Supplemental digital content is available in the text.
Key words/Abbreviations: symptoms, child symptoms, psychological factors, parents, ADHD = attention-deficit/hyperactivity disorder, SDQ = Strengths and Difficulties Questionnaire
ABSTRACT
Objective
Parents make important treatment decisions for their children based on symptoms they perceive their child to be experiencing. Multiple psychological factors are associated with subjective symptom perception, but factors affecting perception of symptoms in others have been explored less. We systematically reviewed the literature to identify parent and child psychological factors associated with parental report of physical symptoms in their child.
Methods
We searched Embase, Ovid, PsycINFO, and Scopus for studies that investigated associations between psychological factors and parental report of symptoms in their child.
Results
Thirty-six citations reporting on 34 studies that assessed the association between parent or child psychological factors and parental report of physical symptoms in the child were included in the review. Three main factors were identified as being associated with parental symptom report. First, there was evidence for an association between parental symptom report and affect, in particular parent and child anxiety. Second, child behavioral and conduct problems, and temperament-related challenges (problems with feeding and sleeping) were associated with parental symptom report. Third, parental expectations and beliefs that symptoms would occur were associated with parental symptom report, although few studies investigated these associations.
Conclusions
Parent and child affect, and parental expectations and beliefs may influence parents’ cognition, causing them to pay more attention to their child, interpret their child’s behavior as symptomatic, and recall symptoms in the child. Given the importance of parental perception of symptoms in driving decisions around care, additional research in this field is needed.
INTRODUCTION
Symptom perception is a complex process. Although a clear correspondence between pathology and symptom occurrence and severity was once presumed, there is now convincing evidence that psychological factors, such as the wider context, the behavior of others, and the attitudes of the person involved, can influence whether one perceives a symptom (1). Models of subjective symptom perception postulate that bodily sensations lead to symptom experience through cognitive processing such as attention to the bodily sensation and interpretation of the sensation as a symptom (see Van den Bergh et al. (2) for summary). Psychological factors such as trait negativity, health anxiety, and learning are proposed to moderate these processes. However, relatively little research has investigated factors affecting the perception of symptoms in someone other than oneself, such as a child or dependent.
The ability to accurately identify symptoms in others is particularly important for parents. If parents are unable to accurately perceive symptoms in their child, they might incorrectly detect or miss signs of illness, symptoms of allergy or intolerance, or adverse effects of medications, and make inappropriate decisions for their child regarding medical care, life-style, or medication adherence as a result. Perceived food intolerance is one example of this. Approximately one-third of parents believe that their child has food sensitivity (3). However, most of these children do not undergo any formal testing of food allergy such as skin prick tests or oral food challenges. When formal testing does occur, the actual prevalence of food hypersensitivity is much lower (approximately 1.9%–4.5%) (3,4).
Although formal data are scarce, one study based on parental report estimated that 56% of children aged 3 to 5 years have experienced symptoms such as headache, stomach ache, tiredness, and dizziness in the last 14 days (5), a broadly similar rate to that seen in adults (6–8). However, agreement between parent-reported and child self-reported symptoms is varied. For example, one study found that, although parent-child agreement was relatively high for headache frequency, agreement was lower for other pain symptoms (9). Another study reported similar results, finding that parent and child symptom reports were highly correlated in children with recurrent stomach aches, but were less strongly correlated in well children and not correlated in children with emotional disorders (10). These results suggest that the process of parental perception of symptoms in one’s child is not straightforward and may depend in part on the type of symptom observed.
Multiple psychological factors have been identified as relevant in subjective symptom perception. In particular, heightened symptom expectations (11,12), psychological traits such as anxiety (13), depression (14), and negative affect (15), as well as beliefs relating to exposures that might trigger symptoms (16), have been associated with symptom reporting. However, it is unclear if the predictors of symptom perception in oneself are the same as those for perceiving symptoms in one’s child. While perception of symptoms in oneself is driven by detection of internal cues and bodily sensations, parental perception of symptoms in one’s child relies on external cues, such as observations of the child’s behavior, or listening to and assessing self-reports from the child. Parents of young or severely disabled children who are unable to verbalize their bodily sensations may have to rely solely on observation of the child’s behavior.
Psychological factors known to be influential in subjective symptom perception may also affect parents’ perception of symptoms in their child. Parents with higher trait negativity may pay more attention to their child’s behavior, be more likely to interpret their child’s behavior as symptomatic, and recall symptoms perceived in the child more readily or frequently (2). Parental expectations for symptoms to develop and beliefs about symptoms may influence these cognitive processes. The child’s behavior, affecting how they display symptoms experienced, may also influence parental symptom perception. It is likely that all three factors are important and interact with each other. To identify parent and child psychological factors that are associated with parent-report of physical symptoms in one’s child, we conducted a systematic review of the available literature. We used search terms relating to parents, perception of symptoms, and symptoms that children might commonly experience.
METHODS
We conducted a systematic review in accordance with PRISMA criteria (17) to identify factors associated with parental perception of symptoms in children. We searched Embase, Ovid, and PsycINFO through OvidSP, and Scopus. The final search used the terms (Parent* ADJ3 (perception OR perceive)) AND (side effect OR symptom* OR pain* OR asthma*). Asthma was included in the search terms because it is a condition experienced commonly in childhood, which was prevalent in our preliminary searches. Medical Subject Headings terms were also searched where possible. Databases were searched from inception to July 12, 2018. References and forward citations of included articles were also searched.
Inclusion Criteria
The following inclusion criteria were used:
Participants: Studies were included if they investigated parents of children aged 0 to 18 years. Studies were excluded if parents discussed symptom report outcome measures with their child or if it was unclear whether the parent or the child completed outcome measures.
Predictors/Exposures: Studies were included if they investigated the association between psychological or social factors and parental report of symptoms.
