Abstract
The social determinants of mental health are societal problems that disrupt optimal mental health, increase risk for and prevalence of mental illnesses, and worsen outcomes among individuals with mental illnesses. The various social determinants, two of which are described herein because they are too often neglected—discrimination and food insecurity—are underpinned by an unequal and unjust distribution of opportunity, which, in turn, is driven by both public policies and social norms. Discrimination and social exclusion, especially based on race and ethnicity, are pervasive and will remain largely resistant to change within society until explicitly antiracist public policy is enacted and overtly racist social norms are replaced by attitudes of acceptance and social inclusion. Similarly, eradicating food insecurity will occur only through changes in both policy and social norms. Psychiatrists have an opportunity to screen for, thoroughly assess, and address social risks (including perceived discrimination and food insecurity) at the clinical level. They also can play an important role in the shaping of policy and changing of social norms at the community and societal levels. All of these interventions and activities will ultimately improve mental health, reduce the prevalence of mental illnesses, and improve outcomes for patients.
Keywords: social determinants of mental health, discrimination, food insecurity, social norms
The concept of social determinants of health has great resonance when considering population health and health care. Mental health is no different (1). In recent years, there has been a spike in articles covering the importance of the social determinants of mental health (2), and there have been countless commissions, reports, and workgroups seeking to better understand how mental health care professionals can take action to improve the social determinants of mental health for the many people either living with behavioral health conditions or at risk for developing mental health problems in the future.
The social determinants of health are defined as the conditions into which people are born, live, and age that are shaped by policy decisions and distribution of opportunity within societies. Social determinants are primarily responsible for the health disparities and health inequities that exist between population groups and are akin to the concept of the “fundamental causes of disease” first described by Link and Phelan (3) and “the causes of the causes” as defined by Rose (4). Because social norms and public policies shape the distribution of opportunity and set the context for the social determinants of mental health, our field’s work in changing the public policies and the social norms that societies use to govern and by which they structure themselves will improve mental health outcomes for the population.
Health professionals often consider risk factors—including poor diet, smoking, and other adverse health behaviors—when considering the development of physical and mental health conditions. Psychiatrists and other mental health professionals are experts in identifying risk factors for suicide, depression, and substance use disorders, among many other psychiatric diagnoses and conditions, but when one attempts to intervene at the level of the risk factor, it is often too late. We advocate for moving interventions further upstream. For example, suicide risk assessments are often conducted to evaluate the risk of suicide and assess whether a patient is safe to go home versus needing to be admitted to the hospital. Given that the rate of suicide is increasing in the United States, one must consider that perhaps the intervention of assessing risk is not far enough upstream. We are now aware that the risk of suicide attempts in adulthood increases at an alarming rate with each adverse childhood experience (5). Therefore, intervention points that are focused on decreasing a child’s exposure to abuse, neglect, and household dysfunction could do more to decrease overall risk of future suicide attempts than actions such as assessing nonmodifiable demographic characteristics and current social support structures. We are advocating for a public health approach in addition to a clinical one.
Similarly, if we consider schizophrenia as an example of a serious mental illness, there is an associated concept of “social drift,” in which people with schizophrenia often end up unemployed, with low education, and eventually homeless, sometimes with regular interaction with the criminal justice system. Depending on perspective, one could see social drift as a biopsychosocial phenomenon associated with schizophrenia—a sequela of a mental illness that renders people who have the diagnosis severely impaired in sustaining employment, housing, and social relationships. However, if one considers social norms and public policies and then reflects that the prevailing social norms that view people with schizophrenia as outsiders and outcasts are fed by false, stigmatizing beliefs about the causes and nature of schizophrenia and the moral character of those who have this particular illness, we can then also identify laws and policies that serve to reinforce these norms and create the circumstances in which social drift is inevitable. For instance, the codified lack of parity in mental health care has historically ensured that individuals with serious mental illnesses do not have mental health care coverage equitable to that of health care and may be subject to caps on inpatient treatment and on reimbursements. Furthermore, the fact that much of health care coverage is tied to employment means that when people develop schizophrenia and find themselves unemployed, they are likely to lose their insurance and have great difficulty accessing effective treatment for their condition. They may often seek care within the safety net system, which is underresourced and overtaxed, and they may have to wait for months for a brief interaction with a mental health care provider and may not receive effective and evidence-based services. Public policies that begin to chip away at these deep-rooted inequities could do much to stem the tide against the social drift so commonly associated with schizophrenia.
