Abstract
PURPOSE:
Patients make treatment decisions based not only on what they want, but what they think their families want. Discordance in such perceived preferences may therefore pose challenges for advance care planning. This study examines discordance in preference for life-extending care versus comfort-focused care and its association with do-not-resuscitate (DNR) order placement.
METHODS:
One hundred eighty-nine patients with advanced cancers refractory to at least one chemotherapy regimen were enrolled in a multisite observational study. In structured interviews, patients reported their preference for treatment maximizing either life extension or comfort; patients also indicated their perception of their families’ preference. DNR placement was reported by patients and verified using medical records.
RESULTS:
Approximately 23% of patients (n = 43) perceived discordance between their preference and their families’ preference. Patients who perceived discordance were less likely to have completed a DNR compared with those who perceived concordance, even after controlling for relevant confounds (odds ratio = .35; P = .02). Subgroups of discordance and concordance showed varying DNR placement rates (χ2, 19.95; P < .001). DNR placement rate was lowest among discordant subgroups, where there was either a personal (26.7%; four of 15) or family preference for comfort care (28.6%; eight of 28), followed by patients who perceived concordance for wanting life-extending care (34.5%; 29 of 84) and by patients who perceived concordance in wanting comfort-focused care (66.1%; 41 of 62).
CONCLUSION:
Many patients may perceive discordance between personal and family treatment preferences, posing impediments to advance care planning. Such patients may benefit from additional decision support.
INTRODUCTION
Among patients with advanced cancer, advance care planning is critical for ensuring preference-consistent care.1-3 As patients’ planning for future care is driven by not only what patients want, but what they think their families want,4-6 patients who perceive discordant preferences may face challenges in advance care planning.7-9 Perceiving conflicting preferences with family would generate more uncertainty for patients regarding what care outcomes to strive for or what plans to make.10,11 Discordance could therefore be paralyzing for care planning, resulting in no action or delayed action. In contrast, perceiving family as holding concordant preferences may provide greater confidence to proceed with making care plans.
To date, there has been little research examining whether patient perception of discordant preferences is associated with a lower likelihood of advance care planning. Such research would be critical for identifying at-risk patients and a modifiable target for intervention. Specifically, examination of patients’ perceptions is important, as such perceptions of family preferences may not match true family preferences8 but are nevertheless central to the internal decision and planning processes of the patient and thus ripe for intervention.
This study examines discordance between patients and their family caregivers in preferences for life-extending care versus comfort-focused care and its association with do-not-resuscitate (DNR) order placement. The preference of prioritizing comfort as the primary goal of treatment is fundamental to guiding care choices in patients with cancer who are nearing death and has been shown to be predictive of actual care outcomes—for example, aggressive care at end of life.12,13 DNR orders are a critical form of advance care planning as they can help to ensure that patients receive care at the end of life in more preference-consistent ways.14,15 Thus, this study examines whether a perception by patients of discordant preferences for a fundamental priority guiding treatment decisions is associated with completion of a concrete step toward planning future care.
METHODS
The current study used data from the Coping With Cancer-II study, a multi-institution, longitudinal, observational study that was conducted from 2010 to 2015 to examine end-of-life communication among patients with advanced cancer. Participating sites included the Weill Cornell Medicine Meyer Cancer Center (New York, NY); Memorial Sloan Kettering Cancer Center (New York, NY); Dana-Farber/Harvard Cancer Center (Brigham and Women’s Hospital, Dana-Farber Cancer Institute, and Massachusetts General Hospital, Boston, MA); Yale Cancer Center (New Haven, CT); Virginia Commonwealth University Massey Cancer Center (Richmond, VA); Simmons Comprehensive Cancer Center (Dallas, TX); Parkland Hospital (Dallas, TX); University of New Mexico Cancer Center (Albuquerque, NM); and Pomona Valley Hospital Medical Center (Pomona, CA). Institutional review boards at all participating sites approved the study protocol and all participants provided written informed consent.
Eligibility criteria for the study included being of black or white race; age 21 years or older; having locally advanced and/or metastatic GI, lung, or gynecologic cancer; disease progression after one or more chemotherapy regimens; and oncologist-estimated life expectancy of 6 or fewer months. Exclusion criteria included cognitive impairment, being too weak to participate in study interviews, or receipt of hospice or specialty palliative care.
