Abstract
Background
Patients with heart failure (HF) and their family caregivers usually consume similar diets, but there is a lack of evidence about diet quality of patients with HF and their family caregivers.
Objective
The specific aim of this study was to compare diet quality of patients with HF with that of their family caregivers.
Methods
In this cross-sectional study, 40 patients with HF and their 40 family caregivers completed a VioScreen-Food Frequency Questionnaire from which Healthy Eating Index-2010 (HEI) diet quality scores (consisting of the total HEI score and 12 component scores) were calculated.
Results
None of the 40 patients-caregivers dyads had a high diet quality score (i.e., total HEI > 80), while 21% of participants had poor diet scores (i.e., total HEI≤50). There were no differences in total HEI scores (58.5 vs. 59.4, p=.58) or the 12 component scores of the HEI within dyads members. Mean scores of 6 of the 12 components (i.e., total fruit, greens and beans, total protein foods, seafood and plant proteins, fatty acids, empty calories) for both members of the HF dyad were below the national average. Interestingly, scores for the sodium component were similarly low in patients and caregivers (4.1 vs. 3.4, p=.24) indicating high sodium intake.
Conclusion
Both patients and caregivers consume poor quality diets that are high in sodium. These findings suggest that nutrition interventions to improve diet quality for patients with HF need to be targeted on the family as a unit.
Introduction
Heart failure (HF) is a major international public health concern because of its increasing prevalence and high direct health care costs related to repeated rehospitalizations.1,2 In America, HF affects 6.2 million adults and is responsible for more than 1 million hospital admissions yearly.1 The mortality rate of patients with HF is high with approximately 50% dying within 5 years of HF diagnosis.1 Worldwide, more than 26 million people are living with HF and up to 45% of patients with HF admitted to the hospital die within 1 year of admission.2
Despite an overall improvement in HF survival with current guideline-driven HF treatment,3 inadequate nutrition is identified a risk factor for poor long-term prognosis for patients.4,5 Unfortunately, the prevalence of malnutrition is high with as many as 70% of hospitalized patients with HF being malnourished.4,5 According to recent National Health Nutrition Examination Survey 24-hour dietary recall data (N=574), only 3.8% of people with HF met the dietary intake goal for fiber, 14% met the goal for saturated fat intake, and 27% met the goals for protein and cholesterol intake.6 Inadequate macro- and micronutrient intake are common in patients with HF.7,8 In addition, poor nutrition is associated with poor functional status, HF progression9,10 and increased mortality risk.11 Thus, maintaining adequate nutrition is particularly important for patients with HF to improve health outcomes.
Consuming a nutritionally balanced healthy diet may be more challenging for patients with HF compared to individuals who do not need to follow a specific dietary regimen. Polypharmacy, limited physical function, and psychological distress can depress appetite and lead to poor nutritional status in patients with HF.12 Having a non-supportive family member is also recognized as a major barrier to maintaining a healthy diet for patients with HF.13 Successful strategies for improving nutrition require support from family members who cook and shop for groceries.
Preparing meals and eating together are important social interactions that occur in families. Family members share the same household food resources in general and family members tend to have similar dietary patterns and mutually influence each others’ food choices.14–16 Evidence of similarities in dietary patterns and diet quality within family members has been shown among adult family members and their children,15 but there is a lack of evidence about similarities in diet quality among patients with a chronic disease and their family members. To date, diet quality has been studied only in patients with HF.6 There has been no comparisons of diet quality within dyad members, patients with HF and their primary family caregivers. Patients with HF who eat a sodium restricted diet and have multiple factors affecting their appetite may consume a lower quality diet than family members. However, this assumption has not been examined. The purpose of this study was to determine whether patients with HF ate a lower quality diet than their family caregivers. Our specific aim was to compare diet quality within dyad members consisting of patients with HF and their family caregivers. We hypothesized that patients with HF would consume a poorer quality diet than their family caregivers but that they would be better in limiting sodium consumption than their family members.