Outcomes: Studies were included if the outcome was parental report of physical symptoms in the child, including pain, asthmatic symptoms, adverse effects from medication, or perceived allergy or food intolerance. Outcomes relating to parental contact with health professionals after symptom perception were excluded. Outcomes based on parental report of a diagnosis for the child by a health care practitioner were also excluded.
Study reporting: Only studies published in English were included.
Data Extraction
We extracted information on study design, inclusion criteria, number of participants, child age, symptom type, symptom measure used, and predictors of symptom report.
Risk of Bias
Risk of bias was measured using an amended version of the Downs and Black checklist (18), as in previous systematic reviews (19). The Downs and Black checklist assesses the methodological quality of randomized and non-randomized studies (18). This version did not include items referring to interventions because they were not relevant for any included study. The Downs and Black checklist has been validated (20) and is suitable for use in systematic reviews (21). Five aspects of the studies’ methods were assessed: reporting (out of 10), internal validity (bias; out of 3), confounding (selection bias; out of 3), external validity (out of 2), and statistical power (1 item). Scores were added to give a total of up to 19. We rated studies as good quality if they scored 16 or over, moderate quality if they scored 11 to 15, and poor quality if they scored 10 or less. Studies scored poorly for reporting if they scored 6 or lower; internal validity (bias), confounding (selection bias) and external validity if they scored 1 or lower; and if they did not include a justification for the sample size used.
Procedure
L.E.S. came up with the search terms, carried out the search, screened articles, extracted data, and completed risk of bias assessment with guidance from J.R. All authors helped devise the idea for the review, assisted with interpretation of results, and critically reviewed and revised the manuscript. Factors were grouped according to psychosocial factor.
RESULTS
Study Characteristics
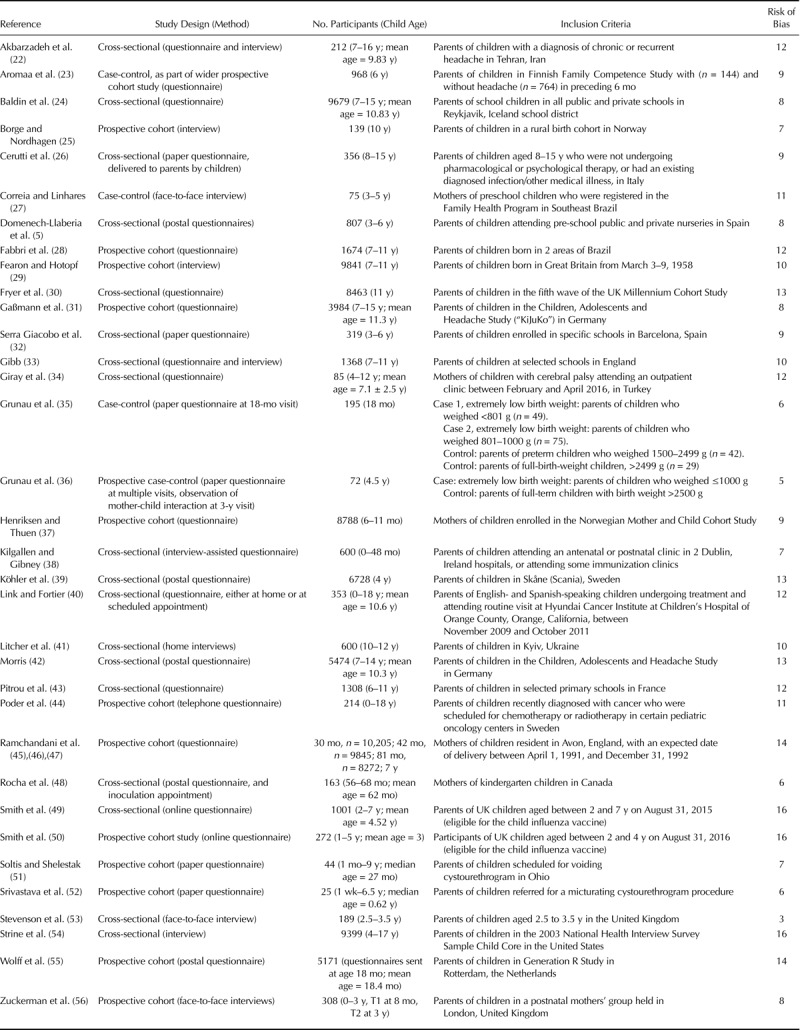
A total of 3765 citations were found by the original search. After removing duplicates, 3232 citations remained. After title, abstract, and full-text screening, seven citations remained. Reference searching and forward citation tracking identified a further 29 citations that met the inclusion criteria, giving a total of 36 citations reporting on 34 studies (Figure 1). Twenty-three studies used a cross-sectional design, eight used a cohort design, and three used case-control design (Table 1). Nine studies investigated somatic symptoms in general, with a further nine investigating solely headache, three investigating stomach ache, and two investigating both headache and stomach ache; one investigated recurrent symptoms (Supplemental Digital Content, http://links.lww.com/PSYMED/A603). Six studies investigated pain. Two studies investigated the incidence of symptoms in response to vaccination, one investigated symptoms attributed to food allergy, and one investigated symptoms attributed by parents to various ailments such as the common cold.
FIGURE 1.
