Abstract
Background
In 2008, there were no pediatric radiologists in Ethiopia, a country of 100 million people. The radiology residency programs lacked training in pediatric imaging acquisition and interpretation.
Objective
We established an accredited local pediatric radiology fellowship program in Ethiopia.
Methods
With assistance from US faculty from the Children's Hospital of Philadelphia, Ethiopian radiologists created a 2-year fellowship training program in a university-based Ethiopian radiology residency program that incorporated formal lectures and seminars, case tutorials, journal clubs, teleradiological conferences, paper presentations, and online courses from collaborating institutions. Formal accreditation of the program was achieved from the university, and core values were established to ensure sustainability and self-sufficiency. The Ethiopian institution provided funding for the fellows, and US faculty volunteered their time.
Results
In 2015, 2 radiologists were recruited to the new fellowship; after graduation in 2017, they formed the first pediatric radiology section at the Ethiopian institution. Three new fellows were recruited in 2019, and the program is now self-sustaining. Pediatric imaging training has also been added to the radiology residency.
Conclusions
Establishing a pediatric radiology fellowship in a country with high need but little existing faculty expertise is feasible through outreach efforts.
What was known and gap
Despite its large population of children, Ethiopia had no pediatric radiologists or faculty to train new ones.
What is new
A local pediatric radiology fellowship program in Ethiopia that used faculty and resources from a US institution for implementation.
Limitations
Due to the brief follow-up period, it is not known if the program will need further outside resources and support. The institutions involved had a history of working together, and the model of collaboration might not be easily replicated.
Bottom line
Establishing a pediatric radiology fellowship in a country with high need but little existing faculty expertise is feasible through outside collaboration.
Introduction
A rise in global health activities and outreach has occurred in the past 2 decades, with global health programs increasingly emphasizing sustainability, effectiveness, and equality.1 As such, we have seen a shift from unilateral outreach to multilateral initiatives reaching for global health goals.2,3
The Children's Hospital of Philadelphia (CHOP) is a large urban tertiary care stand-alone pediatric center (560 beds) in the United States that has focused on global health for several decades, most recently via pediatric radiology programs in Ethiopia.4,5 Of the 100 million people living in Ethiopia, 60% are under the age of 20, and 44% are under the age of 14, yet in 2008, there were no pediatric radiologists in the country.6 Subsequently, there was a lack of expertise, teaching, and training in pediatric imaging in general radiology residency programs. With an increasing number of pediatric subspecialties, the need for adequate pediatric imaging services has grown even more.
Partnering with existing Ethiopian radiologists and programs, we expanded the pediatric radiology component in an Ethiopian institution's radiology residency and conducted regular national pediatric radiology continuing medical education (CME) courses. Ultimately, the purpose of this project was to establish an accredited local pediatric radiology fellowship program in Ethiopia.
Methods
Settings and Participants
At the start of this project, there were 33 medical schools in Ethiopia, 4 three-year radiology residency programs comprising 60 residents, and more than 200 radiologists.7 Two-year fellowships exist in adult body imaging, cardiothoracic imaging, and neuroradiology. At the start, there was no significant dedicated training in pediatric imaging during the radiology residency program.
The need for improved pediatric imaging was most pronounced at the country's main referral center located in Ethiopia's capital, Tikur Anbessa (translated to Black Lion Hospital [BLH]), affiliated with Addis Ababa University. Approximately 48% of admissions to this over 1000-bed hospital were children. The BLH Department of Radiology has approximately 20 attending radiologists. The BLH radiology facilities include one 1.5 Tesla magnetic resonance imaging machine, 2 computed tomography scanners (one 64 slice and one 128 slice), 7 ultrasound machines, 1 fluoroscopy suite, and digital radiography; however, no pediatric protocols existed for these modalities, and there were no policies for radiation reduction.
Intervention
Before CHOP started formal radiology outreach programs in 2008, individual radiologists had been traveling to Ethiopia to give lectures for the radiology residency at BLH once or twice per year. This evolved into a weeklong pediatric radiology lecture series and focused teaching. Most recently, we created an annual pediatric radiology CME course in collaboration with the Radiological Society of Ethiopia. These outreach programs began from the efforts of 1 radiologist and, subsequently, became a department-wide undertaking involving many faculty members from CHOP radiology as well as other US and international institutions.
