Abstract
Optic nerve hypoplasia (ONH) is a congenital malformation with a reduced number of retinal ganglion cell axons in a thin optic nerve. It is a common cause of visual impairment in children and ONH is associated with neurodevelopmental disorders, pituitary hormone deficiencies, and brain malformations. In most cases, the aetiology is unknown, but both environmental factors and genetic causes have been described. This study aimed to identify genetic variants underlying ONH in a well-characterised cohort of individuals with ONH. We performed array comparative genomic hybridization and whole genome sequencing in 29 individuals with ONH. Rare variants were verified by Sanger sequencing and inheritance was assessed in parental samples. We identified 11 rare single nucleotide variants (SNVs) in ten individuals, including a homozygous variant in KIF7 (previously associated with Joubert syndrome), a heterozygous de novo variant in COL4A1 (previously described in an individual with porencephaly), and a homozygous variant in COL4A2. In addition, one individual harboured a heterozygous variant in OPA1 and a heterozygous variant in COL4A1, both were inherited and assessed as variants of unknown clinical significance. Finally, a heterozygous deletion of 341 kb involving exons 7–18 of SOX5 (associated with Lamb-Schaffer syndrome) was identified in one individual. The overall diagnostic yield of pathogenic or likely pathogenic variants in individuals with ONH using whole genome sequencing was 4/29 (14%). Our results show that there is a genetic heterogeneity in ONH and indicate that genetic causes of ONH are not rare. We conclude that genetic testing is valuable in a substantial proportion of the individuals with ONH, especially in cases with non-isolated ONH.
Introduction
Optic nerve hypoplasia (ONH) (MIM 165550) is a congenital ocular malformation with a thin optic nerve due to a reduced number of retinal ganglion cell axons. It is the most common optic nerve malformation [1,2] and one of the most common causes of visual impairment and blindness in children in developed countries [3]. It can be unilateral or bilateral and results in a visual outcome ranging from near normal to blindness. In children with severe bilateral ONH, the most common presenting symptoms are lack of fixation, poor visual behaviour, roving eye movements, nystagmus, and strabismus [1]. ONH is diagnosed by examining the optic disc by ophthalmoscopy or in fundus photographs. The prevalence has been reported to be 10.9/100 000 in Northwest England [4] and 17.3/100 000 in Stockholm, Sweden [1]. Individuals with ONH often have coexisting pituitary hormone deficiencies, intellectual disability, autism, and other brain malformations [3,5,6].
The aetiology of ONH is unknown in the majority of cases. Predominant maternal factors are young maternal age and primiparity, and environmental factors have been suspected [7]. Congenital infections have been associated with ONH, as has prenatal ethanol exposure as a part of the fetal alcohol syndrome [3]. Furthermore, destructive brain lesions have been suggested to cause ONH and associated brain malformations [8]. Although most cases of ONH are sporadic, there are also familial cases suggesting a genetic aetiology [9,10]. HESX1 was the first gene to be associated with ONH [10], but only few cases have been reported [11,12]. Due to the increasing rate of genetic testing of affected individuals, several developmental genes have been proposed as candidate genes for ONH [12,13].
We used custom-designed array comparative genomic hybridization (array-CGH) and whole genome sequencing (WGS) to perform a genome wide screen for large copy number variants (CNVs) as well as a targeted analysis of small CNVs, single nucleotide variants (SNVs), and indels in a population-based cohort of individuals with ONH in Stockholm, Sweden.
Materials and methods
Study population and participant demographics
In Stockholm, a population-based, cross-sectional cohort of children and young adults with ONH has been identified and phenotyped [1,5,6]. The diagnosis of ONH was confirmed when there was a small optic disc in combination with visual deprivation and/or a visual field defect [1]. In the present study cohort of 29 individuals, 18 individuals had bilateral ONH and 11 individuals had unilateral ONH. Fifteen were males and 14 females, and the median age at the time of the genetic analyses was 16.7 years (range 7.6–27 years). Six individuals (21%) were blind with a best-corrected decimal visual acuity (BCVA) of less than 0.05, classified according to the World Health Organization (WHO). Ten individuals (34%) had an intellectual disability and another four individuals had an autism spectrum disorder. Pituitary hormone deficiencies were diagnosed in nine individuals. Isolated ONH, without any combination with neurodevelopmental disorder, other congenital malformation, or pituitary hormone deficiency, was found in nine individuals (31%).
Genomic DNA derived from whole blood from the 29 individuals was collected according to standard protocols for genetic analyses. Written, informed consent for participation and publication of the results was obtained from the parents and from adolescents older than 15 years of age and the regional ethics committee in Stockholm (Regionala etikprövningsnämnden i Stockholm) granted approval of the study. The study was performed according to the Declaration of Helsinki.
Array comparative genomic hybridization
A high-density custom array-CGH design was created using Agilents online web tool for array design, eArray. The used design was Agilent 2x400K HD-CGH microarray, consisting of approximately 400 000 oligonucleotide probes. Design and laboratory protocol for the array have previously been published [14]. Detection limits (log2 ratio) for duplications were set to 0.3 and for deletions 0.6. All aberrations called by Cytosure Interpret Software were manually inspected and classified according to the American College of Medical Genetics guidelines [15].
Whole genome sequencing and variant validation
WGS was performed on 2.2 μg genomic DNA, extracted from whole blood according to standard protocols, at National Genomics Infrastructure (NGI) Stockholm using the Illumina XTen platform. The samples were prepared using a paired end (PE) PCR-free library prep, resulting in an average read depth of 30X and a mean insert size of 350 base pairs. Sequencing data was processed using the NGI-piper pipeline (https://github.com/johandahlberg/piper). Structural variants (balanced and unbalanced) were analysed using the FindSV pipeline (https://github.com/J35P312/FindSV), combining CNVnator [16] and TIDDIT [17]. Variant calling was performed using Bcftools [18] and freebayes [19], the resulting vcf files were merged using GATK combine variants and annotated using VEP [20]. Further, SNVs and indels were filtered with a maximum frequency of 0.01 in several normal variant databases including ExAC [21], the 1000 Genomes Project (1000G) [22], and the Swedish population frequency database (SweFreq) [23]. The variants were scored using SIFT (Sorting Intolerant From Tolerant) [24] and PolyPhen [25], the two most commonly used prediction tools for interpretation of genomic variation. Both algorithms predict whether a SNV has an effect on the protein structure based on sequence conservation and the physical properties of amino acids. The PolyPhen score ranges from 0.0 (tolerated) to 1.0 (deleterious), while the SIFT score ranges the opposite, from 0.0 (deleterious) to 1.0 (tolerated). The two models were interpreted together and deleterious predictions set to moderate or high were kept. Finally, the variants were manually filtered based on their quality through inspection using IGV [26] and previous literature. The remaining candidate variants were confirmed with Sanger sequencing and parental samples were analysed to determine the mode of inheritance. Only variants in genes previously implicated in human disease and with a CADD (combined annotation-dependent depletion) score [27] over 20 are presented and were classified according to the American College of Medical Genetics and Genomic guidelines [28].