The analytic sample used in the current study includes 189 participants who provided valid responses for items that assessed perceived personal and family treatment preferences and DNR placement. These were assessed during the postscan assessment of the parent study. The parent study enrolled 386 patients at baseline for whom valid data were available for 189 patients as a result of loss of participants to follow-up or missing data on study items. Comparing the analytic sample with those patients who were excluded did not show statistically significant differences in age, gender, education, marital status, race, ethnicity, or diagnosis type.
At study entry, we recorded patient demographics and disease characteristics. Data on study variables were collected during structured interviews carried out by trained interviewers. To assess personal treatment preference, participants were asked the following question used in many previous large studies:12,13 “If you could choose, would you prefer: a course of treatment that focused on extending life as much as possible, even if it meant more pain and discomfort; or a plan of care that focused on relieving pain and discomfort as much as possible, even if that meant not living as long?” To assess perceived family preference, the same question was asked with the beginning of the question modified: “If you had to choose your family’s preferences for your treatment, do you think they would prefer that you pursue...” Response options were coded as indicating a care preference for maximizing life extension or comfort. If patients reported their preferences to be same as those of their families, they were considered concordant, and if different, discordant. DNR placement was assessed by asking participants if they had a DNR order on file, and this self-report measure was confirmed by DNR orders that were identified in the medical record. Response options were coded 0 (no) or 1 (yes).
Analytic Plan
We used descriptive statistics to compare the relative distribution of perceived personal and family preferences among the sample. We used odds ratio to assess whether patients perceiving discordance were more likely to have DNR placement compared with patients perceiving concordance (P < .05 considered significant). To control for potential confounding influences, a logistic regression model was computed predicting DNR placement in which perceived discordance was tested as a predictor alongside control variables. Control variables included those sociodemographic and patient characteristics that showed significant or marginally significant bivariable associations with DNR placement (P < .10). These included years of education, age, marital status, insurance status, race, and geographic region of data collection.
RESULTS
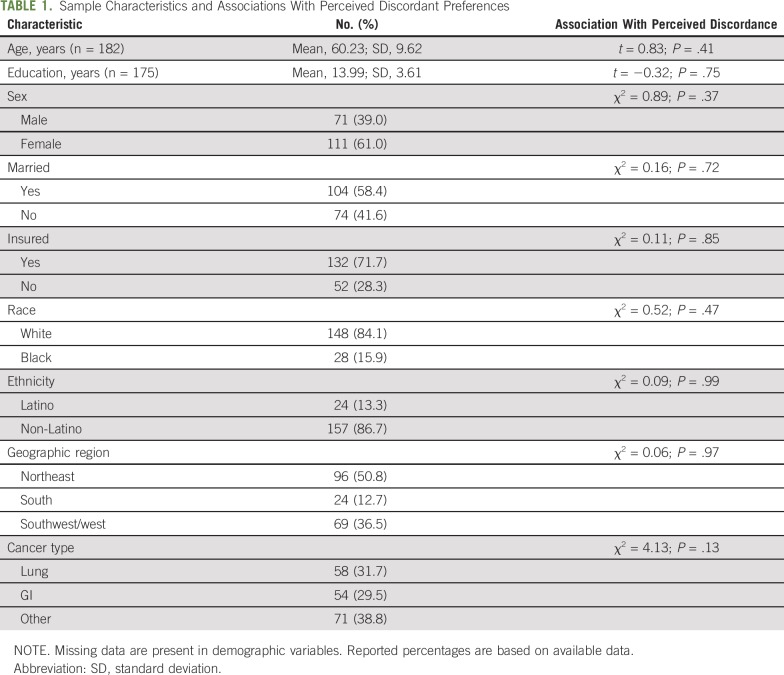
Sample characteristics are listed in Table 1. Participants on average were approximately age 60 years and had some college education. The majority were women (61%), married (58.4%), insured (71.7%), white (84.1%), and non-Latino (86.7%).
TABLE 1.
