Abstract
BACKGROUND:
From 5 to 7.5 million schoolchildren are chronically absent, defined as missing ≥15days of school within a year. Students miss schools due to various reasons such as health, socioeconomic status, and environmental factors. We examined child’s health and behavior, family structure, and sociodemographics to understand chronic absenteeism.
METHODS:
The population included children ages 6 to 17years from the Medical Expenditure Panel Survey years 2008–2013. Multivariable logistic regressions were used to identify the risk factors of chronic absenteeism, adjusting for the complex sampling design.
RESULTS:
Among sociodemographic variables, age ≥14years, race/ethnicity, lower-income family, public health insurance, US born, and speaking English at home were associated with absenteeism. Asians, Mexican Hispanics, and blacks have lower absenteeism than whites. Among health-related variables, children using an inhaler for asthma, having behavioral problems, and less healthy than other children were more likely to be chronically absent. Among family variables, a smaller family size was a risk factor for absenteeism.
CONCLUSIONS:
Asthma and behavioral problems were highly associated with chronic absenteeism. The identification of children at risk for chronic absenteeism will help the educational professionals identify the barriers to academic achievements and develop integrated educational interventions and policies to support disadvantaged children.
Keywords: chronic absenteeism, asthma, race/ethnicity, child behavior, disadvantaged children, Medical Expenditure Panel Survey
A bout 5 to 7.5 million schoolchildren (10–15%) are chronically absent, as defined by missing schools for at least 15days per year. Chronic absenteeism has been associated with poor academic performance and high dropout rates from high school, and is an important predictor of lower income in adulthood and poor lifetime health2,3 such as having potentially preventable chronic conditions.3
Students miss schools due to various reasons such as poor health, low socioeconomic status, and environmental factors.1,4 Acute illnesses such as influenza or strep throat may be the foremost reason for missing school but chronic health conditions also contribute to missed school days. Among these conditions, asthma, attention-deficit hyperactivity disorder (ADHD), and obesity have been frequently reported as having significant associations with chronic absenteeism. Asthmatic children miss more school,5–9 with an increased risk associated with asthma severity level.8 A number of studies report that overweight or obese children are more likely to be absent from school than children of normal weight.10–13 A study using the National Health Interview Survey (NHIS) found children with ADHD had significantly greater odds of missed school days adjusting for demographic factors.14 Besides ADHD, other behavioral and mental health conditions have been reported as risk factors of chronic absenteeism. Several studies found that behavioral or mental problems such as depression, anxiety, disruptive behavior, and substance use are associated with chronic absenteeism.3,15–17 Oral health has also been associated with school absenteeism. Pourat and Nicholson studied 7,240,000 children in California and found 7% of them missed school at least 1 day due to dental problems.18 However, there is a lack of studies addressing the effects of these multiple health and behavioral conditions, relevant in predicting chronic absenteeism.
A few studies have examined how family structure and function affect chronic absenteeism. A study by Ferrell found that children in single-parent households were more likely to miss school days than children in 2-parent households.19 As Belfanze and Byrnes reported, missed school days in single-parent or multigenerational households can be related to young adolescents taking on elder-care responsibilities.1
Chronic absenteeism is prevalent among students from low-income families. Homelessness, transition between foster care facilities, and temporary dislocation are among the major reasons for chronic absenteeism.1 A recent review article stressed the strong association between household food insecurity and school absenteeism.20 Health problems are often tied to socioeconomic status. For instance, children from lower income families are more likely to have asthma, which, in turn, resulted in their being chronically absent from school.3
Racial/ethnic differences are associated with chronic absenteeism. Compared to whites, most minority children such as Hispanics, African Americans, American Indians (AIs), Alaska Natives (ANs), and Native Hawaiian and Pacific Islanders (NHPIs) had higher school absenteeism rates. Asians, by contrast, showed consistently lower rates.13,21 Asians are diverse in socio-economic status, immigration patterns, and English proficiency.22,23 However, Asian ethnicities have often been aggregated due to small sample sizes in the United States. The aggregation of heterogeneous Asian subgroups can mask essential cultural or other important differences. To the best of our knowledge, there are no published studies investigating disaggregated Asian children on chronic absenteeism.
We examined children’s health and behavior, family and sociodemographic variables as predictors of chronic absenteeism using a large nationally representative dataset, the Medical Expenditure Panel Survey (MEPS). Our study adds to the literature on chronic absenteeism with a comprehensive approach by addressing the gap concerning the lack of detailed information for Asian subpopulations and using a large nationally representative data investigating the 3 major groups of variables—health and behavior, family, and sociodemographics. The identification of children vulnerable for chronic absenteeism can help the federal, state, and local governments and educational professionals address the barriers to successful academic outcomes and achievements in a short term and better adulthood income and lifetime health in a long term.
METHODS
Data Source
The annual consolidated data from the MEPS years 2008–2013 were utilized. The MEPS draws 25% of families and individuals from a subsample of the households that participated in the prior year’s NHIS.24 The MEPS household survey component features an overlapping panel design in which each cohort or panel is followed over 2 years through 5 rounds of in-person interviews that collect detailed information on the use and payment of health care services. While Asians were combined as one racial group in the MEPS data 2008–2012, the MEPS data were linked with the corresponding NHIS from 2007 to 2011 to obtain more detailed Asian ethnicity information.
Chronic Absenteeism
The number of missed school days due to illness or injury was calculated using the yearly consolidated files over the 5 rounds of interviews. About 9% of annual records were excluded because information fromatleast1roundwasmissing.Chronicabsenteeism was defined as missing 15 or more days of school within a year (yes/no).
Child’s Health and Behavior Variables
Asthma was identified by the question: “whether a person had ever been diagnosed with asthma.” Only participants identified as having asthma were further investigated with regard to their asthma medication usage for preventive medicine, relief, or both. ADHD was identified by the question: “whether a person had ever been diagnosed with ADHD or attention deficit disorder.” Obesity was categorized based on body mass index (BMI), measured from age 6 to 9 years as underweight or normal (BMI<25), overweight (25≤BMI<30), and obese (BMI≥30). The Columbia Impairment Scale (CIS) was used to assess child’s behavioral problems by measuring 13 items such as getting along with mother and behavior at home (see Table 3 for details). Each item was scored on a 5-point Likert-type scale ranging from 0 (“no problem”) to 4 (“a very big problem”), with higher scores indicating greater impairment.25,26 We used the cut-point of 15 for the combined CIS score to define severe impairment. We also explored each item as a separate predictor of chronic absenteeism. As indicators for dental problems, we considered the number of dental care visits. Perceived general health was asked using a 5-point Likert-type question ‘less healthy than other child,’ ranging from “1=definitely true” to “5=definitely false.” We combined “definitely true” and “mostly true” into “Yes” and the others categories into “No.”
