ABSTRACT
The anatomical safety of intramuscular injections at the deltoid and ventrogluteal sites has been investigated; however, the anatomical relationship between intramuscular injection sites in the thigh and major blood vessels and nerves remains unclear. We aimed to compare intramuscular injection sites in the rectus femoris and vastus lateralis with those at the deltoid and ventrogluteal sites and identify safe intramuscular injection sites in the thigh. Twenty-seven young adult volunteers were recruited, and the thicknesses of subcutaneous tissue and muscle as well as the number of blood vessels present were evaluated at two sites on the deltoid, ventrogluteal, and thigh using ultrasound equipment. The right thighs of 24 cadavers were used, and the thickness of muscle, number of blood vessels or nerves present, and the distance between each examined site and major blood vessels or nerves were evaluated in the rectus femoris and vastus lateralis. A major blood vessel was observed in the middle of the rectus femoris in young adults. In cadavers, the descending branch of the lateral circumflex femoral artery and muscle branch of the femoral nerves to the vastus lateralis were observed at the middle point, distal two-thirds point, and middle point between the middle and distal two-thirds points of the rectus femoris, but not at the middle of the vastus lateralis. The middle of the vastus lateralis is an appropriate site for intramuscular injections because of the low risk of vascular or nerve damage. The present results support good practices for site selection for intramuscular injections.
KEYWORDS: Intramuscular injections, thigh, safety, femoral nerve, femoral artery
Introduction
Intramuscular (IM) injections are a technique used to deliver vaccines, hormonal agents, antibiotics, and high viscosity medication deep into the muscles of patients.1 When considering IM injection sites, a clinician needs to select a site that is (1) a safe distance from nerves, large blood vessels, and bones, (2) free from injury, abscesses, tenderness, necrosis, abrasions, and other pathologies, and (3) sufficiently large to accommodate the volume of medication to be administered.2 Based on these three conditions, deltoid, ventrogluteal, and thigh sites are considered to be safe and, thus, commonly used for IM injections.
The deltoid site has been used in clinical settings and is preferred in Japan because it is easily accessible for clinicians and also for patients to expose.3 Since this area has a small mass, clinicians may only administer small amounts of medication. Although the site located at a one to three finger breadth below the acromion is generally recommended for an IM injection at the deltoid site,4,5 we previously reported that the site at a three finger breadth (approximately 5 cm) below the acromion was not acceptable for IM injections because it is close to the axillary nerve and posterior circumflex humeral artery (PCHA).6,7 Therefore, we proposed the intersection between the anteroposterior axillary line (the line between the upper end of the anterior axillary line and upper end of the posterior axillary line) and the perpendicular line from the mid-acromion as the most appropriate site for IM injections with a low risk of axillary nerve and PCHA damage (This site is shown in Figure 1 (A) in reference).8
A ventrogluteal site is the most commonly used and recommended site for IM injections in adults and children of walking age because of the large muscle mass. This site is located away from the superior and inferior gluteal arteries as well as the sciatic and superior gluteal nerves,9 and is also the least painful.2 Hochstetter10 initially suggested that this site was appropriate for IM injections. The V method is often used to identify IM injection sites in this area.1,11,12 The V method is performed as follows: when the injection site is on the left side, the palm of the right hand is placed over the greater trochanter. The index finger is placed on the anterior superior iliac spine. The middle finger is then positioned towards the iliac crest. The index and middle fingers create a V-shape, and the injection site is in the middle of the V-shape. In Japan, the point of Clark is the most popular IM injection point at the ventrogluteal site.13 This point is defined as the anterior one-third between the anterior and posterior superior iliac spines. However, the posterior superior iliac spine may be difficult to palpate when locating the point of Clark. Therefore, we previously established a novel IM injection point located at the intersection of the horizontal line from the anterior superior iliac spine and the perpendicular line from the middle portion of the trochanter major, and this novel point was shown to be as safe as the point of Clark with a low risk of damage to the superior and inferior gluteal artery as well as the sciatic and superior gluteal nerves.9,14–16
In Japan, IM injections into the thigh are rarely performed in adults because of the outbreak of quadriceps contracture among children in the 1970s. This outbreak was attributed to the repeated administration of antibiotics and antipyretics, and not to vascular or nerve damage.17 Therefore, IM injections into the thigh may be used for Japanese adults. The vastus lateralis site is generally the preferred site for young infants, particularly those not yet walking.18 Moreover, this site is often used by patients who self-administer IM injections because it is easy to access.19 The middle third of the lateral thigh between the trochanter major and the knee is an injection site in the vastus lateralis and is not in close proximity to any major blood vessels or nerves.2,20 However, limited information is currently available on blood vessels or nerves traveling in IM injection sites in the vastus lateralis. Additionally, the rectus femoris (the middle third of the rectus femoris) is no longer a recommended site because it may cause discomfort and pain.1,2,18 A previous study reported that one disadvantage of this site is that nerves and numerous blood vessels run very close to it.21 Although blood vessels and nerves traveling close to or in IM injection sites in the deltoid and ventrogluteal sites have been extensively examined,6,7,9,15 those in the vastus femoris have not.
An evidence-based approach is needed for site selection for successful IM injections and the avoidance of vascular or nerve damage. In order to identify safe IM injection sites in the thigh, the anatomical relationship between IM injection sites and major blood vessels and nerves needs to be elucidated in more detail. Therefore, in the present study, we compared IM injections in the thigh to those at the deltoid and ventrogluteal sites in young adults, observed blood vessels and nerves traveling close to or in IM injection sites in the vastus lateralis and rectus femoris in cadavers, and clarified what site in the thigh is anatomically safe for IM injections.
Materials and methods
Study design and setting
This was a cross-sectional study that was conducted at a university in Japan. It commenced on August 18, 2017 and was completed on December 12, 2018.
