Abstract
Ambulatory blood pressure monitoring (ABPM) is increasingly recommended for confirming hypertension diagnosis and ongoing hypertension monitoring. However, reimbursement in the United States is variable and low compared with other advanced health care systems. We examined the reimbursement of ABPM and factors associated with successful reimbursement. A retrospective analysis of IBM MarketScan® commercial claims database was conducted for patients ≥18 years with ≥1 ABPM claim from January 2012 to December 2016. The date of first the ABPM claim was used as the index date. Per‐beneficiary ABPM episode reimbursements were calculated by aggregating all ABPM‐related reimbursements within a 30‐day post‐index window, considered as an ABPM episode. Multivariable logistic regression was used to identify predictors of successful reimbursement. Of 20 875 beneficiaries with ABPM claims, 16 920 (81.0%) were reimbursed. The median reimbursement per beneficiary for an ABPM episode was $89 (Inter Quartile Range [IQR], $62, $132), driven primarily by reimbursement for the full procedure (median, $86; IQR, $66, $110). Comparing benefit plan types, consumer‐directed health plans provided the highest median reimbursement ($96; IQR, $61, $175). Successful reimbursement was associated with female patient sex (adjusted OR [aOR], 1.20; 95% CI, 1.11‐1.28), having a health maintenance organization (aOR 2.11; 95% CI, 1.82‐2.43) or point of service (aOR 2.08; 95% CI, 1.74‐2.49) as benefit plan types, claim filing by a specialist (aOR 1.26; 95% CI, 1.14‐1.40) and services provided at an outpatient hospital (aOR 1.17; 95% CI, 1.01‐1.35). Among commercially insured Americans, our data suggest significant variability in successful reimbursement. Accordingly, more uniform criteria for ABPM reimbursement may facilitate greater use of guideline‐recommended monitoring.
Keywords: ambulatory blood pressure, cost, economics, guidelines, home blood pressure monitor, treatment and diagnosis
1. INTRODUCTION
Office blood pressure (BP) is routinely measured in the vast majority of health care interactions in the United States and serves as the primary diagnostic and treatment response criteria for hypertension.1 Yet, office BP is known to vary substantially within and across office visits and it is a poorer predictor of cardiovascular risk than BP measured via out‐of‐office methods, such as ambulatory blood pressure monitoring (ABPM).2 Accordingly, ABPM has long been recommended for confirming hypertension diagnosis, in part to rule out “white coat” hypertension (ie, elevated BP only in the health care setting), which is prevalent in up to one‐third of those with elevated office BP and associated with little excess cardiovascular risk compared to those without HTN.1, 4 Furthermore, ABPM is increasingly being recommended for monitoring antihypertensive therapy response in those with confirmed hypertension.1
Limited prior research, primarily in the Medicare population, suggests that ABPM continues to be employed infrequently.5 The Centers for Medicaid and Medicare Services (CMS) allow providers to be reimbursed for performing ABPM on patients with Medicare, but only in those with suspected white coat hypertension (WCH). Between 2007 and 2010, only 0.1% of Medicare beneficiaries had ABPM monitoring claims submitted, despite the fact that hypertension is highly prevalent (>50%) in this population.5, 6 Yet, Medicare covers only approximately 14% of Americans, and there is a paucity of data on ABPM reimbursement for the majority of Americans, who have commercial insurance. Moreover, it remains unclear to what extent commercial insurers follow Medicare requirements regarding utilization of ABPM in cases of suspected WCH. Therefore, we aimed to examine rates and predictors of reimbursement for ABPM among commercially insured US adults. We hypothesized that ABPM reimbursement would vary by commercial plan type, but reimbursement rates would be greater overall compared with prior estimates of Medicare reimbursement. We also hypothesized that ABPM reimbursement would be more successful in the presence of diagnostic codes indicating suspected WCH.
2. METHODS
We conducted a retrospective analysis of the IBM MarketScan® commercial claims database from January 2011 to December 2016. This database is a nationwide administrative claims data that includes records of patient enrollment, inpatient and outpatient medical claims, expenditures, and outpatient prescription drug claims for over 150 million beneficiaries covered under a variety of health benefit plans. The database is generally considered representative of the US population receiving medical insurance under employer‐sponsored programs (≈55% of the US population). This study was approved by the Institutional Review Board at the University of Florida.
2.1. Study population
Beneficiaries aged ≥18 years old with an ABPM claim between January 2012 and December 2016 (inclusive) were identified. ABPM claims were identified using Current Procedural Terminology (CPT) codes for full ABPM procedure (CPT 93784) and individual components, including procedure recording (93786), scan analysis & report (93788), and physician review & report (93790). The date of the first ABPM claim was used as the index date (see Figure S1 for schematic representation of cohort development). Patients were excluded if they did not have continuous medical enrollment for the 365 days before the index ABPM claim (365‐day lookback period) and 30 days after the index ABPM claim.
