Abstract
Objective
To examine the relationships among various organizational values, employee engagement, and patient satisfaction in an academic medical center.
Participants and Methods
Organizational values and engagement data were retrieved from 2015 all-staff survey results from 1876 clinical units at Mayo Clinic. For patient satisfaction data, Press Ganey scores from visits from July 1, 2015, through January 1, 2016, were matched with data for 26 outpatient units from the all-staff survey. The study was performed from January 1, 2016, through December 31, 2017.
Results
From the all-staff survey results, we identified seven constructs related to values and employee engagement, all of which showed high positive correlation with each other. We were able to determine a structural equation model for values and engagement that had an excellent fit (comparative fit index, 0.957). Empowering leadership was positively correlated with the largest number of patient satisfaction items, followed by employee engagement and psychological safety/trust. All items from the care provider category had positive correlations with empowering leadership and psychological safety/trust.
Conclusion
All the organizational values studied showed positive correlation with employee engagement, and all the organizational values and engagement were predictors of excellence and innovation either directly or indirectly. This affirms that honoring organizational values related to respect, psychological safety/trust, empowering leadership, and fairness has a positive influence on employee engagement and desire to pursue excellence. Organizational values, engagement, and empowering leadership behavior were positively correlated with many patient satisfaction items.
Abbreviations and Acronyms: CFI, comparative fit index; RMSEA, root mean square error of approximation; SEM, structural equation modeling; SRMR, standardized root mean square residual
Organizational culture has been known to be an important characteristic that influences behaviors of groups and individuals within an organization.1 Many studies on organizational culture have explored its relationship with organizational effectiveness and performance.2 According to Kotrba et al,3 examples of various indices that are positively related to organizational performance include organizational mission, adaptability, competitiveness and entrepreneurial culture, and innovation. Schein1 analyzed organizational culture at 3 different levels: artifacts, espoused beliefs and values, and basic underlying assumptions. The context of work environment in health care today has changed dramatically, and organizations need to rely more on workers to make decisions about how the work should get done. Burks and Kobus4 highlighted concerns regarding decreased prosocial behaviors and humanistic qualities in medicine because there is increased potential for detachment from patients, decreased patient centeredness, increased burnout, and disengagement.
Shared organizational values provide comfort to employees as well as meaning and purpose to work, which ultimately brings better performance. Pololi et al5 stated that when there is cultural alignment and congruence between organizational cultural values and individual values, employees are committed and more engaged and ultimately perform better. Work climate and cultural values determine how an organization views effective leadership, teamwork, and relationships among staff. According to Anitha’s work on employee engagement,6 how organizational policies are established and implemented is an important determinant of employee engagement, which, in turn, brings the organizational performance.
Although there have been many studies that suggest positive relationships among intrinsic aspects of work motivation (eg, meaningfulness, commitment, engagement, and organizational performance), studies in the health care setting are scarce.
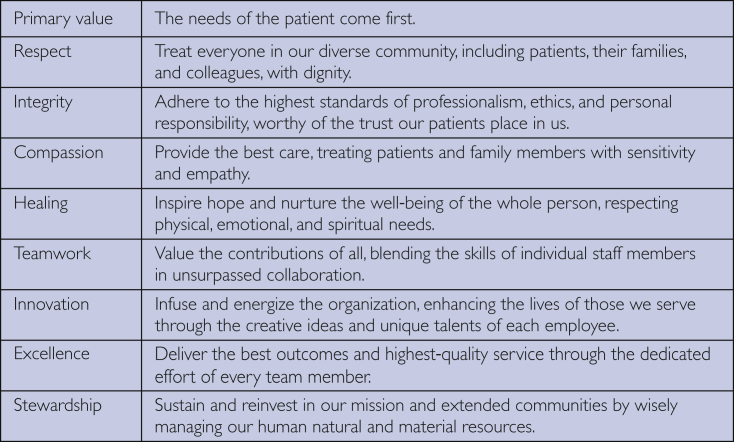
Cultural Values at Mayo Clinic
Values at Mayo Clinic are grounded in its history and are considered part of the “DNA” of the organization. The primary value of patient centeredness and eight additional value statements provide the basis for the Mayo Clinic Model of Care and how we do what we do. The list of Mayo Clinic values is given in Figure 1.
Figure 1.
Mayo Clinic values.
Employee Engagement and Cultural Values
Harter et al7 defined employee engagement as an individual’s involvement in, satisfaction with, and enthusiasm for work. Studies have shown a positive relationship between employee engagement and job performance. Mayo Clinic has a deeply embedded value-based culture with the needs of the patient placed in the center of day-to-day care. Engaging employees in delivering this primary value creates shared meaning and purpose, which drives the patient experience.
Recent studies in organizational science have suggested that workplace climate, empowering management practices, meaningfulness, psychological safety, autonomy, opportunities for development, and recognition have a positive relationship with employee engagement.8, 9, 10 According to Rich et al,11 when there is value congruence between what is expected by the organization and behaviors that employees value as their own they are more likely to engage themselves at work. Chou et al12 studied internal medicine residents who exemplified humanistic patient care and found that physicians attributed their humanistic behavior to a desire to emulate the right way to behave, keeping in mind the basic values of how to treat people and being motivated to do what is right and proper.