The variants (CNVs and SNVs) were submitted to ClinVar database (https://www.ncbi.nlm.nih.gov/clinvar/) with accession numbers: SCV000681429, SCV000887490, SCV000681422, SCV000681432, SCV000681428, SCV000681434, SCV000681433, SCV000681423, SCV000681425, SCV000681430, SCV000681431, SCV000681427, and were named according to the following NCBI GenBank reference transcript accession numbers: SOX5, NM_152989.4; KIF7, NM_198525.2; COL4A1, NM_001845.5; COL4A2, NM_001846.3; OPA1, NM_015560.2; SPG7, NM_003119.3; CYP26A1, NM_057157.2; CYP26C1, NM_183374.2; UBE3B, NM_130466.3.
Statistical analysis
Descriptive statistics were performed using STATISTICA 13 (StatSoft Inc, Tulsa, Oklahoma, USA).
Results
Identification of one rare CNV in SOX5 in one case with ONH
In the cohort of 29 individuals with ONH, array-CGH analysis identified one rare CNV (Case 18, Table 1, Fig 1). The CNV was a heterozygous deletion of 341 kb at 12p12.1 (chr12:23432684–23773692, GRCh37/Hg19) involving exons 7–18 of SOX5 (MIM 604975). SOX5 encodes a transcription factor that is important for neurogenesis [29]. Interestingly, both mutations and similar deletions of SOX5 have previously been described in Lamb-Schaffer syndrome (MIM 616803), an autosomal dominant syndrome with varying phenotypes including ONH, optic atrophy (MIM 165500), developmental delay, behavioural problems, poor expressive speech, mild dysmorphic features, and skeletal abnormalities [30,31]. The affected individual (Case 18) has bilateral ONH, moderate visual impairment, intellectual disability, autistic traits, and a small ventricular septal defect suggestive of Lamb-Schaffer syndrome (Fig 2). DNA was only available from the father and he did not carry the deletion. Subsequently, the SOX5 deletion was assessed as pathogenic.
Table 1. Clinical phenotypes and identified candidate variants in 11 optic nerve hypoplasia cases.
| Case | Sex | Age* (y) | Gene | Inheritance | ONH | Neuro | Hormone deficiency | Other malformations |
|---|---|---|---|---|---|---|---|---|
| 2 | M | 24 | SPG7 | Maternal | Bilat Blind | ID,CP,EP | - | Microcephaly, WMA, facial asymmetry |
| 5 | M | 13 | CYP26A1 | Maternal | Bilat | - | MPHD | Pituitary abnormality |
| 11 | M | 10 | COL4A1 | De novo | Bilat Blind | ID,CP,EP | - | CC hypoplasia, CD, calcification, WMA, microcephaly |
| 14 | M | 14 | UBE3B | Maternal | Bilat | - | - | Unilat syndactyly toes |
| 17 | M | 18 | COL4A2 | Maternal, paternal | Bilat | ASD, hyposmia | MPHD | Pituitary and jaw abnormalities |
| 18 | F | 11 | Het del SOX5 exon 7–18 | Not paternal | Bilat | ID, autistic traits | - | VSD |
| 19 | M | 18 | CYP26C1 | Ni | Unilat | - | - | - |
| 20 | M | 11 | CYP26C1 | Paternal | Unilat | - | - | - |
| 21 | F | 14 | COL4A1 OPA1 | Paternal, paternal | Unilat | - | Precocious puberty | - |
| 27 | F | 16 | COL4A2 | Maternal | Unilat | ID | - | Hypertelorism |
| 29 | F | 23 | KIF7 | Maternal, paternal | Bilat | ID | - | CC agenesis, SP agenesis, MTS, colpocephaly, arachnoid cyst, macrocephaly, hypertelorism, ovarian cysts, liver and uterus abnormalities, bowel malrotation, unilat syndactyly toes |
*Age at the time of the genetic analyses. ONH, optic nerve hypoplasia; Neuro, neurological dysfunction; Bilat, bilateral; ID, intellectual disability; CP, cerebral palsy; EP, epilepsy; WMA, white matter abnormalities; MPHD, multiple pituitary hormone deficiency; CC, corpus callosum; CD, cortical destruction; Unilat, unilateral; ASD, autism spectrum disorder; Het del, heterozygous deletion; VSD, ventricular septal defect; Ni, no information; SP, septum pellucidum; MTS, molar tooth sign.
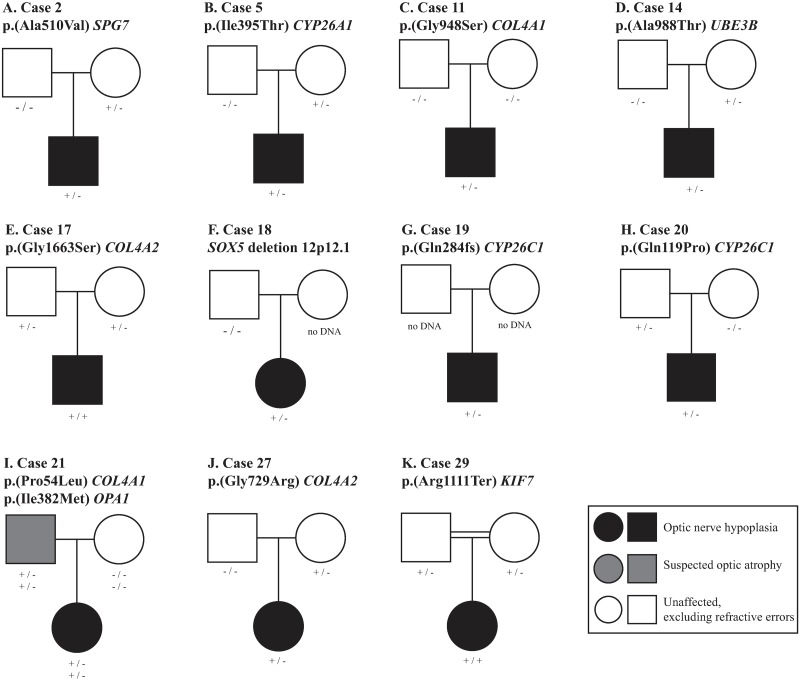
Fig 1. Segregation analyses in 10 of 11 families with rare genomic variants.
DNA samples from 19 parents were available for segregation analysis and revealed that eight SNVs in eight individuals were inherited. The SNV in Case 11 was de novo. The CNV identified in Case 18 had only one parental sample available and the inheritance could not be established. A diagnosis of optic nerve hypoplasia is indicated in black, suspected optic atrophy is indicated in grey, and no ophthalmological disorder, excluding refractive errors, is indicated in white.