Conceptualizing the Social Determinants of Mental Health
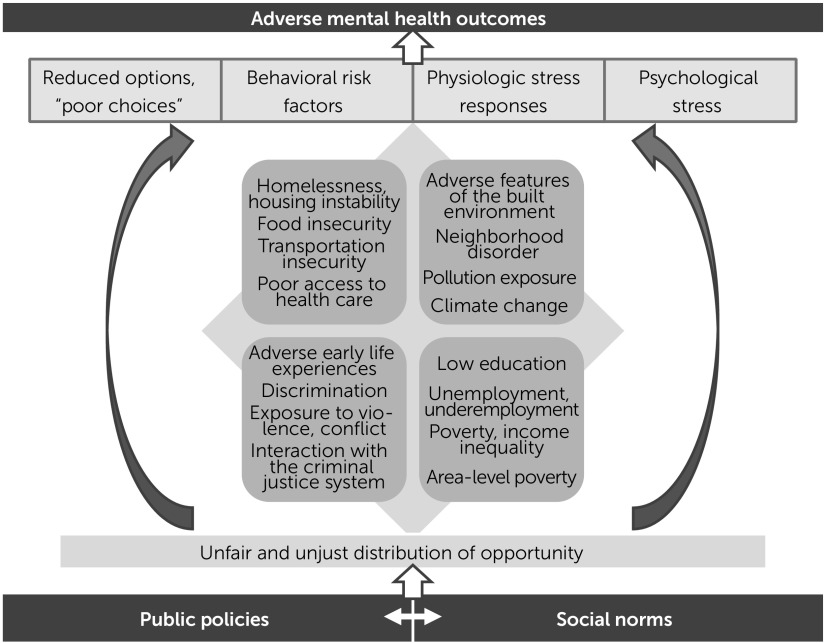
Our original conceptualization of the social determinants of mental health, first presented in The Social Determinants of Mental Health (6) and later revised for the seventh edition of the American Psychiatric Publishing Textbook of Psychiatry (7), laid a foundation for the underlying and driving factors behind poor mental health and mental illnesses in the United States. Specifically, we emphasized the importance of public policies and social norms as the drivers of the unequal distribution of opportunity, which lays the groundwork for 10 specific social determinants of mental health (discrimination and social exclusion; adverse early life experiences; low educational attainment, poor educational quality, and educational inequality; poverty, income inequality, and neighborhood deprivation; food insecurity; unemployment, underemployment, and job insecurity; poor housing quality and housing instability; climate change; adverse features of the built environment; and poor access to health care).
Although not an exhaustive list (e.g., others pertain to access to transportation; exposure to conflict, violence, war, and forced migration; and interaction with an unjust and biased criminal justice system), these social determinants of mental health often drive what appears to be individual-level behavioral patterns, including high-risk behaviors and seemingly poor choices, which can lead to increased risk factors for mental illnesses and substance use disorders and, ultimately, contribute to early mortality for individuals with serious mental illnesses. The full conceptualization is depicted in Figure 1.
FIGURE 1.
A conceptualization of the social determinants of mental health
Two Examples of the Social Determinants of Mental Health
In our previous Focus article on the social determinants of mental health (1), we used the examples of income inequality and poor education to illustrate the clinical and policy relevance of the social determinants of mental health. Here, we explore two other social determinants of mental health—discrimination and food insecurity, because they are commonly neglected by our profession—to further expand on approaches to addressing the underlying public policies and social norms.