Role of Leadership
Leaders create the environment that empowers employees to deliver great care by building teams. Successful teamwork requires leaders to engage employees in their work and to be actively involved in decisions regarding their work.
Leaders who empower staff have strong interpersonal skills, are inclusive, coach, mentor, and provide ongoing feedback. They align the work to the greater good, hold career and leadership discussions, and leverage the strengths individually and collectively of the team.13, 14, 15, 16 They can delegate responsibilities and decision making, which contributes to increased engagement of staff.17 Leaders who create a workplace culture of inclusiveness, trust, and psychological safety foster positive emotion (eg, being more open-minded, resilient, motivated, and persistent), which positively influences employee engagement and ultimately the patient experience.18, 19 Nembhard and Edmondson20 explained the concept of psychological safety as a perception that a staff member can speak up without fear of rejection or negative consequences. It is something people feel when they are not constrained by the possibility of others’ disapproval or the negative personal consequences that might result. Therefore, a leader’s role is to ensure safety in the workplace by demonstrating and reinforcing inclusive and empowering behaviors that ensure trust among employees, a spirit of cooperation, and the ability to speak one’s mind without fear.
Patient Satisfaction, Organizational Values, and Employee Engagement
Patient satisfaction is an important measure of clinical outcome and health care performance. Several studies have reported a positive relationship between organizational culture and customer satisfaction. Greenslade and Jimmieson21 found that organizational climate for service predicted performance, which, in turn, predicted patient satisfaction. Another study by Tzeng et al22 described the strength of organizational culture as the extent to which the staff view the organization as having a set of directions and values for clear communication, which was positively correlated with job satisfaction and patient satisfaction. In a non–health care setting, Gillespie et al23 found that an empowering organizational culture, which also adheres to the organizational vision and mission, positively correlated with customer satisfaction.
Against this backdrop, the purpose of this study was to examine the relationships among organizational values, employee engagement, and the effect on patient satisfaction.
Participants and Methods
This study consists of two parts. The first part focuses on studying the relationships among values and engagement and the second part focuses on relationships among values, engagement, and patient satisfaction scores.
Samples and Measures
Organizational Values and Employee Engagement
We retrieved the sample data from the all-staff survey administered in October 2015 at the Rochester campus of Mayo Clinic to measure organizational values and employee engagement. All the survey results were rolled up to the unit level to ensure anonymity of the respondents. A unit consists of a clinical work group with 5 or more staff reporting to the supervisor. We analyzed the average responses of 1876 units within Mayo Clinic with a total response rate of 72%. This survey was not originally designed for assessing cultural values. However, we found that most questions were relevant for assessing the staff’s perception of the degree to which organizational cultural values aligned at the unit level. During the initial stage, a group of professionals in human resources and quality examined the content questions to ensure that they mapped to the relevant organizational values to assess the feasibility of using the existing survey before running a cluster analysis.
Patient Satisfaction
Press Ganey Associates provided patient satisfaction measurement. To study the relationships between values data from the all-staff survey described in the previous section and patient satisfaction data, we matched the business units used for the 2 surveys. We pulled the patient satisfaction data from July 1, 2015, through January 1, 2016, to match the administration date of the all-staff survey. Because the all-staff surveys used units that were much more granular than patient satisfaction data, the business units were condensed into larger-level units for analysis, which became divisions or departments as the unit of analysis for this part of the study. This generated a sample size of 26 units (allergy, child-adolescent psychology, colon rectal surgery, dental specialties, dermatology, gastroenterology and hepatology, general internal medicine, infectious disease, neurosurgery, medical oncology, nephrology-hypertension, obstetrics, ophthalmology, orthopedics, otorhinolaryngology, pain services, pediatric cardiology, physical medicine and rehabilitation, plastic surgery, preventive medicine, psychiatry and psychology, pulmonary-critical, radiation oncology, rheumatology, thoracic surgery, and urology).
Data Analysis
Cluster Analysis
Without an a priori hypothesis of any particular item-to-construct relationships, we came up with constructs using the statistical method of cluster analysis. All items from both the all-staff survey and the patient satisfaction data were entered into cluster analysis. Cluster analysis partitions variables to homogeneous classes. Hierarchical agglomerative cluster analyses were performed using the Ward method, with squared Euclidean distance as the distance measure. It identifies items that are close in the distance measure and arranges the clusters of the related items in a tree diagram (ie, dendrogram). The content matter experts reviewed the solution from the cluster analysis and gave names to the clusters of items (ie, constructs). Because the all-staff survey was not originally designed to assess values, we tried to derive the constructs that matched the Mayo Clinic values as closely as possible.