Subjects
Thirty healthy volunteers participated in the present study and met the following inclusion criteria: age >17 y old, no history of buttock or upper/lower limb injury/surgery or neurological or muscular diseases of the buttocks or upper/lower limbs, no allergies to the implements used in this study, and a body mass index (BMI) >17 and <30.
No history of neurological, vascular, or muscular disease was an inclusion criterion in cadavers. The embalmed right thighs of Japanese adult cadavers were examined macroscopically. All cadavers were supplied by body donation to Kanazawa University and consent had been obtained for their use for medical education and research. The present study was conducted during anatomy practice for medical students in 2018.
Young adults
Definition of examined sites
All examined sites in males and females were defined by one male and two female nursing students who were trained by a medical doctor specializing in anatomy and a registered nurse acquiring basic nursing skills. The locations of all examined sites in the present study are shown in Figure 1. Sites (a) to (e) are described in Figure 1.
Figure 1.
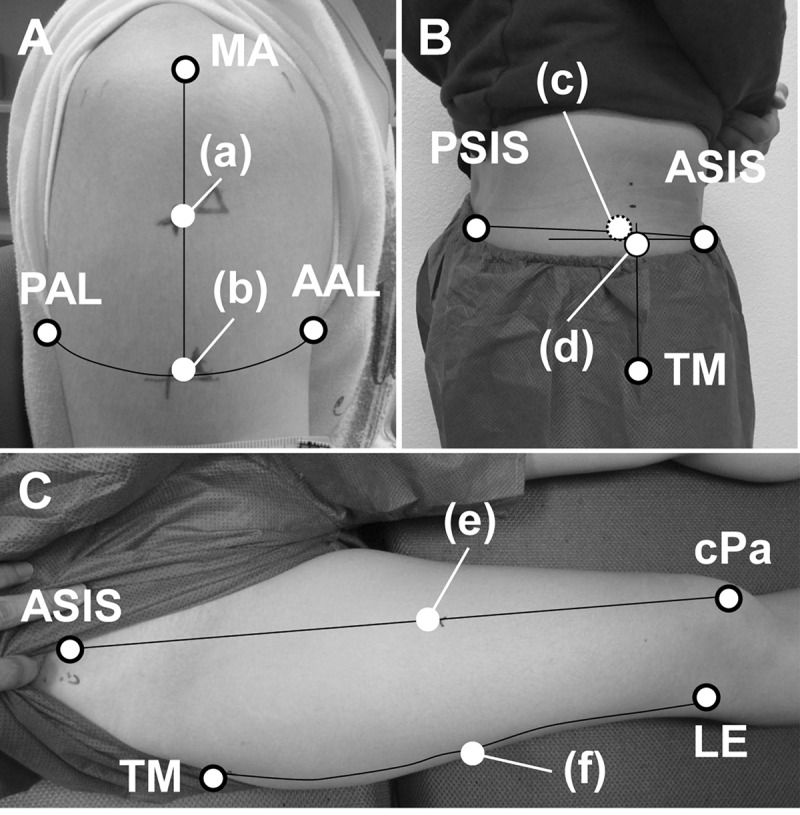
Locations of six examined sites in young adults. A: In the deltoid muscle, three finger breadths below the mid-acromion (MA) was defined as (a), and the point on the anteroposterior axillary line (b) was defined as that located at the intersection of the perpendicular line from MA and the horizontal line between the upper end of the anterior axillary line (AAL) and upper end of the posterior axillary line (PAL). B: In the gluteus medius, the point of Clark (c) was defined as that located at the anterior one-third point between the anterior superior iliac spine (ASIS) and posterior superior iliac spine (PSIS), and the novel point on the gluteus medius (d) was defined as that located at the intersection of the horizontal line from ASIS and the perpendicular line from the middle portion of the trochanter major (TM). C: In the rectus femoris, the middle point of the rectus femoris (e) was defined as that located at the middle point between ASIS and the center of the patella (cPa). In the vastus lateralis, the middle point of the vastus lateralis (f) was defined as that located at the middle point between the TM and lateral epicondyle (LE).
Two IM injection sites were defined in the deltoid muscle: (a) three finger breadths below the acromion, which is frequently used in clinical settings in Japan and (b) our original IM injection site (the point on the anteroposterior axillary line), which was previously proposed as a safer site.6,8 All participants were seated with their arms in the anatomical position before the definition of the examined sites in the deltoid muscle. Site (a) was defined after the acromion on the right arm was identified and the digitus annularis in the left hand was placed on the inferior border of the acromion. Site (b) was defined as described in detail in our previous study.8
In the ventrogluteal site, two IM injection sites were defined: (c) the point of Clark, which is located at the anterior one-third point between the anterior superior iliac spine and (d) our original IM injection site (a novel point on the gluteus medius), which was previously proposed as a safe site similar to the point of Clark. Site (d) was defined as described in detail in our previous studies.14,15 All participants were in the left lateral position with their legs in the anatomical position before the definition of the examined sites.
Two IM injection sites were defined in the thigh: (e) the middle point of the rectus femoris and (f) the middle point of the vastus lateralis because the middle third of these muscles has been recommended for IM injections in clinical settings21,22 and the middle points of these muscles correspond to the middle points of the middle third of these muscles. All participants were in the supine position with their legs in the anatomical position before the definition of the examined sites in the rectus femoris and vastus lateralis.
Data collection
Ultrasound equipment (Noblus, 18–5 MHz probe, Hitachi Aloka Medical Inc., Tokyo, Japan) was used to measure the thickness of subcutaneous tissue and muscle and detect blood vessels by three trained nursing students. Ultrasound images using the B-mode were obtained three times to evaluate the thicknesses of subcutaneous tissue and muscle. Compression by the probe against the skin was avoided and the probe was held at a 90° angle to the plane of the examined sites. Blood vessels were identified with the Doppler mode at (a) to (f), as shown in Figure 2.
Figure 2.
