Abstract
In 2012, the Society for Academic Emergency Medicine convened a consensus conference on the state of medical education research with goals of defining and advancing a future research agenda. Since that time, emergency medicine (EM) education research has grown significantly. A task force of EM education experts was assembled and sought to understand the current state of EM education research and future directions. Among the advances are increases in medical education fellowships, advanced degree and certification programs, faculty development programs, publication venues, and funding. These findings are discussed in light of the prior objectives from the 2012 consensus conference, and recommendations for future directions are provided.
Over a decade ago, leaders in emergency medicine (EM) education identified a need to bring key stakeholders together to form an intentional roadmap to facilitate our specialty’s growth in medical education research. The 2012 Academic Emergency Medicine (AEM) consensus conference “Education Research in Emergency Medicine: Opportunities, Challenges, and Strategies for Success” convened 175 participants who, with the guidance of national and international medical education and research experts, engaged in the work of developing an agenda for EM education research.1 The conference mission was “to stimulate the development of a coordinated initiative within EM to inform a research agenda in education science for the next decade [in order] to advance effective and validated methods of teaching and assessment at all levels” The specific objectives are found in Table 1.
Table 1.
Specific objectives of the 2012 Academic Emergency Medicine consensus conference.1
| 1. Review the current state of research in EM instructional methods and identify the most critical agenda areas within each specific education research domain. |
| 2. Review the current state of research in assessment methods in EM and identify the most critical agenda areas within each core competency. |
| 3. Identify common barriers that educators face in conducting well‐powered, rigorous education research and develop recommendations for overcoming these barriers. |
| 4. Develop a national agenda for strengthening the infrastructure around education research in EM, including: |
| a. Development of postgraduate and longitudinal professional development opportunities for education researchers; |
| b. Constructing a framework for an EM Education Research Consortium designed to foster multi‐institutional and multidisciplinary collaboration; |
| c. Propose a coordinated agenda to promote grant‐funded education research in EM. |
EM, Emergency Medicine
In the years since the conference, our field has seen significant growth in education research training opportunities, EM specialty‐specific venues for publishing education scholarship, and prominence of EM education research leaders in national medical education arenas.2, 3, 4, 5, 6, 7 The topics pursued by EM education researchers have also evolved substantially since 2012 in response to programmatic changes such as the Accreditation Council for Graduate Medical Education (ACGME) milestones project and the influences of novel modalities for education, assessment, and evaluation.8, 9, 10, 11, 12, 13, 14, 15, 16, 17
In 2019, the Society for Academic Emergency Medicine (SAEM) Board of Directors convened a special task force, Advanced Research Methods Evaluation and Design for Medical Education (ARMED MedEd). The mission of this task force is to advance medical education research by providing high‐quality training with a focus on early to midcareer medical education scholars who have some prior knowledge of basic education research principles. All members of the task force were appointed by the SAEM President‐Elect based on their demonstrated expertise in this field. The task force consisted of 12 members ranging from assistant professors to tenured full professors with over 1,000 combined publications. The two objectives for this task force were to: 1) summarize and contextualize the current state of medical education research as a follow up to the 2012 AEM Consensus Conference and 2) design a longitudinal research course whose curriculum is aimed at the early to midcareer medical educator who has basic foundational knowledge of education research methods. To address this first component, the task force sought to identify the degree to which each of the AEM 2012 objectives was met.
The aim of this paper was to describe the progress in EM education research since the 2012 AEM consensus conference. This work will measure and describe changes in formal training opportunities (from episodic faculty development opportunities to dedicated postgraduate fellowships), trends in EM‐sponsored education research funding opportunities, EM education research and publications, and venues for disseminating EM education scholarship. The current state of EM education research will be compared with the 2012 AEM consensus conference objectives as a means to highlight how critical agenda priorities have been addressed by the academic EM community over time. Finally, current gaps and future directions will be considered in order to inform future directions in EM education scholarship.
