ABSTRACT
Older adults share a disproportionately high burden of vaccine-preventable diseases. Despite recommendations from national and international health organizations, vaccination rates among older patients remain suboptimal, suggesting poor access and barriers to vaccination. Pharmacists are uniquely positioned to assist patients in overcoming many of these barriers. In this commentary, we describe some of the common barriers to vaccination that older adults encounter and the role pharmacists have in overcoming these barriers, in the US and abroad. We provide a case study of pharmacists’ impact in supporting herpes zoster vaccination. We also identify areas of opportunities to promote further pharmacist involvement in vaccination efforts.
KEYWORDS: Pharmacist, pharmacy, vaccine, immunization, herpes zoster, shingles, elderly, barriers, access
Introduction – vaccinations for older adults
The World Health Organization (WHO) has listed vaccine hesitancy – the reluctance or refusal to vaccinate despite the availability of vaccines – in the top 10 threats to global health.1 Although vaccines save millions of lives every year and are one of the most cost-effective interventions in public health, many adults remain unvaccinated.2 The economic burden of vaccine-preventable diseases among United States (US) adults is significant, estimated at $9 billion annually.3 Nearly $4.8 billion (53%) of this annual economic burden of vaccine-preventable diseases are placed on adults 65+, and another $2 billion (23%) among adults 50–64.3
The elderly face a disproportionately large burden of vaccine-preventable diseases and should obtain additional vaccination.4 The Advisory Committee on Immunization Practices (ACIP) recommends that older adults be vaccinated with any licensed influenza vaccine annually, tetanus-diphtheria-acellular pertussis (Tdap) or tetanus-diphtheria (Td) vaccine every 10 years, herpes zoster (HZ) vaccine starting at age 50, and pneumococcal vaccine starting at age 65 or earlier for certain indications.5 Other recommended vaccinations for at-risk older adults include hepatitis A and B, Meningococcal, and haemophilus influenza type b (Hib).5
The Healthy People 2020 objectives outlined by the US Department of Health and Human Services (DHHS) set the following vaccination coverage goals for adults: 70% for influenza vaccination for adults 18+, 90% for pneumococcal vaccination for adults 65+, and 30% for herpes zoster (HZ) vaccination for adults 60+.6 Despite these goals and efforts to improve vaccination coverage, vaccination for older adults continue to fall short. The latest available vaccination coverage rates report 2017 coverage of 45.4% for influenza vaccination among adults 19+ and 69.0% for the pneumococcal vaccine for adults 65+.7 HZ vaccination coverage at 34.9% among adults aged 60+ met this target in 2017.
To understand why vaccination coverage for older adults remains low, many potential barriers and determinants of vaccination have been identified. For example, research studies have identified physical determinants (e.g. drug consumption, body-mass-index, physical activity), context determinants (e.g. access, cues to action), sociodemographic determinants (e.g. gender, age, living arrangements) and psychological determinants (e.g. utility, past behavior, experience, knowledge, attitude, subjective norms, and perceived behavioral control).8 The WHO Strategic Advisory Group of Experts working group grouped these into 3Cs of vaccine hesitancy: convenience [do not have access], confidence [do not trust the vaccine or provider], and complacency [do not perceive a need or value for the vaccine].9 Older adults, in particular, may be deterred by barriers to vaccination as they tend to face significant barriers to health-care access.4,10
Pharmacists are in a unique position to improve vaccination access and uptake in older adults. In this commentary, we discuss some of the common barriers to vaccination by older adults using the 3C framework and the role that pharmacists have in overcoming these barriers. We also provide an overview of the role of pharmacists in vaccination globally and offer a descriptive case example of pharmacists’ impact in the context of HZ vaccination. Given adults aged 65+ will represent 27% of the world’s population by 2050, it is critical to adopt strategies to overcome barriers to vaccination for older adults.4
The role of pharmacists in addressing barriers to vaccination
In the US, pharmacists are authorized to administer vaccines in all 50 states, the District of Columbia and Puerto Rico.11 Pharmacists’ role in immunization is largely guided by state-level authorizations. State laws and regulations, typically as part of a pharmacy practice act, determine which vaccine a pharmacist may administer, and to whom (e.g. adults, minors). The trend has been for states to grant greater latitude to pharmacists in prescribing and autonomously administering vaccinations. As of January 2019, pharmacists have been authorized to administer any vaccines in 46 states and some vaccines in four states (New Hampshire, New York, West Virginia, Wyoming).11 For adults, pharmacists have the authority to administer the influenza vaccine, pneumococcal vaccine, HZ vaccine, Td/Tdap, and meningococcal vaccine in all states and jurisdictions, and the hepatitis B vaccine in 49 states, excluding New York.11
Research studies have examined the impact that authorizing pharmacist-based vaccine administration may have on influenza, pneumococcal and HZ vaccination rates.12–14 All studies found significant gains in vaccination coverage when states granted greater authorization for pharmacists to administer vaccinations. Pharmacists improve vaccination coverage by addressing each of the following barriers to vaccination.