2.2. Study outcome
The primary outcome was reimbursement associated with an ABPM claim. The payments reported in the IBM MarketScan® database represent the amount eligible for payment to providers after deducting fee schedules and discounts, deductibles, copayments, and copays. All reimbursement amounts were adjusted to 2016 US dollars using a 3% inflation rate. Because multiple ABPM claims could represent a single ABPM session, we aggregated all ABPM claims submitted within a 30‐day window (beginning with and including the index date) as an ABPM episode per‐beneficiary, under the assumption that any claims within that 30‐day window would not represent a new ABPM order. Patients with at least one ABPM claim reimbursed (amount received by the provider>$0) in the 30‐day ABPM episode window were categorized as being reimbursed. For beneficiaries whose ABPM claims were reimbursed, we calculated the total amounts reimbursed in the 30‐day ABPM episode for the full procedure and individual component procedures.
2.3. Covariates
Demographic and clinical characteristics were assessed during the 365‐day lookback period. Study covariates included age (categorized as 18‐35, 36‐50, 51‐64, and ≥65 years), sex, geographic region (Northeast, North Central, South, West, and Unknown), type of benefit plan (health maintenance organization [HMO], point of service [POS], preferred provider organization [PPO], consumer‐directed health lan [CDHP], and all others), place of service (office, outpatient hospital, ambulatory surgical center, and others), and antihypertensive medication use prior to the index date (0 medications, 1‐2 medications, and ≥3 medications). We are aware anecdotally that some commercial plans give only certain providers (ie, specialists) the ability to submit and receive reimbursement for an ABPM claim. Accordingly, we also assessed provider type, categorizing ABPM episodes by whether they had ≥1 claim within the ABPM episode submitted by a specialist (cardiologist or nephrologist), generalist (Family Medicine, Internal Medicine, and Geriatrics), or neither. Comorbidities, including history of elevated BP without a hypertension diagnosis (ie, suspected WCH), hypertension, diabetes, chronic kidney disease, and coronary heart disease, were identified in the 365‐day lookback period based on the presence of ≥2 ICD‐9 or ICD‐10 codes in outpatient claims or ≥1 ICD‐9 or ICD‐10 code in inpatient claims (see Table S1 for specific codes used).
2.4. Statistical analysis
Descriptive statistics were used to characterize the overall population with any ABPM claim submitted, regardless of reimbursement status. We also compared baseline characteristics between patients with and without suspected WCH during the baseline period using a diagnosis of elevated BP without hypertension (ICD‐9‐CM 796.2 or ICD‐10‐CM R03.0). We used this diagnostic code as Medicare requires it for reimbursement of ABPM. Chi‐square tests were used to compare differences in individuals’ demographic and clinical characteristics between those who were reimbursed vs not within the two groups (with and without a diagnosis of elevated BP without hypertension). The median reimbursement per beneficiary for an ABPM episode were compared across different type of ABPM procedures. We also performed secondary analyses comparing per‐beneficiary episode reimbursement stratified by type of insurance benefit plan. Multivariable logistic regression was used to predict the likelihood of having reimbursement greater than zero. All probability values were considered significant at P < .05. Statistical analyses were performed using SAS 9.4 (SAS Institute Inc).
3. RESULTS
Between January 2012 and December 2016, ABPM claims were submitted for 31 257 beneficiaries, and of these, 20 875 met the inclusion criteria and comprised the primary study cohort (Figure 1). Table 1 describes the characteristics of the study cohort overall and by the presence of an elevated BP without hypertension diagnosis on the ABPM claim. A majority of the patients were aged 51‐64 years (55.1%), and 52.5% patients were women. Nearly two‐thirds of patients had a history of hypertension. An elevated BP without hypertension diagnosis was listed on 10 338 (50%) ABPM claims.
Figure 1.
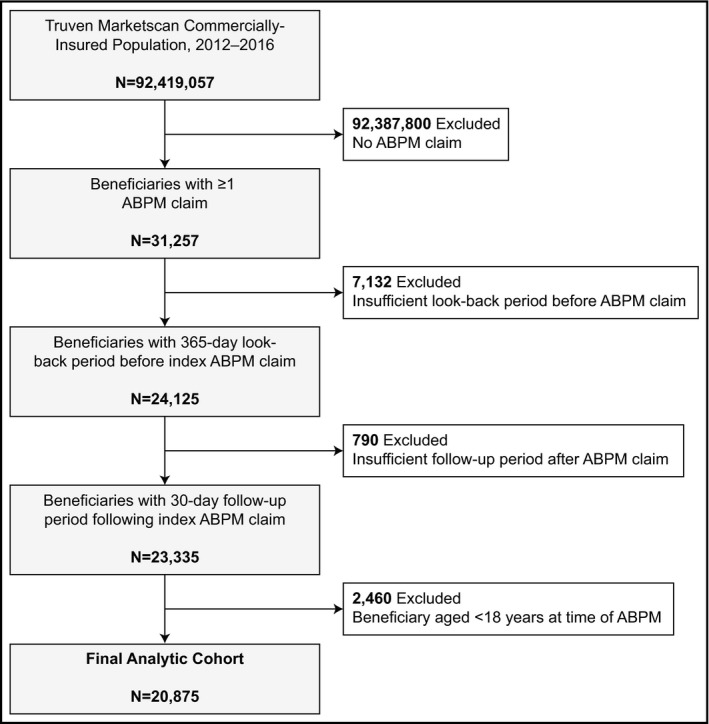
Patient flow during cohort development. ABPM, ambulatory blood pressure monitoring
Table 1.