Sample Characteristics and Associations With Perceived Discordant Preferences
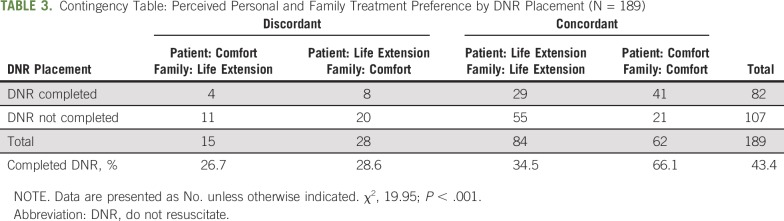
The distribution of perceived patient and family preference and their combinations are listed in Table 2. We found that 7.9% of patients preferred comfort-focused care but perceived their families to hold a discordant preference for life-extending care; 14.8% showed an opposite pattern where they preferred life-extending care but perceived their families to hold a discordant preference for comfort-focused care. In contrast, 32.8% of patients showed concordance between themselves and their families in preferring comfort-focused care, whereas 44.4% showed concordance preferring life-extending care.
TABLE 2.
Contingency Table: Perceived Personal and Family Preference for Comfort-Focused Versus Life-Extending Care (N = 189)
A total of 22.7% of patients (n = 43) perceived discordance between what they wanted and what their families wanted for care. Patients who perceived discordance did not differ from those who perceived concordance on demographics or other patient characteristics (Table 1). However, patients who perceived discordance were less likely to have completed a DNR versus those who perceived concordance (odds ratio, 0.42; P = .02). This association held even after controlling for confounds, such as years of education, age, marital status, insurance status, race, and site of data collection (adjusted odds ratio = 0.35; P = .02).
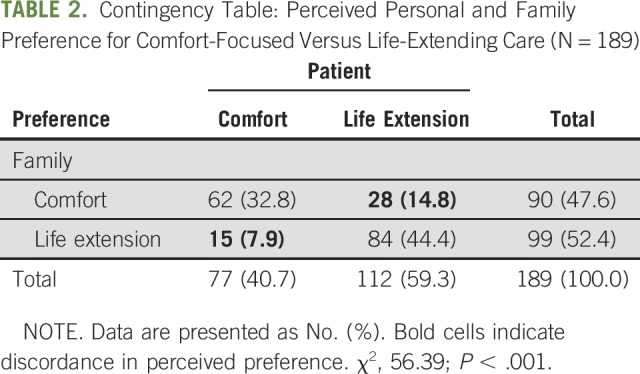
Examining subgroups of discordance and concordance demonstrated that DNR placement rates varied across subgroups (χ2, 19.95; P < .001; Table 3). DNR placement rates were lowest among patients who preferred comfort-focused care but who perceived their families to prefer life-extending care (26.7%; four of 15). This group was followed by patients who preferred life-extending care but who perceived their families to prefer comfort-focused care (28.6%; eight of 28). Next were patients who perceived agreement on preferring life-extending care over comfort care (34.5%; 29 of 84). Finally, patients who perceived agreement on preferring comfort-focused care over life-extending care had the highest rates of DNR placement (66.1%; 41 of 62).
TABLE 3.