Methods
The goal of this narrative review is to provide an overview of the growth of education scholarship within the field of EM since the 2012 AEM consensus conference, tracking general trends in publications and identifying infrastructure changes within academic emergency departments that provide ongoing support and faculty development. Given the intent of this article and the breadth of scholarship that falls under the umbrella of “education research,” the goal of our literature review was to illustrate general publications trends rather than to systematically review and synthesize the available literature.18
The authors searched PubMed and Google Scholar for relevant articles using search terms including medical education, health professions education, and emergency medicine, identifying relevant articles and resolving discrepancies by consensus. The authors then summarized the available information, iteratively discussed how these aligned with the 2012 AEM recommendations, as well as existing gaps, and provided recommendations for how to strengthen the support for EM education research. When existing research was unavailable, the task force members directly extracted publication‐level data from major medical journals. In order to assess trends in publication types, the authors reviewed all original research articles in Academic Emergency Medicine over a 5‐year period (2014–2018) and categorized articles by subtype. The authors specifically assessed the percentage of articles that utilized primarily qualitative methodology as this is more common in the health professions education (HPE) literature when compared with the EM literature. Because AEM Education and Training was started in 2017, the authors also assessed qualitative publications among AEM Education and Training from 2017 to 2018. The authors then compared the percentage of published qualitative studies from 2014 to 2016 with 2017 to 2018. To assess grant funding, the authors reviewed all articles published in Academic Medicine and AEM Education Training from 2018 to 2019 and recorded how many original research articles were funded. The authors then compared the percentage of funded articles between the two journals. When assessing medical education fellowship data, the authors utilized the SAEM Fellowship Directory. As there is not a central database for advanced degree programs HPE, degree programs were identified through group consensus, querying of available literature,19, 20, 21 and review of websites from major medical societies frequented by EM educators (e.g., Association of American Medical Colleges, Accreditation Council for Graduate Medical Education, Council of Emergency Medicine Residency Directors, Society of Academic Emergency Medicine). Task force members engaged in regular phone calls and met in‐person at the 2019 SAEM Scientific Assembly, as well as asynchronously using email and GoogleDocs. The advances and recommendations were iteratively derived based on the available literature and recommendations from the group.
Advances in Medical Education Scholarship
Medical Education Fellowships
During the 2012 AEM consensus conference, a breakout group convened to outline the suggested content and structure for medical education fellowships in EM.17, 22 With a handful of fellowships already in existence, the group envisioned the emergence of two primary formats of education fellowships. The first would be focused on teaching, education innovations, and career development. The second would be devoted to developing education scholars and would focus on research training in addition to developing expertise in teaching, education innovations, curriculum design, programmatic assessment, and theories of learning. The second group was suggested to be longer (i.e., at least 2 years in length) to facilitate completion of an optional advanced degree, to allow sufficient time to produce a body of scholarly output, and to position graduates competitively within the academic EM job market.
The past 7 years have seen a steady growth in the number of EM education fellowships across the country.23 While these fellowships were guided by the recommendations put forth in the original consensus conference documents, many of the program‐specific components (e.g., numbers of shifts, funding of degrees) and expected service activities (e.g., serving as an assistant program director or assistant clerkship director) are determined by the individual site.17, 22 In response, the SAEM Fellowship Approval Committee was formed to review and approve non‐ACGME fellowships (e.g., education, global health, administration, wilderness medicine, geriatric EM) to ensure greater uniformity and standards for these fellowships.24 This process was modeled after the approval process SAEM developed for research fellowships and was intended to ensure that non–ACGME‐accredited fellowships share common standards for academic rigor, curricular breadth, and adequate clinical protection. In addition, SAEM maintains a directory of EM fellowships throughout the United States to raise their visibility and accessibility for potential applicants. The directory currently lists 32 active education fellowships in the United States, nine of which are categorized as education scholarship fellowships.23 Of these programs, 17 are 2‐year programs, 11 are 1‐year programs, and four did not have program length data available.
As the academic job market in EM has become more competitive, fellowship training among applicants is increasingly becoming the norm.25, 26 Within the sphere of medical education, chairs in EM have expressed a growing recognition of the importance of education research, as well as the need for well‐trained education researchers.27 However, while there are an increasing number of medical education fellowships, only a limited number are primarily focused on education scholarship.
Advanced Degree or Certification Programs
There has also been substantial growth in the world of structured HPE degree and certification programs. In 1996, there were only seven established HPE degree programs (University of Illinois at Chicago, University of Southern California, University of Calgary, Cardiff University, University of Dundee, University of Maastricht, and University of New South Wales). In 2012, there were 76 HPE degree programs worldwide.19 By 2013, the number had increased to 121 programs around the world.20 Similarly, doctoral programs have started becoming de rigeur; in 2014, there were 24 PhD programs focused on HPE, with many other adjunctive disciplines (e.g., psychology, generalist education, psychometrics/assessment, sociology, anthropology, kinesiology) also training scientists who enter into HPE.21
Beyond these formal degree programs, there are other advanced certifications being developed in various jurisdictions to train clinical educators. Similar to the medical education fellowships described previously, these programs target advanced or fully qualified clinicians. In the United Kingdom, there is the Academy of Medical Educators,28 which aims to raise the capacity of medical and veterinary educators via their certification program. More recently, the Royal College of Physicians and Surgeons of Canada developed their Clinician Educator Area of Focus Competency Diploma program.29 This is a competency‐based, time‐variable, professional development program leading to an advanced designation.30 These emerging programs represent a new group of clinically relevant, skills‐based training for interested educators. These programs aim to raise capacity in educators’ skills, providing a more practical training opportunity for those interested in the application of theory into practice.