Structural Equation Modeling
Structural equation modeling (SEM) is used to test the hypotheses about the relationships among the latent constructs. We developed a hypothesis about how the constructs uncovered in cluster analysis (described in the previous subsection) are related to each other. We analyzed these relationships using SEM. We used the data from the all-staff survey only because running SEM with patient satisfaction items (n=26 units) was not feasible because of the small sample size. The first step for SEM was to fit the measurement model to test the relationship between the factors and the items that were hypothesized to measure them. We inspected the fit of the measurement model with the guidelines that are indicative of a desirable model fit.24, 25 The fit measures included comparative fit index (CFI), standardized root mean square residual (SRMR), and root mean square error of approximation (RMSEA). In addition, we inspected the reliabilities of the constructs using the H coefficient.24 When the measurement model had a desirable model fit, we proceeded to testing the structural model, which answers the research questions about the relationships among factors. We evaluated the fit indices for the final structural model.
Correlation Analyses
We investigated the relationship between the constructs of values studied in cluster and SEM analyses and the patient satisfaction items for 26 units using the Pearson correlation. We used the Cohen26 method of interpretation. According to Cohen, a Pearson correlation coefficient of 0.3 is a medium effect size (with 9% explained variance) and 0.5 is a large effect size (with 25% explained variance); if 0.3 or higher, then the correlation can be interpreted as a nontrivial relationship.
Results
Cluster Analyses to Identify Coherent Constructs
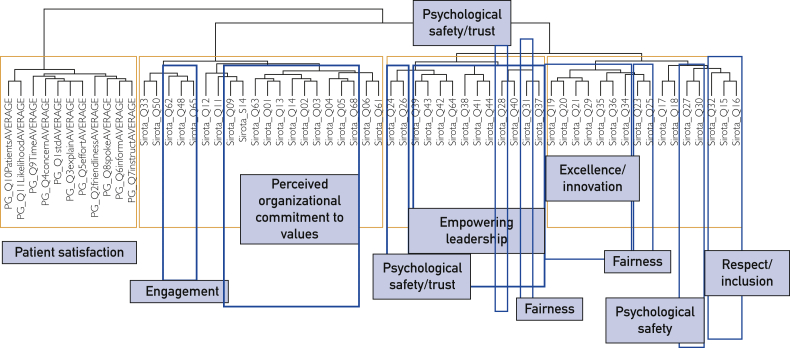
Figure 2 shows the item-to-construct membership from the cluster analyses and the names of these constructs. The constructs were named (1) perceived organizational commitment to values, (2) empowering leadership, (3) excellence/innovation, (4) fairness, (5) psychological safety/trust, (6) respect/inclusion, and (7) engagement. Table1 lists the 7 constructs and examples of statements used. The term psychological safety is based on the definition by Nembhard and Edmonson20 as a perception that staff can speak up without fear of rejection or negative consequences. The term fairness refers to the perceived level of procedural justice in the organization. Based on social exchange theory, interactional justice and fairness increase the perception of organizational support, which, in turn, increase commitment to the organization.27
Figure 2.
Cluster tree diagram or dendrogram.
Table 1.
Reliability and Sample Statements for the 7 Constructs
| Construct | Reliability (H) | Sample statements |
|---|---|---|
| Perceived organizational commitment to values | 0.92 | Mayo Clinic lives up to its primary value of "the needs of the patient come first." Mayo Clinic leaders make decisions that are consistent with Mayo Clinic values. |
| Empowering leadership | 0.94 | Empowers me to do my job. Provides helpful feedback and coaching on my performance. |
