Eosinophils are important innate effector cells that protect the host against invading multicellular parasites, although they also play a deleterious role in allergic diseases. The earliest committed progenitor cell for eosinophils was identified to be positive for both CD34 and IL-5Ra. However, information concerning unique membrane markers to identify the subsequent stages of eosinophil maturation is very limited. In this study we identified multiple membrane markers that distinguish the different middle-late maturation stages of eosinophils in the bone marrow (BM) of healthy human volunteers. BM and peripheral blood were collected from 12 healthy volunteers. Eosinophilic promyelocytes, myelocytes, metamyelocytes and mature eosinophils were morphologically identified and sorted by flow cytometry according to their CD11b/CD62L expression. The expression of other antibodies against known membrane markers on eosinophils, LAIR1 (CD305), Alpha-4 (CD49d), CCR3 (CD193), FcγRIII (CD64), CR1 (CD35), CEACAM-8 (CD66b), SIGLEC-8, IL-5Ra (CD125) and IL-3Ra (CD123), was also determined.
Classically, eosinophils are considered as innate effector cells that are essential in protecting the host against invading multicellular parasites (particularly helminths) by releasing a variety of preformed potent granular mediators and producing toxic reactive oxygen species.1 The synergism between these two mechanisms arms these cells sufficiently to kill large pathogens, at least in vitro.2 At the same time, clonal proliferation of eosinophil precursors can lead to chronic eosinophilic leukemia, a disease accompanied by cardiovascular, respiratory and gastrointestinal symptoms.3
Despite the consensus regarding the importance of eosinophils in homeostasis and disease, remarkably little is known about their life cycle and maturation in the BM in homeostasis (“health”). It has been shown that IL-5R expression in BM-derived CD34+ myeloblasts characterizes the earliest committed eosinophil precursor.4,5 Nevertheless, the fate of these myeloblasts and the sub sequent maturation of eosinophil progenitors in the BM has not been studied so far. In this study, we developed a method to identify the different middle-late stages of eosinophil maturation in the BM of healthy volunteers by flow cytometry analysis. The information gained provides a first critical step in delineating mechanisms underlying normal eosinophil development and eosinophilic disorders.
Blood and BM samples were collected from 12 healthy male volunteers. None of the individuals had a prior history of atopic disease. BM aspirates were obtained from the iliac crest and blood was obtained by venipuncture. Blood was collected in tubes containing sodium heparin (Vacuette® Greiner bio-one, Kremsmünster, Austria) and BM aspirates were collected into Falcon tubes, which were prefilled with isotonic sodium heparin (sodium heparin 150 IU/mL: BM =1:3). Subsequently, erythrocytes were lysed using an ice cold lysis buffer (150 mM NH4Cl, 10 mM KHCO3 and 0.1 mM NA2EDTA). Thereafter, the remaining leukocytes were washed and resuspended in a staining buffer consisting of phosphate-buffered saline (PBS) supplemented with 0.32% w/v trisodium citrate (both prepared by the pharmacy of the University Medical Center Utrecht, the Netherlands) and 10% w/v human pasteurized plasma solution (Sanquin, Amsterdam, the Netherlands). One million cells at a concentration of 40x106 cells/mL were stained with antibodies for 30 min on ice, and washed twice before analysis on a LSR-Fortessa flow cytometer (Becton Dickinson, Mountain View, CA, USA). The following antibodies were used for staining: IL-3Ra-PerCP-Cy5.5 (clone 7G3), IL-5Rα-BV421 (clone A14), CD62L-BV650 (clone DREG-56) and LAIR1-PE (clone DX26) from Becton Dickinson; CD64-APC (clone 10.1), CD193-BV510 (clone 5E8), Siglec-8-PE (clone 7C9), CD66b PerCP-Cy5.5 (clone G10F5), CD16-BV785 (clone 3G8), CD49d-PE-Cy7 (clone 9F10) and CD35-FITC (clone E11) from Biolegend (San Diego, CA, USA); and CD11b-APC-AF750 (clone Bear1) from Beckman Coulter (Pasadena, CA, USA). The viabil ity of the whole BM samples was assessed separately by staining in PBS with the Fixable Violet Dead Cell Stain Kit (Life Technologies, Thermo Fisher Scientific, Waltham, MA, USA). Different cell populations were sorted using an Aria III FACS sorter (Becton Dickinson) and stained with May-Grünwald-Giemsa. Cells were then microscopically scored on the basis of nuclear morphology and cytosolic/granule staining.
