Abstract
Forty-six states and the District of Columbia have enacted insurance mandates that require commercial insurers to cover treatment for children with autism spectrum disorder (ASD). This study examined whether implementing autism mandates altered service use or spending among commercially insured children with ASD. We compared children age twenty-one or younger who were eligible for mandates to children not subject to mandates using 2008–12 claims data from three national insurers. Increases in service use and spending attributable to state mandates were detected for all outcomes. Mandates were associated with a 3.4-percentage-point increase in monthly use and a $77 increase in monthly spending on ASD-specific services. Effects were larger for younger children and increased with the number of years since mandate implementation. These increases suggest that state mandates are an effective tool for broadening access to autism treatment under commercial insurance.
Forty-six states and the District of Columbia have enacted insurance mandate laws to improve access to health care services among commercially insured children with autism spectrum disorder (ASD). ASD is a neurobehavioral condition defined by impairments in social communication, highly restricted interests, repetitive behaviors, and disruption in the development of social and language abilities.1 In the United States, estimates of the incidence of ASD have increased dramatically, from 1 in 150 children (0.67 percent) in 2004 to 1 in 68 children (1.5 percent) in 2010.2
Recommended care for children with ASD includes behavioral, speech-language, occupational, and physical therapy3 and educational interventions delivered for up to forty hours a week.4 Even with the recommended intensive treatments and supports, complete amelioration of symptoms is rare.5 Most people with ASD need care through adulthood.6 ASD often is accompanied by other conditions requiring treatment, including seizures, hearing impairment, sleep problems, gastrointestinal dysfunction, and psychiatric comorbidities.7 The costs of caring for children with ASD can be substantial,8,9 and families of such children report challenges in paying for services.10
Historically, commercial insurers have excluded or provided minimal coverage for ASD services11 on the grounds that ASD treatments are unproven or experimental and because of concerns that mandates would lead to increases in health care spending.12 Medicaid has served as the single largest payer for health care for people with autism and developmental disabilities.13 In 2013 approximately 250,000 children with diagnoses of autism received services through Medicaid (Douglas Leslie, Pennsylvania State University, personal communication based on calculations in 2013 Medicaid claims data, January 14, 2017). State enactment of autism mandates has been viewed as a strategy to broaden access to ASD treatment paid for via commercial insurance.
Autism mandates require commercial insurers to cover ASD-specific behavioral therapies, with annual caps on spending ranging from $12,000 to $50,000 per child, depending on the state and age of the child. These mandates apply to only a subset of a state’s commercially insured population. The Employee Retirement Income Security Act (ERISA) exempts self-insured firms—those contracting with health plans to administer employee health benefits only, not to manage their insurance risk pool—from state insurance regulations. About half of commercially insured Americans are enrolled through self-insured firms14 that are exempt from state mandates.
To date, little is known about the effects of autism mandates. One recent study found that mandate implementation increased the proportion of children diagnosed with ASD who were covered by commercial insurance.15 Another study found that mandates had no effect on access or costs, but it could not determine whether or not children in mandate states were enrolled in insurance plans subject to mandates—an important limitation.16 There is a larger literature on the effects of insurance mandates more broadly that helps shed light on the expected effects of state autism mandates. For example, Jonathan Gruber found that mandates had minimal effect on coverage rates; this lack of effect was because most firms appear to have offered mandated benefits even in the absence of regulation.17 Importantly, this has not been the case for ASD treatments, as noted above.
