Indigenous women are at increased risk for severe maternal morbidity and mortality, particularly those who live in rural areas.
Abstract
OBJECTIVE:
To describe delivery-related severe maternal morbidity and mortality among indigenous women compared with non-Hispanic white (white) women, distinguishing rural and urban residents.
METHODS:
We used 2012–2015 maternal hospital discharge data from the National Inpatient Sample to conduct a pooled, cross-sectional analysis of indigenous and white patients who gave birth. We used weighted multivariable logistic regression and predictive population margins to measure health conditions and severe maternal morbidity and mortality (identified using International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis and procedure codes) among indigenous and white patients, to test for differences across both groups, and to test for differences between rural and urban residents within each racial category.
RESULTS:
We identified an estimated 7,561,729 (unweighted n=1,417,500) childbirth hospitalizations that were included in the analyses. Of those, an estimated 101,493 (unweighted n=19,080) were among indigenous women, and an estimated 7,460,236 (unweighted n=1,398,420) were among white women. The incidence of severe maternal morbidity and mortality was greater among indigenous women compared with white women (2.0% vs 1.1%, respectively; relative risk [RR] 1.8, 95% CI 1.6–2.0). Within each group, incidence was higher among rural compared with urban residents (2.3% for rural indigenous women vs 1.8% for urban indigenous women [RR 1.3, 95% CI 1.0–1.6]; 1.3% for rural white women vs 1.2% for urban white women [RR 1.1, 95% CI 1.1–1.2]).
CONCLUSION:
Severe maternal morbidity and mortality is elevated among indigenous women compared with white women. Incidence is highest among rural indigenous residents. Efforts to improve maternal health should focus on populations at greatest risk, including rural indigenous populations.
There are more than 5.2 million people who identify as indigenous in the United States, and there are 573 federally recognized tribes.1 Approximately 40% of indigenous people live in nonmetropolitan rural areas, both on and off reservations.2 Indigenous people, therefore, have a larger proportion of rural residents than other racial or ethnic groups in the United States, for whom rural residents represent 20% or less of the population.3 Additionally, rural counties in which more than half of residents are indigenous have elevated rates of premature death and face unique health challenges.4
Severe maternal morbidity and mortality have been increasing in the United States,5–7 with non-Hispanic black, rural, and low-income women being disproportionately affected.8–11 Data released by the Centers for Disease Control and Prevention (CDC) in May 2019 indicated strikingly elevated incidence of maternal mortality among American Indian or Alaska Native (indigenous) women.6 Along with non-Hispanic black women, indigenous women are approximately three times as likely as non-Hispanic white (white) women to die of pregnancy-associated causes.6 Despite recent decreases in the proportion of maternal deaths associated with direct obstetric cases of maternal mortality, such as puerperal sepsis, hemorrhage, and hypertensive disorders of pregnancy,12 geographic and racial inequities in severe maternal morbidity and mortality have remained sizeable and problematic. Achieving maternal health equity is an increasing focus in the fields of public health, medicine, and public policy. To date, limitations in available data and evidence have prevented a clear focus on the maternal health of indigenous women who give birth in the United States.13 This analysis provides detailed data on maternal morbidity, in addition to mortality, and explores the geographic aspects of maternal health inequities occurring among indigenous women.
METHODS
We conducted a pooled, cross-sectional analysis of 2012–2015 data from the National Inpatient Sample.14 The National Inpatient Sample is a 20% stratified sample of all hospital discharges in the United States compiled by the Healthcare Cost and Utilization Project at the Agency for Healthcare Research and Quality. The sample includes weights to account for complex sampling design and to allow for national estimates. All analyses comply with methodologic standards for working with the National Inpatient Sample.15 This study of deidentified data was determined exempt from review by the University of Minnesota Institutional Review Board.
We identified all hospital deliveries that occurred between 2012 and 2015 using standard methods.16 In 2015, International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) diagnoses codes were available only for the first three quarters. We adjusted the survey weights in 2015 to generate annualized estimates from the first three quarters of data. Our analyses included deliveries occurring among indigenous and white women. For each year in the study period, approximately 6% of observations had missing data for race or ethnicity. The Healthcare Cost and Utilization Project reports that race and ethnicity data in the National Inpatient Sample are not missing at random.17 We kept with other recent reports and chose not to impute missing data for race or ethnicity.8,18 Instead, we used complete case-based analyses.
