plates was confirmed, the DH82 cells were treated with LPS (200 ng/mL; Sigma-Aldrich) or control for 24 h. Similarly, canine lymphocytes were seeded in 6-well plates (1×106 cells/well) and exposed to Con A (5 μg/mL) or control for 24 h. Next, the medium was removed and replaced with media containing EV (100 μg/well) derived from naïve, si RNA and si TSG-6 cASCs. Next, the cells were incubated for 48 h and then harvested for RNA extraction and flow cytometry analysis.
RNA extraction, cDNA synthesis, and reverse transcription-quantitative polymerase chain reaction
RNA was extracted using the Easy-BLUE Total RNA Extraction Kit (Intron Biotechnology). Next, cDNA was synthesized using LaboPass M-MuLV Reverse Transcriptase (Cosmogenetech, Seoul, Korea), according to the manufacturer’s instructions. cDNA samples were assayed using AMPIGENE® qPCR Green Mix Hi-ROX with SYBR Green Dye (Enzo Life Sciences, Farmingdale, NY, USA), according to the manufacturer’s instructions. Expression levels were normalized to those of glyceraldehyde 3-phosphate dehydrogenase (GAPDH). The sequences of the primers used in this experiment are shown in Table 1.
Table 1. Sequences of PCR primers used in this study.
| Gene | Forward (5’-3’) | Reverse (5’-3’) | Reference |
|---|---|---|---|
| cGAPDH | TTAACTCTGGCAAAGTGGATATTGT | GAATCATACTGGAACATGTACACCA | [2] |
| cTNF-α | TCATCTTCTCGAACCCCAAG | ACCCATCTGACGGCACTATC | [2] |
| cIFN-γ | TTCAGCTTTGCGTGATTTG | CTGCAGATCGTTCACAGGAA | [22] |
| cIL-1β | AGTTGCAAGTCTCCCACCAG | TATCCGCATCTGTTTTGCAG | [23] |
| cIL-6 | ATGATCCACTTCAAATAGTCTACC | AGATGTAGGTTATTTTCTGCCAGTG | [2] |
| cIL-10 | ATTTCTGCCCTGTGAGAATAAGAG | TGTAGTTGATGAAGATGTCAAGCTA | [2] |
| cTSG-6 | TCCGTCTTAATAGGAGTGAAAGATG | AGATTTAAAAATTCGCTTTGGATCT | [2] |
| cCD4 | TGCTCCCAGCGGTCACTCCT | GCCCTTGCAGCAGGCGGATA | [24] |
| cCD25 | GGCAGCTTATCCCACGTGCCAG | ATGGGCGGCGTTTGGCTCTG | [24] |
| cFOXP3 | AAACAGCACATTCCCAGAGTTC | AGGATGGCCCAGCGGATCAG | [25] |
| ciNOS | GAGATCAATGTCGCTGTACTCC | TGATGGTCACATTTTGCTTCTG | [23] |
| cCD206 | GGAAATATGTAAACAGGAATGATGC | TCCATCCAAATAAACTTTTTATCCA | [23] |
| mGAPDH | AGTATGTCGTGGAGTCTACTGGTGT | AGTGAGTTGTCATATTTCTCGTGGT | [14] |
| mTNF-α | CCAGGAGAAAGTCAGCCTCCT | TCATACCAGGGCTTGAGCTCA | [14] |
| mIFN-γ | GATGCATTCATGAGTATTGCCAAGT | GTGGACCACTCGGATGAGCTC | [14] |
| mIL-1β | CACCTCTCAAGCAGAGCACAG | GGGTTCCATGGTGAAGTCAA | [14] |
| mIL-6 | TCCAGTTGCCTTCTTGGGAC | GTACTCCAGAAGACCAGAGG | [14] |
| mIL-10 | TGGCCCAGAAATCAAGGAGC | CAGCAGACTCAATACACACT | [14] |
| mCD4 | GAGAGTCAGCGGAGTTCTC | CTCACAGGTCAAAGTATTGTTG | [26] |
| mCD25 | CTCCCATGACAAATCGAGAAAGC | ACTCTGTCCTTCCACGAAATGAT | [26] |
| mFOXP3 | TTGGCCAGCGCCATCTT | TGCCTCCTCCAGAGAGAAGTG | [26] |
| miNOS | AAAGGAAATAGAAACAACAGGAACC | GCATAAAGTATGTGTCTGCAGATGT | [27] |
| mCD206 | AACGGAATGATTGTGTAGTTCTAGC | TACAGGATCAATAATTTTTGGCATT | [28] |
| mArg | CAGAAGAATGGAAGAGTCAG | CAGATATGCAGGGAGTCACC | [29] |
Flow cytometry analysis
To evaluate Treg polarization, PBMC-derived lymphocytes cocultured with cASC-EVs were harvested. Obtained cells (1 × 106) were suspended in 100μL DPBS and 1 μL of each primary antibody against the following proteins: FOXP3-PE (eBioscience, San Diego, CA, USA; 1:100), CD3-FITC (MCA1774F; Bio-Rad, San Diego, CA, USA; 1:100), CD206-FITC (eBioscience, San Diego, CA, USA; 1:100) and CD11c-PE (eBioscience, San Diego, CA, USA; 1:100). After incubation for 1 h at 23 ± 2°C, the cells were washed with DPBS. Unstained cells were used as controls for autofluorescence. Cell fluorescence was analyzed with a flow cytometer (FACS Aria Ⅱ; BD bioscience). The results were analyzed using FlowJo 7.6.5 software (Tree Star, Inc., Ashland, OR, USA).
ELISA analysis
The protein levels of interleukin 10 (IL-10) in each cell culture supernatant was detected using an IL-10 Enzyme-Linked Immunosorbent Assay Kit (ELISA; eBioscience), according to the manufacturer’s instructions.
