Abstract
Introduction:
Disparities in health and healthcare access remain a major problem in the United States. The current study sought to investigate the relationship between patient insurance status and hospital selection for surgical care.
Methods:
Patients who underwent liver or pancreatic resection for cancer between 2004 and 2014 were identified in the National Inpatient Sample. The association of insurance status and hospital type was examined.
Results:
In total, 22,254 patients were included in the study. Compared with patients with private insurance, Medicaid patients were less likely to undergo surgery at urban non-teaching hospitals (OR=0.36, 95%CI 0.22–0.59) and urban teaching hospitals (OR=0.54, 95%CI 0.34–0.84) than rural hospitals. Medicaid patients were less likely to undergo surgery at private investor-owned hospitals (OR=0.53, 95%CI 0.38– 0.73) than private non-profit hospitals. In contrast, uninsured patients were 2.2-fold more likely to go to government funded hospitals rather than private non-profit hospitals (OR=2.19, 95%CI 1.76–2.71).
Conclusion:
Insurance status was strongly associated with the type of hospital in which patients underwent surgery for liver and pancreatic cancers. Addressing the reasons for inequitable access to different hospital settings relative to insurance status is essential to ensure that all patients undergoing pancreatic or liver surgery receive high quality surgical care.
Keywords: Insurance, hospital utilization, Hepatopancreatic cancer, Medicaid
INTRODUCTION
Disparities in health and healthcare access remain a major problem in the United States. In particular, racial minorities and low-income individuals face significant barriers to access care and often have inferior outcomes across numerous quality measures.[1–3] In addition, insurance status has been linked to discrepancies in outcomes among patients with cancers even after adjusting for cancer stage at the time of diagnosis.[4–8] In fact, utilization rates may vary across different insurance types and there are disparate outcomes among uninsured individuals receiving healthcare.[9, 10] In particular, previous studies showed that the uninsured patients had higher odds of in-hospital mortality among patients undergoing abdominal surgery. [11, 12] Although the implementation of new policies such as the Affordable Care Act (ACA) has expanded insurance coverage to approximately 20 million new individuals, whether this increased access to health insurance has reduced actual healthcare disparities remains debated.[13]
Patients undergoing hepatopancreatic (HP) procedures for a malignant indication are at a particular risk for variable outcomes relative to patient-, surgeon-, and hospital-factors.[14–18] In particular, HP surgery may be associated with high morbidity, as well as variable rates of failure-to-rescue, and health care expenditures depending on the surgeon and hospital.[19–22] As such, disparities in access to high-quality, high-volume surgical care can dramatically impact patient outcomes. In addition, disparities in access to care can affect overall rates of receipt of care concordant with national guidelines compliance and, in turn, lead to worse long-term oncological outcomes.[23–25] Recently, there has been an increased interest in understanding the reasons for the observed disparities in outcomes of among cancer patients undergoing HP procedures across different hospitals settings. Although several previous studies have investigated factors such as the volume outcome relationship among patients with hepatic and pancreatic cancers [26], no study has focused on the impact of insurance status on hospital selection among patients with HP cancers seeking surgical care. Therefore, the objective of the current study was to use a nationally representative database to define the association between insurance coverage and the hospital type at which patients with HP cancers received surgical care. Additionally, hospital charges were assessed across different hospital types and insurance status.
METHODS
Data Source
The National Inpatient Sample (NIS) is the largest publicly available all-payer inpatient database in United States. It is sponsored by the Agency of Healthcare Research and Quality as a part of the Healthcare Cost and Utilization Project (HCUP). The weighted estimates of the sample contain administrative discharge data on approximately 35 million hospitalizations nationwide each year.
Patients who underwent liver or pancreatic resection between 2004 and 2014 were identified with the corresponding International Classification of Diseases, 9th Revision (ICD-9) procedure codes for minor liver resection [partial hepatectomy (5022)] and major liver resections [hepatic lobectomy (503)], as well as minor pancreatic resection [distal pancreatectomy (5252), other partial pancreatectomy (5259)] and major pancreatic resection [proximal pancreatectomy (5251), radical subtotal pancreatectomy/ whipple (5253), total pancreatectomy (526) and radical pancreatoduodenectomy (527)]. Only patients who were 18 years or older were included in the study. Patients who underwent emergency or urgent operations and individuals with benign diseases were excluded.
Primary outcomes and Analytic variables
The primary exposure was the type of insurance coverage among patients undergoing care for HP cancers (private, Medicare, Medicaid, or no/other insurance type). The primary outcome measures were hospital location and teaching status (urban teaching, urban nonteaching, or rural), as well as hospital ownership status (private nonprofit, government [nonfederal], or private investor–owned).
Patient level characteristics included age, sex (male, female), race (White, Black and others), median household income (based on the national quartiles for the patient’s zip code), and mortality risk score (minor, moderate, major and extreme). Hospital characteristics included bed size and hospital volume (low, medium and high). The severity and mortality risk was based on the All Patient Refined–Diagnosis Related Group severity and mortality risk score respectively. [27] This score adjusts for the interactions among primary diagnosis, secondary diagnosis, age, and procedures occurring during hospitalization. On the basis of these factors, 4 subclasses were defined: 1) minor, 2) moderate, 3) major, and 4) extreme.[28] Hospital volume was determined by calculating the number of hepatic and pancreatic surgeries in each individual year (2004–2014) and were assigned to each individual case (patient) as a continuous variable. Hospital volume was divided into quintiles and categorized into three groups: low, medium and high volume. Total hospital charges were used to assess patterns in hospital payments stratified by hospital location, teaching status and insurance types.
