Abstract
Background
Ceftriaxone is one of the most common types of antibiotics used to treat most deadly bacterial infections. One way to alleviate the side effects of medication is to reduce drug consumption by changing the ordinary drug forms into nanostructured forms. In this study, a nanostructured lipid carrier (NLC) containing hydrophilic ceftriaxone sodium drug is developed, and its effect on eliminating gram-negative bacteria Escherichia coli death is investigated.
Methods
Double emulsion solvent evaporation method is applied to prepare NLC. Mathematical modeling based on the solubility study is performed to select the best materials for NLC preparation. Haftyzer-Van Krevelen and Hoy’s models are employed for this purpose. Drug release from optimized NLC is examined under in vitro environment. Then, the efficacy of the optimized sample on eliminating gram-negative bacteria Escherichia coli is investigated.
Results
Mathematical modeling reveals that both methods are capable of predicting drug encapsulation efficiency trends by chaining solid and liquid lipids. However, Haftyzer-Van Krevelen’s method can precisely predict the particle size trend by changing the surfactant types in water and oily phases of emulsions. The optimal sample has a mean particle size of 86 nm and drug entrapment efficiency of 83%. Also, a controlled drug release in prepared nanostructures over time is observed under in-vitro media. The results regarding the effectiveness of optimized NLC in killing Escherichia coli bacteria suggests that by cutting drug dosage of the nanostructured form in half, an effect comparable to that of free drug can be observed at longer times.
Conclusion
Results confirm that NLC structure is an appropriate alternative for the delivery of ceftriaxone drug with a controlled release behavior.
Keywords: Ceftriaxone sodium, Antimicrobial drug resistance, Drug delivery systems, Side effects
Introduction
Ceftriaxone sodium is an antibiotic commonly used for the treatment of bacterial infection such as middle ear infection, meningitis, bone, and joint infection, intra-abdominal infection, skin infection, and pelvic inflammatory diseases [1]. Ceftriaxone vials are among the most prevalent types of antibiotics with the highest mortality rate due to the injection of vials [2]. Ceftriaxone produces several side effects such as diarrhea, elevated liver enzymes, blood urea nitrogen, eosinophilia, thrombocytosis, and other local reactions [1]. Given the inevitability of using this antibiotic in today’s health care system, it is essential to develop new prodrugs [1].
Recently, nanoparticle delivery systems have been employed for the encapsulation of lipophilic, hydrophilic, and poorly water-soluble drugs [3]. The use of lipids for the formation of nanoparticles such as solid lipid nanoparticles (SLN) or nanostructured lipid carrier (NLC), offers multiple benefits compared to other materials, which is due to low cytotoxicity and controlled drug release [4]. The controlled drug release is aimed to maintain drug concentration in the blood or the target tissue at the favorable level [5]. The controlled drug release can be applied to both hydrophilic and hydrophobic drugs. For example, Tamoxifen hydrochloride, as a hydrophilic drug, is encapsulated in a microemulsion system with a controlled release. It is effective in the breast cancer treatment in comparison with the commercial forms of the drug [6]. Raloxifene [7] and Clozapine [8], as hydrophobic drugs in microemulsion and nanostructured lipid forms, have exhibited essential growth in the drug release compared to free dugs.
To date, lipid nanoparticles have been successfully used for hydrophobic drug entrapment, though encapsulating a high content of hydrophilic drugs in these materials is challenging. The key parameters in the preparation of NLC containing hydrophilic drugs are formation method, selection of materials as solid and liquid lipids, and choice of appropriate surfactants used in organic and water phases. Double emulsion solvent evaporation is a technique of NLC preparation that involves hydrophilic drugs [9]. However, the best materials for NLC preparation could be determined by mathematical methods. Group-contribution methods such as Hoy [10, 11] and Hoftyzer-van krevelen [12] are excellent candidates for this purpose. These methods have been successfully applied to predict particle size and drug entrapment efficiency [13, 14].
This is the first study to prepare a nanostructured form of ceftriaxone sodium based on NLC using appropriate controlled drug release. We then test the efficacy of this nanostructure on E.coli bacteria, as a highly resistant gram-negative bacteria, and compare results to that of free drugs. Given that particle size and drug entrapment efficiency have a noticeable effect on the bacteria death efficacy, we also investigate the methods of determining the best materials for forming small-size particles with high drug encapsulation efficiency. Mathematical modeling based on group-contribution methods is utilized for this purpose. Various formulations are explored to investigate the effect of lipid types and surfactants on the particle size and drug entrapment efficiency. The accuracy of mathematical prediction is also evaluated by an experimental study. Finally, the best NLC formulation and a more accurate mathematical model are introduced. The main objectives of the study are as follows:
To determine the accuracy of mathematical modeling based on group-contribution method in predicting the particle size and drug entrapment efficiency.
To determine the effectiveness of ceftriaxone drug in both free and nanostructured forms in cell culture media.
To find the best drug dosage in the nanostructured form to achieve comparable antibacterial efficacy in comparison with the free drug.
To determine rate of bacteria death using NLC form of ceftriaxone drug.
Mathematical modeling
Hoftyzer-Van Krevelen’s method
A group-contribution method for predicting the solubility parameter of components is Hoftyzer-Van Krevelen’s method. In this method, the solubility parameter is calculated from the following equations [12]:
| 1 |
| 2 |
| 3 |
| 4 |
In the above equations, Vm is the molar mass, δd and δp are dispersion and polar forces, δh is the hydrogen bonding of solubility parameters, δt is the total solubility parameter, Fdi and Fpi are dispersion and polarization components in the molar function, respectively, and Ehi is the role of hydrogen bonding force in the tensile energy between molecules.
Hoy’s method
There is another model for predicting the solubility parameter, the equations of which are as follows [11]:
| 5 |
| 6 |
| 7 |
| 8 |
| 9 |
| 10 |
In these equations, α(p) is the number of molecular aggregates in each component, n is units repeated in each part of the molecular chain and B is a constant (equal to 277) [11]. Also, Ft, is the molar attraction function, Fp is its polar components and is the Lydrsen-Hoy constant.