| Excellence/innovation | 0.91 | In my immediate work unit, we have a strong desire to continuously improve service. People where I work are willing to do whatever is necessary to provide excellent service. |
| Fairness | 0.87 | Policies and procedures are fairly enforced in my work unit. I am treated fairly in my workplace. |
| Psychological safety/trust | 0.94 | There is a high level of trust among employees within my work unit. There is a spirit of cooperation and teamwork within my work unit. Where I work, I feel free to speak my mind without fear of negative consequences. |
| Respect/inclusion | 0.61 | Based on my personal experience during the past year, there is mutual respect between physicians/scientists and allied health staff. My department is committed to creating an environment that is inclusive to both men and women. |
| Engagement | 0.74 | I feel a strong sense of ownership and responsibility for the success of Mayo Clinic. My work gives me a sense of achievement. |
SEM Analyses Investigating the Relationships Among Variables
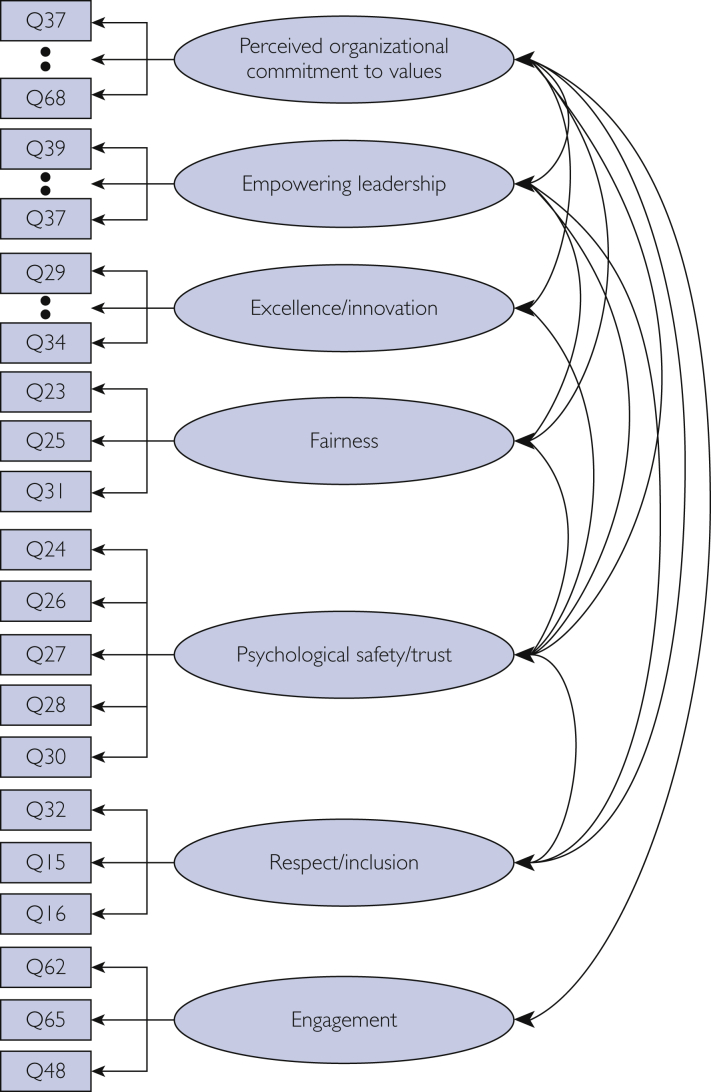
Measurement Model
A measurement model tests the membership of items and their hypothesized constructs as well as the correlations among constructs. The measurement model (Figure 3) of engagement with its 3 items, perceived organizational commitment to values with its 9 items, empowering leadership with its 8 items, excellence/innovation with its 7 items, fairness with its 3 items, psychological safety/trust with its 5 items, and respect/inclusion with its 4 items had excellent fit (CFI=0.958, RMSEA=0.046 [90% CI, 0.044-0.048], and SRMR=0.043). Table 1 shows the H coefficient. Except for respect/inclusion (H=0.61) and engagement (H=0.74), all the constructs had very high reliability (H≥0.87).
Figure 3.
Measurement model.
Correlations among the latent constructs from the measurement model are shown in Table 2. All the organizational value constructs were correlated highly (r≥0.51) and were significant at P<.001. The highest correlation for employee engagement was with respect/inclusion, followed by employee perception of organizational commitment to values. Psychological safety/trust and fairness had a very strong correlation of 0.98, as did fairness and values of excellence/innovation, followed by psychological safety/trust and excellence/innovation.
Table 2.
Correlation Among the Latent Constructs From the Measurement Model (N = 1876)a
| Construct | Statistics | Perceived organizational commit to values | Empowering leadership | Excellence/innovation | Fairness | Psychological safety/trust | Respect/inclusion |
|---|---|---|---|---|---|---|---|
| Empowering leadership | Pearson r | 0.53 | |||||
| P value | <.001 | ||||||
| Excellence/innovation | Pearson r | 0.72 | 0.79 | ||||
| P value | <.001 | <.001 | |||||
| Fairness | Pearson r | 0.64 | 0.80 | 0.98 | |||
| P value | <.001 | <.001 | <.001 | ||||
| Psychological safety/trust | Pearson r | 0.59 | 0.75 | 0.96 | 0.98 | ||
| P value | <.001 | <.001 | <.001 | <.001 | |||
| Respect/inclusion | Pearson r | 0.83 | 0.69 | 0.92 | 0.88 | 0.81 | |
| P value | <.001 | <.001 | <.001 | <.001 | <.001 | ||
| Engagement | Pearson r | 0.83 | 0.51 | 0.74 | 0.66 | 0.59 | 0.85 |
| P value | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 |
P<.001.