Contingency Table: Perceived Personal and Family Treatment Preference by DNR Placement (N = 189)
DISCUSSION
This study examined perceived discordance in personal and family treatment preferences and its association with DNR order placement. A substantial number of patients—approximately 23%—perceived their families’ preference for life-extending care to be different from their own. Furthermore, this perception of discordance was associated with a lower likelihood of DNR placement relative to patients who perceived concordance, even after controlling for confounds. Results were thus consistent with the notion that patients who perceive their families to hold preferences different from their own may face impediments to their advance care planning.10
Examination of subgroups of discordant and concordant preferences further supported the notion that perceiving conflicting preferences may hinder advance care planning.16,17 DNR placement rates varied significantly among the subgroups in the following order: patient prefers comfort, but family prefers life extension (26.7%); patient prefers life extension, but family prefers comfort (28.6%); patient and family prefer life extension (34.5%); and patient and family prefer comfort (66.1%). Of note, DNR placement was lowest among patients who preferred comfort-focused care but perceived their families to have a conflicting preference for life-extending care. In addition, it is particularly noteworthy that DNR placement was not lowest among patients holding both a personal and family preference for life-extending care. Rather, DNR placement rate was lowest in the two discordant subgroups. These results suggest the possibility that discordance may have a paralyzing effect on advance care planning, whereas concordance may facilitate planning.16,17
The relative prevalence of the four subgroups of concordance and discordance among the sample was also informative. The largest group consisted of patients who perceived both themselves and their families to prefer life-extending care over comfort care (44.4%). This is not surprising and is consistent with the rallying phenomenon often observed whereby the family rallies behind the patient in fighting the illness and preserving life, despite worse pain or discomfort. Approximately 8% of the sample felt that they wanted to prioritize comfort but that their families would prefer life extension. This too is consistent with clinical observations whereby some patients report that they pursue aggressive anticancer and life-extending treatments not for themselves but for their families. What was surprising, however, was that there were almost twice as many patients—approximately 15%—who preferred prioritizing extending their lives as much as possible, but who perceived their families to prefer prioritizing comfort, even if they may not live as long. Such a dynamic is less commonly mentioned in clinical anecdotes. Social dynamics wherein patients view their family as not as interested as they are in extending their life as much as possible may make this difference in preference particularly difficult to openly discuss. Such patients may question their family members’ motives and concern for them. These patients may thus represent an underattended group that should be further studied in future research.
It is important to note that, as a cross-sectional study design, it is possible that the direction of causality between variables is the opposite of that presumed here. That is, it is possible that DNR placement led to more concordant treatment preferences. Advance care planning is often seen as a vehicle that facilitates care preference discussions between patients and their families. It is possible therefore that the DNR placement decision was based on a family discussion or stimulated a subsequent family discussion, which allowed patients to resolve any perceived discordant preferences to be concordant.
The cross-sectional and observational design of this study poses some other limitations as well, including confounding explanations. For example, it is possible that the perception of discordance may reflect other patient or family factors—for example, family cohesiveness or functioning—that, in turn, may influence advance care planning.17,18 Future research using longitudinal designs and examining the broader family unit and its functioning would be useful to rule out these alternate explanations. An additional limitation of this study is that the sample was relatively homogenous in terms of race and ethnicity, and, therefore, future research that examines more diverse samples will be beneficial. Finally, the broad assessment of treatment preference—as prioritizing life extension versus comfort—could be a limitation. As patients’ general preferences for life-extending care versus comfort-focused care may not match their preferences for specific interventions (eg, cardiopulmonary resuscitation), future research assessing specific intervention preferences as well may be beneficial.
The findings of the current study have direct clinical relevance. With professional bodies mandating, or strongly recommending, advance care planning discussions, routine clinical assessments and discussions of care preferences are being implemented.1-3 The current results suggest that, during such discussions, it is important to not only assess patients’ preferences, but also whether patients perceive any discrepancies between what they want and what their family wants. If such discrepancies are present, those patients may benefit from additional support around decisions and care planning.10 Clinicians could openly discuss the perceived discrepancies, helping patients to identify ways in which to reconcile preferences and better prepare to make advance care plans. Clinicians openly discussing discordant preferences may empower patients to have similar discussions with their families—regarding what may be a taboo topic—facilitating the identification of care goals and advance care plans.
Footnotes
Supported by the National Cancer Institute Grants No. CA106370, CA197730, P30-CA008748, and T32CA009461.
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Financial support: Holly G. Prigerson
Administrative support: Holly G. Prigerson
Provision of study materials or patients: Holly G. Prigerson
Collection and assembly of data: Holly G. Prigerson
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
“My Family Wants Something Different”: Discordance in Perceived Personal and Family Treatment Preference and Its Association With Do-Not-Resuscitate Order Placement
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jop/site/ifc.
Login S. George
Employment: Walgreens (I)
William Breitbart
Honoraria: Novartis
Consulting or Advisory Role: Novartis
No other potential conflicts of interest were reported.