Material selection based on mathematical methods
In this study, two important NLC parameters, particle size and drug entrapment efficiency, are investigated. To examine the trend variation of these parameters, it is necessary to calculate the solubility parameters of all components separately, and then compare their numerical values with each other. The chemical structure of substances plays a crucial role in computing the solubility parameter. The solubility parameter of lipid components and drug can influence drug entrapment efficiency, while the solubility parameter of surfactants and lipids may affect the particle size.
Since natural oils are composed of several components, it is not possible to calculate their solubility parameters. Hence, another effective parameter called hydrophilic to hydrophobic balance (HLB) is used for comparison.
The HLB value of pure lipids is calculated by Eq. 11, while HLB of natural oils such as sesame oil, which is a mixture of different components, is obtained from Eq. 12.
| 11 |
| 12 |
In Eq. 11, K equals 43 in emulsion systems, δd and δp are dispersion and polar forces, respectively, and δh is the hydrogen bonding of solubility parameters. These parameters are obtained from Haftyzer-van Krevelen and Hoy’s methods. In Eq. 12, WA, WB, and WC represent the weight fraction of components A, B, and C, respectively C [15].
Experiments
Materials
Ceftriaxone sodium was purchased from Exir Pharmaceutical Company (Borujerd, Iran). Stearic acid and glycerol mono-stearate as solid lipids, oleic acid as liquid lipids, soy lecithin, Span 80, polyvinyl alcohol (PVA), Tween 80 as surfactants, and ethanol as solvents were purchased from Merck Company. Deionized water was used in all experiments.
Preparation of NLC
In the first step, 0.3 g of GMS (solid lipid) and 0.09 g of oleic acid (liquid lipid) are mixed with 0.95 ml of ethanol (solvent) and 0.055 g of soy lecithin (oil phase). The resulting mixture is placed in a water bath at 60 °C. Then, 0.15 ml deionized water containing 0.2 g/l drug is placed in a water bath (internal water phase). Due to high hydrophilicity of the drug, it dissolves rapidly in deionized water and generates a light yellowish color. We prepare the external water phase containing deionized water and Tween 80 with a concentration of 0.275 g/l and place it in a water bath. Then, the oily solution is homogenized by the ultrasonic probe at 80 rpm for 5 min. Finally, internal and external water phases are added, respectively. After 5 min of ultrasonication, the sample is cooled at 0–4 °C. In the final step, a magnet is inserted inside the sample and it is stirred for 1 h at ambient temperature to evaporate the solvent [16, 17].
Drug entrapment efficiency
A high-performance liquid chromatography analysis is employed to measure drug loading in the NLC structure. Drug loading efficiency is calculated from the amount of drug not loaded in the structure according to Eq. 13:
| 13 |
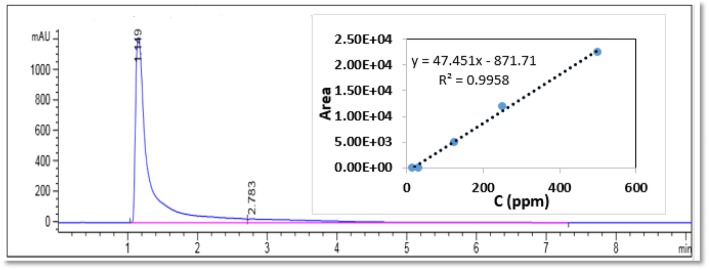
Drug loading was calculated by a high performance liquid chromatographic (HPLC) test using the Agilent 1260 machine. We used C18 column for this purpose. The column diameter and length were 4.6 mm and 100 mm, respectively. The injection volume was 50 μl with a flow rate of 1 ml per min at a pressure of 120 psi and the column temperature of 24 °C. The mobile phase of ceftriaxone drug detection was containing as 95% methanol and 5% water solution. Drug detection was conducted using a UV-visible detector at a wavelength of λ = 240 μm. Figure 1 shows the HPLC diagram. As can be seen, the drug residence time is 1.149 min.
Fig. 1.
HPLC diagram of ceftriaxone sodium drug at a concentration of 500-ppm (internal diagram is HPLC calibration curve)
To calculate the unloaded drug, 5 ml of each sample was centrifuged at 14000 rpm for 20 min at 4 °C. Then, the supernatant solution was transferred from the filter (0.22 μm). After diluting the solution with deionized water with a 1:10 ratio, it was transferred to the chromatography apparatus.
Characterization
Particle size analysis (PSA) and zeta potential of lipid nanoparticles were measured by light scattering analysis (Vasco 3, Cordouan, France). NLC was also diluted with distilled water to obtain a suitable scattering intensity.
The morphology of nanoparticles was measured by the TEM analysis (Leo 912 AB, American). The surface attributes of the sample were determined by an AFM analyzer (Full model Ara pazhoohesh, Iran). Crystallography of samples was examined by X-ray diffraction (XRD) analysis (Bruker D8 Advance, Germany) for lipid, drug, NLC-enricheddrug, and NLC-free drug. To investigate whether all materials are present inside NLC, we conducted the FT-IR analysis for the above four samples (Thermo Nicolet, American)
In vitro drug release
To examine drug efficacy in blood-resembling environment, drug release was implemented under in vitro conditions. PBS buffer at pH = 7.4 was selected for this purpose. Five milliliters NLC sample containing ceftriaxone sodium was placed in a dialysis bag (12 kDa). The same volume of suspension with an identical content of free drug was poured separately into a dialysis bag. The bags were then floated in 50 ml buffer for 48 h in an incubator shaker at 37 °C. After 0.5, 1, 2, 6, 8, 24, and 48 h, 1 ml of the sample was removed from the buffer and the same pure buffer was immediately replaced in the system. Samples were sent to the HPLC machine to determine the amount of drug. According to the HPLC calibration curve, the drug content in each sample was calculated. Then, the profile of drug release versus time was plotted for both pure drug and nanostructure samples. It should be noted that the drug content removed at each sampling time was added to the next dose, and the cumulative effect of the drug was considered in calculations.
Cell culture
In this study, we used the 24-h stratification method for Escherichia coli strain ATCC 35218. For this purpose, the bacterial cell culture was performed in a Muller-Hinton agar medium, a suspension with a half-MacFarland equivalent to 0.85% of normal saline. Under these conditions, the number of bacteria is about 1.5*108 CFU/ml. This suspension was used in the next steps of the experiment [18].