Our study examined whether autism insurance mandates led to changes in the use of and spending on health care services under commercial insurance, using data from three large national health insurance companies. We used a difference-in-differences approach to exploit the geographic and temporal variation in the implementation of mandates, and we compared eligible and ineligible children within states. We also tested whether the effects of mandates varied by a child’s age and by the number of years since the mandate’s implementation. The latter is important because implementation has been slowed by delays in regulatory guidance on licensing and credentialing providers.18
Study Data And Methods
DATA SOURCES AND SAMPLE
We used inpatient, outpatient, and pharmaceutical commercial claims data from the Health Care Cost Institute (HCCI) from January 1, 2008, through December 31, 2012. These data come from three national insurers—UnitedHealthcare, Aetna, and Humana—and they cover more than fifty million individuals per year in all states and the District of Columbia. HCCI data indicate whether a plan enrollee was covered through a self-insured or fully insured firm. Our study sample consisted of children from birth through age twenty-one diagnosed with ASD who had at least two claims on different days containing International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), code 299.xx during the study period. The child-calendar month was the unit of analysis. We included only child-months with commercial insurance for which behavioral health claims were available in the data (89 percent of all child-months). We excluded months when children were covered by individually insured plans (less than 0.2 percent of all child-months). The final study sample included 106,977 children and 3,722,250 child-months. The study was determined to be exempt by the Johns Hopkins Bloomberg School of Public Health and University of Pennsylvania Institutional Review Boards.
MEASURES
Three primary, overlapping outcome categories for monthly service use and spending were examined: all ASD-specific services; outpatient ASD-specific services; and outpatient ASD-specific behavioral and functional therapies. All ASD-specific services consisted of inpatient and outpatient services with claims having a 299.xx diagnosis code. Outpatient ASD-specific services consisted of claims from the outpatient file having a 299.xx diagnosis code. Outpatient ASD-specific behavioral and functional therapies consisted of claims having a 299.xx diagnosis code and a procedure code indicating receipt of an outpatient behavioral, speech, occupational, or physical therapy service. These procedure codes are detailed elsewhere.19,20
Two secondary outcome categories of monthly service use and spending were also examined: all health care services, which included inpatient and outpatient services (not limited to those with a 299.xx diagnosis code on the claim) and prescription medications, and all outpatient health care services, which included outpatient claims only (not limited to those with a 299.xx diagnosis code).
For each of the five outcome categories, we examined two outcomes. Any monthly service use was defined as a binary measure of whether a child-month observation had at least one claim indicating inpatient or outpatient service use in that category (use of a prescription medication only did not qualify as use of a service). Monthly spending was calculated as the sum of the amounts paid by the insurer and the enrollee’s out-of-pocket spending for all services during the month. (Total costs of claims that spanned multiple months were apportioned based on the number of claim-days in each month.) Spending was inflated to 2012 US dollars using the relevant component of the Personal Health Care Index from the Centers for Medicare and Medicaid Services Office of the Actuary.21
To identify the start dates and ages included in each state’s mandate, we compiled information from Autism Speaks detailing which states enacted mandates, the month of enactment, and the age range to which it applied.22 We verified this information with the original state mandate laws (see online Appendix A).23 Indiana, Illinois, South Carolina, and Texas implemented autism mandates prior to the start of our study period. During our study period, mandates were implemented by six states (Arizona, Florida, Louisiana, New Mexico, Pennsylvania, and Wisconsin) in 2009, four states (Colorado, Connecticut, Montana, and New Jersey) in 2010, eight states (Arkansas, Kentucky, Maine, Massachusetts, Missouri, Nevada, New Hampshire, and Vermont) in 2011, and seven states (California, Delaware, Michigan, New York, Rhode Island, Virginia, and West Virginia) in 2012. Texas and Vermont expanded the age range covered two years after initial implementation. All mandates applied to fully insured firms with more than fifty employees; twenty-two of the twenty-nine mandates also applied to fully insured firms with fifty or fewer employees.
