We identified longitudinal patterns of STI risk based on psychological and behavioral characteristics, and these characteristics did not change over time in most participants, irrespective of sexually transmitted infection test results.
Supplemental digital content is available in the text.
Abstract
Background
Great heterogeneity in sexually transmitted infections (STI) risk exists, and investigating individual-level characteristics related to changes in STI risk over time might facilitate the development and implementation of effective evidence-based behavior change interventions. The aim of this study was to identify longitudinal patterns of STI risk based on psychological and behavioral characteristics.
Methods
A longitudinal study was conducted among heterosexual STI clinic visitors aged 18 to 24 years. Latent classes based on behavioral and psychological characteristics at baseline, and transitions from 1 latent class to another at 3-week, 6-month, and 1-year follow-up, were identified using latent transition analysis.
Results
Four latent classes were identified that could be differentiated by psychological and behavioral characteristics and STI risk: overall low-risk (10%), insecure high-risk (21%), condom-users (38%), and confident high-risk (31%). Although the majority of the total study population did not move to another latent class over time, the size of the overall low-risk group increased from 10% at baseline to 30% after 1 year. This was mainly due to transitions from the insecure high-risk, condom-users, and confident high-risk class at 3-week follow-up to the overall low-risk class at 6-month follow-up.
Conclusions
Distinct subgroups among heterosexual STI clinic visitors can be differentiated from each other by multiple psychological and behavioral characteristics, and these characteristics reflecting the risk of acquiring STI are consistent over the course of 1 year in most individuals. An integral approach, adapting behavioral interventions to match multiple psychological and behavioral characteristics of high-risk subgroups, might be more effective in controlling STI transmission.
Sexually transmitted infections (STIs), such as Chlamydia trachomatis and Neisseria gonorrhea, are among the most common causes of morbidity globally.1 Consequences of STI, such as pelvic inflammatory disease, and infertility have a major impact on sexual and reproductive health.2 Much heterogeneity in STI risk exists in the general population, as a result of differences in population- and individual-level characteristics that are associated with increased risk of acquiring STI, such as demographic characteristics (eg, age, education level, or sexual preference)3,4 and sexual behavior (eg, condom use, number of partners).5–7
The interplay between sexual behavior and psychological characteristics, such as knowledge, attitudes, and risk perception, might further differentiate individuals in terms of STI risk. For example, individuals with more knowledge and more positive attitudes regarding STI prevention might be more likely to use condoms, but this does not necessarily influence their number of partners.8 Furthermore, high-risk perception is associated with higher condom use,9,10 and more health care–seeking behavior,11 but many individuals engaging in high-risk behavior underestimate their STI risk.12–14 Better understanding of what motivates people to change their behavior in a more risk-reducing direction is needed to develop more effective behavior change interventions.
It is likely that sexual behavior and STI risk of an individual change over time.15–17 For example, periods of low- and high-risk sexual behavior may alternate during the sexually active years.15,18–20 In addition, sexual behavior might temporarily become less risky after STI18 or HIV diagnosis,19 or become more risky after partnership dissolution.20 Research, to date, on the impact of behavior change on STI risk tends to focus on men who have sex with men (MSM),16,21 in particular the influence of the introduction of preexposure prophylaxis.22,23 Few studies have statistically modeled variation in both behavioral and psychological characteristics over time, and how this might influence STI risk in a heterosexual population. Investigating changes in STI risk over time based on real-life longitudinal data on both psychological and behavioral characteristics might facilitate the development and implementation of more effective evidence-based interventions in clinical practice.
The aim of this study was to identify longitudinal patterns of STI risk based on psychological characteristics and sexual behavior among heterosexual STI clinic visitors. Subgroups of individuals, differentiated by specific psychological and behavioral characteristics, were identified and transitions between these subgroups over time were examined. Demographic and sexual health-related characteristics at baseline, including chlamydia and gonorrhea diagnoses, were compared between the subgroups.
