Abstract
Background:
The Medicare Hospital Readmissions Reduction Program (HRRP) has led to fewer readmissions following hospitalizations with a principal diagnosis of heart failure (HF). Patients with HF are frequently hospitalized for other causes.
Objectives:
To compare trends in Medicare risk-adjusted, 30-day readmissions following principal HF hospitalizations and other hospitalizations with HF.
Methods:
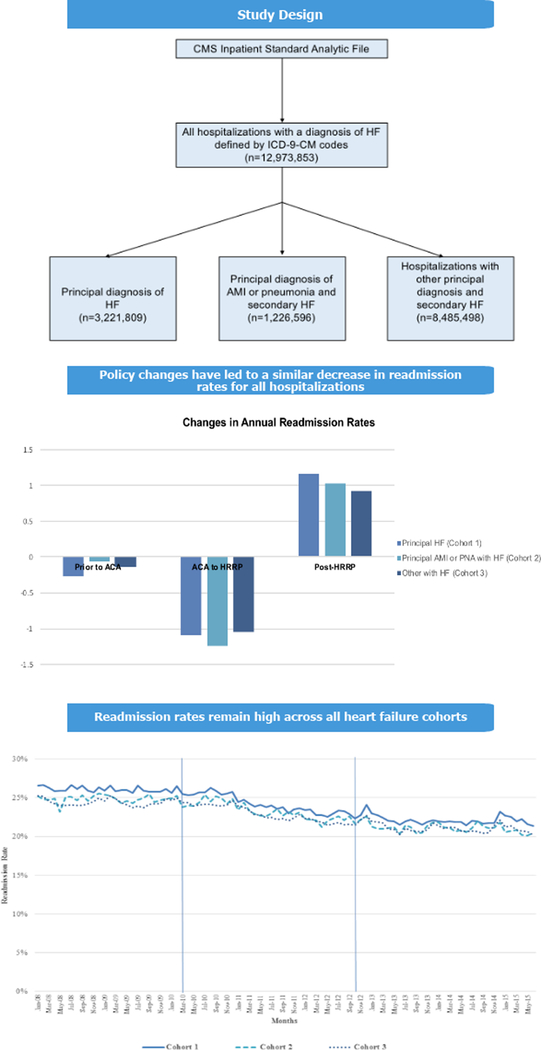
We performed a retrospective study of 12,973,853 Medicare hospitalizations with a principal or secondary diagnosis of HF between January 2008 and June 2015. Hospitalizations were categorized as: principal HF hospitalizations; principal acute myocardial infarction (AMI) or pneumonia hospitalizations with secondary HF; and other hospitalizations with secondary HF. We examined trends in risk-adjusted, 30-day, all-cause readmission rates for each cohort and trends in differences in readmission rates between cohorts using linear spline regression models.
Results:
Prior to passage of the Affordable Care Act (ACA) in March 2010, risk-adjusted, 30-day readmission rates were stable for all three cohorts, with mean monthly rates of 26.1%, 24.9%, and 24.4%, respectively. Risk-adjusted readmission rates started declining after the ACA passage by 1.09% (95% CI 0.51–1.68), 1.24% (95% CI 0.92–1.57) and 1.05% (95% CI 0.52–1.58) per year, respectively, until the implementation of the HRRP in October 2012 and then stabilized for all three cohorts.
Conclusion:
Patients with HF are often hospitalized for other causes and these hospitalizations have high readmission rates. Policy changes led to decrease in readmission rates for both principal and secondary HF hospitalizations. Readmission rates in both groups remain high, suggesting that initiatives targeting all hospitalized patients with HF continue to be warranted.
Keywords: Heart failure, hospitalizations, Medicare, outcomes
Condensed Abstract:
To compare trends in readmissions following principal heart failure (HF) hospitalizations and other hospitalizations with HF, we performed a retrospective study of 12,973,853 Medicare hospitalizations with HF. Readmission rates declined between passage of the Affordable Care Act and implementation of the Medicare Hospital Readmissions Reduction Program (HRRP) by 1.09% per year for patients with a principal diagnosis of HF and 1.05% for HF patients hospitalized for another reason; following HRRP, rates stabilized for both cohorts. These findings suggest policy changes led to decrease in readmission following both principal and secondary HF hospitalizations, though readmission rates remained high in both cohorts.
Introduction
The Hospital Readmission Reduction Program (HRRP) authorized the Centers for Medicare and Medicaid Services (CMS) to reduce payments to hospitals with higher than expected readmissions following hospitalizations for heart failure (HF), acute myocardial infarction (AMI), and pneumonia starting in 2012.(1) Hospitals have responded to HRRP with multimodal strategies to reduce readmissions, including improved patient education, risk stratification, arranging post-discharge follow up, and partnering with community physicians and hospitals;(2–4) concurrently, hospitals may have shifted some potential readmissions to observation units and increased coding of comorbidities.(5,6) As a result, there has been significant reduction in adjusted readmissions in the Medicare program, with reductions primarily occurring after passage of the Affordable Care Act (ACA), which announced HRRP, and then plateauing after implementation of HRRP.(6–10) Although readmissions have decreased following hospitalization for both targeted and non-targeted conditions, the greatest improvements have been observed following hospitalizations for HF, AMI, and pneumonia (6,7,9).