Statistical Analyses
Patient demographics and treatment characteristics were compared among patients undergoing liver or pancreatic surgery stratified by insurance status. Discrete variables were reported as medians and interquartile ranges (IQR); categorical variables were reported as total count and frequencies. Bivariable analyses were performed using chi-squared or Wilcoxon rank test as appropriate. Multivariate multinomial logistic regression models were constructed to determine the association between the hospital location and teaching status, as well as hospital ownership status across insurance categories. All analyses were conducted using SAS 9.4 and a p-value of <0.05 (two tailed) was considered statistically significant.
RESULTS
Patient and Hospital Characteristics
A total of 22,254 patients who underwent a liver or pancreatic resection were included in the analytic cohort (Table 1). Median patient age was 64 years (IQR 55–72) and most patients were male (52.2%, n=11,615) and Caucasian (76.5%, n=17,034). The majority of patients were insured by Medicare (47.1%, n=10,595) or private insurance (44.7%, n=9,766), whereas 6.1% (n=1,418) were insured by Medicaid; 2.2% (n=475) were uninsured. In addition, most patients undergoing HP surgery belonged to the higher income quartiles (29.8%, n=6,470). Majority of patient had moderate mortality risk (42.0%, n=9,347) whereas major severity risk (44.8%, n=9,965) across all insurance types. Overall the most common procedures performed were a major pancreatic resection (36.8%, n=8,189) or a minor liver resection (36.9%, n=8,215). The vast majority of hospitals performing HP procedures were urban teaching hospitals (87.3%, n=19,424) and private non-profit hospitals (78.5%, n=17,477). In addition, most HP procedures were performed at high volume hospitals (98.6%, n=21,947), irrespective of insurance status.
Table 1:
Patient characteristics stratified by the insurance status
| Patient Characteristic, No. (%) | Total | Medicare | Medicaid | Private | Uninsured | P-value |
|---|---|---|---|---|---|---|
| All patient | 22254 (100%) | 10595 (47.1%) | 1418 (6.1%) | 9766 (44.7%) | 475 (2.2%) | |
| Age, year (median, IQR) | 64 (55–72) | 72 (67–77) | 55 (47–61) | 57 (50–62) | 57 (49–63) | <0.001 |
| Gender | 0.090 | |||||
| Male | 11615 (52.2%) | 5484 (51.8%) | 731 (51.6%) | 5148 (52.7%) | 252 (53.1%) | |
| Female | 10638 (47.8%) | 5110 (48.2%) | 687 (48.4%) | 4618 (47.3%) | 223 (46.9%) | |
| Race | <0.001 | |||||
| White | 17034 (76.5%) | 8455 (79.8%) | 756 (53.3%) | 7566 (77.5%) | 257 (54.1%) | |
| Black | 1869 (8.4%) | 775 (7.3%) | 254 (17.9%) | 790 (8.1%) | 50 (10.5%) | |
| Other/Unknown | 3351 (15.1%) | 1365 (12.9%) | 408 (28.8%) | 1410 (14.4%) | 168 (35.4%) | |
| Income quartile | <0.001 | |||||
| 1st (lowest) | 4462 (20.5%) | 2208 (21.2%) | 491 (35.8%) | 1646 (17.3%) | 117 (28.3%) | |
| 2nd | 5231 (24.1%) | 2580 (24.8%) | 417 (30.4%) | 2115 (22.2%) | 119 (28.8%) | |
| 3rd | 5568 (25.6%) | 2631 (25.3%) | 291 (21.2%) | 2543 (26.7%) | 103 (24.9%) | |
| 4th (highest) | 6470 (29.8%) | 2999 (28.8%) | 173 (12.6%) | 3224 (33.8%) | 74 (17.9%) | |
| Mortality risk | <0.001 | |||||
| Minor | 6412 (28.8%) | 2415 (22.8%) | 478 (33.7%) | 3361 (34.4%) | 158 (33.3%) | |
| Moderate | 9347 (42.0%) | 4252 (40.1%) | 576 (40.6%) | 4303 (44.1%) | 216 (45.5%) | |
| Major | 4420 (19.9%) | 2573 (24.3%) | 269 (19%) | 1512 (15.5%) | 66 (13.9%) | |
| Extreme | 2075 (9.3%) | 1355 (12.8%) | 95 (6.7%) | 590 (6%) | 35 (7.4%) | |
| Severity risk | <0.001 | |||||
| Minor | 1668 (7.5%) | 620 (5.9%) | 113 (7.9%) | 890 (9.1%) | 45 (9.5%) | |
| Moderate | 7981 (35.9%) | 3282 (31.0%) | 537 (37.9%) | 3969 (40.6%) | 193 (40.6%) | |
| Major | 9965 (44.8%) | 5138 (48.5%) | 593 (41.8%) | 4043 (41.4%) | 191 (40.2%) | |
| Extreme | 2640 (11.9%) | 1555 (14.7%) | 175 (12.4%) | 864 (8.9%) | 46 (9.7%) | |
| Complexity | <0.001 | |||||
| Pancreas | ||||||
| Major | 8189 (36.8%) | 4476 (42.25%) | 411 (29.0%) | 3128 (32.0%) | 174 (36.6%) | |
| Minor | 2674 (12.02%) | 1397 (13.2%) | 126 (8.9%) | 1104 (11.3%) | 47 (9.9%) | |
| Liver | ||||||
| Major | 8215 (36.9%) | 3381 (31.9%) | 654 (46.1%) | 3995 (40.9%) | 185 (38.9%) | |
| Minor | 3176 (14.3%) | 1341 (12.7%) | 227 (16.01%) | 1539 (15.7%) | 69 (14.5%) | |
| Hospital location/teaching status | <0.001 | |||||
| Rural | 304 (1.4%) | 173 (1.6%) | 28 (2%) | 97 (1%) | 6 (1.3%) | |
| Urban nonteaching | 2526 (11.4%) | 1302 (12.3%) | 105 (7.4%) | 1082 (11.1%) | 37 (7.8%) | |
| Urban teaching | 19424 (87.3%) | 9120 (86.1%) | 1285 (90.6%) | 8587 (87.9%) | 432 (90.9%) | |
| Hospital Control | <0.001 | |||||
| Government (nonfederal) | 3750 (16.9%) | 1534 (14.5%) | 325 (22.9%) | 1721 (17.6%) | 170 (35.8%) | |
| Private nonprofit | 17477 (78.5%) | 8560 (80.8%) | 1048 (73.9%) | 7576 (77.6%) | 293 (61.7%) | |