MATERIALS AND METHODS
Setting
A detailed description of the iMPaCT study has been published elsewhere.24 In short, a longitudinal cohort study was conducted from November 2016 to July 2018. Heterosexual males and females, including females who have sex with both males and females, aged 18 to 24 years, who visited the STI clinic for STI testing in November 2016 to July 2017, were eligible to participate. Participants were recruited during the process of making an appointment at the STI clinics of the public health services in Amsterdam, Kennemerland, Hollands Noorden, and Twente in the Netherlands. Individuals who signed the informed consent, completed an online questionnaire, and provided contact information for follow-up, were enrolled for 1 year. Online questionnaires assessing psychological and behavioral characteristics were administered at 4 different time points: baseline (before STI clinic consultation), 3-week, 6-month, and 1-year follow-up. Furthermore, all participants were tested for chlamydia and gonorrhea at the STI clinic at baseline, and were invited for repeat testing with a home-based test kit for chlamydia and gonorrhea at 6-month follow-up (all nucleic acid amplification tests). The iMPaCT study was approved by the Medical Ethical Committee of the University Medical Center Utrecht, the Netherlands (NL57481.094.16/METC18-363/D/Dutch Trial Register NTR-6307).
Data Collection
Demographic and sexual health-related data registered by the STI clinics were extracted from the national STI surveillance database, using a unique identification number of the iMPaCT study. Data on psychological and behavioral characteristics were measured in the online questionnaires, using the same questions in each follow-up questionnaire. The development and content of the questionnaire has been described in detail elsewhere,24 and the complete questionnaire is available online.25 The following psychological characteristics were assessed in the questionnaires: perceived importance of (sexual) health or “health goals,” attitudes regarding prevention of chlamydia, intentions regarding condom use and STI testing, anticipated stigma and shame regarding chlamydia diagnosis, impulsiveness, knowledge on sexual health in terms of prevention and consequences of chlamydia, self-efficacy regarding condom use, social context regarding condom use and STI testing (ie, social support, social and subjective norms), self-esteem, and risk perception for chlamydia. Behavioral data included the number of partners in the past 6 months, and condom use in general (scale from 1 = never to 5 = always). A detailed description of the data collection is provided in Supplemental Digital Content 2 http://links.lww.com/OLQ/A448, text S1 and Table S1.
All psychological and behavioral variables from the questionnaire were included in the statistical analysis. To improve the interpretability of the identified subgroups and to provide clear cutoff values, which are practically applicable in clinical practice, variables were dichotomized. The psychological and behavioral variables were divided in 2 categories at the median: “low” (values < median), and “medium/high” (values ≥ median).
Statistical Analysis
All participants who completed the baseline questionnaire were included in the statistical analyses. Latent class analysis (LCA) was performed to determine the number of subgroups, or “latent classes,” based on psychological and behavioral characteristics. In the LCA, models with 2 to 6 latent classes were fitted to baseline data (before STI clinic consultation), minimizing the potential influence of the STI clinic consultation on the reporting of psychological and behavioral characteristics.26 The psychological and behavioral variables in the questionnaires were selected based on their association with (changes in) STI risk, and, therefore, all these variables were included in the LCA. The number of latent classes was determined by examining a combination of model fit indices: the Akaike information criterion and Bayesian Information Criterion values (BIC) (ie, lower values indicating a better model fit), the Voung-Lo-Mendell-Rubin Likelihood Ratio Test (VLMR), and Bootstrapped Likelihood Ratio Test (BLRT) (ie, P < 0.05 indicating significant improvement in model fit when 1 more class is added).27,28
To identify movement from 1 latent class to another over time, latent transition analysis (LTA), a longitudinal extension of LCA, was performed. The number and characteristics of the latent classes were fixed at each time point. To test this assumption, the BIC of the model with fixed classes over time was compared with the BIC of a model without fixations (ie, characteristics of each latent class may vary over time) with lower BIC values indicating a better model fit. The LTA was optimized by increasing the number of iterations and random sets of start values until the optimal maximum likelihood solution was achieved, and classification performance was evaluated using the entropy value, and the interpretability of the latent class characteristics. Entropy values are indicators of classification performance, and values of 0.8 to 1.0 indicate good classification of the latent classes.27,28 This means that the probability that an individual was correctly allocated to a latent class at baseline and each follow-up moment is high, suggesting