The two primary independent variables were binary indicators for whether or not a child was living in a mandate state and whether or not the child was eligible to be covered by that mandate in a given month. The latter variable captured whether a specific child in a given month had employer-based insurance that was fully insured and whether the child met the mandate’s age criteria. For states that did not pass a mandate during the study period, we designated children with ASD as mandate eligible based on having fully insured coverage and age between birth and age twenty-one, the modal age range covered under mandates in ten states. Other covariates included sex, age in the given month (estimated based on July 1 in their birth year), insurance product type, whether the child is enrolled in a consumer-directed health plan (defined as a high-deductible/consumer-driven plan), calendar month, calendar year, and state of residence. Models of total spending also included whether the child had prescription drug coverage (38 percent of children with ASD in our sample did not have pharmacy benefits observable in our data).
STATISTICAL ANALYSIS
To evaluate the effect of autism insurance mandates on outcomes, we used a difference-in-differences approach with state and year fixed effects. (See Appendix B for more information about our analytic approach.)23 Analyses compared outcomes within states before and after mandate implementation and between groups of children eligible and ineligible for the mandates based on whether they received insurance via a self-insured or fully insured firm and their age. The treatment group included children who lived in states with active mandates and were eligible for the mandate. The three comparison groups consisted of children in states with an active mandate who were not subject to the mandate; children in states without a mandate who would have been subject to a mandate if one were active; and children in states without a mandate who would not have been subject to a mandate if one were active. The difference-in-differences design accounted for secular trends in outcomes unrelated to state autism mandates.
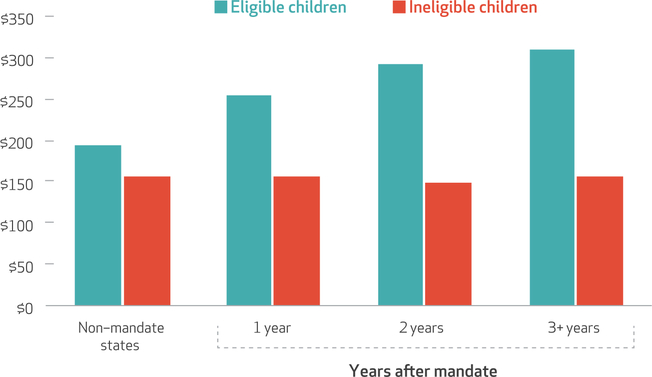
The impact of mandates on service use and average spending increased along with time since enactment.
We calculated descriptive statistics for children in the sample overall and for those in mandate and non-mandate states who were eligible and ineligible for insurance coverage under the requirements of the mandate. To strengthen our confidence in the quasi-experimental design, we compared unadjusted trends for outcomes in the years before and after implementation of the state mandates among enrollees eligible and ineligible for the mandates (see Appendix C).23
Next, we estimated unadjusted and adjusted regression models to examine the effects of mandates on use and spending outcomes. Because a high proportion of child-month observations had no service use, we analyzed spending using a two-part model.24 The first part was a logistic regression predicting any service use in the month, and the second part was a generalized linear model predicting nonzero mean monthly spending with a log link and the best-fitting error distribution as identified by the modified Park test.25 Adjusted analyses included child-level control variables and state and year fixed effects. Confidence intervals were adjusted to account for the clustering of observations within states.26 To ease interpretation, we converted results to predictive margins on their original scales.27
In addition to the main difference-in-differences model specification, we examined whether the effects of mandates on outcomes differed based on a child’s age by estimating separate models for children ages 0–5, 6–12 and 13–21. To examine whether the effects of mandates differed based on the number of years following their implementation, we estimated models that included three cohort indicators to measures effects in the first year, second year, and third or more years after implementation.
We conducted three sensitivity analyses. First, we reestimated the main service use and spending models using a nonparametric block bootstrap procedure as an alternative way to account for clustering (see Appendix D).23 In addition, we re-estimated the models of all health care spending using only the 62 percent of child-months with complete pharmacy claims (see Appendix E).23 Finally, we tested the effects of the mandates in a sample in which the age eligibility in non-mandate states was limited to birth to age eighteen (rather than birth to age twenty-one: see Appendix F).23 Results were qualitatively identical across all sensitivity analyses.