The characteristics (mean ± standard error of mean) of the male volunteers were: age 23±1 years, weight 85±2 kg, height 1.84±0.02 m and body mass index 25.0±0.4 kg/m2. The concentration of blood eosinophils was 0.14±0.091x106 cells/mL.
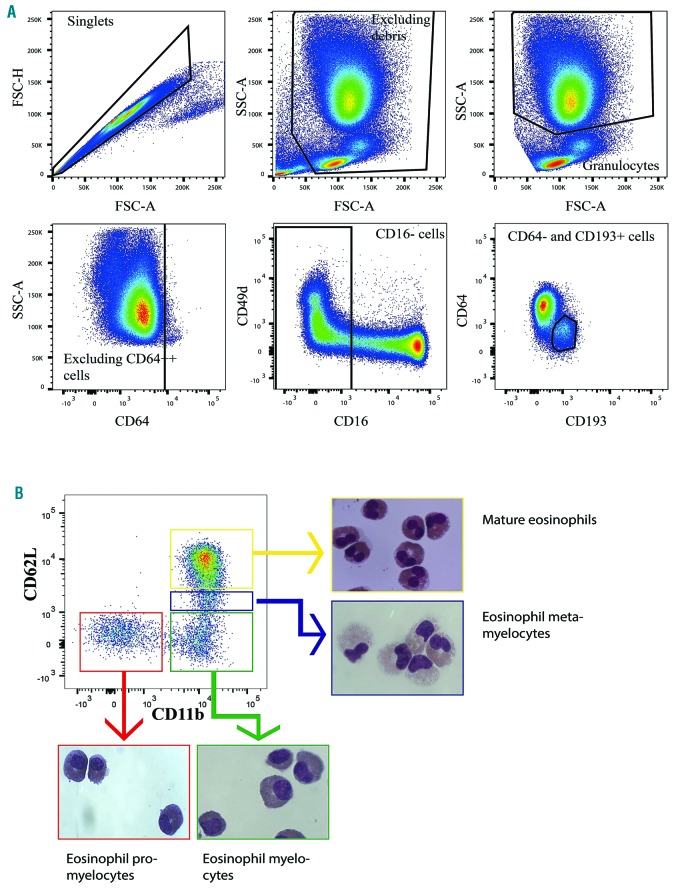
BM and blood eosinophils and their middle-late precursors were first identified based on their forward and side scatter (FSC/SSC) properties. Dead cells were excluded based on FSC and SSC. Cells with a high SSC were then gated, followed by exclusion of monocytes using CD64 expression. Subsequently eosinophils and their progenitors were identified as CD16−, CD64low and CD193+ cells (Figure 1A). We applied two markers, CD11b and CD62L to distinguish between immature and mature eosinophils. These two markers provided a similar expression pattern as is seen with CD16 and CD11b in neutrophils (Online Supplementary Figure S1).6 Analyzing both markers in a biplot revealed four different populations of cells in the eosinophil gate (Figure 1B). We applied fluorescence activated cell sorting and microscopic evaluation of cytospin preparations to isolate and morphologically assess these four different groups. Based on different nuclear morphology and cytosolic/granule staining, as described previously,7 we observed that CD11b− and CD62L− cells showed the characteristics of eosinophilic promyelocytes, CD11bbright and CD62L− cells those of eosinophilic myelocytes, CD11bbright and CD62Ldim cells those of eosinophilic metamyelocytes and finally CD11bbright and CD62Lbright cells resembled mature eosinophils (Figure 1B and Online Supplementary Figure S1). A direct comparison of cytospins from sorted neutrophilic and eosinophilic precursors showed that eosinophilic precursors were characterized by eosinophil-specific (dark) orange granules that were lacking in neutrophil precursors (Online Supplementary Figure S1). The purity of the different sorted populations was at least 80%. Staining cells separately for viability showed a viability of at least 95% and non-viable cells were eventually gated out on the basis of FSC and SSC and not analyzed.