clear delimitation of the latent classes. Furthermore, for the latent class interpretation, a smaller number of latent classes that can be well distinguished from each other was preferred over a larger number of latent classes with characteristics that are less distinctive. Missing values in the follow-up data were handled using the full-information maximum likelihood technique,29 which is an iterative process using all the available data of complete and incomplete cases to predict the most likely latent class membership. To assess the uncertainty of this method, sensitivity analyses were performed comparing the transition probabilities of an LTA, including only the complete cases (ie, participants who filled out all 4 questionnaires) and the participants who filled out at least 1 follow-up questionnaire, with the main analyses. From the final model, the following data were extracted: the item-response probabilities of the latent classes for each psychological and behavioral variable, the estimated transition probabilities between successive data collection moments, and the most likely latent class pattern for each participant. The latent classes were labeled based on the most distinctive psychological and/or behavioral characteristics. Participants were classified to their most likely latent class pattern, which is justified if entropy of the LTA is higher than 0.8.30 Subsequently, potential covariates (ie, demographic and sexual health-related data) were compared between the latent classes at baseline using univariable logistic regression analyses. All statistical analyses were done using Mplus version 8.2.31s
RESULTS
Participant Characteristics
In total, 810 (6% of all eligible STI clinic visitors) individuals signed the informed consent, completed the online questionnaire and provided contact information for follow-up. Participants were more likely to be female, highly educated, older (>20 years), and ethnic Dutch, to have had ≥3 partners in the past 6 months, and less likely to report STI-related symptoms, to have been notified by a partner, to have had condomless sex, compared to other eligible STI clinic visitors who did not participate in the iMPaCT study.25 The response rate during follow-up was 53% at 3-week, 51% at 6-month, and 43% at 1-year follow-up. Of the 810 participants included in the statistical analyses, 26% completed all follow-up questionnaires, and 72% completed ≥1 follow-up questionnaire. Participants who were lost to follow-up were more likely to report low perceived importance of health compared with participants who were retained, but chlamydia diagnosis at baseline was not a predictor of loss to follow-up.25
The majority of the study population was ≥22 years old (61%), female (80%), ethnic Dutch (81%), and highly educated (90%). Furthermore, 106 participants (13%) were diagnosed with chlamydia and 7 participants were diagnosed with gonorrhea (0.1%) at baseline. Among those participants who tested again within 1 year after baseline (n = 423), 50 participants (12%) were diagnosed with chlamydia and zero participants with gonorrhea. Among those diagnosed with chlamydia at baseline, 15 (30%) participants were diagnosed with chlamydia again within 1 year after baseline.
Latent Classes
Based on the AIC value, the VLMR and BLRT, the best fitting model in the LCA was the 4-class model (Supplemental Digital Content 2 http://links.lww.com/OLQ/A448, Table S2). The AIC value was lower in the 4-class model compared with the 3-class model (lowest BIC value), and the VLMR and BLRT showed that the 4-class model improved model fit compared with 3-class model (P < 0.05). Furthermore, an LTA with fixed classes over time was more parsimonious (ie, lower BIC) than a model without fixations (data not shown). Therefore, the LTA was performed with 4 fixed latent classes (entropy = 0.83). At baseline, 10% of the participants (n = 75) were in class 1, 21% in class 2 (n = 166), 38% in class 3 (n = 315), and 31% in class 4 (n = 254). Psychological and behavioral characteristics differed significantly between the latent classes (Fig. 1, Supplemental Digital Content 2 http://links.lww.com/OLQ/A448 Table S3). Based on the most distinctive characteristics of each class, class 1 could be referred to as “overall low-risk,” class 2 as “insecure high-risk,” class 3 as “condom-users,” and class 4 as “confident high-risk.” The latent classes also differed in terms of demographic and sexual health-related characteristics. The proportion of individuals diagnosed with chlamydia at baseline and/or during follow-up was highest in the insecure high-risk and confident high-risk classes (Supplemental Digital Content 2 http://links.lww.com/OLQ/A448, Table S4). Furthermore, in the confident high-risk class, 4 participants (of 7 gonorrhea diagnoses in total) were diagnosed with gonorrhea at baseline, of which 2 were coinfected with chlamydia. Comparing potentially confounding variables showed that participants in the overall low-risk class reported significantly less casual partners compared with the other classes. Furthermore, participants in the confident high-risk class were more likely to be male, highly educated, and to have been notified by their partner for STI exposure, compared with the other classes at baseline (Supplemental Digital Content 2 http://links.lww.com/OLQ/A448, Table S5).
Figure 1.