| Private investor–owned | 1027 (4.6%) | 501 (4.7%) | 45 (3.2%) | 469 (4.8%) | 12 (2.5%) | |
| Bed size | <0.001 | |||||
| Small | 1549 (7%) | 722 (6.8%) | 74 (5.2%) | 732 (7.5%) | 21 (4.4%) | |
| Medium | 3021 (13.6%) | 1524 (14.4%) | 193 (13.6%) | 1244 (12.7%) | 60 (12.6%) | |
| Large | 17684 (79.5%) | 8349 (78.8%) | 1151 (81.2%) | 7790 (79.8%) | 394 (82.9%) | |
| Hospital Volume | 0.004 | |||||
| Low | 233 (0.6%) | 80 (0.8%) | 70 (0.7%) | 38 (0.4%) | 5 (1.05%) | |
| Medium | 174 (0.78%) | 93 (0.9%) | 12 (0.9%) | 63 (0.7%) | 6 (1.26%) | |
| High | 21947 (98.6%) | 10422 (98.4%) | 1396 (98.5%) | 9665 (98.7%) | 464 (97.6%) |
IQR = Interquartile range
Factors Associated with the Hospital Location and Teaching Status
On multivariate analysis, after controlling for multiple competing factors, patients with Medicaid were 64% less likely to have surgery at an urban non-teaching hospital (OR 0.36, 95% CI 0.22–0.59) and 46% less likely to go to an urban teaching hospital (OR 0.54, 95% CI 0.34–0.84) versus a rural hospital compared with patients who had private insurance. In addition, male patients were 23% less likely to undergo HP surgery at an urban non-teaching (OR 0.77, 95% CI 0.60 – 0.99) hospital compared with female patients. Moreover, patient income was an important factor associated with hospital location and teaching status. Specifically, patients in the 3rd and 4th quartile of median household income were more likely to go to an urban teaching (3rd quartile: 3.63, 95% CI 2.49 – 5.28; 4th quartile: 26.01, 95% CI 12.98 – 52.23) or urban non-teaching hospital (OR 2.88, 95% CI 2.01– 4.12; 4th quartile: 16.94, 95% CI 8.52 – 33.70) than a rural hospital. In addition, patients undergoing a major liver resection were also more likely to undergo surgery at an urban non-teaching (OR 1.95, 95% CI 1.15–3.30) and urban teaching hospital (OR 2.06, 95% CI 1.23–3.44) than a rural hospital (Table 2).
Table 2:
Multivariate associations between insurance status and hospital location/ teaching
| Variable | Rural | Urban Nonteaching | Urban teaching | ||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | P-value | OR | 95% CI | P-value | ||
| Insurance | |||||||
| Private | Reference | ||||||
| Medicare | Reference | 0.75 | 0.53 – 1.06 | 0.11 | 0.83 | 0.59 – 1.16 | 0.27 |
| Medicaid | Reference | 0.36 | 0.22 – 0.59 | <0.001 | 0.54 | 0.34 – 0.84 | 0.007 |
| Uninsured | Reference | 0.58 | 0.23 – 1.45 | 0.24 | 0.80 | 0.34 – 1.88 | 0.60 |
| Gender | |||||||
| Male | 0.77 | 0.60 – 0.99 | 0.043 | 0.84 | 0.66 – 1.06 | 0.14 | |
| Female | Reference | Reference | |||||
| Age | 1.00 | 0.98 – 1.00 | 0.81 | 1.00 | 0.98 – 1.01 | 0.07 | |
| Income quartile | |||||||
| 1st | Reference | ||||||
| 2nd | Reference | 1.12 | 0.83 – 1.50 | 0.45 | 0.96 | 0.73 – 1.26 | 0.76 |
| 3rd | Reference | 3.63 | 2.49 – 5.28 | <0.001 | 2.88 | 2.01 – 4.12 | <0.001 |
| 4th | Reference | 26.04 | 12.98 – 52.23 | <0.001 | 16.94 | 8.52 – 33.70 | <0.001 |
| Mortality Risk | |||||||
| Minor | Reference | ||||||
| Moderate | Reference | 1.21 | 0.88 – 1.66 | 0.24 | 1.00 | 0.74 – 1.35 | 0.99 |
| Major | Reference | 1.19 | 0.83 – 1.71 | 0.33 | 0.87 | 0.62 – 1.22 | 0.41 |
| Extreme | Reference | 1.48 | 0.93 – 2.36 | 0.10 | 0.95 | 0.61 – 1.49 | 0.82 |
| Race | |||||||
| White | Reference | ||||||
| Black | Reference | 3.16 | 1.75 – 5.68 | <0.001 | 3.17 | 1.79 – 5.61 | <0.001 |
| Other | Reference | 8.13 | 4.12 – 16.03 | <0.001 | 5.87 | 3.00 – 11.50 | <0.001 |
| Complexity | |||||||
| Pancreas | |||||||
| Minor | Reference | Reference | |||||
| Major | Reference | 0.90 | 0.62 – 1.30 | 0.56 | 1.35 | 0.94 – 1.93 | 0.10 |
| Liver | |||||||
| Minor | Reference | 0.79 | 0.55 – 1.15 | 0.21 | 1.21 | 0.85 – 1.73 | 0.29 |
| Major | Reference | 1.95 | 1.15 – 3.30 | 0.013 | 2.06 | 1.23 – 3.44 | 0.006 |
| Hospital Volume | |||||||
| Low | Reference | Reference | |||||
| Medium | Reference | 1.59 | 0.74 – 3.41 | 0.23 | 3.05 | 1.34 – 6.97 | 0.008 |
| High | Reference | 2.31 | 1.33 – 4.03 | 0.003 | 52.01 | 28.00 – 96.63 | <0.001 |
OR: Odds Ratio CI: Confidence Interval
Factors Associated with Hospital Control Status
Compared with patients who had private insurance, patients with Medicaid had 47% lower odds of undergoing HP surgery at a private investor-owned hospital (OR 0.53, 95% CI 0.38– 0.73) than at a private non-profit hospital. In contrast, patients who were uninsured were 2.2-fold more likely to go to a government funded hospital than a private non-profit hospital (OR 2.19, 95% CI 1.76–2.71). Additionally, patients in the highest income quartile were 34% less likely to have surgery at a government hospital versus private non-profit hospital (OR 0.66, 95% CI 0.59–0.82). Patients undergoing a major hepatectomy were 18% more likely to go to a government hospital versus a private non-profit hospital (OR 1.18, 95% CI 1.02–1.35) (Table 3).