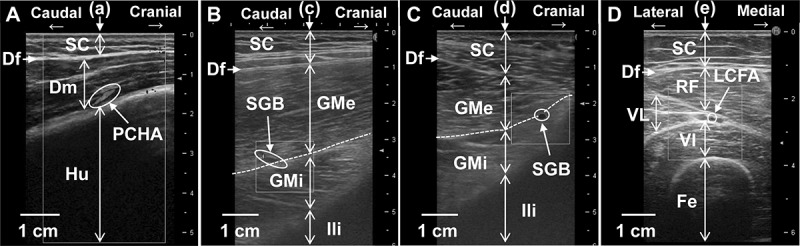
Detection of major blood vessels at four examined sites by ultrasound images. A: The posterior circumflex humeral artery (PCHA) was detected between the deltoid muscle (Dm) and humerus (Hu) at three finger breadths below the acromion (a). B: The superior gluteal artery or vein (SGB) was detected between the gluteus medius (GMe) and gluteus minimus (GMi) at the point of Clark (c). C: The superior gluteal artery or vein (SGB) was detected between GMe and GMi at the novel point on the gluteus medius (d). D: The lateral circumflex femoral artery (LCFA) was detected between the rectus femoris (RF) and vastus lateralis (VL) at the middle point of the rectus femoris (e). SC; subcutaneous tissue, Df; deep fascia, Ili; ilium, VI; vastus intermedius, Fe; femur.
Cadavers
Definition of examined sites
All examined sites in males and females were defined by one medical doctor specialized in anatomy. The dissection and definition of the examined sites were performed in the supine position. The locations of the four examined sites are shown in Figure 3(B): (e) the middle point of the rectus femoris, (f) the middle point of the vastus lateralis, (g) the middle point between the middle of the rectus femoris and distal two-thirds point of the rectus femoris, and (h); the distal two-third points of the rectus femoris.
Figure 3.
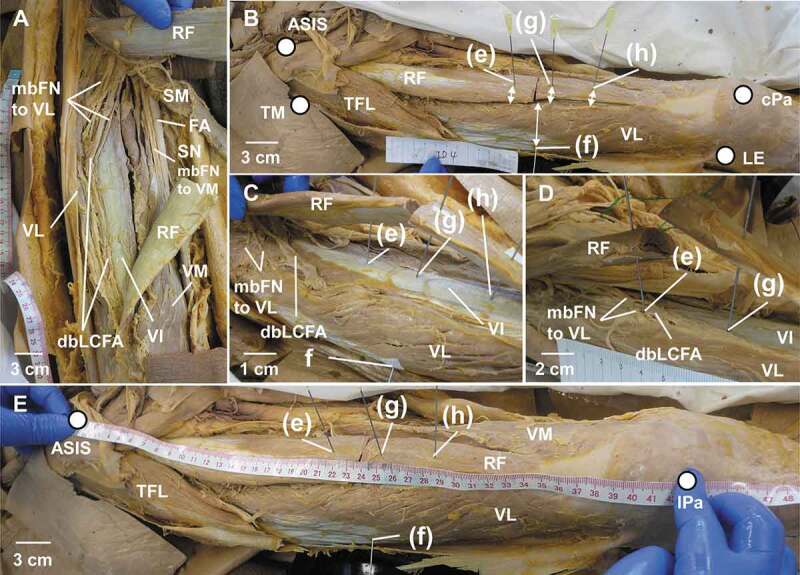
Dissection of the right thigh and evaluation of the risk of vascular or nerve damage at examined sites in cadavers. A: Dissection of the right anterior thigh in a female. B: Locations of the examined sites in the rectus femoris (RF) and vastus lateralis (VL) in a female. Two direction arrows revealed the distance between each examined site and a major blood vessel or nerve. C: A case of no blood vessel or nerve damage at any examined site in the thigh of a male. D: A case of damage to the descending branch of the lateral circumflex femoral artery (dbLCFA) at the middle point of RF in a female. E: The line connecting the anterior superior iliac spine (ASIS) to the lateral border of the patella (lPa) corresponds to the boundary line between RF and VL. mbFN to VL; muscle branches of the femoral nerve to VL, VI; vastus intermedius, VM; vastus medialis, SM; sartorius muscle, mbFN to VM; muscle branches of the femoral nerve to VM, FA; femoral artery, SN; saphenous nerve, TFL; tensor fascia latae, TM; trochanter major, cPa; center of the patella, LE; lateral epicondyle. (e); the middle point of RF, (f); the middle point of VL, (g); the middle point between (e) and (h), (h); the distal two-thirds point of RF.
Data collection
Surface skin was removed and the rectus femoris and vastus lateralis were exposed by medical students. The four examined sites were marked using seals and needles (14 G) were perpendicularly inserted into each site until they made contact with the femur. The needle insertion length was expressed as the thickness of muscle. Dissections were subsequently performed by one medical doctor, and distances from major blood vessels or nerves were measured at each examined site using a tape measure (two direction arrows in Figure 3(B)). The findings obtained were recorded with photographs. We defined anatomically safe sites as those located 1 cm from blood vessels and nerves in the present study.
Statistical analysis
Data on subcutaneous tissue and muscle thicknesses and distances from major blood vessels or nerves were expressed as the mean ± SD (minimum – maximum). The thicknesses of subcutaneous tissue and muscle in young adults and distances from major blood vessels or nerves in cadavers were analyzed by the Kruskal-Wallis and Steel-Dwass tests, and the thickness of muscle in cadavers by an ANOVA and Tukey’s HSD test using JMP12 (SAS Institute Inc., NC). Differences were considered to be significant at p < .05.
Ethical considerations
The present study was approved by the Kanazawa University Ethical Committee (Approval No. 784–1 and No. 834–1). Young adult participants were informed of the aim and benefits of this study before their inclusion. They were also informed that they were free to take part or not in the study as they chose. Written and verbal consent was obtained from all participants. All the cadavers were supplied by body donation and consent had been obtained for their use for education and research. Data obtained from subjects were only used for statistical analyses.