Severe maternal morbidity and mortality was the primary outcome of this study, identified using ICD-9-CM diagnosis and procedure codes compiled by the CDC or by a discharge disposition of “died.”7 Consistent with prior studies, childbirth hospitalizations with a diagnosis code indicating severe maternal morbidity and an implausibly short length of stay (less than the 90th percentile calculated separately for vaginal, primary, and repeat cesarean deliveries) were reclassified as hospitalizations without severe maternal morbidity and mortality to obtain the most valid estimates. Reclassification based on length of stay was not applied to cases of in-hospital death or among those identified by procedure codes (blood transfusion, hysterectomy, mechanical ventilation, temporary tracheostomy, and cardiac conversion).19 We also conducted a sensitivity analysis that excluded cases in which blood transfusion was the only indicator of severe maternal morbidity and mortality, because including these cases may constitute an overestimate of truly severe morbidity.
We defined location of residence as rural or urban using the patient's address in the hospital discharge record, as classified and coded by HCUP. This dichotomous variable is a county-based measure of metropolitan compared with nonmetropolitan status based on the National Center for Health Statistics Classification and Urban Influence Codes.20
We included maternal sociodemographic characteristics based on known or plausible association with severe maternal morbidity and mortality. These included age, median income in ZIP code of residence, primary payer, and hospital census region. We grouped payment sources into public insurance (Medicaid and Medicare), commercial insurance, and uninsured or self-pay. Given Medicare funded less than 0.6% of the childbirth hospitalizations, we refer to public sources as Medicaid throughout the study. The number of observations with missing values for these sociodemographic characteristics was 1.3% of all childbirth hospitalizations, and these were excluded from analyses.
We examined chronic conditions associated with severe maternal morbidity and mortality, including chronic respiratory disease (asthma), chronic hypertension, preexisting diabetes mellitus, chronic kidney disease, depression or anxiety, serious mental illness (bipolar or psychotic disorders), and substance use disorders (opioids, amphetamine, cocaine, alcohol, cannabis, and tobacco) as defined in previous work and HCUP algorithms.21,22 Depression or anxiety was defined using ICD-9-CM codes 311, 296.2–296.3, 300.4, 309.1, 301.12, 300.0; serious mental illness was defined with ICD-9-CM codes 295 and 296. In addition, we examined delivery-related outcomes including preterm (ICD-9-CM code 644.2x) and cesarean delivery (ICD-9-CM codes 74.0–74.2, 74.4, 74.99 and DRG codes 765, 766).
We first used weighted frequencies to describe sociodemographic characteristics across each racial category. Owing to the design of the National Inpatient Sample, we used weighted frequencies to describe sociodemographic characteristics between rural and urban residents within each racial category. Differences were compared statistically using Rao-Scott χ2 tests and two-sample t-tests.
We used weighted multivariable logistic regression and predictive population margins to generate prevalence and incidence estimates and relative risks (RRs) with 95% CIs for comorbid physical health conditions and delivery-related outcomes, including severe maternal morbidity and mortality. The incidence of blood transfusion, disseminated intravascular coagulation, and hysterectomy were also estimated for each group. These were the only individual indicators of severe maternal morbidity and mortality with a large enough unweighted sample size to present for each group of women. We used multivariate models to test for statistical differences in study outcomes between indigenous women and white women and conducted stratified analyses between rural and urban residents within each racial category (comparing rural and urban indigenous women, for example). Finally, we estimated the excess incidence of severe maternal morbidity and mortality among rural, indigenous, and rural indigenous women. We did so by multiplying the total number of weighted cases for each group by that group's adjusted incidence rate of severe maternal morbidity and mortality and subtracting the number of cases calculated when instead using the adjusted incidence rate for the appropriate referent group.
All models were adjusted for age, insurance payer, income, and hospital region. P values less than .01 were considered statistically significant. All analyses were conducted using SAS 9.4.