Table 3:
Multivariate associations between insurance status and the hospital control status
| Variable | Private Nonprofit | Government (Nonfederal) | Private Investor–Owned | ||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | P-value | OR | 95% CI | P-value | ||
| Insurance | |||||||
| Private | Reference | ||||||
| Medicare | Reference | 0.94 | 0.85 – 1.03 | 0.18 | 0.85 | 0.72 – 1.01 | 0.06 |
| Medicaid | Reference | 1.12 | 0.97 – 1.29 | 0.11 | 0.53 | 0.38 – 0.73 | <0.001 |
| Uninsured | Reference | 2.19 | 1.77 – 2.71 | <0.001 | 0.58 | 0.32 – 1.06 | 0.07 |
| Gender | |||||||
| Male | Reference | ||||||
| Female | Reference | 1.07 | 0.99 – 1.15 | 0.07 | 0.91 | 0.80 – 1.03 | 0.13 |
| Age | 0.99 | 0.99 – 0.99 | <0.001 | 1.00 | 0.99 – 1.00 | 0.42 | |
| Income quartile | |||||||
| 1st | Reference | ||||||
| 2nd | Reference | 0.85 | 0.76 – 0.94 | 0.002 | 0.86 | 0.72 – 1.03 | 0.10 |
| 3rd | Reference | 0.82 | 0.74 – 0.91 | <0.001 | 0.73 | 0.61 – 0.88 | <0.001 |
| 4th | Reference | 0.66 | 0.59 – 0.73 | <0.001 | 0.48 | 0.40 – 0.58 | <0.001 |
| Mortality Risk | |||||||
| Minor | Reference | ||||||
| Moderate | Reference | 0.95 | 0.87 – 1.03 | 0.22 | 1.29 | 1.08 – 1.53 | 0.004 |
| Major | Reference | 0.85 | 0.76 – 0.95 | 0.003 | 1.74 | 1.44 – 2.11 | <0.001 |
| Extreme | Reference | 0.88 | 0.77 – 1.02 | 0.09 | 2.06 | 1.64 – 2.59 | <0.001 |
| Race | |||||||
| White | Reference | ||||||
| Black | Reference | 1.05 | 0.92 – 1.20 | 0.44 | 1.32 | 1.06 – 1.64 | 0.013 |
| Other | Reference | 1.62 | 1.47 – 1.78 | <0.001 | 1.72 | 1.45 – 2.03 | <0.001 |
| Complexity | |||||||
| Pancreas | |||||||
| Minor | Reference | ||||||
| Major | Reference | 1.05 | 0.93 – 1.19 | 0.46 | 0.86 | 0.70 – 1.04 | 0.12 |
| Liver | |||||||
| Minor | Reference | 1.01 | 0.89 – 1.14 | 0.87 | 0.68 | 0.55 – 0.83 | <0.001 |
| Major | Reference | 1.18 | 1.02 – 1.35 | 0.026 | 0.82 | 0.64 – 1.04 | 0.09 |
| Hospital Volume | |||||||
| Low | Reference | Reference | |||||
| Medium | Reference | 0.97 | 0.45 – 2.09 | 0.93 | 0.63 | 0.33 – 1.20 | 0.16 |
| High | Reference | 1.43 | 0.80 – 2.58 | 0.23 | 0.23 | 0.14 – 0.37 | <0.001 |
OR: Odds Ratio CI: Confidence Interval
Impact of Hospital Charges across different hospital locations and teaching status
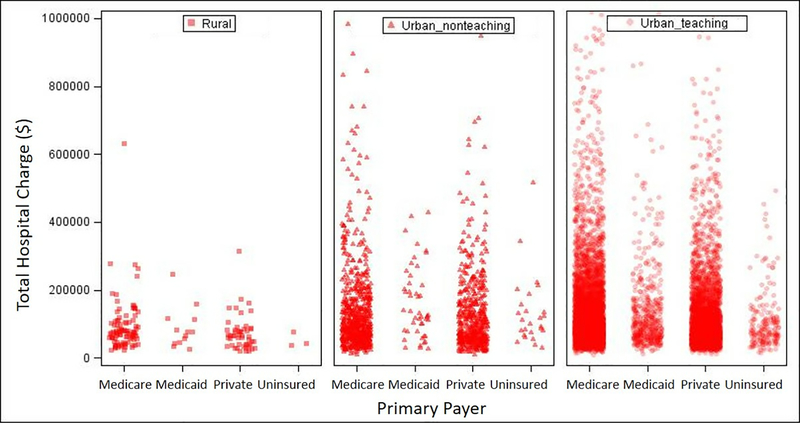
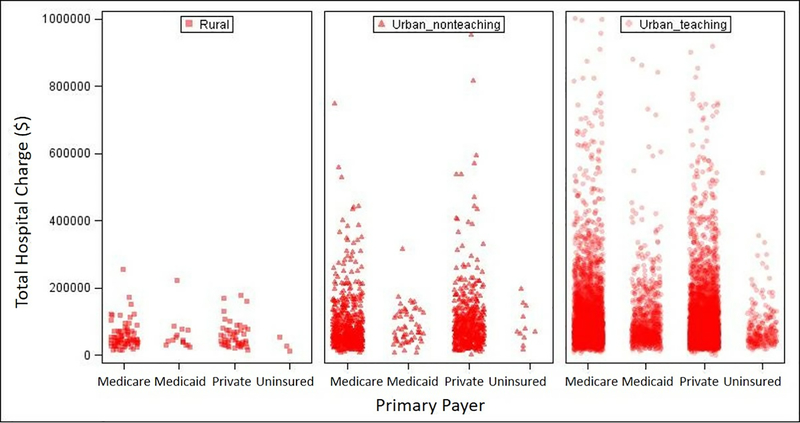
Overall, hospital charges for patients undergoing pancreatic surgery were higher than charges among patients undergoing liver surgery, irrespective of insurance status and hospital location (Figure 1 and 2). In addition, rural hospitals had lower median charges compared with hospital charges at urban teaching and non-teaching hospitals (Rural: $60,052; IQR $38,066 - $84,022, Urban non-teaching: $83,092, IQR $51,914 - $143,278; Urban teaching: $82,444, IQR $55,189 - $134,387 p<0.001). Among patients undergoing pancreatic surgery, hospital charges for patients with Medicaid were higher at urban non-teaching hospitals versus charges at urban teaching hospitals and rural hospitals (Rural: $76,138; IQR $44,983-$112,728; Urban non-teaching: $127,754; IQR $80,477-$220,428; Urban teaching: $98,932, IQR $ 63,376-$162,866 p=0.013). Similar trends were observed for uninsured patients undergoing pancreatic surgery at different hospital locations (Rural: $44,054, IQR $36,809 - $75,568; Urban non-teaching: $107,061, IQR $77,173 - $158,939; Urban teaching: $80,441, IQR $54,512 - $118,312, p=0.029). Conversely, among patients undergoing hepatic surgery, hospital charges for patients insured by Medicaid were comparable at urban non-teaching and urban teaching hospitals (Urban non-teaching: $69,333, IQR $46,742 - $127,978; Urban teaching: $74,364, IQR $49,672 - $123,718 p=0.614). Moreover, irrespective of the insurance status, private investor-owned hospitals had higher charges compared with government and non-profit hospitals.
Figure 1.
Hospital charges stratified by insurance status and hospital location / teaching status among patients undergoing pancreatic surgery.
Figure 2.
Hospital charges stratified by insurance status and hospital location / teaching status among patients undergoing hepatic surgery