Results
Subjects
Young adults
Thirty healthy volunteers were recruited. Three volunteers (two males and one female) were excluded based on BMI <17 or >30. Therefore, 27 participants were included in the present study. Thirteen participants (48.1%) were male, the average age was 22.7 ± 2.1 (19–28) y, and average BMI was 21.2 ± 3.6 (18.9–23.4). Fourteen participants (51.9%) were female, the average age was 22.3 ± 2.0 (21–29) y, and average BMI was 21.7 ± 5.1 (18.0–23.6).
Cadavers
Twenty-four subjects were recruited. Thirteen subjects (54.2%) were males and the average age was 83.4 ± 9.9 (66–98) y. Eleven subjects (45.8%) were female and the average age was 87.0 ± 11.4 (60–103) y.
Data obtained from young adults
Thickness of subcutaneous tissue
Six examined sites were evaluated. As shown in Table 1, mean subcutaneous thickness in males was not significantly different between any examined sites, whereas it was significantly greater in females at (e) and (f) than at (a) (p = .0009, p = .0042, respectively). Mean subcutaneous thickness was significantly greater at (e) than at (c) (p = .0499). The average thickness of subcutaneous tissue in males was within 10 mm at all examined sites, but was greater than 10 mm at all examined sites, except at (a), in females.
Table 1.
Thickness of subcutaneous tissue at each injection site in young adults.
| Male | Female | |
|---|---|---|
| (a) | 5 ± 1 (3–8) |
8 ± 2 (5–13) |
| (b) | 6 ± 2 (4–11) |
11 ± 4 (5–16) |
| (c) | 6 ± 6 (2–13) |
10 ± 3‡ (5–17) |
| (d) | 7 ± 3 (2–15) |
10 ± 5 (6–22) |
| (e) | 7 ± 2 (4–9) |
13 ± 2† (9–17) |
| (f) | 6 ± 2 (3–8) |
13 ± 4† (8–21) |
(a); three finger breadths below the acromion, (b); the point on the anteroposterior axillary line, (c); the point of Clark, (d); the novel point on the gluteus medius, (e); the middle of the rectus femoris, (f); the middle of the vastus lateralis. Unit; mm, Data; mean ± SD, Brackets: a range of minimum to maximum values, Males; n = 13, Females; n = 14. † Kruskal-Wallis and Steel-Dwass tests compared with (a), ‡ Kruskal-Wallis and Steel-Dwass tests compared with (e) (p < 0.05).
Thickness of muscle
The thickness of muscle was measured using ultrasound equipment. Since only the deltoid muscle was observed at the deltoid site, the deep fascia – bone margin was measured as the thickness of the deltoid muscle (Figure 2(A), Table 2). At the ventrogluteal site, the gluteus minimus was observed under the gluteus medius in some participants. The deep fascia – bone margin was measured as the total thickness of muscle, and the deep fascia – fascia between the gluteus medius and gluteus minimus was measured as the thickness of the gluteus medius (Figure 2(B,C), Table S). In the thigh, the rectus femoris and vastus intermedius were observed at (e), while the vastus lateralis and vastus intermedius were noted at (f). The deep fascia – bone margin was measured as the total thickness of muscle in the thigh, and the deep fascia – fascia between the rectus femoris or vastus lateralis and vastus intermedius was measured as the thickness of the rectus femoris or vastus lateralis (Figure 2(D), Table 2).
Table 2.
Thickness of each muscle at examined injection sites in young adults.
| Sites | Muscle | Thickness | Muscle | Thickness | Total thickness |
|---|---|---|---|---|---|
| Male | |||||
| (a) | Deltoid | 23 ± 5 (17–34) |
- | - | 23 ± 5†‡ (17–34) |
| (b) | Deltoid | 24 ± 4 (17–31) |
- | - | 24 ± 4†‡ (17–31) |
| (c) | Gluteus medius | 25 ± 10 (9–40) |
Gluteus minimus | 5 ± 7 (0–14) |
30 ± 11† (8–42) |
| (d) | Gluteus medius | 27 ± 9 (9–39) |
Gluteus minimus | 7 ± 6 (0–15) |
34 ± 12 (12–46) |
| (e) | Rectus femoris | 23 ± 3 (18–27) |
Vastus intermedius | 19 ± 7 (4–33) |
41 ± 6 (29–47) |
| (f) | Vastus lateralis | 19 ± 5 (13–29) |
Vastus intermedius | 18 ± 5 (10–25) |
37 ± 8 (26–47) |
| Female | |||||
| (a) | Deltoid | 17 ± 2 (13–22) |
- | - | 17 ± 2†‡ (13–20) |
| (b) | Deltoid | 16 ± 2† (11–20) |
- | - | 16 ± 2†‡ (11–20) |
| (c) | Gluteus medius | 16 ± 7 (8–30) |
Gluteus minimus | 2 ± 3 (0–8) |
18 ± 9†‡ (8–36) |
| (d) | Gluteus medius | 16 ± 8 (7–30) |
Gluteus minimus | 3 ± 5 (0–14) |
19 ± 11† (7–42) |
| (e) | Rectus femoris | 20 ± 3 (15–26) |
Vastus intermedius | 18 ± 4 (12–26) |
38 ± 6 (30–52) |
| (f) | Vastus lateralis | 17 ± 6 (9–23) |
Vastus intermedius | 13 ± 6 (5–23) |
30 ± 8 (21–44) |
(a); three finger breadths below the acromion, (b); the point on the anteroposterior axillary line, (c); the point of Clark, (d); the novel point on the gluteus medius, (e); the middle of the rectus femoris, (f); the middle of the vastus lateralis. Unit; mm, Data; mean ± SD, Brackets: a range of minimum to maximum values, Males; n = 13, Females; n = 14. † Kruskal-Wallis and Steel-Dwass tests compared with (e), ‡ Kruskal-Wallis and Steel-Dwass tests compared with (f) (p < 0.05).