Faculty Development Programs
In addition to fellowships and advanced degrees, external faculty development programs are also on the rise. Interprofessional courses, such as the Harvard Macy Program for Educators in Health Professions and the Association of American Medical Colleges’ (AAMC) Medical Education Research Certificate (MERC) programs, offer interprofessional opportunities for learning teaching and curricular best practices as well as the basics of education research. While few specialty‐specific faculty development programs existed,31, 32, 33 the “MERC at CORD Scholars Program” within the community of EM educators provided an innovative structure for longitudinal project development, interinstitutional collaborations, and mentorship.34, 35, 36
With the advent of the Free Open Access Medical education (FOAM) movement, initiatives like the Academic Life in Emergency Medicine (ALiEM) Medical Education in Cases series,37 the Education Theory Made Practical electronic books,38 the Simulcast podcast for simulation educators,39 and the KeyLIME podcast40 have all emerged to help with the mission of fostering the continuing development of clinician educators and scholars.41, 42, 43
There has also been an increase in more robust faculty development offerings in medical education at university‐ or hospital‐affiliated institutions, as well as at the national level.36, 44, 45, 46, 47 Externally, faculty development courses have also sprung up. Courses run by The Teaching Co‐Op,48 Medutopia,49 ALiEM Faculty Incubator,50 and Emergency Medicine Educators Course51 have emerged, developed by interested and entrepreneurial educators looking to improve education.16
Publication Venues and Research
An earlier study of EM academic leaders perceived a lack of venues for publishing education scholarship.52 In recent years, there has been an increase in the number of outlets for medical education research. The number of HPE journals listed in the AAMC Annotated Bibliography of Journals for Education Scholarship increased 20% between 2016 and 2017.53 More specifically, the number of outlets for medical education research within EM has also increased. Examples of newer journals and special issues focused on EM education research include AEM Education and Training, Journal of Education and Teaching in Emergency Medicine (JETem), and the annual Council of Emergency Medicine Residency Directors/Clerkship Directors in Emergency Medicine supplemental issue of the Western Journal of Emergency Medicine. Many of these were developed in direct response to the needs identified by the AEM consensus conference. These offer increased opportunities for publishing medical education research within EM as well as allowing for targeted EM‐specific education research to be published.
As a result of many of the above initiatives, there has been a significant increase in the number of medical education and HPE publications within EM. A search of PubMed from 2010 to 2018 assessing for the number of publications on medical education and health professions education in association with EM identified a greater than threefold increase in publications from 2010 to 2018 (Figure 1).
Figure 1.
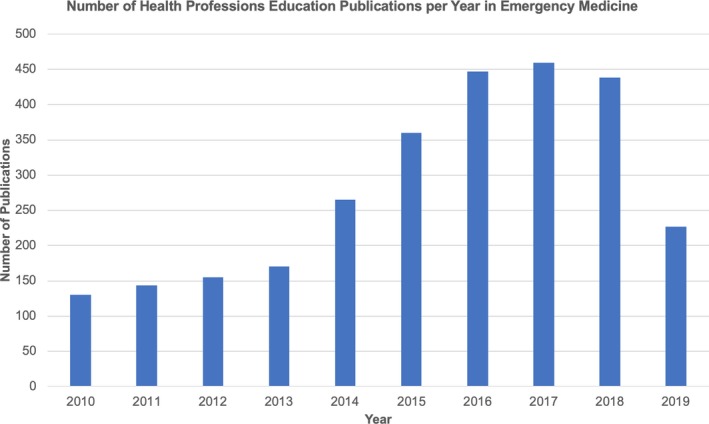
Number of articles per year searching PubMed for (“Medical Education” OR “Health Professions Education”) AND “Emergency Medicine” from 2010 to 2018 (search performed June 14, 2019).
Additionally, there has been an overall increase in the quality of education research and expectations from EM and other fields.4, 53, 54, 55, 56, 57, 58, 59, 60, 61 As consumers of research, educators are looking for more rigorous methods and conceptual frameworks in published research.54 In fact, the overall impact factor of medical education publications has also been increasing over time, which is likely due to a combination of greater number of publications and higher‐quality research.62 EM education researchers are increasingly publishing in both EM and non‐EM journals.63 This has resulted in increasing application of methods that are more common in other fields, such as the social sciences.
One example is the increased use of qualitative research within the EM literature. Historically, qualitative methods were rarely represented in traditional EM journals, but with increased availability of education‐focused journals, the method was increasingly appreciated and accepted. This can be seen when comparing data in Academic Emergency Medicine from 2014 to 2016 with 2017 and 2018, wherein the percentage of qualitative publications increased from 2.8% to 4.2%. Of note, AEM Education and Training was created as a companion journal to Academic Emergency Medicine in 2017. During that same period in 2017 and 2018, 11.4% of all publications in AEM Education and Training used qualitative methods. This suggests an increased recognition of qualitative research within more traditional EM and EM education journals. As this trend grows, there will be an increased need for more peer reviewers with expertise in social science– and education‐based research methodology to match the rise in these publications.