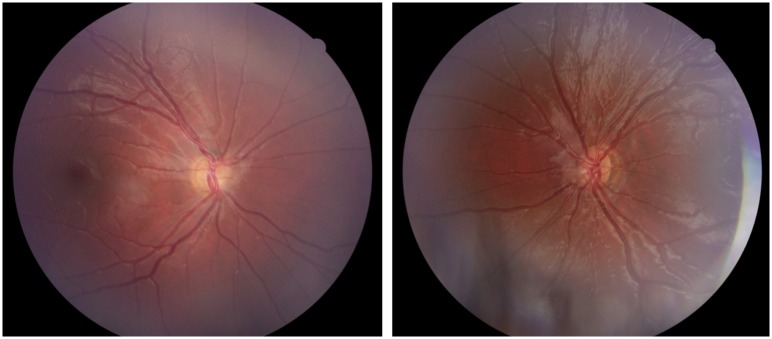
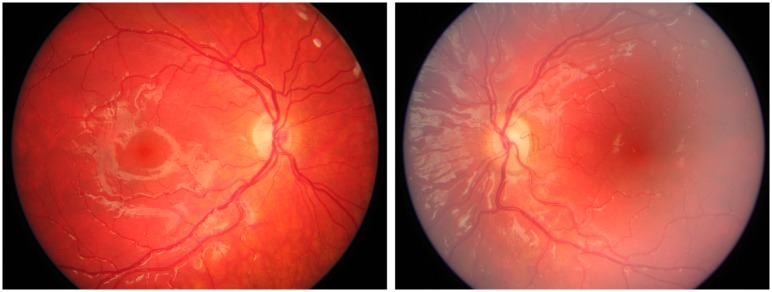
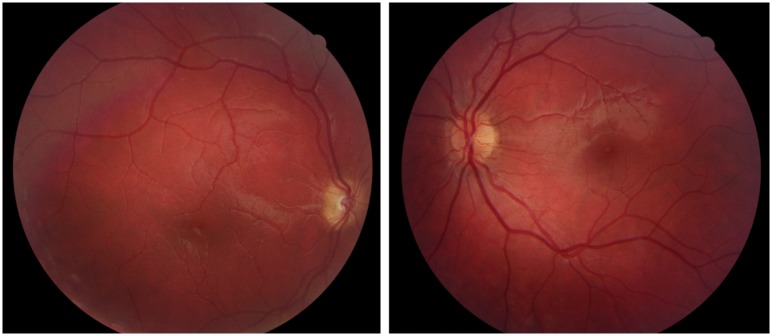
Fig 2. Fundus photographs from Case 18 with bilateral optic nerve hypoplasia.
Case 18 was born full term and developmental delay was noticed at one year of age. She was diagnosed with moderate intellectual disability and has autistic traits. She had strabismus and bilateral optic nerve hypoplasia was diagnosed at three years of age. The BCVA was 0.12 right and left eye at six years of age.
Whole genome sequencing identifies 11 rare SNVs in 10 ONH cases
SNVs in COL4A1 and COL4A2
WGS of the 29 individuals with ONH resulted in 11 rare SNVs identified in 10 ONH cases (Tables 1 and 2, Fig 1). Of these, two variants were located in COL4A1 (MIM 120130) and two variants in COL4A2 (MIM 120090) (Fig 3).
Table 2. Rare single nucleotide variants identified in the optic nerve hypoplasia cohort.
| Case | Gene | cDNA change | Amino acid change | rsID | Zygosity | CADD [27] | ExAC [21] | SweFreq [23] |
|---|---|---|---|---|---|---|---|---|
| 2 | SPG7 | c.1529C>T | p.(Ala510Val) | rs61755320 | Het | 32 | 0.0036 | 0.0035 |
| 5 | CYP26A1 | c.1184T>C | p.(Ile395Thr) | rs757601865 | Het | 23.8 | 0 | 0 |
| 11 | COL4A1 | c.2842G>A | p.(Gly948Ser) | - | Het | 25.6 | 0 | 0 |
| 14 | UBE3B | c.2962G>A | p.(Ala988Thr) | rs753221661 | Het | 34 | 0.0001 | 0 |
| 17 | COL4A2 | c.4987G>A | p.(Gly1663Ser) | rs12877501 | Hom | 23.7 | 0.0009 | 0.001 |
| 19 | CYP26C1 | c.845_851dup CCATGCA | p.(Gln284fs) | rs565866662 | Het | 34 | 0.0029 | 0.007 |
| 20 | CYP26C1 | c.356A>C | p.(Gln119Pro) | rs201284617 | Het | 23.5 | 0.0001 | 0.0055 |
| 21 | COL4A1 | c.161C>T | p.(Pro54Leu) | rs34004222 | Het | 26.5 | 0.0035 | 0.0035 |
| 21 | OPA1 | c.1146A>G | p.(Ile382Met) | rs143319805 | Het | 24.4 | 0.0008 | 0 |
| 27 | COL4A2 | c.2185G>A | p.(Gly729Arg) | rs201058867 | Het | 24.2 | 0.0004 | 0.0015 |
| 29 | KIF7 | c.3331C>T | p.(Arg1111Ter) | rs778139192 | Hom | 43 | 0 | 0 |
CADD, combined annotation-dependent depletion; Het, heterozygous; Hom, homozygous.
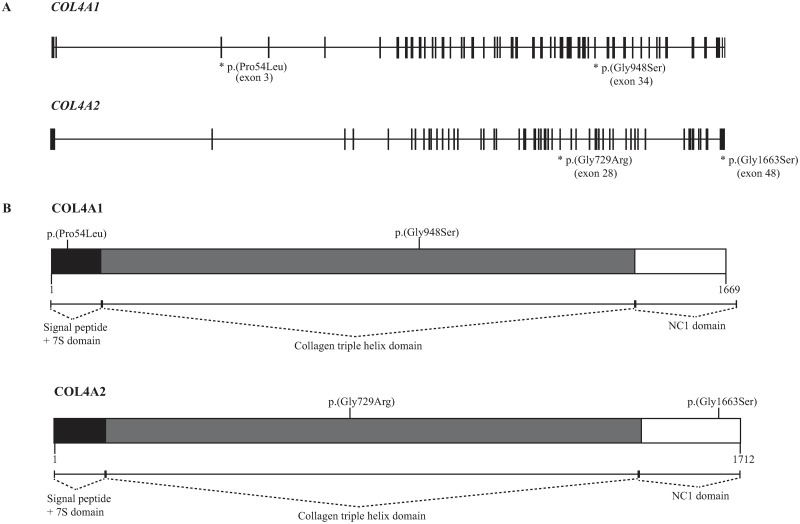
Fig 3. Rare variants in COL4A1 and COL4A2.
Rare variants in COL4A1 and COL4A2 were identified in 4/29 (14%) individuals with optic nerve hypoplasia (A). Of these four variants, two affected the collagen triple helix domain of COL4A1 or COL4A2, one affected the 7S domain of COL4A1, and one affected the noncollagenous (NC1) domain of COL4A2 (B).
Three of the variants in COL4A1 or COL4A2 were very interesting. In Case 11, we identified a rare variant COL4A1 p.(Gly948Ser) confirmed to be de novo by segregation studies. The same variant has previously been reported and described as pathogenic in an individual with porencephaly, calcification, cerebral palsy, epilepsy, and intellectual disability [32]. Case 11 had similar symptoms except porencephaly (Table 1). He was born full term and was diagnosed with bilateral ONH at four months of age due to lack of fixation. Besides blindness, he had infantile spasms and continued to have epilepsy, but also severe bilateral spastic cerebral palsy as well as severe intellectual disability. This finding is further evidence of the pathogenicity of the COL4A1 p.(Gly948Ser) mutation.