DISCUSSION
Disparities in access to different treatments and hospital based services can lead to differences in clinical outcomes among cancer patients.[25, 29, 30] As such, understanding the factors that mediate disparities in access to high-quality care among patients undergoing surgery is an important topic for investigation.[31] To date, most studies that have examined health care disparities have focused on factors such as sex, race, geographical location, and socioeconomic status. [32, 33] Fewer studies have specifically reported on the role of insurance status relative to health care outcomes.[34] Specifically, while several studies have investigated the role of insurance status among patients undergoing HP surgery, these reports have largely focused on differences in perioperative outcomes among patients already admitted to a certain type of hospital (e.g. urban, teaching, not-for-profit, etc.).[24, 35] While informative, such data do not provide insight into the “up-stream” process regarding what factors may have impacted how patients actually end up at a specific hospital. The current study was important because it demonstrated that insurance status was an important factor driving where cancer patients underwent HP procedures. Specifically, patients with Medicaid and uninsured individuals were more likely to undergo surgery for HP cancers at rural hospitals, and less likely to undergo surgery at teaching hospitals compared with patients who had private insurance. In addition, Medicaid patients were less likely to undergo surgery at private investor-owned hospitals than at private non-profit hospitals. In contrast, patients who were insured were more likely to receive surgical care at private hospitals and urban teaching centers. Collectively the data demonstrated that patients insured by Medicaid and uninsured patients were much more likely to undergo surgery at hospitals often associated with worse outcomes.
The specific type of hospital (i.e. rural vs. urban, teaching vs. non-teaching) where patients receive care can drive outcomes for patients with a variety of different cancers.[18, 36–38] Christopher et al. reported that patients who underwent surgery for colorectal cancer at hospitals in rural areas had worse outcomes versus individuals who had surgery in metropolitan areas.[39] In a separate study, Burke et al. noted that major teaching hospital status was associated with lower mortality rates compared with nonteaching hospitals.[40] In a separate study, Hyder et al. reported that, even among high-volume hospitals, patients undergoing complex HP procedures had better outcomes at teaching versus non-teaching hospitals. [41] While the reason for these hospital-based differences is likely multifactorial, management of HP cancer patients often requires a complex multidisciplinary decision-making process with the use of multimodality therapy including surgical resection, chemotherapy, radiotherapy, and interventional radiology.[42] Such complex care is typically provided best at specialized, high-volume academic centers, which are often located in urban settings.[37] Given the well-established relationship between hospital characteristics, such as operative volume and teaching status with improved outcomes among patients with cancer, there have been increased efforts by policymakers and hospital administrators within the United States to promote regionalization of care for complex surgical conditions.[14, 43, 44] [45, 46] The relative impact of insurance status on regionalization of care to major, urban teaching hospitals has not, however, been well-studied. In the current study, compared with privately insured patients, individuals who were insured by Medicaid were at a markedly decreased odds of undergoing surgery for HP cancers at urban non-teaching (OR 0.36) and urban teaching hospitals (OR 0.54). Importantly, insurance status remained strongly associated with hospital type even after controlling for multiple competing factors such as race and income.