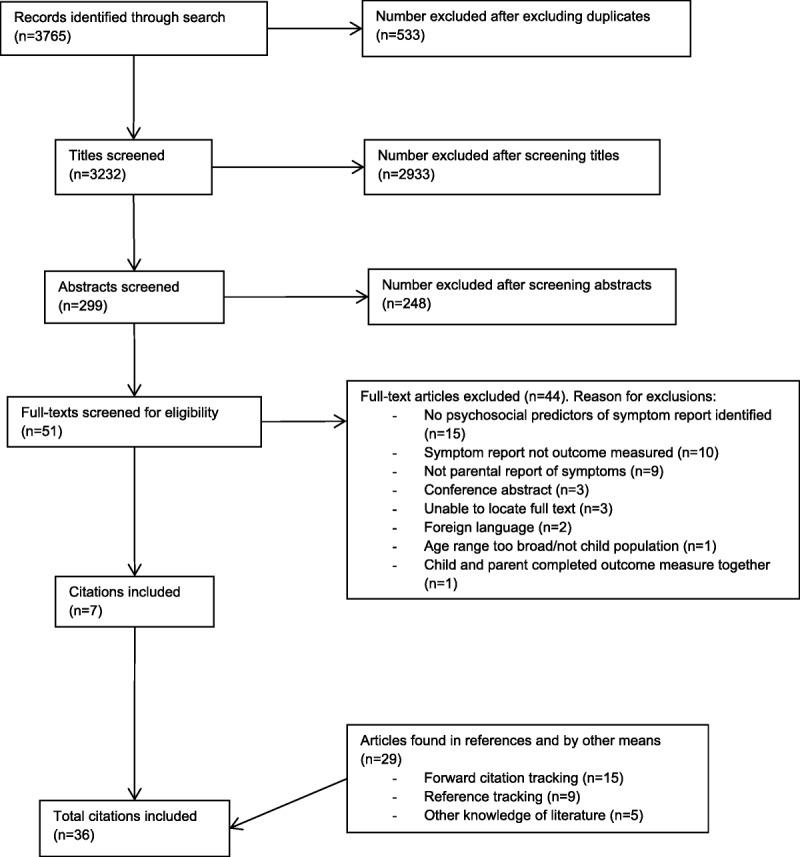
Flowchart depicting the selection of studies included in the systematic review with reasons for exclusion.
TABLE 1.
Methods of Articles Included in Systematic Review
Risk of Bias
Scores ranged between 3 and 16 of a possible 19 (Table 1). Most studies were poor quality (n = 19), with 12 moderate-quality studies. There were three good quality studies. Only four studies gave a justification for the sample size used (28,42,49,50) (Figure 2). With respect to internal validity, 10 studies scored poorly for confounding (26,32,33,35,36,41,48,51–53) and 13 scored poorly for bias (5,23,25,26,32,35,36,38,41,48,52,53,56). External validity was acceptable in only four studies (30,38,49,54). Reporting was poor in 24 studies (5,22–38,44,48,51–53,56).
FIGURE 2.
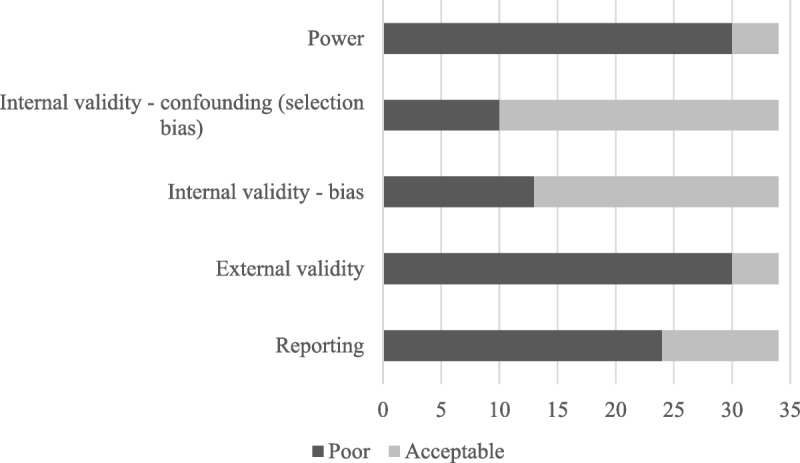
Chart indicating number of studies displaying different aspects of risk of bias.
Only studies that were moderate or good quality are reported narratively.
Instruments Used to Measure Parental Perception of Symptoms
Studies used many different measures of parental perception of symptoms. Few studies used validated questionnaires to measure parental perception of symptoms. Three studies used the parent-report version of the Children’s Somatization Inventory (57), with another study using the short version; one study used the Child Behaviour Checklist (58); one study used a modified version of the Memorial Symptom Assessment Scale (59); and another used the Non-Communicating Children’s Pain Checklist – Revised (60). All other studies used their own measure of parental perception of symptoms; this was often a single item asking how frequently the child had experienced a given symptom over a certain period (see supplementary materials for full details, http://links.lww.com/PSYMED/A603).
Predictors of Parental Symptom Report
Parent and child psychosocial factors associated with parental report of symptoms are reported in Table 2. Where studies used adjusted analyses, only these are reported. Many studies used the Strengths and Difficulties Questionnaire (61), which is made up of five components: emotional problems, conduct problems, hyperactivity-inattention, peer problems, and prosocial behavior. Where possible, we have reported each component individually.
TABLE 2.