As shown in Table 2, the thickness of muscle was significantly thicker at (e) than at (b) in females (p = .0254). In males, total thickness was significantly greater at (e) than at (a), (b), and (c) (p = .0004, 0.0004, and 0.0169, respectively), and total thickness was significantly greater at (f) than at (a) and (b) (p = .0007 and 0.0012, respectively). In females, total thickness was significantly greater at (e) than at (a), (b), (c), and (d) (p = .0001, 0.0001, 0.0025, and 0.0025, respectively), and total thickness was significantly greater at (f) than at (a), (b), and (c) (p = .0002, 0.0001, and 0.0190, respectively).
Observed major blood vessels
Major blood vessels were detected at (a), (c), (d), and (e) by the Doppler mode of ultrasound equipment. At the deltoid site, a blood vessel, which ran between the deltoid muscle and humerus, was observed in two females within a range of 1 cm at (a) (Figure 2(A), Table 3), while no major blood vessel was noted at (b). At the ventrogluteal site, blood vessels, which ran between the gluteus medius and gluteus minimus, were observed in one male and one female at (c) and in one male at (d) (Figure 2(B,C), Table 3). In the thigh, blood vessels were observed between the rectus femoris and vastus lateralis in seven males and eleven females at (e), while no major blood vessel was observed at (f) (Figure 2(D), Table 3).
Table 3.
Number of observed blood vessels within 1 cm of each injection site in young adults.
| Males (%) |
Females (%) |
|||
|---|---|---|---|---|
| Sites | Observed | Not observed | Observed | Not observed |
| (a) | 0 (0.0) | 13 (100.0) | 2 (14.3) | 12 (85.7) |
| (b) | 0 (0.0) | 13 (100.0) | 0 (0.0) | 14 (100.0) |
| (c) | 1 (7.7) | 12 (92.3) | 1 (7.1) | 13 (92.9) |
| (d) | 1 (7.7) | 12 (92.3) | 0 (0.0) | 14 (100.0) |
| (e) | 7 (53.8) | 6 (46.2) | 11 (78.6) | 3 (21.4) |
| (f) | 0 (0.0) | 13 (100.0) | 0 (0.0) | 14 (100.0) |
(a); three finger breadths below the acromion, (b); the point on the anteroposterior axillary line, (c); the point of Clark, (d); the novel point on the gluteus medius, (e); the middle of the rectus femoris, (f); the middle of the vastus lateralis. Males; n = 13, Females; n = 14.
Data obtained from cadavers
Anatomy of major blood vessels and nerves in the anterior thigh
Twenty-four right thighs were dissected because blood vessels were observed at the middle of the rectus femoris in many young adults. The profundal femoris artery, which is one branch of the femoral artery, gave off the lateral and medial circumflex femoral arteries in the proximal thigh. The lateral circumflex femoral artery (LCFA) passed horizontally and was divided into two branches; ascending and descending. The descending branch of LCFA (dbLCFA) ran downward behind the rectus femoris or on the vastus intermedius obliquely with veins and nerves to the vastus lateralis. It then descended along the border between the vastus intermedius and vastus lateralis and supplied muscles with a long branch that traveled through the muscle downward as far as the knee (Figure 3(A)). The nerves accompanying dbLCFA on the vastus intermedius originated from the femoral nerve, and it was the muscle branch of the femoral nerve to the vastus lateralis (mbFN to VL). mbFN to VL descended obliquely to the border between the vastus lateralis and vastus intermedius and approximately passed through or around (e) (Figure 3(A,C,D)).
As shown in (e) to (h) in Figure 3(B), four points were examined in order to identify safe IM injection sites in the thigh in the following sections.
Thickness of muscle
The total thickness of muscle at four sites was measured by the insertion of a 14G needle (Table 4). No significant differences were observed between the examined sites.
Table 4.
Thickness of muscle at each injection site in the thigh of cadavers.
| Sites | Male | Female |
|---|---|---|
| (e) | 15 ± 7 (6–34) |
13 ± 5 (4–20) |
| (f) | 15 ± 7 (6–30) |
12 ± 6 (3–22) |
| (g) | 13 ± 6 (7–30) |
11 ± 5 (6–19) |
| (h) | 10 ± 6 (5–27) |
10 ± 5 (5–20) |
(e); the middle point of the rectus femoris, f; the middle point of the vastus lateralis, g; the middle point between (e) and (h), (h); the distal two-thirds point of the rectus femoris. (e), (g), (h); sum of the rectus femoris and vastus intermedius, (f); sum of the vastus lateralis and vastus intermedius. Unit; mm, Data; mean ± SD, Brackets: a range of minimum to maximum values. Males; n = 13, Females; n = 11.
Observed major blood vessels or nerves
Needle insertion into dbLFCA or mbFN to VL was evaluated at all examined sites to assess the risk of vascular and nerve damage. No blood vessel or nerve was observed within the range of 1 cm at (f) (Figure 3(C), Table 5). On the other hand, dbLCFA or mbFN to VL was observed at (e), (g), and (h). They were frequently observed at (e) (Figure 3(D), Table 5).
Table 5.
Number of observed blood vessels or nerves within 1 cm of each injection site in the thigh of cadavers.
| Males (%) |
Females (%) |
|||
|---|---|---|---|---|
| Sites | Observed | Not observed | Observed | Not observed |
| (e) | 9 (69.2) | 4 (30.8) | 10 (90.9) | 1 (9.1) |
| (f) | 0 (0.0) | 13 (100.0) | 0 (0.0) | 11 (100.0) |
| (g) | 3 (23.1) | 10 (76.9) | 4 (36.4) | 7 (63.6) |
| (h) | 5 (38.5) | 8 (61.5) | 5 (45.5) | 6 (54.5) |
(e); the middle point of the rectus femoris, f; the middle point of the vastus lateralis, g; the middle point between (e) and (h), (h); the distal two-thirds point of the rectus femoris. Males; n = 13, Females; n = 11.