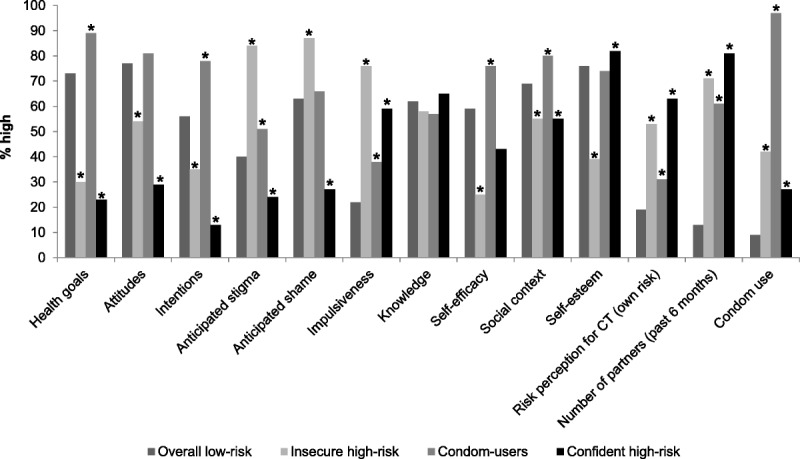
Psychological and behavioral characteristics of each latent class. a Health goals = perceived importance of (sexual) health. b Attitudes = attitudes regarding prevention of chlamydia. c Intentions = intentions regarding condom use and STI testing. d Knowledge = knowledge on sexual health in terms of prevention and consequences of chlamydia. e Self-efficacy = self-efficacy regarding condom use. f Social context = social context regarding condom use and STI testing (ie, social support, social and subjective norms). g Condom use = condom use in general, high = usually/always. * Univariate logistic regression P < 0.05, Overall low-risk = reference group. Abbreviation(s): CT = Chlamydia trachomatis.
Longitudinal Patterns of STI Risk
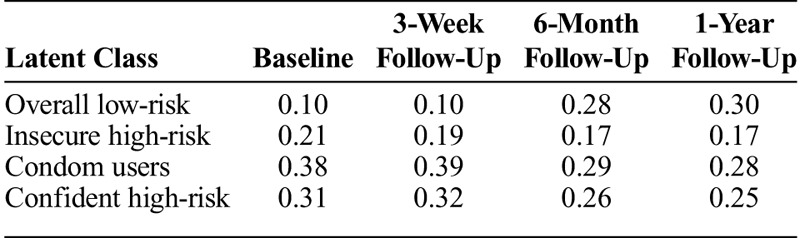
In the LTA, 32 different longitudinal patterns out of 256 possible patterns were observed. The majority of the participants stayed in the same latent class throughout the whole year, and 20% of the participants were movers. Figure 2 is an interactive diagram, which shows the study flows (ie, number of participants) between different latent classes over time. Transition probabilities to move from 1 latent class to another were highest between 3-week follow-up and 6-month follow-up (Table 1). The most common transitions among movers (n = 166) over 1-year follow-up were from the insecure or confident high-risk classes to the overall low-risk and condom-using classes (33%) or between the overall low-risk and the condom-using classes (54%). Less common transitions were from the overall low-risk or the condom-using latent classes to the insecure or confident high-risk latent classes (8%) or between the insecure or confident high-risk classes (5%). All identified transitions resulted in an increase in the size of the overall low-risk class from 10% of the total population at baseline to 30% after 1 year (Table 2). The sensitivity analyses showed similar transition probabilities for the complete cases, and all participants who filled out at least 1 follow-up questionnaire (Supplemental Digital Content 2 http://links.lww.com/OLQ/A448, Table S6 and Table S7). Longitudinal patterns stratified for participants who were diagnosed with an STI at baseline and participants who tested STI negative were comparable (Supplemental Digital Content 2 http://links.lww.com/OLQ/A448, Figure S1 and Figure S2).
Figure 2.