Insurance status may be an important factor driving disparities in the treatment and outcomes of patients with cancers. Abraham et al. reported that lack of private insurance coverage was associated with a lower likelihood of presenting with resectable disease at the time of diagnosis.[23] Visser et al. similarly noted that type of insurance coverage was associated with variations in receipt of care in accordance with standard treatment guidelines for pancreatic cancer.[47] In a separate study, Zak et al. reported that patients with resectable primary liver cancer were at a 3-fold higher chance of undergoing resection if the patient had private insurance compared with being uninsured.[48] While these data suggested that insurance status was associated with variations in receipt of treatment, the impact of insurance status and hospital type to mediate this effect had not been examined. In the current study, we noted that type of insurance coverage was an important determinant of access to different hospital settings. Specifically, insurance-related differences translated into access to hospital types that were variable. Data from the current study highlight that differences in outcomes among patients with variable insurance status may at least in part be mediated through disparate access to hospitals.
Another interesting finding was the variation in hospital ownership status noted among privately insured versus Medicaid patients treated for HP cancers. Perhaps not surprisingly, Medicare patients were 47% less likely to undergo surgical treatment for HP cancers at a private investor-owned hospital than at non-profit organizations. In addition, uninsured patients had 2.2-fold higher odds of undergoing surgery at government hospitals. In a study of the National Cancer Database, Bilimoria et al. noted that only 12% of the Commission on Cancer (CoC) approved hospitals were government hospitals, and less than 4% were located in small rural areas or were rural referral centers.[49] Similarly, Gupta et al. reported patients with head and neck cancers patients with Medicaid, Medicare, or uninsured patients were less likely to undergo surgery at teaching hospitals and more likely to seek care at urban nonteaching, rural, private for-profit, and government hospitals compared with patients who had private insurance.[31] Collectively, the data suggests that patients who were uninsured or underinsured – such as those insured by Medicaid - were not generally within referral patterns to high volume, academic centers. In addition, hospital charges also differed widely based on insurance and teaching status of the hospital (Figure 1 and 2). Differences in hospital charges and reimbursement patterns relative to primary payer may be related to insurance acceptance policies among different hospital settings, which might further complicate equitable access to high quality care for all patients with HP cancers.
There were several limitations that should be considered when analyzing the results of the current study. As with any study utilizing administrative databases, the results may have been affected by coding accuracy.[50] We were also not able to account for repeat visits among patients since NIS reports data from each index hospitalization separately. This limitation prevented us from accounting for clustering effects related to visits by the same patient, as well as the ability to assess whether the choice of hospital or insurance type changed with subsequent visits. Moreover, the introduction of the Affordable Care Act may have expanded cancer coverage and improved access to high-volume institutions for uninsured patients. In addition, the current study could not account for individual patient decision making regarding their choice of treatment setting. In addition, information regarding tumor characteristics (i.e. size, number, stage of tumor, chemoradiotherapy) are not captured in NIS dataset.
In conclusion, regardless of age, race, income and complexity of surgery, insurance status was strongly associated with the type of hospital in which patients underwent surgery for HP cancers. Specifically, patients with government insurance undergoing surgery for HP cancer were less likely to seek care at urban nonteaching, urban teaching and private investor-owned hospitals, while uninsured patients were more likely to undergo care at government hospitals. In light of poor outcomes associated with certain hospital settings among patients undergoing HP surgery, the results from the current study suggest that insurance-related disparities may contribute to differences in access to high-quality hospitals. Addressing the reasons for inequitable access to different hospital settings relative to insurance status is essential to ensure that all patients undergoing pancreatic or liver surgery receive high quality surgical care. Following evidence collection, next steps should be to further implement health policies to bridge the gap between insurance types and access to different hospital settings. Further studies are necessary to promote health policies that identify interventions to promote equitability to approach optimal hospital settings for patients, irrespective of their insurance type.
Footnotes
Conflict of Interest: All authors declare that they have no disclosures to report.