Discrimination is a powerful social determinant of mental health, with outcomes more robust in affecting mental health than general medical health. In fact, data on the effect of discrimination are inconsistent around general health outcomes but much clearer and more widely available when considering mental health outcomes (8). Discrimination exists in many forms and is targeted at people with specific demographic characteristics of age, gender, race, ethnicity, sexual orientation/preference, nationality, and religion. With available data, much of the analysis, particularly in the United States, has examined the effects of racial and ethnic discrimination, and most of the data focus on perceived discrimination among African Americans. Some of the various types of discrimination, along with definitions and examples of each, are given in Table 1 (9, 10).
TABLE 1.
Types, definitions, and examples of discrimination
| Type of discrimination | Definition | Example |
|---|---|---|
| Interpersonal (individual) | Face-to-face or covert acts of discrimination toward a person | Physician’s implicit bias that leads to poorer treatment of a patient |
| Institutional (organizational) | Policies and practices within and across institutions that disadvantage certain groups | Denial of mortgage applications to black and Latinx populations compared with white populations with similar credit histories |
| Structural (systemic) | A system in which public policies, institutional practices, cultural representations, and other norms work in various, often reinforcing, ways to perpetuate group inequities | Mass incarceration and its disproportionate effects on people of color |
| Legal (de jure) | Discrimination that is mandated by law | Jim Crow laws; racial housing covenants |
| Illegal (de facto) | Discrimination that is without legal basis but sanctioned by custom or practice | Underrepresentation of women and minorities in leadership roles in medicine |
| Overt | Blatant forms of discrimination | Racist or sexist epithets |
| Covert | Subtle forms of discrimination | Microaggressions |
Discrimination has been tied to multiple mental health conditions—including posttraumatic stress disorder, major depressive disorder, and generalized anxiety disorder—and poor self-rated mental health (11). Again, although much of the evidence shows that perceived discrimination against African Americans leads to poor mental health outcomes, robust findings have also been documented with regard to perceived discrimination among Native Americans; Asian Americans; Latinx populations; transgender youth; lesbian, gay, and bisexual populations; people of Jewish and Muslim faiths; and other populations that commonly experience discrimination (12–18). In addition, perceived discrimination (commonly measured by the Everyday Discrimination Scale) (19) can lead to a worsening of other social determinants, including poor access to health care, housing, and employment opportunities; income inequality; and a greater likelihood of experiencing adverse features of the built environment. The concept of perceived discrimination is, indeed, worth exploring, in that the negative effects are not dependent on whether an individual has actually been discriminated against; the perception that one has been discriminated against is enough for an individual to experience the negative effects of discrimination. Nonetheless, we know that discrimination remains rampant in society, and as such, members of minority groups continuously perceive that discrimination.
Although considering individual- and clinical-level interventions is important, the types of interventions that will be most effective in addressing this social determinant are upstream interventions that work to dismantle structural racism, sexism, and other systemic forms of discrimination at their roots. Within health care, this includes examining the many built-in inequities in the health care delivery system, including inequities in access to mental health care such as insurance inequities and a workforce that is unable and unequipped to meet the needs of those seeking mental health services because of high levels of implicit bias and a lack of cultural humility and structural competence (20, 21). Similarly, comprehensive, active plans to dismantle systemic racism in medicine, as well as across other systems, including those pertaining to housing, food access, employment, and income, must be undertaken to make progress in addressing discrimination as a social determinant of mental health. Part of this work involves helping educate individuals on the pervasiveness of structural racism and its history of being solidified and perpetuated as a social norm in the United States. Most important, to effectively reduce systemic racism and discrimination, policies must be enacted to dismantle the structures that have been created over centuries along racialized and gendered lines.
Our second example of a social determinant of mental health—which, like discrimination, is not entirely considered by most psychiatrists—is food insecurity. The United Nations notes that food security means that all people, at all times, have physical, social, and economic access to sufficient, safe, and nutritious food that meets their food preferences and dietary needs for an active and healthy life (22). Unfortunately, too many people—even in the United States, where there is an overabundance of food and even when the mechanics and logistics of ensuring equal access to food should be readily attainable—live with food insecurity. Food insecurity occurs at the family or individual level when the availability of nutritionally adequate and safe foods is limited or uncertain, most often because of financial constraints. Food insecurity is an ongoing public health problem, affecting about 12% of U.S. households (23).