Methods
Sample and setting
This was a cross-sectional descriptive study of patient-caregiver dyads who completed data collection about diet quality while participating in the parent study, the Family Sodium Watchers Program clinical trial. The Family Sodium Watchers Program is a randomized controlled study designed to improve adherence to a sodium restricted diet in patients with HF and their family caregivers (clinical trial #). Eligible patients and their primary family caregivers were recruited at outpatient clinics. Eligible patients were outpatients with HF living with a family caregiver and both needed to speak and write English. We excluded patients who were younger than 20 years old or who had another terminal illness (i.e., end-stage of kidney disease, cancer), or severe cognitive impairment (i.e., dementia or Alzheimer’s disease). Eligible family members were primary caregivers identified by patients who lived with the patient. Any family members who had a major medical comorbidity such as cancer, terminal illness, or severe cognitive impairment were excluded.
Procedures
The study was approved by the Institutional Review Board. Potentially eligible patients and their family caregiver were referred by health care providers. A trained nurse researcher confirmed eligibility via medical record review. Eligible participants were contacted during outpatient clinic visits. In the parent study, after informed consent was obtained from both patients and their family caregivers, they completed data collection at their home. All participants were instructed to complete the questionnaires without discussing them with each other. When trained research staff visited participants’ homes, they reviewed the questionnaires or assisted participants to complete them. For this cross-sectional study, we additionally collected diet quality data from those dyads who agreed to participate in this substudy and 40 dyads completed diet quality data.
Measures
Diet Quality
Healthy Eating Index-2010 (HEI) diet quality scores were calculated from the VioScreen Food Frequency Questionnaire (Vio-FFQ) data.17 The HEI-2010 is composed of 9 diet adequacy components and 3 diet moderation components. Adequacy components include total fruit (5 points), whole fruit (5 points), total vegetables (5 points), greens and beans (5 points), whole grains (10 points), dairy (10 points), total protein foods (5 points), seafood and plant proteins (5 points), and fatty acids (10 points). Higher scores indicate more consumption of these components. Moderation components are those recommended to be limited in the diet and include refined grains (10 points), sodium (10 points), and empty calories (i.e., energy from solid fats, alcohol and added sugars; 20 points). Higher scores indicate less consumption of these components. Total HEI score (range 0–100) is the sum of 12 component scores with higher scores indicating better conformance with healthy eating dietary guidelines. A total score below 50 is indicative of a low quality diet; scores between 51 to 80 correspond to a diet that requires improvement; scores above 80 correspond to a healthy diet.18 Validity and reliability (Cronbach’s coefficient α= 0.7) of the HEI-2010 have been established using the National Health Nutrition Examination Survey.19,20
Demographic characteristics
Demographic characteristics (i.e., age, gender, ethnicity, and education) were obtained from patients and caregivers by structured questionnaire. Patients’ clinical characteristics (i.e., left ventricular ejection fraction, New York Heart Association functional class, and medication) were obtained by interview and medical record review using a structured questionnaire. Perceived financial status was obtained using one item with three response options: (1) not having enough to make ends meet, (2) having enough to make ends meet, and (3) having more than enough to make ends meet.
Analysis
Descriptive statistics (i.e., frequency, percentile, mean, standard deviation) were used to describe sample characteristics. Paired t-test and chi-square were used to describe difference in sample characteristics (i.e., age, gender, marital status, ethnicity, education) within dyad members. Paired t-tests and Pearson correlations on were used to compare diet quality (HEI total score and 12-component scores) within the two members of the dyad. All analysis was conducted with SPSS version 25.
Results
Demographic characteristics
A total of 80 adults (40 patients with HF and 40 caregivers) completed data collection. Table 1 presents comparison of demographic characteristics within dyad members. The mean age of the whole sample was 59.7 years (SD=16.4). Most were married (86%) and non-Hispanic white (81%). About one third completed high school or less. Among the 40 dyads, 75% were in spousal relationships. Dyad members differed in age and gender. Patients were 5 years older on average than their caregivers (P = .014) and were predominantly male (60%) while family caregivers were predominately female (80%) (P <.001).
Table 1.