RESULTS
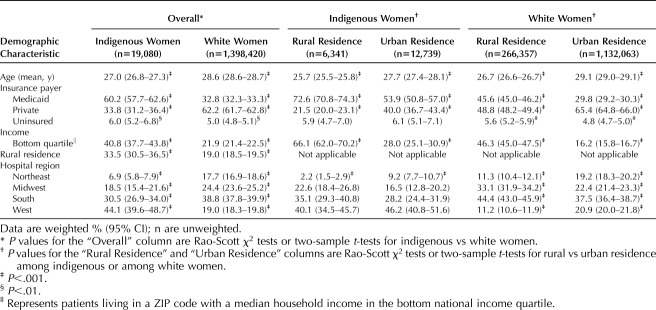
We identified an estimated 7,561,729 (unweighted n=1,417,500) childbirth hospitalizations that were included in the analyses (Table 1). Of those, an estimated 101,493 (unweighted n=19,080) were among indigenous women, and an estimated 7,460,236 (unweighted n=1,398,420) were among white women. One third (33.5%, 95% CI 30.5–36.5) of indigenous women resided in rural counties, compared with 19.0% (95% CI 18.5–19.5, P<.001) of white women.
Table 1.
Demographic Characteristics of Indigenous and White Women by Rural Compared With Urban Residence, National Inpatient Sample, 2012–2015 (N=1,417,500)
There were substantial differences in sociodemographic characteristics by race and when examining each population by rural compared with urban residence (Table 1; [Appendix 1, is available online at http://links.lww.com/AOG/B693]). Overall, nearly twice as many births to indigenous women were paid for by Medicaid compared with white women, twice as many indigenous women lived in ZIP codes with a median household income in the bottom national income quartile compared with white women, and rural women were almost three times more likely to live in bottom income quartile ZIP codes than urban women among both racial categories (P<.001 for all comparisons).
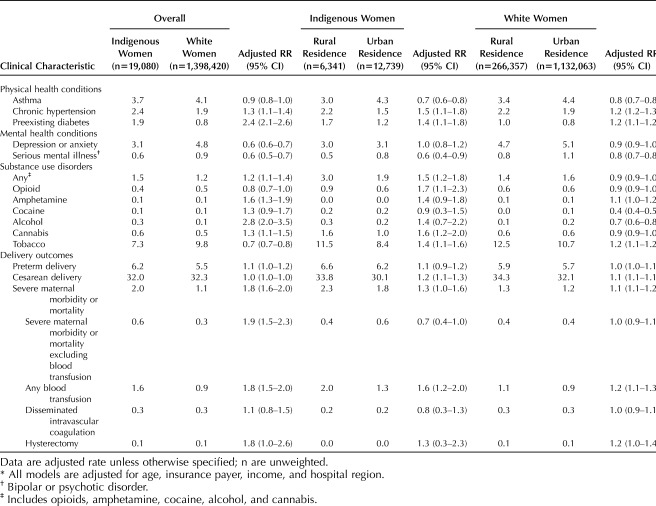
Clinical differences were identified in the prevalence of many comorbid conditions (Table 2; [Appendix 2 is available online at http://links.lww.com/AOG/B693]). Indigenous women had higher prevalence of both chronic hypertension and preexisting diabetes compared with white women. In contrast, white women had higher prevalence of depression, anxiety, and serious mental illness. Patterns of substance use also varied, with higher prevalence of opioid and tobacco use among white women and higher prevalence of amphetamine, alcohol, and cannabis use among indigenous women. Among indigenous women, the prevalence of any substance use disorder (excluding tobacco) was 40% higher among rural compared with urban residents (P<.001).
Table 2.