Summary of Studies Investigating the Association Between Psychosocial Characteristics and Parental Report of Physical Symptoms in the Child
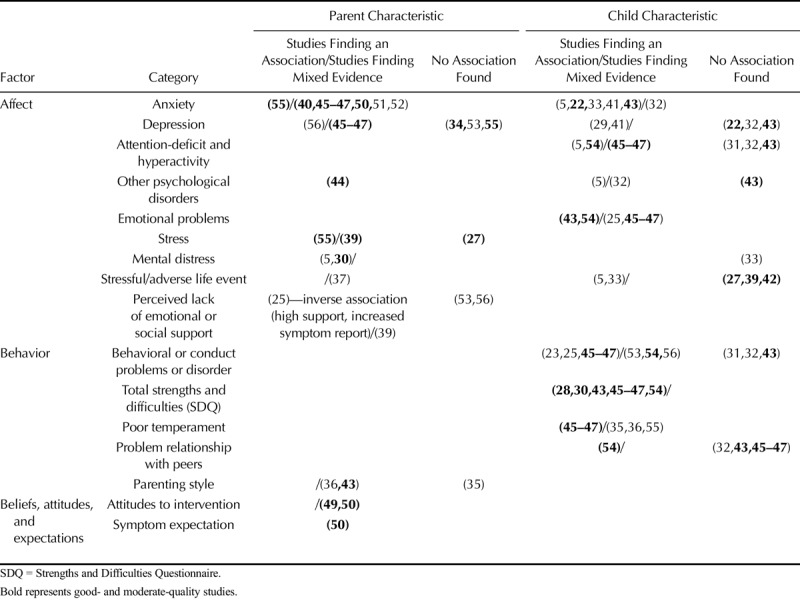
Parent Psychosocial Characteristics
There was some evidence for associations between parental affect and parental symptom report. Evidence was stronger for the role of parental anxiety than other psychological traits or stressful events. Studies measured trait anxiety, apart from two which investigated anticipatory and experienced anxiety (51,52), and another which used the Crown-Crisp index (45–47). One study found an association between parent anxiety and report of somatic symptoms (55), whereas three studies found mixed evidence of an association with increased report of child chronic pain, recurrent stomach aches, and perception of adverse effects from influenza (40,45–47,50). One study found evidence for an association between maternal depression and reporting of recurrent child symptoms (45–47), whereas two studies (34,55) found no association between parental depression and presence and frequency of parent-reported somatic complaints and child pain. Parental post-traumatic stress disorder was associated with symptom report (44). There was mixed evidence for an association between parent distress or stress and parental symptom report. Distress was associated with frequency of parent-reported pain in one study (30). Three studies investigated the association between parental stress and parent-reported symptoms. One investigating somatic symptoms found an association (55); one investigating recurrent stomach aches found mixed evidence for an association (39); and one investigating general physical symptoms found no association (27). Paternal, but not maternal, low emotional support was associated with report of recurrent stomach aches (39).
Few studies investigated the association between parental behavioral factors and parental symptom report. One study found an association between punitive behaviors and less frequent report of headaches (43).
There was some evidence for an association between negative parental beliefs and attitudes and parental symptom report. Two studies investigated the association between parental reporting of adverse effects from the child influenza vaccine and multiple parental beliefs, such as believing that vaccines cause adverse effects, and attitudes, such as not liking vaccines in general (49,50). Beliefs and attitudes were associated with parental report of adverse effects in both studies (see supplementary materials for full details, http://links.lww.com/PSYMED/A603). One of these studies also investigated parents’ expectation that their child would experience a symptom, finding an association between parental expectation of adverse effects and later adverse effect reporting (50).
Child Psychosocial Characteristics
There was mixed evidence for associations between child affect and parental symptom report. Evidence was strongest for an association between parental symptom report and child anxiety, emotional problems, and attention-deficit/hyperactivity disorder (ADHD). Child emotional problems were associated with parent-reported frequent or severe headaches in two studies (43,54), whereas another study found mixed evidence for an association with parent-report of recurrent symptoms (45–47). Studies investigating child anxiety used measures that could be used as diagnostic tools for general anxiety disorder. Increased parent-reported presence, frequency, and severity of headaches were associated with child anxiety in two studies (22,43). One study investigated parent-reported child anxiety (22), whereas the other investigated child-reported anxiety (43). One study found an association between ADHD and frequency and severity of parent-reported headache (54), whereas another found mixed evidence for an association with recurrent stomach ache (45–47). One study found no evidence for an association between ADHD and frequency of parent-reported headache (43). Two studies found no association between child depression (parent-reported child depression (22), child-reported depression (43)) and presence, frequency, and severity of parent-reported headache. Parent-reported anxiety and depression were not associated with parental report of recurrent headache (42). Three studies found no association between adverse or stressful life events and parent-reported headache or stomach ache (27,39,42). There was also no evidence for an association between oppositional defiant disorder, social phobia, or separation anxiety and parent-reported frequent headache (43).
There was some evidence for an association between child behavioral factors and parental symptom report. All studies that investigated whether total high difficulties on the Strengths and Difficulties Questionnaire were associated with parental symptom report found evidence for an association (28,30,43,45–47,54). Conduct problems were associated with parent-reported recurrent stomach ache in one study (45–47), whereas another investigating parent-reported headaches found mixed evidence (54). Temperament-related challenges, such as problems with feeding or sleeping, were also associated with parent-reported recurrent stomach ache (45–47). Evidence for an association between child problematic relationships with peers and parental symptom report was mixed, with one study investigating parent-reported headaches finding an association (54); two further studies investigating parent-reported headache and recurrent abdominal pain found no association (43,45–47).
DISCUSSION
Although mechanisms underlying symptom perception in oneself are more clearly understood, less research has explored psychological factors associated with parental perception and report of symptoms in one’s child. Our review identified three broad categories of factors affecting parental report of symptoms: affect, behavior, and expectations and beliefs about symptoms. These build upon categories previously identified in the literature (62).
There was good evidence for an association between parental anxiety and report of symptoms in the child, but less evidence for associations with other psychological traits. In models of subjective symptom perception (e.g., Ref. (2)), anxiety is thought to heighten attention to bodily sensations and lower the threshold at which sensations are detected (13,63). In parental perception of symptoms in one’s child, heightened parental anxiety may increase attention to the child’s behavior and may cause a more negative interpretation of the reasons underlying ambiguous behaviors. There was also evidence that child anxiety, as well as emotional problems and ADHD, were associated with parental report of physical symptoms. Because somatic symptoms are common in children with anxiety (64) and other emotional and behavioral disorders (65), this finding is perhaps unsurprising.
Most of the research investigating the association between behavioral factors and parental symptom report has focused on child, rather than parent, behavioral factors. How child behavioral difficulties, such as having problems with peers, may affect parental symptom report is poorly understood. Although all studies investigating child temperament in the review found an association with parent-reported symptoms, no rationale was given for investigating these factors. One mechanism that may explain this pattern of findings is that children perceived as “difficult” may verbally report more symptoms, leading to increased parental symptom report. In addition, parents may pay more attention to their child’s behavior if he/she are perceived as “difficult”, causing parents to notice and report more symptoms. Children may also behave differently in the presence of their parents, leading to increased possibility of symptom detection by parents. For example, children display more pain in the presence of a parent than a stranger (66). Better quality research is necessary to clarify the nature of, and reasons underlying, associations between child behavioral factors and parental symptom report.