Convenience
Pharmacists are one of the most accessible health-care professionals to patients. There are over 67,000 pharmacies in the US, with retail chain and independent pharmacies accounting for 40% and 35% of all pharmacies, respectively.15 More than 90% of Americans live within 2 miles of a pharmacy.15 In 2018, 4 billion prescriptions, or 11.6 prescriptions per-capita, were filled at community pharmacies in the US.16 Pharmacies typically have consistent and longer hours of operation and are open on weekends, as opposed to physician offices with limited hours and availability.17 Research suggests that patients see a pharmacist significantly more throughout the year than their primary care provider, possibly up to 10 times as frequently.18 This is corroborated by evidence from the Medical Expenditures Panel Survey (MEPS), which found that there were over 31 prescription purchases including refills in a 12-month period for adults aged 65–74,19 as compared to approximately five physician office visits on average per year.20
The Centers for Disease Control and Prevention (CDC) and the National Vaccine Advisory Committee (NVAC) promote the recommendation and integration of vaccination in routine care and have identified pharmacists as an integral part of improving vaccination rates.5,21 Although the majority of primary care providers adhere to the ACIP guidelines on recommending vaccination, many primary care providers do not consistently stock vaccines in their offices.22 Thus, administering recommended vaccines during physician office visits is often not feasible.23 Pharmacists, who nearly always stock commonly administered vaccines and frequently stock less commonly administered vaccines,22,24 are well positioned to be at the forefront of vaccination for older adults by facilitating greater convenience and access to vaccines, particularly in rural regions.25 Surveys have found that the majority of Americans prefer visiting their local pharmacy for vaccinations as opposed to visiting the doctor’s office, primarily due to convenience.26 Convenience was found to be a major factor in vaccination decisions of adult prescription recipients.27
Research studies have found that the probability of becoming vaccinated is associated with the frequency of walking by or in a vaccinating clinic.28 Frequent contact with a pharmacist, as is the case for the many older adults who take medications for chronic conditions, presents an unparalleled opportunity to improve vaccination rates.
Confidence
Pharmacists are rated as one of the most trusted professionals in the US, consistently ranked in the top three along with nurses and medical doctors.29 Pharmacists have also been ranked the second most highly trusted health-care professional to deliver vaccinations after physicians.17 Pharmacy-based immunization services have become widely accepted by both patients and pharmacy staff, where most US patients feel comfortable with pharmacists delivering vaccinations in pharmacies.17 Research has found that older adults trust doctors and pharmacists much more than other sources to provide information on prescription drugs.30 Trust in pharmacists is important in building people’s confidence in pharmacists’ reliability and competence to provide information about and deliver vaccination.