Mice
To determine the therapeutic effect of ASC-derived EVs on colitis, we induced mouse colitis with DSS (36–50 kDa; MP Biomedical, Solon, OH, USA). Male C57BL/6 mice (6 to 8-week-old and weighing 18 to 20 g) were purchased from Nara Bio (Gyeonggi, Korea) and acclimatized for 7 days with a 12 h light/dark cycle at 22°C and 60% humidity before performing the experiments. For environmental enrichment, 3 to 4 mice were raised in polycarbonate cages (324 × 221.5 × 130 mm) containing clean bedding (shavings; Nara Biotech), cardboard boxes, and tunnels. Mice were fed a standard laboratory rodent diet (Central Lab Animal Inc., Seoul, Korea) and water ad libitum. At the start of the experiments, the health status of the mice was evaluated by measuring their weight, vitality, and defecation; the experiments were conducted on mice with no abnormal symptoms. The mice were administered 3% DSS in their drinking water from days 0 to 7. The studies were conducted using 46 animals, and the mice were randomly divided into 6 groups with 6–8 mice per group (naïve = 6, Sham = 8, PBS = 8, EV = 8, CTL-EV = 8, TSG-6 depleted EV = 8). The mice were treated with 100 μL DPBS, with or without cASC-EV (100 μg/mouse), by intraperitoneal (IP) injection on days 1, 3 and 5. The disease-activity index (DAI) represents the combined score of weight loss relative to the initial body weight (grades 0–4; 0, no weight loss; 1, < 10% loss; 2, 10–20% loss; 3, 20–30% loss; and 4, 30–40% loss), stool consistency (grades 0–2; 0, normal; 1, soft; and 2, liquid), the presence of blood in the feces and anus (grades 0–2; 0, negative fecal occult bleeding; 1; positive fecal occult bleeding; and 3, visible fecal occult bleeding), and general activity (grades 0–2; 0, normal; 1, mildly to moderate depressed and 2, severely depressed). The DAI score of colitis was calculated independently by two blinded investigators. The score for each parameter was summed from day 0 to the day of sacrifice, and the summed score was averaged to yield the final score. Since this model has been verified in several studies, it is unlikely to be accompanied by unexpected pain. However, should three or more of the following abnormal behaviors be observed: behaviorally excessive waist bending, self-cutting, aggressive behavior, stabbing of other mice, injury due to fall, failure to build a nest, abnormally rough hair, abnormal posture, or convulsions, the animal was euthanized within one day and the experiment terminated. On day 10 of the study, the veterinarian euthanized all mice with xylazine infusion and CO2 inhalation according to the approved institutional animal ethics protocol.
Histological evaluation
Colon tissues were fixed in 10% formaldehyde for 48 h, embedded in paraffin, cut into 4-μm sections, and stained with hematoxylin and eosin (H&E). Histological scores are provided in Table 2. Because DSS-related injury varies, two slides from each colon section were assessed per mouse, and at least three areas on each slide were examined.
Table 2. Histological assessment.
| Score | Mucosal thickness & hyperplasia | Inflammatory cell extent | Damaged to the crypt |
|---|---|---|---|
| 0 | Normal | Normal | An intact crypt |
| 1 | Minimal | 11–25% of mucosa | Loss of the basal 1/3 of crypt |
| 2 | Mild | 26–50% of mucosa | Loss of basal 2/3 of crypt |
| 3 | Moderate | Mucosa and submucosa | Entire loss of crypt |
Immunofluorescence analysis
Colon sections were deparaffinized and rehydrated, and antigen retrieval was carried out in 10 mM citrate buffer. Sections were then washed and blocked with blocking buffer containing 1% bovine serum albumin and 0.1% tween 20 for 30 min. The sections were then incubated overnight at 4ଌ with mouse monoclonal anti-Forkhead box (Fox) P3 (1:100; Santa Cruz Biotechnology) and mouse monoclonal anti CD206 (1:100; Santa Cruz Biotechnology). The colon sections were washed three times with DPBS. Then, the sections were incubated FITC conjugated anti mouse (1:500; Santa Cruz) for 1 hr. After that, they were washed three times with DPBS. All samples were mounted using Vectashield mounting medium containing 4’,6-diamidino-2-phenylindole (DAPI; Vector Laboratories, Burlingame, CA, USA). The samples were observed using an EVOS FL microscope (Life Technologies, Darmstadt, Germany). Immunoreactive cells were counted in 20 random fields per group, and the percentage of CD206+ positive cells and FOXP3+ positive cells was calculated in colon sections from the same mice.
Statistical analysis
GraphPad prism (version 6.01) software (GraphPad, Inc., La Jolla, CA, USA) was used for statistical analysis. the differences between two groups were analyzed using Student’s t-tests and differences between more than two groups were analyzed using one-way analysis of variance (ANOVA) followed by Bonferroni multiple comparison test. The results are presented as the mean value ± standard deviation (SD). Differences with a value of P < 0.05 were considered as statistically significant.
Results
Characterization of cASC-EV
The characterization of stem cells used for these studies are described in detail in S1 Fig. The EVs were separated from stem cell culture media by ultracentrifugation. Schematic overview describing this protocol is presented in Fig 1A. Approximately 100 μg of EVs was produced in the media in which 1 × 106 cells were seeded and grown for 2 days. Electron microscopic analysis demonstrated that the EVs were round-shaped and 50–100 nm in diameter (Fig 1B). Using a particle-size analyzer, the EVs were confirmed to be less than 100 nm in diameter (Fig 1C). In addition, positive markers of EVs such as CD63 and CD9 were identified by western blotting, whereas negative markers of EVs such as Lamin A (a nuclear marker) and beta actin (a cytosolic marker) were present in lower abundance (Fig 1D). Whole-cell lysates were used as a positive control. Our findings suggest that the EVs contained little or no cellular matrix and nuclei, which are intracellular components.
Production of EVs containing less TSG-6 from cASCs
To reduce TSG-6 in EVs, cASCs were transfected with si-TSG-6. No differences were observed in the cell viability and cell differentiation potentials between transfected and untreated stem cells. Furthermore, the size and shape of the EVs secreted from the transfected stem cells did not differ from those of the untreated stem cells, and no difference occurred in the amount of EVs produced (S1 Fig). Further, the TSG-6 mRNA levels in the transfected cASCs were reduced by over 50% (S2 Fig) while the TSG-6 protein levels in the EVs were reduced to less than half of those in the naïve and control siRNA-treated groups (S2 Fig)).