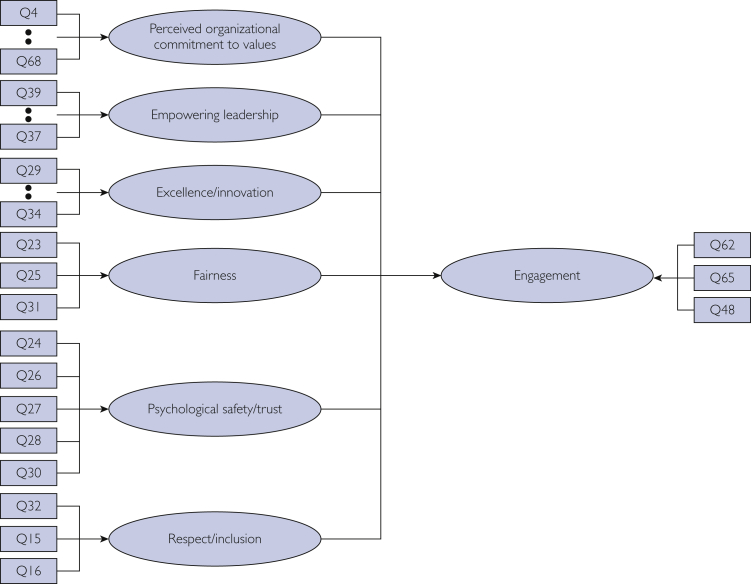
Structural Model
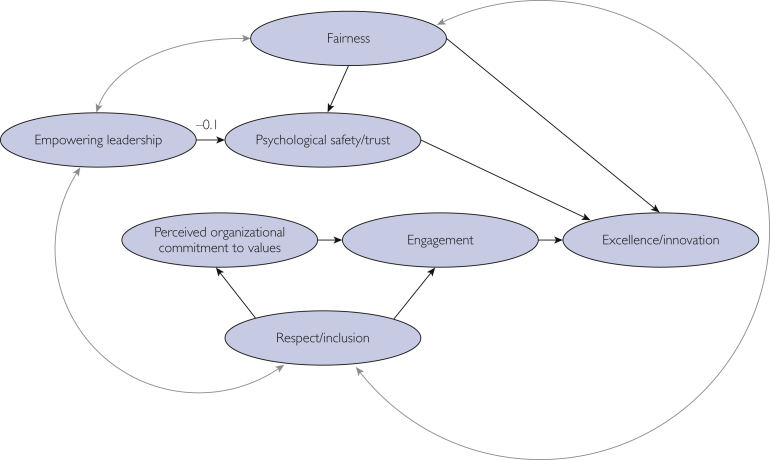
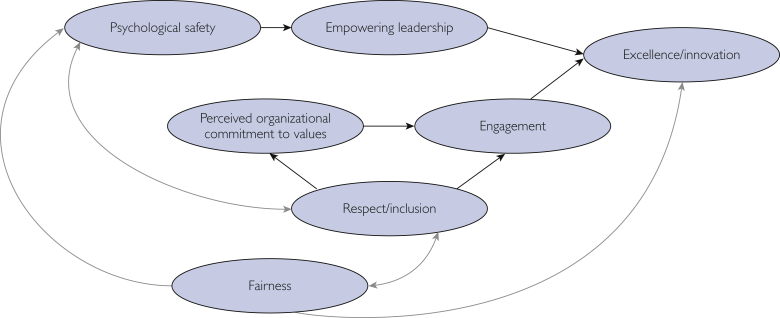
The first hypothesized model is presented in Figure 4. This model failed to converge, which precluded obtaining any fit indices. We modified the hypothesis so that excellence is the final outcome rather than engagement. We also put psychological safety as a mediator between empowerment and excellence. The SEM produces modification indices that display the degree to which the model fit improves when alternative paths are added between constructs. We used these modification indices and the past literature when making decisions to add or drop paths, which was an iterative process. Figure 5 shows a competing model that had good fit, but the negative coefficient from empowerment to psychological safety/trust (ie, empowerment negatively affects psychological safety/trust) ran counter to the accumulated knowledge. The alternative model was fit: instead of empowerment predicting psychological safety/trust, the relationship was reversed to psychological safety/trust predicting empowerment. This model (Figure 6) had excellent fit (CFI=0.957, Tucker-Lewis index=0.951, RMSEA=0.046 [90% CI, 0.045-0.048], and SRMR=0.044) and it also aligned with what is known about the relationships among these constructs from past literature. Its path coefficients (Table 3) were all significant at P<.001.
Figure 4.
Initial hypothesis.
Figure 5.
A competing structural equation model. Single-headed arrows denote regressions and double-headed arrows denote correlations.
Figure 6.
Alternative model that was chosen as the final model. Single-headed arrows denote regressions and double-headed arrows denote correlations.
Table 3.
Coefficients From the Final Structural Model
| Outcome | Predictor | Standardized coefficient β | z statistic | P value | R2 |
|---|---|---|---|---|---|
| Psychological safety/trust | Fairness | 0.99 | 48.9 | <.001 | 0.984 |
| Empowering leadership | Psychological safety/trust | 0.77 | 35.5 | <.001 | 0.586 |
| Engagement | 0.754 | ||||
| Perceived organizational commitment to values | 0.53 | 12.3 | <.001 | ||
| Respect/inclusion | 0.38 | 8.4 | <.001 | ||
| Perceived organizational commitment to values | Respect/inclusion | 0.79 | 21.8 | <.001 | 0.619 |
| Excellence/innovation | 0.988 | ||||
| Fairness | 0.81 | 33.98 | <.001 | ||
| Engagement | 0.18 | 10.6 | <.001 | ||
| Empowering leadership | 0.07 | 4.6 | <.001 |
The results of the best-fitting structural model showed that the end outcome was excellence/innovation rather than engagement. Engagement was a mediator between commitment and excellence, as well as inclusiveness and excellence. Fairness and empowerment were also strong predictors of excellence/innovation. More fairness increased psychological safety/trus. More psychological safety/trust increased empowerment, which positively influenced excellence/innovation. This model explained 99% of the variance in the end outcome excellence/innovation, 75% of the variance in engagement, and 98% in psychological safety/trust (Table 3).