The second variant of interest was found in Case 17 who had a homozygous variant in COL4A2 p.(Gly1663Ser) with each allele inherited from two unrelated parents (Figs 1 and 4). Interestingly, there are no homozygous individuals with this variant reported in the ExAC database [21]. The third individual (Case 21) had two rare variants, a heterozygous missense variant in COL4A1 p.(Pro54Leu) and a heterozygous missense variant in OPA1 p.(Ile382Met) (MIM 605290) (Fig 5). Both variants were inherited from the father, who had a suspected traumatic unilateral optic atrophy. Moreover, the fourth individual (Case 27) had a heterozygous missense variant in COL4A2 p.(Gly729Arg) inherited from a healthy mother (Fig 6).
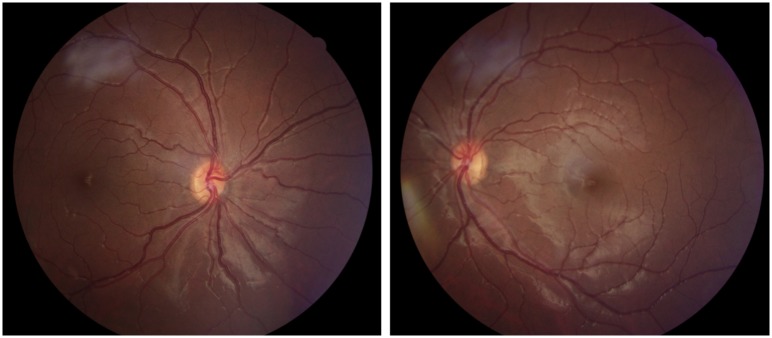
Fig 4. Fundus photographs from Case 17 with bilateral optic nerve hypoplasia.
Case 17 was born full term and due to nystagmus bilateral optic nerve hypoplasia was diagnosed at one month of age. He was visually impaired with a BCVA of 0.15 right and 0.03 left eye at 12 years of age. Extreme thirst and weight gain at three months of age revealed a diabetes insipidus. In addition, he had adrenocorticotropic hormone deficiency. At ten years of age he was diagnosed with an autism spectrum disorder, but he has normal intelligence. Furthermore, he has hyposmia, mild gross motor function impairment, and jaw abnormalities.
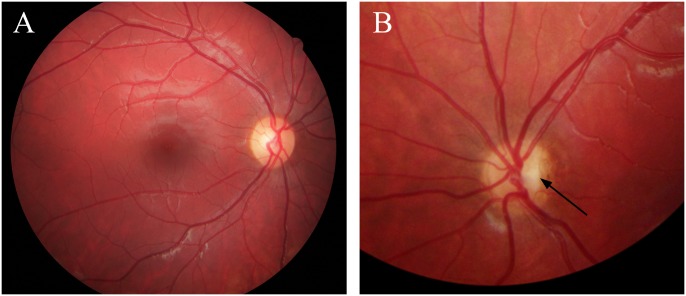
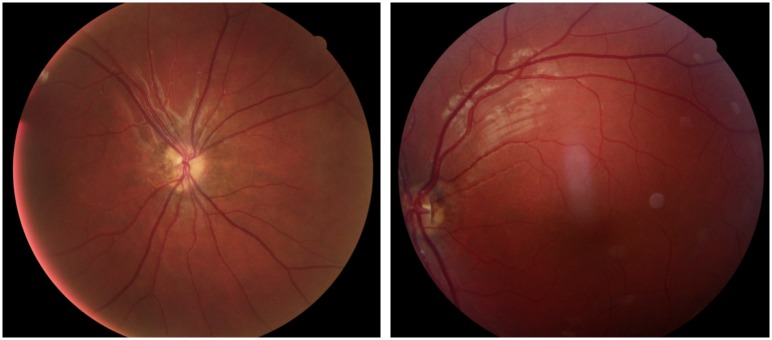
Fig 5. Fundus photographs from Case 21 with unilateral optic nerve hypoplasia left eye.
Fundus photographs from Case 21 with unilateral optic nerve hypoplasia and heterozygous missense variants in COL4A1 and OPA1 showing (A) a normal optic disc in the right eye and (B, magnified image) optic nerve hypoplasia in the left eye with a small optic disc (arrow) and a surrounding peripapillary atrophy. Case 21 was born full term and was treated with patching from 11 months of age because of strabismus (esotropia left eye). She was lost to follow-up and unilateral optic nerve hypoplasia was diagnosed after the visual screening at four years of age. The BCVA was 1.0 right and 0.03 left eye at 15 years of age. She had a precocious puberty from seven years of age and is normally developed.
Fig 6. Fundus photographs from Case 27 with unilateral optic nerve hypoplasia right eye.
Case 27 was born at 37 weeks of gestation. She developed strabismus (exotropia right eye) and unilateral optic nerve hypoplasia was diagnosed at two years of age. The BCVA was 0.5 right and 1.0 left eye at 11 years of age. She has a mild intellectual disability.
In total, 4/11 (36%) of all the rare SNVs identified were in COL4A1 or COL4A2, and 4/29 (14%) of the individuals in the cohort carried a rare missense variant in either of these two genes. Constraint metrics retrieved from the ExAC browser indicated a z-score for missense variants of 2.46 in COL4A1 and 1.76 in COL4A2. Hence, the increased number of missense variants in these particular genes could not directly be explained by decreased constraint.
Pathogenic homozygous SNV in KIF7
Another striking finding was a homozygous nonsense variant in KIF7 p.(Arg1111Ter) (MIM 611254) in Case 29, inherited from both of her consanguineous parents. The KIF7 variant has previously been reported as pathogenic in an individual with Joubert syndrome (MIM 213300) [33]. The phenotype in Case 29 is concordant with Joubert syndrome with molar tooth sign on magnetic resonance imaging, ataxia, impairments in gross and fine motor function, and intellectual disability. In addition, Case 29 has craniofacial features fitting acrocallosal syndrome (MIM 200990) [34], namely macrocephaly, prominent forehead, hypertelorism, downslanting palpebral fissures as well as wide and depressed nasal bridge (Table 1, Fig 7). Acrocallosal syndrome is an autosomal recessive neurodevelopmental ciliopathy often caused by KIF7 mutations and phenotypically overlaps with Joubert syndrome [34].
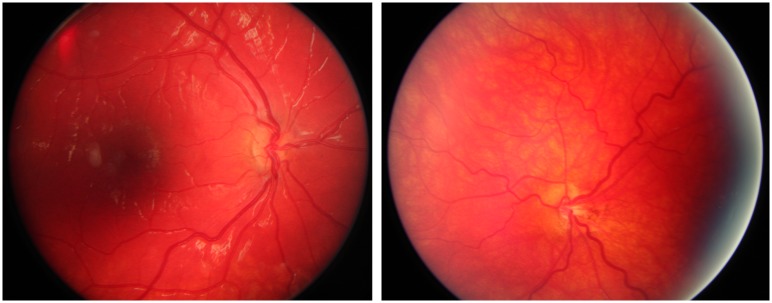
Fig 7. Fundus photographs from Case 29 with bilateral optic nerve hypoplasia.
Case 29 was born full term and came to Sweden from Iraq at four years of age. She had strabismus (exophoria left eye) and multiple brain malformations, including thin optic nerves, on magnetic resonance imaging. However, bilateral optic nerve hypoplasia was not diagnosed until she was 17 years of age. At 18 years of age the BCVA was 0.8 right and 0.5 left eye. She was further diagnosed with a moderate intellectual disability and has mild motor impairments.