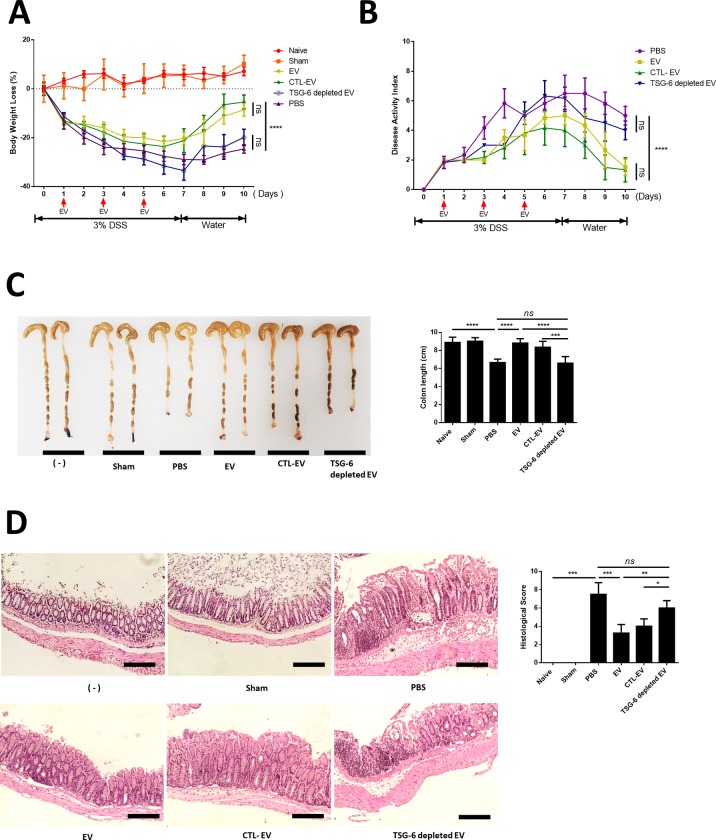
IP administration of cASC-EVs containing TSG-6 played a crucial role in alleviating IBD
In this study, all animals met the euthanasia criteria before being sacrificed. Injecting EV into mice that did not induce colitis (sham group) showed no difference in vitality, weight, and stool consistency from naive mice. In addition, the sham group was not different from the naive group in the colon length and histological examination. In the DSS-administered group, significant weight loss and clinical indices including DAI which is based on body weight (Fig 2A), stool consistency, bloody diarrhea and general activity were found to worsen compared to the healthy group; while the EV group exhibited improved weight and DAI compared to the DSS group (Fig 2B). Moreover, shortening of the colon length significantly improved in the EV group compared with that in the PBS-treated group. However, in TSG-6 depleted EV group was found to have a shorter colon length than the EV and CTL-EV groups (Fig 2C). The EV group showed greatly decreased histological colitis scores for mucosal thickness, mucosal hyperplasia, extent of inflammation, and crypt damage. In addition, the anti-inflammatory effect of CTL-EV was similar to that of naive-EV, whereas the effect of TSG-6-depleted EV was insignificantly decreased. (Fig 2D).
Fig 2. cASC-EV injection ameliorated DSS-induced colitis in mice.
EVs (100 μg), TSG-6 depleted EVs (100 μg), control EVs (100 μg), or vehicle control were injected IP one day after mice were administered 3% DSS. On days 3 and 5, the mice in each group were re-injected with EVs (100 μg), TSG-6 depleted EVs (100 μg), control EVs (100 μg), or vehicle control (PBS). Mice were monitored for changes in (A) body weight, (B) DAIs, and (C) colon lengths. (D) H&E staining of colon sections and histological scores are shown. Scale bars, 100 μm. The results are shown as mean ± standard deviation (n = 6–8 in each group, *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001, as determined by one-way ANOVA)
TSG-6 in cASC-EV modulate pro- and anti- inflammatory cytokine inflamed colon
The colon of EV-treated mice showed reduced levels of inflammatory cytokines (TNF-α, IFN-γ, IL-1β, IL-6 and iNOS) and elevated levels of an anti-inflammatory/regulatory cytokine (IL-10), compared to that of untreated mice with colitis and TSG-6-depleted EV-treated mice (Fig 3).
Fig 3. EVs from cASCs inhibited inflammatory responses in the colon.
mRNA-expression levels of pro- and anti-inflammatory cytokines in the colon were determined by qRT-PCR. These data show that TSG-6 in EVs played a major role in regulating inflammatory cytokine levels in the colon. The results are shown as the mean ± standard deviation (n = 6–8 in each group, *P < 0.05, **P < 0.01, ***P < 0.001, as determined by one-way ANOVA).
TSG-6 was a major factor in increasing Tregs in Con A stimulated lymphocytes in vitro
We found that CD4, CD25 mRNA expression levels increased in the EV group, but decreased in the TSG-6 depleted EV group (Fig 4A). Additionally, the protein levels of IL-10 were measured in the lymphocyte cultured medium. The EV group showed increased IL-10 expression, whereas the TSG-6-depleted EV group showed decreased IL-10 expression (Fig 4B). In addition, to determine whether the increased number of Tregs among total T cells was associated with TSG-6 in the EVs, the degree of Treg activation was confirmed by fluorescence-activated cell sorting. Accordingly, the number of FOXP+ cells among CD3+ cells increased in the EV group. However, in the TSG-6-depleted EV group, the proportion of FOXP+ cells decreased (Figs 4C and S5). These results demonstrate that the immunomodulatory effects of EV were related to TSG-6.
Fig 4. cASC-EV TSG-6 increased Treg proliferation in vitro.
Con A-stimulated canine lymphocytes were cocultured for 48 h with cASC-EVs transfected with TSG-6 siRNA (si-TSG6) or scrambled siRNA (siCTL), or naïve EVs. (A) CD4 and CD25 mRNA-expression levels were measured, confirming that TSG-6 was associated with increased Treg production. (B) IL-10, which is known to be secreted from Tregs, was also measured in the supernatant medium, and the results confirmed that IL-10 production in lymphocytes was associated with TSG-6 (n = 6 in each group). (C) The Treg population was determined by measuring FOXP3 and CD3 double-positive cells by flow cytometry (n = 6 in each group). The results are presented as the mean ± standard deviation (*P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001, as determined by one-way ANOVA).
TSG-6 in EV is a major factor in macrophage polarization from M1 to M2 type in vitro
LPS-stimulated macrophages cocultured with EVs showed reduced levels of TNF-α and increased IL-10 levels, compared to untreated and TSG-6-depleted EV-treated. Moreover, we found that CD206 and Arg mRNA expression levels increased in the EV group but decreased in the TSG-6 depleted EV group (Fig 5A). To determine the effect TSG-6 contained in EV on macrophage polarization, the extent of M1 and M2 were confirmed. Accordingly, the number of CD206+cells increased in the EV group. However, in the TSG-6-depleted EV group, the proportion of CD206+cells decreased (Figs 5B and S5). Contrary, the number of CD11c+cells decreased in the EV group compared to PBS group. However, in the TSG-6-depleted EV group, the proportion of CD11c+cells increased compared to EV group.
Fig 5. cASC-EV TSG-6 induced macrophage polarization from M1 to M2 type in vitro.
LPS-stimulated canine macrophage (DH82) were cocultured for 48 h with cASC-EVs transfected with TSG-6 siRNA (si-TSG6) or scrambled siRNA (siCTL), or naïve EVs. (A) TNF-α, IL-10, CD206 and Arg mRNA-expression levels were measured (C) The M1 and M2 population were determined by measuring CD206 and CD11c positive cells by flow cytometry (n = 6 in each group). The results are presented as the mean ± standard deviation (*P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001, as determined by one-way ANOVA).