Unlike AMI and pneumonia, HF is a chronic disease. Patients with HF, which is associated with multiple other chronic diseases, are commonly hospitalized for causes other than acute HF; approximately three-fourths of the four million annual hospitalizations of HF patients are for other causes.(11,12) However, HRRP focuses only on acute HF. As a result, while some hospital initiatives to reduce readmissions, such as improving medicine reconciliation and discharge summaries,(2–4,13) may improve care for the entire population of patients with HF, other initiatives likely target only hospitalizations with a principal diagnosis of HF. For instance, many hospitals report having teams dedicated to reduce readmissions for acute HF,(3,14) but such teams may not be cost-effective for hospitalizations with a secondary diagnosis of HF, which are not subject to Medicare payment penalties.
The purpose of this study was to evaluate trends in readmission rates for patients with either a principal or secondary diagnosis of HF, i.e. those hospitalized for HF and those with HF hospitalized for other causes. We hypothesized that readmissions would decrease for all HF-related hospitalizations, due to the HRRP-driven incentives for patients hospitalized principally for HF and presumed spillover effect for HF patients hospitalized for other causes. However, because incentives only targeted principal HF hospitalizations, we further hypothesized that readmissions following these hospitalizations would decrease faster than hospitalizations for other causes.
Methods
We performed a retrospective cohort study of hospitalizations of Medicare beneficiaries discharged from non-federal, short-term acute care United States hospitals between January 2008 and June 2015. We included hospitalizations of patients with HF, age≥65, with continuous enrollment in Part A Medicare fee-for-service for at least one year prior and 30 days after the hospitalization (15). HF was defined based on standard International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes (9) as either a principal or secondary discharge diagnosis. We excluded hospitalizations of patients with prior hospice care or who had a discharge disposition of death, transfer to another acute hospital, or left against medical advice (AMA). Hospitalizations discharged in June 2012 were excluded because of an irregularity in data availability for that month. The primary data sources were the CMS Inpatient Standard Analytic File and the Medicare Enrollment Data Base.
Hospitalizations were categorized into one of three cohorts: 1) principal HF hospitalizations, i.e. those with HF listed as a principal diagnosis; 2) principal AMI or pneumonia hospitalizations with HF, i.e. those with a principal diagnosis of AMI or pneumonia based on standard ICD-9-CM codes and a secondary diagnosis of HF; 3) other hospitalizations with HF, i.e. those with a principal diagnosis other than HF, AMI, or pneumonia and a secondary diagnosis of HF. We separated hospitalizations with a principal diagnosis of AMI and pneumonia from other hospitalizations since HRRP targeted these two conditions and HF during the entire study period; therefore, the HRRP may have differentially affected readmission efforts related to these hospitalizations as compared to other hospitalizations.
For each cohort, we estimated monthly risk-adjusted unplanned readmission rates within 30 days of discharge, with adjustment for age and prior comorbidity based on publicly reported measures.(9,15) Comorbidities were defined using ICD-9-CM codes from any inpatient claim in the prior 12 months or as a secondary diagnosis in the index admission; codes were then grouped into CMS chronic condition categories.(15) Additionally, for cohort 2, we included an indicator in the model for whether the hospitalization was for AMI versus pneumonia; for cohort 3, we included variables for principal diagnosis based on the Agency for Healthcare Research and Quality (AHRQ) clinical classification software(16) plus an indicator variable for whether the hospitalization was a surgical hospitalization, based on categorization used in the CMS hospital-wide readmission measure (15). Planned readmissions were defined by the CMS algorithm as readmissions in which a typically planned procedure occurred in a hospitalization with a non-acute principal diagnosis (17).
To address concerns of increased documentation of comorbidity over time,(5,18) we capped the number of comorbidity risk factors adjusted by models at nine for each hospitalization. We chose nine risk factors because CMS increased the number of allowable diagnostic codes per hospitalization claim from nine to 25 in January 2011.(18) As a result, the percent of hospitalizations with more than nine risk factors increased from 7.4 to 16.5, 6.4 to 14.7, and 7.7 to 18.6 for the three cohorts, respectively, between pre-2011 and post-2011. To make hospitalization risk profiles comparable over time, we allowed each hospitalization to have a maximum of nine comorbidity-related risk factors. For hospitalizations with more than nine risk factors, we chose the nine most influential risk factors to be included in risk adjustment.
We examined trends in readmission rates for each of the three cohorts as well in trends in differences in readmission rates between the principal HF cohort and the other two cohorts. Our primary difference analysis was testing the trend in the difference in readmission rates between the principal HF and other with HF cohorts. Given concerns of competing risk between readmission and mortality following HF hospitalizations,(19,20) we also examined trends in a secondary, composite outcome of 30-day unplanned readmission or mortality.