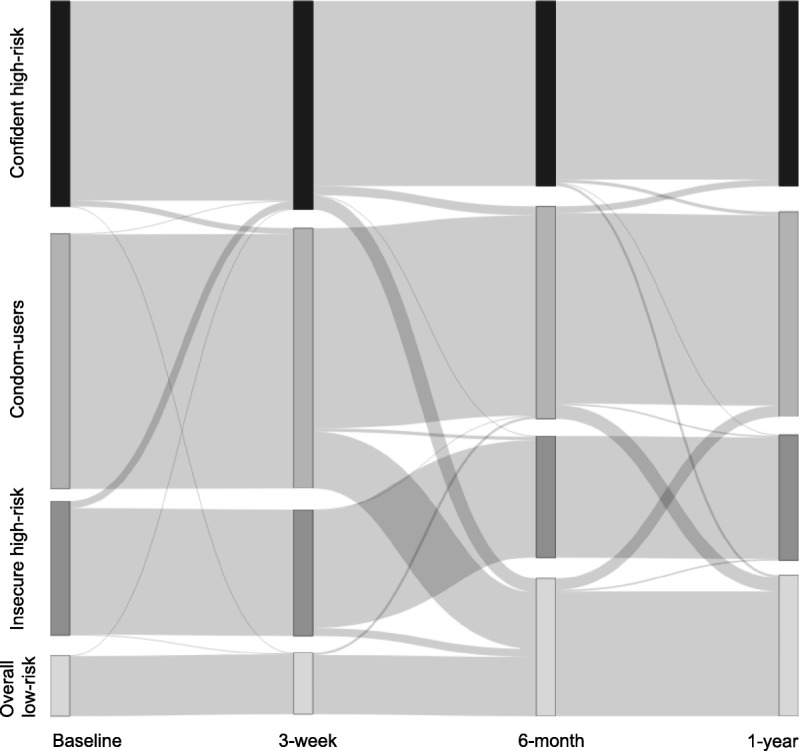
Longitudinal patterns with 4 latent classes based on psychological and behavioral characteristics over 1 year follow-up among heterosexual STI clinic visitors aged 18–24 years (n = 810). At baseline, people start in a class, and can stay in that class (broad straight lines to next follow-up moment), or move to another class (diagonal gray lines to next follow-up moment). http://rpubs.com/dvwees/Figure2.
TABLE 1.
Latent Transition Probabilities at Baseline, 3-Week, 6-Month, and 1-Year Follow-up for the Total Study Population (N = 810)
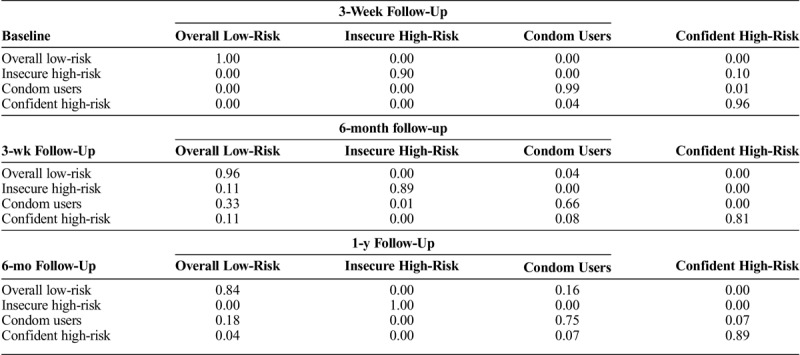
TABLE 2.
Class Proportions in the LTA at Baseline, 3-Week, 6-Month and 1-Year Follow-Up Based on the Estimated Model
DISCUSSION
Four latent classes were identified that could be differentiated by psychological and behavioral characteristics, and STI risk: overall low-risk, insecure high-risk, condom-users, and confident high-risk. The proportion of STI diagnoses at baseline was higher in individuals characterized by high-risk psychological characteristics (eg, low health goals, high impulsiveness), and high-risk sexual behavior (eg, high number of partners, inconsistent condom use). The majority of the total study population did not move to another latent class over time. Among those who did move to another latent class, the most common transitions were from the insecure high-risk, condom users, and confident high-risk class at 3-week follow-up to the overall low-risk class at 6-month follow-up, thereby increasing the size of the overall low-risk group over the course of this 1-year study. These transitions over time might be explained by the impact of receiving an STI diagnosis on psychological and behavioral characteristics.