Table 3.
Distribution of Each Item of Columbia Impairment Scale
| Variable | 0 | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|
| Getting along with mother*** | ||||||
| Missed school days <15days | 67.7 (0.6) | 16.8 (0.4) | 11.1 (0.3) | 2.1 (0.1) | 1.3 (0.1) | 1.0 (0.1) |
| Missed school days ≥15days | 51.3 (2.5) | 17.3 (2.0) | 18.2 (2.2) | 6.6 (1.2) | 5.1 (1.2) | 1.5 (0.7) |
| Getting along with father*** | ||||||
| Missed school days <15days | 64.5 (0.5) | 15.9 (0.4) | 9.7 (0.3) | 2.6 (0.1) | 2.5 (0.1) | 4.7 (0.2) |
| Missed school days ≥15days | 45.1 (2.4) | 17.2 (2.1) | 13.4 (1.9) | 6.5 (1.3) | 9.1 (1.2) | 8.7 (1.4) |
| Feeling unhappy or sad*** | ||||||
| Missed school days <15days | 65.9 (0.6) | 20.4 (0.4) | 10.4 (0.3) | 2.1 (0.1) | 0.9 (0.1) | 0.3 (0.1) |
| Missed school days ≥15days | 38.4 (2.6) | 22.4 (2.0) | 23.2 (2.0) | 9.3 (1.5) | 6.2 (1.1) | 0.4 (0.3) |
| Behavior at school*** | ||||||
| Missed school days <15days | 78.6 (0.4) | 11.8 (0.3) | 6.5 (0.2) | 1.7 (0.1) | 1.2 (0.1) | 0.3 (0.1) |
| Missed school days ≥15days | 62.3 (2.1) | 11.8 (1.5) | 12.6 (1.3) | 5.8 (1.0) | 7.4 (1.4) | 0.2 (0.1) |
| Having fun*** | ||||||
| Missed school days <15days | 88.8 (0.3) | 7.0 (0.2) | 3.0 (0.2) | 0.6 (0.1) | 0.4 (0.0) | 0.2 (0.1) |
| Missed school days ≥15days | 74.0 (2.5) | 12.2 (1.9) | 10.6 (1.7) | 2.0 (0.6) | 1.1 (0.3) | 0.1 (0.1) |
| Getting along with adults*** | ||||||
| Missed school days <15days | 85.5 (0.4) | 9.0 (0.3) | 4.1 (0.2) | 0.7 (0.1) | 0.5 (0.1) | 0.2 (0.0) |
| Missed school days ≥15days | 72.9 (2.0) | 11.8 (1.5) | 9.8 (1.4) | 3.5 (0.9) | 1.8 (0.6) | 0.1 (0.1) |
| Feeling nervous or afraid*** | ||||||
| Missed school days <15days | 60.7 (0.6) | 23.0 (0.4) | 11.9 (0.3) | 2.9 (0.1) | 1.2 (0.1) | 0.3 (0.1) |
| Missed school days ≥15days | 41.5 (2.7) | 21.9 (2.2) | 21.9 (2.1) | 8.9 (1.5) | 5.7 (1.2) | 0.0 (0.0) |
| Getting along with brothers and sisters*** | ||||||
| Missed school days <15days | 48.3 (0.7) | 22.0 (0.5) | 17.8 (0.5) | 3.9 (0.2) | 2.2 (0.1) | 5.8 (0.3) |
| Missed school days ≥15days | 37.8 (2.5) | 17.0 (1.9) | 22.6 (2.1) | 8.0 (1.3) | 6.8 (1.3) | 7.8 (1.6) |
| Getting along with other kids*** | ||||||
| Missed school days <15days | 76.6 (0.5) | 14.8 (0.4) | 6.6 (0.2) | 1.3 (0.1) | 0.6 (0.1) | 0.2 (0.0) |
| Missed school days ≥15days | 61.3 (2.3) | 17.5 (1.7) | 13.6 (1.6) | 5.3 (1.2) | 2.3 (0.7) | 0.1 (0.1) |
| Getting involved in activities like sports or hobbies*** | ||||||
| Missed school days <15days | 78.1 (0.4) | 10.4 (0.3) | 6.7 (0.2) | 2.3 (0.1) | 2.0 (0.1) | 0.5 (0.1) |
| Missed school days ≥15days | 54.3 (2.6) | 11.3 (1.5) | 16.1 (1.9) | 8.3 (1.4) | 9.6 (1.3) | 0.4 (0.2) |
| Schoolwork*** | ||||||
| Missed school days <15days | 69.8 (0.5) | 14.4 (0.4) | 10.6 (0.3) | 2.9 (0.1) | 2.0 (0.1) | 0.3 (0.1) |
| Missed school days ≥15days | 45.3 (2.7) | 15.2 (1.9) | 17.9 (1.9) | 8.9 (1.5) | 12.7 (1.7) | 0.1 (0.1) |
| Behavior at home*** | ||||||
| Missed school days <15days | 62.7 (0.6) | 22.0 (0.5) | 11.6 (0.3) | 2.5 (0.1) | 1.1 (0.1) | 0.1 (0.1) |
| Missed school days ≥15days | 42.6 (2.3) | 22.5 (2.2) | 22.0 (2.1) | 7.2 (1.2) | 5.7 (1.1) | 0.0 (0.0) |
| Staying out of trouble*** | ||||||
| Missed school days <15days | 77.0 (0.5) | 14.0 (0.4) | 6.2 (0.2) | 1.5 (0.1) | 1.0 (0.1) | 0.2 (0.1) |
| Missed school days ≥15days | 62.3 (2.4) | 14.5 (1.5) | 13.7 (1.6) | 4.5 (1.1) | 5.0 (1.1) | 0.0 (0.0) |
p < .001.