Funding
Following the rapid growth of EM education fellowships and EM‐specific HPE journals, there has been increased recognition of the need for investment and support for new scholars and research in this emerging field.6 External funding has been shown to be a crucial step toward the maturation of successful investigators and increasing the knowledge base complexity of publications.64 One series of articles evaluating EM education research found that the number of funded studies increased from 16% in 2014 to 20% in 2015, although this declined to 11% in 2016.4, 60, 61 We conducted a review of all publications from 2018 and 2019 in AEM Education and Training and found that 34% of original manuscripts had reported some form of funding. By contrast, the multidisciplinary medical education journal Academic Medicine had 41% of original literature publications reported some form of funding. This is encouraging, although further research is needed to better quantify the amount, breadth, competitiveness, and sources of funding as well as the role that funding plays in medical education research success.
Importantly, investment in primary investigators takes several forms as they mature within their field. While initial internal support is integral for a new investigator, sustained and often increasing demands for funding necessitate external support from other funding agencies. Within the clinical and basic sciences, receiving initial K12 grant funding through the National Institute of Health (NIH) has been associated with significant increases in future grant funding and scholarly productivity within EM.65 While NIH funding is limited, there have been increasing numbers of specialty‐specific funding opportunities for EM HPE research through organizations such as the American College of Emergency Physicians,66 the Canadian Association of Emergency Physicians,67 the Council of Emergency Medicine Residency Directors,68 the Emergency Medicine Foundation,69 and the Society for Academic Emergency Medicine.70 However, the number of funding opportunities remains limited and it is essential that, as a specialty, we work to both increase internal and external funding opportunities and develop frameworks for education researchers to overcome funding obstacles through collaboration.
Discussion
The objectives set forth for the 2012 AEM Consensus Conference have progressed at varying rates and the community of education scholars in EM has grown in numbers and quality.
Objective 1: Review the Current State of Research in EM Instructional Methods and Identify the Most Critical Agenda Areas Within Each Specific Education Research Domain
This objective established a baseline for experts in the discipline and identified a process by which the domain of education research could advance in a manner similar to emergency care research, by applying translational research principles (Table 2).71 The T1 level aims to take theoretical research and apply results to patient care in controlled settings. For medical education research, this involves applying cognitive, psychological, and educational principles and theories to learners in classrooms, simulation centers, and clinical settings to understand how theories behave in learners.72, 73 The T2 level translates clinical trials outcomes to generate treatment guidelines to be applied broadly to patient care. In medical education research, once the learning process is understood, guidelines for educators can be developed and ideal educational methods for various types of learning needs can be identified.74 The T3 level broadens the scope of effective treatments to populations for a greater impact. An example in medical education research is the widespread adoption of simulation as a means to teach about a variety of teamwork, procedural, and rare patient conditions to learners.75
Table 2.
Comparison of Emergency Care Research and Health Professions Research using a Translational Research Model
| Translational Research Level | Emergency Care Research | Medical Education Research |
|---|---|---|
| T1 | Bench research and clinical trials | Cognitive education theory and how learners learn in situ |
| T2 | Clinical research and evidence‐based guidelines | Learner processing and educational program comparisons, development of practice guidelines for educators |
| T3 | Individual patient care and population care | Individual modalities, widespread standard of education practice, and impact on patient care |
Adapted from Santen et al.71
Objective 2: Review the Current State of Research in Assessment Methods in EM and Identify the Most Critical Agenda Areas Within Each Core Competency
Assessment strategies in medical education were a relatively nascent field at the time of the AEM Consensus Conference. Educators at all levels were interested in finding optimal methods for assessing their learners. This was also at a time when core competencies in residency education were being modified to identify milestone‐based subcompetencies.76 The conference’s keynote address, “The focus on competencies and individual learner assessment as emerging themes in medical education research” set the stage for eight of the breakout consensus sessions. Assessment has been a popular focus of education research in the ensuing years since the consensus conference.
Objective 3: Identify Common Barriers that Educators Face in Conducting Well‐powered, Rigorous Education Research and Develop Recommendations for Overcoming These Barriers
Educators have reported barriers in obtaining protected time, departmental support, and funding for their research.77 They cited a lack of proper training in research methods and unavailability of appropriate training programs to develop this skill set.77 As described in our paper, numerous specialized fellowships have arisen and there are both society‐driven and institutionally‐driven short courses to establish basic knowledge. With these options, educators are now ready to advance their skills in research and scholarship. The emergence of graduate degree programs and focused longitudinal courses for intermediate skill development, such as ARMED MedEd, aim to further fill this need.