LIMITATIONS
Several limitations are important to note. First, diagnoses of ASD in insurance claims were not verified through clinical interview, although they have been shown to have high specificity.28 Second, our analysis did not consider differences by state in mandate provisions beyond age inclusion criteria. For example, state mandates differ in dollar-cap requirements, and these differences could affect both service use and spending. Third, our data do not capture any services delivered to children in schools or paid for completely out of pocket by families. Finally, our study period of 2008–12 captured the most active phase of state mandate adoption and allowed us observe a large number of children before and after these policies were implemented. Given the fast pace of change in the US health system, however, the timing of our study period is an important limitation; understanding the impact of mandates on children and adults over a longer trajectory is an important area for further research.
Study Results
Exhibit 1 summarizes the descriptive characteristics of children with autism spectrum disorder in our study sample (a fuller version of the exhibit is available in Appendix G).23 Exhibit 2 shows the effects of autism insurance mandates on use and spending. Among eligible children, the adjusted probability of using any ASD-specific service in a month was 27.9 percent in mandate states and 25.0 percent in non-mandate states, and mean adjusted monthly spending on all ASD-specific services was $278 in mandate states and $205 in non-mandate states. Among ineligible children, the adjusted probability of using any ASD-specific service in a month was 22.0 percent in mandate states and 22.6 percent in non-mandate states, and mean adjusted monthly spending on all ASD-specific services was $154 in mandate states and $157 in non-mandate states. Adjusted difference-in-differences estimates indicated that mandates were associated with a 3.4-percentage-point relative increase in the probability of using ASD-specific services (95% confidence interval: 1.2, 5.6) and a $77 increase in monthly ASD spending (95% CI: 33, 121). A similar pattern was observed for the other four outcome categories.
Exhibit 1:
Descriptive statistics for children with autism spectrum disorder (ASD) in the study sample, 2008–12
| Characteristic | Children with ASD (n = 106,977) |
Children in mandate states |
Children in non-mandate states |
||
|---|---|---|---|---|---|
| Fully insured (n = 23,105) |
Self-insured (n = 55,511) |
Fully insured (n = 7,985) |
Self-insured (n = 20,376) |
||
| Male | 81.4% | 81.2% | 81.2% | 82.0% | 81.8% |
| Age at study entry (mean years) | 8.1 | 8.3 | 7.9 | 8.5 | 8.3 |
| Age group | |||||
| 0–5 years | 35.2% | 34.4% | 36.7% | 32.3% | 33.0% |
| 6–12 years | 43.4 | 43.2 | 42.8 | 44.5 | 44.5 |
| 13–17 years | 17.7 | 18.4 | 16.9 | 19.1 | 18.8 |
| 18–21 years | 3.7 | 4.0 | 3.6 | 4.1 | 3.7 |
| Type of benefit plan | |||||
| Exclusive provider organization | 7.3 | 2.9 | 9.1 | 1.0 | 10.0 |
| Health maintenance organization | 13.5 | 32.3 | 5.1 | 40.8 | 4.6 |
| Point-of-service plan | 64.7 | 49.6 | 72.6 | 43.9 | 68.5 |
| Preferred provider organization | 14.1 | 15.1 | 12.8 | 13.8 | 16.5 |
| Other plan types | 0.4 | 0.1 | 0.4 | 0.5 | 0.4 |
| Consumer-directed health plan | 11.9 | 9.2 | 11.7 | 10.0 | 16.4 |
SOURCE Authors’ analysis of inpatient, outpatient, and pharmaceutical commercial claims data from the Health Care Cost Institute.
NOTES For mandate states, n = 29; for non-mandate states, n = 22. Information for each child with an ASD diagnosis in the study sample is based on the child’s characteristics in the first year he or she entered the data set. A fuller version of the exhibit, including sample sizes and standard deviations, as well as definitions of the plan types, is available as Appendix G (see Note 23 in text).