Higher score indicates a greater impairment (0 = no problem, 4 = a very big problem; 5 = do not know or this question is not applicable to the child).
Family Variables
The following family variables were considered: family type (categorized as 2-parent, single-parent, and no-parent family), family size (categorized as >4 vs ≤4), number of adults (categorized as 0–1, 2, and ≥3), number of preschool child(ren), and number of elderly. Family type was defined based on the presence of parental identifiers (IDs) in the MEPS database. A child was defined living in 2-parent family home if both parents’ IDs existed in the database. Living in a single-parent family home was assigned if only one parent’s ID was present. If no parent’s ID was present, the child was assumed living without a parent in his/her home. Family size was computed by counting the number of family members sharing the same family ID, and categorized for analysis as ≤4 and >4. The number of adults (aged ≥18years), preschool children (aged 0–5 years), and elderly (aged ≥65years) were calculated using family members’ ages.
Sociodemographic Variables
After exploring the distribution of race/ethnicity with the rates of chronic absenteeism, we categorized race/ethnicity as white, black, Mexican Hispanic (MH), Other Hispanic, Filipino, Other Asian, AI/AN/NHPI, and Other. Several other sociodemographic variables were considered: child’s age; sex; born in the United States (categorized as Yes vs No); language spoken at home (English vs Other); highest education level of family members (categorized as less than or equal to high school or general education degree (GED), some college, college graduate, and graduate level); income (poor: federal poverty level [FPL]<100%; low: 100%≤FPL<200%; middle: 200%≤FPL<400%; and high: FPL≥400%); and insurance status (categorized as any private, public only, and uninsured). The regions where children lived were categorized as Northeast, Midwest, South, and West.
Data Analysis
Data were summarized using frequencies with percentages and means with standard errors. Univariable logistic regression was used to explore the association between each predictor and chronic absenteeism. We then conducted multivariable logistic regressions using a backward stepwise selection method to determine significant predictors for chronic absenteeism. The results are presented as odds ratios (ORs) and 95% confidence intervals (CIs). Variance was estimated using the Taylor-series linearization. The c-statistic was computed to assess the goodness of fit of the final model. Individual predictors of p<.05 were considered statistically significant. All analyses were conducted in SAS version 9.4 using survey procedures such as PROC SURVEYLOGISTIC, adjusting for the MEPS complex sampling design and repeated measures by incorporating person-level weight, strata, primary sampling unit, and personal identifier (due to repeated measures).
RESULTS
This study includes 22,511 children with 35,927 records (1 or 2 annual records per child). Table 1 summarizes the characteristics of the study sample at the child level. About half were boys (51.0%) and 31.7% were aged 14–17years. Race/ethnicity was distributed as 56.4% white, followed by MH (14.8%), black (14.4%), Other Hispanic (7.0%), Other Asian (3.4%), Other (1.8%), AI/AN/NHPI (1.3%), and Filipino (1.0%). At home, use of a language other than English was reported by 17.3% of the children. Geographically, 37.2% of the children lived in the South and 16.8% of children lived in the Northeast of the United States. For health and behavior variables, 13.1% reported having asthma, 13.6% reported having behavioral problems, and 7.0% reported less healthy than other children. For family structure, 69.4% of the children lived with both parents and 27.8% lived with a single parent.
Table 1.
Summary of Characteristics of the Study Sample at the Child Level
| Total | ||
|---|---|---|
| Variable | Unweighted N | Weighted % (SE) |
| Sociodemographic variable | ||
| Age | ||
| 6–13years | 15,815 | 68.3 (0.4) |
| 14–17years | 6696 | 31.7 (0.4) |
| Sex | ||
| Boy | 11,524 | 51.0 (0.5) |
| Girl | 10,987 | 49.0 (0.5) |
| Race/ethnicity | ||
| White | 7342 | 56.4 (1.3) |
| Black | 4992 | 14.4 (0.8) |
| Mexican Hispanic | 5762 | 14.8 (1.2) |
| Other Hispanic | 2415 | 7.0 (0.4) |
| Filipino | 275 | 1.0 (0.2) |
| Other Asians | 979 | 3.4 (0.2) |
| AI/AN/NHPI | 330 | 1.3 (0.3) |
| Other | 416 | 1.8 (0.2) |
| Highest education in family | ||
| ≤High school Some college | 9828 | 31.7 (0.9) |
| Some college | 6358 | 28.6 (0.6) |
| Bachelor’s | 3689 | 21.8 (0.7) |
| ≥Graduate | 2622 | 17.9 (0.8) |
| Income | ||
| Poor | 8815 | 25.0 (0.8) |
| Low | 4195 | 15.6 (0.4) |
| Middle | 5833 | 32.0 (0.7) |
| High | 3668 | 27.4 (0.9) |
| Insurance | ||
| Any private | 10,168 | 61.0 (1.0) |
| Public only | 10,666 | 32.4 (1.0) |
| Uninsured | 1677 | 6.6 (0.4) |
| Born in United States | ||
| No | 6522 | 17.3 (0.9) |
| Yes | 15,981 | 82.7 (0.9) |
| Language at home | ||
| Other | 1542 | 4.7 (0.2) |
| English | 20,952 | 95.3 (0.2) |
| Region | ||
| Northeast | 3347 | 16.8 (0.9) |
| Midwest | 4401 | 21.7 (0.9) |
| South | 8322 | 37.2 (1.1) |
| West | 6440 | 24.3 (1.0) |
| Health/behavior | ||
| Asthma | ||
| Yes | 2989 | 13.1 (0.3) |
| No | 19,522 | 86.9 (0.3) |
| Asthma medication | ||
| No asthma | 19,522 | 87.0 (0.3) |
| Both inhaler and preventive medicine | 1496 | 6.5 (0.2) |
| Inhaler only | 125 | 0.7 (0.1) |
| Preventive medicine only | 931 | 4.0 (0.2) |
| Neither inhaler nor preventive medicine | 417 | 1.8 (0.1) |
| ADHD | ||
| Yes | 2194 | 10.7 (0.4) |
| No | 20,314 | 89.3 (0.4) |
| Obesity | ||
| Normal | 13,771 | 83.1 (0.5) |
| Overweight | 2240 | 11.5 (0.4) |
| Obese | 1197 | 5.4 (0.2) |
| Behavioral problem | ||
| CIS< 15 | 19,636 | 86.4 (0.4) |
| CIS≥ 15 | 2875 | 13.6 (0.4) |
| Number of dental care visits, weighted mean (SE) | 22,511 | 1.38 (0.03) |
| Less healthy than other child | ||
| No | 20,720 | 93.0 (0.2) |
| Yes | 1776 | 7.0 (0.2) |
| Family structure variable | ||
| Family type Two-parent | ||
| Two-parent | 22,524 | 69.4 (0.8) |
| Single-parent | 12,236 | 27.9 (0.8) |
| No-parent | 1167 | 2.7 (0.2) |
| Family size | ||
| ≤4 | 18,632 | 58.2 (0.9) |
| >4 | 17,295 | 41.8 (0.9) |
| Number of elderly (≥65years), weighted mean (SE) | 35,927 | 0.05 (0.00) |
| Number of preschool children (≤5 years), weighted mean (SE) | 35,927 | 0.34 (0.01) |
| Number of adult age (≥18years) | ||
| 0–1 | 6255 | 15.0 (0.5) |
| 2 | 19,585 | 60.2 (0.7) |
| ≥3 | 10,087 | 24.8 (0.6) |
SE, standard error; AI, American Indian; AN, Alaskan Native; NHPI, Native Hawaiian and Pacific Islander; ADHD, attention-deficit hyperactivity disorder; CIS, Columbia Impairment Scale.