Figure 1.
Gating strategy to identify eosinophils in blood and bone marrow. (A) Example of a gating strategy to identify all eosinophils and their progenitors in the bone marrow (BM). Granulocytes in blood and BM were identified on the basis of forward and side scatter (FSC/SSC). Monocytes were then excluded using CD64. Subsequently eosinophils and their progenitors were identified as CD16−, CD64low and CD193+ cells. (B) After gating all eosinophils and their progenitors, the different stages of eosinophil maturation can be identified using CD62L and CD11b. Representative cytospins are shown of sorted cells after staining the different stages of cells from each gate with May-Grünwald-Giemsa (light microscopy; objective used: 100x, Axioskop 40, Carl Zeiss, Goettingen, Germany).
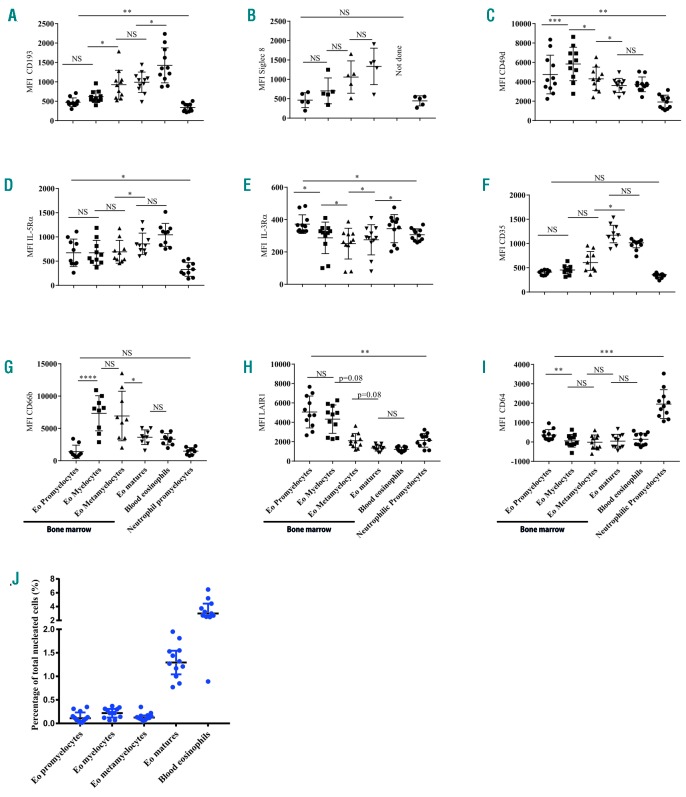
After validating our gating strategy, we then assessed putative changes in expression of eosinophil surface markers during maturation (Figure 2 and Table 1). Cell surface expression of the eotaxin receptor CCR3 (CD193) and Siglec-8 were both upregulated during maturation. The comparison of these markers with those on neutrophils and neutrophil progenitors, which do not express these proteins,8,9 indicated that eosinophilic promyelocytes and myelocytes also expressed both proteins at low levels (Figure 2 and Online Supplementary Figure S2). We also gated eosinophils and their progenitors independently of CD193 by using only CD64 and CD49d, because the initial gating strategy involved CD193 (Online Supplementary Figure S1). This alternative method showed a similar CD11b and CD62L biplot for eosinophil progenitors (Figure 1B). With this gating strategy we still detected higher expression of CD193 on eosinophilic promyelocytes than on neutrophilic promyelocytes (Figure 2A). The expression of the a chain of VLA-4 (CD49d) and CEACAM-8 (CD66b) reached peak levels during the myelocyte stage and expression of both proteins was maintained throughout maturation. (Figure 2C, G). This is in marked contrast to neutrophils, which lose CD49d expression after the myelocyte stage.10 The a-chain of the IL-5 receptor (CD125) was expressed during all stages of maturation, but the expression was highest on mature eosinophils in the BM and circulation (Figure 2D). The expression of the a chain of the IL-3 receptor (CD123) was quite variable amongst the different maturation stages (Figure 2E). However, the overall expression was low, limiting the interpretation of this finding.