Statistical Analysis
To estimate the risk-adjusted readmission rate by month, we first constructed a linear probability model for each of the three cohorts. The dependent variable of the model was 30-day unplanned readmission, and covariates included risk factors from the publicly reported measures(15) and dummy variables for each calendar month of the study period. To calculate the risk-adjusted readmission rate for a given month, all risk factors were set at their means for the cohort, the dummy variable for the given month was set to one, and dummy variables for all other months were set at zero. We used generalized estimating equations (GEE) models to account for correlation of outcomes within hospital (21) and used linear probability models in order to obtain monthly rates; logistic regression models would have required additional transformations to produce rates.
We then fit regression models for each of the three cohorts to estimate trends in readmission rates. The dependent variable was adjusted monthly rate of readmission, calculated as described above. The primary independent variable was time in years, included as a linear spline with knots at time of ACA passage and time of introduction of HRRP.(22) We evaluated time trend in readmission rates for three time periods based on coefficients of the three time variables: baseline trend (January 2008 to March 2010), change in trend after ACA but before HRRP (April 2010 through September 2012), and the additional change in trend post-HRRP (October 2012 through June 2015). Our models also included indicators for calendar quarter to account for seasonal effects. To account for serial correlation of monthly rates, we used ARIMA models; we first estimated a series of empty models to identify which autoregressive terms to include, if any, and included the corresponding lags in the final models.
We constructed two more linear spline regression models to evaluate the trends in differences in readmission rate between the principal HF cohort and the other two cohorts.(9) For these two models the dependent variables were the differences in monthly rates between cohorts 1 and 2 and cohorts 1 and 3. Again we used a linear spline with two knots to assess change in trends in differences in readmission rates for the three time periods of pre-ACA, between ACA and HRRP, and post-HRRP. For these models, no autocorrelations terms approached significance so none were included in the final models. We further evaluated the difference in risk-adjusted readmission rates between cohorts by calculating the difference in the fitted risk-adjusted readmission rates between cohorts at each of the four critical time points (beginning of study period, introduction of ACA, introduction of HRRP, and end of study period).We performed sensitivity analyses, in which we used the same linear probability models described above to estimate the monthly risk-adjusted rate of a composite outcome of post-discharge 30-day unplanned readmission or mortality for each cohort. We then fit the same linear spline regression models with two knots to estimate trends in the composite outcome rates over time for each cohort as well as trends in between-cohort differences in the composite outcome rates. Due to incomplete mortality data in February 2014, we excluded this month from the analyses of the composite outcome.
All analyses were done in SAS version 9.3 (SAS Institute Inc., Cary, NC) and Stata version 15.1 (StataCorp LLC, College Station, TX). Statistical significance was pre-specified at an alpha level of 0.05 (two-tailed).
Results
We included 12,973,853 hospitalizations in the study, of which 3,221,809 (24.8%) had a principal diagnosis of HF, 1,226,596 (9.8%) had a secondary diagnosis of HF with a principal diagnosis of AMI or pneumonia, and 8,485,498 (65.4%) had a secondary diagnosis of HF with another principal diagnosis. The mean age for the three cohorts was similar at 80.6, 80.4, and 80.0, respectively (Table 1, online Table 1).
Table 1. Baseline characteristics of Medicare hospitalizations with a diagnosis of heart failure (HF).
Cohort 1 represents hospitalizations with a principal diagnosis of HF; cohort 2, hospitalizations with a principal acute myocardial infarction (AMI) or pneumonia (PNA) with a secondary diagnosis of HF; cohort 3, hospitalizations with a principal diagnosis other than HF, AMI, or PMA and a secondary diagnosis of HF.