EXHIBIT 2:
Adjusted estimates of state mandates’ effects on the probability of health services use and mean monthly spending among children with autism spectrum disorder (ASD), 2008–12
| Probability of use among children |
Average monthly spending among children |
Change in value attributable to insurance mandatesa |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mandate eligible |
Mandate ineligible |
Mandate eligible |
Mandate ineligible |
|||||||
| Mandate states | Non-mandate states | Mandate states | Non-mandate states | Mandate states | Non-mandate states | Mandate states | Non-mandate states | Probability of use | Average monthly spending | |
| ASD-specific health care services | 27.9% | 25.0% | 22.0% | 22.6% | $278 | $205 | $154 | $157 | 3.4** | $77** |
| ASD-specific outpatient health care services | 27.7 | 24.9 | 21.9 | 22.5 | 236 | 166 | 126 | 128 | 3.4** | 72** |
| ASD-specific behavioral and functional therapy services | 20.8 | 18.2 | 15.8 | 16.1 | 158 | 107 | 74 | 77 | 2.9** | 54** |
| All health care services | 66.7 | 65.1 | 63.4 | 63.4 | 662 | 583 | 518 | 525 | 1.7** | 86 |
| All outpatient health care services | 58.6 | 56.0 | 55.1 | 55.3 | 496 | 420 | 372 | 378 | 2.7** | 82** |
SOURCE Authors’ analysis of inpatient, outpatient, and pharmaceutical commercial claims data from the Health Care Cost Institute. NOTES Adjusted models included child sex, age in the given month (estimated based on July 1 in child’s year of birth), insurance product type (health maintenance organization, point-of-service plan, preferred provider organization, exclusive provider organization, indemnity/other), enrollment in a high-deductible plan, and calendar month.
Difference-in-differences estimate of change in outcomes attributable to the mandates calculated as {(eligible children in mandate states - eligible children in non-mandate states) - (ineligible children in mandate state - ineligible children in non-mandate states)}.
p < 0.05
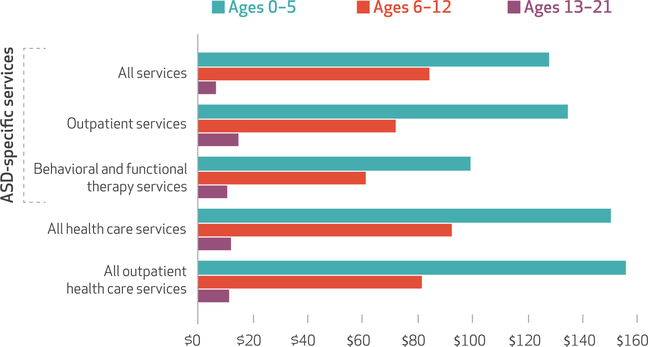
The effects of mandates on adjusted spending outcomes were substantially larger for younger children with ASD than for older children across all outcomes (see Appendix H).23 For example, mandates were associated with a $128 increase in monthly total ASD-specific health care spending among children with ASD ages 0–5 and a $84 increase among children ages 6–12, but no significant change among older children ages 13–21 (Exhibit 3).
EXHIBIT 3: Adjusted estimates of state mandates’ effects on mean monthly spending among children with autism spectrum disorder (ASD), by age group, 2008–12.
SOURCE Authors’ analysis of inpatient, outpatient, and pharmaceutical commercial claims data from the Health Care Cost Institute. NOTES The exhibit shows difference-in-differences estimates. All results for ages 0–5 and 6–12 are significantly different from zero (p < 0.05). Full results, including difference-in-differences estimates, are in Appendix H (see Note 23 in text). Adjusted analyses include child-level control variables and state and year fixed effects.