Characteristics of participants (N=80; 40 dyads)
| Characteristics | Total sample (N=80) | Patients (n=40) | Caregivers (n=40) | Paired- t test/ χ2 P-value |
|---|---|---|---|---|
| Mean ± SD or n (%) | ||||
| Age, years | 59.7 ± 16.4 | 62.6 ± 15.2 | 57.6± 17.1 | .014 |
| Gender, male | 32 (40.0%) | 24 (60%) | 8 (20.0%) | < .001 |
| Marital status, married/ co-habitants | 69 (86.3%) | 36 (90%) | 33 (82.5%) | < .001 |
| Ethnicity, non-Hispanic white | 65 (81.3%) | 31 (77.5%) | 33 (82.5%) | < .001 |
| Education, ≤ High school diploma | 26 (32.5%) | 11 (27.5%) | 15 (37.5%) | .273 |
Half of the patients (52.5%) reported their financial status as having enough to make ends meet; 27.5% patients reported not having enough to make ends meet and 20% reported themselves as comfortable and having more than enough to make ends meet. Most patients were in New York Heart Association functional Class II (42%) or III (55.3%), and prescribed beta blockers (84%), diuretics (95%), and angiotensin-converting enzyme inhibitors (58%).
Diet quality
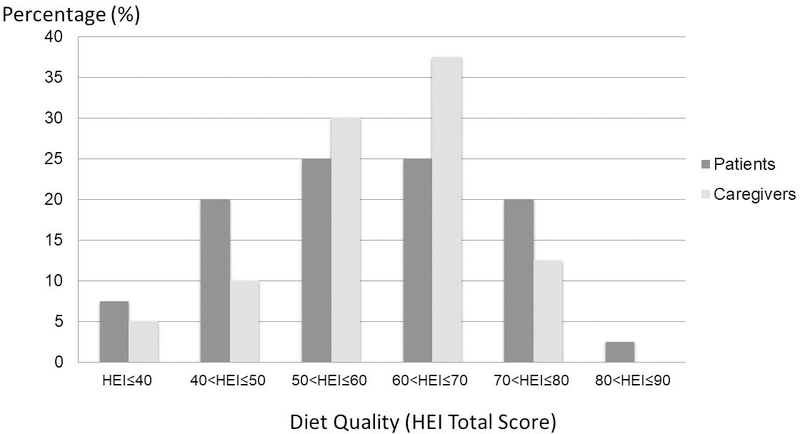
Figure 1 presents the distribution of total HEI scores of patients and caregivers. Only one patient and no caregivers had a high HEI score (total HEI > 80), whereas 21% of participants (11 patients and 6 caregivers) had low diet quality scores (total HEI ≤ 50). Both members of 4 (10%) out of the 40 dyads had low diet quality scores (total HEI < 50) while both members of 2 dyads (5%) achieved diet quality scores greater than 70.
Figure 1.
Distribution of overall diet quality score in patients and caregivers percentage (%)
Total HEI scores were significantly associated with age (r = .32, P = .04) for patients but not for caregivers (r = .20, P= .21). There were no differences in mean total HEI scores between male and female patients (male = 59.1 vs. female = 57.6, P = .74) or caregivers (male = 59.0 vs female = 59.7, P = .89) as well as among financial status groups (comfortable = 66.5 ± 14.2, enough to make ends meet = 58.8 ± 11.6, not enough = 52.1 ± 14.9, P = .07).
Comparison of diet quality within dyad members
Table 1 presents comparison of diet quality within dyad members (i.e., patients and family caregivers). There was no significant difference in total HEI scores within dyad members (58.8 vs. 59.4, P = .58, respectively), which were also highly correlated (Pearson r = .706; P < .05). There was also no statistical difference in mean scores within dyad members for any of the 12 individual HEI components including sodium scores (4.1 vs. 3.4, respectively; P = .24). There were strong to moderate correlations of diet quality scores in 10 of the components (Pearson correlation ranges 0.383 – 0.614, P < .05) within dyad members, with the strongest correlation being fatty acids (r = .614, P < .05). In contrast, there was no significant correlation of sodium scores (r = .275, P > .05) or dairy consumption scores (r = .077, P > .05) within dyad members.