Food insecurity is associated with poor nutrition, high health care costs, and poor physical and mental health outcomes. It is a social determinant of health that is linked to a higher probability of obesity (particularly in women), diabetes, hypertension, cardiovascular disease, and oral health problems, to name a few, as well as nutritional deficiencies such as anemia and iron deficiency in pregnant women (24, 25) due to disrupted eating patterns. Some of the associations relate to “poor food choices” that are actually driven by insufficient financial resources (and, thus, not enough options). That is, if one has limited dollars to spend on food, those dollars are usually used to buy inexpensive, calorie-dense foods, which often are highly processed and lacking essential nutrients. What might superficially appear to be poor food choices may, in fact, be an effective means of staving off the uncomfortable physical sensation of being hungry. Food insecurity thus commonly results in reduced consumption of fruits, vegetables, and other micronutrient-rich foods important for proper growth and development and for maintenance of good health (and a concurrent increased consumption of high-calorie foods).
Food insecurity undoubtedly leads to continuous psychological stress: anxiety, frustration, a sense of powerlessness, shame, guilt, and disconnection from others. Psychological and social outcomes of food insecurity include worrying about food access, being forced to acquire food in socially unacceptable ways (e.g., theft), and disruptions in the regularity and content of meals as well as the personal or family rituals around meals. Like perceived discrimination, the ongoing stress that food insecurity creates can trigger diverse physiological stress responses (e.g., a ramped-up stress response of the hypothalamic-pituitary-adrenal axis) that elevate the risk for mental illnesses such as depression and anxiety disorders. Important to note, and as with discrimination, food insecurity likely also worsens course, treatment response, and outcomes among those with existing mental illnesses. Additionally, many individuals with serious mental illnesses have diabetes, metabolic syndrome, and other conditions associated with poor nutrition that contribute to early mortality; food insecurity (which is very common among those with serious mental illnesses) exacerbates those conditions.
Food insecurity has been linked to specific mental illnesses and behavioral conditions, including depression and generalized anxiety disorder, as well as impaired academic performance and social skills and hyperactivity/inattention among children, as reviewed elsewhere (6, 26). Food insecurity is also relevant to poor mental health, beyond associations with specific mental illnesses. One example comes from analyses using data from 149 countries, where food insecurity was associated in a dose–response fashion—independent of socioeconomic and demographic characteristics of respondents—with poorer scores on mental health indices; within-region analyses (11 regions) confirmed these trends (27).
Food security is necessary for good mental health, and good mental health is important to one’s ability to maintain food security. As such, we must screen for and address food insecurity (6) just as we do other social risks in domains such as education, employment, income, and housing. Screening for food insecurity in clinical settings has the potential to limit its adverse effects on patients’ health outcomes and can ensure timely referral of those in need to available food and nutrition support programs, including the Supplemental Nutrition Assistance Program (SNAP; formerly known as food stamps); Special Supplemental Nutrition Program for Women, Infants, and Children (WIC); Child and Adult Care Food Program; school meals; and, if necessary, local emergency food services (e.g., food pantries).
In regard to standardized screening, many electronic health record systems now include prompts for social determinant screening, including a brief food insecurity screening, and allow providers to record responses and provide information on referrals. Given the known time constraints on clinical practice, a straightforward two-question food security screening (which is derived from the 18-item Food Security Supplement by the U.S. Department of Agriculture [USDA] to the Census Bureau’s annual Current Population Survey) is recommended by several national organizations and can be directed toward the individual or with regard to the individual’s household (Box 1). A response of “sometimes true” or “often true” to either question may indicate food insecurity. The purpose of screening is to determine who needs a more extensive evaluation, as exemplified in Box 1, and who would benefit from additional resources and supports.