| Characteristics | Principal HF (Cohort 1) | Principal AMI/PNA with HF (Cohort 2) | Other Principal with HF (Cohort 3) |
|---|---|---|---|
| Cohort Size | 3,221,809 | 1,266,546 (AMI, 41.2%; PNA, 58.8%) | 8,485,498 |
| Age, mean(SD) | 80.6 (8.2) | 81.0 (8.3) | 80 (8.2) |
| Metastatic cancer/acute leukemia | 1.58 | 2.02 | 2.23 |
| Severe cancer | 3.82 | 5.12 | 4.39 |
| Other cancers | 4.36 | 3.61 | 4.87 |
| Severe hematological disorders | 2.5 | 2.19 | 2.43 |
| Coagulation defects and other specified hematological disorders | 5.48 | 3.65 | 5.5 |
| Iron deficiency or other unspecified anemias and blood disease | 47.73 | 46.68 | 50.87 |
| End-stage liver disease | 1.96 | 1.18 | 2.36 |
| Pancreatic disease; peptic ulcer, hemorrhage, other specified gastrointestinal disorders | 1.49 | 1.55 | 2.29 |
| Dialysis status | 2.91 | 2.87 | 3.38 |
| Renal failure | 40.76 | 30.47 | 36.02 |
| Transplants | 0.58 | 0.5 | 0.69 |
| Severe infection | 1.07 | 1.44 | 1.63 |
| Other infectious disease & pneumonias | 35.35 | 34.28 | 36.26 |
| Septicemia, sepsis, systemic inflammatory response syndrome/shock | 3.41 | 3.31 | 4 |
| Coronary atherosclerosis or angina, cerebrovascular disease | 80.15 | 71.74 | 71.11 |
| Specified arrhythmias and other heart rhythm disorders | 44.67 | 32.22 | 39.7 |
| Cardio-respiratory failure and shock | 19.97 | 18.54 | 19.36 |
| Coronary obstructive pulmonary disease (COPD) | 41.35 | 45.58 | 39.87 |
| Fibrosis of lung or other chronic lung disorders | 4.38 | 6.67 | 4.78 |
| Protein-calorie malnutrition | 8.2 | 9.66 | 12.01 |
| Other significant endocrine and metabolic disorders; disorders of fluid/electrolyte/acid-base balance | 38.08 | 32.92 | 38.61 |
| Rheumatoid arthritis and inflammatory connective tissue disease | 3.63 | 4.74 | 4.86 |
| Diabetes mellitus | 45.75 | 42.65 | 42.99 |
| Decubitus ulcer or chronic skin ulcer | 7.58 | 6.36 | 9.64 |
| Hemiplegia, paraplegia, paralysis, functional disability | 3.71 | 5.08 | 5.73 |
| Seizure disorders and convulsions | 2.72 | 3.12 | 3.52 |
| Respirator dependence/tracheostomy status | 0.29 | 0.5 | 0.59 |
| Drug/alcohol psychosis or dependence | 1.66 | 2.08 | 2.83 |
| Psychiatric comorbidity | 19.45 | 18.32 | 19.26 |
| Hip fracture/dislocation | 2.48 | 2.75 | 2.96 |
| Congestive heart failure | 57.16 | 44.51 | 53.2 |
For principal HF hospitalizations (cohort 1), the risk-adjusted readmission rate was 26.6% in January 2008 and rates remained relatively stable until the introduction of ACA in March 2010 (Figure 1). Between the introduction of ACA and HRRP, the risk-adjusted readmission rate following principal HF hospitalizations declined by 1.09% (95% CI 0.51–1.68) per year (Table 2). At time of introduction of HRRP in October 2012, readmission rate was 22.3%. Following introduction of HRRP, readmission rates following principal HF hospitalizations increased by 1.16% (95% CI 0.72–1.61) per year relative to the prior period. That is, the downward trend in risk-adjusted readmission rates observed before the introduction of the HRRP was offset by the slowdown after the HRRP and the readmission rates achieved a steady status in the post-HRRP period (Table 2).
Figure 1. Trends in adjusted readmission rates for hospitalizations with heart failure.
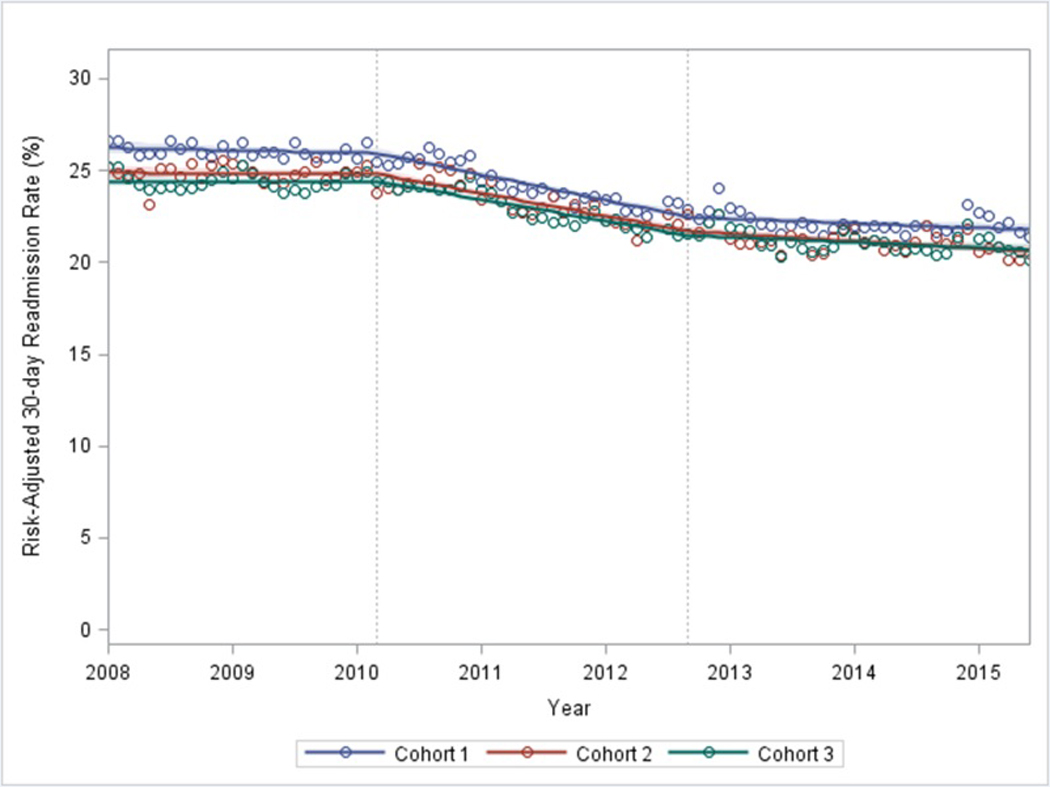
Cohort 1 represents hospitalizations with a principal diagnosis of HF; cohort 2, hospitalizations with a principal acute myocardial infarction (AMI) or pneumonia with a secondary diagnosis of HF; cohort 3, hospitalizations with a principal diagnosis other than HF, AMI, or pneumonia and a secondary diagnosis of HF. For each cohort, the circles represent the risk-adjusted 30-day readmission rate for a given month and the lines represent fitted regression lines of those rates, with shading for 95% confidence intervals. Vertical lines represent introduction of the Affordable Care Act (ACA) in March 2010 and the Hospital Readmission Reduction Program (HRRP) in October 2012.