The effects of some psychosocial factors on parental symptom report were conspicuous by their absence in our review. In particular, only one study investigated the effect of parental expectation of symptoms (50). Given the wealth of evidence suggesting that expectation influences symptom perception in oneself (11,12,67,68), it is surprising that so few studies have investigated the influence of parental expectation on parent-reported symptoms. One possible explanation for this dearth of research is that studies have so far focused on finding factors associated with increases in symptoms experienced by the child rather than parental report of symptoms. However, given that decision making about medical treatments or potential life-style adjustments will be made based on parental perception and recall of symptoms, it is important to identify factors that may influence this process.
Limitations of Studies Included in the Review
Most studies included in our review were poor quality. In particular, studies fell short on reporting and external validity. Studies used a wide range of questions to assess parental report of symptoms in the child, with very few studies using validated measures. Studies were also heterogeneous with regard to their populations, investigating parents of children of different ages. Statistical analyses were also heterogeneous, with some studies using inappropriate tests, not reporting statistical tests used (53,56), or using small sample sizes. Symptom report was also defined differently by different studies, with some studies using higher thresholds for symptom report than others. Studies included in the review used many different scales to measure the same construct; this was particularly notable for temperament and behavior (69) and made it difficult to compare results between studies.
Limitations of the Review
Several limitations of our review should also be considered. First, symptoms perceived by parents in this review were wide ranging. We were unable to investigate whether predictive factors differed in relation to different symptoms. However, literature investigating the nocebo effect supports the notion that factors such as expectations and anxiety are associated with perceiving a wide range of subjective symptoms (11).
Second, we did not differentiate predictors of parent-report of child symptoms by age of the child. This was due to the wide age range used in some studies (e.g., 0–18 years) and the small number of studies investigating each factor. Although it is likely that some child psychological factors, such as school-based stressors, would be more prevalent in older rather than younger children, no studies included in the review investigated these. The lack of comparable measures for psychosocial factors, such as temperament, across age groups is recognized as a problem for the identification, and relative importance, of factors associated with medically unexplained symptoms in children and adolescents (70).
Third, few studies investigated the same factors, meaning that our conclusions for some risk factors are based on limited results and should be treated with caution.
Fourth, it was notable that only seven citations were identified through our search strategy, with most citations being found through forward citation and reference tracking. To date, parental perception of child symptoms has rarely been studied as a topic in its own right and has no specific easily searchable terminology, making relevant data difficult to find. It is likely that other studies investigating relevant risk factors exist, but we were unable to locate them.
Fifth, we restricted our search to psychosocial predictors of parental symptom report. Other studies exist investigating personal and clinical factors such as breastfeeding (71), smoke exposure (72), exposure to indoor dampness and mold (73), attending day care (74), and number of siblings (75), particularly in relation to child asthma and allergic symptoms. A full model of parental symptom perception may need to account for these factors.
Sixth, we used parental report of symptoms as a proxy for parental perception of symptoms. Retrospective symptom reports are often biased compared with momentary symptom assessments, with the former often leading to greater estimates of symptoms (76). This is likely due to multiple memory biases playing a role in retrospective reports [see Van den Bergh and Walentynowicz (76) for a review]. Because diary methodologies were not used by any of the studies included in the review, parental report of symptoms may have been affected by these factors and therefore may not have mapped exactly onto symptom perception. However, because retrospective parental reports of symptoms are commonly relied upon by physicians when making diagnoses for children and by parents when making health-related decisions for their child, it is important to identify psychological factors that may influence parental report of symptoms in the child.
Lastly, an important question to consider is whether parent and child psychosocial factors are associated with increased symptoms experienced by the child or increased parental detection of symptoms, irrespective of the child’s subjective experience. We were unable to differentiate between these outcomes. This distinction has already been identified as a concern in the literature (55), and it is likely that both mechanisms are relevant (40,45,46,55).
CONCLUSIONS
Psychological factors from three categories were found to be associated with parental report of symptoms: affect; behavior; and expectations, attitudes, and beliefs. The influence of both parent and child affect was investigated. Factors most often associated with parental report of symptoms were parent anxiety and stress, and child anxiety, emotional problems, and ADHD. Behavioral factors were mostly investigated with reference to the child, with problems in conduct and temperament being consistently associated with greater parental report of symptoms. Beliefs, attitudes, and symptom expectations may also influence parent symptom report, but there was a dearth of research investigating these factors. Better quality research using more standardized methods and measures is needed to more fully understand the impact of, and mechanisms through which, psychosocial factors influence parental report of symptoms.
Acknowledgments
The authors would like to thank Dr. Richard Amlôt for his help with reviewing the manuscript.
Acknowledgments
Source of Funding and Conflicts of Interest: L.E.S. was funded by the Economic and Social Research Council through a Doctoral Training Centre Studentship. The research was funded by the National Institute for Health Research Health Protection Research Unit in Emergency Preparedness and Response at King’s College London in partnership with Public Health England, in collaboration with the University of East Anglia and Newcastle University. The views expressed are those of the authors and not necessarily those of the NHS, the National Institute for Health Research, the Department of Health, or Public Health England. The authors have no conflicts of interest relevant to this article to disclose.
The authors have no financial relationships relevant to this article to disclose.
Footnotes
Supplemental Content
REFERENCES
- 1.Cioffi D. Beyond attentional strategies: cognitive-perceptual model of somatic interpretation. Psychol Bull 1991;109:25–41. [DOI] [PubMed] [Google Scholar]
- 2.Van den Bergh O, Witthöft M, Petersen S, Brown RJ. Symptoms and the body: taking the inferential leap. Neurosci Biobehav Rev 2017;74(pt A):185–203. [DOI] [PubMed] [Google Scholar]
- 3.Dean T. Prevalence and incidence of food allergies and food intolerance—a prospective birth cohort study to establish the incidence and a concurrent cross-sectional study of whole population cohorts at 1,2,3,6,11 and 15. 2006.