BOX 1. Two-item screening for food insecurity and examples of questions that clinicians can ask to follow up on a positive screening
Food Insecurity Screening Questions
Now I’m going to read you two statements that people have made about their food situation. Please tell me whether the statement was often true, sometimes true, or never true for (you/your household) in the past 12 months—that is, since last (name current month).
1. (I/We) worried whether (my/our) food would run out before (I/we) got money to buy more.
Was that often true, sometimes true, or never true for (you/your household) in the past 12 months?
2. The food (I/we) bought just didn’t last, and (I/we) didn’t have money to get more.
Was that often true, sometimes true, or never true for (you/your household) in the past 12 months?
[A response of “sometimes true” or “often true” to either question may indicate food insecurity. The purpose of screening is to determine who needs a more extensive evaluation and who would benefit from additional resources and supports.]
Suggested Interview Questions to Follow Up on a Positive Screena
[These are suggested questions to structure a discussion. Bulleted questions are optional and for further probing, if needed.]
Do you currently follow any particular diet?
Tell me about your usual eating habits, like what you eat and when.
Who do you eat with for each of your meals?
Do you have access to clean drinking water?
How many meals do you eat per day?
• When do you eat breakfast, and what do you eat and drink?
• When do you eat lunch, and what do you eat and drink?
• When do you eat dinner, and what do you eat and drink?
• What else do you eat and drink throughout the day?
When and how often do you feel hungry?
Do you have variety in your diet (different fruits, vegetables, grains, and proteins daily)?
• How often do you eat fast food?
• How often do you eat chips, cookies, sweets, or candy?
• How often do you drink soft drinks, sodas, or sweetened tea?
• How often do you eat convenience/packaged foods (e.g., frozen meals or other premade meals)?
Do you eat most meals at home or away from home (food consumed outside the home is more likely to be processed and higher in salt, sugar, and fat, and lower in micronutrients)?
How often do you eat in restaurants, and which ones?
Do you buy your own groceries? If not, who does? If so, where do you shop?
Can you easily access a grocery store (i.e., is there access to a wide variety of healthful food choices, or is access limited to corner/convenience shops)?
Do you have personal transportation, or do you utilize public transportation (the latter may result in limitations on the quantity and type of food that may be purchased at one time)?
Do you have the ability to prepare food at home? What type of cooking equipment do you have (e.g., microwave, oven, cooking tools, pans)?
Do you have the ability to store food safely (e.g., access to refrigerator/freezer)?
What is in your refrigerator right now? And in your cupboards and cabinets?
How do you go about planning your meals, or does someone else plan and provide them for you?
Are you satisfied with your current eating habits? What would you like to be different?
Are you satisfied with your weight? What would you prefer it to be?
How do you think your current eating habits are affecting your health?
Do you have enough to eat? What would you prefer to have more of?
Do you ever cut the size of your meals, skip meals, or feed a child or dependent instead of yourself because there isn't enough money for food?
Do you ever feel hungry but don't eat because there isn't enough money for food?
Do you currently participate in SNAP, WIC, and/or Meals on Wheels programs?
Do you ever obtain food from food pantries or soup kitchens?
Do you ever forget to eat?
aSuggested interview questions were developed by the second author in collaboration with Karli Mack, R.D., C.D.N., and Valerie Messina-Root, R.D., at the New York State Office of Mental Health. SNAP, Supplemental Nutrition Assistance Program; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Many resources are available, including those provided by Feeding America, the largest hunger relief organization in the United States, which organizes a nationwide network of approximately 200 food banks and 60,000 food pantries and meal programs (28, 29). Although many clinicians may be familiar with SNAP, they may be less familiar with other benefits that most states provide beyond the electronic benefits transfer (EBT) itself, such as nutrition outreach and education programs.