Addis Ababa University supported the expansion of subspecialty training and research PhD programs in various departments. In addition, prior international collaborations at the hospital showed value and fostered successful partnerships.8 With an increase in pediatric clinical subspecialties at BLH, including surgery and oncology, and a neonatal intensive care unit, the radiology faculty recognized a need for dedicated pediatric imaging expertise. Furthermore, regular exposure to the breadth of pediatric imaging through visiting lectureships stimulated the BLH radiologists to advance their expertise.
Despite unanimous agreement that consolidated training in pediatric radiology was necessary, there was disagreement about how to implement it. Some of the Ethiopian faculty suggested sending local radiologists abroad for training with the expectation that they would return to Ethiopia. However, the financial incentives of remaining abroad to work and the well-documented “brain drain” phenomenon posed threats to this option.9 After exhaustive discussions at different levels, the fellowship model gained acceptance because of the potentially significant impact of this resource on an entire population and medical system. It also fulfilled a core value of our mission: the creation of self-sufficiency. Most importantly, the motivation for the model came from local faculty themselves, not the visiting physicians.
The following core values were considered essential for sustainability and self-sufficiency of the pediatric radiology fellowship: (1) empowering local radiologists to lead the curriculum design with support provided by visiting faculty; (2) securing formal accreditation of the program from the university; (3) establishing Ethiopia as the primary site of training; and (4) supporting on-the-job training of faculty with the goal to teach the teachers. As it was impractical to train these radiologists at CHOP unilaterally, the curriculum design included a majority presence in Ethiopia with local teaching supplemented by distance learning and a limited observership at CHOP, supported by CHOP's education funds and with observers covering their own travel expenses.
The training within the pediatric radiology fellowship program is based on the 6 Accreditation Council for Graduate Medical Education (ACGME) core competencies. The final curriculum was crafted through consensus expertise of CHOP radiologists and Ethiopian radiologists from BLH who had past pediatric radiology exposure abroad. Ethiopian faculty were tasked with adopting the curriculum to ensure its relevance to local pathology and disease management algorithms. The 34-page curriculum has been made available on the World Federation of Pediatric Imaging website.10 We based our education model on the 6-step approach for medical education curriculum development as outlined by Thomas and colleagues,11 which includes the following: (1) problem identification and general needs assessment; (2) needs assessment for targeted learners; (3) goals and objectives; (4) educational strategies; (5) implementation; and (6) evaluation and feedback.
In order to establish the credibility and visibility of the fellowship program and graduating pediatric radiologists with the university and the Ministry of Health, a 2-year process of formal accreditation through the university was undertaken. This involved gaining approval from the Academic Commission of the Faculty of Medicine, the Council of Graduate Studies, and the senate of the university.
Outcomes
After the curriculum was completed and accredited, the Department of Radiology selected 2 senior faculty members (n = 2 total possible participants) who had expressed interest throughout the planning process to become pediatric radiologists. Teaching formats included on-site training by visiting international pediatric radiologists (Figure 1) and distance learning that incorporated formal lectures and seminars, anonymized radiology case tutorials, journal clubs, participation in teleradiological conferences, paper presentations, and online courses from collaborating institutions or affiliates (including the World Federation of Pediatric Imaging and the Society for Pediatric Radiology10,12).
Figure 1.

Visiting Children's Hospital of Philadelphia Pediatric Neuroradiologists Teaching at Black Lion Hospital
Senior radiology faculty selected from among themselves a radiologist to be the director of the fellowship—someone who was already involved in residency education, had experience abroad, and could easily coordinate with the CHOP radiologists. A global assessment tool was developed for the faculty, including formative and summative assessment tools for the director to use on a semiannual basis. Periodic evaluation of the program itself was also conducted by the collaborating institutions. Fellows were required to complete online modules, maintain a logbook for all pediatric imaging and interventional activities, and collect all certificates of attendance at national and international professional meetings. The training culminated in a final oral examination conducted by international visiting faculty from CHOP and collaborating institutions. The fellows were paid according to the university-determined wages for trainees.
This project was considered exempt from review by the CHOP Institutional Review Board.
Results
In 2015, the pediatric radiology fellowship was successfully launched in Ethiopia with 2 fellows; it included components of distance learning, local instruction, a limited observership at CHOP, and a research requirement (Table). The fellows were periodically assessed to ensure that they were meeting ACGME competencies and milestones. During this 2-year fellowship, CHOP's radiology outreach lectures and CME meetings continued, providing additional opportunities for visiting faculty to assess the fellows and evaluate the program.
Table.