Objective 4: Develop a National Agenda for Strengthening the Infrastructure Around Education Research in EM, Including
Development of postgraduate and longitudinal professional development opportunities for education researchers;
Constructing a framework for an EM Education Research Consortium designed to foster multi‐institutional and multidisciplinary collaboration;
Propose a coordinated agenda to promote grant‐funded education research in EM.
Educators who are research experts began to address the task of strengthening the infrastructure by designing and implementing fellowships in education scholarship for graduates of EM residency programs.78 The creation of the Fellowship Approval Committee at SAEM is a good first step toward standardization of educational goals and objectives of education scholarship fellowships. Additional programs, such as MERC and the ALiEM Faculty Incubator, are longitudinal programs that have been developed to help address these needs.16, 34, 35, 36
With the increased number of trained researchers, informal networks and consortia have formed to create multi‐institutional collaborations. However, the establishment of a formal education research consortium remains a desired outcome among the community of researchers. Enacting this type of structured system would provide greater knowledge sharing and improve generalizability of educational innovations. Expansion of this network to include education researchers from medical school departments of education and scholars who practice in various clinical disciplines would further enhance the collaborative research enterprise.
A major barrier to high‐quality research is the lack of funding available to education researchers. In general, funded research is of higher quality and the availability of targeted sources for education research is limited.6, 64 However, limited mentorship and the absence of prior research funding remain major barriers to future research.79 Future efforts are needed to increase medical education research mentorship and funding to continue to advance this field.
Conclusion
The 2012 Academic Emergency Medicine consensus conference was instrumental in gathering like‐minded experts with a goal of establishing an agenda for advancing the field of emergency medicine education research. Since that time, there have been significant advances in the field with respect to education, training, publication outlets, and funding for education researchers. However, despite these advances, we recognize a need for greater development and collaboration among investigators to continue the growth and sophistication of scholarship within the field. Scholarship in medical education requires unique knowledge and skills that are often not taught during medical school or residency training. This has contributed to a need for additional and advanced training, as evidenced by the increasing number of fellowships, degree and certification programs, and faculty development programs. Finally, individual institutions, as well as large funding agencies, must recognize the value of supporting continued training and collaboration to allow individual investigators to continue their growth. This will drive not only individual success but also that of the field at large.
AEM Education and Training 2020;4:S57–S66
The authors have no relevant financial information to disclose.
MG serves as Chief Academic Officer for the ALiEM Faculty Incubator. TMC serves as Chief Strategic Officer of the ALiEM Faculty Incubator. The other authors have no potential conflicts to disclose.
Author contributions: All authors contributed to the study concept and design, acquisition of the data, analysis and interpretation of the data, drafting of the manuscript, and critical revision of the manuscript for important intellectual content.
References
- 1. LaMantia J, Deiorio NM, Yarris LM. Executive summary: education research in emergency medicine‐opportunities, challenges, and strategies for success. Acad Emerg Med 2012;19:1319–22. [DOI] [PubMed] [Google Scholar]
- 2. Jordan J, Coates WC, Clarke S, et al. Exploring scholarship and the emergency medicine educator: a workforce study. West J Emerg Med 2017;18:163–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gottlieb M, Dehon E, Jordan J, et al. Getting published in medical education: overcoming barriers to scholarly production. West J Emerg Med 2018;19:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dubosh NM, Jordan J, Yarris LM, et al. Critical appraisal of emergency medicine educational research: the best publications of 2016. AEM Educ Train 2018;3:58–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yarris LM, Jordan J, Coates WC. Education scholarship fellowships: an emerging model for creating educational leaders. J Grad Med Educ 2016;8:668–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gottlieb M, Lee S, Burkhardt J, et al. Show me the money: successfully obtaining grant funding in medical education. West J Emerg Med 2019;20:71–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chan TM, Gottlieb M, Fant AL, et al. Academic primer series: five key papers fostering educational scholarship in junior academic faculty. West J Emerg Med 2016;17:519–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Accreditation Council for Graduate Medical Education . Emergency Medicine Milestones. Available at: https://www.acgme.org/Specialties/Milestones/pfcatid/7/Emergency%2520Medicine. Accessed August 6, 2019.
