Abstract
Objective
To assess how staff attitudes before, during, and after implementation of a real-time location system (RTLS) that uses radio-frequency identification tags on staff and patient identification badges and on equipment affected staff’s intention to use and actual use of an RTLS.
Participants and Methods
A series of 3 online surveys were sent to staff at an emergency department with plans to implement an RTLS between June 1, 2015, and November 29, 2016. Each survey corresponded with a different phase of implementation: preimplementation, midimplementation, and postimplementation. Multiple logistic regression with backward elimination was used to assess the relationship between demographic variables, attitudes about RTLSs, and intention to use or actual use of an RTLS.
Results
Demographic variables were not associated with intention to use or actual use of the RTLS. Before implementation, poor perceptions about the technology’s usefulness and lack of trust in how employers would use tracking data were associated with weaker intentions to use the RTLS. During and after implementation, attitudes about the technology’s use, not issues related to autonomy and privacy, were associated with less use of the technology.
Conclusion
Real-time location systems have the potential to assess patterns of health care delivery that could be modified to reduce costs and improve the quality of care. Successful implementation, however, may hinge on how staff weighs attitudes and concerns about their autonomy and personal privacy with organizational goals. With the large investments required for new technology, serious consideration should be given to address staff attitudes about privacy and technology in order to assure successful implementation.
Abbreviations and Acronyms: ED, emergency department; RFID, radio-frequency identification; RTLS, real-time location system; TAM, technology acceptance model
Providing high-quality, evidence-based care in a safe and efficient manner is a ubiquitous challenge for health care professionals.1, 2, 3 With the complexity of care and costs increasing exponentially, health care systems are looking to other industries, such as manufacturing and courier delivery for technological solutions to reduce costs and improve safety and quality. Other industries have adopted real-time location systems (RTLSs) to reduce costs and improve efficiencies in the delivery of services. An RTLS uses a computerized location application that allows workers to visually locate and track equipment, movable goods, and employees that have been tagged with radio-frequency identification (RFID) or similar technologies. Real-time location system data also can be aggregated to identify strategies to improve safety, efficiency, and quality of services.4
Despite the potential for improving efficiency, patient safety, and health care quality,4,5 uptake of RTLSs in hospitals has been slow.6,7 Critics have suggested that in addition to cost, slow uptake and failed attempts to implement have been due to a limited and narrow focus on implementation, with more emphasis on how best to engineer a system into an existing organizational and physical structure and less on fitting the technology to the social environment, culture, policies, and legal requirements of the organization.6,8 Understanding factors documented in other settings to be critical for implementation success9,10 is not always straightforward, especially when individual attitudes and beliefs differ from institutional culture.11 Staff identification badges embedded with RFID, for example, can track the physical positions of staff in a specific area. Because of this, staff has to weigh their own personal privacy and autonomy concerns against organizational goals of patient safety and efficiency.5,12 If organizational culture or personal attitudes are not addressed, a new technology can disrupt a previously stable environment and create early resistance to implementation, sometimes in the form of recalcitrant (eg, not using or rarely using technology) or covert (eg, sabotaging) behaviors.5,13, 14, 15, 16, 17 Previous studies, for example, have described sabotage of technology by staff that included putting RFID tags in water to destroy them, hiding them in ceiling tiles or flower pots, or dismantling the RTLS.17 When facing a large investment in technology, assessing and addressing personal attitudes and beliefs about the technology and the organizational culture may help shape training protocols deemed critical to bolster RTLS implementation success in hospital settings.18
Because of the slow uptake and failed attempts of others to implement RTLSs, our objective was to assess staff attitudes and beliefs throughout the implementation of an RTLS into an emergency department (ED) of a large quaternary medical center and assess their correlation with intended and actual use of the technology, all with an eye toward potential interventions to improve technology adoption.