The magnitude of the effect of mandates also increased with the number of years following mandate implementation for all outcomes (see Appendix I). Monthly spending on ASD-specific services among eligible children in states without mandates was $194, while monthly ASD-specific spending among eligible children in states with mandates in the first, second, and third or more years after implementation was $253, $293, and $311, respectively (Exhibit 4). Adjusted difference-in-differences were $59 (95% CI: 21, 97) in the first year, $106 (95% CI: 48, 163) in the second year, and $115 (95% CI: 47, 183) in the third and later years after implementation (see Appendix Exhibit I).
Exhibit 4: Adjusted estimates of mean monthly spending on autism spectrum disorder–specific treatment services, by number of years after mandate implementation and children’s mandate eligibility, 2008–12.
SOURCE Authors’ analysis of inpatient, outpatient, and pharmaceutical commercial claims data from the Health Care Cost Institute. NOTES Quantities shown are mean spending levels. Full results, including difference-in-differences estimates, are in Appendix I (see Note 24 in text). Adjusted analyses include child-level control variables and state and year fixed effects.
Discussion
Study findings indicate that autism insurance mandates were associated with large increases in both the likelihood of using health care services and average spending on these services among children with autism spectrum disorder. The magnitude of these increases was quite sizable: Children with ASD covered by mandates were 3.4 percentage points more likely to use ASD-specific services in a month. Likewise, among children with ASD, mandates raised spending on ASD-specific services by an estimated annual average of $924 ($77 per month multiplied by 12 months). Most of this spending increase occurred in outpatient settings and was associated with an ASD diagnosis.
The effects of mandates on use and spending were larger among younger children with ASD than older children. For the youngest group in particular, mandates appeared to make a substantial difference in the amount of care received. For example, they were associated with about $1,872 more spent annually on outpatient services ($156 per month multiplied by 12 months), on average, in this age group (Exhibit 3). RAND used 2013 commercial claims data to estimate that mean reimbursement rates for applied behavioral analysis varied from $24.64 to $160.00 per hour for a bachelor’s level provider and $36.90 to $196.50 per hour for a master’s- or doctoral-level provider.29 This suggests that mandates could result in a child’s obtaining 10–50 additional hours of applied behavioral analysis services from a master’s-trained clinician over the course of a year.
Larger effects among younger children make sense for several reasons. First, much less research has been conducted to inform the evidence base for treating adolescents and young adults than for younger children with ASD.30 Perhaps as a result, the provider system is much better oriented toward treatment for younger children than for adolescents,19,31,32 which makes access an issue for older youths even in insurance plans subject to the mandates. Second, when children reach school age, much of the responsibility for care is transferred from the health care system to the education system.8 Third, as children age and demands of school and other activities increase, they have less time for intensive treatment.33 Lastly, many of the mandate laws apply only to younger children.
The impact of mandates on service use and average spending increased along with time since enactment. This underscores the lag from mandate enactment to full implementation, which occurs in part because establishing regulatory, clinician credentialing, and reimbursement processes often takes many years following passage of a state mandate.18
This study did not examine whether autism mandates had differential effects based on an enrollee’s firm size. Gail Jensen and Michael Morrisey reviewed evidence suggesting that the burden of state mandates tends to fall disproportionately on smaller employers, with potential negative effects including large premium increases or the decision to stop offering insurance; firms might also be prompted to self-in-sure.34 This is an important area for future study.
Conclusion
Among children with autism spectrum disorder, autism insurance mandates were associated with increases in the probability of service use. This supports mandate proponents’ belief that the mandates are an effective tool for broadening access to treatment under commercial insurance. However, our finding that mandates have led to large increases in health care spending are likely to exacerbate insurers’ and employers’ concerns about the mandates’ effects on health insurance premiums. ■
Supplementary Material
Acknowledgments
All phases of this study were supported by National Institute of Mental Health (NIMH) Grant No. R01MH096848. Steven Marcus reports receiving consulting fees from Alkermes, Shire, Johnson & Johnson, Forest, and Sunovion.