Characteristics of beneficiaries with an ambulatory blood pressure monitoring claim, overall and by the presence of an elevated blood pressure without hypertension diagnosis on the ABPM claim
| Characteristics |
Overall cohort (N = 20 875) |
Elevated BP without HTN Diagnosis on ABPM claim | ||
|---|---|---|---|---|
|
Absent (n = 10 537) |
Present (n = 10 338) |
P value | ||
| Beneficiary | ||||
| Age, years | ||||
| 18‐35 | 2895 (13.9%) | 1440 (13.7%) | 1455 (14.1%) | .11 |
| 36‐50 | 6454 (30.9%) | 3202 (30.4%) | 3252 (31.4%) | |
| 51‐64 | 11 504 (55.1%) | 5881 (55.8%) | 5623 (54.4%) | |
| ≥65 | 22 (0.1%) | 14 (0.1%) | 8 (0.1%) | |
| Female sex | 10 963 (52.5%) | 5551 (52.7%) | 5412 (52.4%) | .63 |
| History of elevated BP without HTN | 6906 (33.1%) | 3458 (32.8%) | 3448 (33.4%) | .41 |
| History of HTN | 13 732 (65.8%) | 6910 (65.6%) | 6822 (66.0%) | .53 |
| History of DM | 2780 (13.3%) | 1417 (13.4) | 1363 (13.2) | .58 |
| History of CKD | 1212 (5.8%) | 607 (5.8%) | 605 (5.9%) | .78 |
| History of CHD | 1771 (8.5%) | 907 (8.6%) | 864 (8.4%) | .52 |
| No. of antihypertensivesd | ||||
| Beneficiaries with pharmacy benefits | 17 879 (85.7%) | 9149 (86.8%) | 8730 (84.4%) | |
| 0 | 10 444 (59.0%) | 5394 (59.0%) | 5050 (57.9%) | .28 |
| 1‐2 | 5844 (32.4%) | 2961 (32.3%) | 2883 (33.0%) | |
| ≥3 | 1591 (8.6) | 794 (8.7%) | 797 (9.1%) | |
| Region | ||||
| Northeast | 8437 (40.4%) | 3410 (32.4%) | 5027 (48.6%) | <.0001 |
| North Central | 3417 (16.4%) | 1789 (17.0%) | 1628 (15.8%) | |
| South | 6015 (28.8%) | 3567 (33.8%) | 2448 (23.7%) | |
| West | 2781 (13.3%) | 1654 (15.7%) | 1127 (10.9%) | |
| Unknown | 225 (1.1%) | 117 (1.1%) | 108 (1.0%) | |
| Type of benefit plan | ||||
| HMO | 2367 (11.3%) | 1255 (11.9%) | 1112 (10.8%) | <.0001 |
| POS | 1707 (8.2%) | 813 (7.7%) | 894 (8.6%) | |
| PPO | 12 671 (60.7%) | 6354 (60.3%) | 6317 (61.1%) | |
| CDHP | 1461 (7.0%) | 811 (7.7%) | 650 (6.3%) | |
| Othersc | 2669 (12.8%) | 1304 (12.4%) | 1365 (13.2%) | |
| ABPM factors | ||||
| Reimbursed ABPM claim | 16 920 (81.0%) | 8507 (80.7%) | 8413 (81.4%) | .24 |
| ABPM procedure claim type | ||||
| Full procedure | 15 216 (72.9%) | 7363 (69.9%) | 7853 (76.0%) | <.0001 |
| Components | 5659 (27.1%) | 3174 (30.1%) | 2485 (24.0%) | |
| Provider factors | ||||
| ABPM claim filed under generalista | 8180 (39.2%) | 3779 (35.9%) | 4401 (42.6%) | <.0001 |
| ABPM claim filed under specialistb | 8112 (38.9%) | 3918 (37.2%) | 4194 (40.6%) | <.0001 |
| Place of service | ||||
| Office | 16 579 (79.4%) | 8151 (77.4%) | 8428 (81.5%) | <.0001 |
| Outpatient hospital | 3912 (18.7%) | 2055 (19.5%) | 1857 (18.0%) | |
| Ambulatory Surgical Center | 189 (0.9%) | 188 (1.8%) | 1 (0.00%) | |
| Others | 195 (1.0%) | 143 (1.3%) | 52 (0.5%) | |
Data are presented as N (%).