The results showed that the overall low-risk and condom users latent class could be referred to as lower risk classes based on their psychological and behavioral characteristics, but the proportion of chlamydia diagnoses at baseline in the condom users was similar to that in the insecure and confident high-risk classes. An explanation for this might be that the condom-users reported less STI testing in the year before baseline compared with other risk classes. As chlamydia infections are usually asymptomatic, a large proportion of the chlamydia infections at baseline in the condom users may have gone undetected for months.32s The finding that the proportion of individuals diagnosed with chlamydia during follow-up was low in both the overall low-risk and condom users class, compared with the insecure and confident high-risk classes, supports this explanation. In addition, individuals in the insecure and confident high-risk classes were more likely to have been tested for STI in the past year at baseline compared with condom users, which suggests that even though most high-risk individuals did not reduce their risky behavior over time, they do test for STI regularly (ie, secondary prevention instead of primary prevention). This has been described before by other researchers, who argued that STI testing was often viewed as a substitute to condom use.33s
The findings in this study regarding the characteristics of the insecure and confident high-risk classes are consistent with those from other studies, including the association between high impulsiveness,34s lower health goals,35s less positive attitudes toward the prevention of chlamydia,36s lower intentions to use condoms,36s and increased STI risk. Also, in accordance with a previous study into STI risk perception and the association with risky sexual behavior,11 the present study demonstrated that risk perception was higher in individuals in high-risk classes, indicating realistic assessments of their STI risk in agreement with their behavior. Furthermore, males were more likely to be in the confident high-risk class. This is in line with a previous study showing gender discrepancies in reporting of sexual behavior among heterosexuals, such as males reporting a higher number of partners than females.37s It is difficult to compare the longitudinal patterns in the current study to other longitudinal studies into sexual behavior change and STI risk among young heterosexuals, which usually report change for each variable separately. There are previous studies that used similar techniques (ie, cluster analysis, latent class growth mixture modeling) to identify longitudinal trajectories of sexual behavior in MSM, but it should be kept in mind that psychological and behavioral characteristics in a population of MSM might be very different from a heterosexual population. Similar to the 80% of participants in the present study who did not move to another latent class over time, 1 study among HIV-negative MSM in the Netherlands found that 90% of individuals showed stable sexual behavior during follow-up.16 Another study among Swiss MSM found sexual behavior over time to be more variable, but still the majority of the study population 53% showed stable sexual behavior over time.21
The main strength of this study was the extensive collection of longitudinal data on psychological characteristics, sexual behavior, demographic characteristics, and sexual health outcomes. Furthermore, this is, to our knowledge, the first study to uncover longitudinal patterns of STI risk based on multiple psychological and behavioral characteristics among heterosexual STI clinic visitors. This study also had several limitations. First, the findings from this study should be interpreted with the characteristics of the study population in mind, as STI clinic visitors tend to be more high-risk compared with the general population.4,38s However, this can also be viewed as a strength of this study, as these findings could be used to tailor interventions to subgroup characteristics at the STI clinic, which might increase the impact of these interventions on reducing risk behavior and STI risk in a high-risk population. Second, although the total sample size in the LTA was relatively large, the small sample size of the lowest risk class hampered adjustment for possible effect modifiers and confounders in the comparison of demographic and sexual health-related characteristics between risk classes (ie, possibly biased estimates). Finally, as in most longitudinal cohort studies, there was substantial loss to follow-up, which could have led to more uncertainty in the classification of participants with missing data. Thus, the full-information maximum likelihood technique to deal with missing follow-up data was used. Furthermore, the sensitivity analysis showed similar transition probabilities for the complete and incomplete case analysis compared with the main analysis, which means that the longitudinal patterns were similar to the main analysis including missing data.
The findings of this study suggest that even though the participants might have been exposed to interventions at the STI clinic, as health care professionals often apply risk reduction counseling during a face-to-face test consultation (eg, motivational interviewing),39s the impact of these interventions on behavioral and psychological characteristics was limited in the majority of the study population (ie, no behavior change). Furthermore, the identified transitions to lower risk latent classes were mainly 6 months or 1 year after the STI clinic visit at baseline, suggesting that these transitions might not be related to the STI clinic visit. These findings highlight the need for an integral approach when deploying behavior change interventions, targeting multiple characteristics at once. Adapting interventions to match the psychological and behavioral characteristics of distinct subgroups might increase the impact of behavior change interventions on STI transmission. For example, combining strategies to increase health goals (eg, stimulating sexual health goal pursuit35s), attitudes and intentions toward condom use (eg, implementation intentions40s), and to decrease impulsiveness (eg, time-based interventions41s), during a face-to-face consultation might be more effective in achieving risk-reducing behavior in the insecure and confident high-risk subgroups than targeting only 1 distinctive characteristic. Psychological characteristics differentiating subgroups could be assessed with a few simple questions during (the online intake for) the STI clinic consultation. Furthermore, as resources to offer face-to-face consultations are often limited, alternative strategies based on behavior change theories,42s such as waiting room–delivered videos, printed materials, and online interventions, could be used.43s–46s Future research should investigate the impact of interventions adapted to subgroup characteristics on sexual behavior and STI risk over time, including identifying the best timing of interventions, examining how to combine different strategies, and how to implement effective evidence-based interventions in clinical practice.