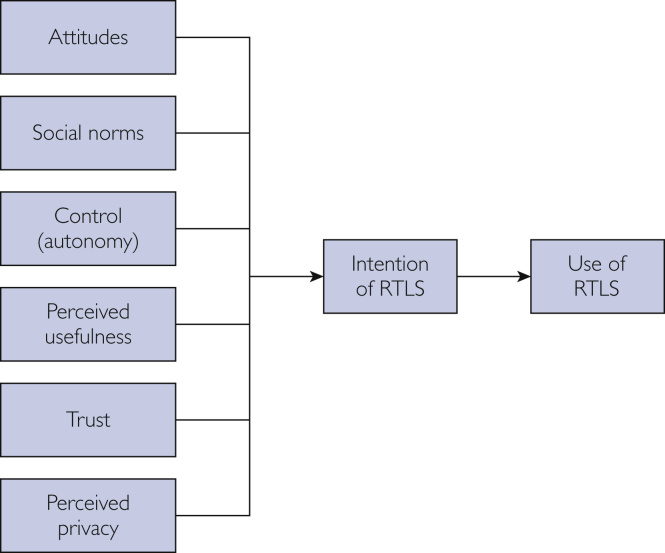
The Ajzen theory of planned behavior19,20 posits that engagement in a behavior can be explained by attitudes and beliefs about the behavior, the social norms of the behavior, and the perceived control over performing the behavior. The technology acceptance model (TAM and TAM2) extends the theory of planned behavior to examine factors, such as the perceived usefulness of the technology, associated with adopting new technologies.21, 22, 23 Given the inherent issues related to privacy and trust with RTLSs, we augmented the TAM to include additional questions about trust and privacy (Figure 1). We hypothesized that negative attitudes about the RTLS, weak coworker endorsement (social norms), lack of autonomy or control over RTLS use, low perceived usefulness, lack of trust about how location data would be used, and concerns about personal privacy would correlate with weaker intended and early RTLS use. We expected that a subgroup of participants would remain skeptical of the technology at each stage of implementation and that another subgroup would convert from having weak intention to use the RTLS to becoming active users of the technology.
Figure 1.
Hypothesized association between constructs from the theory of planned behavior, technology acceptance model, trust and privacy, and intention to use and actual use of the real-time location system.
Participants and Methods
Intervention Overview
In EDs, the unpredictability of patient flow and variability of patient conditions can cause unintended delays in care and increase the risks for patient morbidity and mortality and staff safety. An RTLS in the ED, therefore, may be especially useful for creating opportunities for efficiency and safety in care.24,25 For example, patient and staff tracking using the RTLS may reduce safety risks, avoid adverse events, and optimize patient flow if it is used as intended.26, 27, 28
A comprehensive RTLS implementation plan was developed, with emphasis on engaging multiple stakeholders, including administrative and physician leadership. Stakeholder engagement strategies included (1) early representation of stakeholders (eg, ED leadership, physicians, nurses, technicians) on an implementation advisory board that met throughout the planning and all implementation phases, (2) “town hall meetings” for all ED staff before implementation, (3) an email campaign before and early in the implementation that included frequently asked questions about the technology and its intended use, with repeated departmental leadership mention of the implementation’s strategic importance, and (4) on-site technical training with all staff before and during implementation, including the highly visible implementation team taking shifts and shadowing ED staff.
During implementation, RFID readers were installed throughout the ED. Key pieces of equipment were tagged. Staff assigned to the ED and patients had RFID chips embedded in their employee identification badges and patient wristbands, respectively. Once implemented, staff could visualize the locations of equipment, staff, and patients in the ED in real time via an encrypted Web-based application.
Study Overview
Three staff surveys were conducted at our academic level 1 trauma center ED, which has an annual patient volume of 75,000 patients. Surveys corresponded with the preimplementation, midimplementation, and postimplementation phases of RTLS. The Mayo Clinic Institutional Review Board reviewed this study and considered it to be “quality improvement.”
Survey
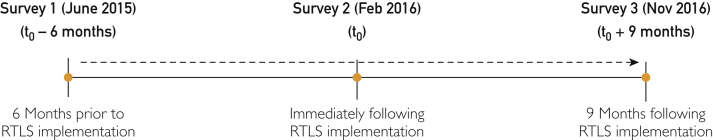
As shown in Figure 2, we administered a Web survey (Qualtrics) at 3 different time points: (1) 1 month after town hall meetings, which was approximately 6 months before RFID implementation (June 1, 2015), (2) immediately after implementing RFID into staff identification badges (February 16, 2016), and (3) 9 months after RFID implementation (November 29, 2016).
Figure 2.
Data collection flow before, during, and after implementation of real-time location system (RTLS).
For each time period, hyperlinks for the study questionnaire were sent to all current ED staff via email. Five days after the initial survey, an email reminder was sent to everyone on the distribution list. Ten days after the original email, a physician coinvestigator sent an email reminder. Finally, 17 days after the original email, a final reminder was sent. Surveys were sent to staff email addresses, but only the institution’s survey center could link email addresses with responses. Participants did not receive remuneration for participation.