Abbreviations: ABPM, ambulatory blood pressure monitoring; BP, blood pressure; CDHP, consumer‐directed health plan; CHD, coronary heart disease; CKD, chronic kidney disease; DM, diabetes mellitus; HMO, health maintenance organization; HTN, hypertension; POS, point of service; and PPO, preferred provider organization.
Generalists include Family Medicine, Internal Medicine, and Geriatrics.
Specialists include cardiology and nephrology.
Others include Basic/major medical, Comprehensive, Exclusive Provider Organization and High‐deductible health plan.
Measured as number of antihypertensive classes filled at any time during the 365‐day lookback period; the denominator for percentages includes only those beneficiaries having pharmacy benefits.
Among the 20 875 submitted ABPM claims, 16 920 (81.1%) were reimbursed. Figure 2 summarizes reimbursement rates overall (per‐beneficiary) and by CPT code, among individuals with any reimbursement. The median reimbursement per beneficiary for an ABPM episode was $89 (IQR, $62, $132), driven primarily by full procedure codes which comprised 63% of all reimbursed claims, with a median reimbursement amount of $86 (IQR, $66, $110). Characteristics of outliers (top 1%, 5%, and 10% of overall reimbursement rates) are summarized in Supplemental Table S2. Per‐beneficiary reimbursement was similar across insurance types, with CDHP providing the highest median reimbursement ($96; IQR, $61, $175) followed by PPO ($89; IQR, $63, $128), HMO ($87; IQR, $60, $136) and POS ($86; IQR, $63, $132) plans (P < .0001; Figure 3). Figure S2 depicts the amount reimbursed per beneficiary and for each component for an ABPM episode, stratified by benefit plan type.
Figure 2.
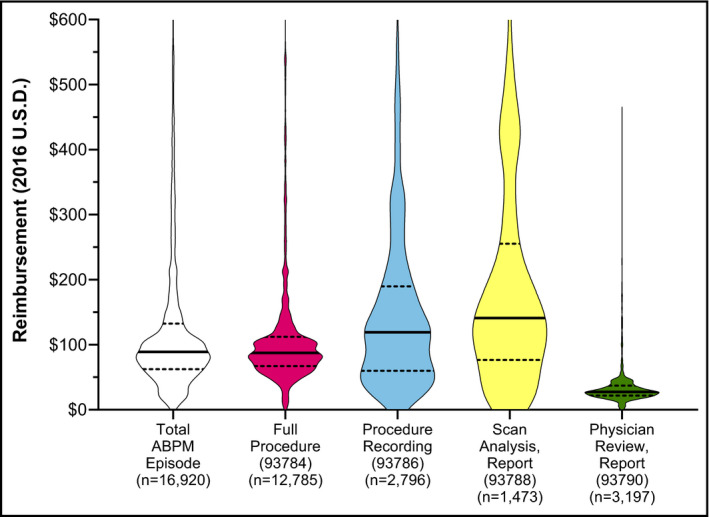
Reimbursement amounts per ABPM episode (aggregate) and stratified by CPT code. Data are represented in violin plots to display distribution of reimbursement amounts. Specific HCPCS codes are provided in x‐axis label parentheses. The thick black line represents the median reimbursement amount. The dotted lines represent the 25th and 75th percentiles for reimbursement amount (ie, the interquartile range). The figures are displayed with a maximum y‐axis value of $600, and thus, a small number of outliers are excluded from the graphical representation but included in median and interquartile range calculations
Figure 3.
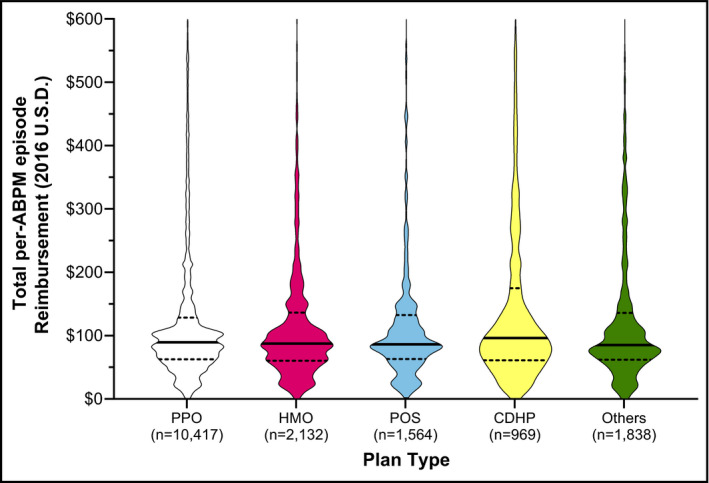
Amount reimbursed per beneficiary for an entire ABPM episode (aggregated), stratified by benefit plan type. Data are represented in violin plots to display distribution of reimbursement amounts. Reimbursement amounts represent aggregated values for all ABPM codes submitted within a 1‐month period following the first ABPM claim submission. The dotted lines represent the 25th and 75th percentiles for reimbursement amount (ie, the interquartile range). The figures are displayed with a maximum y‐axis value of $600, and thus, a small number of outliers are excluded from the graphical representation but included in median and interquartile range calculations. CDHP, consumer‐directed health plan; HMO, health maintenance organization; POS, point of service; and PPO, preferred provider prganization. Others include basic/major medical, comprehensive, emergency operation plans and high‐deductible health plans
Table 2 displays unadjusted comparisons between reimbursed and non‐reimbursed claims for beneficiary, ABPM, and provider characteristics, stratified on the presence/absence of a diagnosis of elevated BP without hypertension. In unadjusted analyses, there was no appreciable difference in the proportion of claims reimbursed comparing individuals with a diagnosis of elevated BP without hypertension (81.4%) versus those without (80.7%). Figure 4 summarizes independent predictors of successful ABPM claim reimbursement. We identified factors associated with receiving reimbursement including the followings: antihypertensive use. The odds of reimbursement varied by benefit plan type (greatest in POS and HMO plans) and geographic region (greatest in Northeast). Odds of reimbursement were also modestly greater for women than men (aOR 1.20; 95% CI, 1.11‐1.28), when the ABPM claim was filed under a specialist physician vs. a non‐specialist (aOR 1.26; 95% CI, 1.14‐1.40) and when ABPM services were provided at an outpatient hospital compared with the office (aOR 1.17; 95% CI, 1.01‐1.35).