As educators and promoters, pharmacists can improve vaccination coverage by increasing people’s confidence in vaccines.31 Pharmacists maintain vaccine competency through mandatory continuing education and are thus well equipped to address patient questions and concerns about vaccine indications, efficacy, and safety. This is important as nearly 4 out of 5 patients report that they are more likely to vaccinate if it is recommended by a health-care professional, including pharmacists.26 Implementation and expansion of immunization programs in community pharmacies have generally increased the number of vaccinations administered.17
Complacency
The level of familiarity that older adults have with vaccines and vaccination guidelines is variable. Based on a national survey, older adults tended to be aware of vaccinations for influenza (97%), pneumococcal (87%), and Td/Tdap (87%); however, awareness of vaccinations for HZ (73%) and hepatitis B (59%) was lower.32 Some research suggests that physicians are also not prioritizing all vaccinations. Hurley et al. found that for a hypothetical adult patient aged 67, physicians prioritized certain vaccines, such as Tdap and HZ, well-below other preventive services as recommended by the US Preventive Services Task Force.23
Pharmacists have a significant opportunity to fill this awareness gap and reduce complacency. The American Society of Health-System Pharmacists (ASHP) lists multiple educational and promotional activities beyond vaccine administration that pharmacists engage in to improve vaccination rates: 1) examining the patient history and screening for immunization needs; 2) patient counseling and education on the guidelines, recommendations, and safety of vaccination; 3) formulary management to ensure that a sufficient stock of vaccines is available for the patient population served; 4) promoting organizational vaccine initiatives through administrative measures; and 5) public education through community outreach.33 The American Pharmacists Association (APhA) encourages pharmacists to serve as an advocate for vaccines, to facilitate the provision of immunization services in their practices, and, where permitted by state law, to administer vaccines to eligible patients.34
Role of pharmacists in vaccination worldwide
Globally, the role of pharmacists in vaccination varies widely from little to broad involvement.35 The US is part of the leading group of countries (e.g. Argentina, Australia, Philippines, South Africa, and the United Kingdom) that have legally authorized vaccination by pharmacists or in pharmacies. These countries have gradually provided the legal authority for pharmacists to perform immunization activities, as the benefits of having pharmacists involved as educators, facilitators, and immunizers have grown in appreciation in these countries. Pharmacists may be empowered to manage patients’ vaccination schedules and organize vaccination activities and campaigns. However, pharmacists may still not be allowed to provide certain vaccines or administer immunization to certain populations (e.g. children).36 In some settings, pharmacists may require other health-care providers to administer vaccines in pharmacies.35
In low- and middle-income countries, pharmacists may not be involved at all in the national expanded program on immunization (EPI), or may only be minimally involved in ensuring safe supply and dispensing of vaccines, as well as advocating for immunization.37 In some countries, retail drug shops may sell and administer vaccines even if national regulations may not allow the administration of vaccines by pharmacists.38 One of the key reported steps to greater pharmacist involvement in low- and middle-income countries is introducing immunization training in pharmacists’ curriculum such that pharmacists could be involved in immunization education, counseling, vaccine adverse event reporting and advocacy to patients.39 Few research articles discuss pharmacist involvement in immunization services in developing countries, where greater evidence should be generated to demonstrate the benefits of pharmacists’ involvement in vaccination worldwide.
The case of Herpes zoster
Herpes zoster, also known as shingles, is an infection that occurs when the varicella zoster (chickenpox) virus reactivates, causing a painful rash.40 Although cases of HZ sometimes occur in younger adults, older adults face the majority of the disease burden. Approximately 30% of Americans become infected with HZ at some point during their lifetime.40 Beyond the pain experienced during active infection, complications called post-herpetic neuralgia may result where patients experience persistent or recurrent debilitating pain. In June 2008, ACIP recommended that all persons 60+ be vaccinated with the zoster vaccine (ZVL, Zostavax®).40 Zostavax is a live vaccine (i.e. uses a weakened attenuated virus), given as a single injection, which can offer protection against HZ for about 5 years. ACIP updated these recommendations in 2018 to preferentially recommend another vaccine option when the Food and Drug Administration (FDA) approved the recombinant zoster vaccine (RZV, Shingrix®) for people aged 50+. Shingrix is an inactivated vaccine made of a virus component and is given in two doses, offering protection against shingles beyond 5 years.