Table 2 presents percentages of chronic absenteeism by category per each variable. Overall, chronic absenteeism was 2.2%. Compared to 2.6% in whites, only 0.5% of Other Asians missed school more than 15days per year. Children with health issues were more often chronically absent than children without health issues: asthma (with 5.1% vs without 1.8%), ADHD (with 3.8% vs without 2.0%); behavioral problem (higher CIS 6.1% vs lower CIS 1.6%); and less than healthy than other children (Yes 10.1% vs No 1.6%). Children from single-parent homes (3.0%) or no-parent homes (3.4%) had higher rates of chronic absenteeism than children from 2-parent homes (1.8%). Children with low sociodemographic status showed higher rates of chronic absenteeism. For example, children from families with all their members having education level lower than a bachelor’s degree were more often absent from school than children from families with someone having a bachelor’s degree or higher. All variables were significantly associated with chronic absenteeism in univariable analysis except for sex, number of dental care visits, and the number of preschool children.
Table 2.
Weighted Percentage, Odds Ratio, and 95% Confidence Interval for Univariable and Multivariable Logistic Regression for Chronic Absenteeism
| Odds Ratio and 95% Confidence Interval | |||
|---|---|---|---|
| Variable | WD % (SE) | Univariable | Multivariable |
| Sociodemographic variable | |||
| Age | |||
| <14years | 1.7 (0.1) | Ref | Ref |
| ≥14years | 3.1 (0.3) | 1.80 (1.46–2.20)*** | 1.92 (1.55–2.37)*** |
| Sex | |||
| Boy | 2.1 (0.1) | Ref | |
| Girl | 2.3 (0.2) | 1.09 (0.90–1.34) | |
| Race/ethnicity White | 2.6 (0.2) | Ref | Ref |
| Black | 1.7 (0.3) | 0.64 (0.49–0.85) | 0.42 (0.31–0.57) |
| Mexican Hispanic | 1.4 (0.1) | 0.52 (0.40–0.67) | 0.53 (0.38–0.75) |
| Other Hispanic | 2.4 (0.3) | 0.91 (0.66–1.26) | 0.83 (0.58–1.19) |
| Filipino | 2.1 (1.1) | 0.82 (0.31–2.20) | 1.30 (0.46–3.67) |
| Other Asians | 0.5 (0.2) | 0.20 (0.08–0.51) | 0.30 (0.11–0.78) |
| AI/AN/NHPI | 3.5 (0.8) | 1.36 (0.78–2.37) | 1.02 (0.57–1.82) |
| Other | 2.1 (0.7) | 0.82 (0.44–1.53) | 0.85 (0.44–1.62) |
| Highest education in family | |||
| ≤High school | 2.6 (0.2) | 1.72 (1.16–2.53)** | |
| Some college | 2.4 (0.2) | 1.59 (1.07–2.36)* | |
| Bachelor’s | 1.8 (0.3) | 1.18 (0.76–1.84) | |
| ≥Graduate | 1.5 (0.3) | Ref | |
| Income | |||
| Poor | 3.1 (0.2) | 2.49 (1.82–3.41) | 2.27 (1.51–3.41) |
| Low | 2.4 (0.3) | 1.95 (1.38–2.77) | 1.92 (1.30–2.84) |
| Middle | 2.2 (0.2) | 1.77 (1.26–2.48) | 1.69 (1.19–2.40) |
| High | 1.3 (0.2) | Ref | Ref |
| Insurance | |||
| Any private | 1.8 (0.1) | Ref | Ref |
| Public only vs any private | 3.1 (0.2) | 1.74 (1.41–2.13)*** | 1.39 (1.04–1.87)* |
| Uninsured vs any private | 1.3 (0.4) | 0.74 (0.45–1.23) | 0.78 (0.45–1.36) |
| Born in the United States | |||
| No | 0.8 (0.2) | Ref | Ref |
| Yes | 2.3 (0.1) | 3.03 (1.73–5.29)*** | 1.93 (1.06–3.50)* |
| Language at home | |||
| Other | 1.2 (0.1) | ||
| English | 2.4 (0.1) | 2.01 (1.56–2.59)*** | 1.46 (1.05–2.02)* |
| Region | |||
| Northeast | 2.7 (0.4) | Ref | |
| Midwest | 2.7 (0.3) | 0.98 (0.72–1.34) | |
| South | 1.8 (0.2) | 0.65 (0.48–0.89)** | |
| West | 2.1 (0.2) | 0.75 (0.54–1.04) | |
| Health/behavior variable | |||
| Asthma/medication | |||
| No asthma | Ref | Ref | |
| Both inhaler and preventive medicine | 6.34 (4.36–9.26)*** | 4.05 (2.66–6.17)*** | |
| Inhaler only | 3.18 (2.15–4.71)*** | 2.14 (1.42–3.22)*** | |
| Preventive medicine only | 1.95 (0.91–4.17) | 1.62 (0.74–3.57) | |
| Neither inhaler nor preventive medicine | 2.06 (1.51–2.83)*** | 1.69 (1.23–2.34)** | |
| ADHD | |||
| No | 2.0 (0.1) | Ref | |
| Yes | 3.8 (0.4) | 1.95 (1.51–2.51)*** | |
| Obesity | |||
| Normal | 2.2 (0.1) | Ref | |
| Overweight | 2.5 (0.3) | 1.14 (0.84–1.55) | |
| Obese | 4.8 (0.8) | 2.26 (1.59–3.21)*** | |
| Behavioral problem | |||
| CIS< 15 | 1.6 (0.1) | Ref | Ref |
| CIS≥ 15 | 6.1 (0.5) | 4.01 (3.29–4.88)*** | 2.41 (1.91–3.05)*** |
| Number of dental care visits† | 1.53 (0.19) | 1.02 (0.97–1.08) | |
| Less healthy than other child | |||
| No | 1.6 (0.1) | Ref | Ref |
| Yes | 10.1 (0.8) | 6.82 (5.43–8.57)*** | 4.44 (3.36–5.87)*** |
| Family structure variable Family type | |||
| Two-parent | 1.8 (0.1) | Ref | |
| Single-parent | 3.0 (0.2) | 1.71 (1.39–2.09)*** | |
| No-parent | 3.4 (0.8) | 1.90 (1.21–2.99)** | |