The survey included questions about demographic characteristics and job classification and questions for each construct in the conceptual model (Table 1). Whenever possible, previously developed questions were used or revised.13,22,29 Although all 3 surveys had an identical core set of questions, the first survey was worded in anticipation of the implementation (eg, “Using RTLS will help me do my job better”). The second and third surveys were worded to assess their current state (eg, “Using RTLS helps me do my job better”). Response options were strongly agree, somewhat agree, neutral, somewhat disagree, and strongly disagree.
Table 1.
Survey Questions by Constructs in the Conceptual Model
| Construct | Question |
|---|---|
| Attitude | I like the idea of using RTLS |
| Social norms | Coworkers think RTLS is a good idea |
| Control | I have complete control over whether to use RTLS |
| I doubt my ability to use the data from RTLS | |
| Perceived usefulness | Using RTLS improves patient care |
| RTLS makes me more efficient in my work | |
| Using RTLS helps me do my job better | |
| Trust | Confident my employer will keep RTLS data in a secure manner |
| Confident my employer is taking measures to prevent unauthorized access to RTLS data | |
| Confident my employer will not use my personal information for other purposes | |
| Privacy | Comfortable disclosing personal information online (eg, online banking, Facebook, Instagram, etc) |
RTLS = real-time location system.
Intention to use the RTLS was assessed in the preimplementation survey with the following question: “I intend to use RTLS to help me on the job.” Actual use of the RTLS was assessed during and after implementation by asking, “I use RTLS to help me on the job.” Responses to questions were strongly agree, somewhat agree, neither agree nor disagree, somewhat disagree, or strongly disagree. Because we were interested in shifts toward positive responses over time, we recoded responses to all questions into either agree (strongly agree and somewhat agree) or neutral/disagree (neither agree nor or disagree, somewhat disagree, strongly disagree).
To test for discriminant validity, a question about comfort in disclosing personal information online, such as online banking or social media sites, was included. We assumed that while attitudes and beliefs about the RTLS may change throughout the implementation process, comfort in disclosing personal information likely would not change over time or as a result of RTLS implementation.
Participants
All ED staff, including physicians, nurses, residents, technicians, administrative and support staff, and others who support the ED and had the potential to use the RTLS after implementation, such as radiology technologists and phlebotomists, were sent the preimplementation survey. For the midimplementation and postimplementation surveys, all current ED personnel who had RFID technology embedded in their identification badge were included in the study sample.
Statistical Analyses
Analyses included fitting logistic regression models to describe the differences between staff characteristics and our outcomes—the intention to use and actual use of the RTLS. To examine differences in the associations between constructs in the conceptual model and intention or actual use of the RTLS, we fit all variables into a multivariate logistic regression model and then used backward elimination, with a cut point of P<.1, for the most parsimonious model.
Results
Survey Responses and Demographic Distribution
Nearly 56% of staff (314 of 564 [55.7%]) responded to at least one question on the preimplementation survey. For the midimplementation survey, 40.0% (236 of 592) responded to the survey, but 22 had either not yet received RFID-enabled badges or no longer worked in the ED, making them ineligible for analysis. For the postimplementation survey, 26.5% (157 of 592) responded, but 13 were either not current employees in the ED or did not have RFID-enabled badges. Final sample sizes for the surveys, therefore, were 314 (preimplementation), 214 (midimplementation), and 144 (postimplementation). Because of staff changes over time, each survey had a slightly different sample, and changes in independent and dependent variables at the individual level could not be tracked over time. No data were available for nonresponders, and therefore, we were not able to evaluate the potential for nonresponse bias.
Most of the respondents were women between the ages of 26 and 35 years, were nurses, and had worked less than 5 years at the institution. The proportion of respondents who either intended to use or used the RTLS significantly increased with each subsequent survey (P<.01). For the preimplementation survey, 60.2% (162 of 269) agreed or strongly agreed that they intended to use the RTLS. For the midimplementation and postimplementation surveys, 66.7% (142 of 213) and 79.2% (114 of 144), respectively, agreed or strongly agreed that they used the RTLS.