REFERENCES
- 1.Smedley BD, Stith AY, Nelson AR: Institute of Medicine Committee on, Understanding Eliminating, Racial Ethnic Disparities in Health, Care. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care 2003. [PubMed] [Google Scholar]
- 2.Sommers BD, Mc MC, Blendon RJ, Benson JM, Sayde JM: Beyond Health Insurance: Remaining Disparities in US Health Care in the Post-ACA Era. The Milbank quarterly 2017, 95(1):43–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frieden TR, Centers for Disease C, Prevention: CDC Health Disparities and Inequalities Report - United States, 2013. Foreword. MMWR Suppl 2013, 62(3):1–2. [PubMed] [Google Scholar]
- 4.Niu X, Roche LM, Pawlish KS, Henry KA: Cancer survival disparities by health insurance status. Cancer medicine 2013, 2(3):403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosenberg AR, Kroon L, Chen L, Li CI, Jones B: Insurance status and risk of cancer mortality among adolescents and young adults. Cancer 2015, 121(8):1279–1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roetzheim RG, Pal N, Gonzalez EC, Ferrante JM, Van Durme DJ, Krischer JP: Effects of health insurance and race on colorectal cancer treatments and outcomes. American journal of public health 2000, 90(11):1746–1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen AY, Schrag NM, Halpern M, Stewart A, Ward EM: Health insurance and stage at diagnosis of laryngeal cancer: does insurance type predict stage at diagnosis? Archives of otolaryngology--head & neck surgery 2007, 133(8):784–790. [DOI] [PubMed] [Google Scholar]
- 8.Chen AY, Schrag NM, Halpern MT, Ward EM: The impact of health insurance status on stage at diagnosis of oropharyngeal cancer. Cancer 2007, 110(2):395–402. [DOI] [PubMed] [Google Scholar]
- 9.Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM: Unmet health needs of uninsured adults in the United States. Jama 2000, 284(16):2061–2069. [DOI] [PubMed] [Google Scholar]
- 10.Lillie-Blanton M, Hoffman C: The role of health insurance coverage in reducing racial/ethnic disparities in health care. Health affairs (Project Hope) 2005, 24(2):398–408. [DOI] [PubMed] [Google Scholar]
- 11.Armenia SJ, Pentakota SR, Merchant AM: Socioeconomic factors and mortality in emergency general surgery: trends over a 20-year period. J Surg Res 2017, 212:178–186. [DOI] [PubMed] [Google Scholar]
- 12.Ho VP, Nash GM, Feldman EN, Trencheva K, Milsom JW, Lee SW: Insurance But Not Race Is Associated With Diverticulitis Mortality in a Statewide Database. 2011, 54(5):559–565. [DOI] [PubMed] [Google Scholar]
- 13.Cohen RA MM: Health insurance coverage: Early release of estimates from the National Health Interview Survey, 2014. National Center for Health Statistics; June, 2015. [Google Scholar]
- 14.Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, Welch HG, Wennberg DE: Hospital volume and surgical mortality in the United States. N Engl J Med 2002, 346(15):1128–1137. [DOI] [PubMed] [Google Scholar]
- 15.Ghaferi AA, Birkmeyer JD, Dimick JB: Variation in hospital mortality associated with inpatient surgery. N Engl J Med 2009, 361(14):1368–1375. [DOI] [PubMed] [Google Scholar]
- 16.Merath K, Bagante F, Chen Q, Beal EW, Akgul O, Idrees J, Dillhoff M, Cloyd J, Schmidt C, Pawlik TM: The Impact of Discharge Timing on Readmission Following Hepatopancreatobiliary Surgery: a Nationwide Readmission Database Analysis. J Gastrointest Surg 2018. [DOI] [PubMed] [Google Scholar]
- 17.Merath K, Chen Q, Bagante F, Sun S, Akgul O, Idrees JJ, Dillhoff M, Schmidt C, Cloyd J, Pawlik TM: Variation in the cost-of-rescue among medicare patients with complications following hepatopancreatic surgery. HPB (Oxford) 2018. [DOI] [PubMed] [Google Scholar]
- 18.Sheetz KH, Dimick JB, Ghaferi AA: Impact of Hospital Characteristics on Failure to Rescue Following Major Surgery. Ann Surg 2016, 263(4):692–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amini N, Kim Y, Hyder O, Spolverato G, Wu CL, Page AJ, Pawlik TM: A nationwide analysis of the use and outcomes of perioperative epidural analgesia in patients undergoing hepatic and pancreatic surgery. Am J Surg 2015, 210(3):483–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cerullo M, Gani F, Chen SY, Canner JK, Dillhoff M, Cloyd J, Pawlik TM: Routine intensive care unit admission among patients undergoing major pancreatic surgery for cancer: No effect on failure to rescue. Surgery 2018. [DOI] [PubMed] [Google Scholar]
- 21.Kneuertz PJ, Pitt HA, Bilimoria KY, Smiley JP, Cohen ME, Ko CY, Pawlik TM: Risk of morbidity and mortality following hepato-pancreato-biliary surgery. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 2012, 16(9):1727–1735. [DOI] [PubMed] [Google Scholar]
- 22.Merath K, Chen Q, Johnson M, Mehta R, Beal EW, Dillhoff M, Cloyd J, Pawlik TM: Hot spotting surgical patients undergoing hepatopancreatic procedures. HPB : the official journal of the International Hepato Pancreato Biliary Association 2018. [DOI] [PubMed] [Google Scholar]
- 23.Abraham A, Al-Refaie WB, Parsons HM, Dudeja V, Vickers SM, Habermann EB: Disparities in pancreas cancer care. Annals of surgical oncology 2013, 20(6):2078–2087. [DOI] [PubMed] [Google Scholar]
- 24.Hoehn RS, Hanseman DJ, Jernigan PL, Wima K, Ertel AE, Abbott DE, Shah SA: Disparities in care for patients with curable hepatocellular carcinoma. HPB : the official journal of the International Hepato Pancreato Biliary Association 2015, 17(9):747–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nathan H, Frederick W, Choti MA, Schulick RD, Pawlik TM: Racial disparity in surgical mortality after major hepatectomy. Journal of the American College of Surgeons 2008, 207(3):312–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schneider EB, Ejaz A, Spolverato G, Hirose K, Makary MA, Wolfgang CL, Ahuja N, Weiss M, Pawlik TM: Hospital volume and patient outcomes in hepato-pancreatico-biliary surgery: is assessing differences in mortality enough? Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 2014, 18(12):2105–2115. [DOI] [PubMed] [Google Scholar]
- 27.NIS Description of Data Elements [https://www.hcup-us.ahrq.gov/db/vars/aprdrg_risk_mortality/nisnote.jsp accessed 2nd May, 2019.]