Antibiotic solutions, as free and nanostructure forms, were prepared in sterile distilled water freshly during the day.
MIC determination
To determine the minimum growth inhibitory concentration (MIC) of ceftriaxone in free and nanostructure forms, the broth dilution method (macro dilution) was used under Clinical and Laboratory Standard Institute (CLSI) guidelines [19]. The antibiotic solution (ceftriaxone sodium) was prepared in pre-sterilized water and preserved at − 70 °C in a frozen state until it was used. In the serial dilution, we used concentrations of 0.0078, 0.0156, 0.0312, 0.0625, 0.125, 0.25, 0.5, 1, 2, 4, 8, 16, 32, 64 and 128 μg/mL and a tube as the positive control (no antibiotics). We prepared a 24-h bacterial culture in a sterile suspension physiological serum equivalent to 0.5 McFarland standard turbidity. The culture was followed by incubation of media containing antibiotics, which were then transferred to 35R oven and remained there for 24 h to grow completely. After 24 h, tubers were examined for ocular hyperactivity as a sign of bacteria growth. Any type of opacity (in a specific or concise manner) was considered as resistance to dilution. The minimum concentration of bacteria without visible growth was considered as MIC [19].
Bacterial death kinetics
To plot the bacterial death curve at the specified time, E. coli was cultured on a nutrient agar medium at 37 °C for 24 h. In the next step, 3–5 colonies of pure culture were removed and inoculated in Muller Hinton Broth medium containing a suspension equal to 0.5 MacFarland turbidity in normal saline (0.85%). Under these conditions, the number of bacteria was about 1.5*108 CFU / ml. Then, 100 μl of this standard suspension was added to the culture tubes containing 2 ml of Muller Hinton broth medium, which consisted of the free form of ceftriaxone sodium and nanostructured ceftriaxone sodium with various concentrations. The tubes were placed at 35 °C with continuous movement in a shaker incubator. Then, after 2, 4, 6, 8, and 10 h, using 100 μl of each sample, the number of living bacteria was counted using the sequential dilution method [20].
Results
Mathematical results
The results of solubility parameters calculated from Hoy and Haftyzer-Van Krevelen’s methods are presented in Table 1.
Table 1.
Calculated solubility parameters using Hoy and Haftyzer- Van Krevelen methods
| Material type | Material name | Solubility Parameter Hoftyzer-van krevelen method | Solubility Parameter Hoy method |
|---|---|---|---|
| Solid lipid | Stearic acid | 17.43 | 18.16 |
| Solid lipid | GMS | 19.37 | 20.93 |
| Liquid lipid | Oleic acid | 17.31 | 18.31 |
| Surfactant | Soy lecithin | 18.84 | 17.42 |
| Surfactant | Span 80 | 22.48 | 22.01 |
| Surfactant | PVA | 28.98 | 21,012 |
| Surfactant | Tween 80 | 19.17 | 21.86 |
| Drug | Ceftriaxone sodium | 32.14 | 22.09 |
To study the effect of chaining materials on drug entrapment efficiency, it is necessary to calculate the difference between solubility parameters of drug and lipids. For liquid lipids, the HLB value is examined. Sesame oil is composed of linoleic acid (39–59%), oleic acid (35–54%), palmitic acid (10%) and stearic acid (5%). These values were extracted from our previous study based on GC analysis [21]. Results are shown in Table 2.
Table 2.
Difference in solubility parameters of various components
| Solubility parameters difference (Δδt) | |||
| Drug | Lipid | Haftyzer -van krevelen method | Hoy method |
| Ceftriaxone sodium | Stearic acid | 14.71 | 4.79 |
| Ceftriaxone sodium | GMS | 12.77 | 2.02 |
| HLB of Solid and Liquid lipids | |||
| Lipid type | Lipid | Haftyzer -van krevelen method | Hoy method |
| Solid lipid | GMS | 17.603 | 17.569 |
| Solid lipid | Stearic acid | 17.328 | 17.568 |
| Liquid lipid | Oleic acid | 17.292 | 17.564 |
| Liquid lipid components | Linoleic acid | 16.880 | 17.227 |
| Oleic acid | 17.392 | 17.564 | |
| Palmitic acid | 17.473 | 17.908 | |
| Stearic acid | 17.328 | 17.568 | |
| Liquid lipid | Sesame oil | 17.146 | 17.433 |
As shown in Table 2, in both methods of solubility parameter calculation, the solubility parameter difference in drug-GMS is lower than the drug-stearic acid. It is therefore anticipated that the nanocarrier provided with GMS will have a higher drug content compared to nano-carriers provided with the stearic acid lipid. However, drug molecules are usually solved in liquid lipids, too. The HLB value for various lipids is reported in Table 2.
As shown in Table 2, the amount of HLB associated with lipids is not significantly different, indicating a similar ratio for the hydrophobic and hydrophilic property of these lipids. However, since ceftriaxone sodium has a hydrophilic nature, it dissolves in the hydrophilic lipid. Therefore, based on HLB calculation, the selected solid and liquid lipids will be glycerol mono-stearates (HLBGMS > HLBSA) and oleic acid (HLBoleic acid > HLBsesame oil), respectively. The entrapment efficiency is predicted based on solid-liquid lipids as follows:
Stearic acid- sesame oil< Stearic acid- oleic acid< GMS- sesame oil < GMS- oleic acid
The accuracy of the predicted trend can be determined by an experimental data later.
To predict the trend of NLC particle size with various solid and liquid lipids, we investigated the difference between solubility parameters of solid lipids and surfactants (Table 3). A lower difference between solubility parameters of surfactants and solid lipid indicates a smaller nanoparticle size. Since the lipid content of solid lipid is higher than that of liquid lipid, the effect of solid lipid solubility parameter on nanoparticle size is expected to be higher than that of the liquid lipid.
Table 3.