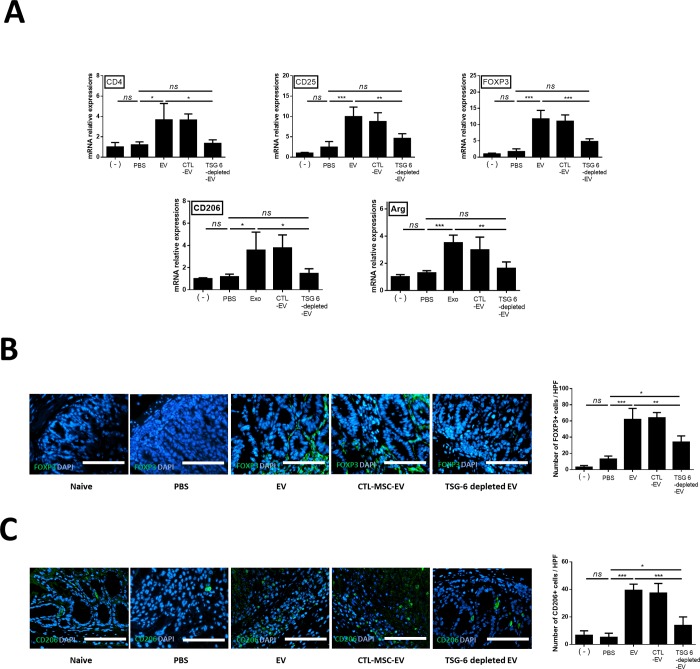
TSG-6 in EV induced phenotypic enhancement of Tregs and M2 macrophage in inflamed colon
The FOXP3, CD4, CD25, CD206 and Arg mRNA levels were evaluated to examine whether stem cell EVs affected the activation of Tregs and polarization of macrophage in the inflamed colon. FOXP3 (6.8 fold), CD4 (3.0 fold), CD25 (4.0 fold), CD206 (3.0 fold) and Arg (2.7 fold) mRNA levels increased in the EV group compared to the PBS group. However, their levels significantly decreased in the TSG-6-depleted EV group compared to the EV and CTL-EV group (Fig 6A). To determine whether the increase in the number of Tregs and M2 was associated with TSG-6 in the EVs, quantitative analysis of FOXP3+ cells and CD206+ cells detected in colon tissue sections by immunofluorescence showed that the percentage of FOXP+ cells (4.76 fold) and (7.61 fold) increased significantly in the cASC-EV group compared to that in the PBS group. However, the enhancement of the number of FOXP3+ cells (0.54 fold) and CD206+ cells (0.35 fold) in the EVs of the colon tissue decreased when TSG-6 was inhibited (Fig 6B).
Fig 6. TSG-6 increases regulatory T cells in the inflamed colon.
TSG-6 in EVs increased the proportion of Tregs in the inflamed colon. (A) Relative gene-expression levels of CD4, CD25, FOXP3, CD206 and Arg in the inflamed colon. (B) FOXP3+ (green) cells (C) CD206+ (gren)cells were detected in colon tissue sections by immunofluorescence. The data shown demonstrated that TSG-6 in EVs played a major role in increasing the number of Tregs and M2 in the colon. Scale bar, 50 μm. The results are shown as the mean ± standard deviation (n = 6–8 in each group, *P < 0.05, ****P < 0.0001, as determined by one-way ANOVA).
Discussion
Our data suggests the following important points: (1) TSG-6 in the stem cell derived EVs is a key factor in immune regulation and relieving inflammation in the DSS-induced mouse model of colitis. (2) TSG-6 in EVs alleviates inflammation by enhancing colonic Tregs and polarizing colonic macrophage from M1 and M2 in an IBD mouse model.
Previous studies have shown that stem cells affect recipient cells in a paracrine manner, considering that EVs largely account for the paracrine effect of stem cells [3, 4, 30]. In our, preliminary study, the immune regulatory capacity of stem cells was significantly decreased when GW4869 (a noncompetitive neutral sphingomyelinase (N-SMase) inhibitor; exosome inhibitor) was applied to cASCs (S3 Fig). Moreover, EVs and stem cells have similar immunomodulatory effects (S4 Fig).
In addition, with this tendency, various studies have been conducted since the introduction of EV as a therapeutic agent [3, 31]. However, the exact mechanism by which they relieve colitis has not been revealed. Therefore, it is noteworthy that this study demonstrated that TSG-6 in EVs is a major factor in relieving colitis symptoms.
Previous studies have shown that immune cells play a role in controlling inflammation in the colon [32]. Among these immune cells, Tregs have been described as having important roles in regulating the pathogenesis of IBD [33, 34] and the balance between Tregs and other T cells in the intestinal tract is known to influence IBD pathogenesis [35]. To a large extent, FOXP3 amplifies and stabilizes the molecular features of Treg precursor cells, which is beneficial for their function and maintenance, and attenuates features that are deleterious to Treg functions [36]. FOXP3-expressing Tregs, which belong to a suppressive subset of CD4+ T cells, can regulate infection, tumor development, allergy, and autoimmunity [37]. It was reported that FOXP3+ Tregs are lower in patients with IBD progression than in healthy controls. It was also reported that an increase in the number of Tregs after treating IBD patients correlated with relief of IBD symptoms [35]. In other words, increasing the number of Tregs may serve as a method for treating IBD.
Colon macrophages are essential for maintaining mucosal homeostasis for the ongoing need for epithelial regeneration but are also an important component of protective immunity and are involved in the pathology of IBD [38]. M1 preferentially metabolize arginine to nitric oxide via inducible nitric oxide synthase (iNOS; NOS2), while M2 preferentially metabolize arginine to ornithine via arginase -1. Therefore, it is known that M1 are involved in pre-inflammatory and M2 are involved in anti-inflammatory [39]. The importance of macrophages in maintaining immune homeostasis has shown that IL-10 secreted from M2 acts on Treg to maintain Foxp3 expression [40]. These Foxp3-expressed Tregs relieved inflammation by suppressing the activity of Th1 and Th17 cells [41]. Therefore, increasing M2 in the colon is noted as a way to alleviate colitis [21]. Accumulated evidence shows that infusion of EVs into colitis models relieves inflammation [42], but the relationship between colonic immune cells and EVs is not clear. Therefore, our study is valuable in that it clarifies the relationship between TSG-6 in EV and colonic immune cells such as Tregs and macrophages.