Discussion
This study adds to the limited research on diet quality of patient-caregiver dyads in HF. We hypothesized that diet quality in patients with HF would be lower than that of family caregivers because of multiple factors that potentially affect their diet. The principal finding in this study, however, was that the diet quality within patient-caregiver dyad members was similar. In a national survey study (n = 4356) using the HEI-2005, American patients with diet-related chronic diseases (at least one or more chronic disease among diabetes, hypertension, heart disease, hypercholesterolemia, or cancer) were found to have healthier diets and better quality of diets than non-patients.21 When each disease was examined separately, patients with diabetes and hypercholesterolemia had better diet quality than non-patients while patients with heart disease or hypertension had diet quality similar to non-patients. However, non-patient groups were individuals who were not in interdependent relationship as same were the participants in this study. Our findings of similar diet quality in both members of a family dyad provides additional evidence that a diagnosis of HF is not associated with healthier dietary behaviors.
The similarity of diet quality in this study could be explained by family environment. Family members generally consume the same diet. It is common that food choices are made by the family member who shops for and cooks meals. As patients with HF become dependent on caregivers or family members, they eat what is served to them, which can lead to changes in food preference. For example, family members’ preferences for vegetables are associated with the foods served at family meals.16 Although the importance of family support to adherence to the dietary regimen in HF (i.e., sodium restricted diet) has been suggested and family-focused education and support intervention improved adherence to sodium restricted diet in patients with HF,22 how caregivers influence patients’ diet quality or healthy dietary behaviors has not been studied.
The diet quality seen in this study sample was lower than the dietary quality of a national sample from the National Health Nutrition Examination Survey.19 The low quality of diets in this study may be not surprising given the living environment. The sample in this study was from an austere rural region where fried and calorie-dense foods (e.g., bacon, fried potatoes) are favored. In economically poor regions, families experience food insecurity and often consume processed foods because healthier foods cost are more expensive.23 Although there was not a significance association between self-reported financial status and diet quality in our study, perhaps due to sample size, there was a trend for patients who reported being financially comfortable to have better diet quality than those who reported financial strain. Further investigation with a larger sample is needed to determine whether environmental or family financial factors predict the quality of diet in HF patients and family caregivers.
The low scores for the sodium component of the HEI for both patients and caregivers indicates sodium intake above recommended levels. Thus, despite recommendations to follow a low sodium diet, patients did not successfully limit sodium and consumed levels of sodium similar to their family caregivers. Interestingly, sodium was one of the few components of the HEI where patient and caregiver scores were not significantly correlated. We previously reported that patients with HF were 2.3 times more likely to be adherent to a sodium restricted diet when their family member ate a low sodium diet than patients whose family member did not eat low sodium diet.13 The American Heart Association recommends that all adults limit sodium intake to less than 2,300mg per day with an ideal limit of no more than 1,500mg to prevent CVD development.1 Consequently, caregivers should also limit sodium intake. Thus, a family intervention approach may be needed to improve adherence to a sodium restricted diet.
Researchers have emphasized the importance of maintaining good nutritional status to improve health outcomes of patients with HF.4,7,9 Our data suggest that the focus on patients may underestimate the families’ influence on patients’ dietary management. Given the fact that caregivers are vulnerable to physical health problems and at high risk of cardiovascular disease due to their caregiving responsibility24–26 it is equally important for them to engage in a health promoting life style that includes eating a healthy diet. However, caregivers who are more highly burdened are less likely to engage in eating a heart healthy diet compared to caregivers who do not report such burden.25 Thus, there is a need for family intervention programs that not only improve sodium intake but also improve overall diet quality for caregivers and patients.
Limitations
This study has several limitations. The relatively small sample size (80 individuals =40 dyads) from one region of a southern state in the United States can limit generalizability of the findings. The sample was also homogenous with respect to ethnicity and the majority of the dyads represented spousal relationships which may not reflect the diversity of the HF population. Diet quality was assessed by self-report food frequency which may have produced measurement error related to recall bias.