- 4.Roehr CC, Edenharter G, Reimann S, Ehlers I, Worm M, Zuberbier T, Niggemann B. Food allergy and non-allergic food hypersensitivity in children and adolescents. Clin Exp Allergy 2004;34:1534–41. [DOI] [PubMed] [Google Scholar]
- 5.Domenech-Llaberia E, Jane C, Canals J, Ballespi S, Esparo G, Garralda E. Parental reports of somatic symptoms in preschool children: prevalence and associations in a Spanish sample. J Am Acad Child Adolesc Psychiatry 2004;43:598–604. [DOI] [PubMed] [Google Scholar]
- 6.Eriksen HR, Ihlebaek C. Subjective health complaints. Scand J Psychol 2002;43:101–3. [DOI] [PubMed] [Google Scholar]
- 7.Eriksen HR, Svendsrod R, Ursin G, Ursin H. Prevalence or subjective health complaints in the Nordic European countries in 1993. Eur J Public Health 1998;8:294–8. [Google Scholar]
- 8.Ihlebaek C, Eriksen HR, Ursin H. Prevalence of subjective health complaints (SHC) in Norway. Scand J Public Health 2002;30:20–9. [PubMed] [Google Scholar]
- 9.Kroner-Herwig B, Morris L, Heinrich M, Gassmann J, Vath N. Agreement of parents and children on characteristics of pediatric headache, other pains, somatic symptoms, and depressive symptoms in an epidemiologic study. Clin J Pain 2009;25:58–64. [DOI] [PubMed] [Google Scholar]
- 10.Garber J, Van Slyke DA, Walker LS. Concordance between mothers’ and children’s reports of somatic and emotional symptoms in patients with recurrent abdominal pain or emotional disorders. J Abnorm Child Psychol 1998;26:381–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Webster RK, Weinman J, Rubin GJ. A systematic review of factors that contribute to nocebo effects. Health Psychol 2016;35:1334–55. [DOI] [PubMed] [Google Scholar]
- 12.Barsky AJ, Saintfort R, Rogers MP, Borus JF. Nonspecific medication side effects and the nocebo phenomenon. JAMA 2002;287:622–7. [DOI] [PubMed] [Google Scholar]
- 13.Henningsen P, Zimmermann T, Sattel H. Medically unexplained physical symptoms, anxiety, and depression: a meta-analytic review. Psychosom Med 2003;65:528–33. [DOI] [PubMed] [Google Scholar]
- 14.Linton SJ. A review of psychological risk factors in back and neck pain. Spine (Phila Pa 1976) 2000;25:1148–56. [DOI] [PubMed] [Google Scholar]
- 15.Watson D, Pennebaker JW. Health complaints, stress, and distress: exploring the central role of negative affectivity. Psychol Rev 1989;96:234–54. [DOI] [PubMed] [Google Scholar]
- 16.Cooper V, Metcalf L, Versnel J, Upton J, Walker S, Horne R. Patient-reported side effects, concerns and adherence to corticosteroid treatment for asthma, and comparison with physician estimates of side-effect prevalence: a UK-wide, cross-sectional study. NPJ Prim Care Respir Med 2015;25:15026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52:377–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith LE, Amlôt R, Weinman J, Yiend J, Rubin GJ. A systematic review of factors affecting vaccine uptake in young children. Vaccine 2017;35:6059–69. [DOI] [PubMed] [Google Scholar]
- 20.Petticrew M, Roberts H. Systematic Reviews in the Social Sciences: A Practical Guide. Malden, MA; Oxford: Blackwell; 2006. xv, 336 p. p. [Google Scholar]
- 21.Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, Petticrew M, Altman DG, International Stroke Trial Collaborative Group, European Carotid Surgery Trial Collaborative Group. Evaluating non-randomised intervention studies. Health Technol Assess 2003;7:iii-x, 1–173. [DOI] [PubMed] [Google Scholar]
- 22.Akbarzadeh G, Daniali H, Javdzadh M, Caes L, Ranjbar S, Habibi M. The relationship of parental pain catastrophizing with parents reports of children’s anxiety, depression, and headache severity. Iran J Child Neurol 2018;12:55–66. [PMC free article] [PubMed] [Google Scholar]
- 23.Aromaa M, Rautava P, Helenius H, Sillanpaa ML. Factors of early life as predictors of headache in children at school entry. Headache 1998;38:23–30. [DOI] [PubMed] [Google Scholar]
- 24.Baldin E, Ludvigsson P, Mixa O, Hesdorffer DC. Prevalence of recurrent symptoms and their association with epilepsy and febrile seizure in school-aged children: a community-based survey in Iceland. Epilepsy Behav 2012;23:315–9. [DOI] [PubMed] [Google Scholar]
- 25.Borge AI, Nordhagen R. Development of stomach-ache and headache during middle childhood: co-occurrence and psychosocial risk factors. Acta Paediatr 1995;84:795–802. [DOI] [PubMed] [Google Scholar]
- 26.Cerutti R, Spensieri V, Valastro C, Presaghi F, Canitano R, Guidetti V. A comprehensive approach to understand somatic symptoms and their impact on emotional and psychosocial functioning in children. PLoS One 2017;12:e0171867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Correia LL, Linhares MB. Temperament and behavioral problems of preschool children with headache—a controlled study. Span J Psychol 2013;16:E34. [DOI] [PubMed] [Google Scholar]
- 28.Fabbri CE, Barbieri MA, Silva AM, Gutierrez MR, Bettiol H, Speciali JG, Rona RJ. Maternal smoking during pregnancy and primary headache in school-aged children: a cohort study. Cephalalgia 2012;32:317–27. [DOI] [PubMed] [Google Scholar]