Although the Healthy People 2020 goals of reaching 30% HZ vaccination coverage have been met, vaccination coverage for HZ is considerably lower than other commonly recommended vaccines for older adults.41 This may be due in part to the low availability of the vaccine in physician offices, the large burden of cost-sharing borne by patients, and low perceived severity as compared to pneumococcal or influenza infections.
HZ vaccination by pharmacists
All US states currently allow pharmacists to administer the HZ vaccine under full prescriptive authority or under a broad, non-patient-specific protocol.11 This is an increase from the 39 states that authorized this practice in 2014.14 The authorization of HZ vaccination without a prescription order has been associated with 2–3% absolute increase in vaccination coverage across the population.13,14 As more states have begun to allow pharmacists to administer the HZ vaccine without a patient-specific prescription, states’ pharmacy associations, board of pharmacy, and departments of health need to collaborate to develop state-specific protocols.33
Over 91% of pharmacies in the US carry the HZ vaccine.22 In comparison, research studies have found that only half of the physician offices that routinely recommend HZ vaccinations stock the vaccine.22 Further, difficulties with Medicare Part D billing for HZ vaccination in physician offices have positioned pharmacies to offer the service more easily. Vaccine availability and insurance payments have together rendered pharmacies to be the best access points for HZ vaccination.
At the pharmacy, pharmacists can improve the uptake of the HZ vaccine by improving awareness of vaccination needs. Studies examining the effect of immunization recommendations on vaccine uptake in pharmacist-led wellness visits found that 42% of patients accepted pharmacists’ recommendation to receive the HZ vaccine, a similar rate to the 50% for influenza and pneumococcal vaccination.42 By leveraging state immunization registries, community pharmacists have also been able to effectively screen adults requesting influenza vaccination for other immunization needs, increasing administered HZ vaccinations by 12%.43
Educational outreach by pharmacists has also been effective in improving HZ vaccination in older adults. Patients have reported being educated about the HZ vaccine at much higher rates by pharmacists as compared to other sources, resulting in more HZ vaccinations.44 Another research study on pharmacist-led educational outreach via electronic medical record messages and postal messages found a 2.7–2.9 fold increase in HZ vaccination rates.45 Similarly, automated telephone messages sent by community pharmacies were associated with a 2% relative increase in the number of patients receiving HZ vaccinations as compared to a control group.46
Areas of opportunity
While US pharmacists have demonstrated their role in improving vaccination coverage by addressing various barriers to vaccination, there are additional challenges and opportunities that could further increase their effectiveness. For example, not all currently practicing US pharmacists are trained to be vaccinators.17 While all accredited PharmD programs are required to train students as vaccinators, immunization training has lagged behind among non-junior pharmacists. This has resulted in geographic and socioeconomic disparities in vaccine access for pharmacist-based immunization services.17 Since immunization training is associated with increased uptake of pharmacists and pharmacy technicians participating in immunizing activities, additional training would improve patient access to vaccinations.17,47
Although pharmacists currently stock and administer many of the common vaccines, there is potential for expanding this further. One study across eight states found that HZ, influenza, pneumococcal, and Tdap vaccines were available at nearly 100% of the studied pharmacies, while the availability of other vaccines, such as hepatitis A, hepatitis B, human papillomavirus (HPV), and travel vaccinations, was much lower.24 Pharmacists cite authorization to administer these vaccines as a major barrier to carrying them.24 State authorization would allow pharmacists to engage in a greater role in preventing the spread of infectious diseases. Further, timely pharmacist access to immunization information systems (IIS) is essential for pharmacists to conduct patient assessment and report immunizations provided.34
Pharmacies in the US report reimbursement and insurance coverage to be a major barrier to vaccine administration.24 High levels of cost-sharing deter patients from vaccination and stymie pharmacists’ efforts to improve vaccination coverage. To ensure patients are able to receive the vaccine when offered by the pharmacist, patient out-of-pocket expenditures need to be minimized. Other significant barriers to vaccine administration reported by pharmacists include time constraints and external factors affecting the supply of vaccines.24
Even after adjusting for factors typically associated with vaccination uptake such as demographic characteristics and general accessibility to the health-care system, studies have found that there is significant heterogeneity in vaccination rates across states. For example, state-level data reveal large differences in HZ vaccination rates among adults aged 60+ (Figure 1).49 This suggests that local factors, such as attitudes, beliefs, reimbursement policies, and vaccination policies, have a substantial impact on adult vaccination rates.48 Promoting well-crafted state vaccine policies will propitiously position pharmacists to participate in vaccination activities.