In summary, three of the SNVs (COL4A1 p.(Gly948Ser), COL4A2 p.(Gly1663Ser), and KIF7 p.(Arg1111Ter)) were assessed as pathogenic or likely pathogenic, and the remaining eight SNVs were heterozygous variants of unknown clinical significance.
Discussion
In the present study, we performed a systematic screening for rare genomic variants in 29 individuals with ONH and identified 11 rare SNVs in ten individuals and one rare CNV in one individual. This is the first WGS study of a cohort with ONH and the results show that there is a genetic heterogeneity in ONH and indicates that genetic causes of ONH are not rare. The diagnostic yield of pathogenic or likely pathogenic variants in individuals with ONH using WGS was 4/29 (14%), all of whom had non-isolated ONH. Consequently, in the group of non-isolated ONH, 4/20 (20%) had a presumed genetic cause.
SNVs in COL4A1 and COL4A2 genes were frequent in our cohort (4/29, 14%). In particular, two of the rare variants were especially interesting. They were the heterozygous de novo variant COL4A1 p.(Gly948Ser) previously described as pathogenic and the homozygous variant COL4A2 p.(Gly1663Ser) [32]. COL4A1 and COL4A2 encode, respectively, the alpha-1 and alpha-2 subunits of collagen type IV. Together they form a heterotrimer of two alpha-1 chains and one alpha-2 chain. Collagen type IV is essential for basement membranes and is involved in cell adhesion, migration, proliferation, and differentiation [35]. The two genes are arranged head-to-head on opposite strands at 13q34 with a common bidirectional promotor [35]. Mutations in COL4A1 have been associated with small-vessel brain disease including porencephaly, schizencephaly, cerebrovascular disease, ophthalmological disorders (retinal arterial tortuosity, congenital cataract, anterior segment dysgenesis, glaucoma, microphthalmia/anophthalmia, optic atrophy, and ONH), but also with renal and muscular abnormalities [32,36,37]. There is an autosomal dominant pattern of inheritance, broad phenotypic variation with reduced penetrance, and a wide heterogeneity of symptoms within families. Similarly, mutations in COL4A2 have been associated with porencephaly, intracerebral haemorrhages, optic atrophy, and ONH [37–41]. Animal studies further support their involvement in ONH and the variability of phenotypic penetrance [42]. Col4a1+/Δex41 mutant mice develop ONH, but this is dependent on the genetic background of these mice [43]. In addition, these mice show changes in the retinal inner limiting membrane, suggesting that abnormalities of the basement membranes may cause ONH [43]. However, despite the evidence for a role of Col4 paralogues in ONH, only a few ONH cases with mutations in COL4A1 and COL4A2 are described in the literature [32,38].
Here we report two rare variants in COL4A1 and two rare variants in COL4A2. The location of the variants in COL4A1 and COL4A2 seems to be of major importance. Two of these variants were located in the triple helix domain, one in the amino-terminal 7S domain of COL4A1, and one in the carboxy-terminal noncollagenous (NC1) domain of COL4A2 (Fig 3). The two variants located in the triple helix domain resulted in the substitution of a glycine (Fig 3). The first was the heterozygous de novo variant COL4A1 p.(Gly948Ser) and the second was the heterozygous variant COL4A2 p.(Gly729Arg). In the triple helix domain, the triple amino acid repeats with glycine in every third position are essential for the proper triple helical formation and mutations in this region are known to disrupt the normal folding and protein function [44]. Hence, substitutions of the glycine in these repeats have been predicted to be pathogenic and are assumed to have a dominant-negative effect on the protein [35,37]. In contrast, the homozygous variant COL4A2 p.(Gly1663Ser) were located in in the NC1 domain, which has a prominent role in regulating the stoichiometry of the α1α1α2 heterotrimer [35]. One may hypothesise that this homozygous variant could affect the composition of the heterotrimer and subsequently, the function of collage typ IV.
Previous research has shown a high de novo mutation rate in COL4A1 and COL4A2 as well as inherited pathogenic or likely pathogenic mutations [37]. In our cohort, only one COL4A1 variant was shown to be de novo. Moreover, because of the broad phenotypic variation with reduced penetrance, the inherited heterozygous rare variants COL4A1 p.(Pro54Leu) and COL4A2 p.(Gly729Arg) could not be assessed as likely benign and were assessed as variants of unknown clinical significance. The substitution of a glycine in the triple helix domain in the variant COL4A2 p.(Gly729Arg) even suggests that it may be pathogenic. Consequently, functional studies would be helpful to understand the clinical significance of the inherited variants identified in this study.
In Case 21, in addition to the COL4A1 variant, an OPA1 variant p.(Ile382Met) was identified. Mutations in OPA1 are usually associated with optic atrophy 1, but it has previously been suggested that OPA1 may also be involved in ONH [45]. The variant identified in Case 21 is enriched in individuals with autosomal dominant optic atrophy, but is also present in both the dbSNP and ExAC databases (rs143319805) [46]. In two other optic atrophy studies, the OPA1 variant p.(Ile382Met) was identified in a compound heterozygous state in a total of five cases, and heterozygous carriers were an asymptomatic father and a mother with myopia and mild sensorineural hearing loss [47,48]. The authors hypothesised that this variant may have a semi-dominant mode of inheritance [48]. Case 21 has a clinically significant unilateral ONH shown in Fig 5. The rare variants in OPA1 and COL4A1 were inherited from the father who had strabismus as a child, suffered from a traumatic macular haemorrhage in the left eye as an adolescent and went through cataract surgery in adulthood (Fig 1). He was never diagnosed with ONH, but suspected to have a traumatic optic atrophy in his left eye.
In Case 29, we found a pathogenic homozygous nonsense variant in KIF7 p.(Arg1111Ter). Mutations in KIF7 are associated with the ciliopathy Joubert syndrome [33] and especially acrocallosal syndrome [34], which both fit with the patient’s symptoms. The kinesin KIF7 is an important regulator for the sonic hedgehog signaling pathway at the primary cilium [49]. Sonic hedgehog signaling is essential for patterning and brain development [49]. Furthermore, prenatal ethanol exposure causes ONH by inhibition of sonic hedgehog signaling in retinal progenitor cells in mice, resulting in failure to extend axons to the optic nerve [50]. Accordingly, both genetic and environmental factors may affect the sonic hedgehog signaling pathway and cause ONH. However, in Case 29, ONH could be a result of a primary optic nerve malformation and/or secondary to trans-synaptic degeneration due to the other brain malformations.
Moreover, rare SNVs were identified in four additional genes in five individuals; SPG7 (1/29), CYP26A1 (1/29), CYP26C1 (2/29), UBE3B (1/29), and one rare CNV affecting SOX5 (1/29) was detected. The variant identified in SPG7 p.(Ala510Val) (MIM 602783) has previously been described in individuals with spastic paraplegia 7 (MIM 607259), and another SPG7 variant, c.1232A>C, p.(Asp411Ala), segregated with the disease in a family with an autosomal dominant optic neuropathy [51]. The individual carrying the heterozygous SPG7 variant in this study (Case 2) was born full term and developed strabismus and nystagmus, but was not diagnosed with bilateral ONH until he was 17 years of age despite blindness. In addition to ONH, he has severe intellectual disability, bilateral spastic cerebral palsy, epilepsy, microcephaly, and facial asymmetry. The specific p.(Ala510Val) variant is commonly described in autosomal recessive spastic paraplegia, nevertheless, in a study of 285 individuals with spastic paraplegia, a dominant effect was suggested for the p.(Ala510Val) [52]. In Case 2, the variant SPG7 p.(Ala510Val) was inherited from a healthy mother. Nonetheless, considering previous evidence of involvement in brain dysfunction, we speculate that this variant could be a partial explanation of the patient’s symptoms, including ONH, and it was assessed as a variant of unknown clinical significance.