| Family size | |||
| ≤4 | 2.5 (0.2) | Ref | Ref |
| >4 | 1.7 (0.2) | 0.67 (0.55–0.82)*** | 0.73 (0.59–0.90)** |
| Number of elderly† | 0.08 (0.01) | 1.44 (1.08–1.92)* | |
| Number of preschool children† | 0.31 (0.03) | 0.92 (0.79–1.08) | |
| Number of adult (≥18years) | |||
| 0–1 | 2.8 (0.3) | 1.47 (1.13–1.88)** | |
| 2 | 1.9 (0.1) | Ref | |
| ≥3 | 2.5 (0.2) | 1.29 (1.03–1.63)* | |
p<.05.
p<.01.
p<.001.
The weighted percentage is reported based on number of records. WD, weighted; SE, standard error; AI, American Indian; AN, Alaskan Native; NHPI, Native Hawaiian and Pacific Islander; ADHD, attention-deficit hyperactivity disorder; CIS, Columbia Impairment Scale. The c-statistic of the final model is 0.78. 0.2% of the data (N = 85) were not used for the final analysis due to missing values.
Weighted mean (SE).
Before conducting multivariable logistic regressions, we first investigated multicollinearity among the independent variables. None were highly correlated (r<.7) except for asthma status and asthma medication. Since asthma medication requires asthma status, to investigate the effect of asthma medications, we included asthma medication use (combined with the asthma indicator). To determine important predictors for chronic absenteeism, we implemented multivariable logistic regressions with a backward stepwise selection. The final model includes age, race/ethnicity, income, insurance, born in the United States, and language spoken at home as sociodemographic variables; asthma related medication use, behavioral problems, and less healthy than other child as health and behavior variables; and family size as a family variable. All are significant predictors for chronic absenteeism (Table 2).
Children aged 14years or older were more likely to be chronically absent than children aged less than 14years old (OR=1.92). Other Asians, blacks, and MHs were less likely to chronically miss school than whites (ORs=0.30, 0.42, and 0.53, respectively). Children who were born in the United States missed more school than those who were born elsewhere (OR=1.93) and children who speak English at home were more chronically absent than children who speak another language at home (OR=1.46). Children whose family income was in the middle, low, and poor categories were more likely to be chronically absent from school than children from high-income families (ORs=1.77, 1.95, and 2.49, respectively). Insurance type was also associated with chronic absenteeism: the odds of chronic absenteeism for children with only public health insurance were 1.39 times higher than those for the children with private health insurance. Children whose family size was greater than 4 were less likely to be chronically absent from school than children from smaller-sized families (OR=0.73). The goodness of fit of the final model was good (c-statistic= 0.78).
Asthmatic children who used both an inhaler and preventive medication, who used an inhaler only, and who did not use inhaler or preventive medicine were more likely to be chronically absent than children without asthma (ORs=4.05, 2.14, and 1.69, respectively). Children with behavioral problems (CIS score≥15) were more likely to chronically miss school (OR=2.41). Children who were less healthy than the other children were more often chronically absent from school (OR=4.44).
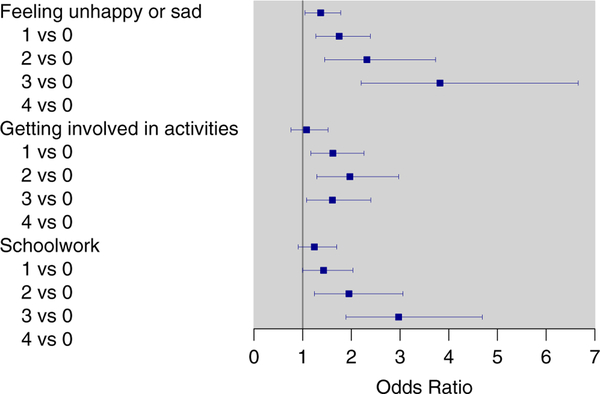
We also investigated the effects of individual CIS items on chronic absenteeism (Table 3). In the final multivariable logistic regression based on a backward selection, 3 of the 13 items were retained as significant items: problems in feeling unhappy or sad, getting involved in activities like sports or hobbies, and schoolwork. All the variables in the multivariable model in Table 2 were included except language spoken at home. Effects were similar to the model in strength and significance (not shown). Figure 1 illustrates the ORs and 95% CI of the 3 CIS items. Overall, the ORs for chronic absenteeism increase as score increases.
Figure 1.
Odds Ratios and 95% Confidence Intervals of Chronic Absenteeism for Columbia Impairment Scales Note. Higher score indicates a greater impairment (0= no problem, 4 = a very big problem). The model was adjusted for age, race/ethnicity, income, insurance, spoken language at home, asthma medication, less healthy than other child, and family size. The c-statistic was 0.79.