Figure 1.
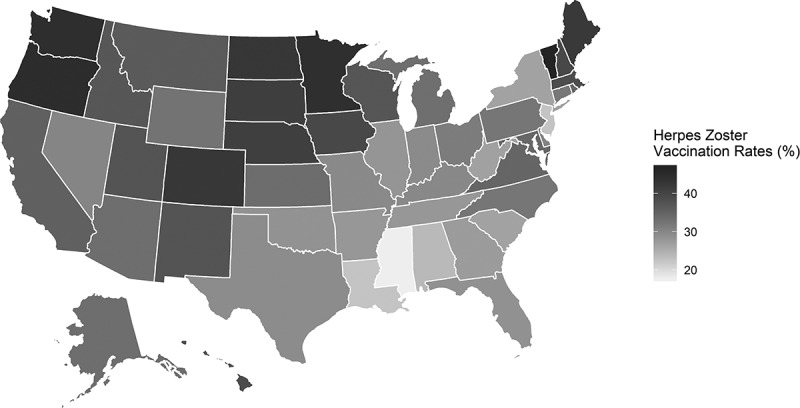
State-Level Herpes Zoster Vaccination Rates for Adults Aged 60+, 2014.
Notes: Map created based on state-level data from Lu PJ, O’Halloran A, Williams WW, Harpaz R. National and State-Specific Shingles Vaccination Among Adults Aged >/= 60 Y. American journal of preventive medicine. 2017;52(3):362–372. RStudio was used to create the map: RStudio (2019). RStudio: Integrated development environment for R (Version 1.1.456) Boston, MA.
Conclusions
Vaccination is a national priority in the US. While older adults encounter many barriers to vaccination, pharmacists are positioned to address many of these barriers. Pharmacists facilitate vaccination by providing a convenient point of access, building confidence in vaccination, and actively increasing awareness to reduce complacency. When pharmacists are involved in the vaccination process, either as educators, facilitators, or administrators, research studies have repeatedly shown improvement in vaccination coverage.50 Ensuring that mechanisms are in place to support pharmacist-administered vaccination, such as immunization training, state authorization, and low patient cost-sharing requirements, can further propel pharmacists to engage in vaccination and disease prevention.
Disclosure of potential conflicts of interest
The spouse of MWM is an employee of the American Pharmacists Association. No other potential conflicts of interest were reported by the authors.
References
- 1.World Health Organization . Ten threats to global health in 2019. 2019; [Accessed 2019 May24]. https://www.who.int/emergencies/ten-threats-to-global-health-in-2019.
- 2.Leidner AJ, Murthy N, Chesson HW, Biggerstaff M, Stoecker C, AM Harris, Acosta A, Dooling K, CB Bridges. Cost-effectiveness of adult vaccinations: a systematic review. Vaccine. 2019;37(2):226–34. doi: 10.1016/j.vaccine.2018.11.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ozawa S, Portnoy A, Getaneh H, Clark S, Knoll M, Bishai D, HK Yang, PD Patwardhan. Modeling the economic burden of adult vaccine-preventable diseases in the United States. Health Aff (Millwood). 2016;35(11):2124–32. doi: 10.1377/hlthaff.2016.0462. [DOI] [PubMed] [Google Scholar]
- 4.Esposito S, Principi N, Rezza G, Bonanni P, Gavazzi G, Beyer I, Sulzner M, Celentano LP, Prymula R, Rappagliosi A, et al. Vaccination of 50+ adults to promote healthy ageing in Europe: the way forward. Vaccine. 2018;36(39):5819–24. doi: 10.1016/j.vaccine.2018.08.041. [DOI] [PubMed] [Google Scholar]
- 5.Kim DK, Hunter P.. Advisory Committee on immunization P. Recommended adult immunization schedule, United States, 2019. Ann Intern Med. 2019;170(3):182–92. doi: 10.7326/M18-3600. [DOI] [PubMed] [Google Scholar]
- 6.Office of Disease Prevention and Health Promotion . Immunization and infectious diseases. Healthy People 2020 2019. [Accessed 2019 May24]. https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives.