Table 2.
Characteristics of beneficiaries with an ambulatory blood pressure monitoring claim, stratified by the presence of an elevated blood pressure without hypertension diagnosis on the ABPM claim and reimbursement status
| Characteristics | Elevated BP diagnosis on ABPM claim | |||||
|---|---|---|---|---|---|---|
| Present | Absent | |||||
|
ABPM not reimbursed (n = 1925) |
ABPM reimbursed (n = 8413) |
P value |
ABPM not reimbursed (n = 2030) |
ABPM reimbursed (n = 8507) |
P value | |
| Beneficiary factors | ||||||
| History of elevated BP without HTN | 612 (31.8%) | 2836 (33.7%) | .11 | 658 (32.4%) | 2800 (32.9%) | .67 |
| History of HTN | 1277 (66.3%) | 5545 (65.9%) | .72 | 1349 (66.4%) | 5561 (65.4%) | .36 |
| No. of antihypertensivesd | ||||||
| Beneficiaries with pharmacy benefits | 1745 (90.6%) | 6985 (83.0%) | 1812 (89.3%) | 7337 (86.2%) | ||
| 0 | 1010 (57.9%) | 4040 (57.8%) | .92 | 1110 (61.3%) | 4284 (58.4%) | .07 |
| 1‐2 | 580 (33.2%) | 2303 (33.0%) | 547 (30.2%) | 2414 (32.9%) | ||
| ≥3 | 155 (8.9%) | 642 (9.2%) | 155 (8.5%) | 639 (8.7%) | ||
| History of DM | 251 (13.0%) | 1112 (13.2%) | .83 | 262 (12.9%) | 1155 (13.6%) | .43 |
| History of CKD | 116 (6.0%) | 489 (5.8%) | .72 | 108 (5.3%) | 499 (5.9%) | .34 |
| History CHD | 148 (7.7%) | 716 (8.5%) | .24 | 168 (8.3%) | 739 (8.7%) | .55 |
| Beneficiary age, years | ||||||
| 18‐35 | 287 (14.9%) | 1168 (13.9%) | .31 | 291 (14.3%) | 1149 (13.5%) | .66 |
| 36‐50 | 609 (31.6%) | 2643 (31.4%) | 624 (30.8%) | 2578 (30.3%) | ||
| 51‐64 | 1026 (53.3%) | 4597 (54.6%) | 1113 (54.8%) | 4768 (56.1%) | ||
| ≥65 | 3 (0.2%) | 5 (0.1%) | 2 (0.1%) | 12 (0.1%) | ||
| Beneficiary sex | ||||||
| Male | 980 (50.9%) | 3946 (46.9%) | .002 | 1017 (50.1%) | 3969 (46.7%) | .005 |
| Female | 945 (49.1%) | 4467 (53.1%) | 1013 (49.9%) | 4538 (53.3%) | ||
| Region | ||||||
| Northeast | 606 (31.5%) | 4421 (52.5) | <.0001 | 444 (21.9%) | 2966 (34.9%) | <.0001 |
| North Central | 389 (20.2%) | 1239 (14.7%) | 409 (20.1%) | 1380 (16.2%) | ||
| South | 600 (31.2%) | 1848 (22.0%) | 793 (39.1%) | 2774 (32.6%) | ||
| West | 313 (16.3%) | 814 (9.7%) | 370 (18.2%) | 1284 (15.1%) | ||
| Unknown | 17 (0.8%) | 91 (1.1%) | 14 (0.7%) | 103 (1.2%) | ||
| Type of benefit plan | ||||||
| HMO | 111 (5.8%) | 1001 (11.9%) | <.0001 | 124 (6.1%) | 1131 (13.3%) | <.0001 |
| POS | 60 (3.1%) | 834 (9.9%) | 83 (4.1%) | 730 (8.6%) | ||
| PPO | 1117 (58.0%) | 5200 (61.8%) | 1137 (56.0%) | 5217 (61.3%) | ||
| CDHP | 236 (12.3%) | 414 (4.9%) | 256 (12.6%) | 555 (6.5%) | ||
| Othersc | 401 (20.8%) | 964 (11.5%) | 430 (21.2%) | 874 (10.3%) | ||
| ABPM factors | ||||||
| ABPM procedure claim type | ||||||
| Full procedure | 1457 (75.7%) | 6396 (76.0%) | .76 | 1387 (68.3%) | 5976 (70.3%) | .09 |
| Components | 468 (24.3%) | 2017 (24.0%) | 643 (31.7%) | 2531 (29.7%) | ||
| Provider factors | ||||||
| ABPM claim filed under generalista | 921 (47.8%) | 3480 (41.4%) | <.0001 | 813 (40.0%) | 2966 (34.9%) | <.0001 |