Difference between lipid solubility parameter and stabilizer
| Samples | Solid Lipid | Stabilizer | Δδt (Hoftyzer-Van krevelen) | Δδt (Hoy) |
|---|---|---|---|---|
| S1 | Stearic acid | Soy lecithin | 1.41 | 0.74 |
| S2 | Stearic acid | Span 80 | 5.05 | 3.85 |
| S3 | Stearic acid | Tween 80 | 1.74 | 3.70 |
| S4 | Stearic acid | PVA | 11.55 | 2.96 |
| S5 | GMS | Soy lecithin | 0.53 | 3.51 |
| S6 | GMS | Span 80 | 3.11 | 1.08 |
| S7 | GMS | Tween 80 | 0.20 | 0.93 |
| S8 | GMS | PVA | 9.61 | 0.19 |
As depicted in Table 3, based on the Haftyzer-Van krevelen’s method, the solubility parameter of the active surface material for the internal NLC phase is comparable to that of soy lecithin for both solid lipids. Nevertheless, this parameter is predicted by the Hoy’s method in a completely different manner. It introduces Span 80 as the best surfactant for the system containing glycerol mono-stearate and soy lecithin for a stearic acid solid lipid.
With regard to the external water phase surfactant, it is recommended to use Tween 80 in Hoftyzer-van-krevelen’s method and PVA in the Hoy’s method for both solid lipid systems. Besides, in both methods, the solubility parameter difference in the system containing glycerol mono-stearate is lower than the system containing stearic acid lipid.
Finally, as predicted by Hoftyzer-van krevelen’s method, in the system containing glycerol mono-stearate and soy lecithin, Tween 80 has the minimum size, while in the system containing glycerol mono-stearate, span 80 and polyvinyl alcohol have the minimum particle size, as determined by the Hoy’s method.
It should be noted that the effect of external aqueous phase surfactant on decreasing the nanoparticle size is more significant than that of the internal surfactant water phase. The accuracy of mathematical methods can be verified by experimental methods.
Comparing mathematical and experimental results
The results of nanoparticles prepared with various components are displayed in Table 4. It is worth noting that we used the same amount of materials in all formulations and only changed the material type.
Table 4.
Experimental results for particle size and drug entrapment efficiency of various formulations
| Sample | Solid lipid | Liquid lipid | Surfactant of the internal water phase | Surfactant of the external water phase | Particle size (nm) | Drug loading(%) |
|---|---|---|---|---|---|---|
| S1 | GMS | Oleic acid | Soy lecithin | Tween 80 | 86.09 | 83% |
| S2 | GMS | Oleic acid | Span 80 | PVA | 112.41 | 80% |
| S3 | GMS | Sesame oil | Soy lecithin | Tween 80 | 101.95 | 75% |
| S4 | GMS | Sesame oil | Span 80 | PVA | 127.41 | 73% |
| S5 | Stearic acid | Oleic acid | Soy lecithin | Tween 80 | 202.74 | 72% |
| S6 | Stearic acid | Oleic acid | Span 80 | PVA | 260.52 | 69% |
| S7 | Stearic acid | Sesame oil | Soy lecithin | Tween 80 | 306.75 | 60% |
| S8 | Stearic acid | Sesame oil | Span 80 | PVA | 369.67 | 58% |
As Table 4 shows, according to experimental results, the drug entrapment efficiency can be boosted by chaining solid and liquid lipids as follows:
stearic acid- sesame oil< stearic acid- oleic acid< GMS- sesame oil < GMS- oleic acid
The comparison of mathematical prediction and experimental results confirms the accuracy of both Haftyzer van-Krevelen and Hoy’s methods.
The trend of particle size change based on experiments is as follows:
stearic acid- sesame oil> stearic acid- oleic acid> GMS- sesame oil > GMS- oleic acid
According to the mathematical models and Table 3, it is predicted that in the Haftyzer van-Krevelen’s method, the solubility of internal phase surfactants in both solid lipids correspond to soy lecithin solubility parameter. The sample prepared with soy lecithin as the surfactant in the internal water phase has a smaller nanoparticle size. The results of Table 4 corroborate this prediction. However, the prediction of this parameter with the Hoy’s method is completely different. According to the Hoy’s method, Span 80 is the best surfactant for the system containing glycerol mono-stearate and soy lecithin is the best surfactant for the stearic acid lipid. This prediction is inconsistent with experimental results. As far as the aqueous external phase surfactant is concerned, it is recommended to use Tween 80 in Hoftyzer van-krevelen’s method, and Polyvinyl alcohol in the Hoy’s method for both solid lipid systems. According to Table 4, the particle size of the sample with Tween 80 as the external water phase surfactant is smaller, which confirms the prediction of the Hoftyzer-van krevelen’s method.
Finally, the system containing glycerol mono-stearate and oleic acid as the solid and liquid lipid and soy lecithin and Tween 80 as the surfactant of internal and external water phase was chosen as the optimum sample with a small particle size and high drug loading.
Characterization of optimized structure
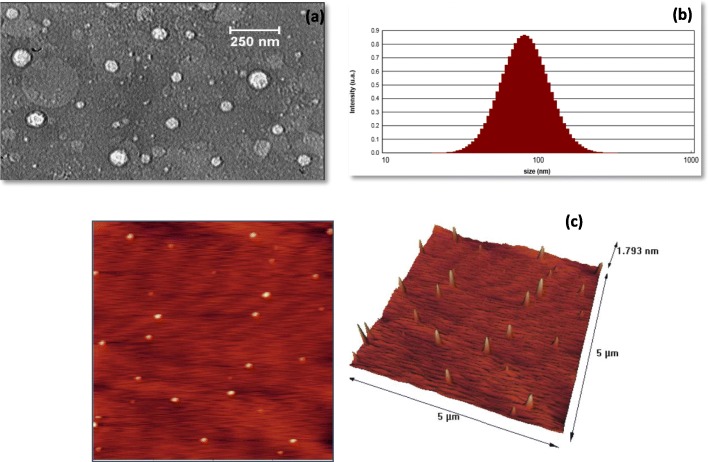
Characterization was performed following the determination of the optimum sample. Figure 2 shows TEM, PSA and AFM images of the optimum sample. As Fig. 2a illustrates, NLC particles have a spherical structure with a mean particle size of 70 nm, while DLS calculation estimated a particle size of 86 nm (Fig. 2b). TEM and DLS results are relatively identical, and the difference between TEM and DLS analysis is due to the measurement method. The DLS analysis measures the hydrodynamic diameter of particles in the solution, indicating a larger diameter for particles [22, 23]. Moreover, the polydispersity index (PDI) of 0.131 reveals the uniform distribution of particles, which is aligned with AFM images (Fig. 2c). Based on the amount of PDI, values close to zero manifest higher stability of nanoparticles [24]. The zeta potential of the sample is − 20.26, which is acceptable for lipid nanoparticles. This numerical value can be attributed to functional groups with a negative charge on the structure, which generates sufficient repulsion to prevent the agglomeration of particles in the solution in a short time.