- 7.Hung M-C, Williams WW, Lu PJ, Woods LO, Koppaka R, Lindley MC. Vaccination Coverage among Adults in the United States, National Health Interview Survey, 2017. Atlanta (GA)2018. [Google Scholar]
- 8.Schmid P, Rauber D, Betsch C, Lidolt G, Denker ML. Barriers of influenza vaccination intention and behavior - a systematic review of influenza vaccine hesitancy, 2005–2016. PLoS One. 2017;12:e0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014;32(19):2150–59. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 10.Alici DE, Sayiner A, Unal S. Barriers to adult immunization and solutions: personalized approaches. Hum Vaccin Immunother. 2017;13(1):213–15. doi: 10.1080/21645515.2016.1234556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Pharmacists Association . Pharmacist administered vaccines. 2019. [Accessed 2019 May23]. https://media.pharmacist.com/practice/IZ_Authority_012019_corrected_April_2019.pdf.
- 12.Steyer TE, Ragucci KR, Pearson WS, Mainous AG, 3rd . The role of pharmacists in the delivery of influenza vaccinations. Vaccine. 2004;22(8):1001–06. doi: 10.1016/j.vaccine.2003.08.045. [DOI] [PubMed] [Google Scholar]
- 13.Taitel MS, Fensterheim LE, Cannon AE, Cohen ES. Improving pneumococcal and herpes zoster vaccination uptake: expanding pharmacist privileges. Am J Manag Care. 2013;19:e309–e313. [PubMed] [Google Scholar]
- 14.CR Tak, Gunning K, Kim Jet al. The effect of a prescription order requirement for pharmacist-administered vaccination on herpes zoster vaccination rates. Vaccine. 2019;37(4):631–36. doi: 10.1016/j.vaccine.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Qato DM, Zenk S, Wilder J, Harrington R, Gaskin D, Alexander GC. The availability of pharmacies in the United States: 2007–2015. PLoS One. 2017;12(8):e0183172. doi: 10.1371/journal.pone.0183172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaiser Family Foundation . Retail prescription drugs filled at pharmacies (Annual per Capita). 2018; http://kff.org/other/state-indicator/retail-rx-drugs-per-capita/. Accessed 2019 May23.
- 17.Burson RC, Buttenheim AM, Armstrong A, Feemster KA. Community pharmacies as sites of adult vaccination: a systematic review. Hum Vaccin Immunother. 2016;12(12):3146–59. doi: 10.1080/21645515.2016.1215393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsuyuki RT, Beahm NP, Okada H, Al Hamarneh YN. Pharmacists as accessible primary health care providers: review of the evidence. Can Pharm J (Ott). 2018;151(1):4–5. doi: 10.1177/1715163517745517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stagnitti MN. Average number of total (Including Refills) and unique prescriptions by select person characteristics, 2006. Rockville (MD): Agency for Healthcare Research and Quality; 2009. [Google Scholar]
- 20.Rui P, Okeyode T. National ambulatory medical care survey: 2016 State and National Summary tables . [Accessed 2019 May24]. https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2016_namcs_web_tables.pdf.