| ABPM claim filed under specialistb | 667 (34.6%) | 3527 (41.9%) | <.0001 | 646 (31.8%) | 3272 (38.5%) | <.0001 |
| Place of service | ||||||
| Office | 1575 (81.8%) | 6853 (81.5%) | .40 | 1579 (77.8%) | 6572 (77.3%) | .003 |
| Outpatient hospital | 336 (17.5%) | 1521 (18.1%) | 375 (18.4%) | 1680 (19.7%) | ||
| Ambulatory Surgical Center | 0 (0.0%) | 1 (0.0%) | 32 (1.6%) | 156 (1.8%) | ||
| Others | 14 (0.7%) | 38 (0.4%) | 44 (2.2%) | 99 (1.2%) | ||
Data are presented as N (%).
Abbreviations: ABPM, ambulatory blood pressure monitoring; BP, blood pressure; CDHP, consumer‐directed health plan; CHD, coronary heart disease; CKD, chronic kidney disease; and DM, diabetes mellitus; HMO, health maintenance organization; HTN, hypertension; POS, point of service; PPO, preferred provider organization.
Generalists include Family Medicine, Internal Medicine, and Geriatrics.
Specialists include cardiology and nephrology.
Others include Basic/major medical, Comprehensive, Exclusive Provider Organization and High‐deductible health plan.
Measured as number of antihypertensive classes filled at any time during the 365‐day lookback period; the denominator for percentages includes only those beneficiaries having pharmacy benefits.
Figure 4.
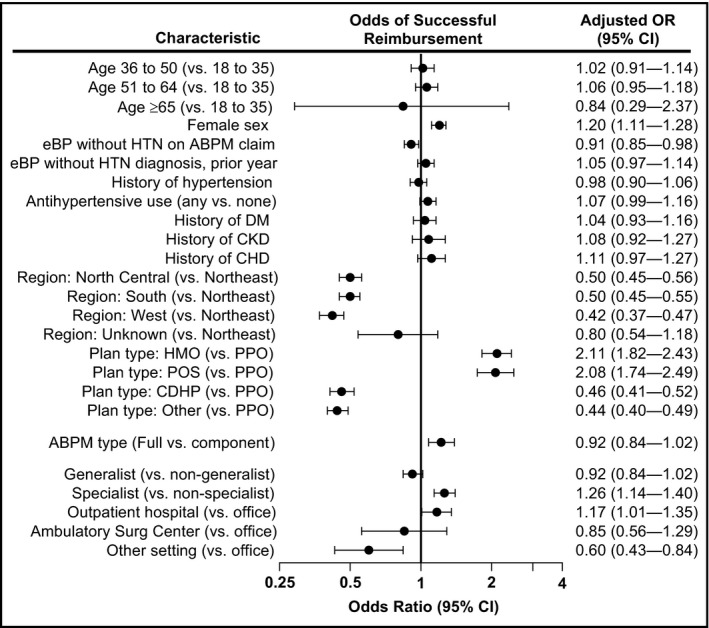
Predictors of successful reimbursement of an ambulatory blood pressure monitoring claim. ABPM, ambulatory blood pressure monitoring; CDHP, consumer‐driven health plan; CHD, coronary heart disease; CKD, chronic kidney disease; DM, diabetes mellitus; eBP, elevated blood pressure; HMO, health maintenance organization; HTN, hypertension; POS, point of service; and PPO, preferred provider organization
4. DISCUSSION
Ambulatory blood pressure monitoring has been recommended in national US hypertension guidelines for at least two decades, and the most recent guidelines suggest that nearly half of all hypertensive individuals in the United States (>100 million individuals) meet at least one indication for performing out‐of‐clinic BP monitoring.7 Yet, real world data on clinical use and reimbursement of out‐of‐office monitoring, including ABPM, remain sparse. Accordingly, we analyzed claims submitted for ABPM among a large, diverse population of US adults receiving employer‐sponsored commercial insurance between 2012 and 2016. Our major findings are that ABPM claims are filed infrequently, yet among submitted claims, reimbursement appears to be common, with approximately 80% of claims reimbursed. Furthermore, reimbursement amounts for the procedures are relatively high overall, with relatively little variance across insurance plan types. We also found several predictors of successful reimbursement, suggesting that individual plans may differ significantly with regard to criteria required for successful reimbursement and it appears that many plans do not follow Medicare criteria limiting ABPM reimbursement to those with suspected WCH.