Finally, deletions of CYP26A1 (MIM 602239) and CYP26C1 (MIM 608428) have previously been implicated in both nonsyndromic bilateral and unilateral optic nerve aplasia [53], and mutations in UBE3B (MIM 608047) have been described in Kaufman Oculocerebrofacial Syndrome (MIM 244450) [54]. However, since the three variants where parental DNA was available showed inheritance from a healthy parent, they were assessed as less likely to be the cause of the ONH phenotype (Figs 1 and 8–11).
Fig 8. Fundus photographs from Case 5 with bilateral optic nerve hypoplasia.
Case 5 was born full term and had neonatal hypoglycemia and seizures. Bilateral optic nerve hypoplasia was diagnosed at two months of age due to lack of fixation and nystagmus. At the same age he was diagnosed with adrenocorticotropic hormone deficiency, and later on he was also treated for growth hormone deficiency and central hypothyroidism. The BCVA was 0.125 right and left eye at seven years of age. He is normally developed.
Fig 11. Fundus photographs from Case 14 with bilateral optic nerve hypoplasia.
Case 14 was born preterm at 27 weeks of gestation. He had strabismus and was diagnosed with left sided optic nerve hypoplasia at 13 months of age, which on closer assessment proved to be bilateral optic nerve hypoplasia when he was 13 years of age. The BCVA was 1.0 right and 0.1 left eye at eight years of age, but he had a significant visual field defect in his right eye. He is normally developed.
Fig 9. Fundus photographs from Case 19 with unilateral optic nerve hypoplasia right eye.
Case 19 was born full term. He had severe strabismus (esotropia right eye) and was diagnosed with unilateral optic nerve hypoplasia at two months of age. He is blind in his right eye, but the BCVA was 1.0 left eye at 12 years of age. He is normally developed.
Fig 10. Fundus photographs from Case 20 with unilateral optic nerve hypoplasia right eye.
Case 20 was born full term and unilateral optic nerve hypoplasia was discovered at the ophthalmology department after detection at the visual screening at four years of age. He had strabismus (esotropia right eye) and the BCVA was 0.1 right and 1.0 left eye at five years of age. He has normal intelligence.
Likely, ONH can be caused of monogenic, polygenic and environmental factors, single or in combinations. Lubinsky previously hypothesised that septo-optic dysplasia (MIM 182230), including ONH, is a result of a vascular disruptive sequence, possibly involving the proximal trunk of the anterior cerebral artery [55]. Risk factors such as early gestational vaginal bleeding and use of vasoconstrictors (tobacco and cocaine) may increase the risk of a vascular insult [56], and so could mutations in COL4A1 or COL4A2. We speculate that the broad phenotype seen in children with ONH may be explained by the disease gene and the overall mutational burden, modified by the regulatory landscape and environmental factors. This could also explain why so few family members are affected and the reduced penetrance seen in many of the candidate genes. We used WGS to analyse protein-coding sequences of known disease causing genes, but it would also be very interesting to look at novel genes and non-coding sequences, including regulatory elements. It is reasonable to assume that genetic mutations in these parts may contribute to the broad phenotype and reduced penetrance, and this should be further studied. Chen et al have published an excellent review of genetic causes of ONH which highlighted 16 genes [12]. To this list we suggest to add COL4A1 and COL4A2, which seem to be important genetic contributors to ONH.
In conclusion, the present study elucidates the genetic heterogeneity in ONH and indicates that genetic causes of ONH are not rare. We conclude that genetic testing is valuable in a substantial proportion of the individuals with ONH, especially in cases with non-isolated ONH. With the increased use of WGS more individuals with ONH should be able to receive a genetic diagnosis in the future.
Acknowledgments
We are grateful to neuroradiologist Maria Kristoffersen Wiberg for reviewing the neuroradiological imaging and to ortoptist Monica Olsson for visual and orthoptic assessments.
Data Availability
All the reported rare genetic variants were submitted to ClinVar database (https://www.ncbi.nlm.nih.gov/clinvar/) with accession numbers: SCV000681429, SCV000887490, SCV000681422, SCV000681432, SCV000681428, SCV000681434, SCV000681433, SCV000681423, SCV000681425, SCV000681430, SCV000681431, SCV000681427.
Funding Statement
This research was supported by the Swedish Research Council [2013-2603] (AL), the Swedish Society for Medical Research (AL), Marianne and Marcus Wallenberg Foundation [2014.0084] (AL), Stockholm County Council (AL), the Swedish Brain Foundation (AL), SciLifeLab National projects (AL), Linnea och Josef Carlsson Foundation (SD, BMA), Sunnerdahl’s Handicap Foundation (SD, RW), Sällskapet Barnavård (SD), Frimurare barnhuset Foundation (SD, BMA), HRH Crown Princess Lovisa and Axel Tielman’s Foundation (BMA), and Sigvard och Marianne Bernadotte Foundation (KTF). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Tear Fahnehjelm K, Dahl S, Martin L, Ek U. Optic nerve hypoplasia in children and adolescents; prevalence, ocular characteristics and behavioural problems. Acta Ophthalmol. 2014; 92: 563–570. 10.1111/aos.12270 [DOI] [PubMed] [Google Scholar]
- 2.Kim MR, Park SE, Oh SY. Clinical feature analysis of congenital optic nerve abnormalities. Jpn J Ophthalmol. 2006; 50: 250–255. 10.1007/s10384-006-0310-8 [DOI] [PubMed] [Google Scholar]
- 3.Garcia-Filion P, Borchert M. Optic nerve hypoplasia syndrome: a review of the epidemiology and clinical associations. Curr Treat Options Neurol. 2013; 15: 78–89. 10.1007/s11940-012-0209-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel L, McNally RJ, Harrison E, Lloyd IC, Clayton PE. Geographical distribution of optic nerve hypoplasia and septo-optic dysplasia in Northwest England. J Pediatr. 2006; 148: 85–88. 10.1016/j.jpeds.2005.07.031 [DOI] [PubMed] [Google Scholar]
- 5.Dahl S, Wickstrom R, Ek U, Tear Fahnehjelm K. Children with optic nerve hypoplasia face a high risk of neurodevelopmental disorders. Acta Paediatr. 2018; 107: 484–489. 10.1111/apa.14163 [DOI] [PubMed] [Google Scholar]