- 21.National Vaccine AC. Recommendations from the National vaccine advisory committee: standards for adult immunization practice. Public Health Reports (washington, DC: 1974). 2014;129(2):115–23. doi: 10.1177/003335491412900203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lutz CS, Kim DK, Black CL, Ball SW, Devlin RG, Srivastav A, Fiebelkorn AP, Bridges CB. Clinicians’ and pharmacists’ reported implementation of vaccination practices for adults. Am J Prev Med. 2018;55(3):308–18. doi: 10.1016/j.amepre.2018.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hurley LP, Bridges CB, Harpaz R, MA Allison, ST Leary, LA Crane, Brtnikova M, Stokley S, BL Beaty, Jimenez-Zambrano A, et al. Physician attitudes toward adult vaccines and other preventive practices, United States, 2012. Public Health Reports (Washington, DC: 1974). 2016;131(2):320–30. doi: 10.1177/003335491613100216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Islam JY, Gruber JF, Lockhart A, Kunwar M, Wilson S, Smith SB, Brewer NT, Smith JS. Opportunities and challenges of adolescent and adult vaccination administration within pharmacies in the United States. Biomed Inform Insights. 2017;9:1178222617692538. doi: 10.1177/1178222617692538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Talbert JC, Schadler A, Freeman PR. Rural/urban disparities in pneumococcal vaccine service delivery among the Fee-for-service medicare population. Kentucky (USA): Rural & Underserved Health Research Center; 2018. [Google Scholar]
- 26.Johnson M. Survey: Americans prefer pharmacy over physician when it comes to vaccines. 2017. [Accessed 2017 March21]. http://www.drugstorenews.com/article/survey-americans-prefer-pharmacy-over-physician-when-it-comes-vaccines.
- 27.Grabenstein JD, Guess HA, Hartzema AG, Koch GG, Konrad TR. Attitudinal factors among adult prescription recipients associated with choice of where to be vaccinated. J Clin Epidemiol. 2002;55:279–84. [DOI] [PubMed] [Google Scholar]
- 28.Beshears J, Choi JJ, Laibson DI, Madrian BC, Reynolds GI. Vaccination rates are associated with functional proximity but not base proximity of vaccination clinics. Med Care. 2016;54(6):578–83. doi: 10.1097/MLR.0000000000000523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brenan M Nurses again outpace other professions for honesty, ethics. 2018. [Accessed 2019 May24]. https://news.gallup.com/poll/245597/nurses-again-outpace-professions-honesty-ethics.aspx.
- 30.Donohue JM, Huskamp HA, Wilson IB, Weissman J. Whom do older adults trust most to provide information about prescription drugs? Am J Geriatr Pharmacother. 2009;7(2):105–16. doi: 10.1016/j.amjopharm.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grabenstein JD, Hartzema AG, Guess HA, Johnston WP. Community pharmacists as immunisation advocates: a pharmacoepidemiologic experiment. Int J Pharm Prac. 1993;2(1):5–10. doi: 10.1111/ijpp.1993.2.issue-1. [DOI] [Google Scholar]
- 32.Lu PJ, O’Halloran A, Kennedy ED, et al. Awareness among adults of vaccine-preventable diseases and recommended vaccinations, United States, 2015. Vaccine. 2017;35(23):3104–15. doi: 10.1016/j.vaccine.2017.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.ASHP: American Society of Health System Pharmacists Council on Professional Affairs. ASHP guidelines on the pharmacist’s role in immunization. Amer J Health Syst Pharm off J Amer Soc Health Syst Pharm. 2003;60(13):1371–77. doi: 10.1093/ajhp/60.13.1371. [DOI] [PubMed] [Google Scholar]
- 34.American Pharmacists Association . House of Delegates Policy and Procedure Manual, 1963–2018. 2018.