We observed ABPM claims filed for approximately 1.5 per 1000 individuals between 2012 and 2016, in line with prior estimates from the Medicare population (~1 per 1000 individuals per year).5, 6 Infrequent use of ABPM could occur because of low reimbursement (eg, due to ABPM being a non‐covered procedure or because of strict criteria for reimbursement) or reimbursement amounts (ie, making ABPM use financially unappealing to providers). However, our data suggest that neither of these factors satisfactorily explain infrequent claim submissions. Of the submitted ABPM claims, approximately 80% were successfully reimbursed in our analysis. A previous analysis of Medicare beneficiaries found only two‐thirds of submitted claims were successfully reimbursed using the same criteria for defining reimbursement.6 We anticipated that ABPM reimbursement might be more common among Medicare patients than the commercially insured population, given the former's population characteristics (older, more likely to exhibit elevated office BP) and the fact that Medicare has reimbursed ABPM since 2001, with clear guidance as to requirements for reimbursement.4 However, it may be that, in practice, ABPM tends to be used earlier (ie, before patients transition to Medicare coverage) or that some employer‐based insurance programs provide greater flexibility in terms of patient eligibility for ABPM coverage. Unlike CMS, which requires a diagnosis of suspected WCH to receive reimbursement for ABPM, this diagnosis was present in only 50% of successfully reimbursed claims overall (n = 8413) and 80% of claims without this diagnosis were still successfully reimbursed (Table 2). In fact, in adjusted analyses, odds of reimbursement were modestly lower (OR 0.91; 95% CI 0.85‐0.98) for claims associated with a suspected WCH diagnosis. Thus, it appears that many commercial plans do not strictly follow Medicare guidance with respect to requirements for utilization of ABPM. Unfortunately, our data source did not allow for identification of individual plans and review of ABPM requirements for confirmation.
The median per‐beneficiary reimbursement amount was $89, with little difference observed comparing insurance types. Although inflation adjusted to 2016 US dollars, this reimbursement amount is significantly higher than that observed in the Medicare population between 2007 and 2010. In the overall cohort herein, we observed a median reimbursement of $86 for the full ABPM procedure (CPT 93784) that was lower than the median reimbursement for the individual components of procedure recording (CPT 93786, $118) and scan analysis and report (CPT 93788, $140). However, reimbursement amounts for both of these individual components were derived from relatively few claims, and these claims were remarkably heterogenous with regard to reimbursement amounts. This finding is discordant with prior Medicare analyses where the full procedure was associated with a greater median reimbursement amount than the individual components.6 We hypothesized that this finding could be in part due to different reimbursement rates among plan types; however, similar patterns were observed comparing reimbursement amounts by procedure code when stratifying on plan type. Nevertheless, it is likely that individual plans differ with regard to reimbursement for the individual components and full procedure and we suspect that, for most plans, the full procedure is associated with greater reimbursement than the components.
We found several factors to be associated with increased odds of successful ABPM reimbursement, including a specialist physician submitting the claim (OR 1.27). We are aware, anecdotally, of some plans establishing criteria as to the type of provider that may submit ABPM claims, and our data suggest that this practice may be somewhat widespread. Further, both beneficiary region and plan type were associated with successful reimbursement. Approximately 40% of claims were submitted for beneficiaries in the Northeast, where claims were more likely to be reimbursed. This finding may reflect less restrictive criteria for ABPM reimbursement in this area. Alternatively, it may be that the relatively high proportion of claims from this region indicates greater experience among providers and billing staff with ABPM and claims submittal. Interestingly, about one‐quarter of claims submitted were for beneficiaries residing in the South, where hypertension and hypertensive heart disease are most prevalent.8, 9, 10 Yet, odds of reimbursement for these beneficiaries were roughly half that of patients in the Northeast. Future research is needed to better understand this apparent disparity and the factors that drive it.