- 9. Cadogan M, Thoma B, Chan TM, Lin M. Free Open Access Meducation (FOAM): the rise of emergency medicine and critical care blogs and podcasts (2002–2013). Emerg Med J 2014;31:e76–7. [DOI] [PubMed] [Google Scholar]
- 10. Choo EK, Ranney ML, Chan TM, et al. Twitter as a tool for communication and knowledge exchange in academic medicine: a guide for skeptics and novices. Med Teach 2015;37:411–6. [DOI] [PubMed] [Google Scholar]
- 11. Chan TM, Jo D, Shih AW, et al. The Massive Online Needs Assessment (MONA) to inform the development of an emergency haematology educational blog series. Perspect Med Educ 2018;7:219–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gottlieb M, Wagner E, Wagner A, Chan T. Applying design thinking principles to curricular development in medical education. AEM Educ Train 2017;1:21–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. King AM, Gottlieb M, Mitzman J, Dulani T, Schulte SJ, Way DP. Flipping the classroom in graduate medical education: a systematic review. J Grad Med Educ 2019;11:18–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Estes M, Gopal P, Siegelman JN, Bailitz J, Gottlieb M. Individualized interactive instruction: a guide to best practices from the council of emergency medicine residency directors. West J Emerg Med 2019;20:363–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gottlieb M, Riddell J, Crager SE. Alternatives to the conference status quo: addressing the learning needs of emergency medicine residents. Ann Emerg Med 2016;68:423–30. [DOI] [PubMed] [Google Scholar]
- 16. Chan TM, Gottlieb M, Sherbino J, et al. The ALiEM faculty incubator: a novel online approach to faculty development in education scholarship. Acad Med 2018;93:1497–502. [DOI] [PubMed] [Google Scholar]
- 17. Coates WC, Lin M, Clarke S, et al. Defining a core curriculum for education scholarship fellowships in emergency medicine. Acad Emerg Med 2012;19:1411–8. [DOI] [PubMed] [Google Scholar]
- 18. Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J 2009;26:91–108. [DOI] [PubMed] [Google Scholar]
- 19. Tekian A, Harris I. Preparing health professions education leaders worldwide: a description of masters‐level programs. Med Teach 2012;34:52–8. [DOI] [PubMed] [Google Scholar]
- 20. Tekian A, Roberts T, Batty HP, Cook DA, Norcini J. Preparing leaders in health professions education. Med Teach 2014;36:269–71. [DOI] [PubMed] [Google Scholar]
- 21. Tekian A. Doctoral programs in health professions education. Med Teach 2014;36:73–81. [DOI] [PubMed] [Google Scholar]
- 22. Yarris LM, Coates WC, Lin M, et al. A suggested core content for education scholarship fellowships in emergency medicine. Acad Emerg Med 2012;19:1425–33. [DOI] [PubMed] [Google Scholar]
- 23. Society for Academic Emergency Medicine . Fellowship Directory. Available at: https://member.saem.org/SAEMIMIS/SAEM_Directories/Fellowship_Directory/SAEM_Directories/P/FellowshipList.aspx. Accessed August 6, 2019.
- 24. Society for Academic Emergency Medicine . Fellowship Approval Program. Available at: https://www.saem.org/resources/services/fellowship-approval-program. Accessed August 6, 2019.
- 25. Stern S. Fellowship training: a necessity in today's academic world. Acad Emerg Med 2002;9:713–6. [DOI] [PubMed] [Google Scholar]
- 26. Jordan J, Hwang M, Kaji KH, Coates WC. Scholarly tracks in emergency medicine residency programs are associated with increased choice of academic careers. West J Emerg Med 2018;19:593–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Clarke SO, Jordan J, Yarris LM, et al. The view from the top: academic emergency department chairs' perspectives on education scholarship. AEM Educ Train 2017;2:26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Academy of Medical Educators. Available at: https://www.medicaleducators.org/. Accessed October 11, 2019.
- 29. Royal College of Physicians and Surgeons of Canada . Clinician Educator Diploma Program Available at: http://www.royalcollege.ca/rcsite/credentials-exams/exam-eligibility/clinician-educator-diploma-e. Accessed October 11, 2019.
- 30. Sherbino J, Frank JR, Snell L. Defining the key roles and competencies of the clinician‐educator of the 21st century: a national mixed‐methods study. Acad Med 2014;89:783–9. [DOI] [PubMed] [Google Scholar]
- 31. Friedrich MJ. Harvard Macy Institute helps physicians become better educators and change agents. JAMA 2002;287:3197–9. [PubMed] [Google Scholar]
- 32. Armstrong EG, Doyle J, Bennett NL. Transformative professional development of physicians as educators: assessment of a model. Acad Med 2003;78:702–8. [DOI] [PubMed] [Google Scholar]
- 33. Armstrong EG, Barsion SJ. Using an outcomes‐logic‐model approach to evaluate a faculty development program for medical educators. Acad Med 2006;81:483–8. [DOI] [PubMed] [Google Scholar]
- 34. Coates WC, Love JN, Santen SA, et al. Faculty development in medical education research: a cooperative model. Acad Med 2010;85:829–36. [DOI] [PubMed] [Google Scholar]
- 35. Love JN, Coates WC, Santen SA, Hobgood CD, Mavis BE, Farrell SE. The MERC at CORD Scholars Program in medical education research: a novel faculty development opportunity for emergency physicians. Acad Emerg Med 2009;16:S37–41. [DOI] [PubMed] [Google Scholar]
- 36. Love JN, Yarris LM, Santen SA, et al. A novel specialty‐specific, collaborative faculty development opportunity in education research: program evaluation at five years. Acad Med 2016;91:548–55. [DOI] [PubMed] [Google Scholar]
- 37. Academic Life in Emergency Medicine . Medical Education in Cases. Available at: https://www.aliem.com/medic/. Accessed October 11, 2019.