Distance from major blood vessels or nerves
The average distance from dbLCFA or mbFN to VL was measured to identify safe IM injection sites in the thigh (Figure 3(B)). As shown in Table 6, in males, (f) was more distant from dbLCFA or mbFN to VL than (e), (g), and (h) (p = .0007, 0.0016, and 0.0012, respectively). Moreover, in females, (f) was more distant from dbLCFA or mbFN to VL than (e), (g), and (h) (p = .0004, 0.0015, and 0.0009, respectively), and (g) was more distant from dbLCFA and mbFN to VL than (e) in females (p = .0052).
Table 6.
Distance from major blood vessels or nerves to each injection site in the thigh of cadavers.
| Sites | Male | Female |
|---|---|---|
| (e) | 7 ± 9‡ (0–25) |
4 ± 4‡ (0–12) |
| (f) | 31 ± 13 (10–60) |
35 ± 11 (18–50) |
| (g) | 13 ± 5‡ (1–20) |
13 ± 6†‡ (7–25) |
| (h) | 12 ± 5‡ (6–25) |
10 ± 7‡ (0–20) |
(e); the middle point of the rectus femoris, f; the middle point of the vastus lateralis, g; the middle point between (e) and (h), (h); the distal two-thirds point of the rectus femoris. Unit; mm, Data; mean ± SD, Brackets: a range of minimum to maximum values. Males; n = 13, Females; n = 11. † Kruskal-Wallis and Steel-Dwass tests compared with (e), ‡ Kruskal-Wallis and Steel-Dwass tests compared with (f) (p < 0.05).
The present results revealed that dbLCFA descended the anterior border of the vastus lateralis (the boundary line between the rectus femoris or vastus intermedius and vastus lateralis). This line corresponded to the line between the anterior superior iliac spine and the lateral border of the patella (Figure 3(E)). In brief, the route of dbLCFA and mbFN to VL after reaching the vastus lateralis corresponded to the line between the anterior superior iliac spine and lateral patella.
Discussion
Many types of vaccines, such as diphtheria and tetanus toxoids, hepatitis B, and inactivated influenza vaccines, are administered by IM injections. These vaccines are necessary to prevent vaccine-preventable diseases that occur in infants, children, adolescents, and adults. When vaccinators inject vaccines, they need to be familiar with the anatomy of the area into which they are injecting the vaccine.
The present study compared IM injection sites in the thigh with those at the deltoid and ventrogluteal sites. In young male adults, mean subcutaneous thickness was less than 10 mm at all examined sites and its maximum value was 15 mm at (d), while it was between 8 and 13 mm at all examined sites in young female adults and its maximum value was 21 mm at (f) (Table 1). When an IM injection is performed, a 21 to 23 gauge (14G) needle is generally used.23 The 23G, regular bevel 1.1/4 injection needle has a length of 32 mm. Hence, these needles completely penetrated subcutaneous tissue at all examined sites in the present study. The total thickness of muscle in males and females was greater in the thigh than at the deltoid and ventrogluteal sites. It is important to select the largest muscle for IM injections in order to avoid any disparity between muscle mass and the volume of injected fluid.24 Hence, large volumes of medication and repeated injections may be performed at the thigh.
Major blood vessels were detected at (a), (c), (d), and (e) by Doppler ultrasonography (Figure 2). In the deltoid site, we previously reported that an IM injection at three finger breadths below the acromion (approximately 5 cm below the acromion) was associated with a risk of axillary nerve and PCHA damage because the axillary nerve with the accompanying PCHA is located 3.1 to 7.4 cm below the acromion6,25,26 and in close contact with the deep surface of the deltoid muscle.7 Based on previous findings, a major blood vessel, which was observed at (a) in the present study, was PCHA. Therefore, the site of three finger breadths below the acromion needs to be avoided for use as an IM injection site. On the other hand, there were no blood vessels at (b) (Table 3). The point on the anteroposterior axillary line is distant to PCHA.6,8 Therefore, we recommend the point on the anteroposterior axillary line when IM injections are performed at the deltoid site. At the ventrogluteal site, we previously attempted to identify safe sites for IM injections at (c) and (d).9,14–16 In these studies, we found that the superior and inferior branches of the super gluteal artery or vein (SGB) ran in a V-sharp, sandwiching these two points, and the SGB was observed at (c) and (d) in some participants. Hence, we confirmed that the blood vessel observed in the present study was the superior and inferior branches of the SGB. The numbers of blood vessels observed at (c) and (d) were 2 and 1, respectively, in the present study (Table 3), and this result is consistent with our previous findings.14 The present study showed that the novel point on the gluteus medius is as safe as the point of Clark. In the thigh, major blood vessels were observed at (e) in 7 males and 11 females young adults (Table 3). The number of observed blood vessels was higher at (e) than at the other examined sites. In cases in which a needle does not completely penetrate the rectus femoris, dbLCFA or mbFN to VL is not damaged and IM injections may be performed at this site; however, the minimum value of the thickness of the rectus femoris was only 15 mm in young female adults and may be smaller in the elderly. Therefore, the middle point of the rectus femoris is not recommended as a safe IM injection site because of dbLCFA or mbFN to VL injuries.
The right thighs of 24 cadavers were dissected to identify blood vessels observed at (e) by Doppler ultrasonography in young adults. The results obtained showed that dbLCFA and mbFN to VL were frequently observed at (e) in cadavers (Table 5, Figure 3(D)). LCFA generally arises from the profunda femoris artery, and divides into three branches: ascending, transverse, and descending branches.27 dbLCFA supplies a long branch and descends in the vastus lateralis to the knee accompanied by the nerve to the vastus lateralis.28 The route of the observed blood vessels at the examined sites in the thigh in the present study was consistent with that of dbLCFA. Therefore, we confirmed that the observed blood vessels at the examined sites were dbLCFA. Moreover, mbFN to VL was detected at (e), (g), and (h) in the thigh. The femoral nerve classically has three main divisions: the nerve to the pectineus, anterior, and posterior divisions.28 The posterior division gives the saphenous nerve and muscular branches to the quadriceps femoris. A large branch to the vastus lateralis forms a neurovascular bundle with the descending branch of LCFA in its distal part. In the present study, the observed nerves at (e) originated from the femoral nerves and supplied the vastus lateralis. Therefore, we confirmed that the observed nerves at the examined sites were mbFN to VL.