Although proteins other than TSG-6, such as TGF-beta, IDO and PGE2 may also be contributing to the protective effect of EVs in relieving inflammation [43]. Previous studies have reported that TGF-β plays a role in inhibiting activated immunity by inducing FoxP3+ regulatory t cells in an inflammatory environment and has been shown to play an important role in relieving inflammation in colitis models [44]. Zhang et al. reported that TGF-beta in bone marrow derived stem cells plays a major role in polarizing macrophage from M1 to M2 [45]. IDO expression and activity is an important mediator of intestinal homeostasis both in health and disease [46]. In addition, IDO appears to be the most promising candidate, which plays an important role in the immunomodulatory effects of stem cells by inhibiting T cell activation and enhancing Tregs [47]. Also, IDO has been shown to play a major role in suppressing immunity by polarizing macrophage from M1 to M2.[48]. Furthermore, IDO as an anti-inflammatory agent has been reported to reduce inflammation in colitis models [49]. In addition, in our previous study, we confirmed the efficacy of adipose-derived stem cells in murine-derived macrophage cell lines in inflammatory environments and demonstrated that PGE2 secreted from stem cells is a key factor in polarizing macrophage [50, 51]. Moreover, we previous showed that PGE2 secreted feline ASC is a key factor for enhancing regulatory T cell in inflamed colon [52]
Although further research on the correlation between these immunomodulatory factors of EV and immune cell regulation is needed, results of the current study confirm that TSG-6-depleted EVs significantly reduce the immunoregulatory ability, which clearly indicates that TSG-6 is a major factor in immune regulation and anti-inflammatory action. Furthermore, the finding that TSG-6 in EVs plays an important role in immune regulation will serve as evidence to support increasing the level of TSG-6 in EVs as a strategy to develop EVs with enhanced immunomodulating properties.
Although EV-specific studies have not been conducted, other studies have shown that pretreatment of stem cells with TNF-alpha (TNF-α) resulted in an increase in mRNA levels of TSG-6 in stem cells as well as increased levels of TSG-6 protein in the culture medium [21, 53]. Further studies on pre-treated stem cell-derived EVs are needed.
Nuclear transcription factor kappaB (NF-κB) is a central mediator of pro-inflammatory gene induction and function in immune cells and has a significant effect on mucosal inflammatory process [54]. Moreover, in IBD patients, its activation is markedly induced. Therefore, the NF-κB pathway is considered to be an attractive target of therapeutic intervention in IBD [55]. In our previous study, TSG-6 from stem cells significantly suppressed nuclear factor kappa B (NF-κB) activity and alleviated inflammation and reduced apoptosis in acute pancreatitis model [20]. However, the relationship between EV and NF-kB has not been studied in this study, and it is necessary to confirm whether EV's TSG-6 lowers NF-kB in inflammatory colon.
This study is also an important basis for future transitional studies. Like human IBD, canine idiopathic IBD is a commonly observed chronic IBD that occurs spontaneously with similar multifocal etiology due to the interactions between abnormal host immune responses, and genetic and environmental factors. Histological evaluation of intestinal biopsies reveals extensive or multifocal inflammatory cell infiltration (most commonly lymphoid evolutive, eosinophilic, and neutrophilic), with simultaneous changes in mucosal structures (e.g. villous atrophy and fusion). In severe cases, intestinal protein loss, similar to in human disease, can be observed [1, 56, 57]. This study has been carried out with EVs derived from canine cells and is of great value in facilitating subsequent experiments in dogs. Therefore, evaluating the efficacy of TSG-6 in EVs conducted in this study is valuable for applications in veterinary medicine, particularly for intractable immune-mediated diseases such as IBD, however, much of these finds may also be applicable to human IBD in the future.
Conclusion
We demonstrated that TSG-6 in EVs secreted from cASCs ameliorated DSS-induced colitis in mice by enhancing the Treg population and polarizing macrophage from M1 to M2 in the inflamed colon. Our findings provide an insight to improve the current understanding of the role that EVs have in immunoregulation and serve as a foundation for applying EVs as a therapeutic agent in IBD. Also, this study is the basis of a strategy for developing EVs with improved immunomodulatory properties by increasing TSG-6 levels in EVs.
Supporting information
(A) Immunophenotypes of the cultured cASCs were examined by flow cytometry. The vast majority of cells were positive for CD90, CD44, CD29, and CD73, but a few cells expressed CD34 and CD45. (B) The naïve and si TSG-6 cASCs were maintained in specific differentiation media for 3 weeks, and the differentiated cells were stained by Oil red O to identify adipocytes, Alizarin Red S for osteocytes and Alcian Blue for chondrocytes. Scale bars, 200 μm. (C) Cell-viability assays of naïve and siTSG6-cASCs. si TSG-6 transfection was not cytotoxic when applied to stem cells. (n = 6 in each group) (D) Morphology of EVs from siTSG6-cASCs, as studied by transmission electron microscopy. EV was identified as a circular particle with a diameter of less than 100 nm. (E) EV production by naïve and siTSG6-cASCs. The production of exosome does not differ between naive and siTSG-6 groups. (n = 6 in each group) The results are shown as the mean ± standard deviation (ns, not significant, were analyzed using Student’s t-tests)
(TIF)
(A) TSG-6 mRNA-expression levels in naïve cASCs, cASCs transfected with a scrambled siRNA (CTL-cASC), or cASCs transfected with TSG-6 (siTSG-6-cASC) was determined by agarose gel electrophoresis and RT-qPCR. (Lane 1 and 2: Naïve, Lane 3 and 4: CTL-cASC, Lane 5 and 6: si TSG-6 cASC in gel PCR) (B) TSG-6 protein-expression levels in naïve cASC-EVs, EVs from cASCs transfected with a scrambled siRNA (CTL-EV), or EVs from cASCs transfected with TSG-6 (TSG-6 depleted-EV) were determined by western blot analysis. The results are presented as the mean ± standard deviation. (n = 6 in each group) (ns = Not Statistically Significant *P < 0.05, **P < 0.01, ***P < 0.001 by one-way ANOVA analysis).
(TIF)
(A) Treatment with 0.005% DMSO, 10 μM, 20 μM GW4869, or 1% DMSO showed no cytotoxic effects on cASCs, as shown by similar viability rates following all treatments, compared to the non-treated group (n = 6 in each group) (B) Pre-treatment with GW4869(10 μM, for 12h) significantly reduced production of EV proteins by cASCs. EV production was reduced by more than 70% in the GW4869-treated group (n = 6 in each group ) (* p< 0.05, were analyzed using Student’s t-tests)(C) The mRNA levels of TNA-α, IL-1β, IL-6, IFN-γ, and IL-10 were detected by qRT-PCR. Con A-treated lymphocytes showed significantly increased levels of pro-inflammatory cytokines, such as TNF-α, IFN-γ, IL-1β, and IL-6, compared to the untreated group. cASCs depressed activated lymphocyte. however, pre-treatment with GW4869 significantly reduced the modulatory effects of cASCs. (n = 6 in each group)The results are presented as the mean ± standard deviation (**P < 0.01, ***P < 0.001, ****P < 0.0001 as determined by one-way ANOVA).