Table 2. Annualized changes in risk-adjusted 30-day readmission rates following hospitalizations with a diagnosis of heart failure (HF) with introduction of the Affordable Care Act (ACA) and the Hospital Readmission Reduction Program (HRRP).
Cohort 1 represents hospitalizations with a principal diagnosis of HF; cohort 2, hospitalizations with a principal acute myocardial infarction (AMI) or pneumonia (PNA) with a secondary diagnosis of HF; cohort 3, hospitalizations with a principal diagnosis other than HF, AMI, or PNA and a secondary diagnosis of HF. Results for the second two time periods reflect annualized changes in risk-adjusted 30-day readmission rates as compared to the prior period.
| Prior to ACA | ACA to HRRP | Post-HRRP | ||||
|---|---|---|---|---|---|---|
| (January 2008 to March 2010) | (April 2010-September 2012) | (October 2012-June 2015) | ||||
| Annualized Change in Readmission Rate | p-value | Annualized Change in Readmission Rate, as compared to prior period | p-value | Annualized Change in Readmission Rate, as compared to prior period | p-value | |
| Principal HF (Cohort 1) | −0.27 [−0.68,0.14] | 0.19 | −1.09 [−1.68,−0.51] | <0.001 | 1.16 [0.72,1.61] | <0.001 |
| Principal AMI or PNA with HF (Cohort 2) | −0.06 [−0.27,0.15] | 0.55 | −1.24 [−1.57,−0.92] | <0.001 | 1.02 [0.69,1.36] | <0.001 |
| Other with HF (Cohort 3) | −0.13 [−0.47,0.21] | 0.46 | −1.05 [−1.58,−0.52] | <0.001 | 0.92 [0.44,1.41] | <0.001 |
Trends in risk-adjusted readmission rates followed a similar pattern for both hospitalization cohorts with a secondary diagnosis of heart failure: principal AMI or pneumonia hospitalizations with HF (cohort 2) and other hospitalizations with HF (cohort 3). Readmission rates were stable in the pre-ACA period, with mean monthly risk-adjusted rates of 24.9% for cohort 2 and 24.4% for cohort 3 (Figure 1, Table 2). Following introduction of ACA, the adjusted readmission rates decreased annually by 1.24% (95% CI 0.92–1.57) and 1.05% (95% CI 0.52–1.58) for cohorts 2 and 3, respectively. Following HRRP, readmission rates then increased as compared to the prior period by 1.02% (95% CI 0.69–1.36) and 0.92% (95% CI 0.44–1.41) per year for cohorts 2 and 3, respectively (Table 2). Overall, readmission rates were stable after the introduction of HRRP through June 2015, with mean risk-adjusted rates of 21.1% both cohorts 2 and 3.
In the analysis examining trends in differences between cohorts, we found that during the pre-ACA period, annualized readmission rates following principal HF hospitalizations decreased by 0.19% (95% CI 0.08–0.31) relative to those following other hospitalizations with HF (Online Table 2). Following introduction of ACA, there was no additional change in the relative difference in risk-adjusted readmission rates between these two cohorts, suggesting a continued small relative decrease in readmissions following principal HF hospitalizations as compared to other hospitalizations with HF (Figure; Online Table 2). Risk-adjusted readmission rates following principal HF hospitalizations versus other hospitalizations with HF then increased after HRRP as compared to the prior period (Online Table 2). As a result of these trends, the difference in risk-adjusted readmission rates following principal HF hospitalizations versus other hospitalizations with HF decreased from 1.6% at the beginning of the study period to 1.3% with the introduction of ACA and 0.9% with introduction of HRRP. This difference then slightly increased to 1.0% at the end of the study period. The difference in risk-adjusted readmission rates between cohorts 2 and 1 remained stable throughout the study period (Online Table 2).