In conclusion, distinct subgroups among heterosexual STI clinic visitors can be differentiated from each other by multiple psychological and behavioral characteristics, and these characteristics reflecting STI risk are consistent over the course of 1 year in most individuals. Adapting interventions to match the characteristics of high-risk subgroups could help to achieve the changes in psychological characteristics and sexual behavior needed to reduce STI risk. Thus, an integral approach, combining different intervention strategies targeted at multiple psychological and behavioral characteristics at once, might be more effective in controlling STI transmission.
Supplementary Material
Appendix
For further references, please see “Supplemental References,” http://links.lww.com/OLQ/A454.
Footnotes
Acknowledgments: The authors are grateful to the staff at the STI clinics of Amsterdam, Kennemerland, Hollands Noorden, Twente, especially Karin Westra, Anne de Vries, and Karlijn Kampman, who were involved in the recruitment and data collection of participants at baseline. The authors also thank Marlous Ratten and Klazien Visser from Soapoli-online, who coordinated the laboratory testing of the home-based test kits at 6-month follow-up, and the staff at Epidemiology and Surveillance Department at the National Institute for Public Health and the Environment, especially Birgit van Benthem, for fruitful discussions and Loes Soetens for her assistance in the data visualization.
Conflict of Interest and Sources of Funding: None declared.
Sources of Funding: The Strategic Programme (SPR) of the National Institute for Public Health and the Environment (RIVM) provided funding for this study (project number S/113004/01/IP).
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (http://www.stdjournal.com).
REFERENCES
- 1.GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388:1545–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Unemo M, Bradshaw CS, Hocking JS, et al. Sexually transmitted infections: Challenges ahead. Lancet Infect Dis 2017; 17:e235–e279. [DOI] [PubMed] [Google Scholar]
- 3.Sonnenberg P, Clifton S, Beddows S, et al. Prevalence, risk factors, and uptake of interventions for sexually transmitted infections in Britain: Findings from the National Surveys of sexual attitudes and lifestyles (Natsal). Lancet 2013; 382:1795–1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Visser M, van Aar F, Op de Coul ELM, et al. Sexually transmitted infections in the Netherlands in 2017. Bilthoven: Centre for Infectious Disease Control, National Institute for Public Health and the Environment (RIVM), 2018. [Google Scholar]
- 5.Mercer CH, Tanton C, Prah P, et al. Changes in sexual attitudes and lifestyles in Britain through the life course and over time: Findings from the National Surveys of sexual attitudes and lifestyles (Natsal). Lancet 2013; 382:1781–1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mercer CH, Copas AJ, Sonnenberg P, et al. Who has sex with whom? Characteristics of heterosexual partnerships reported in a national probability survey and implications for STI risk. Int J Epidemiol 2009; 38:206–214. [DOI] [PubMed] [Google Scholar]
- 7.Velicko I, Ploner A, Sparen P, et al. Sexual and testing behaviour associated with chlamydia trachomatis infection: A cohort study in an STI clinic in Sweden. BMJ Open 2016; 6:e011312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thorsen ML. A latent class analysis of behavioral and psychosocial dimensions of adolescent sexuality: Exploring race differences. J Sex Res 2018; 55:45–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abel G, Brunton C. Young people's use of condoms and their perceived vulnerability to sexually transmitted infections. Aust NZ J Public Health 2005; 29:254–260. [DOI] [PubMed] [Google Scholar]
- 10.Leval A, Sundstrom K, Ploner A, et al. Assessing perceived risk and STI prevention behavior: A national population-based study with special reference to HPV. PLoS One 2011; 6:e20624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clifton S, Mercer CH, Sonnenberg P, et al. STI risk perception in the British population and how it relates to sexual behaviour and STI healthcare use: Findings from a cross-sectional survey (Natsal-3). EClinicalMedicine 2018;2-3:29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ten Hoor GA, Ruiter RAC, van Bergen JEAM, et al. Predictors of chlamydia trachomatis testing: Perceived norms, susceptibility, changes in partner status, and underestimation of own risk. BMC Public Health 2016; 16:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wolfers ME, de Zwart O, Kok G. Adolescents in the Netherlands underestimate risk for sexually transmitted infections and deny the need for sexually transmitted infection testing. AIDS Patient Care STDS 2011; 25:311–319. [DOI] [PubMed] [Google Scholar]