- 6.Dahl S, Kristoffersen Wiberg M, Tear Fahnehjelm K, Savendahl L, Wickstrom R. High prevalence of pituitary hormone deficiency in both unilateral and bilateral optic nerve hypoplasia. Acta Paediatr. 2019; 108: 1677–1685. 10.1111/apa.14751 [DOI] [PubMed] [Google Scholar]
- 7.Garcia-Filion P, Fink C, Geffner ME, Borchert M. Optic nerve hypoplasia in North America: a re-appraisal of perinatal risk factors. Acta Ophthalmol. 2010; 88: 527–534. 10.1111/j.1755-3768.2008.01450.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Margalith D, Jan JE, McCormick AQ, Tze WJ, Lapointe J. Clinical spectrum of congenital optic nerve hypoplasia: review of 51 patients. Dev Med Child Neurol. 1984; 26: 311–322. 10.1111/j.1469-8749.1984.tb04447.x [DOI] [PubMed] [Google Scholar]
- 9.Cidis MB, Warshowsky JH, Goldrich SG, Meltzer CC. Mirror-image optic nerve dysplasia with associated anisometropia in identical twins. J Am Optom Assoc. 1997; 68: 325–329. [PubMed] [Google Scholar]
- 10.Dattani MT, Martinez-Barbera JP, Thomas PQ, Brickman JM, Gupta R, Martensson IL, et al. Mutations in the homeobox gene HESX1/Hesx1 associated with septo-optic dysplasia in human and mouse. Nat Genet. 1998; 19: 125–133. 10.1038/477 [DOI] [PubMed] [Google Scholar]
- 11.McNay DE, Turton JP, Kelberman D, Woods KS, Brauner R, Papadimitriou A, et al. HESX1 mutations are an uncommon cause of septooptic dysplasia and hypopituitarism. J Clin Endocrinol Metab. 2007; 92: 691–697. 10.1210/jc.2006-1609 [DOI] [PubMed] [Google Scholar]
- 12.Chen CA, Yin J, Lewis RA, Schaaf CP. Genetic causes of optic nerve hypoplasia. J Med Genet. 2017; 54: 441–449. 10.1136/jmedgenet-2017-104626 [DOI] [PubMed] [Google Scholar]
- 13.McCabe MJ, Alatzoglou KS, Dattani MT. Septo-optic dysplasia and other midline defects: the role of transcription factors: HESX1 and beyond. Best Pract Res Clin Endocrinol Metab. 2011; 25: 115–124. 10.1016/j.beem.2010.06.008 [DOI] [PubMed] [Google Scholar]
- 14.Pettersson M, Viljakainen H, Loid P, Mustila T, Pekkinen M, Armenio M, et al. Copy Number Variants Are Enriched in Individuals With Early-Onset Obesity and Highlight Novel Pathogenic Pathways. J Clin Endocrinol Metab. 2017; 102: 3029–3039. 10.1210/jc.2017-00565 [DOI] [PubMed] [Google Scholar]
- 15.Richards CS, Bale S, Bellissimo DB, Das S, Grody WW, Hegde MR, et al. ACMG recommendations for standards for interpretation and reporting of sequence variations: Revisions 2007. Genet Med. 2008; 10: 294–300. 10.1097/GIM.0b013e31816b5cae [DOI] [PubMed] [Google Scholar]
- 16.Abyzov A, Urban AE, Snyder M, Gerstein M. CNVnator: an approach to discover, genotype, and characterize typical and atypical CNVs from family and population genome sequencing. Genome Res. 2011; 21: 974–984. 10.1101/gr.114876.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eisfeldt J, Vezzi F, Olason P, Nilsson D, Lindstrand A. TIDDIT, an efficient and comprehensive structural variant caller for massive parallel sequencing data. F1000Res. 2017; 6: 664 10.12688/f1000research.11168.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N, et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics. 2009; 25: 2078–2079. 10.1093/bioinformatics/btp352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garrison E, Marth G. Haplotype-based variant detection from short-read sequencing; 2012. arXiv:1207.3907. Accessed 17 July 2012.
- 20.McLaren W, Gil L, Hunt SE, Riat HS, Ritchie GR, Thormann A, et al. The Ensembl Variant Effect Predictor. Genome Biol. 2016; 17: 122 10.1186/s13059-016-0974-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lek M, Karczewski KJ, Minikel EV, Samocha KE, Banks E, Fennell T, et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature. 2016; 536: 285–291. 10.1038/nature19057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abecasis GR, Altshuler D, Auton A, Brooks LD, Durbin RM, Gibbs RA, et al. A map of human genome variation from population-scale sequencing. Nature. 2010; 467: 1061–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ameur A, Dahlberg J, Olason P, Vezzi F, Karlsson R, Martin M, et al. SweGen: a whole-genome data resource of genetic variability in a cross-section of the Swedish population. Eur J Hum Genet. 2017; 25: 1253–1260. 10.1038/ejhg.2017.130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kumar P, Henikoff S, Ng PC. Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc. 2009; 4: 1073–1081. 10.1038/nprot.2009.86 [DOI] [PubMed] [Google Scholar]
- 25.Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P, et al. A method and server for predicting damaging missense mutations. Nat Methods. 2010; 7: 248–249. 10.1038/nmeth0410-248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thorvaldsdottir H, Robinson JT, Mesirov JP. Integrative Genomics Viewer (IGV): high-performance genomics data visualization and exploration. Brief Bioinform. 2013; 14: 178–192. 10.1093/bib/bbs017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kircher M, Witten DM, Jain P, O'Roak BJ, Cooper GM, Shendure J. A general framework for estimating the relative pathogenicity of human genetic variants. Nat Genet. 2014; 46: 310–315. 10.1038/ng.2892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015; 17: 405–424. 10.1038/gim.2015.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lai T, Jabaudon D, Molyneaux BJ, Azim E, Arlotta P, Menezes JR, et al. SOX5 controls the sequential generation of distinct corticofugal neuron subtypes. Neuron. 2008; 57: 232–247. 10.1016/j.neuron.2007.12.023 [DOI] [PubMed] [Google Scholar]
- 30.Lee RW, Bodurtha J, Cohen J, Fatemi A, Batista D. Deletion 12p12 involving SOX5 in two children with developmental delay and dysmorphic features. Pediatr Neurol. 2013; 48: 317–320. 10.1016/j.pediatrneurol.2012.12.013 [DOI] [PubMed] [Google Scholar]
- 31.Nesbitt A, Bhoj EJ, McDonald Gibson K, Yu Z, Denenberg E, Sarmady M, et al. Exome sequencing expands the mechanism of SOX5-associated intellectual disability: A case presentation with review of sox-related disorders. Am J Med Genet A. 2015; 167A: 2548–2554. 10.1002/ajmg.a.37221 [DOI] [PubMed] [Google Scholar]
- 32.Yoneda Y, Haginoya K, Kato M, Osaka H, Yokochi K, Arai H, et al. Phenotypic spectrum of COL4A1 mutations: porencephaly to schizencephaly. Ann Neurol. 2013; 73: 48–57. 10.1002/ana.23736 [DOI] [PubMed] [Google Scholar]