Figure 2.
Expression of surface markers on eosinophil progenitors and mature cells. Cells were gated as described in Figure 1. Eosinophilic promyelocytes are CD11b− and CD62L−, eosinophilic myelocytes are CD11b+ and CD62L−, eosinophilic metamyelocytes are CD11b+ and CD62Ldim and mature eosinophils [in blood and bone marrow (BM)] are CD11b+ and CD62L+. The median fluorescence intensity (without subtraction of fluorescence minus one or isotype fluorescence) is plotted for the different surface markers of eosinophils in BM and blood, and their progenitors in the BM at baseline. Neutrophilic promyelocytes have been added as a negative control as a comparator. (A) CCR3 (CD193), (B) Siglec-8, (C) CD49d, (D) IL-5Ra (CD125), (E) IL-3Ra (CD123), (F) CR1 (CD35), (G) CEACAM-8 (CD66b), (H) LAIR1 (CD305), (I) FcγRI (CD64). (J) The percentages of total nucleated cells for the eosinophil precursors and eosinophils in blood and BM are shown. All results are presented as medians ± interquartile ranges. A Friedman test with an uncorrected Dunn test was performed. NS: not significant *P≤0.05, **P≤ 0.01 and ***P≤ 0.001. Eo: eosinophil; MFI: median fluorescence intensity.
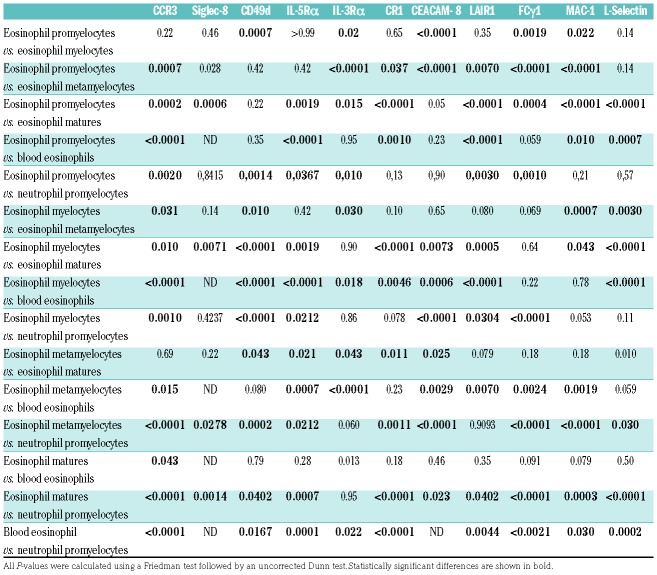
Table 1.
P-values of the comparison of the different surface markers between all stages of eosinophil maturation.
Similarly to neutrophils,11 the expression of complement receptor 1 (CD35) was late during maturation of eosinophils and was only found on mature eosinophils (Figure 2F). LAIR1 (CD305) was expressed on eosinophils at all stages of maturation, but its expression was highest during the promyelocyte and myelocyte stages. This expression pattern is comparable with that of neutrophils.12 Finally, Fcγ receptor I (CD64) was only expressed on eosinophil promyelocytes, and at a low level. This is in contrast to neutrophils, on which CD64 expression is maintained until the metamyelocyte stage.13
This is the first study characterizing different stages of eosinophil maturation in the human BM during homeostasis using the expression of a variety of membrane markers. This method did not provide clear indications for banded eosinophils as has been described for neutrophils.14 A limitation of this study is, however, the lack of other methods of validation, such as IL-5 responsiveness or differences in transcriptome of the different sorted populations. Nonetheless the distinct nuclear morphology and cytosol staining of the sorted populations in combination with a gradual increase in expression of several eosinophil markers on the cells at different stages of maturation will facilitate future studies focusing on differentiation in eosinophilic diseases.