DISCUSSION
Chronic absenteeism among schoolchildren remains a pervasive challenge despite considerable efforts made to reduce it.27 This study identified important risk factors of chronic absenteeism including sociodemographic factors, children’s health and behavior, and family structure using the nationally representative MEPS data.
Of the sociodemographic variables, child’s age, race/ethnicity, income, insurance, birth country, and spoken language at home were associated with chronic absenteeism.Consistentwiththeliterature,1,28 the rate of absenteeism was higher among socioeconomically disadvantaged children, ie, lower income with public health insurance like Medicaid. Since low income often reflects challenges associated with poverty such as food insecurity, unstable housing, unreliable transportation and limited access to quality health care including oral health care,29 the school absences for students from low-income families are frequently tied to health problems such as asthma, dental problems, and learning disabilities. Since disparity in socio-economic status is a persistent problem, special programs are necessary to support socioeconomically disadvantaged students.
As several other studies also recognized,13,21,27 significant racial/ethnic differences were found in chronic absenteeism. Contradictory to other studies, ours showed a lower rate of chronic absenteeism among blacks and MHs compared to whites. One explanation for this discrepancy is that the question used to evaluate absenteeism, “missed school days due to illness or injury,” might not capture some important reasons for school absence such as violence or bullying. Studies have reported that black and MH parents are less likely to get involved school events.30 Low absenteeism among blacks and MHs might reflect the lower levels of parents’ involvement with school events or poor teacher-parent communication so the parents might not know whether their children missed school or were truant. In addition, consistent with the literature, we found that Other Asians have a lower rate of chronic absenteeism than whites; however, this result did not apply to Filipinos. This may be because Filipinos often travel to their home countries for extended vacations.31 Further studies are needed to elucidate how differences in cultural background and motivation affect the pattern of missing school.
Our study shows that children who are not born in the United States or speak a language other than English at home are less likely to be chronically absent. These children are often first- or second-generation immigrants. The low rate of chronic absenteeism among such children is not a novel finding. Studies have shown that English language learners (ELLs) are less likely to be chronically absent than nonELLs.27,28 ELLs are students who cannot communicate fluently or learn effectively in English because they come from non-English-speaking backgrounds. The reasons for lower absenteeism among ELLs are not clear; however, many immigrant children may be motivated to learn English to adjust to a new life in the United States so they do not miss school to fill the need. Further research is needed to identify the reasons for low absenteeism rate among ELLs and how the transition from ELLs to non-ELLs influences chronic absenteeism.
As expected, perceived child’s health was associated with chronical absenteeism; the highest OR occurred for children who are less healthy compared with their counterparts. Besides this finding, asthma medication and CIS also appear as important risk factors. Consistent with other studies, having asthma showed a positive association with chronic absenteeism. We observed dissimilar ORs of chronic absenteeism by asthma medication use. Compared to children who were never diagnosed asthma, asthmatic children both using inhaler and taking preventive medicine had the highest absenteeism rate, followed by asthmatic children who use an inhaler only followed by asthmatic children who did not use inhaler or take preventive medicine. The higher rate of chronic absenteeism among asthmatic children who used inhalers (either alone or combined with preventive medicine) is not unexpected. As noted by Moonie et al, the severity of asthma is positively associated with the number of missing school days8 and inhaler users can be deemed having more severe asthma. Failure to use an inhaler can increase the risk of more frequent episodes. However, compared to the chronic absenteeism rate of healthy children, the insignificantly different rate among children who used preventive medicine only, and the higher rate among asthmatic children who did not use inhaler or preventive medicine, are noteworthy. A potential contributing factor for these differences can be socioeconomic status. Low-income children are more likely to have asthma and miss school more days as a consequence.3 Since children with persistent asthma usually need to take daily preventive medication to control inflammation and prevent asthma symptoms, purchasing preventive asthma medications can be a huge burden for low-income families.32 The inability to access the needed asthma medication for low-income families becomes a serious public health issue.
Regarding child’s behavioral problem, to the best of our knowledge, there are no studies investigating the association between the CIS and chronic absenteeism. However, this significant association is not unexpected because behavioral or mental problems such as depression, anxiety, disruptive behavior, and substance use are recognized as risk factors of chronic absenteeism.3,15–17 These risk factors are associated with the individual CIS items found in the additional analysis result. The item “feeling unhappy or sad,” is a symptom of depression and the second item, “getting involved in activities,” also indicates depression or disruptive behavior.
Although family type, size, and number of elderly and adults were significant in univariable analysis, only family size remained in the final multivariable model. The insignificant result of family type is not astonishing because single-parent families, or families with old adults who do not economically contribute, are not in as a good financial condition as those with both parents.8,33 However, it is unclear why children who live in a larger family (size>4) were less likely to be chronically absent than those who live a smaller family (size≤4). We presume that more individuals in a family can provide more physical, emotional, or educational support to the children but further studies are needed to understand the dynamics of family function.
Limitations
The findings from this study should be interpreted in consideration of several limitations. First, the variables used in this study were based on parental reports. The recalled information may not reflect the true status for their children and produce biased results. Second, we could not account for other potential predictors (eg, bullying, environment) that were not available in the MEPS database. Recent studies showed electronic bullying and particular matter air pollution are associated with chronic absenteeism.34,35 Therefore, these potential risk factors should be considered to predict chronic absenteeism. Third, due to the small subgroup sizes, some races/ethnicities were combined to obtain more robust results. Although the combined ethnic groups are culturally and historically diverse, their absenteeism rates were similar. Fourth, about 9% of the sample was missing the outcome variable and those children were excluded from the analyses. A sensitivity analysis was performed using multiple imputation and the results were similar (not shown). Despite these limitations, our study has several strengths. The use of a nationally representative dataset allows the generalization of our findings to the entire US children population. In addition, the use of the CIS is another strength of our study because it is a reliable and valid tool to assess children’s global impairment.36 Our study also showed good reliability (Cronbach’s alpha= 0.90).
Conclusions
This study provides further evidence that lower socioeconomic status, asthma, and child’s behavioral problems contribute to chronic absenteeism. The identification of vulnerable children at risk for chronic absenteeism will help governments and educational professionals identify the barriers to academic achievement and develop integrated interventions or adjust educational policies to support disadvantaged children.