We conducted sensitivity analyses, in which we created a composite outcome of post-discharge 30-day readmission or mortality and found trends in the composite outcomes generally followed a similar pattern (Online Figure 1). The risk-adjusted composite outcome rates following principal HF hospitalizations were stable in the pre-ACA period, with an annual change of −0.17% (95% CI −0.71 to 0.37), and then decreased by 1.11% (95% CI 0.33–1.88) per year between ACA and HRRP (Online Table 3). Following HRRP, rates for this composite outcome increased by 1.20% (95% CI 0.61–1.79) per year relative to the prior period. Similarly, following principal AMI or pneumonia hospitalizations with HF, the risk-adjusted composite outcome rates decreased by an average of 1.16% (95% CI 0.79–1.52%) per year following the introduction of the ACA until the introduction of the HRRP and then, relative to the prior period, increased by 0.76% (95% CI 0.32–1.19) following HRRP. We found no statistically significant changes in composite outcome rates over time for other hospitalizations with HF (Online Table 3). The difference in risk-adjusted composite outcome rates was stable between principal HF hospitalizations and the secondary HF cohorts in the pre-ACA period and the period between introduction of ACA and HRRP. In the post-HRRP period, the risk-adjusted composite outcome rate for principal HF hospitalizations was increasing relative to the composite outcome rate for principal AMI or pneumonia hospitalizations with HF by an average of 0.47% (95% CI 0.13–0.81) per year; in addition, the difference in composite outcome rates between principal HF hospitalizations and other hospitalizations with HF increased by an average of 0.41% (95% CI 0.20–0.62%) per year (Online Table 4).
Discussion
Among a national cohort of Medicare patients hospitalized with a diagnosis of heart failure between 2008 and 2015, we found that readmissions for both patients with a principal diagnosis of HF and patients with a secondary of HF significantly decreased after passage of the ACA. Readmissions following principal HF hospitalizations decreased marginally more than those following other hospitalizations with HF, a trend which had begun even prior to ACA. Following introduction of HRRP, the decrease in readmissions plateaued for both groups and the difference in readmission rates stabilized between groups. Trends in a composite outcome of 30-day risk-adjusted readmission or mortality generally followed a similar trend pattern, although this outcome improved following secondary HF hospitalizations as compared to principal HF hospitalizations in the post-HRRP period. In general, readmissions were frequent with relatively similar trends for all HF hospitalizations throughout the study period. Notably, readmission rates were above one-fifth for all three cohorts even by study end.
Hospitalizations with a principal diagnosis other than HF accounted for three-fourths of the nearly 13 million hospitalizations in our study. The frequency of these hospitalizations is notable given their high rates of readmission: during the first two years of the study period, over 24% of these hospitalizations resulted in a readmission. By comparison, the full population of Medicare patients with AMI or pneumonia had a much lower readmission rates (AMI: 20%, pneumonia 18%), and readmissions for all other conditions were even lower (17%) during this period.(9,23) The fact that readmission rates for patients with a secondary HF were nearly the same as the rates for patients with principal diagnosis of HF in our study suggests that any diagnosis of HF may be a more important risk factor for readmission than the principal discharge diagnosis. Although other studies have shown HF to be a risk factor for readmission and it is included in the CMS readmission risk model,(11,15) our findings specifically suggest that hospitalized patients with HF represent a high risk group that may be an appropriate target for readmission reduction efforts.
Similar to prior studies (6,9,10), we observed success in readmission reduction following principal HF hospitalization with the introduction of ACA. Concurrently, passage of ACA was associated with reduced readmissions for HF-related hospitalizations for other causes. This readmission reduction was likely a spillover effect of policy changes that had hospitals more focused on readmissions both generally and specifically for HF patients. Other studies have demonstrated readmission reduction across all conditions not targeted to ACA, findings that have been attributed to broad attention given to readmissions, general behavioral changes to reduce readmission, large scale implementation efforts to reduce them, and changes in coding practices.(5,6,9,18) Additionally, a number of initiatives to reduce readmissions following principal HF hospitalizations may reduce readmissions following HF-related hospitalizations for any cause. For instance, improving processes of transitional care including medicine reconciliation, appropriate transfer of information to the primary care provider, and ensuring early follow up appointments can likely be implemented across diagnoses.(2,4,24) Conversely, some higher intensity interventions such as follow up phone calls, individualized care management, and telemonitoring may be prioritized towards hospitalizations with a principal HF hospitalization that are subject to HRRP penalties.(2,4,25,26) Such prioritization may explain why secondary HF hospitalizations had a slightly lower decrease in readmissions when compared to principal HF hospitalizations. Nonetheless, even some of the hospitalizations for other causes may have received such high intensity interventions, as hospitalizations for HF may be difficult to differentiate clinically from hospitalizations related to common comorbidities such as COPD, pneumonia, or kidney disease. Since the final discharge diagnosis is only determined after many of these transitional care interventions are introduced, some of these higher cost interventions may have been utilized for hospitalizations for other causes.