RTLS Intention and Actual Use by Demographic Characteristics
Before implementation, the intention to use the RTLS was not associated with any demographic characteristic, including job title (Table 2). However, during early implementation, compared with those with the most work experience at the study site (≥16 years), those with the least experience (<1 year) had higher odds of reporting actual use of the RTLS. After implementation, the odds of actual use of the RTLS did not differ by number of years working at the study site, but more women were likely to use the RTLS.
Table 2.
Logistic Regression Models of the Association of Demographic Characteristics With Self-Reported Intent or Actual Use of the Real-Time Location System in the Emergency Departmenta
| Variable | Preimplementation: intent to use, OR (95% CI) | Midimplementation: actual use, OR (95% CI) | Postimplementation: actual use, OR (95% CI) |
|---|---|---|---|
| Job | |||
| Otherb | 0.77 (0.35-1.71) | 0.49 (0.19-1.28) | 0.77 (0.24-2.38) |
| Nurse | 0.49 (0.21-1.12) | 0.88 (0.33-2.33) | 1.72 (0.47-6.30) |
| Physician | Reference | Reference | Reference |
| Years at institution | |||
| <1 | 1.11 (0.32-3.84) | 12.12 (1.14-128.45) | NA |
| 1-5 | 1.16 (0.44-3.03) | 2.21 (0.71-6.91) | 1.03 (0.24-4.40) |
| 6-10 | 1.19 (0.48-2.96) | 3.19 (0.94-10.83) | 1.30 (0.23-7.30) |
| 11-15 | 1.48 (0.55-3.94) | 1.92 (0.65-5.68) | 1.86 (0.44-7.77) |
| ≥16 | Reference | Reference | Reference |
| Age (y) | |||
| 18-25 | 1.94 (0.39-9.77) | 1.99 (0.16-24.51) | NA |
| 26-35 | 0.72 (0.24-2.19) | 1.16 (0.31-4.38) | 2.36 (0.38-14.72) |
| 36-45 | 1.34 (0.45-3.94) | 1.17 (0.35-3.87) | 1.44 (0.29-7.24) |
| 46-55 | 1.52 (0.57-4.09) | 1.29 (0.44-3.77) | 1.54 (0.34-6.93) |
| ≥56 | Reference | Reference | Reference |
| Sex | |||
| Female | 0.86 (0.46-1.62) | 1.28 (0.62-2.64) | 3.38 (1.36-8.40) |
| Male | Reference | Reference | Reference |
NA = not available; OR = odds ratio.
Included administrators/finance personnel, health unit coordinators, therapists and technicians, patient care assistants, pharmacists, social workers, and chaplains.
Association Between Conceptual Model Constructs and Intention and Actual Use of the RTLS
Negative or neutral attitudes and beliefs about RTLSs were associated with less intention to use the RTLS before implementation and less actual use during and after implementation (Table 3).
Table 3.
Logistic Regression Models Examining the Association of Conceptual Model Constructs on Self-Reported Intent or Actual Use of the Real-Time Location System in the Emergency Departmenta
| Preimplementation survey | Reference category | Intention to use RTLS, OR (95% CI) |
|---|---|---|
| I like the idea of using RTLS | Strongly agree/agree | 6.35 (2.45-16.50) |
| I doubt my ability to use the data from RTLS | Strongly agree/agree | 5.15 (1.39-19.09) |
| Using RTLS improves patient care | Strongly agree/agree | 0.29 (0.11-0.78) |
| Using RTLS helps me do my job better | Strongly agree/agree | 0.09 (0.03-0.28) |
| Confident my employer will keep RTLS data in a secure manner | Strongly agree/agree | 0.25 (0.01-0.67) |
| Comfortable disclosing personal information online | Strongly agree/agree | 3.55 (1.23-10.28) |
| Midimplementation survey—strongly disagree/disagree/neutral | Reference category | Actual use, OR (95% CI) |
|---|---|---|
| I like the idea of using RTLS | Strongly agree/agree | 0.12 (0.04-0.39) |
| Using RTLS improves patient care | Strongly agree/agree | 0.18 (0.06-0.51) |
| RTLS makes me more efficient in my work | Strongly agree/agree | 0.11 (0.03-0.38) |
| Postimplementation survey—strongly disagree/disagree/neutral | Reference category | Actual use, OR (95% CI) |
|---|---|---|
| I like the idea of using RTLS | Strongly agree/agree | 0.01 (<0.01-0.04) |
OR = odds ratio; RTLS = real-time location system.