IMPLICATIONS FOR SCHOOL HEALTH
The finding that asthma and behavioral problems are associated with chronic absenteeism suggests several actions that can be taken at school to help reduce chronic absenteeism among K-12 students. First, each school should make an effort to develop and implement a systematic and coordinated management protocol for its asthmatic students. As suggested by the National Heart, Lung, and Blood Institute37 and Thornton et al,38 the protocol should contain a confidential list of asthmatic children, identified stimuli or triggers causing or worsening asthma and asthma medications the children take, and contact information. The protocol also should include an action plan for monitoring asthma, administering medications, and dealing with proper therapy for an early sign and emergency steps to a severe asthma episode. Because each student’s asthma can be different, however, the action plan must be specific to each student’s need developed by a physician, signed by a parent/guardian and the physician, and renewed every year. A strong partnership among parent(s)/guardian(s), physician, and the school will help improve attendance and the positive educational outcomes of students with asthma.
In addition, since an acute asthma attack can entail hospitalization or immediate medical attention,8 the protocol should include established procedures to make sure asthmatic students have easy access to asthma medicines or monitor adherence to the medicines at school and school-sponsored activities, and during transportation to and from school and school events, especially for low socioeconomically disadvantaged children. A randomized controlled trial with school nurses who delivered prescribed asthma medicine to students with asthma and administered their asthma medication during school hours showed significant improvement in school outcomes including school attendance compared to the usual care group.39 These trial results highlight the importance of easy access to asthma medicines at school and medication adherence.
Second, school air quality should be examined frequently and regularly. A study found that unhealthy building conditions including poor ventilation, mold, vermin, and dust are associated with absenteeism.40 Thus, schools must monitor their air quality and inspect building structural problems, such as heating or air conditioning system issues. Schools can also take actions to improve ventilation by replacing and upgrading ventilation systems and frequently remove dusts from surfaces, carpets, blinds, curtains, etc.
Third, our study suggests that the CIS can be used as a potential predictor for chronic absenteeism. Based on student CIS, schools can assess the risk of potential behavioral problems of their students and provide counseling to those with high CIS. Furthermore, schools can take a comprehensive approach to create individual student action plans for the students with high CIS, communicate frequently among the students, their parents/guardians, teachers, and school counselors, to monitor and help motivate and improve their school attendance. The comprehensive action plan can include counseling, selection of interventions designed to reduce the behavioral issue identified by CIS, and better optimization of medication or pharmacotherapy if necessary.
Acknowledgments
This work was partially funded by U54MD007584, U54MD007601, P20GM103466, andU54GM104944 grant fromNational Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent official views of NIH. The authors thankMs.Munirih Taafaki for reviewing and editing themanuscript.
Footnotes
Human Subjects Approval Statement
All procedures of this study were approved by the Institutional Review Board (IRB) of the University of Hawaii at Manoa (#2018-00214).
REFERENCES
- 1.Belfanz R, Byrnes V. The importance of being in school: a report on absenteeism in the nation’s public schools. Baltmore, MD: Johns Hopkins University Center for Social Organization of Schools; 2012. Available at: http://www.everystudentpresent.org/application/files/6114/8787/9522/Balfanz_2012_Importance_of_being_in_school.pdf. Accessed March 1, 2018. [Google Scholar]
- 2.Robert Wood Johnson Foundation. The relationship between school attendance and health; 2016. Available at: http://www.rwjf.org/en/library/research/2016/09/the-relationshipbetween-school-attendance-and-health.html. Accessed March 1, 2018.
- 3.Henderson T, Hill C, Norton K. The connection between missing school and health: a review of chronic absenteeism and student health in Oregon; 2014. Available at: http://www.attendanceworks.org/wordpress/wp-content/uploads/2014/10/Chronic-Absence-and-Health-Review-10.8.14-FINALREVISED.pdf Accessed March 1, 2018.
- 4.Weitzman M, Klerman LV, Lamb G, Menary J, Alpert JJ. School absence: a problem for the pediatrician. Pediatrics. 1982;69(6):739–746. [PubMed] [Google Scholar]
- 5.Tsakiris A, Iordanidou M, Paraskakis E, et al. The presence of asthma, the use of inhaled steroids, and parental education level affect school performance in children. Biomed Res Int. 2013;2013:762805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mizan SS, Shendell DG, Rhoads GG. Absence, extended absence, and repeat tardiness related to asthma status among elementary school children. J Asthma. 2011;48(3):228–234. [DOI] [PubMed] [Google Scholar]
- 7.Bener A, Abdulrazzaq YM, Debuse P, Abdin AH. Asthmaand wheezing as the cause of school absence. J Asthma. 1994;31(2):93–98. [DOI] [PubMed] [Google Scholar]
- 8.Moonie SA, Sterling DA, Figgs L, Castro M. Asthma status and severity affects missed school days. J Sch Health. 2006;76(1):1824. [DOI] [PubMed] [Google Scholar]
- 9.Bonilla S, Kehl S, Kwong KY, Morphew T, Kachru R, Jones CA. School absenteeism in children with asthma in a Los Angeles inner city school. J Pediatr. 2005;147(6):802–806. [DOI] [PubMed] [Google Scholar]
- 10.Pan L, Sherry B, Park S, Blanck HM. The association of obesity and school absenteeism attributed to illness or injury among adolescents in the United States, 2009. J Adolesc Health. 2013;52(1):64–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Echeverria SE, Velez-Valle E, Janevic T, Prystowsky A. The role of poverty status and obesity on school attendance in the United States. J Adolesc Health. 2014;55(3):402–407. [DOI] [PubMed] [Google Scholar]
- 12.Geier AB, Foster GD, Womble LG, et al. The relationship between relative weight and school attendance among elementary schoolchildren. Obesity (Silver Spring). 2007;15(8):21572161. [DOI] [PubMed] [Google Scholar]