Contributor Information
Colleen L. Barry, Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, and codirector of the Johns Hopkins Center for Mental Health and Addiction Policy Research, in Baltimore, Maryland.
Andrew J. Epstein, Medicus Economics, in Philadelphia, Pennsylvania.
Steven C. Marcus, School of Social Policy and Practice, University of Pennsylvania, in Philadelphia.
Alene Kennedy-Hendricks, Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health.
Molly K. Candon, Leonard Davis Institute of Health Economics, Wharton School, University of Pennsylvania.
Ming Xie, Center for Mental Health Policy and Services Research, Perelman School of Medicine, University of Pennsylvania.
David S. Mandell, Center for Mental Health Policy and Services Research, Perelman School of Medicine, University of Pennsylvania.
NOTES
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington (DC): APA; 2013. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2010. MMWR Surveill Summ. 2014;63: 1–21. [PubMed] [Google Scholar]
- 3.Myers SM, Johnson CP. Management of children with autism spectrum disorders. Pediatrics. 2007; 120(5):1162–82. [DOI] [PubMed] [Google Scholar]
- 4.Behavior Analyst Certification Board. Applied behavior analysis treatment of autism spectrum disorder: practice guidelines for healthcare funders and managers. 2nd ed. [Internet]. Littleton (CO): The Board; 2014. [cited 2017 Aug 30]. Available from: https://bacb.com/wp-content/uploads/2016/08/ABA_Guidelines_for_ASD.pdf [Google Scholar]
- 5.Howlin P Autism and Asperger syndrome: preparing for adulthood. New York (NY): Routledge; 2004. [Google Scholar]
- 6.Croen LA, Zerbo O, Qian Y, Massolo ML, Rich S, Sidney S, et al. The health status of adults on the autism spectrum. Autism. 2015;19(7): 814–23. [DOI] [PubMed] [Google Scholar]
- 7.Gillberg C, Billstedt E. Autism and Asperger syndrome: coexistence with other clinical disorders. Acta Psychiatr Scand. 2000;102(5): 321–30. [DOI] [PubMed] [Google Scholar]
- 8.Buescher AV, Cidav Z, Knapp M, Mandell DS. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr. 2014;168(8):721–8. [DOI] [PubMed] [Google Scholar]
- 9.Leslie DL, Martin A. Health care expenditures associated with autism spectrum disorders. Arch Pediatr Adolesc Med. 2007;161(4):350–5. [DOI] [PubMed] [Google Scholar]
- 10.Chiri G, Warfield ME. Unmet need and problems accessing core health care services for children with autism spectrum disorder. Matern Child Health J. 2012;16(5):1081–91. [DOI] [PubMed] [Google Scholar]
- 11.Peele PB, Lave JR, Kelleher KJ. Exclusions and limitations in children’s behavioral health care coverage. Psychiatr Serv. 2002;53(5): 591–4. [DOI] [PubMed] [Google Scholar]
- 12.Bouder JN, Spielman S, Mandell DS. Brief report: Quantifying the impact of autism coverage on private insurance premiums. J Autism Dev Disord. 2009;39(6):953–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Semansky RM, Xie M, Mandell DS. Medicaid’s increasing role in treating youths with autism spectrum disorders. Psychiatr Serv. 2011; 62(6):588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buchmueller TC, Cooper PF, Jacobson M, Zuvekas SH. Parity for whom? Exemptions and the extent of state mental health parity legislation. Health Aff (Millwood). 2007;26(4):w483–7. 10.1377/healthaff.26.4.w483 [DOI] [PubMed] [Google Scholar]
- 15.Mandell DS, Barry CL, Marcus SC, Xie M, Shea K, Mullan K, et al. Effects of autism spectrum disorder insurance mandates on the treated prevalence of autism spectrum disorder. JAMA Pediatr. 2016;170(9): 887–93. [DOI] [PubMed] [Google Scholar]