Preimplementation
Before implementation, those who felt neutral, disagreed, or strongly disagreed with the usefulness of RTLSs had higher odds of reporting an intention to use the RTLS compared with those who agreed or strongly agreed (eg, improve patient care, allow them to do their job better). Likewise, those who were neutral or did not feel assured that their employer was taking measures to keep RTLS data in a secure manner had lower odds of intending to use the RTLS.
Unexpectedly, those who were neutral or disagreed that they liked the idea of using the RTLS reported stronger intentions to use the technology. Likewise, those who were neutral or not comfortable about disclosing personal information on social media and those who doubted their ability to use data from the RTLS also reported stronger intentions to use the RTLS. On further examination, using unadjusted bivariate comparisons, those who had neutral feelings about liking the idea of the RTLS, being comfortable disclosing personal information, and doubted their ability to use the RTLS were more likely to report an intention to use compared with those who disagreed or strongly disagreed with these statements. Social norms and control over RTLS use were not associated with intention to use RTLS .
Midimplementation
During implementation, those who were neutral or disliked the idea of RTLSs were also less likely to use the technology. Those who were neutral or disagreed that the RTLS would improve patient care or make them more efficient had higher odds of using RTLS compared with those with positive feelings about the usefulness of the RTLS. Questions on social norms, control, trust, or privacy were not associated with RTLS use during implementation.
Postimplementation
After implementation, those who were neutral or disliked the idea of using RTLSs had lower odds of using it compared with those with positive attitudes about RTLS . Questions on social norms, control, perceived usefulness, trust, or privacy were not associated with RTLS use postimplementation.
Discussion
The RTLS was implemented to promote high-quality care and safety in the ED. Implementation of any new technology, however, can disrupt routine and familiar practices, and because of this, staff may perceive the innovation as a risk for patient and staff safety and care quality. Fisher and Monahan5,17,30 have documented numerous cases of RFID sabotage because of clinical staff concerns about their privacy, lack of institutional trust, and not finding the technology to be helpful. A key interest of the current study, therefore, was understanding if staff balanced the potential benefits for patient care and safety with their concerns about privacy and control over RTLS data collected on them and if, over time, they reassessed the risks and benefits of using the technology.
Although we did not find notable demographic differences in intended use or adoption of the technology, we did find some support for our hypothesis. Indeed, negative or neutral attitudes about RTLSs, low perceived usefulness, a lack of trust about how location data would be used, and concerns about personal privacy were associated with weaker intended and actual use of the RTLS. Negative or neutral attitudes and a lack of perceived usefulness were more consistently associated with lower intention to use the RTLS. Before implementation, doubts about the ability to use the RTLS and about the employer keeping data secure and concerns about personal privacy were associated with the intention, but in the second and third surveys, these same concerns were no longer statitistically different. Initial concerns before implementation about usefulness, privacy, and use of RTLS data by management may have waned over time. This change could have occurred as participants began to gain confidence and integrate RTLS use into everyday practice, learned more about how the data were used by their employer, and personally observed the usefulness of the data in their daily activities.
In the preimplementation survey, there were also a number of findings that were unexpected. For example, those who were neutral or disagreed with the question “I like the idea of using RTLS” were more likely to report an intention to use RTLS. During and after implementation, however, those who were neutral or disagreed with the same question were less likely to report actual use of the technology. Similarly, those who were neutral or disagreed with feeling comfortable about sharing personal information on social media were also more likely to report intention to use the RTLS before implementation but not during or after implementation.Those who were unsure or neutral about whether they would like the RTLS or were unsure of their feelings about sharing personal information before implementation possibly needed hands-on experience to inform their attitudes. With more experience in using the RTLS, those with neutral attitudes before RTLS implementation may have shifted to more positive attitudes.
Preimplementation efforts to engage stakeholders and staff should focus on fostering positive attitudes about the perceived usefulness of the technology and the benefits of improving patient care, doing one’s job better, and being more efficient. Moreover, real concerns from staff about privacy of personal information and clarity on the parameters of how data will and will not be used need to be addressed and consistently reinforced. Instituting a data governance board to determine acceptable procedures related to data access, consulting with experts from departments including human resources, legal, and ethics, and engaging administrators who oversee and enforce policy, as was done at our institution, may be helpful in regularly assuring staff that dependable safeguards exist and that consequences of inappropriate use exist and are enforced.