Conclusion
This study provided new evidence that the diet quality of patients with HF and their family caregivers who are in interdependent relationships is similar and is lower in quality than that of Americans without HF. This similarity in diet and low levels of diet quality suggests that improving diet quality is of equal importance for patients with HF and their family caregivers. Thus, nutrition interventions should be aimed toward the family as a unit.
Table 2.
Diet Quality between patients and caregivers dyads (N = 40 dyads)
| Components | Maximum points | Patients with HF | Family caregivers | Paired t-test p-value | Correlation r (* P < .05) |
|---|---|---|---|---|---|
| Adequacy: | |||||
| Total fruit | 5 | 2.59 ± 1.75 | 3.02 ± 1.54 | .123 | .445* |
| Whole fruit | 5 | 3.20 ± 1.89 | 3.55 ± 1.67 | .177 | .588* |
| Total vegetables | 5 | 4.00 ± 1.29 | 4.30 ± 1.12 | .158 | .407* |
| Greens and beans | 5 | 3.21 ± 1.86 | 3.19 ± 1.58 | .920 | .600* |
| Whole grains | 10 | 3.85 ± 3.27 | 3.52 ± 3.02 | .480 | .577* |
| Dairy | 10 | 5.23 ± 2.13 | 5.98 ± 2.48 | .141 | .077 |
| Total protein foods | 5 | 4.27 ± 1.14 | 4.50 ± 0.90 | .155 | .532* |
| Seafood and plant proteins | 5 | 3.66 ± 1.68 | 3.38 ± 1.74 | .239 | .620* |
| Moderation: | |||||
| Fatty acids | 10 | 4.36 ± 3.28 | 4.33 ± 3.33 | .940 | .614* |
| Refined grain | 10 | 8.67 ± 1.82 | 8.22 ± 2.22 | .210 | .383* |
| Sodium | 10 | 4.10 ± 3.28 | 3.34 ± 2.93 | .204 | .275 |
| Empty calories | 20 | 11.35 ± 6.05 | 12.04 ± 5.19 | .475 | .432* |
| Total HEI Score | 100 | 58.8 ± 13.70 | 59.35 ± 11.16 | .584 | .706* |
Acknowledgements
Funding was received from the National Institutes of Nursing Research (R01NR012967, principal investigator: ML Chung). We thank the University of Kentucky HealthCare, University of Kentucky Center for Clinical and Translational Science (UL1TR001998), and the Norton Healthcare, and staff of the RICH Heart Program.
Footnotes
Conflict: The authors have no conflict of interest to disclose.
Contributor Information
Misook L. Chung, College of Nursing, University of Kentucky, Lexington, Kentucky, USA.
Suk Jeong Lee, Red Cross College of Nursing, Chung Ang University, Seoul, Republic of Korea.
Debra K. Moser, College of Nursing, University of Kentucky, Lexington, Kentucky, USA.
JungHee Kang, College of Nursing, University of Kentucky, Lexington, Kentucky, USA.
Terry A. Lennie, College of Nursing, University of Kentucky, Lexington, Kentucky, USA.