- 14.van Wees DA, den Daas C, Kretzschmar MEE, et al. Double trouble: Modelling the impact of low risk perception and high-risk sexual behaviour on chlamydia transmission. J R Soc Interface 2018; 15:20170847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pines HA, Gorbach PM, Weiss RE, et al. Sexual risk trajectories among MSM in the United States: Implications for pre-exposure prophylaxis delivery. JAIDS 2014; 65:579–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Basten M, Heijne JCM, Geskus R, et al. Sexual risk behaviour trajectories among MSM at risk for HIV in Amsterdam, the Netherlands. AIDS 2018; 32:1185–1192. [DOI] [PubMed] [Google Scholar]
- 17.Wilkinson AL, El-Hayek C, Fairley CK, et al. Measuring transitions in sexual risk among men who have sex with men: The novel use of latent class and latent transition analysis in HIV sentinel surveillance. Am J Epidemiol 2017; 185:627–635. [DOI] [PubMed] [Google Scholar]
- 18.Soetens LC, van Benthem BHB, Op de Coul EL. Chlamydia test results were associated with sexual risk behavior change among participants of the chlamydia screening implementation in the Netherlands. Sex Transm Dis 2015; 42:109–114. [DOI] [PubMed] [Google Scholar]
- 19.Heijman T, Zuure F, Stolte I, et al. Motives and barriers to safer sex and regular STI testing among MSM soon after HIV diagnosis. BMC Infect Dis 2017; 17:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moreau C, Beltzer N, Bozon M, et al. Sexual risk-taking following relationship break-ups. Eur J Contracept Reprod Health Care 2011; 16:95–99. [DOI] [PubMed] [Google Scholar]
- 21.Salazar-Vizcaya L, Kusejko K, Schmidt AJ, et al. Clusters of sexual behaviour in HIV-positive men who have sex with men reveal highly dissimilar time trends. Clin Infect Dis 2020; 70:416–424. [DOI] [PubMed] [Google Scholar]
- 22.Rozhnova G, Heijne JCM, Basten M, et al. Impact of sexual trajectories of men who have sex with men on the reduction in HIV transmission by pre-exposure prophylaxis. Epidemics 2019; [in press] doi: 10.1016/j.epidem.2019.03.003; 28:100337. [DOI] [PubMed] [Google Scholar]
- 23.Hoornenborg E, Coyer L, van Laarhoven A, et al. Change in sexual risk behaviour after 6 months of pre-exposure prophylaxis use: Results from the Amsterdam pre-exposure prophylaxis demonstration project. AIDS 2018; 32:1527–1532. [DOI] [PubMed] [Google Scholar]
- 24.van Wees DA, Heijne JCM, Heijman T, et al. Study protocol of the iMPaCT project: A longitudinal cohort study assessing psychological determinants, sexual behaviour and chlamydia (re)infections in heterosexual STI clinic visitors. BMC Infect Dis 2018; 18:559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Wees DA, den Daas C, Kretzschmar MEE, et al. Who drops out and when? Demographic, sexual health-related, behavioural and psychological predictors of different stages of non-response and loss to follow-up in a longitudinal cohort study among STI clinic visitors. PLoS One 2019; 14:e0218658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuyper L, de Wit J, Heijman T, et al. Influencing risk behavior of sexually transmitted infection clinic visitors: Efficacy of a new methodology of motivational preventive counseling. AIDS Patient Care STDS 2009; 23:423–431. [DOI] [PubMed] [Google Scholar]
- 27.Collins LM, Lanza ST. Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences. Hoboken, New Jersey: John Wiley & Sons, 2010. [Google Scholar]
- 28.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equ Modeling 2007; 14:535–569. [Google Scholar]
- 29.Cham H, Reshetnyak E, Rosenfeld B, et al. Full information maximum likelihood estimation for latent variable interactions with incomplete indicators. Multivariate Behav Res 2017; 52:12–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clark SL, Muthén B. Relating latent class analysis results to variables not included in the analysis 2019. Available at: http://www.statmodel.com/download/relatinglca.pdf. Accessed August 3, 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