Clinical Characteristics of Indigenous and White Women by Rural–Urban Residence, United States, 2012–2015 (N=1,417,500)*
Rates of severe maternal morbidity and mortality were twice as high among indigenous women compared with white women (2.0% vs 1.1%, respectively; RR 1.8, 95% CI 1.6–2.0; Fig. 1), and within these groups, rates for rural residents were higher than urban residents: 2.3% for rural indigenous women, 1.8% for urban indigenous women (RR 1.3, 95% CI 1.0–1.6), 1.3% for rural white women, and 1.2% for urban white women (RR 1.1, 95% CI 1.1–1.2). This was largely driven by blood transfusion, which occurred with greater frequency among indigenous women compared with white women (1.6% vs 0.9%, respectively; RR 1.8, 95% CI 1.5–2.0), particularly rural indigenous women (2.0%; rural vs urban indigenous women RR 1.6, 95% CI 1.2–2.0). When cases in which blood transfusion was the only indicator of severe maternal morbidity and mortality were excluded in our sensitivity analysis, indigenous women continued to incur higher rates of severe maternal morbidity and mortality compared with white women (0.6% vs 0.3%, respectively; RR 1.9, 95% CI 1.5–2.3). Rural and urban differences were no longer significant, but sample size was very limited among indigenous women, particularly rural indigenous women for whom only 32 unweighted cases of severe maternal morbidity and mortality were identified.
Fig. 1. Incidence of severe maternal morbidity and mortality and blood transfusion among indigenous and white women by rural–urban residence, United States 2012–2015 (N=1,417,500).* *All results are represented as incidence per 100 childbirth hospitalizations (95% CI) unless otherwise noted; N are unweighted. All models are adjusted for age, insurance payer, income, and hospital region. †Any severe maternal morbidity and mortality including blood transfusion.
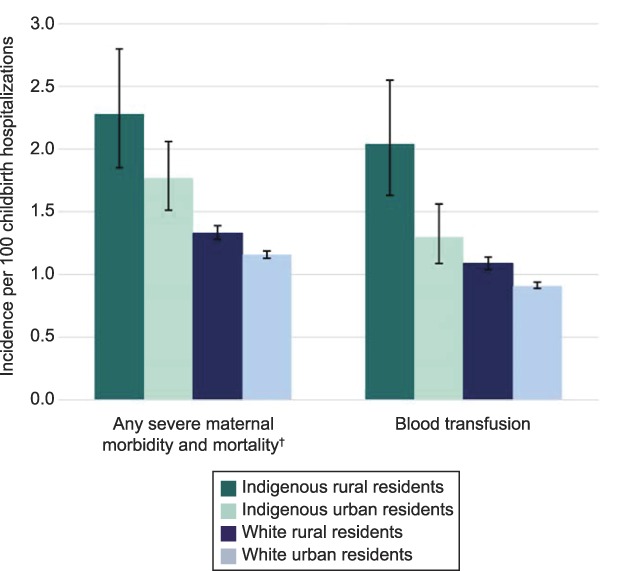
Kozhimannil. Maternal Morbidity and Mortality Among Indigenous Women. Obstet Gynecol 2020.
Taken together, these data indicate that, if indigenous women experienced severe maternal morbidity and mortality at the same rate as white women, this would result in a 43.9% (95% CI 38.5–49.1) reduction in cases of severe maternal morbidity and mortality among indigenous women (an estimated 228 [95% CI 178–287] fewer cases per year). Further, if rural indigenous women experienced severe maternal morbidity and mortality at the same rate as urban white women, this would result in a 49.1% (95% CI 38.9–57.5) reduction in cases.
DISCUSSION
Both race and geography affect maternal health. From 2012 to 2015, the incidence of severe maternal morbidity and mortality associated with childbirth was twice as high among indigenous compared with white women. These findings add nuance to recently released CDC data that indicate significantly elevated risk of maternal mortality among indigenous women.6 Within racial groups in this analysis, the incidence of severe maternal morbidity and mortality was higher among rural residents compared with urban residents. This finding is consistent with existing evidence on rural–urban differences in maternal health, including maternal mortality.11,23,24 The highest incidence of severe maternal morbidity and mortality was detected among indigenous women residing in rural counties, who experienced severe maternal morbidity and mortality during 2.3% of all hospitalizations for childbirth. This analysis provides empirical data at the intersection between racial and geographic disparities in maternal health outcomes among indigenous women and should inform efforts to advance maternal health equity in the United States.