Correlational Analyses Investigating the Relationships Among Values, Engagement, and Patient Satisfaction Scores
Pearson correlations among the summed item scores for values, summed scores for employee engagement, and item-level scores for patient satisfaction data are listed in Table 4. Empowering leadership had the largest number of patient satisfaction items (17 of 19) that had correlation coefficients of medium effect size or larger. Employee engagement and psychological safety/trust both had 16 items that had correlation coefficients of medium effect size or larger. For care provider category, all the questions were positively correlated with medium effect size or larger with empowering leadership and psychological safety/trust.
Table 4.
Correlations Among Values, Engagement, and Patient Satisfaction (N = 26)
| Category | Satisfaction items | Statistics | Engagement | Excellence/innovation | Empowering leadership | Fairness | Perceived organizational commitment to values | Psychological safety/trust | Respect/inclusion |
|---|---|---|---|---|---|---|---|---|---|
| Access and moving through visit | Ease of scheduling | Pearson r | 0.54a | 0.37 | 0.46b | 0.36 | 0.36 | 0.33 | 0.22 |
| P value | .005 | .061 | .029 | .068 | .073 | .104 | .29 | ||
| Information about delays | Pearson r | 0.46b | 0.47b | 0.39 | 0.47b | 0.36 | 0.36 | 0.31 | |
| P value | .017 | .016 | .067 | .016 | .072 | .072 | .129 | ||
| Wait time | Pearson r | 0.30 | 0.38 | 0.38b | 0.42b | 0.32 | 0.32 | 0.27 | |
| P value | .136 | .053 | .049 | .032 | .117 | .11 | .188 | ||
| Nurse/assistant | Friendliness/courtesy | Pearson r | 0.35 | 0.20 | 0.29 | 0.17 | 0.22 | 0.09 | 0.00 |
| P value | .083 | .321 | .26 | .397 | .288 | .649 | .991 | ||
| Concern for problems | Pearson r | 0.48b | 0.27 | 0.29 | 0.19 | 0.26 | 0.18 | 0.03 | |
| P value | .014 | .177 | .309 | .351 | .207 | .393 | .879 | ||
| Prompt return of calls | Pearson r | 0.34 | 0.30 | 0.38 | 0.18 | 0.21 | 0.25 | –0.02 | |
| P value | .087 | .143 | .127 | .37 | .316 | .213 | .926 | ||
| Care provider | Explanation of problems | Pearson r | 0.31 | 0.27 | 0.50b | 0.30 | 0.20 | 0.39b | 0.14 |
| P value | .123 | .184 | .012 | .132 | .339 | .046 | .499 | ||
| Concern for questions/worries | Pearson r | 0.22 | 0.32 | 0.54a | 0.38 | 0.17 | 0.46b | 0.22 | |
| P value | .278 | .117 | .004 | .056 | .411 | .019 | .271 | ||
| Information about medication | Pearson r | 0.25 | 0.33 | 0.49a | 0.38 | 0.16 | 0.44b | 0.22 | |
| P value | .22 | .1 | .009 | .055 | .443 | .025 | .279 | ||
| Spoke using words | Pearson r | 0.30 | 0.29 | 0.42b | 0.32 | 0.13 | 0.42b | 0.22 | |
| P value | .132 | .146 | .031 | .11 | .513 | .034 | .29 | ||
| Time spent with patients | Pearson r | 0.01 | 0.22 | 0.52a | 0.40b | –0.06 | 0.46b | 0.23 | |
| P value | .979 | .274 | .005 | .042 | .784 | .02 | .268 | ||
| Confidence in provider | Pearson r | 0.38 | 0.25 | 0.47b | 0.27 | 0.22 | 0.38 | 0.09 | |
| P value | .057 | .22 | .013 | .177 | .285 | .058 | .68 | ||
| Likelihood of recommend | Pearson r | 0.35 | 0.23 | 0.48b | 0.26 | 0.21 | 0.35 | 0.11 | |
| P value | .079 | .259 | .015 | .193 | .293 | .076 | .597 | ||
| Personal issues | Sensitivity to your needs | Pearson r | 0.37 | 0.39 | 0.49b | 0.36 | 0.23 | 0.46b | 0.22 |
| P value | .06 | .051 | .013 | .07 | .257 | .018 | .29 | ||
| Concern for privacy | Pearson r | 0.36 | 0.33 | 0.42b | 0.31 | 0.18 | 0.39 | 0.13 | |
| P value | .07 | .097 | .032 | .118 | .374 | .051 | .544 | ||
| Pain controlled | Pearson r | 0.39 | 0.32 | 0.48 | 0.21 | 0.32 | 0.30 | 0.04 | |
| P value | .047 | .114 | .022 | .304 | .112 | .135 | .859 | ||
| Response to concerns/complaints | Pearson r | 0.51a | 0.34 | 0.40 | 0.28 | 0.25 | 0.42b | 0.13 | |
| P value | .008 | .094 | .054 | .16 | .21 | .031 | .513 | ||
| Overall | Care received during visit | Pearson r | 0.44b | 0.29 | 0.48b | 0.33 | 0.32 | 0.30 | 0.21 |
| P value | .024 | .15 | .015 | .095 | .107 | .137 | .303 | ||
| Staff worked together | Pearson r | 0.48b | 0.35 | 0.43b | 0.30 | 0.30 | 0.30 | 0.12 | |
| P value | .013 | .081 | .047 | .14 | .144 | .143 | .55 |
P<.05 (2-tailed).