- 38. Academic Life in Emergency Medicine . Education Theory Made Practical Series: An ALiEM Faculty Incubator Project. Available at: https://www.aliem.com/education-theory-made-practical-series/. Accessed October 11, 2019.
- 39. Simulcast: A Hi‐Fidelity Podcast About Healthcare Simulation Available at: http://simulationpodcast.com/. Accessed October 11, 2019.
- 40. KeyLIME: Key Literature in Medical Education Available at: https://keylimepodcast.libsyn.com/. Accessed October 11, 2019.
- 41. Chan TM, Thoma B, Lin M. Creating, curating, and sharing online faculty development resources: the medical education in cases series experience. Acad Med 2015;90:785–9. [DOI] [PubMed] [Google Scholar]
- 42. Chan TM, Gottlieb M, Sherbino J, Boysen‐Osborn M, Papanagnou D, Yarris L, editors. Education Theory Made Practical (1st ed.). eBook. San Francisco, CA; Academic Life in Emergency Medicine, 2017. Available at: https://www.aliem.com/2017/08/education-theory-made-practical-volume-1/. Accessed August 6, 2019.
- 43. Gottlieb M, Chan TM, Krzyzaniak S, Grossman C, Robinson D, Papanagnou D, editors. Education Theory Made Practical: Volume 2 (1st ed.). Digital File. San Francisco, CA: Academic Life in Emergency Medicine, 2018. Available at: https://www.aliem.com/2018/11/education-theory-made-practical-volume-2-ebook/. Accessed August 6, 2019.
- 44. Leslie K, Baker L, Egan‐Lee E, Esdaile M, Reeves S. Advancing faculty development in medical education: a systematic review. Acad Med 2013;88:1038–45. [DOI] [PubMed] [Google Scholar]
- 45. Steinert Y, Mann K, Anderson B, et al. A systematic review of faculty development initiatives designed to enhance teaching effectiveness: a 10‐year update: BEME Guide No. 40. Med Teach 2016;38:769–86. [DOI] [PubMed] [Google Scholar]
- 46. LaMantia J, Yarris LM, Dorfsman ML, Deiorio NM, Wolf S. The Council of Emergency Medicine Residency Directors' (CORD) Academy for Scholarship in Education in Emergency Medicine: a five‐year Update. West J Emerg Med 2017;18:26–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Jordan J, Dorfsman ML, Wagner MJ, Wolf SJ. The Council of Emergency Medicine Residency Directors academy for scholarship coaching program: addressing the needs of academic emergency medicine educators. West J Emerg Med 2019;20:105–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. The Teaching Co‐Op. Available at: https://www.theteachingcoop.com/. Accessed October 11, 2019.
- 49. Medutopia. Available at: https://www.mymedutopia.com/. Accessed October 11, 2019.
- 50. Academic Life in Emergency Medicine . The ALiEM Faculty Incubator. Available at: https://www.aliem.com/faculty-incubator/. Accessed October 11, 2019.
- 51. The Emergency Medicine Educators Course. Available at: http://www.the-emec.com/. Accessed October 11, 2019.
- 52. Jordan J, Jones D, Williams D, Druck J. Publishing venues for education scholarship: a needs assessment. Acad Emerg Med 2016;23:731–5. [DOI] [PubMed] [Google Scholar]
- 53. AAMC‐Regional Groups on Educational Affairs (GEA) . Annotated Bibliography of Journals for Education Scholarship. Available at: https://www.aamc.org/download/456646/data/annotated-bibliography-of-journals-july-2017.pdf. Accessed August 6, 2019.