Psychiatrists’ and Mental Health Professionals’ Roles
In considering discrimination, the role of the psychiatrist (and other mental health professionals) is one of observing, understanding, commenting on, and helping to change social norms—essentially determining which norms promote or detract from positive mental health. Therefore, mental health professionals have an important responsibility to determine whether social norms pertaining to discrimination, racism, sexism, and social exclusion are advanced and promoted or are outwardly challenged and disavowed. The educator Mary McLeod Bethune said, “If we simply accept and acquiesce in the face of discrimination, we accept the responsibility ourselves. . . . We should, therefore, protest openly everything . . . that smacks of discrimination or slander (30).” This quote is undoubtedly relevant when considering the role of psychiatrists in either tacitly condoning discriminatory behaviors and actions or publicly voicing concerns about these behaviors. This approach to addressing social norms not only is specific to discrimination but also could be effectively applied to all social determinants of mental health.
With regard to food insecurity, diverse policies affect a community’s—as well as an individual’s and family’s—access to sufficient, safe, and nutritious food. At the federal level, the primary policy tool affecting food security is the Farm Bill, which many have heard of but few understand, given its complexity. The Farm Bill is a comprehensive omnibus bill focused on agricultural and food policy; it is renewed about every five years and funds the USDA. The Farm Bill is a mental health bill, given the clear links between food security and mental health. As such, there is an unrealized opportunity for mental health professionals to share their voices. Many other policies pertain to food access and, thus, mental health. Local zoning decisions, for example, affect where food outlets—whether healthy (e.g., organic grocery stores and farmers markets) or unhealthy (like fast food restaurants and gas stations)—are ultimately located within a community.
Conclusions
Ultimately, the laws that society passes do more to change the distribution of opportunity—and thus affect the social determinants of mental health and, in turn, mental health and mental illness outcomes—than clinical interventions. Similarly, social norms clearly shape how we collectively decide to distribute opportunity. Laws and other forms of public policy shape mindsets and social norms, and vice versa. To address discrimination as a social determinant of mental health, antiracist laws, policies, and practices that work to dismantle structural racism will need to be advanced and enacted. Implicit in this advancement is the understanding that addressing discrimination and passing laws that are antiracist do not harm or disadvantage people with privilege or power and that improving the collective and shared social and environmental milieu allows us all to thrive. Likewise, public policies and social norms must be changed to address food insecurity and other social determinants of mental health, ranging from adverse early life experiences to global climate change.
Footnotes
Drs. Shim and Compton report no financial relationships with commercial interests.
References
- 1.Compton MT, Shim RS: The social determinants of mental health. Focus 2015; 13:419–425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shim RS, Compton MT: Addressing the social determinants of mental health: if not now, when? If not us, who? Psychiatr Serv 2018; 69:844–846 [DOI] [PubMed] [Google Scholar]
- 3.Link BG, Phelan J: Social conditions as fundamental causes of disease. J Health Soc Behav 1995; [Supplemental issue]:80–94 [PubMed] [Google Scholar]
- 4.Rose G: The Strategy of Preventive Medicine. Oxford, Oxford University Press, 1992 [Google Scholar]
- 5.Dube SR, Anda RF, Felitti VJ, et al. : Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA 2001; 286:3089–3096 [DOI] [PubMed] [Google Scholar]
- 6.Compton MT, Shim RS: The Social Determinants of Mental Health. Arlington, VA, American Psychiatric Publishing, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roberts LW: The American Psychiatric Association Publishing Textbook of Psychiatry, 7th ed. Washington, DC, American Psychiatric Publishing, 2019 [Google Scholar]