Fig. 2.
a TEM image, b PSA image and c AFM analysis results at both 2D and 3D view
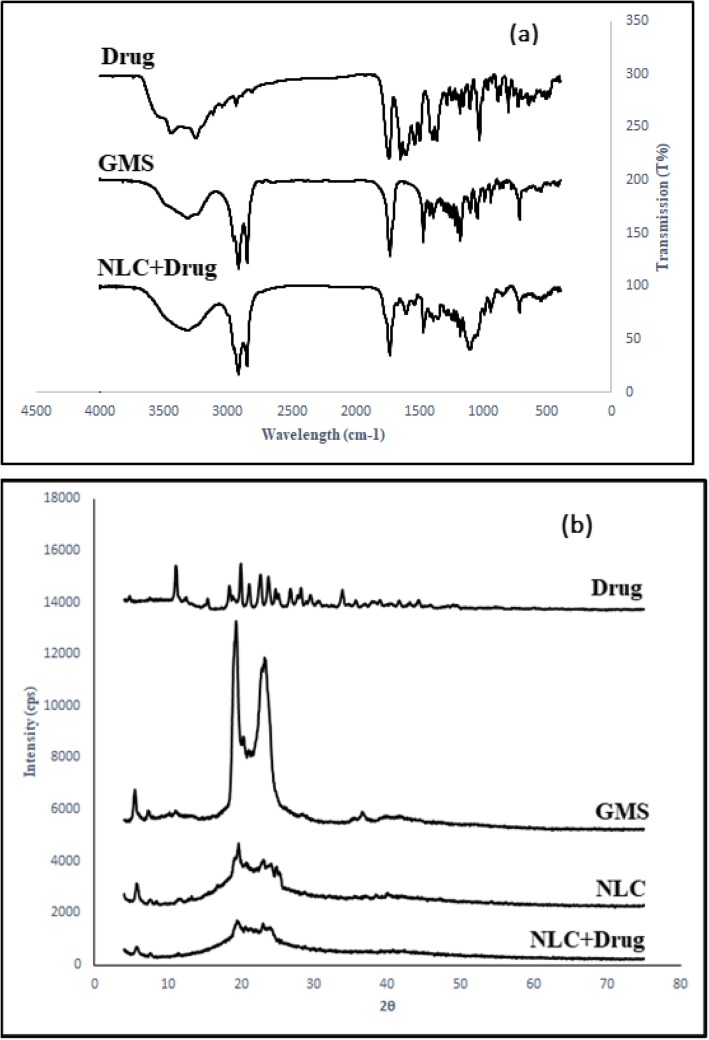
FT-IR analysis was used to examine functional groups on the nano-carrier surface. Figure 3a shows the results of the FT-IR analysis for ceftriaxone sodium, Glycerol Monostearate, and nano-carriers containing ceftriaxone sodium. The FT-IR analysis of ceftriaxone sodium exhibits a band at 3444.63 cm− 1, which can be attributed to the stretching vibration of O-H and N-H. The bands appearing at 1747.39 cm− 1 and 1649.02 cm− 1 are due to the C=O stretching vibrational frequency [25]. Moreover, the bands emerging at 3303.8 cm− 1, 1734.8 cm− 1, 1179.6 cm− 1 are attributable to the O-H bond, C=O bond, and C-O transplant, and bands emerging at 2912 cm− 1 and 2846.6 cm− 1 are related to the C-H bond of the GMS structure, respectively [26].
Fig. 3.
a FTIR and b XRD analysis
As shown in Fig. 3a, the FT-IR spectrum obtained from the NLC sample containing ceftriaxone sodium resembles that of glycerol mono-stearates. This indicates that the drug has been successfully encapsulated in the lipid structure. By comparing the spectra of nanoparticles to each pure component, the presence of all materials can be verified. The peak at 1649.02, which is caused by the C=O amide, confirms drug presence in the NLC structure. Due to low drug content in the nano-structure, the effects of drug-related peaks are weaker.
In the next step, XRD patterns of ceftriaxone sodium, GMS, and NLC with/without drug are measured. According to Fig. 3b, ceftriaxone sodium has sharp edges at 11.18 °, 12.56 °, 18.92 °, 21.24 °, 22.74 °, 23.80 °, 25.20 °, 28.28 ° [27]. Also, glycerol mono-stearate has sharp peaks in the range of 19.97 ° to 23.38 °[28] and glycerol mono-stearate has a crystalline structure. However, as shown by XRD patterns of NLCs containing drug and non-drug, peaks are broader and less sharp than those of pure patterns. These results exhibit the amorphous structure of the prepared NLCs. The changes of crystallography nature can be attributed to the presence of other materials such as surfactants and liquid lipids. Comparing the peaks of pure drug to that of NLC-containing drug reveals that there is no comparable peak in the NLC pattern. This implies that drug has been successfully loaded in the nanocarrier [29, 30].