- 54. Sullivan GM, Simpson D, Cook DA, et al. Redefining quality in medical education research: a consumer's view. J Grad Med Educ 2014;6:424–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Farrell SE, Coates WC, Khun GJ, Fisher J, Shayne P, Lin M. Highlights in emergency medicine medical education research: 2008. Acad Emerg Med 2009;16:1318–24. [DOI] [PubMed] [Google Scholar]
- 56. Kuhn GJ, Shayne P, Coates WC, et al. Critical appraisal of emergency medicine educational research: the best publications of 2009. Acad Emerg Med 2010;17:S16–25. [DOI] [PubMed] [Google Scholar]
- 57. Shayne P, Coates WC, Farrell SE, et al. Critical appraisal of emergency medicine educational research: the best publications of 2010. Acad Emerg Med 2011;18:1081–9. [DOI] [PubMed] [Google Scholar]
- 58. Fisher J, Lin M, Coates WC, et al. Critical appraisal of emergency medicine educational research: the best publications of 2011. Acad Emerg Med 2013;20:200–8. [DOI] [PubMed] [Google Scholar]
- 59. Farrell SE, Kuhn GJ, Coates WC, et al. Critical appraisal of emergency medicine education research: the best publications of 2013. Acad Emerg Med 2014;21:1274–83. [DOI] [PubMed] [Google Scholar]
- 60. Yarris LM, Juve AM, Coates WC, et al. Critical appraisal of emergency medicine education research: the best publications of 2014. Acad Emerg Med 2015;22:1327–36. [DOI] [PubMed] [Google Scholar]
- 61. Heitz CR, Coates W, Farrell SE, Fisher J, Juve AM, Yarris LM. Critical appraisal of emergency medicine educational research: the best publications of 2015. Acad Emerg Med 2017;24:1212–25. [DOI] [PubMed] [Google Scholar]
- 62. Scimago Journal and Country Rank: Education. Available at: https://www.scimagojr.com/journalrank.php?category=3304. Accessed August 6, 2019.
- 63. Munzer BW, Love J, Shipman BL, et al. An analysis of the top‐cited articles in emergency medicine education literature. West J Emerg Med. 2017;18:60–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Reed DA, Cook DA, Beckman TJ, Levine RB, Kern DE, Wright SM. Association between funding and quality of published medical education research. JAMA 2007;298:1002–9. [DOI] [PubMed] [Google Scholar]
- 65. Newgard CD, Morris CD, Smith L, et al. The first National Institutes of Health institutional training program in emergency care research: productivity and outcomes. Ann Emerg Med 2018;72:679–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. American College of Emergency Physicians . Section Grants. Available at: https://www.acep.org/how-we-serve/sections/sections-grants/. Accessed October 11, 2019.
- 67. Canadian Association of Emergency Physicians . Available Grants. Available at: https://caep.ca/research/grant-competition/. Accessed October 11, 2019.
- 68. Council of Emergency Medicine Residency Directors . CORD Grants. Available at: https://www.cordem.org/opportunities/cord-grants/. Accessed October 11, 2019.
- 69. Emergency Medicine Foundation .Grant Opportunities. Available at: https://www.emfoundation.org/grants/apply-for-a-grant/. Accessed October 11, 2019.
- 70. Society for Academic Emergency Medicine . Grants. Available at: https://www.saem.org/saem-foundation/grants. Accessed October 11, 2019.
- 71. Santen SA, DeIorio NM, Gruppen LD. Medical education research in the context of translational science. Acad Emerg Med 2012;19:1323–7. [DOI] [PubMed] [Google Scholar]
- 72. Eva KW. What every teacher needs to know about clinical reasoning. Med Educ 2005;39:98–106. [DOI] [PubMed] [Google Scholar]
- 73. Ilgen JS, Bowen JL, McIntyre LA, et al. Comparing diagnostic performance and the utility of clinical vignette‐based assessment under testing conditions designed to encourage either automatic or analytic thought. Acad Med 2013;88:1545–51. [DOI] [PubMed] [Google Scholar]
- 74. Goyal N, Aldeen A, Leone K, Ilgen JS, Banzetti J, Kessler C. Assessing medical knowledge of emergency medicine residents. Acad Emerg Med 2012;19:1360–5. [DOI] [PubMed] [Google Scholar]
- 75. McGaghie WC, Draycott TJ, Dunn WF, Lopez CM, Stefanidis D. Evaluating the impact of simulation on translational patient outcomes. Simul Healthc 2011;6:S42–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Beeson MS, Holmboe ES, Korte RC, et al. Initial validity analysis of the emergency medicine milestones. Acad Emerg Med 2015;22:838–44. [DOI] [PubMed] [Google Scholar]
- 77. Jordan J, Coates WC, Clarke S, et al. The uphill battle of performing education scholarship: barriers educators and education researchers face. West J Emerg Med 2018;19:619–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Coates WC, Runde DP, Yarris LM, et al. Creating a cadre of fellowship‐trained medical educators: a qualitative study of faculty development program leaders' perspectives and advice. Acad Med 2016;91:1696–704. [DOI] [PubMed] [Google Scholar]
- 79. Coates WC, Yarris LM, Clarke SO, et al. Research pioneers in emergency medicine‐reflections on their paths to success and advice to aspiring researchers: a qualitative study. Ann Emerg Med 2019;73:555–64. [DOI] [PubMed] [Google Scholar]