- 8.Williams DR, Neighbors HW, Jackson JS: Racial/ethnic discrimination and health: findings from community studies. Am J Public Health 2003; 93:200–208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krieger N: Embodying inequality: a review of concepts, measures, and methods for studying health consequences of discrimination. Int J Health Serv 1999; 29:295–352 [DOI] [PubMed] [Google Scholar]
- 10.11 Terms You Should Know to Better Understand Structural Racism, Washington, DC, Aspen Institute, 2016. https://www.aspeninstitute.org/blog-posts/structural-racism-definition/ [Google Scholar]
- 11.Paradies Y, Ben J, Denson N, et al. : Racism as a determinant of health: a systematic review and meta-analysis. PLoS One 2015; 10:e0138511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whitbeck LB, McMorris BJ, Hoyt DR, et al. : Perceived discrimination, traditional practices, and depressive symptoms among American Indians in the upper midwest. J Health Soc Behav 2002; 43:400–418 [PubMed] [Google Scholar]
- 13.Hatzenbuehler ML, McLaughlin KA, Keyes KM, et al. : The impact of institutional discrimination on psychiatric disorders in lesbian, gay, and bisexual populations: a prospective study. Am J Public Health 2010; 100:452–459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gee GC: A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. Am J Public Health 2002; 92:615–623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jordanova V, Crawford MJ, McManus S, et al. : Religious discrimination and common mental disorders in England: a nationally representative population-based study. Soc Psychiatry Psychiatr Epidemiol 2015; 50:1723–1729 [DOI] [PubMed] [Google Scholar]
- 16.Cook B, Alegría M, Lin JY, et al. : Pathways and correlates connecting Latinos’ mental health with exposure to the United States. Am J Public Health 2009; 99:2247–2254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mouzon DM, Taylor RJ, Keith VM, et al. : Discrimination and psychiatric disorders among older African Americans. Int J Geriatr Psychiatry 2017; 32:175–182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilson EC, Chen Y-H, Arayasirikul S, et al. : The impact of discrimination on the mental health of trans*female youth and the protective effect of parental support. AIDS Behav 2016; 20:2203–2211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams DR, Mohammed SA: Discrimination and racial disparities in health: evidence and needed research. J Behav Med 2009; 32:20–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tervalon M, Murray-García J: Cultural humility versus cultural competence: a critical distinction in defining physician training outcomes in multicultural education. J Health Care Poor Underserved 1998; 9:117–125 [DOI] [PubMed] [Google Scholar]
- 21.Metzl JM, Hansen H: Structural competency: theorizing a new medical engagement with stigma and inequality. Soc Sci Med 2014; 103:126–133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Food Security, Washington, DC, International Food Policy Research Institute, 2019. http://www.ifpri.org/topic/food-security [Google Scholar]
- 23.Food Security and Nutrition Assistance, Washington, DC, US Department of Agriculture, Economic Research Service, 2019. https://www.ers.usda.gov/data-products/ag-and-food-statistics-charting-the-essentials/food-security-and-nutrition-assistance/ [Google Scholar]
- 24.Gundersen C, Ziliak JP: Food insecurity and health outcomes. Health Aff 2015; 34:1830–1839 [DOI] [PubMed] [Google Scholar]
- 25.Holben DH, Marshall MB: Position of the Academy of Nutrition and Dietetics: food insecurity in the United States. J Acad Nutr Diet 2017; 117:1991–2002 [DOI] [PubMed] [Google Scholar]
- 26.Compton MT: Food insecurity as a social determinant of mental health. Psychiatr Ann 2014; 44:46–51 [Google Scholar]
- 27.Jones AD: Food insecurity and mental health status: a global analysis of 149 countries. Am J Prev Med 2017; 53:264–273 [DOI] [PubMed] [Google Scholar]
- 28.Food Insecurity and Health: A Tool Kit for Physicians and Health Care Organizations, Chicago, Feeding America, 2017. https://hungerandhealth.feedingamerica.org/wp-content/uploads/2017/11/Food-Insecurity-Toolkit.pdf [Google Scholar]
- 29.Health Care Provider Training: Screening for and Addressing Food Insecurity in Clinical Settings, Chicago, Feeding America, 2017. https://hungerandhealth.feedingamerica.org/wp-content/uploads/2014/05/FA_Clinical-Training_2017.pdf [Google Scholar]
- 30.Bethune MM: Certain unalienable rights; in What the Negro Wants. Edited by Logan R. Chapel Hill, University of North Carolina Press, 1944 [Google Scholar]