Previous studies recommended the rectus femoris as an IM injection site when other sites are contraindicated because of discomfort, pain, and injuries to a nerve and numerous blood vessels.2,21 In the present study, we showed for the first time that dbLCFA and mbFN to VL were frequently observed at (e), (g), and (h) in the rectus femoris (Table 5). Therefore, IM injections into the rectus femoris need to be avoided because of the risk of dbLCFA and mbFN to VL injuries. Moreover, we found that the route of dbLCFA and mbFN to VL after reaching the vastus lateralis was on the line between the anterior superior iliac spine and lateral border of the patella. We may visualize the route of dbLCFA and mbFN to VL on surface skin using this approach before IM injections. On the other hand, the present study showed that no major blood vessel or nerve was observed at (f) and this site was sufficiently far from dbLCFA and mbFN to VL (Tables 5 and 6). Previous studies recommended the middle third of the vastus lateralis as an IM injection site because of its ease of access and, more importantly, the absence of major blood vessels or significant nerves.2,29,30 The present results support these findings. We recommend the middle of the vastus lateralis as a safe injection site with a low risk of dbLCFA and mbFN to VL injuries. We consider the present results to be beneficial as an evidence-based approach towards site selection for successful IM injections and the avoidance of vascular or nerve damage.
In conclusion, the present results demonstrated that the rectus femoris is not appropriate as a safe IM injection site because of the risk of damage to the descending branch of the LCFA and the muscle branch of the femoral nerve to the vastus lateralis. The middle of the vastus lateralis is an appropriate site for IM injections because it is distant from the descending branch of the LCFA and the muscle branch of the femoral nerve to the vastus lateralis.
Limitations to the study
This study was limited in terms of the number of subjects, normal BMI, and age. Regarding obese subjects, we cannot confirm whether the vastus lateralis is a safe IM injection site because we did not examine the subcutaneous thickness of obese subjects or whether needles used for IM injections penetrate their subcutaneous tissue and reach muscle. Regarding age, we did not obtain any data on the location of dbLCFA and mbFN to VL or subcutaneous thickness in infants, toddlers, children, and young adults. We also did not directly compare data between volunteers and cadavers or generalize results obtained for all ages and ethnicities. Large-scale studies are needed to examine safe IM injection sites in obese and individuals of various ages. Further studies are needed to support the present results.
Funding Statement
This study was supported by JSPS KAKENHI under Grant Number [18H03072].
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- 1.Nicoll LH, Hesby A.. Intramuscular injection: an integrative research review and guideline for evidence-based practice. Appl Nurs Res. 2002;15(3):149–62. doi: 10.1053/apnr.2002.34142. [DOI] [PubMed] [Google Scholar]
- 2.Treas LS, Wilkinson JM.. Basic nursing: concepts, skills & reasoning. Philadelphia (PA): F. A. Davis Company; 2014. p. 792–836. [Google Scholar]
- 3.Fujimoto E. The problem of using deltoid muscle for intramuscular injection. Aino J. 2007;6:49–53. [Google Scholar]
- 4.Beyea SC, Nicoll LH. Administration of medications via the intramuscular route: an integrative review of the literature and research-based protocol for the procedure. Appl Nurs Res. 1995;8:23–33. [DOI] [PubMed] [Google Scholar]
- 5.Davidson LT, Carter GT, Kilmer DD, Han JJ. Latrogenic axillary neuropathy after intramuscular injection of the deltoid muscle. Am J Phys Med Rehabil. 2007;86(6):507–11. doi: 10.1097/PHM.0b013e31805b7bcf. [DOI] [PubMed] [Google Scholar]
- 6.Nakatani T, Sanada H, Sugama J, Nagakawa T, Konya C, Ohkuwa M. Appropriate site for intramuscular injection in the deltoid muscle evaluated in 35 cadaverous arms. Memoirs Health Sci Med Kanazawa Univ. 2000;24:27–31. [Google Scholar]
- 7.Nakatani T, Kitagawa A, Kitayama Y, Tanaka A, Yamazaki M, Konya C, Tanaka S. The course of the axillary nerve projected on the skin covering the deltoid muscle of a cadaver for safety administering intramuscular injection in the deltoid muscle. J Tsuruma Health Sci Soc Kanazawa Univ. 2003;27:33–37. [Google Scholar]
- 8.Nakajima Y, Mukai K, Urai T, Takaoka K, Hirose T, Morishita K, Yamamoto T, Yoshida Y, Urai T, Nakatani T. Establishing a new appropriate intramuscular injection site in the deltoid muscle. Hum Vaccin Immunother. 2017;13:2123–29. doi: 10.1080/21645515.2017.1334747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nakajima Y, Mukai K, Kon Y, Iuchi T, Kitayama Y, Okuwa M, Nakatani T. A novel injection point for intramuscular injection in the gluteal muscle: an anatomical examination in cadavers in comparison with the well-known point of Clark. Struct Funct. 2012;10:108–14. [Google Scholar]
- 10.Hochstetter VAV. Über die intraglutäale injektion, ihre Komplikationen und deren Verhütung. Schweiz Med Wochenschr. 1954;84:1226–27. [PubMed] [Google Scholar]