Concerning the process of eosinophil maturation, we propose a model in which eosinophil progenitors are proliferating and maturing as if on a linear “conveyor belt”. A comparable model was first described for neutrophils in 1964 by Cartwright et al.15 It assumes that cells gradually go through each phase: proliferation and maturation of promyelocytes and myelocytes in a mitotic pool that is followed by maturation of metamyelocytes and mature cells in a post-mitotic pool. This hypothesis is supported by the observations that various surface markers such as CD193, IL-5Ra and Siglec-8 are gradually upregulated upon maturation and reach highest levels in mature, circulating eosinophils.
Supplementary Material
Acknowledgments
The authors thank Manita Bremmers, the physician who performed the bone marrow aspirations.
Footnotes
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
- 1.Meeusen EN, Balic A. Do eosinophils have a role in the killing of helminth parasites? Parasitol Today. 2000;16(3):95–101. [DOI] [PubMed] [Google Scholar]
- 2.Yazdanbakhsh M, Tai PC, Spry CJ, Gleich GJ, Roos D. Synergism between eosinophil cationic protein and oxygen metabolites in killing of schistosomula of Schistosoma mansoni. J Immunol. 1987;138(10):3443–3447. [PubMed] [Google Scholar]
- 3.Xiao Z, Zhang Y, Wang J, Hao Y. Study on clinical and laboratory Characteristics of chronic eosinophilic leukemia CEL/hypereosinophilic syndrome (CEL/HES). Blood. 2007;110(11):4637. [Google Scholar]
- 4.Sehmi R, Wood LJ, Watson R, et al. Allergen-induced increases in IL-5 receptor alpha-subunit expression on bone marrow-derived CD34+ cells from asthmatic subjects. A novel marker of progenitor cell commitment towards eosinophilic differentiation. J Clin Invest. 1997;100(10):2466–2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mori Y, Iwasaki H, Kohno K, et al. Identification of the human eosinophil lineage-committed progenitor: revision of phenotypic definition of the human common myeloid progenitor. J Exp Med. 2009;206(1):183–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loken MR, van de Loosdrecht A, Ogata K, Orfao A, Wells DA. Flow cytometry in myelodysplastic syndromes: report from a working conference. Leuk Res. 2008;32(1):5–17. [DOI] [PubMed] [Google Scholar]
- 7.Buitenhuis M. Cell Signalling during human eosinophil differentiation. Methods Mol Biol. 2014;1178:53–70. [DOI] [PubMed] [Google Scholar]
- 8.Höchstetter R, Dobos G, Kimmig D, Dulkys Y, Kapp A, Elsner J. The CC chemokine receptor 3 CCR3 is functionally expressed on eosinophils but not on neutrophils. Eur J Immunol. 2000;30(10):2759–2764. [DOI] [PubMed] [Google Scholar]
- 9.Floyd H, Ni J, Cornish AL, et al. Siglec-8. A novel eosinophil-specific member of the immunoglobulin superfamily. J Biol Chem. 2000;275(2):861–866. [DOI] [PubMed] [Google Scholar]
- 10.Lund-Johansen F, Terstappen LWM. Differential surface expression of cell adhesion molecules during granulocyte maturation. J Leukoc Biol. 1993;54(1):47–55. [DOI] [PubMed] [Google Scholar]
- 11.Ahearn JM, Fearon DT. Structure and function of the complement receptors, CR1 (CD35) and CR2 (CD21). Adv Immunol. 1989;46:183–219. [DOI] [PubMed] [Google Scholar]
- 12.Verbrugge A, de Ruiter T, Geest C, Coffer PJ, Meyaard L. Differential expression of leukocyte-associated Ig-like receptor-1 during neutrophil differentiation and activation. J Leukoc Biol. 2006;79(4):828– 836. [DOI] [PubMed] [Google Scholar]
- 13.Kerst JM, van de Winkel JG, Evans AH, et al. Granulocyte colony-stimulating factor induces hFc gamma RI (CD64 antigen)-positive neutrophils via an effect on myeloid precursor cells. Blood. 1993;81(6):1457–1464. [PubMed] [Google Scholar]
- 14.Schudel L. Leitfaden der Blutmorphologie: Manual of Bood Morphology. 11 edition. Zurich: Thieme; 1965. [Google Scholar]
- 15.Cartwright GE, Athens JW, Wintrobe MM. The kinetics of granulopoiesis in normal man. Blood. 1964;24:780–803. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.