A final noteworthy point regarding predictors of successful reimbursement is that they suggest inconsistency in ABPM reimbursement and, by extension, criteria required by different health plans for successful reimbursement. Such inconsistency may also explain the relatively infrequent use of ABPM despite clear recommendations in national guidelines. Given current burdens on practitioners, it seems unreasonable to expect individual providers to have a thorough knowledge of each plan's requirements and significant differences in criteria may deter providers from attempting to utilize ABPM in patients whose clinical picture warrants such use. Greater clarity and, ideally, greater uniformity in criteria for ABPM reimbursement may improve utilization and consistency of ABPM reimbursement. Furthermore, alignment of ABPM reimbursement with recommended use scenarios in national guidelines is likely to significantly improve the use of ABPM. The Centers for Medicare and Medicaid Services has proposed expanding policies surrounding ABPM reimbursement for Medicare recipients, but such changes still fall far short of covering guideline‐recommended ABPM uses.11 Whether these proposed changes will prompt changes in reimbursement criteria among commercial plans is also unknown.
The strengths of our study include a focus on a large, diverse population of commercially insured individuals, who make up the majority of insured individuals in the United States. Nevertheless, our study has limitations. First, our study included only claims data and may not capture all uses of ABPM among this population. For example, some providers may bill patients directly for ABPM without submitting a claim to the insurance. Although we suspect this practice is relatively infrequent, it is likely that our data source underestimates total ABPM use among this population. Further, we cannot say with any certainty whether provider reimbursement under this type of model differs from that observed herein. Second, as noted above, we were unable to identify individual plans and link these with explicit criteria for ABPM reimbursement. We are aware of no prior surveys of plan‐specific ABPM criteria, but such may be helpful in confirming the presumed variation in criteria suggested by our data. Finally, our data do not capture ABPM use after publication of the most recent national guidelines that include the strongest recommendations for ABPM. Future research is needed to assess real world ABPM use and reimbursement subsequent to clinical implementation of these guidelines.
In conclusion, we found a low rate of utilization of ABPM for commercially insured patients. Reimbursement rates varied considerably across CPT codes, but minimally across plan types. Our data suggest that, unlike Medicare, ABPM is not often limited to individuals suspected WCH in the commercial market. Nevertheless, more uniform guidelines for ABPM reimbursement may facilitate increased utilization and allow greater implementation of evidence‐based guidelines for the diagnosis and ongoing management of hypertension.
AUTHOR CONTRIBUTIONS
Eric Detirich contributed to the study design, interpretation of results, and drafting and editing the manuscript; Raj Desai contributed to the study design, statistical design, data analysis, and drafting and editing the manuscript; Mahek Garg contributed to statistical design, data analysis, and editing the manuscript; Haesuk Park contributed to the study design, statistical design, data analysis, and editing the manuscript; Steven Smith contributed to the study design, statistical design, data analysis, and drafting and editing the manuscript.
Supporting information
Dietrich E, Desai R, Garg M, Park H, Smith SM. Reimbursement of ambulatory blood pressure monitoring in the US commercial insurance marketplace. J Clin Hypertens. 2020;22:6–15. 10.1111/jch.13772
Funding information
Dr Smith is supported by the National Heart, Lung and Blood Institute (K01 HL138172).
REFERENCES
- 1. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2018;71:1269‐1324. [DOI] [PubMed] [Google Scholar]
- 2. Eoin O, Gianfranco P, George S. Ambulatory blood pressure measurement. Hypertension. 2013;62:988‐994. [DOI] [PubMed] [Google Scholar]
- 3. The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch. Intern. Med. 1997;157:2413–2446. [DOI] [PubMed] [Google Scholar]
- 4. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560‐2572. [DOI] [PubMed] [Google Scholar]
- 5. Shimbo D, Kent ST, Diaz KM, et al. The use of ambulatory blood pressure monitoring among medicare beneficiaries in 2007–2010. J Am Soc Hypertens. 2014;8:891‐897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kent ST, Shimbo D, Huang L, et al. Rates, amounts, and determinants of ambulatory blood pressure monitoring claim reimbursements among medicare beneficiaries. J Am Soc Hypertens. 2014;8:898‐908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Booth JN, Hubbard D, Sakhuja S, et al. Proportion of US adults recommended out‐of‐clinic blood pressure monitoring according to the 2017 hypertension clinical practice guidelines. Hypertension. 2019;74:399‐406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Olives C, Myerson R, Mokdad AH, Murray CJL, Lim SS. Prevalence, awareness, treatment, and control of hypertension in united states counties, 2001–2009. PLoS ONE. 2013;8:e60308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Park S, Gillespie C, Baumgardner J, et al. Modeled state‐level estimates of hypertension prevalence and undiagnosed hypertension among US adults during 2013–2015. J Clin Hypertens (Greenwich). 2018;20:1395‐1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Roth GA, Dwyer‐Lindgren L, Bertozzi‐Villa A, et al. Trends and patterns of geographic variation in cardiovascular mortality among US counties, 1980–2014. JAMA. 2017;317:1976‐1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Proposed Decision Memo for Ambulatory Blood Pressure Monitoring (ABPM) (CAG‐00067R2), www.cms.gov/medicare-coverage-database/details/nca-proposed-decision-memo.aspx?NCAId=294
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