- 29.Fearon P, Hotopf M. Relation between headache in childhood and physical and psychiatric symptoms in adulthood: national birth cohort study. BMJ 2001;322:1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fryer BA, Cleary G, Wickham SL, Barr BR, Taylor-Robinson DC. Effect of socioeconomic conditions on frequent complaints of pain in children: findings from the UK Millennium Cohort Study. BMJ Paediatr Open 2017;1:e000093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gaßmann J, Barke A, van Gessel H, Kröner-Herwig B. Sex-specific predictor analyses for the incidence of recurrent headaches in German schoolchildren. Psychosoc Med 2012;9:Doc03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Serra Giacobo R, Jané MC, Bonillo A, Ballespí S, Díaz-Regañon N. Somatic symptoms, severe mood dysregulation, and aggressiveness in preschool children. Eur J Pediatr 2012;171:111–9. [DOI] [PubMed] [Google Scholar]
- 33.Gibb J. Communication and confiding in mothers (and others): relationships with anxiety and somatic symptoms among children aged seven to eleven. London: University of London; 2014. [Google Scholar]
- 34.Giray E, Şimşek HI, Aydoğduoğlu M, Kangal AÇ, Çelik A, Kurt C, Karadağ Saygi E. Pain evaluation in a sample of Turkish children with cerebral palsy and its association with dependency level, verbal abilities, and the quality of life of patients and sociodemographic status, depression, and quality of life of their caregivers. Turk J Phys Med Rehabil 2018;64:222–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grunau RV, Whitfield MF, Petrie JH. Pain sensitivity and temperament in extremely low-birth-weight premature toddlers and preterm and full-term controls. Pain 1994;58:341–6. [DOI] [PubMed] [Google Scholar]
- 36.Grunau RV, Whitfield MF, Petrie JH, Fryer EL. Early pain experience, child and family factors, as precursors of somatization: a prospective study of extremely premature and fullterm children. Pain 1994;56:353–9. [DOI] [PubMed] [Google Scholar]
- 37.Henriksen RE, Thuen F. Marital quality and stress in pregnancy predict the risk of infectious disease in the offspring: the Norwegian Mother and Child Cohort Study. PLoS One 2015;10:e0137304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kilgallen I, Gibney MJ. Parental perception of food allergy or intolerance in children under 4 years of age. J Hum Nutr Diet 1996;9:473–8. [Google Scholar]
- 39.Köhler M, Emmelin M, Rosvall M. Parental health and psychosomatic symptoms in preschool children: a cross-sectional study in Scania, Sweden. Scand J Public Health 2017;45:846–53. [DOI] [PubMed] [Google Scholar]
- 40.Link CJ, Fortier MA. The relationship between parent trait anxiety and parent-reported pain, solicitous behaviors, and quality of life impairment in children with cancer. J Pediatr Hematol Oncol 2016;38:58–62. [DOI] [PubMed] [Google Scholar]
- 41.Litcher L, Bromet E, Carlson G, Gilbert T, Panina N, Golovakha E, Goldgaber D, Gluzman S, Garber J. Ukrainian application of the Children’s Somatization Inventory: psychometric properties and associations with internalizing symptoms. J Abnorm Child Psychol 2001;29:165–75. [DOI] [PubMed] [Google Scholar]
- 42.Morris L. Weekly Headache in Children and Adolescents: Biopsychosocial Correlates and Their Specificity. Göttingen: Georg-August-Universität zu Göttingen; 2006. [Google Scholar]
- 43.Pitrou I, Shojaei T, Chan-Chee C, Wazana A, Boyd A, Kovess-Masfety V. The associations between headaches and psychopathology: a survey in school children. Headache 2010;50:1537–48. [DOI] [PubMed] [Google Scholar]
- 44.Poder U, Ljungman G, von Essen L. Parents’ perceptions of their children’s cancer-related symptoms during treatment: a prospective, longitudinal study. J Pain Symptom Manage 2010;40:661–70. [DOI] [PubMed] [Google Scholar]
- 45.Ramchandani PG, Hotopf M, Sandhu B, Stein A, ALSPAC Study Team. The epidemiology of recurrent abdominal pain from 2 to 6 years of age: results of a large, population-based study. Pediatrics 2005;116:46–50. [DOI] [PubMed] [Google Scholar]
- 46.Ramchandani PG, Stein A, Hotopf M, Wiles NJ, ALSPAC STUDY TEAM. Early parental and child predictors of recurrent abdominal pain at school age: results of a large population-based study. J Am Acad Child Adolesc Psychiatry 2006;45:729–36. [DOI] [PubMed] [Google Scholar]
- 47.Ramchandani PG, Fazel M, Stein A, Wiles N, Hotopf M. The impact of recurrent abdominal pain: predictors of outcome in a large population cohort. Acta Paediatr 2007;96:697–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rocha EM, Prkachin KM, Beaumont SL, Hardy CL, Zumbo BD. Pain reactivity and somatization in kindergarten-age children. J Pediatr Psychol 2003;28:47–57. [DOI] [PubMed] [Google Scholar]
- 49.Smith LE, Webster RK, Weinman J, Amlôt R, Yiend J, Rubin GJ. Psychological factors associated with uptake of the childhood influenza vaccine and perception of post-vaccination side-effects: a cross-sectional survey in England. Vaccine 2017;35:1936–45. [DOI] [PubMed] [Google Scholar]
- 50.Smith LE, Weinman J, Amlôt R, Yiend J, Rubin GJ. Parental expectation of side effects following vaccination is self-fulfilling: a prospective cohort study. Ann Behav Med 2019;53:267–82. [DOI] [PubMed] [Google Scholar]