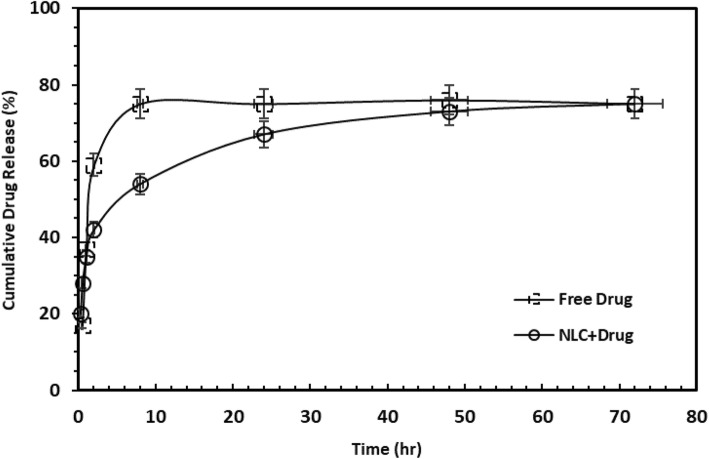
In vitro drug release
The graphs in Fig. 4 indicate the release of drug in both commercial and NLC forms. As can be seen, the commercial drug has explosive release while there are two types of drug release in the NLC form: explosive and controlled release. About 42% of the drug is released after 6 h from both formulations. In the case of the commercial market ampoule, the rapid release persists for 10 h and then drug release rate is stabilized (about 80%). However, the gradual release of the nano-carrier sample in this study lasted for 72 h with a moderate gradient. The efficacy of the two drug forms will be further determined by conducting experiments that contain bacterial culture.
Fig. 4.
In vitro drug release from free drug and nanostructured NLC form
Cell culture results
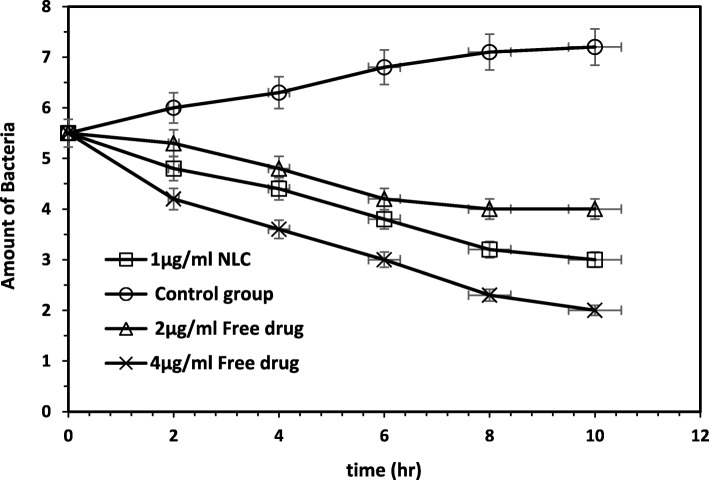
The results of MIC analysis showed that 2 μg / ml concentration of ceftriaxone in free form and 1 μg / ml concentration of ceftriaxone in nanostructured form inhibited the growth of Escherichia coli bacteria.
The bactericidal activity of ceftriaxone sodium at different concentrations in both free and nanostructure forms was studied by counting bacteria after 0, 2, 4, 6, 8 and 10 h. The results of the death kinetics test are presented in Fig. 5. In this case, we investigated variation in the number of bacteria after 0, 2, 4, 6, 8 and 10 h based on MIC concentration of ceftriaxone sodium in the form of nanostructures under different concentrations of sodium ceftriaxone in free form and antibiotic-free sample.
Fig. 5.
Results of cell culture
As Fig. 5 shows, at the same time, the number of bacteria in the system containing the nanostructured form of drug with a concentration of 1 μg/ml is lower than that of a system containing free drug with a concentration of 2 μg/ml.
Discussion
In this study, a double emulsion solvent evaporation method was used to construct NLC for the delivery of ceftriaxone sodium drug. Hoftyzer-Van Krevelen and Hoy’s methods were applied to calculate solubility parameters. Based on the prediction of two mathematical models and the experimental results, both Hoy and Hoftyzer-van krevelen’s models appear to be strong predictors of drug loading in different NLC systems. However, Haftyzer van-krevelen’s model is capable of predicting the components of NLC to achieve a smaller particle size whereas the Hoy’s method is unable to predict the trend accurately. These results align well with those reported in the literature. Tian et al. demonstrated that the solubility parameter can be a suitable guide for the design and identification of a stable micellar system with a high drug loading capacity [31]. Bahrami et al. argued that solubility parameters based on group-contribution model offer a useful guide for preparing NLC with various formulations containing Fentanyl citrate as the hydrophobic drug. They illustrated that the surfactants-lipids solubility parameter had a bearing on the nanoparticle size, while the drug-lipid solubility parameter affected drug entrapment efficiency [13].
In vitro drug release at pH = 7.4 indicates the controlled release of drug from the structure and the accuracy of the proposed nanostructured behavior. The explosive release of antibiotics from the nanostructure in early hours of injection leads to bacterial death. Then, the gradual release of the nanocarrier sample over time with a mild gradient can diminish the bacterial resistance and enhance drug efficacy. This claim is approved by the cell culture study. The kinetics curve of bacteria mortality indicates that the system containing nanostructure form can last bacterial death for a longer time. Moreover, the slope of curve in the nanostructure sample is more controlled than that of the curve in the free drug. Furthermore, it suggests that by cutting the drug dosage of the nanostructure in half, the same efficacy can be achieved. It should be noted that the permeability of E.coli against antibiotics and antimicrobial agents is low. It is a gram-negative bacterium with a thinner peptidoglycan layer and lipopolysaccharide as the outer membrane. For this reason, E. coli’s resistance is higher than bacteria such as Staphylococcus aureus [32, 33]. Chaining the common form of the drug to a nanostructure with a controlled drug release can undermine the resistance of the bacteria membrane wall over time and improves the bacterial mortality rate. These observations are aligned with Kumar et al.’s study. They prepared a SLN structure containing Ceftriaxone sodium drug and examined its inhibition effect on E. coli bacteria, with their results revealing a slower and sustained release of drug from the SLN structure. Drug release profiles in their study exhibited a sustained release from the SLN structure where only 6% of the drug was released from the nano-formulation in 24 h, whereas 80% of the drug was released for the drug alone [1].
The present study has some strong points worth mentioning. Using mathematical modeling in this study helps overcome some of issues associated with the selection of best materials without experiments. It can affect assessment method and modeling in this field. Moreover, investigating the effect of the NLC form of drug with various doses on E. coli, as a highly resistant gram-negative bacterium, is another advantage of this research.