In spite of the strength of having data assessed at different times throughout the implementation process, our study has a number of limitations. First, surveys were anonymous to the research team, and therefore, we were not able to link people across surveys. Because of attrition and new hires, it is likely that some participants responded to one survey but not others. This factor may also account for differences in response rates across surveys. Because of this limitation, we were also impeded from looking at continuous trends over time and relied on cross-sectional snapshots of staff attitudes at different points during the implementation. Second, because of limited statistical power, we were not able to examine unique differences between those who agreed, were neutral, or disagreed with attitudinal questions. Although we examined bivariate relationships between these questions and our outcomes, we were not able to test fully adjusted models. Therefore, it is possible that a more robust model with all variables fit could have different findings. Third, we examined differences at 3 different times during the implementation process but did not track the impact of different implementation efforts (eg, town hall meetings, new releases of frequently asked questions) on changes in behaviors or how technology challenges during implementation, such as glitches in the timely distribution of RFID on identification badges, affected the results. Most of the implementation efforts began before the first survey and were intended to facilitate ease of implementation, answer questions, and encourage uptake. Finally, our specific findings may not be generalizable to RTLS implementation at other EDs in other health systems or academic medical centers, but we are confident that a process evaluation of organizational culture and staff attitudes throughout implementation is beneficial for planning successful uptake of RTLS. Although we are limited by having only one site and one type of technology, we are encouraged that our findings are consistent with research on best practices for implementation success, including early stakeholder engagement, building trust over time, and clear communication.9
Conclusion
In addition to designing the technical installation and implementation of an RTLS in a dynamic clinical setting, strong attention and consideration should be paid to organizational culture and perceptions of staff about implementation, including the impact the new technology has on attitudes about privacy, organizational use of data, and the technology’s implicit and explicit usefulness. Building trust, communication about the technology’s purpose, and training staff’s self-efficacy may be critical to ensure that negative or neutral attitudes at the onset shift over time.
Footnotes
Grant Support: This work was supported by the Robert D. and Patricia E. Kern Center for the Science of Healthcare Delivery’s Care Experiences Program and Health Systems Engineering Program and Mayo Clinic Department of Emergency Medicine.
Potential Competing Interests: The authors report no competing interests.
References
- 1.McGlynn E.A., Asch S.M., Adams J., et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 2.Berwick D.M., Calkins D.R., McCannon C.J., Hackbarth A.D. The 100,000 Lives Campaign: setting a goal and a deadline for improving health care quality. JAMA. 2006;295(3):324–327. doi: 10.1001/jama.295.3.324. [DOI] [PubMed] [Google Scholar]
- 3.Sinkowitz-Cochran R.L., Garcia-Williams A., Hackbarth A.D., et al. Evaluation of organizational culture among different levels of healthcare staff participating in the Institute for Healthcare Improvement's 100,000 Lives Campaign. Infect Control Hosp Epidemiol. 2012;33(2):135–143. doi: 10.1086/663712. [DOI] [PubMed] [Google Scholar]
- 4.Kamel Boulos M.N., Berry G. Real-time locating systems (RTLS) in healthcare: a condensed primer. Int J Health Geogr. 2012;11(1):25. doi: 10.1186/1476-072X-11-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fisher J.A., Monahan T. Evaluation of real-time location systems in their hospital contexts. Int J Med Inform. 2012;81(10):705–712. doi: 10.1016/j.ijmedinf.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 6.Guédon A.C., Wauben L.S., de Korne D.F., Overvelde M., Dankelman J., van den Dobbelsteen J.J. A RFID specific participatory design approach to support design and implementation of real-time location systems in the operating room. J Med Syst. 2015;39(1):168. doi: 10.1007/s10916-014-0168-0. [DOI] [PubMed] [Google Scholar]
- 7.Bowen M.E., Wingrave C.A., Klanchar A., Craighead J. Tracking technology: lessons learned in two health care sites. Technol Health Care. 2013;21(3):191–197. doi: 10.3233/THC-130738. [DOI] [PubMed] [Google Scholar]