Addressing the intersection of risks based on both race- and place-based inequities requires 1) inclusion of rural and indigenous people in planning and implementation of maternity care improvement, 2) measuring maternal health outcomes based on race and geography, and 3) recognizing that indigenous populations are heterogeneous groups with salient individual characteristics. Profound disadvantage was identified among indigenous women residing in rural counties, with two thirds living in counties with median incomes in the bottom national income quartile. Concordantly, three quarters of these women had childbirth hospitalizations paid for by Medicaid. Indigenous women residing in rural counties also incurred the greatest risk for preexisting, chronic conditions complicating childbirth, including diabetes and substance use disorders. Improving maternal outcomes for indigenous women requires engagement with medical and social determinants of health in both clinical and policy efforts aimed at addressing these inequities. In many ways, these findings shed light on the perfect storm of conditions that create difficulty for both patients and clinicians who aim to meaningfully improve maternal health outcomes. Access to obstetric services is declining in rural areas, and efforts to expand health care provider incentives and resources aimed at recruiting and retaining rural providers have been slow to take shape. These policies are integral to the sustainability of rural maternity care and to improving health outcomes among rural residents, including indigenous women.
Additionally, pregnancy-related categorical eligibility for Medicaid—the primary type of Medicaid coverage for women included in this analysis—lasts from conception until 60 days postpartum. This makes addressing long-term health conditions that often influence obstetric outcomes more difficult. In fact, recent work reveals that 65% of women with Medicaid at birth were without insurance for at least 1 month in the 9 months leading up to delivery, and 55% were uninsured for at least 1 month during the 6 months after birth.25 Insurance gaps and transitions likely influence the ability of patients and health care providers to work together to address and optimize preexisting conditions before pregnancy and during early prenatal care. Pregnancy-related insurance eligibility expansions, as recently called for by political leaders, the American Medical Association, and the American College of Obstetricians and Gynecologists,26–29 may be one solution for addressing the challenges encountered under the current system of financing pregnancy-related care.
Next, the findings of this study suggest that blood transfusion is largely driving the high incidence of severe maternal morbidity and mortality among indigenous women who reside in rural counties. Blood transfusion is frequently associated with obstetric hemorrhage in the context of childbirth, and a significant proportion of obstetric hemorrhages are considered preventable.8 The implementation of quality improvement initiatives addressing obstetric hemorrhage, such as the Alliance for Innovation in Maternity Care's Obstetric Hemorrhage Safety Bundle,30 should focus on geographic equity in implementation by improving quality of care for populations at the greatest risk of adverse outcomes, including rural indigenous women.
Finally, maternal mortality review committees have been established in almost every state to review cases of maternal death and to identify and make recommendations on ways to prevent future cases of morbidity and mortality.31 However, as of December 2018, only three states had legislation directing their maternal mortality review committees to explicitly focus review on rural communities, and only two states required rural representation on their committees.31 Many tribes have deep traditions of healing and a broad understanding of both personal and historical trauma, which could helpfully inform strategies for improving health outcomes for indigenous women during pregnancy. Specifically addressing the unique needs and challenges of rural residents, particularly rural indigenous residents, is essential to addressing inequities in maternal outcomes. Additionally, including attention to severe maternal morbidity in mortality review proceedings may improve prevention efforts.
The findings of this study should be interpreted in light of the limitations of the data source and study design. These data derive from the childbirth hospitalization, and severe maternal morbidity and mortality may occur up to 1 year after childbirth. Further, as with the use of any claims database, codes that do not generate a specific payment, such as codes for comorbid conditions or severe maternal morbidity and mortality codes not indicating a procedure was performed, may be associated with low sensitivity. Such coding irregularity can differentially affect different groups of women. Challenges exist in generalizing these findings, even when stratified by rural and urban residence, to broader groups of indigenous women owing to vast social differences among tribal governances, local health care resources, and social structures. Local differences are hard to discern in many nationally available survey and administrative data sources, which often include relatively low numbers of indigenous women, making it difficult to detect differences across subgroups. Data on race or ethnicity were missing in 6% of cases included in this analysis. Additionally, hospitals administered by the Indian Health Service cannot be distinguished in these data. Understanding and addressing the challenges faced in local contexts where excess morbidity and mortality is identified will be important for addressing the troubling patterns identified in this study, and maternal mortality review committees may be an important avenue for this work.