Consistent with our hypothesis, we found that post-ACA readmission reduction was slightly greater following hospitalizations for HF than following other hospitalizations with HF. However, we were surprised that this difference began in 2008. This was two years prior to passage of ACA. Nonetheless, a number of initiatives may account for a small relative decline in readmissions for principal versus secondary HF during this period. Concerns for HF readmissions began well before ACA passage(27) and Medicare instituted publicly reporting of hospital readmission rates following hospitalizations for HF in 2009.(28) HF quality metrics were applied to hospitalizations for HF at the beginning of our study period; as a result, these metrics, which have been associated with improved post-discharge outcomes and are appropriate for all patients with HF, were more commonly achieved in hospitalizations for HF than hospitalizations for other causes.(29,30) Finally, many local hospital initiatives to reduce readmissions for heart failure were incorporated prior to ACA (25,31,32).
Our study should be interpreted in the context of potential limitations. Our categorization of heart failure was based on discharge diagnosis, which is subject to misclassification. As noted above, differentiating the principal reason for hospitalization as HF versus another condition such as COPD can be difficult. Although misclassification of the principal discharge diagnosis could have led to misclassification of study cohorts, this limitation would result in a conservative bias. Additionally, our study is limited to older Medicare beneficiaries so may not be generalizable to younger or privately insured patients. Finally, we did not account for observation stays in our analysis. Prior work has suggested that observation stays increased during this period; however, they do not appear to account for the decrease in readmissions over time (6).
Conclusion
Over three-fourths of Medicare hospitalizations with a diagnosis of HF were for causes other than acute HF and readmissions following other HF-related hospitalizations were similar to rates following acute HF hospitalizations. Although policy initiatives such as HRRP have targeted reducing readmissions following principal HF hospitalizations, such initiatives have had a spillover effect in reducing readmissions for other HF-related hospitalizations as well.
Supplementary Material
Central Illustration. Trends in Readmissions for Patients with Heart Failure in the Medicare Population. Hospitalized patients with heart failure (HF) were categorized into cohort based on principal diagnosis. Hospitalizations with a principal diagnosis of HF, hospitalizations with a principal diagnosis of acute myocardial infarction (AMI) or pneumonia and a secondary diagnosis of HF, and hospitalizations with a principal diagnosis other than HF, AMI, or pneumonia and a secondary diagnosis of HF all had similar reductions in adjusted readmission rates following introduction of the Affordable Care Act (ACA) followed by a relative increase in readmission rates following introduction of the Hospital Readmission Reduction Program (HRRP). Readmission rates were similar throughout the period for all three cohorts.
Core Clinical Competencies and Translational Outlook implications.
Medical Knowledge:
Patients with heart failure are frequently hospitalized for causes other than heart failure and are at high risk of readmission.
Systems Based Practice: In response to policy changes, hospitals have been effective at reducing readmissions for patients with heart failure, regardless of reason for hospitalization.
Translational Outlook 1:
Although readmission rates decreased for patients with heart failure, rates stabilized in more recent years. Whether systems of care will be able to implement additional programs to reduce readmissions remains to be seen.
Translational Outlook 2:
The specific strategies by which readmission reduction was achieved for both patients with a principal and secondary diagnosis of heart failure requires further investigation.
Acknowledgments
Funding: This study was supported by the Agency for Healthcare Research and Quality (AHRQ) grants R01HS022882 and K08HS23683.
Abbreviations
- HRRP
Hospital Readmission Reduction Program
- CMS
Centers for Medicare and Medicaid Services
- HF
heart failure
- AMI
acute myocardial infarction
- ACA
Affordable Care Act
- AMA
against medical advice
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- COPD
chronic obstructive pulmonary disease
Footnotes
Disclosures: Saul Blecker has received consulting fees from Medtronic outside of the submitted work. Jeph Herrin, Li Li Huihui Yu, Jacqueline Grady, and Leora Horwitz have received funding from CMS to develop readmission measures.
References
- 1.Centers for Medicare & Medicaid Services. Readmissions Reduction Program. Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed September 21,2018.
- 2.Kociol RD, Peterson ED, Hammill BG et al. National survey of hospital strategies to reduce heart failure readmissions: findings from the Get With the Guidelines-Heart Failure registry. Circ Heart Fail 2012;5:680–7. [DOI] [PubMed] [Google Scholar]
- 3.Ahmad FS, Metlay JP, Barg FK, Henderson RR, Werner RM. Identifying hospital organizational strategies to reduce readmissions. Am J Med Qual 2013;28:278–85. [DOI] [PubMed] [Google Scholar]
- 4.Bradley EH, Curry L, Horwitz LI et al. Hospital strategies associated with 30-day readmission rates for patients with heart failure. Circ Cardiovasc Qual Outcomes 2013;6:444–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ibrahim AM, Dimick JB, Sinha SS, Hollingsworth JM, Nuliyalu U, Ryan AM. Association of Coded Severity With Readmission Reduction After the Hospital Readmissions Reduction Program. JAMA Intern Med 2018;178:290–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, Observation, and the Hospital Readmissions Reduction Program. N Engl J Med 2016;374:1543–51. [DOI] [PubMed] [Google Scholar]
- 7.Medicare Hospital Quality Chartbook Performance Report on Outcome Measure. September 2014. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Downloads/Medicare-Hospital-Quality-Chartbook-2014.pdf. Accessed September 21, 2018.