Required Educational Activities Needed to Complete the Radiological Fellowship
| Activity | Contact Hours | ECTS Equivalent | Credit Hours/Year | ||
| Lectures/tutorials and e-learning | 300 | 20 | 12.25 | ||
| Seminars/conferences | 10 | 0.4 | 0.25 | ||
| Clinical | 2560 | 102.4 | 62.2 | ||
| Clinical Activity | Year 1, Months | Year 2, Months | Contact Hours | ECTS Equivalent | Credit Hours |
| Ultrasound | 3 | 2 | 800 | 32 | 19.4 |
| MRI | 1 | 1 | 320 | 12.8 | 7.8 |
| Plain film | 2 | 1 | 480 | 19.2 | 11.6 |
| Fluoroscopy | 1 | 1 | 320 | 12.8 | 7.8 |
| Computed tomography | 1 | 1 | 320 | 12.8 | 7.8 |
| Intervention | N/A | 1 | 160 | 6.4 | 3.9 |
| Nuclear medicine | N/A | 1 | 160 | 6.4 | 3.9 |
| Research/external observership | 3 | 3 | N/A | N/A | N/A |
| Total | 11 | 11 | 2560 | 102.4 | 62.2 |
Abbreviations: ECTS, European Credit Transfer and Accumulation System; MRI, magnetic resonance imaging; N/A, not available.
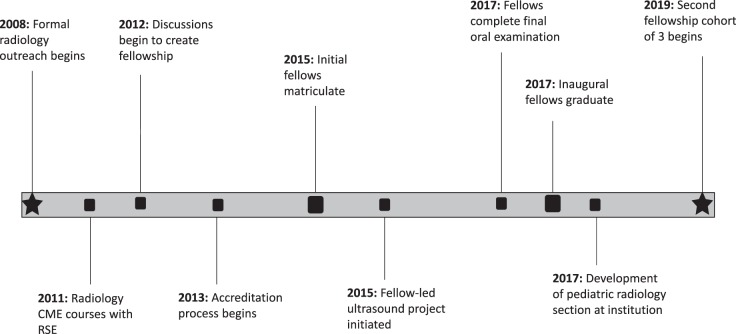
In 2017, the BLH Department of Radiology, in conjunction with CHOP, graduated its first 2 pediatric radiologists (Figure 2), who are currently based at BLH and have established a pediatric radiology section. One of the fellows has become the new director of the fellowship. Throughout this process, the university and radiology faculty at BLH have held the program in high regard. The pediatric radiology fellowship program has continued, and 3 fellows were recruited in 2019 (Figure 3). At the onset of the fellowship, the CHOP Department of Radiology played a significant role in planning until graduation. However, after successful graduation of the first cohort, the approach has been to transfer ownership of the program to the BLH Department of Radiology. Now CHOP primarily plays a supportive role to the program while BLH leads it.
Figure 2.
Graduation of Ethiopia's First Pediatric Radiologists, Dr Daniel Zewdneh (left) and Dr Yocabel Gorfu (right), From Black Lion Hospital After Successful Completion of the Fellowship Program
Figure 3.
Pediatric Radiology Fellowship Creation Timeline
Abbreviations: CME, continuing medical education; RSE, Radiological Society of Ethiopia.
Successful research projects from this program include a fellow-instituted initiative of implementing ultrasound-guided hydrostatic reduction; this novel method for treating intussusception has had a positive impact on patient care.13 Another focus of research was pediatric pulmonary hydatidosis. The fellows also took part in different research projects during their 3-month observership at CHOP.
Discussion
With outreach from a US institution's radiology department with a history of prior faculty teaching in Ethiopia, a large Ethiopian training institution successfully established the first 2-year pediatric radiology fellowship, with university accreditation, in a country with no existing pediatric radiologists and little pediatric training in radiology residencies. Although the visiting US faculty members were volunteer pediatric radiologists, they had to take time away from clinical activity and fund their travel. Many volunteers used funds from their personal CME budgets; external grants were rarely used. Many free online resources were available.10,12
Global health outreach should not be viewed as a zero-sum game but rather a win-win experience in which volunteers gain valuable experience.14,15 This international experience offered faculty opportunities to be visiting professors, exposure to low-resource radiology and clinical diseases otherwise not seen at their home institution, and opportunities for research collaboration.
In addition to the funding considerations described earlier, generalizability of this project may be limited by the specific institutions involved, which had a considerable prior history of working together; thus, other institutions may not be able to replicate this model. Although the self-sustaining goal appears to have been met, the follow-up time is brief; it will be vital to determine if additional US support or local resources are needed to continue this program. Also, the improvement of resident skills has not yet been assessed.