- 11.Kaya N, Salmaslıoğlu A, Terzi B, Turan N, Acunaş B. The reliability of site determination methods in ventrogluteal area injection: a cross-sectional study. Int J Nurs Stud. 2015;52(1):355–60. doi: 10.1016/j.ijnurstu.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 12.Greenway K. Rituals in nursing: intramuscular injections. J Clin Nurs. 2014;23:3583–88. doi: 10.1111/jocn.12627. [DOI] [PubMed] [Google Scholar]
- 13.Satoh Y, Mori M. Evaluation of methods for identifying Gluteal intramuscular injection sites, focusing on distribution of the identified sites. Jpn J Nurs Sci. 2011;10(2):4–13. (in Japanese, abstract in English). doi: 10.18892/jsnas.10.2_4. [DOI] [Google Scholar]
- 14.Nakajima Y, Mukai K, Kon Y, Kitayama Y, Okuwa M, Ozaki N, Nakatani T. A study of safe site about intramuscular injection based on examination of a novel intramuscular injection point in the gluteal muscle as opposed to the well-known point of Clark. Struct Funct. 2012;10(2):65–72. doi: 10.11172/keitaikinou.10.65. [DOI] [Google Scholar]
- 15.Nakajima Y, Iuchi T, Mukai K, Komatsu E, Kitayama Y, Ozaki N, Nakatani T. Evaluation of the safety of a novel intramuscular injection point by insertion of gel and determination of the optimal depth of insertion in cadavers. Struct Funct. 2013;11(2):102–08. doi: 10.11172/keitaikinou.11.102. [DOI] [Google Scholar]
- 16.Nakajima Y, Mukai K, Komatsu E, Iuchi T, Kitayama Y, Nakatani T. A comparative study between a novel intramuscular injection point in the gluteal muscle at 0°, 45° and 90° hip joint flexion and the point of Clark in living bodies. Struct Funct. 2013;11(2):109–15. doi: 10.11172/keitaikinou.11.109. [DOI] [Google Scholar]
- 17.Nakagawa T, Ono Y, Hisanaga N, Iwata K, Sibata E, Kanada S, Kobayashi F, Sumi K, Moritani M, Mori M. A study of quadriceps contracture-causing factor by the analysis of muscle injection according to medical records. Nihon Eiseigaku Zasshi. 1988;43(3):724–35. doi: 10.1265/jjh.43.724. [DOI] [PubMed] [Google Scholar]
- 18.Schechter NL, Zempsky WT, Cohen LL, McGrath PJ, McMurtry CM, Bright NS. Pain reduction during pediatric immunizations: evidence-based review and recommendations. Pediatrics. 2007;119(5):e1184–98. doi: 10.1542/peds.2006-1107. [DOI] [PubMed] [Google Scholar]
- 19.Johnstone J, Hobbins S, Parekh D, O’Hickey S. Excess subcutaneous tissue may preclude intramuscular delivery when using adrenaline autoinjectors in patients with anaphylaxis. Allergy. 2015;70(6):703–06. doi: 10.1111/all.12595. [DOI] [PubMed] [Google Scholar]
- 20.Cocoman A, Murray J. Intramuscular injections: a review of best practice for mental health nurses. J Psychiatr Ment Health Nurs. 2008;15(5):424–34. doi: 10.1111/j.1365-2850.2007.01236.x. [DOI] [PubMed] [Google Scholar]
- 21.Rosdahl CB, Kowalski MT. Study guide to accompany textbook of basic nursing. 9th ed. Philadelphia (USA): Wolters Kluwer Health; 2007. p. 854–56. [Google Scholar]
- 22.University of Michigan comprehensive cancer center . Intramuscular (IM) self-injection. 2008. [accessed 2018 December16]. http://www.med.umich.edu/cancer/files/im-self-injection.pdf.
- 23.Tanioka T, Takase K, Yasuhara Y, Zhao Y, Noda C, Hisashige S, Locsin R. Efficacy and safety in intramuscular injection techniques using ultrasonographic data. Health. 2018;10(3):334–50. doi: 10.4236/health.2018.103027. [DOI] [Google Scholar]
- 24.Sarkar PK, Pan GD, Biswas SK, Mukherjee PK. Ideal technique and sites for intramuscular injection in infants and children. Pediatr Surg Int. 1989;4:140–42. doi: 10.1007/BF00181856. [DOI] [Google Scholar]
- 25.Burkhead WZ Jr, Scheinberg RR, Box G. Surgical anatomy of the axillary nerve. J Shoulder Elbow Surg. 1992;1(1):31–36. doi: 10.1016/S1058-2746(09)80014-1. [DOI] [PubMed] [Google Scholar]
- 26.Kido M, Matsuzaki A, Nakamura H, Irei Y, Kato K, Koga T. Position of the axillary nerve in the deltoid muscle. Shoulder Joint. 1996;20(1):27–29. doi: 10.11296/katakansetsu1977.20.1_27. [DOI] [Google Scholar]
- 27.Burusapat C, Nanasilp T, Kunaphensaeng P, Ruamthanthong A. Effect of atherosclerosis on the lateral circumflex femoral artery and its descending branch: comparative study to nonatherosclerotic risk. Plast Reconstr Surg Glob Open. 2016;4(9):e856. doi: 10.1097/GOX.0000000000000790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mahadevan V. Pelvic girdle and lower limb. In: Standring S, editor. Gray’s anatomy. 40th ed. London (UK): Churchill Livingstone Elsevier Ltd; 2008. p. 1327–464. [Google Scholar]
- 29.Rodger MA, King L. Drawing up and administering intramuscular injections: a review of the literature. J Adv Nurs. 2000;31:574–82. [DOI] [PubMed] [Google Scholar]
- 30.Walters MC, Furyk J. Pediatric intramuscular injections for developing world settings: a review of the literature for best practices. J Transcult Nurs. 2012;23(4):406–09. doi: 10.1177/1043659612451600. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- University of Michigan comprehensive cancer center . Intramuscular (IM) self-injection. 2008. [accessed 2018 December16]. http://www.med.umich.edu/cancer/files/im-self-injection.pdf.