The incidence of severe maternal morbidity and mortality is highest among rural indigenous residents, who also more likely to live in low-income communities and have Medicaid coverage at the time of childbirth. Efforts to improve maternal health should focus on populations at greatest risk, including rural indigenous women who give birth.
Footnotes
This research was supported in part with funding from the Federal Office of Rural Health Policy (FORHP), Health Resources and Services Administration (HRSA), US Department of Health and Human Services (HHS) Cooperative Agreement U1CRH03717. The information, conclusions and opinions expressed are those of the authors and no endorsement by FORHP, HRSA, or HHS is intended or should be inferred.
Financial Disclosure The authors did not report any potential conflicts of interest.
The authors thank the Healthcare Cost and Utilization Project's data partners for data collection efforts: https://www.hcup-us.ahrq.gov/partners.jsp. The authors also thank Curtis D. Travers, MPH, for statistical support.
Each author has confirmed compliance with the journal's requirements for authorship.
Peer reviews and author correspondence are available at http://links.lww.com/AOG/B694.
REFERENCES
- 1.Norris T, Vines PL, Hoeffel EM. The American Indian and Alaska native population: 2010. Washington, DC: United States Department of Commerce; 2012. [Google Scholar]
- 2.Dewees S, Marks B. Twice Invisible: Understanding Rural Native America. Albuquerque, NM: First Nations Development Institute; 2017. [Google Scholar]
- 3.Ratcliffe M, Burd C, Holder K, Fields A. American community survey and geography brief: defining rural at the U.S. Census bureau. Available at: https://www.census.gov/content/dam/Census/library/publications/2016/acs/acsgeo-1.pdf. Retrieved August 21, 2019. [Google Scholar]
- 4.Henning-Smith C, Hernandez AM, Ramirez M, Hardeman R, Kozhimannil K. Dying too soon: County-level disparities in premature death by rurality, race, and ethnicity. Available at: https://3pea7g1qp8f3t9ooe3z3npx1-wpengine.netdna-ssl.com/wp-content/uploads/2019/03/1552267547UMNpolicybriefPrematureDeath.pdf. Retrieved July 30, 2019. [Google Scholar]
- 5.MacDorman MF, Declercq E, Cabral H, Morton C. Is the United States maternal mortality rate increasing? Disentangling trends from measurement Issues. Obstet Gynecol 2016;128:447–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petersen EE, Davis NL, Goodman D, Cox S, Mayes N, Johnston E, et al. Vital signs: pregnancy-related deaths, United States, 2011–2015, and strategies for prevention, 13 states, 2013–2017. MMWR Morb Mortal Wkly Rep 2019;68:423–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Severe maternal morbidity in the United States.Available at: www.cdc.gov/reproductivehealth/maternalinfanthealth/severematernalmorbidity.html. Retrieved September 1, 2019. [Google Scholar]
- 8.Admon LK, Winkelman TNA, Zivin K, Terplan M, Mhyre JM, Dalton VK. Racial and ethnic disparities in the incidence of severe maternal morbidity in the United States, 2012–2015. Obstet Gynecol 2018;132:1158–66. [DOI] [PubMed] [Google Scholar]
- 9.Howell EA, Egorova N, Balbierz A, Zeitlin J, Hebert PL. Black-white differences in severe maternal morbidity and site of care. Am J Obstet Gynecol 2016;214:122.e1–e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nelson DB, Moniz MH, Davis MM. Population-level factors associated with maternal mortality in the United States, 1997–2012. BMC Public Health 2018;18:1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kozhimannil KB, Interrante JD, Henning-Smith C, Admon LK. Rural-urban differences in severe maternal morbidity and mortality in the US, 2007–15. Health Affairs 2019;38:2077–85. [DOI] [PubMed] [Google Scholar]