However, there are a number of drawbacks that should be mentioned. In NLC preparation, we changed one parameter and kept others constant. Hence, the inter-variable relationships were not investigated [34]. For the cell culture study, a strict control is required to perform experiments properly. At the same time, a greater degree of control makes experiments artificial. These problems can be solved by performing several experiments to get a clearer picture of the process [35]. Future studies can take measured to address this shortcoming.
A number of limitations should also be noted. First, NLC was prepared using double-emulsion solvent evaporation method by an ultrasonication device. Future studies can utilize other methods and investigate their effects on the particle size and drug entrapment efficiency. Second, we focused on the impact of the NLC form of ceftriaxone on E-coli bacteria in a cell culture study, while the use of nanostructured form of ceftriaxone sodium can have beneficial effects on other types of gram-positive and gram-negative bacteria. A direction of research for future research can be evaluating the impact of nanostructured form of ceftriaxone on various resistant bacteria. Finally, we only measured the effect of the NLC form of the drug under in vitro environment. Future research can conduct similar tests under in vivo media.
Conclusion
In the present study, the nanostructured lipid carrier was prepared to load ceftriaxone sodium as a hydrophilic drug. The effect of drug on E. coli was investigated in bacterial culture media. Based on the mathematical modeling, the Haftyzer-van krevelen’s model appeared to be more accurate than the Hoy’s method in predicting the trend of NLC particle size with different materials. Nevertheless, both Haftyzer-van krevelen and Hoy’s methods were able to predict the trend of change in drug entrapment efficiency accurately. Informed by the kinetics of bacteria cell, the results revealed that the NLC form of drug had higher antibacterial activity against E.coli gram-negative bacteria compared to the free drug. The greater antibacterial effect of the drug at a lower dose in the NLC form is another important finding of this study with regard to antibiotic-dose reduction and cost-effective treatment of resistant microbes.
Acknowledgements
Not applicable.
Abbreviations
- AFM
Atomic force microscopy
- ATCC
American Type Culture Collection
- CLSI
Clinical and Laboratory Standard Institute
- DLS
Dynamic light scattering
- E.Coli
Escherichia coli bacteria
- FT-IR
Fourier-transform infrared spectroscopy
- GC
Gas chromatography
- GMS
Glycerol mono-stearate
- HLB
Hydrophilic-Lipophilic Balance
- HPLC
High performance liquid chromatographic
- MIC
Minimum growth inhibitory concentration
- NLC
Nanostructure lipid carrier
- PDI
Polydispersity index
- PSA
Particle size analysis
- PVA
Polyvinyl alcohol
- SLN
Solid lipid nanoparticle
- TEM
Transmission electron microscopy
- XRD
X-ray diffraction
Authors’ contributions
SE performed experimental tests and mathematical modeling. She also wrote the initial draft of the paper. NF checked the accuracy of experimental and mathematical modeling and composed the final manuscript. MK and ME performed microbiological tests and analyzed the microbial results. All authors read and approved the final manuscript.
Funding
The study was not funded by any institutions.
Availability of data and materials
The datasets used in the study are available and can be provided by the corresponding author upon request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kumar S, et al. Synthesis and optimization of ceftriaxone-loaded solid lipid nanocarriers. Chem Phys Lipids. 2016;200:126–132. doi: 10.1016/j.chemphyslip.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 2.Manten A. Side effects of antibiotics. Vet Q. 1981;3(4):179–182. doi: 10.1080/01652176.1981.9693824. [DOI] [PubMed] [Google Scholar]
- 3.El-Salamouni NS, et al. Effect of sterilization on the physical stability of brimonidine-loaded solid lipid nanoparticles and nanostructured lipid carriers. Int J Pharm. 2015;496(2):976–983. doi: 10.1016/j.ijpharm.2015.10.043. [DOI] [PubMed] [Google Scholar]
- 4.Qu J, et al. Nanostructured lipid carriers, solid lipid nanoparticles, and polymeric nanoparticles: which kind of drug delivery system is better for glioblastoma chemotherapy? Drug Deliv. 2016;23(9):3408–3416. doi: 10.1080/10717544.2016.1189465. [DOI] [PubMed] [Google Scholar]
- 5.Dash S, et al. Kinetic modeling on drug release from controlled drug delivery systems. Acta Pol Pharm. 2010;67(3):217–223. [PubMed] [Google Scholar]
- 6.Dehghani F, et al. Preparation, characterization and in-vivo evaluation of microemulsions containing tamoxifen citrate anti-cancer drug. Eur J Pharm Sci. 2017;96:479–489. doi: 10.1016/j.ejps.2016.09.033. [DOI] [PubMed] [Google Scholar]
- 7.Golmohammadzadeh S, et al. Preparation, characterization and in vitro evaluation of microemulsion of raloxifene hydrochloride. Drug Dev Ind Pharm. 2017;43(10):1619–1625. doi: 10.1080/03639045.2017.1328430. [DOI] [PubMed] [Google Scholar]
- 8.Venkateswarlu V, Manjunath K. Preparation, characterization and in vitro release kinetics of clozapine solid lipid nanoparticles. J Control Release. 2004;95(3):627–638. doi: 10.1016/j.jconrel.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 9.Zhang K, et al. Preparation, characterization, and in vivo pharmacokinetics of nanostructured lipid carriers loaded with oleanolic acid and gentiopicrin. Int J Nanomedicine. 2013;8:3227. doi: 10.2147/IJN.S45031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoy K. New values of the solubility parameters from vapor pressure data. J Paint Technol. 1970;42(541):76–118. [Google Scholar]
- 11.Hoy K. Solubility parameter as a design parameter for water borne polymers and coatings. J Coated Fabr. 1989;19(1):53–67. doi: 10.1177/152808378901900106. [DOI] [Google Scholar]
- 12.Van Krevelen DW, Te Nijenhuis K. Properties of polymers: their correlation with chemical structure; their numerical estimation and prediction from additive group contributions. 4th ed., Elsevier Science; 2009.