(TIF)
(A) Changes in the expression levels of mRNAs encoding several canine lymphocyte-derived cytokines including TNF-α, IL-1β, IFN-γ, IL-6, and IL-10 in the presence of cASC-Evs (100ug/well). After Con A-stimulated lymphocytes were cocultured with EV (100 ug), the levels of activated pro-inflammatory cytokines (TNF-α, IFN-γ, IL-1β, and IL-6) decreased significantly. Production of the anti-inflammatory cytokine IL-10 significantly increased, compared to that in the untreated group. (B) Changes in the expression levels of mRNAs encoding several canine macrohage-derived cytokines including TNF-α, IL-6, iNOS and IL-10 in the presence of cASC-Evs (100ug/well). After LPS-stimulated DH82 were cocultured with EV (100 ug), the levels of activated pro-inflammatory cytokines (TNF-α, IL-6 and iNOS) decreased significantly. Production of the anti-inflammatory cytokine IL-10 significantly increased, compared to that in the untreated group. The data show that EVs exerted immunosuppressive effects as much as stem cells. The results are presented as the mean ± standard deviation (n = 6 in each group), **P < 0.01, ***P < 0.001, ****P < 0.0001, as determined by one-way ANOVA).
(TIF)
TSG-6 in EV plays an important role in the increase of regulatory t cells and macrophage polarization. (A) Tregs (FOXP3+CD3+ cells) level in canine lymphocytes (B) M1 (CD11+cells) and M2 macrophages (CD206+ cells) level in canine macrophage cell line (DH82). FACS plots (right panel) show representative examples and bar graphs (left panel) represent mean values +SD (ns = Not Statistically Significant *P < 0.05, **P < 0.01, ***P < 0.001 by one-way ANOVA analysis)
(TIF)
The original underlying images of CD63, CD9, Lamin A and β-actin in Fig 1D.
(TIF)
(DOCX)
Abbreviations
- ANOVA
Analysis of variance
- BCA
Bicinchoninic acid
- cASC
Canine adipose tissue-derived mesenchymal stem/stromal cell
- CD
Cluster of differentiation
- Con A
Concanavalin A
- CTL
Control
- cPBMC
Canine peripheral blood mononuclear cell
- DAI
Disease-activity index
- DMEM
Dulbecco's modified Eagle's medium
- DMSO
Dimethyl sulfoxide
- DPBS
Dulbecco’s phosphate-buffered saline
- DSS
Dextran sulfate sodium
- ELISA
Enzyme-linked immunosorbent assay
- EV
Extracellular vesicle
- FBS
Fetal bovine serum
- FITC
Fluorescein isothiocyanate
- FOXP3
Forkhead box P3
- GAPDH
Glyceraldehyde 3-phosphate dehydrogenase
- H&E
Hematoxylin and eosin
- IBD
Inflammatory bowel disease
- IFN
Interferon
- IL
Interleukin
- IP
Intraperitoneal
- LPS
Lipopolysaccharides
- M1
Macrophage M1 type
- M2
Macrophage M2 type
- NO
Nitric oxide
- PBMC
Peripheral blood mononuclear cell
- PBS
Phosphate-buffered saline
- PE
Phycoerythrin
- RBC
Red blood cell
- RT-qPCR
Reverse transcription quantitative polymerase chain reaction
- siRNA
Small-interfering RNA
- siTSG-6
Small-interfering TSG-6
- TEM
Transmission Electron Microscope
- TGF-β
Transforming growth factor-β
- TNF-α
Tumor necrosis factor-α
- Treg
Regulatory T cell
- TSG-6
Tumor necrosis factor-α-stimulated gene/protein-6
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This study received support from the Research Institute for Veterinary Science, Seoul National University and Basic Science Research Program of the National Research Foundation of Korea. Author YCJ receives support in the form of salary from the commercial company the Chaon Corporation. The funders did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of YCJ are articulated in the ‘author contributions’ section.
References
- 1.Cerquetella M, Spaterna A, Laus F, Tesei B, Rossi G, Antonelli E, et al. Inflammatory bowel disease in the dog: differences and similarities with humans. World journal of gastroenterology: WJG. 2010;16(9):1050 10.3748/wjg.v16.i9.1050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yi Z, Stunz LL, Bishop GA. CD40-mediated maintenance of immune homeostasis in the adipose tissue microenvironment. Diabetes. 2014:DB_131657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katsuda T, Kosaka N, Takeshita F, Ochiya T. The therapeutic potential of mesenchymal stem cell‐derived extracellular vesicles. Proteomics. 2013;13(10–11):1637–53. 10.1002/pmic.201200373 [DOI] [PubMed] [Google Scholar]
- 4.Burrello J, Monticone S, Gai C, Gomez Y, Kholia S, Camussi G. Stem cell-derived extracellular vesicles and immune-modulation. Frontiers in cell and developmental biology. 2016;4:83 10.3389/fcell.2016.00083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hartjes TA, Mytnyk S, Jenster GW, van Steijn V, van Royen ME. Extracellular Vesicle Quantification and Characterization: Common Methods and Emerging Approaches. Bioengineering. 2019;6(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qian X, Xu C, Fang S, Zhao P, Wang Y, Liu H, et al. Exosomal microRNAs derived from umbilical mesenchymal stem cells inhibit hepatitis C virus infection. Stem Cells Translational Medicine. 2016;5(9):1190–203. 10.5966/sctm.2015-0348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bai L, Shao H, Wang H, Zhang Z, Su C, Dong L, et al. Effects of mesenchymal stem cell-derived exosomes on experimental autoimmune uveitis. Scientific reports. 2017;7(1):4323 10.1038/s41598-017-04559-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bruno S, Grange C, Collino F, Deregibus MC, Cantaluppi V, Biancone L, et al. Microvesicles derived from mesenchymal stem cells enhance survival in a lethal model of acute kidney injury. PloS one. 2012;7(3):e33115 10.1371/journal.pone.0033115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mao F, Wu Y, Tang X, Kang J, Zhang B, Yan Y, et al. Exosomes derived from human umbilical cord mesenchymal stem cells relieve inflammatory bowel disease in mice. BioMed research international. 2017;2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee RH, Yu JM, Foskett AM, Peltier G, Reneau JC, Bazhanov N, et al. TSG-6 as a biomarker to predict efficacy of human mesenchymal stem/progenitor cells (hMSCs) in modulating sterile inflammation in vivo. Proceedings of the National Academy of Sciences. 2014;111(47):16766–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Song W-J, Li Q, Ryu M-O, Ahn J-O, Bhang DH, Jung YC, et al. TSG-6 secreted by human adipose tissue-derived mesenchymal stem cells ameliorates DSS-induced colitis by inducing M2 macrophage polarization in mice. Scientific Reports. 2017;7(1):5187 10.1038/s41598-017-04766-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang N, Li Q, Zhang L, Lin H, Hu J, Li D, et al. Mesenchymal stem cells attenuate peritoneal injury through secretion of TSG-6. PloS one. 2012;7(8):e43768 10.1371/journal.pone.0043768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Milner CM, Day AJ. TSG-6: a multifunctional protein associated with inflammation. Journal of cell science. 2003;116(10):1863–73. [DOI] [PubMed] [Google Scholar]