Given the ongoing need to find strategies to reduce brain drain from countries with a lack of critical specialists and an inadequate number of faculty to train new ones, it will be important to determine if this model of on-site residency enhancement and fellowship creation can be achieved at other sites and for other specialties. The resources needed to initiate and maintain these new programs should be determined for other settings.
Conclusions
It is feasible to establish a pediatric radiology fellowship in a host institution and country without subspecialized faculty through outreach from a program with extensive faculty expertise. Our experience suggests that the request for a fellowship should arise from the host country. Furthermore, the needs of key stakeholders in the host country should be identified, and these stakeholders should be fully engaged in the development process. Finally, accreditation should be sought and achieved, and fellowship training should be based in the host country.
Footnotes
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
This work was previously presented at the Society of Pediatric Radiology Annual Meeting, Memphis, Tennessee, May 15–19, 2018.
References
- 1.Center for Strategic and International Studies Global Health Policy Center. Global health programs and partnerships: evidence of mutual benefit and equity. 2019 https://csis-prod.s3.amazonaws.com/s3fs-public/publication/160315_Muir_GlobalHealthPrograms_Web.pdf Accessed December 2.
- 2.Frenk J, Gómez-Dantés O, Moon S. From sovereignty to solidarity: a renewed concept of global health for an era of complex interdependence. Lancet. 2014;383(9911):94–97. doi: 10.1016/S0140-6736(13)62561-1. [DOI] [PubMed] [Google Scholar]
- 3.Center for Strategic and International Studies. Sustainability and growth of university global health programs. 2019 http://csis.org/publication/sustainability-and-growth-university-global-health-programs Accessed December 2.
- 4.Children's Hospital of Philadelphia. Global health center. 2019 https://www.chop.edu/centers-programs/global-health-center Accessed December 2.
- 5.Ludwig S, Finalle R. Developing international partnerships with long-term impact. Clin Pediatr Emerg Med. 2012;13(1):44–48. doi: 10.1016/j.cpem.2011.12.002. [DOI] [Google Scholar]
- 6.Central Intelligence Agency. The World Factbook. 2019 https://www.cia.gov/library/publications/the-world-factbook/geos/et.html Accessed December 2.
- 7.Radiological Society of Ethiopia. Home page. 2019 http://www.ethiopianrads.com/ Accessed December 2.
- 8.University of Toronto. Toronto Addis Ababa academic collaboration. 2019 http://taaac.com/ Accessed December 2.
- 9.Kolars JC, Cahill K, Donkor P, Kaaya E, Lawson A, Serwadda D, et al. Perspective: partnering for medical education in sub-Saharan Africa: seeking the evidence for effective collaborations. Acad Med. 2012;87(2):216–220. doi: 10.1097/ACM.0b013e31823ede39. [DOI] [PubMed] [Google Scholar]
- 10.The World Federation of Pediatric Imaging. Pediatric radiology education. 2019 https://www.wfpiweb.org/Education/Radiologiststrainees.aspx Accessed December 2.
- 11.Thomas PA, Kern DE, Hughes MT, Chen BY. Curriculum Development for Medical Education A Six-Step Approach. Baltimore, MA: John Hopkins University Press; 2016. [Google Scholar]
- 12.Society for Pediatric Radiology. Educational resources. 2019 https://www.pedrad.org/Education/Resources Accessed December 2.
- 13.Wakjira E, Sisay S, Zember J, Zewdneh D, Gorfu Y, Kebede T, et al. Implementing ultrasound-guided hydrostatic reduction of intussusception in a low-resource country in sub-Saharan Africa: our initial experience in Ethiopia. Emerg Radiol. 2018;25(1):1–6. doi: 10.1007/s10140-017-1546-y. [DOI] [PubMed] [Google Scholar]
- 14.Sewankambo N, Tumwine JK, Tomson G, Obua C, Bwanga F, Waiswa P, et al. Enabling dynamic partnerships through joint degrees between low- and high-income countries for capacity development in global health research: experience from the Karolinska Institutet/Makerere University partnership. PLoS Med. 2015;12(2):1–8. doi: 10.1371/journal.pmed.1001784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Larkan F, Uduma O, Lawal SA, van Bavel B. Developing a framework for successful research partnerships in global health. Global Health. 2016;12(1):17. doi: 10.1186/s12992-016-0152-1. [DOI] [PMC free article] [PubMed] [Google Scholar]