- 51.Soltis CM, Shelestak D. Children, voiding cystourethrograms, and family perceptions. J Radiol Nurs 2011;30:153–7. [Google Scholar]
- 52.Srivastava T, Betts G, Rosenberg AR, Kainer G. Perception of fear, distress and pain by parents of children undergoing a micturating cystourethrogram: a prospective study. J Paediatr Child Health 2001;37:271–3. [DOI] [PubMed] [Google Scholar]
- 53.Stevenson J, Simpson J, Bailey V. Research note: recurrent headaches and stomachaches in preschool children. J Child Psychol Psychiatry 1988;29:897–900. [DOI] [PubMed] [Google Scholar]
- 54.Strine TW, Okoro CA, McGuire LC, Balluz LS. The associations among childhood headaches, emotional and behavioral difficulties, and health care use. Pediatrics 2006;117:1728–35. [DOI] [PubMed] [Google Scholar]
- 55.Wolff N, Darlington AS, Hunfeld J, Verhulst F, Jaddoe V, Hofman A, Passchier J, Tiemeier H. Determinants of somatic complaints in 18-month-old children: the generation R study. J Pediatr Psychol 2010;35:306–16. [DOI] [PubMed] [Google Scholar]
- 56.Zuckerman B, Stevenson J, Bailey V. Stomachaches and headaches in a community sample of preschool children. Pediatrics 1987;79:677–82. [PubMed] [Google Scholar]
- 57.Walker LS, Beck JE, Garber J, Lambert W. Children’s Somatization Inventory: psychometric properties of the revised form (CSI-24). J Pediatr Psychol 2009;34:430–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms and Profiles. Burlington: University of Vermont: Research Center for Children, Youth, and Families; 2000. [Google Scholar]
- 59.Collins JJ, Byrnes ME, Dunkel IJ, Lapin J, Nadel T, Thaler HT, Polyak T, Rapkin B, Portenoy RK. The measurement of symptoms in children with cancer. J Pain Symptom Manage 2000;19:363–77. [DOI] [PubMed] [Google Scholar]
- 60.Breau LM, McGrath PJ, Camfield CS, Finley GA. Psychometric properties of the Non-communicating Children’s Pain Checklist – Revised. Pain 2002;99:349–57. [DOI] [PubMed] [Google Scholar]
- 61.Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581–6. [DOI] [PubMed] [Google Scholar]
- 62.Husain K, Browne T, Chalder T. A review of psychological models and interventions for medically unexplained somatic symptoms in children. Child Adolesc Ment Health [Internet] 2007;12:2–7. Available at: http://onlinelibrary.wiley.com/doi/10.1111/j.1475-3588.2006.00419.x/abstract. https://onlinelibrary.wiley.com/doi/pdf/10.1111/j.1475-3588.2006.00419.x. [DOI] [PubMed] [Google Scholar]
- 63.Kolk AM, Hanewald GJ, Schagen S, Gijsbers van Wijk CM. A symptom perception approach to common physical symptoms. Soc Sci Med 2003;57:2343–54. [DOI] [PubMed] [Google Scholar]
- 64.Ginsburg GS, Riddle MA, Davies M. Somatic symptoms in children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry 2006;45:1179–87. [DOI] [PubMed] [Google Scholar]
- 65.Masi G, Favilla L, Millepiedi S, Mucci M. Somatic symptoms in children and adolescents referred for emotional and behavioral disorders. Psychiatry 2000;63:140–9. [DOI] [PubMed] [Google Scholar]
- 66.Vervoort T, Goubert L, Eccleston C, Verhoeven K, De Clercq A, Buysse A, Crombez G. The effects of parental presence upon the facial expression of pain: the moderating role of child pain catastrophizing. Pain 2008;138:277–85. [DOI] [PubMed] [Google Scholar]
- 67.Faasse K, Grey A, Jordan R, Garland S, Petrie KJ. Seeing is believing: impact of social modeling on placebo and nocebo responding. Health Psychol 2015;34:880–5. [DOI] [PubMed] [Google Scholar]
- 68.Faasse K, Parkes B, Kearney J, Petrie K. The influence of social modeling, gender, and empathy on treatment side effects. Ann Behav Med 2018;52:560–70. [DOI] [PubMed] [Google Scholar]
- 69.Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine (Phila Pa 1976) 2002;27:E109–20. [DOI] [PubMed] [Google Scholar]
- 70.Eminson DM. Medically unexplained symptoms in children and adolescents. Clin Psychol Rev 2007;27:855–71. [DOI] [PubMed] [Google Scholar]
- 71.Lodge CJ, Tan DJ, Lau MX, Dai X, Tham R, Lowe AJ, Bowatte G, Allen KJ, Dharmage SC. Breastfeeding and asthma and allergies: a systematic review and meta-analysis. Acta Paediatr 2015;104:38–53. [DOI] [PubMed] [Google Scholar]
- 72.Burke H, Leonardi-Bee J, Hashim A, Pine-Abata H, Chen Y, Cook DG, Britton JR, McKeever TM. Prenatal and passive smoke exposure and incidence of asthma and wheeze: systematic review and meta-analysis. Pediatrics 2012;129:735–44. [DOI] [PubMed] [Google Scholar]
- 73.Jaakkola MS, Quansah R, Hugg TT, Heikkinen SA, Jaakkola JJ. Association of indoor dampness and molds with rhinitis risk: a systematic review and meta-analysis. J Allergy Clin Immunol 2013;132:1099–110.e18. [DOI] [PubMed] [Google Scholar]
- 74.Ochoa Sangrador C, Vazquez Blanco A. Day-care center attendance and risk of asthma—a systematic review. Allergol Immunopathol 2018;46:578–84. [DOI] [PubMed] [Google Scholar]
- 75.Karmaus W, Botezan C. Does a higher number of siblings protect against the development of allergy and asthma? A review. J Epidemiol Community Health 2002;56:209–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Van den Bergh O, Walentynowicz M. Accuracy and bias in retrospective symptom reporting. Curr Opin Psychiatry 2016;29:302–8. [DOI] [PubMed] [Google Scholar]