- 13.Rappaport EB, Daskalakis C, Andrel J. Obesity and other predictors of absenteeism in Philadelphia school children. J Sch Health. 2011;81(6):341–344. [DOI] [PubMed] [Google Scholar]
- 14.Classi P, Milton D, Ward S, Sarsour K, Johnston J. Social and emotional difficulties in children with ADHD and the impact on school attendance and healthcare utilization. Child Adolesc Psychiatry Ment Health. 2012;6(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Basch CE. Healthier students are better learners: a missing link in school reforms to close the achievement gap. J Sch Health. 2011;81(10):593–598. [DOI] [PubMed] [Google Scholar]
- 16.Engberg J, Morral AR. Reducing substance use improves adolescents’ school attendance. Addiction. 2006;101(12):17411751. [DOI] [PubMed] [Google Scholar]
- 17.Wood JJ, Lynne SD, Langer DA, et al. School attendance problems and youth psychopathology: structural cross-lagged regression models in three longitudinal datasets. Child Dev. 2012;83(1):351–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pourat N, Nicholson G. Unaffordable dental care is linked to frequent school absences. Los Angeles, CA: UCLA Center for Health Policy Research; 2009. Available at: https://escholarship.org/uc/item/14g1w8sy Accessed March 1, 2018. [PubMed] [Google Scholar]
- 19.Ferrell RT. The Effects of Single-Parent Households Versus Two-Parent Households on Student Academic Success, Attendance, and Suspensions [dissertation]. St. Charles, MO: Lindenwood University; 2009. [Google Scholar]
- 20.Tamiru D, Belachew T. The association of food insecurity and school absenteeism: systematic review. Agric Food Secur. 2017;6(1):5. [Google Scholar]
- 21.Kaul G Chronic absence is the most important education problem in Minnesota that no one is talking about. MINNPOST. March 14, 2017. Available at: https://www.minnpost.com/education/2017/03/chronic-absence-mostimportant-education-problem-minnesota-no-one-talkingabout. Accessed March 1, 2018. [Google Scholar]
- 22.Chen J, Gee GC, Spencer MS, Danziger SH, Takeuchi DT. Perceived social standing among Asian immigrants in the U.S.: do reasons for immigration matter? Soc Sci Res. 2009;38(4):858869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim W, Keefe RH. Barriers to healthcare among Asian Americans. Soc Work Public Health. 2010;25(3):286–295. [DOI] [PubMed] [Google Scholar]
- 24.Gotay CC, Lipscomb J. Data for cancer outcomes research: identifying and strengthening the empirical base In: Lipscomb J, Gotay CC, Snyder C, eds. Outcomes Assessment in Cancer: Measures, Methods, and Applications. Cambridge, UK: Cambridge University Press; 2005:522–549. [Google Scholar]
- 25.Singer JB, Eack SM, Greeno CM. The Columbia Impairment Scale: factor analysis using a community mental health sample. Res Soc Work Pract. 2010;21(4):458–468. [Google Scholar]
- 26.Bird HR, Andrews H, Schwab-Stone M, et al. Global measures of impairment for epidemiologic and clinical use with children and adolescents. Int J Methods Psychiatr Res. 1996;6(4):295–307. [Google Scholar]
- 27.U. S. Department of Education. Chronic absenteeism in the nations’ schools: an unprecedented look at a hidden education crisis; 2016. Available at: https://www2.ed.gov/datastory/chronicabsenteeism.html Accessed March 1, 2018.
- 28.Romero M, Lee Y-S. The influence of maternal and family risk on chronic absenteeism in early schooling. New York, NY: National Center for Children in Poverty; 2008. Available at: https://eric.ed.gov/?id=ED522733. Accessed March 1, 2018. [Google Scholar]
- 29.Chang HN, Daivs R. Mapping the early attendence gap: charting a course for school success. San Francisco, CA: Attendance Works; 2015. Available at: https://eric.ed.gov/?id=ED580365. Accessed March 1, 2018. [Google Scholar]
- 30.Noel A, Stark P, Redford J. Parent and family involvement in education, from the National Household Education Surveys Program of 2012. First Look NCES 2013–028. Jessup, MD: National Center for Education Statistics; 2013. Available at: https://eric.ed.gov/?id=ED544174 Accessed March 1, 2018. [Google Scholar]
- 31.Olagundoye SS, Erbstein N. Chronic absense research brief series: chronic absenteeism in SCUSD: 2016–2017. Davis, CA: Center for Regional Change University of California at Davis; 2017. Available at: https://regionalchange.ucdavis.edu/sites/g/files/dgvnsk986/files/inline-files/Brief%201%20FINAL.pdf. Accessed March 1, 2018. [Google Scholar]
- 32.Ungar WJ, MacDonald T, Cousins M. Better breathing or better living? A qualitative analysis of the impact of asthma medication acquisition on standard of living and quality of life in low-income families of children with asthma. J Pediatr Health Care. 2005;19(6):354–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee SM, Kushner J. Single-parent families: the role of parent’s and child’s gender on academic achievement. Gender Educ. 2008;20(6):607–621. [Google Scholar]
- 34.Grinshteyn E, Yang YT. The association bewteen electronic bullying and school absenteeism among high school students in the United States. J Sch Health. 2017;87(2):142–149. [DOI] [PubMed] [Google Scholar]
- 35.MacNaughton P, Eitland E, Kloog I, Schwartz J, Allen J. Impact of particulate matter exposure and surrounding “greenness” on chronic absenteeism in Massachusetts public schools. Int J Environ Res Public Health. 2017;14(2):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zielinski K, Wood JJ, Renno P, Whitham S, Sterling L. Examining the validity of the Columbia Impairment Scale for assessing level of functioning in youth with autism spectrum disorder. J Child Adolesc Psychopharmacol. 2014;24(9): 509–512. [DOI] [PubMed] [Google Scholar]
- 37.National Heart, Lung, and Blood Institute. Managing asthma: a guide for schools. NIH Publication No. 14–2650; Updated December 2014. Available at: https://www.nhlbi.nih.gov/files/docs/resources/lung/NACI_ManagingAsthma-508%20FINAL.pdf Accessed March 1, 2018. [Google Scholar]
- 38.Thornton E, Kennedy S, Hayes-Watson C, et al. Adapting and implementing an evidence-based asthma counseling intervention for resource-poor populations. J Asthma. 2016;53(8):825834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Halterman JS, Szilagyi PG, Fisher SG, et al. Randomized controlled trial to improve care for urban children with asthma. Arch Pediatr Adolesc Med. 2011;165(3):262–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Simons E, Hwang S-A, Fitzgerald EF, Kielb C, Lin S. The impact of school building conditions on student absenteeism in upstate New York. Am J Public Health. 2010;100(9):1679–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]