- 8.Suter LG, Li SX, Grady JN et al. National patterns of risk-standardized mortality and readmission after hospitalization for acute myocardial infarction, heart failure, and pneumonia: update on publicly reported outcomes measures based on the 2013 release. J Gen Intern Med 2014;29:1333–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Desai NR, Ross JS, Kwon JY et al. Association Between Hospital Penalty Status Under the Hospital Readmission Reduction Program and Readmission Rates for Target and Nontarget Conditions. JAMA 2016;316:2647–2656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wasfy JH, Zigler CM, Choirat C, Wang Y, Dominici F, Yeh RW. Readmission Rates After Passage of the Hospital Readmissions Reduction Program: A Pre-Post Analysis. Ann Intern Med 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blecker S, Matsushita K, Fox E et al. Left ventricular dysfunction as a risk factor for cardiovascular and noncardiovascular hospitalizations in African Americans. Am Heart J 2010;160:488–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blecker S, Paul M, Taksler G, Ogedegbe G, Katz S. Heart failure-associated hospitalizations in the United States. J Am Coll Cardiol 2013;61:1259–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bradley EH, Sipsma H, Horwitz LI, Curry L, Krumholz HM. Contemporary data about hospital strategies to reduce unplanned readmissions: what has changed? JAMA Intern Med 2014;174:154–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bradley EH, Sipsma H, Curry L, Mehrotra D, Horwitz LI, Krumholz H. Quality collaboratives and campaigns to reduce readmissions: what strategies are hospitals using? J Hosp Med 2013;8:601–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Horwitz LI, Partovian C, Lin Z et al. Development and use of an administrative claims measure for profiling hospital-wide performance on 30-day unplanned readmission. Ann Intern Med 2014;161:S66–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.HCUP CCS. Healthcare Cost and Utilization Project (HCUP). March 2017. Agency for Healthcare Research and Quality, Rockville, MD: www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. [PubMed] [Google Scholar]
- 17.2016. Condition-Specific Measures Updates and Specifications Report Hospital-Level 30-Day Risk-Standardized Readmission Measures. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Downloads/AMI-HF-PN-COPD-and-Stroke-Readmission-Updates.zip. Accessed January 19,2017.
- 18.Blecker S, Herrin J, Kwon JY, Grady JN, Jones S, Horwitz LI. Effect of Hospital Readmission Reduction on Patients at Low, Medium, and High Risk of Readmission in the Medicare Population. J Hosp Med 2018;13:537–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gorodeski EZ, Starling RC, Blackstone EH. Are all readmissions bad readmissions? N Engl J Med 2010;363:297–8. [DOI] [PubMed] [Google Scholar]
- 20.Gupta A, Allen LA, Bhatt DL et al. Association of the Hospital Readmissions Reduction Program Implementation With Readmission and Mortality Outcomes in Heart Failure. JAMA Cardiol 2018;3:44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika 1986;73:13–22. [Google Scholar]
- 22.Greene WH. 2012. Econometric Analysis. 7th ed Upper Saddle River, NJ: Prentice Hall. [Google Scholar]
- 23.Centers for Medicare & Medicaid Services. Hospital Compare data archive. Available at: https://data.medicare.gov/data/archives/hospital-compare. Accessed March 5, 2018.
- 24.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med 2011;155:520–8. [DOI] [PubMed] [Google Scholar]
- 25.Amarasingham R, Patel PC, Toto K et al. Allocating scarce resources in real-time to reduce heart failure readmissions: a prospective, controlled study. BMJ Qual Saf 2013;22:998–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jenq GY, Doyle MM, Belton BM, Herrin J, Horwitz LI. Quasi-Experimental Evaluation of the Effectiveness of a Large-Scale Readmission Reduction Program. JAMA Intern Med 2016;176:681–90. [DOI] [PubMed] [Google Scholar]
- 27.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 2009;360:1418–28. [DOI] [PubMed] [Google Scholar]
- 28.Centers for Medicare & Medicaid Services. Hospital Compare Datasets. Available at: https://data.medicare.gov/data/hospital-compare. Accessed September 21, 2018.
- 29.Blecker S, Agarwal SK, Chang PP et al. Quality of care for heart failure patients hospitalized for any cause. J Am Coll Cardiol 2014;63:123–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bonow RO, Bennett S, Casey DE Jr et al. ACC/AHA clinical performance measures for adults with chronic heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Heart Failure Clinical Performance Measures) endorsed by the Heart Failure Society of America. J Am Coll Cardiol 2005;46:1144–78. [DOI] [PubMed] [Google Scholar]
- 31.Mudge A, Denaro C, Scott I, Bennett C, Hickey A, Jones MA. The paradox of readmission: effect of a quality improvement program in hospitalized patients with heart failure. J Hosp Med 2010;5:148–53. [DOI] [PubMed] [Google Scholar]
- 32.Krumholz HM, Amatruda J, Smith GL et al. Randomized trial of an education and support intervention to prevent readmission of patients with heart failure. J Am Coll Cardiol 2002;39:83–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.