- 28.Baram D, Daroowalla F, Garcia R, Zhang G, Chen JJ, Healy E, Riaz SA, Richman P: Use of the All Patient Refined-Diagnosis Related Group (APR-DRG) Risk of Mortality Score as a Severity Adjustor in the Medical ICU. Clinical medicine Circulatory, respiratory and pulmonary medicine 2008, 2:19–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Swords DS, Mulvihill SJ, Brooke BS, Skarda DE, Firpo MA, Scaife CL: Disparities in utilization of treatment for clinical stage I-II pancreatic adenocarcinoma by area socioeconomic status and race/ethnicity. Surgery 2018. [DOI] [PubMed] [Google Scholar]
- 30.Wasif N, Etzioni D, Habermann EB, Mathur A, Pockaj BA, Gray RJ, Chang YH: Racial and Socioeconomic Differences in the Use of High-Volume Commission on Cancer-Accredited Hospitals for Cancer Surgery in the United States. Annals of surgical oncology 2018, 25(5):1116–1125. [DOI] [PubMed] [Google Scholar]
- 31.Gupta A, Sonis ST, Schneider EB, Villa A: Impact of the insurance type of head and neck cancer patients on their hospitalization utilization patterns. Cancer 2018, 124(4):760–768. [DOI] [PubMed] [Google Scholar]
- 32.Okunrintemi V, Khera R, Spatz ES, Salami JA, Valero-Elizondo J, Warraich HJ, Virani SS, Blankstein R, Blaha MJ, Pawlik TM et al. : Association of Income Disparities with Patient-Reported Healthcare Experience. J Gen Intern Med 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schneider EB, Calkins KL, Weiss MJ, Herman JM, Wolfgang CL, Makary MA, Ahuja N, Haider AH, Pawlik TM: Race-based differences in length of stay among patients undergoing pancreatoduodenectomy. Surgery 2014, 156(3):528–537. [DOI] [PubMed] [Google Scholar]
- 34.Sedney CL, Khan U, Dekeseredy P: Traumatic spinal cord injury in West Virginia: Disparities by insurance and discharge disposition from an acute care hospital. J Spinal Cord Med 2018:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schwartz DA, Hui X, Schneider EB, Ali MT, Canner JK, Leeper WR, Efron DT, Haut E, Velopulos CG, Pawlik TM et al. : Worse outcomes among uninsured general surgery patients: does the need for an emergency operation explain these disparities? Surgery 2014, 156(2):345–351. [DOI] [PubMed] [Google Scholar]
- 36.Bhattacharyya N, Abemayor E: Patterns of hospital utilization for head and neck cancer care: changing demographics. JAMA otolaryngology-- head & neck surgery 2015, 141(4):307–312; quiz 400. [DOI] [PubMed] [Google Scholar]
- 37.Dimick JB, Cowan JA, Colletti LM, Upchurch GR: Hospital teaching status and outcomes of complex surgical procedures in the United States. Arch Surg 2004, 139(2):137–141. [DOI] [PubMed] [Google Scholar]
- 38.Gruber K, Soliman AS, Schmid K, Rettig B, Ryan J, Watanabe-Galloway S: Disparities in the Utilization of Laparoscopic Surgery for Colon Cancer in Rural Nebraska: A Call for Placement and Training of Rural General Surgeons. J Rural Health 2015, 31(4):392–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hocking C, Broadbridge VT, Karapetis C, Beeke C, Padbury R, Maddern GJ, Roder DM, Price TJ: Equivalence of outcomes for rural and metropolitan patients with metastatic colorectal cancer in South Australia. The Medical journal of Australia 2014, 201(8):462–466. [DOI] [PubMed] [Google Scholar]
- 40.Avall Lundqvist E, Nordstrom L, Sjovall K, Eneroth P: Evaluation of seven different tumour markers for the establishment of tumour marker panels in gynecologic malignancies. European journal of gynaecological oncology 1989, 10(6):395–405. [PubMed] [Google Scholar]
- 41.Hyder O, Sachs T, Ejaz A, Spolverato G, Pawlik TM: Impact of hospital teaching status on length of stay and mortality among patients undergoing complex hepatopancreaticobiliary surgery in the USA. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 2013, 17(12):2114–2122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nathan H, de Jong MC, Pulitano C, Ribero D, Strub J, Mentha G, Gigot JF, Schulick RD, Choti MA, Aldrighetti L et al. : Conditional survival after surgical resection of colorectal liver metastasis: an international multi-institutional analysis of 949 patients. Journal of the American College of Surgeons 2010, 210(5):755–764, 764–756. [DOI] [PubMed] [Google Scholar]
- 43.Finks JF, Osborne NH, Birkmeyer JD: Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med 2011, 364(22):2128–2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Idrees JJ, Merath K, Gani F, Bagante F, Mehta R, Beal E, Cloyd JM, Pawlik TM: Trends in centralization of surgical care and compliance with National Cancer Center Network guidelines for resected cholangiocarcinoma. HPB : the official journal of the International Hepato Pancreato Biliary Association 2018. [DOI] [PubMed] [Google Scholar]
- 45.Harrington C, Woolhandler S, Mullan J, Carrillo H, Himmelstein DU: Does investor ownership of nursing homes compromise the quality of care? American journal of public health 2001, 91(9):1452–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Amini A, Jones BL, Ghosh D, Schefter TE, Goodman KA: Impact of facility volume on outcomes in patients with squamous cell carcinoma of the anal canal: Analysis of the National Cancer Data Base. Cancer 2017, 123(2):228–236. [DOI] [PubMed] [Google Scholar]
- 47.Visser BC, Ma Y, Zak Y, Poultsides GA, Norton JA, Rhoads KF: Failure to comply with NCCN guidelines for the management of pancreatic cancer compromises outcomes. HPB (Oxford) 2012, 14(8):539–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zak Y, Rhoads KF, Visser BC: Predictors of surgical intervention for hepatocellular carcinoma: race, socioeconomic status, and hospital type. Archives of surgery (Chicago, Ill : 1960) 2011, 146(7):778–784. [DOI] [PubMed] [Google Scholar]
- 49.Bilimoria KY, Bentrem DJ, Stewart AK, Winchester DP, Ko CY: Comparison of commission on cancer-approved and -nonapproved hospitals in the United States: implications for studies that use the National Cancer Data Base. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 2009, 27(25):4177–4181. [DOI] [PubMed] [Google Scholar]
- 50.Haut ER, Pronovost PJ, Schneider EB: Limitations of Administrative Databases. Jama 2012, 307(24):2589–2590. [DOI] [PubMed] [Google Scholar]