REFERENCES
- 1.Walling A, Lorenz KA, Dy SM, et al. Evidence-based recommendations for information and care planning in cancer care. J Clin Oncol. 2008;26:3896–3902. doi: 10.1200/JCO.2007.15.9509. [DOI] [PubMed] [Google Scholar]
- 2.Von Roenn JH. Advance care planning: Ensuring that the patient’s voice is heard. J Clin Oncol. 2013;31:663–664. doi: 10.1200/JCO.2012.46.8181. [DOI] [PubMed] [Google Scholar]
- 3.Narang AK, Wright AA, Nicholas LH. Trends in advance care planning in patients with cancer: Results from a national longitudinal survey. JAMA Oncol. 2015;1:601–608. doi: 10.1001/jamaoncol.2015.1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kutner JS, Vu KO, Prindiville SA, et al. Patient age and cancer treatment decisions. Patient and physician views. Cancer Pract. 2000;8:114–119. doi: 10.1046/j.1523-5394.2000.83004.x. [DOI] [PubMed] [Google Scholar]
- 5.Schäfer C, Putnik K, Dietl B, et al. Medical decision-making of the patient in the context of the family: Results of a survey. Support Care Cancer. 2006;14:952–959. doi: 10.1007/s00520-006-0025-x. [DOI] [PubMed] [Google Scholar]
- 6.Mead EL, Doorenbos AZ, Javid SH, et al. Shared decision-making for cancer care among racial and ethnic minorities: A systematic review. Am J Public Health. 2013;103:e15–e29. doi: 10.2105/AJPH.2013.301631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shin DW, Cho J, Roter DL, et al. Preferences for and experiences of family involvement in cancer treatment decision-making: Patient-caregiver dyads study. Psychooncology. 2013;22:2624–2631. doi: 10.1002/pon.3339. [DOI] [PubMed] [Google Scholar]
- 8.Shin DW, Cho J, Kim SY, et al. Discordance among patient preferences, caregiver preferences, and caregiver predictions of patient preferences regarding disclosure of terminal status and end-of-life choices. Psychooncology. 2015;24:212–219. doi: 10.1002/pon.3631. [DOI] [PubMed] [Google Scholar]
- 9.Tang ST, Liu T-W, Lai M-S, et al. Concordance of preferences for end-of-life care between terminally ill cancer patients and their family caregivers in Taiwan. J Pain Symptom Manage. 2005;30:510–518. doi: 10.1016/j.jpainsymman.2005.05.019. [DOI] [PubMed] [Google Scholar]
- 10.LeBlanc A, Kenny DA, O’Connor AM, et al. Decisional conflict in patients and their physicians: A dyadic approach to shared decision making. Med Decis Making. 2009;29:61–68. doi: 10.1177/0272989X08327067. [DOI] [PubMed] [Google Scholar]
- 11.O’Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15:25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 12.Weeks JC, Cook EF, O’Day SJ, et al. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA. 1998;279:1709–1714. doi: 10.1001/jama.279.21.1709. [DOI] [PubMed] [Google Scholar]
- 13.Wright AA, Mack JW, Kritek PA, et al. Influence of patients’ preferences and treatment site on cancer patients’ end-of-life care. Cancer. 2010;116:4656–4663. doi: 10.1002/cncr.25217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brinkman-Stoppelenburg A, Rietjens JA, van der Heide A. The effects of advance care planning on end-of-life care: A systematic review. Palliat Med. 2014;28:1000–1025. doi: 10.1177/0269216314526272. [DOI] [PubMed] [Google Scholar]
- 15.Garrido MM, Balboni TA, Maciejewski PK, et al. Quality of life and cost of care at the end of life: The role of advance directives. J Pain Symptom Manage. 2015;49:828–835. doi: 10.1016/j.jpainsymman.2014.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Winter L, Parks SM. Family discord and proxy decision makers’ end-of-life treatment decisions. J Palliat Med. 2008;11:1109–1114. doi: 10.1089/jpm.2008.0039. [DOI] [PubMed] [Google Scholar]
- 17.Parks SM, Winter L, Santana AJ, et al. Family factors in end-of-life decision-making: Family conflict and proxy relationship. J Palliat Med. 2011;14:179–184. doi: 10.1089/jpm.2010.0353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yun YH, You CH, Lee JS, et al. Understanding disparities in aggressive care preferences between patients with terminal illness and their family members. J Pain Symptom Manage. 2006;31:513–521. doi: 10.1016/j.jpainsymman.2005.11.009. [DOI] [PubMed] [Google Scholar]