- 16.Chatterji P, Decker SL, Markowitz S. The effects of mandated health insurance benefits for autism on out-of-pocket costs and access to treatment. J Policy Anal Manage. 2015; 34(2):328–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gruber J State mandated benefits and employer provided insurance. J Public Econ. 1994;55(3):433–64. [Google Scholar]
- 18.Baller JB, Barry CL, Shea K, Walker MM, Ouellette R, Mandell DS. Assessing early implementation of state autism insurance mandates. Autism. 2016;20(7):796–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cidav Z, Lawer L, Marcus SC, Mandell DS. Age-related variation in health service use and associated expenditures among children with autism. J Autism Dev Disord. 2013; 43(4):924–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mandell DS, Xie M, Morales KH, Lawer L, McCarthy M, Marcus SC. The interplay of outpatient services and psychiatric hospitalization among Medicaid-enrolled children with autism spectrum disorders. Arch Pediatr Adolesc Med. 2012; 166(1):68–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Medicare and Medicaid Services. National Health Expenditure Accounts: methodology paper, 2014. [Internet]. Baltimore (MD): CMS; 2015 [cited 2017 Jul 27]. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/dsm-14.pdf [Google Scholar]
- 22.Autism Speaks. State initiatives [Internet]. New York (NY): Autism Speaks; 2017. [cited 2017 Jul 27]. Available from: https://www.autismspeaks.org/state-initiatives [Google Scholar]
- 23. To access the Appendix, click on the Details tab of the article online.
- 24.Buntin MB, Zaslavsky AM. Too much ado about two-part models and transformation? Comparing methods of modeling Medicare expenditures. J Health Econ. 2004;23(3): 525–42. [DOI] [PubMed] [Google Scholar]
- 25.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001; 20(4):461–94. [DOI] [PubMed] [Google Scholar]
- 26.Cameron AC, Miller DL. A practitioner’s guide to cluster-robust inference. J Hum Resources. 2015; 50(2):317–72. [Google Scholar]
- 27.Kleinman LC, Norton EC. What’s the risk? A simple approach for estimating adjusted risk measures from nonlinear models including logistic regression. Health Serv Res. 2009; 44(1):288–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burke JP, Jain A, Yang W, Kelly JP, Kaiser M, Becker L, et al. Does a claims diagnosis of autism mean a true case? Autism. 2014;18(3): 321–30. [DOI] [PubMed] [Google Scholar]
- 29.Maglione MA, Kadiyala S, Kress AM, Hastings JL, O’Hanlon CE. TRICARE applied behavior analysis (ABA) benefit: comparison with Medicaid and commercial benefits [Internet]. Santa Monica (CA): RAND Corporation; 2016. [cited 2017 Jul 27]. Available from: https://www.rand.org/content/dam/rand/pubs/research_reports/RR1300/RR1334/RAND_RR1334.pdf [PMC free article] [PubMed] [Google Scholar]
- 30.Wong C, Odom SL, Hume KA, Cox AW, Fettig A, Kucharczyk S, et al. Evidence-based practices for children, youth, and young adults with autism spectrum disorder: a comprehensive review. J Autism Dev Disord. 2015;45(7):1951–66. [DOI] [PubMed] [Google Scholar]
- 31.Hodgetts S, Zwaigenbaum L, Nicholas D. Profile and predictors of service needs for families of children with autism spectrum disorders. Autism. 2015;19(6):673–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vohra R, Madhavan S, Sambamoorthi U, St Peter C. Access to services, quality of care, and family impact for children with autism, other developmental disabilities, and other mental health conditions. Autism. 2014;18(7):815–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cidav Z, Marcus S, Mandell D. Implications of childhood autism for parental employment and earnings. Pediatrics. 2012;129:617–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jensen GA, Morrisey MA. Employer-sponsored health insurance and mandated benefit laws. Milbank Q. 1999;77(4):425–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.