P<.01 (2-tailed).
Discussion
This study presents a theoretical framework on relationships among important organizational values, leadership behaviors, and employee engagement. In the structural phase of SEM, we found that excellence/innovation was the ultimate outcome variable, which affirms many of the studies previously mentioned on organizational values and engagement that they are antecedents of organizational performance. The present results showed that fairness was a strong predictor for psychological safety/trust (β=0.99) and values of excellence/innovation (β=0.81), which provides evidence that employees need to feel they are being treated fairly to feel safe in the workplace more than being treated respectfully.
We found that employee perception of an organization’s level of commitment to its values along with respect/inclusion were the strongest predictors of employee engagement. One explanation is that the contents of engagement items were mostly related to organization-level engagement rather than to individual roles (eg, “I feel a sense of ownership and responsibility for the success of the organization” or “I would choose to stay with this organization even if offered the same pay and benefits elsewhere”).
One interesting finding was the relationship between psychological safety/trust and empowering leadership. The model fit was superior when psychological safety/trust was the predictor of empowering leadership compared with the other way, which may mean that unit leaders tend to show more empowering behavior when work units have a higher level of psychological safety/trust. Fairness, engagement, and empowering leadership together explained approximately 99% of the variance in excellence/innovation. This provides strong evidence for a positive impact of perceived procedural fairness in organizations and leaders’ empowering behavior on employees’ excellent service. This study also showed that unit (division/department)-level values are positively correlated with many patient satisfaction criteria. Empowering leadership behaviors had the most patient satisfaction scores with correlation of medium effect size or higher (range, 0.29-0.54), which highlights the importance of leadership styles and empowering behaviors on patient outcome. For the patient satisfaction study, the unit of analysis was either division or department. The leadership data used refer to the empowering behaviors of 26 division or department chairpersons. All the scores from satisfaction with care provider were positively correlated with leadership scores with medium or large effect sizes (range, 0.42-0.54). The empowering leadership scores represent all departmental or divisional physician leaders. The physician leadership behaviors were found to influence patient satisfaction with care provider item scores. How leaders foster a learning climate and an empowering environment affects the culture of patient centeredness.
Psychological safety and trust were positively correlated with at least medium effect size for all items in the care provider category (range, 0.35-0.46). This finding coincides with a review article by DiCuccio28 in which psychological safety was found to be positively correlated with patient satisfaction and perception of nurse responsiveness.
Employee engagement had a positive correlation with many of the patient satisfaction items with a medium effect size or larger except for time spent with patient because providers have less control over time with patients. Most questions in the “access and moving through visit” and “overall” categories were positively correlated with most of the values and engagement except for respect/inclusion. The respect/inclusion domain was correlated with the fewest questions with at least small effect sizes. This may be because the respect/inclusion construct had relatively low reliability (H=0.61).
Conclusion
All the organizational values studied were highly correlated with employee engagement, and all the organizational values and engagement were the predictors of values of excellence/innovation either directly or indirectly. This affirms the fact that honoring values in the organization has a positive influence on employee engagement and desire to pursue excellence. Organizational values, engagement, and empowering leadership behavior were positively correlated with many items of patient satisfaction scores measured by the Press Ganey score.
Footnotes
Grant Support: This study was funded by the Mayo Clinic Values Council.
Potential Competing Interests: The authors report no competing interests.