- 14.Arseneau KO, Tamagawa H, Pizarro TT, Cominelli F. Innate and adaptive immune responses related to IBD pathogenesis. Current gastroenterology reports. 2007;9(6):508–12. 10.1007/s11894-007-0067-3 [DOI] [PubMed] [Google Scholar]
- 15.Sartor RB. Pathogenesis and immune mechanisms of chronic inflammatory bowel diseases. American Journal of Gastroenterology. 1997;92. [PubMed] [Google Scholar]
- 16.Banz A, Peixoto A, Pontoux C, Cordier C, Rocha B, Papiernik M. A unique subpopulation of CD4+ regulatory T cells controls wasting disease, IL‐10 secretion and T cell homeostasis. European journal of immunology. 2003;33(9):2419–28. 10.1002/eji.200324205 [DOI] [PubMed] [Google Scholar]
- 17.Mowat AM, Bain CC. Mucosal macrophages in intestinal homeostasis and inflammation. Journal of innate immunity. 2011;3(6):550–64. 10.1159/000329099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Atri C, Guerfali FZ, Laouini D. Role of human macrophage polarization in inflammation during infectious diseases. International journal of molecular sciences. 2018;19(6):1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu H, Liang Z, Wang F, Zhou C, Zheng X, Hu T, et al. Exosomes from Mesenchymal Stromal Cells Reduce Murine Colonic Inflammation via a Macrophage-Dependent Mechanism. Available at SSRN 3408050. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li Q, Song W-J, Ryu M-O, Nam A, An J-H, Ahn J-O, et al. TSG-6 secreted by human adipose tissue-derived mesenchymal stem cells ameliorates severe acute pancreatitis via ER stress downregulation in mice. Stem cell research & therapy. 2018;9(1):255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Song W-J, Li Q, Ryu M-O, Ahn J-O, Bhang DH, Jung YC, et al. TSG-6 released from intraperitoneally injected canine adipose tissue-derived mesenchymal stem cells ameliorate inflammatory bowel disease by inducing M2 macrophage switch in mice. Stem cell research & therapy. 2018;9(1):91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schmitz S, Garden OA, Werling D, Allenspach K. Gene expression of selected signature cytokines of T cell subsets in duodenal tissues of dogs with and without inflammatory bowel disease. Veterinary immunology and immunopathology. 2012;146(1):87–91. 10.1016/j.vetimm.2012.01.013 [DOI] [PubMed] [Google Scholar]
- 23.Manning K, Rachakonda PS, Rai MF, Schmidt MF. Co-expression of insulin-like growth factor-1 and interleukin-4 in an in vitro inflammatory model. Cytokine. 2010;50(3):297–305. 10.1016/j.cyto.2010.01.010 [DOI] [PubMed] [Google Scholar]
- 24.Lee K, Cha S-H, Kang H, Song J-Y, Lee K, Ko K, et al. Effects of serial passage on the characteristics and chondrogenic differentiation of canine umbilical cord matrix derived mesenchymal stem cells. Asian-Australasian journal of animal sciences. 2013;26(4):588 10.5713/ajas.2012.12488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Biller B, Elmslie R, Burnett R, Avery A, Dow S. Use of FoxP3 expression to identify regulatory T cells in healthy dogs and dogs with cancer. Veterinary immunology and immunopathology. 2007;116(1–2):69–78. 10.1016/j.vetimm.2006.12.002 [DOI] [PubMed] [Google Scholar]
- 26.Jo H, Eom YW, Kim H-S, Park HJ, Kim HM, Cho M-Y. Regulatory dendritic cells induced by mesenchymal stem cells ameliorate dextran sodium sulfate-induced chronic colitis in mice. Gut and liver. 2018;12(6):664 10.5009/gnl18072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maloney J, Keselman A, Li E, Singer SM. Macrophages expressing arginase 1 and nitric oxide synthase 2 accumulate in the small intestine during Giardia lamblia infection. Microbes and infection. 2015;17(6):462–7. 10.1016/j.micinf.2015.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bruno S, Deregibus MC, Camussi G. The secretome of mesenchymal stromal cells: role of extracellular vesicles in immunomodulation. Immunology letters. 2015;168(2):154–8. 10.1016/j.imlet.2015.06.007 [DOI] [PubMed] [Google Scholar]
- 29.Monk JM, Richard CL, Woodward B. A non-inflammatory form of immune competence prevails in acute pre-pubescent malnutrition: new evidence based on critical mRNA transcripts in the mouse. British Journal of Nutrition. 2012;107(9):1249–53. 10.1017/S0007114511004399 [DOI] [PubMed] [Google Scholar]
- 30.Biancone L, Bruno S, Deregibus MC, Tetta C, Camussi G. Therapeutic potential of mesenchymal stem cell-derived microvesicles. Nephrology Dialysis Transplantation. 2012;27(8):3037–42. [DOI] [PubMed] [Google Scholar]
- 31.Zhang B, Yin Y, Lai RC, Tan SS, Choo ABH, Lim SK. Mesenchymal stem cells secrete immunologically active exosomes. Stem cells and development. 2013;23(11):1233–44. [DOI] [PubMed] [Google Scholar]
- 32.Cook MD, Allen JM, Pence BD, Wallig MA, Gaskins HR, White BA, et al. Exercise and gut immune function: evidence of alterations in colon immune cell homeostasis and microbiome characteristics with exercise training. Immunology and cell biology. 2016;94(2):158–63. 10.1038/icb.2015.108 [DOI] [PubMed] [Google Scholar]