- 13.Bahrami MA, Farhadian N. Experimental study and mathematical modeling for encapsulation of fentanyl citrate drug in nanostructured lipid carrier. J Biomol Struct Dyn. 2019;16:1–9. 10.1080/07391102.2019.1599732 [DOI] [PubMed]
- 14.He Q, et al. Chemically surface tunable solubility parameter for controllable drug delivery—an example and perspective from hollow PAA-coated magnetite nanoparticles with R6G model drug. Materials. 2018;11(2):247. doi: 10.3390/ma11020247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xavier-Junior FH, et al. Match of solubility parameters between oil and surfactants as a rational approach for the formulation of microemulsion with a high dispersed volume of copaiba oil and low surfactant content. Pharm Res. 2016;33(12):3031–3043. doi: 10.1007/s11095-016-2025-y. [DOI] [PubMed] [Google Scholar]
- 16.Emami J, Rezazadeh M, Varshosaz J. Formulation of LDL targeted nanostructured lipid carriers loaded with paclitaxel: a detailed study of preparation, freeze drying condition, and in vitro cytotoxicity. J Nanomater. 2012;2012:3. doi: 10.1155/2012/358782. [DOI] [Google Scholar]
- 17.Zambaux M, et al. Influence of experimental parameters on the characteristics of poly (lactic acid) nanoparticles prepared by a double emulsion method. J Control Release. 1998;50(1–3):31–40. doi: 10.1016/S0168-3659(97)00106-5. [DOI] [PubMed] [Google Scholar]
- 18.Baron EJ, Finegold SM. Diagnostic microbiology. 8th ed. NewYork: Mosby Company; 1990. p. 171–86.
- 19.National Committee for Clinical Laboratory Standards. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard. 6th ed. NCCLS document M7-A6, Wany PA: NCCLS; 2003.
- 20.Beaulac C, Sachetelli S, Lagace J. In-vitro bactericidal efficacy of sub-MIC concentrations of liposome-encapsulated antibiotic against gram-negative and gram-positive bacteria. J Antimicrob Chemother. 1998;41(1):35–41. doi: 10.1093/jac/41.1.35. [DOI] [PubMed] [Google Scholar]
- 21.Ghorbanzadeh M, et al. Formulation, clinical and histopathological assessment of microemulsion based hydrogel for UV protection of skin. Colloids Surf B: Biointerfaces. 2019;179:393–404. doi: 10.1016/j.colsurfb.2019.04.015. [DOI] [PubMed] [Google Scholar]
- 22.Huang Wei, Dou Huating, Wu Houjiu, Sun Zhigao, Wang Hua, Huang Linhua. Preparation and Characterisation of Nobiletin-Loaded Nanostructured Lipid Carriers. Journal of Nanomaterials. 2017;2017:1–10. [Google Scholar]
- 23.Singh SK, et al. Intranasal delivery of asenapine loaded nanostructured lipid carriers: formulation, characterization, pharmacokinetic and behavioural assessment. RSC Adv. 2016;6(3):2032–2045. doi: 10.1039/C5RA19793G. [DOI] [Google Scholar]
- 24.Joshi M, Patravale V. Nanostructured lipid carrier (NLC) based gel of celecoxib. Int J Pharm. 2008;346(1–2):124–132. doi: 10.1016/j.ijpharm.2007.05.060. [DOI] [PubMed] [Google Scholar]
- 25.Junejo Y, Baykal A. Green chemical synthesis of silver nanoparticles and its catalytic activity. J Inorg Organomet Polym Mater. 2014;24(2):401–406. doi: 10.1007/s10904-013-9974-y. [DOI] [Google Scholar]
- 26.Han L, Wang T. Preparation of glycerol monostearate from glycerol carbonate and stearic acid. RSC Adv. 2016;6(41):34137–34145. doi: 10.1039/C6RA02912D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jeon O-C, et al. Oral delivery of ionic complex of ceftriaxone with bile acid derivative in non-human primates. Pharm Res. 2013;30(4):959–967. doi: 10.1007/s11095-012-0932-0. [DOI] [PubMed] [Google Scholar]
- 28.Carrillo-Navas H, et al. Shear rheology of water/glycerol monostearate crystals in canola oil dispersions interfaces. Colloids Surf A Physicochem Eng Asp. 2013;436:215–224. doi: 10.1016/j.colsurfa.2013.06.021. [DOI] [Google Scholar]
- 29.Shete H, Patravale V. Long chain lipid based tamoxifen NLC. Part I: preformulation studies, formulation development and physicochemical characterization. Int J Pharm. 2013;454(1):573–583. doi: 10.1016/j.ijpharm.2013.03.034. [DOI] [PubMed] [Google Scholar]
- 30.Tamjidi F, et al. Design and characterization of astaxanthin-loaded nanostructured lipid carriers. Innovative Food Sci Emerg Technol. 2014;26:366–374. doi: 10.1016/j.ifset.2014.06.012. [DOI] [Google Scholar]
- 31.Thian Y, et al. Designing micellar nanocarriers with improved drug loading and stability based on solubility parameter. Mol Pharm. 2015;12:816–825. doi: 10.1021/mp5006504. [DOI] [PubMed] [Google Scholar]
- 32.Feng QL, et al. A mechanistic study of the antibacterial effect of silver ions on Escherichia coli and Staphylococcus aureus. J Biomed Mater Res. 2000;52(4):662–668. doi: 10.1002/1097-4636(20001215)52:4<662::AID-JBM10>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 33.Kim JS, et al. Antimicrobial effects of silver nanoparticles. Nanomedicine. 2007;3(1):95–101. doi: 10.1016/j.nano.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 34.Zarei baygi F, Farhadian N, Malaekeh-Nikouei B, Maghsoud Z. Co-encapsulation of tamoxifen citrate and quercetin using 2HP-b-cyclodextrin: a response surface experimental design. RSC Adv. 2016;6:111517. doi: 10.1039/C6RA21166F. [DOI] [Google Scholar]
- 35.Hatefi L, Farhadian N. A safe and efficient method for encapsulation of ferrous sulfate in solid lipid nanoparticle for non-oxidation and sustained iron delivery. Colloid Interface Sci Commun. 2020;34:100227. doi: 10.1016/j.colcom.2019.100227. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used in the study are available and can be provided by the corresponding author upon request.