References
- 1.Schein E.H. Vol 2. John Wiley & Sons; Hoboken, NJ: 2010. pp. 7–22. (Organizational Culture and Leadership). [Google Scholar]
- 2.Gregory B.T., Harris S.G., Armenakis A.A., Shook C.L. Organizational culture and effectiveness: a study of values, attitudes, and organizational outcomes. J Bus Res. 2009;62(7):673–679. [Google Scholar]
- 3.Kotrba L.M., Gillespie M.A., Schmidt A.M., Smerek R.E., Ritchie S.A., Denison D.R. Do consistent corporate cultures have better business performance? exploring the interaction effects. Hum Relat. 2012;65(2):241–262. [Google Scholar]
- 4.Burks D.J., Kobus A.M. The legacy of altruism in health care: the promotion of empathy, prosociality and humanism. Med Educ. 2012;46(3):317–325. doi: 10.1111/j.1365-2923.2011.04159.x. [DOI] [PubMed] [Google Scholar]
- 5.Pololi L., Kern D.E., Carr P., Conrad P., Knight S. The culture of academic medicine: faculty perceptions of the lack of alignment between individual and institutional values. J Gen Intern Med. 2009;24(12):1289–1295. doi: 10.1007/s11606-009-1131-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anitha J. Determinants of employee engagement and their impact on employee performance. Int J Prod Perform Manag. 2014;63(3):308–323. [Google Scholar]
- 7.Harter J.K., Schmidt F.L., Hayes T.L. Business-unit-level relationship between employee satisfaction, employee engagement, and business outcomes: a meta-analysis. J Appl Psychol. 2002;87(2):268–279. doi: 10.1037/0021-9010.87.2.268. [DOI] [PubMed] [Google Scholar]
- 8.Chalofsky N., Krishna V. Meaningfulness, commitment, and engagement: the intersection of a deeper level of intrinsic motivation. Adv Develop Hum Resour. 2009;11(2):189–203. [Google Scholar]
- 9.Kahn W.A. Psychological conditions of personal engagement and disengagement at work. Acad Manag J. 1990;33(4):692–724. [Google Scholar]
- 10.May D.R., Gilson R.L., Harter L.M. The psychological conditions of meaningfulness, safety and availability and the engagement of the human spirit at work. J Occup Organ Psychol. 2004;77(1):11–37. [Google Scholar]
- 11.Rich B.L., Lepine J.A., Crawford E.R. Job engagement: antecedents and effects on job performance. Acad Manag J. 2010;53(3):617–635. [Google Scholar]
- 12.Chou C.M., Kellom K., Shea J.A. Attitudes and habits of highly humanistic physicians. Acad Med. 2014;89(9):1252–1258. doi: 10.1097/ACM.0000000000000405. [DOI] [PubMed] [Google Scholar]
- 13.Browning HW, Torain DJ, Patterson TE Collaborative healthcare leadership: a six-part model for adapting and thriving during a time of transformative change. http://media.ccl.org/wp-content/uploads/2015/04/CollaborativeHealthcareLeadership.pdf Center for Creative Leadership website. Published 2011. Accessed October 2, 2018.
- 14.Van Dierendonck D. Servant leadership: a review and synthesis. J Manag. 2011;37(4):1228–1261. [Google Scholar]
- 15.Warren O.J., Carnall R. Medical leadership: why it's important, what is required, and how we develop it. Postgrad Med J. 2011;87(1023):27–32. doi: 10.1136/pgmj.2009.093807. [DOI] [PubMed] [Google Scholar]
- 16.Yukl G. Effective leadership behavior: what we know and what questions need more attention. Acad Manag Perspect. 2012;26(4):66–85. [Google Scholar]
- 17.Ray R.L., Hyland P., Dye D.A., et al. DNA of engagement 2018: moments that matter throughout the employee life cycle. https://www.conference-board.org/publications/publicationdetail.cfm?publicationid=7758 The Conference Board website.
- 18.Delizonna L. High-performing teams need psychological safety: here’s how to create it. Harvard Business Review. August 24, 2017:2-5. https://socialscience.fas.harvard.edu/files/socialscience/files/hbr_2017aug_highperformteamspsychsafety.pdf
- 19.Edmondson A. Speaking up in the operating room: How team leaders promote learning in interdisciplinary action teams. J Manag Stud. 2003;40(6):1419–1452. [Google Scholar]
- 20.Nembhard I.M., Edmondson A. Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J Organ Behav. 2006;27:941–966. [Google Scholar]
- 21.Greenslade J.H., Jimmieson N.L. Organizational factors impacting on patient satisfaction: a cross sectional examination of service climate and linkages to nurses’ effort and performance. Int J Nurs Stud. 2011;48(10):1188–1198. doi: 10.1016/j.ijnurstu.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 22.Tzeng H.M., Ketefian S., Redman R.W. Relationship of nurses’ assessment of organizational culture, job satisfaction, and patient satisfaction with nursing care. Int J Nurs Stud. 2002;39(1):79–84. doi: 10.1016/s0020-7489(00)00121-8. [DOI] [PubMed] [Google Scholar]
- 23.Gillespie M.A., Denison D.R., Haaland S., Smerek R., Neale W.S. Linking organizational culture and customer satisfaction: results from two companies in different industries. Eur J Work Organ Psychol. 2008;17(1):112–132. [Google Scholar]
- 24.Mueller R.O., Hancock G.R. In: Best Practices in Quantitative Methods. Osborne J.W., editor. Sage Publications; Thousand Oaks, CA: 2008. Best practices in structural equation modeling; pp. 488–508. [Google Scholar]
- 25.Yu C.Y. University of California; Los Angeles: 2002. Evaluating cutoff criteria of model fit indices for latent variable models with binary and continuous outcomes [unpublished doctoral dissertation] [Google Scholar]
- 26.Cohen J. Routledge; Abingdon, UK: 2013. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- 27.Schminke M., Cropanzano R., Rupp D.E. Organizational structure and fairness perceptions: the operating effects of organizational level. Organ Behav Hum Decis Process. 2002;89(1):881–905. [Google Scholar]
- 28.DiCuccio M.H. The relationship between patient safety culture and patient outcomes: a systematic review. J Patient Saf. 2015;11(3):135–142. doi: 10.1097/PTS.0000000000000058. [DOI] [PubMed] [Google Scholar]