- 35.International Pharmaceutical Federation (FIP) . An overview of current pharmacy impact on immunisation A global report 2016. The Hague (Netherlands)2016. [Google Scholar]
- 36.Baker L. The role of pharmacists in travel medicine in South Africa. Pharmacy (Basel). 2018;6:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McMillian S, Yemeke T, Ozawa S. Role of pharmacists in vaccination in low- and middle-income countries: multi-country survey. Working paper. University of North Carolina at Chapel Hill. NC ; 2019. [Google Scholar]
- 38.Mayora C, Kitutu FE, Kandala NB, Ekirapa-Kiracho E, Peterson SS, Wamani H. Private retail drug shops: what they are, how they operate, and implications for health care delivery in rural Uganda. BMC Health Serv Res. 2018;18(1):532. doi: 10.1186/s12913-018-3343-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Al-lela OQ, Bahari MB, Elkalmi RM, Jawad Awadh AI. Incorporating an immunization course in the pharmacy curriculum: malaysian experience. Am J Pharm Educ. 2012;76(10):206. doi: 10.5688/ajpe76232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Varicella CDC (Chickenpox) and Herpes Zoster (Shingles): Overview of VZV Disease and Vaccination for Healthcare Professionals. 2013.
- 41.Williams WW, Lu PJ, O’Halloran A, Kim DK, Grohskopf LA, Pilishvili T, Skoff TH, Nelson NP, Harpaz R, Markowitz LE, et al. Surveillance of vaccination coverage among adult populations - United States, 2015. Morbidity Mortality Weekly Rep Surveillance Summaries (Washington, DC: 2002). 2017;66(11):1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sparkman A, Brookhart AL, Goode JKR. The impact of an immunization check-up at a pharmacist-provided employee health screening. J Am Pharm Assoc (2003). 2017;57(3S):S274–S278. doi: 10.1016/j.japh.2017.02.010. [DOI] [PubMed] [Google Scholar]
- 43.Wehbi NK, Wani RJ, Klepser DG, Murry J, Khan AS. Impact of implementing a technology platform in community pharmacies to increase adult immunizations rates. Vaccine. 2019;37(1):56–60. doi: 10.1016/j.vaccine.2018.11.043. [DOI] [PubMed] [Google Scholar]
- 44.Wang J, Ford LJ, Wingate L, Jaber N, CT Smith, Randolph R, Lane S, SL Foster. Effect of pharmacist intervention on herpes zoster vaccination in community pharmacies. J Am Pharm Assoc (2003). 2013;53(1):46–53. doi: 10.1331/JAPhA.2013.12019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Otsuka SH, Tayal NH, Porter K, Embi PJ, Beatty SJ. Improving herpes zoster vaccination rates through use of a clinical pharmacist and a personal health record. Am J Med. 2013;126(9):e831–e836. doi: 10.1016/j.amjmed.2013.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hess R. Impact of automated telephone messaging on zoster vaccination rates in community pharmacies. J Am Pharm Assoc (2003). 2013;53(2):182–87. doi: 10.1331/JAPhA.2013.12222. [DOI] [PubMed] [Google Scholar]
- 47.Lin JL, Bacci JL, Reynolds MJ, Li Y, Firebaugh RG, Odegard PS. Comparison of two training methods in community pharmacy: project VACCINATE.. J Am Pharm Assoc. 2003;58(4s):S94–S100.e103. doi: 10.1016/j.japh.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 48.La EM, Trantham L, Kurosky SK, Odom D, Aris E, Hogea C. An analysis of factors associated with influenza, pneumoccocal, Tdap, and herpes zoster vaccine uptake in the US adult population and corresponding inter-state variability. Hum Vaccin Immunother. 2018;14(2):430–41. doi: 10.1080/21645515.2017.1403697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lu PJ, O’Halloran A, Williams WW, National HR. State-specific shingles vaccination among adults aged >/=60 years. Am J Prev Med. 2017;52(3):362–72. doi: 10.1016/j.amepre.2016.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Isenor JE, Edwards NT, Alia TA, Slayter KL, MacDougall DM, McNeil SA, Bowles SK. Impact of pharmacists as immunizers on vaccination rates: a systematic review and meta-analysis. Vaccine. 2016;34(47):5708–23. doi: 10.1016/j.vaccine.2016.08.085. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- World Health Organization . Ten threats to global health in 2019. 2019; [Accessed 2019 May24]. https://www.who.int/emergencies/ten-threats-to-global-health-in-2019.