- 33.Asseman C, Mauze S, Leach MW, Coffman RL, Powrie F. An essential role for interleukin 10 in the function of regulatory T cells that inhibit intestinal inflammation. Journal of Experimental Medicine. 1999;190(7):995–1004. 10.1084/jem.190.7.995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Round JL, Mazmanian SK. Inducible Foxp3+ regulatory T-cell development by a commensal bacterium of the intestinal microbiota. Proceedings of the National Academy of Sciences. 2010;107(27):12204–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yamada A, Arakaki R, Saito M, Tsunematsu T, Kudo Y, Ishimaru N. Role of regulatory T cell in the pathogenesis of inflammatory bowel disease. World Journal of Gastroenterology. 2016;22(7):2195 10.3748/wjg.v22.i7.2195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tang Q, Bluestone JA. The Foxp3+ regulatory T cell: a jack of all trades, master of regulation. Nature immunology. 2008;9(3):239 10.1038/ni1572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sakaguchi S, Ono M, Setoguchi R, Yagi H, Hori S, Fehervari Z, et al. Foxp3+ CD25+ CD4+ natural regulatory T cells in dominant self‐tolerance and autoimmune disease. Immunological reviews. 2006;212(1):8–27. [DOI] [PubMed] [Google Scholar]
- 38.Bain CC, Mowat AM. Macrophages in intestinal homeostasis and inflammation. Immunological reviews. 2014;260(1):102–17. 10.1111/imr.12192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Isidro RA, Appleyard CB. Colonic macrophage polarization in homeostasis, inflammation, and cancer. American Journal of Physiology-Gastrointestinal and Liver Physiology. 2016;311(1):G59–G73. 10.1152/ajpgi.00123.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Murai M, Turovskaya O, Kim G, Madan R, Karp CL, Cheroutre H, et al. Interleukin 10 acts on regulatory T cells to maintain expression of the transcription factor Foxp3 and suppressive function in mice with colitis. Nature immunology. 2009;10(11):1178 10.1038/ni.1791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xavier R, Podolsky D. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007;448(7152):427 10.1038/nature06005 [DOI] [PubMed] [Google Scholar]
- 42.Wu Y, Qiu W, Xu X, Kang J, Wang J, Wen Y, et al. Exosomes derived from human umbilical cord mesenchymal stem cells alleviate inflammatory bowel disease in mice through ubiquitination. American journal of translational research. 2018;10(7):2026 [PMC free article] [PubMed] [Google Scholar]
- 43.Soleymaninejadian E, Pramanik K, Samadian E. Immunomodulatory properties of mesenchymal stem cells: cytokines and factors. American journal of reproductive immunology. 2012;67(1):1–8. 10.1111/j.1600-0897.2011.01069.x [DOI] [PubMed] [Google Scholar]
- 44.Becker C, Fantini MC, Neurath MF. TGF-beta as a T cell regulator in colitis and colon cancer. Cytokine & growth factor reviews. 2006;17(1–2):97–106. [DOI] [PubMed] [Google Scholar]
- 45.Zhang F, Wang H, Wang X, Jiang G, Liu H, Zhang G, et al. TGF-β induces M2-like macrophage polarization via SNAIL-mediated suppression of a pro-inflammatory phenotype. Oncotarget. 2016;7(32):52294 10.18632/oncotarget.10561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ciorba MA. Indoleamine 2, 3 dioxygenase (IDO) in intestinal disease. Current opinion in gastroenterology. 2013;29(2):146 10.1097/MOG.0b013e32835c9cb3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yan Y, Zhang G-X, Gran B, Fallarino F, Yu S, Li H, et al. IDO upregulates regulatory T cells via tryptophan catabolite and suppresses encephalitogenic T cell responses in experimental autoimmune encephalomyelitis. The Journal of Immunology. 2010;185(10):5953–61. 10.4049/jimmunol.1001628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang X-F, Wang H-S, Wang H, Zhang F, Wang K-F, Guo Q, et al. The role of indoleamine 2, 3-dioxygenase (IDO) in immune tolerance: focus on macrophage polarization of THP-1 cells. Cellular immunology. 2014;289(1–2):42–8. 10.1016/j.cellimm.2014.02.005 [DOI] [PubMed] [Google Scholar]
- 49.Coquerelle C, Oldenhove G, Acolty V, Denoeud J, Vansanten G, Verdebout J-M, et al. Anti-CTLA-4 treatment induces IL-10-producing ICOS+ regulatory T cells displaying IDO-dependent anti-inflammatory properties in a mouse model of colitis. Gut. 2009;58(10):1363–73. 10.1136/gut.2008.162842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yang H-M, Song W-J, Li Q, Kim S-Y, Kim H-J, Ryu M-O, et al. Canine mesenchymal stem cells treated with TNF-α and IFN-γ enhance anti-inflammatory effects through the COX-2/PGE2 pathway. Research in veterinary science. 2018;119:19–26. 10.1016/j.rvsc.2018.05.011 [DOI] [PubMed] [Google Scholar]
- 51.Chae H-K, Song W-J, Ahn J-O, Li Q, Lee B-Y, Kweon K, et al. Immunomodulatory effects of soluble factors secreted by feline adipose tissue-derived mesenchymal stem cells. Veterinary immunology and immunopathology. 2017;191:22–9. 10.1016/j.vetimm.2017.07.013 [DOI] [PubMed] [Google Scholar]
- 52.AN J-H, Woo-Jin S, Qiang L, Sang-Min K, Ji-In Y, Min-Ok R, et al. Prostaglandin E 2 secreted from feline adipose tissue-derived mesenchymal stem cells alleviate DSS-induced colitis by increasing regulatory T cells in mice. BMC veterinary research. 2018;14(1):354 10.1186/s12917-018-1684-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Xiao Q, Wang S-k, Tian H, Xin L, Zou Z-g, Hu Y-l, et al. TNF-α increases bone marrow mesenchymal stem cell migration to ischemic tissues. Cell biochemistry and biophysics. 2012;62(3):409–14. 10.1007/s12013-011-9317-y [DOI] [PubMed] [Google Scholar]
- 54.Liu T, Zhang L, Joo D, Sun S-C. NF-κB signaling in inflammation. Signal transduction and targeted therapy. 2017;2:17023 10.1038/sigtrans.2017.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Atreya I, Atreya R, Neurath M. NF‐κB in inflammatory bowel disease. Journal of internal medicine. 2008;263(6):591–6. 10.1111/j.1365-2796.2008.01953.x [DOI] [PubMed] [Google Scholar]
- 56.Coelho LP, Kultima JR, Costea PI, Fournier C, Pan Y, Czarnecki-Maulden G, et al. Similarity of the dog and human gut microbiomes in gene content and response to diet. Microbiome. 2018;6(1):72 10.1186/s40168-018-0450-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vázquez-Baeza Y, Hyde ER, Suchodolski JS, Knight R. Dog and human inflammatory bowel disease rely on overlapping yet distinct dysbiosis networks. Nature microbiology. 2016;1(12):16177. [DOI] [PubMed] [Google Scholar]