- 33.Bachmann-Gagescu R, Dempsey JC, Phelps IG, O'Roak BJ, Knutzen DM, Rue TC, et al. Joubert syndrome: a model for untangling recessive disorders with extreme genetic heterogeneity. J Med Genet. 2015; 52: 514–522. 10.1136/jmedgenet-2015-103087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Asadollahi R, Strauss JE, Zenker M, Beuing O, Edvardson S, Elpeleg O, et al. Clinical and experimental evidence suggest a link between KIF7 and C5orf42-related ciliopathies through Sonic Hedgehog signaling. Eur J Hum Genet. 2018; 26: 197–209. 10.1038/s41431-017-0019-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khoshnoodi J, Pedchenko V, Hudson BG. Mammalian collagen IV. Microsc Res Tech. 2008; 71: 357–370. 10.1002/jemt.20564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Plaisier E, Gribouval O, Alamowitch S, Mougenot B, Prost C, Verpont MC, et al. COL4A1 mutations and hereditary angiopathy, nephropathy, aneurysms, and muscle cramps. N Engl J Med. 2007; 357: 2687–2695. 10.1056/NEJMoa071906 [DOI] [PubMed] [Google Scholar]
- 37.Meuwissen ME, Halley DJ, Smit LS, Lequin MH, Cobben JM, de Coo R, et al. The expanding phenotype of COL4A1 and COL4A2 mutations: clinical data on 13 newly identified families and a review of the literature. Genet Med. 2015; 17: 843–853. 10.1038/gim.2014.210 [DOI] [PubMed] [Google Scholar]
- 38.Verbeek E, Meuwissen ME, Verheijen FW, Govaert PP, Licht DJ, Kuo DS, et al. COL4A2 mutation associated with familial porencephaly and small-vessel disease. Eur J Hum Genet. 2012; 20: 844–851. 10.1038/ejhg.2012.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yoneda Y, Haginoya K, Arai H, Yamaoka S, Tsurusaki Y, Doi H, et al. De novo and inherited mutations in COL4A2, encoding the type IV collagen alpha2 chain cause porencephaly. Am J Hum Genet. 2012; 90: 86–90. 10.1016/j.ajhg.2011.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jeanne M, Labelle-Dumais C, Jorgensen J, Kauffman WB, Mancini GM, Favor J, et al. COL4A2 mutations impair COL4A1 and COL4A2 secretion and cause hemorrhagic stroke. Am J Hum Genet. 2012; 90: 91–101. 10.1016/j.ajhg.2011.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gunda B, Mine M, Kovacs T, Hornyak C, Bereczki D, Varallyay G, et al. COL4A2 mutation causing adult onset recurrent intracerebral hemorrhage and leukoencephalopathy. J Neurol. 2014; 261: 500–503. 10.1007/s00415-013-7224-4 [DOI] [PubMed] [Google Scholar]
- 42.Kuo DS, Labelle-Dumais C, Mao M, Jeanne M, Kauffman WB, Allen J, et al. Allelic heterogeneity contributes to variability in ocular dysgenesis, myopathy and brain malformations caused by Col4a1 and Col4a2 mutations. Hum Mol Genet. 2014; 23: 1709–1722. 10.1093/hmg/ddt560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gould DB, Marchant JK, Savinova OV, Smith RS, John SW. Col4a1 mutation causes endoplasmic reticulum stress and genetically modifiable ocular dysgenesis. Hum Mol Genet. 2007; 16: 798–807. 10.1093/hmg/ddm024 [DOI] [PubMed] [Google Scholar]
- 44.Engel J, Prockop DJ. The zipper-like folding of collagen triple helices and the effects of mutations that disrupt the zipper. Annu Rev Biophys Biophys Chem. 1991; 20: 137–152. 10.1146/annurev.bb.20.060191.001033 [DOI] [PubMed] [Google Scholar]
- 45.Barboni P, Carbonelli M, Savini G, Foscarini B, Parisi V, Valentino ML, et al. OPA1 mutations associated with dominant optic atrophy influence optic nerve head size. Ophthalmology. 2010; 117: 1547–1553. 10.1016/j.ophtha.2009.12.042 [DOI] [PubMed] [Google Scholar]
- 46.Schimpf S, Fuhrmann N, Schaich S, Wissinger B. Comprehensive cDNA study and quantitative transcript analysis of mutant OPA1 transcripts containing premature termination codons. Hum Mutat. 2008; 29: 106–112. 10.1002/humu.20607 [DOI] [PubMed] [Google Scholar]
- 47.Schaaf CP, Blazo M, Lewis RA, Tonini RE, Takei H, Wang J, et al. Early-onset severe neuromuscular phenotype associated with compound heterozygosity for OPA1 mutations. Mol Genet Metab. 2011; 103: 383–387. 10.1016/j.ymgme.2011.04.018 [DOI] [PubMed] [Google Scholar]
- 48.Bonneau D, Colin E, Oca F, Ferre M, Chevrollier A, Gueguen N, et al. Early-onset Behr syndrome due to compound heterozygous mutations in OPA1. Brain. 2014; 137: e301 10.1093/brain/awu184 [DOI] [PubMed] [Google Scholar]
- 49.Ruat M, Roudaut H, Ferent J, Traiffort E. Hedgehog trafficking, cilia and brain functions. Differentiation. 2012; 83: S97–104. 10.1016/j.diff.2011.11.011 [DOI] [PubMed] [Google Scholar]
- 50.Kahn BM, Corman TS, Lovelace K, Hong M, Krauss RS, Epstein DJ. Prenatal ethanol exposure in mice phenocopies Cdon mutation by impeding Shh function in the etiology of optic nerve hypoplasia. Dis Model Mech. 2017; 10: 29–37. 10.1242/dmm.026195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Klebe S, Depienne C, Gerber S, Challe G, Anheim M, Charles P, et al. Spastic paraplegia gene 7 in patients with spasticity and/or optic neuropathy. Brain. 2012; 135: 2980–2993. 10.1093/brain/aws240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sanchez-Ferrero E, Coto E, Beetz C, Gamez J, Corao AI, Diaz M, et al. SPG7 mutational screening in spastic paraplegia patients supports a dominant effect for some mutations and a pathogenic role for p.A510V. Clin Genet. 2013; 83: 257–262. 10.1111/j.1399-0004.2012.01896.x [DOI] [PubMed] [Google Scholar]
- 53.Meire F, Delpierre I, Brachet C, Roulez F, Van Nechel C, Depasse F, et al. Nonsyndromic bilateral and unilateral optic nerve aplasia: first familial occurrence and potential implication of CYP26A1 and CYP26C1 genes. Mol Vis. 2011; 17: 2072–2079. [PMC free article] [PubMed] [Google Scholar]
- 54.Flex E, Ciolfi A, Caputo V, Fodale V, Leoni C, Melis D, et al. Loss of function of the E3 ubiquitin-protein ligase UBE3B causes Kaufman oculocerebrofacial syndrome. J Med Genet. 2013; 50: 493–499. 10.1136/jmedgenet-2012-101405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lubinsky MS. Hypothesis: septo-optic dysplasia is a vascular disruption sequence. Am J Med Genet. 1997; 69: 235–236. [PubMed] [Google Scholar]
- 56.Atapattu N, Ainsworth J, Willshaw H, Parulekar M, MacPherson L, Miller C, et al. Septo-optic dysplasia: antenatal risk factors and clinical features in a regional study. Horm Res Paediatr. 2012; 78: 81–87. 10.1159/000341148 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the reported rare genetic variants were submitted to ClinVar database (https://www.ncbi.nlm.nih.gov/clinvar/) with accession numbers: SCV000681429, SCV000887490, SCV000681422, SCV000681432, SCV000681428, SCV000681434, SCV000681433, SCV000681423, SCV000681425, SCV000681430, SCV000681431, SCV000681427.