- 12.Creanga AA, Syverson C, Seed K, Callaghan WM. Pregnancy-related mortality in the United States, 2011–2013. Obstet Gynecol 2017;130:366–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baldwin L-M, Grossman DC, Murowchick E, Larson EH, Hollow WB, Sugarman JR, et al. Trends in perinatal and infant health disparities between rural American Indians and Alaska natives and rural whites. Am J Public Health 2009;99:638–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.HCUP National Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality. Available at: https://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp. Retrieved September 1, 2019. [Google Scholar]
- 15.Khera R, Angraal S, Couch T, Welsh JW, Nallamothu BK, Girotra S, et al. Adherence to methodological standards in research using the national inpatient sample. JAMA 2017;318:2011–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuklina EV, Whiteman MK, Hillis SD, Jamieson DJ, Meikle SF, Posner SF, et al. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J 2008;12:469–77. [DOI] [PubMed] [Google Scholar]
- 17.Houchens R. Missing data methods for the NIS and the SID. HCUP methods series report #2015-01. Available at: www.hcup-us.ahrq.gov/reports/methods/methods.jsp. Retrieved October 12, 2019. [Google Scholar]
- 18.Booker WA, Gyamfi-Bannerman C, Sheen JJ, Wright JD, Siddiq Z, D'Alton ME, et al. Maternal outcomes by race for women aged 40 Years or older. Obstet Gynecol 2018;132:404–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol 2012;120:1029–36. [DOI] [PubMed] [Google Scholar]
- 20.National Center for Health Statistics. NCHS urban-rural classification scheme for counties. Available at: www.cdc.gov/nchs/data_access/urban_rural.htm. Retrieved September 1, 2019. [Google Scholar]
- 21.Admon LK, Winkelman TNA, Moniz MH, Davis MM, Heisler M, Dalton VK. Disparities in chronic conditions among women hospitalized for delivery in the United States, 2005–2014. Obstet Gynecol 2017;130:1319–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heslin K, Elixhauser A, Steiner C. Hospitalizations involving mental and substance use disorders among adults, 2012. HCUP Stat Br 2015;191. [PubMed] [Google Scholar]
- 23.Fine Maron D. Maternal health care is disappearing in rural America. Available at: https://www.scientificamerican.com/article/maternal-health-care-is-disappearing-in-rural-america/. Retrieved July 1, 2019. [Google Scholar]
- 24.Kozhimannil KB, Hung P, Prasad S, Casey M, Moscovice I. Rural-urban differences in obstetric care, 2002–2010, and implications for the future. Med Care 2014;52:4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Daw JR, Hatfield LA, Swartz K, Sommers BD. Women in the United States experience high rates of coverage “churn” in months before and after childbirth. Health Aff 2017;36:598–606. [DOI] [PubMed] [Google Scholar]
- 26.Booker CA. S.3494 MOMMIES Act. 115th Congress (2017–2018). Available at: https://www.congress.gov/bill/115th-congress/senate-bill/3494. Retrieved August 21, 2019. [Google Scholar]
- 27.Kelly RL. H.R. 1897 MOMMA's Act. 116th Congress (2019–2020). Available at: https://www.congress.gov/bill/116th-congress/house-bill/1897/text. Retrieved August 6, 2019. [Google Scholar]
- 28.ACOG statement on AMA support for 12 months of postpartum coverage under Medicaid. Available at: https://www.acog.org/About-ACOG/News-Room/Statements/2019/AMA-Support-for-12-Months-Postpartum-Medicaid-Coverage?IsMobileSet=false. Retrieved December 11, 2019.
- 29.AMA adopts new policies at 2019 annual meeting. Available at: www.ama-assn.org/press-center/press-releases/ama-adopts-new-policies-2019-annual-meeting. Retrieved June 13, 2019. [Google Scholar]
- 30.Main EK, Goffman D, Scavone BM, Low LK, Bingham D, Fontaine PL, et al. National Partnership for Maternal Safety: consensus bundle on obstetric hemorrhage. J Obstet Gynecol Neonatal Nurs 2015;44:462–70. [DOI] [PubMed] [Google Scholar]
- 31.Kozhimannil KB, Interrante JD, Corbett A, Heppner S, Burges J, Henning-Smith C. Rural focus and representation in state maternal mortality review committees: review of policy and legislation. Women's Heal Issues 2019;29:357–63. [DOI] [PubMed] [Google Scholar]