- 8.Wu W.-Y., Li C.-Y. A contingency approach to incorporate human, emotional and social influence into a TAM for KM programs. J Inform Sci. 2007;33(3):275–297. [Google Scholar]
- 9.Damschroder L.J., Aron D.C., Keith R.E., Kirsh S.R., Alexander J.A., Lowery J.C. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4(1):50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fernandez M.E., Walker T.J., Weiner B.J., et al. Developing measures to assess constructs from the Inner Setting domain of the Consolidated Framework for Implementation Research. Implement Sci. 2018;13(1):52. doi: 10.1186/s13012-018-0736-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holden R.J., Karsh B.-T. A theoretical model of health information technology usage behaviour with implications for patient safety. Behav Inform Technol. 2009;28(1):21–38. [Google Scholar]
- 12.Parlak S., Sarcevic A., Marsic I., Burd R.S. Introducing RFID technology in dynamic and time-critical medical settings: requirements and challenges. J Biomed Inform. 2012;45(5):958–974. doi: 10.1016/j.jbi.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 13.Kim H.-W., Kankanhalli A. Investigating user resistance to information systems implementation: a status quo bias perspective. MIS Q. 2009;33(3):567–582. [Google Scholar]
- 14.Marakas G.M., Hornik S. Passive resistance misuse: overt support and covert recalcitrance in IS implementation. Eur J Inform Syst. 1996;5(3):208–219. [Google Scholar]
- 15.Bhattacherjee A., Hikmet N. Physicians' resistance toward healthcare information technology: a theoretical model and empirical test. Eur J Inform Syst. 2007;16(6):725–737. [Google Scholar]
- 16.Lapointe L., Rivard S. A multilevel model of resistance to information technology implementation. MIS Q. 2005;29(3):461–491. [Google Scholar]
- 17.Monahan T., Fisher J.A. Surveillance impediments: recognizing obduracy with the deployment of hospital information systems. Surveillance Soc. 2011;9(1/2):1–16. [Google Scholar]
- 18.Lorenzi N.M., Novak L.L., Weiss J.B., Gadd C.S., Unertl K.M. Crossing the implementation chasm: a proposal for bold action. J Am Med Inform Assoc. 2008;15(3):290–296. doi: 10.1197/jamia.M2583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ajzen I. In: Action Control: From Cognition to Behavior. Kuhl J., Beckmann J., editors. Springer; Berlin, Germany: 1985. From intentions to actions: a theory of planned behavior; pp. 11–39. Springer Series in Social Psychology. [Google Scholar]
- 20.Mathieson K. Predicting user intentions: comparing the technology acceptance model with the theory of planned behavior. Inform Syst Res. 1991;2(3):173–191. [Google Scholar]
- 21.Bagozzi R.P., Davis F.D., Warshaw P.R. Development and test of a theory of technological learning and usage. Hum Relat. 1992;45(7):659–686. [Google Scholar]
- 22.Davis F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989;13(3):319–340. [Google Scholar]
- 23.Venkatesh V., Morris M.G., Davis G.B., Davis F.D. User acceptance of information technology: toward a unified view. MIS Q. 2003;27(3):425–478. [Google Scholar]
- 24.Institute of Medicine . National Academies Press; Washington, DC: 2007. Emergency Medical Services: At the Crossroads. [Google Scholar]
- 25.Miró O., Antonio M.T., Jiménez S., et al. Decreased health care quality associated with emergency department overcrowding. Eur J Emerg Med. 1999;6(2):105–107. doi: 10.1097/00063110-199906000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Martínez Pérez M., Cabrero-Canosa M., Vizoso Hermida J., et al. Application of RFID technology in patient tracking and medication traceability in emergency care. J Med Syst. 2012;36(6):3983–3993. doi: 10.1007/s10916-012-9871-x. [DOI] [PubMed] [Google Scholar]
- 27.Hellmich T.R., Clements C.M., El-Sherif N., et al. Contact tracing with a real-time location system: a case study of increasing relative effectiveness in an emergency department. Am J Infect Control. 2017;45(12):1308–1311. doi: 10.1016/j.ajic.2017.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arunachalam S, Sir S, Marisamy G, et al. Identifying factors influencing patient alone time at the emergency department using RFID data: what is next? Paper presented at: 4th IEEE EMBS International Conference on Biomedical and Health Informatics (BHI); February 16-19, 2017; Orlando, FL.
- 29.Venkatesh V., Davis F.D. A theoretical extension of the technology acceptance model: four longitudinal field studies. Manage Sci. 2000;46(2):186–204. [Google Scholar]
- 30.Fisher J.A. In: Surveillance and Security: Technological Politics and Power in Everyday Life. Monahan T., editor. Routledge; New York, NY: 2006. Indoor positioning and digital management: emerging surveillance regimes in hospitals; pp. 77–88. [Google Scholar]