References
- 1.Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019;139(10):e56–e66. [DOI] [PubMed] [Google Scholar]
- 2.Ponikowski P, Anker SD, AlHabib KF, et al. Heart failure: preventing disease and death worldwide Ponikowski, P. ESC Heart Fail. 2014;1(1):4–25. [DOI] [PubMed] [Google Scholar]
- 3.Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation. 2018;137(12):e67–e492. [DOI] [PubMed] [Google Scholar]
- 4.Bonilla-Palomas JL, Gamez-Lopez AL, Anguita-Sanchez MP, et al. [Impact of malnutrition on long-term mortality in hospitalized patients with heart failure]. Rev Esp Cardiol. 2011;64(9):752–758. [DOI] [PubMed] [Google Scholar]
- 5.Narumi T, Arimoto T, Funayama A, et al. Prognostic importance of objective nutritional indexes in patients with chronic heart failure. J Cardiol. 2013;62(5):307–313. [DOI] [PubMed] [Google Scholar]
- 6.Lemon SC, Olendzki B, Magner R, et al. The dietary quality of persons with heart failure in NHANES 1999–2006. J Gen Intern Med. 2010;25(2):135–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grossniklaus DA, O’Brien MC, Clark PC, Dunbar SB. Nutrient intake in heart failure patients. J Cardiovasc Nurs. 2008;23(4):357–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sanchez-Tainta A, Zazpe I, Bes-Rastrollo M, et al. Nutritional adequacy according to carbohydrates and fat quality. Eur J Nutr. 2016;55(1):93–106. [DOI] [PubMed] [Google Scholar]
- 9.Aquilani R, Opasich C, Verri M, et al. Is nutritional intake adequate in chronic heart failure patients? J Am Coll Cardiol. 2003;42(7):1218–1223. [DOI] [PubMed] [Google Scholar]
- 10.Rifai L, Silver MA. A Review of the DASH Diet as an Optimal Dietary Plan for Symptomatic Heart Failure. Prog Cardiovasc Dis. 2016;58(5):548–554. [DOI] [PubMed] [Google Scholar]
- 11.Anker SD, Ponikowski P, Varney S, et al. Wasting as independent risk factor for mortality in chronic heart failure. Lancet. 1997;349(9058):1050–1053. [DOI] [PubMed] [Google Scholar]
- 12.Lennie TA, Moser DK, Heo S, Chung ML, Zambroski CH. Factors influencing food intake in patients with heart failure: a comparison with healthy elders. J Cardiovasc Nurs. 2006;21(2):123–129. [DOI] [PubMed] [Google Scholar]
- 13.Chung ML, Lennie TA, Mudd-Martin G, Moser DK. Adherence to a low-sodium diet in patients with heart failure is best when family members also follow the diet: a multicenter observational study. J Cardiovasc Nurs. 2015;30(1):44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gillespie A, Gillespie G. Family food decision-making: an ecological system framwork. Journal of Family and Consumer Science. 2007;99(2):22–27. [Google Scholar]
- 15.Wang Y, Beydoun MA, Li J, Liu Y, Moreno LA. Do children and their parents eat a similar diet? Resemblance in child and parental dietary intake: systematic review and meta-analysis. J Epidemiol Community Health. 2011;65(2):177–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wenrich TR, Brown JL, Miller-Day M, Kelley KJ, Lengerich EJ. Family members’ influence on family meal vegetable choices. J Nutr Educ Behav. 2010;42(4):225–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Viocare. VioScreen. Published 2019. Accessed 10/25/2018.
- 18.Kennedy ET, Ohls J, Carlson S, Fleming K. The Healthy Eating Index: design and applications. J Am Diet Assoc. 1995;95(10):1103–1108. [DOI] [PubMed] [Google Scholar]
- 19.HEI-2010 Total and components scores for children, adults, and old adults during During 2011–2012. U.S. Department of Agriculture Food and Nurtition Service. HEI Scores for American Web site. Accessed 2019. [Google Scholar]
- 20.Guenther PM, Kirkpatrick SI, Reedy J, et al. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J Nutr. 2014;144(3):399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen X, Cheskin LJ, Shi L, Wang Y. Americans with diet-related chronic diseases report higher diet quality than those without these diseases. J Nutr. 2011;141(8):1543–1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dunbar SB, Clark PC, Stamp KD, et al. Family partnership and education interventions to reduce dietary sodium by patients with heart failure differ by family functioning. Heart & Lung. 2016;45(4):311–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hardin-Fanning F, Rayens MK. Food cost disparities in rural communities. Health Promot Pract. 2015;16(3):383–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bidwell JT, Vellone E, Lyons KS, et al. Caregiver determinants of patient clinical event risk in heart failure. Eur J Cardiovasc Nurs. 2017;16(8):707–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hooker SA, Schmiege SJ, Trivedi RB, Amoyal NR, Bekelman DB. Mutuality and heart failure self-care in patients and their informal caregivers. Eur J Cardiovasc Nurs. 2018;17(2):102–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee S, Colditz GA, Berkman LF, Kawachi I. Caregiving and risk of coronary heart disease in U.S. women: a prospective study. Am J Prev Med. 2003;24(2):113–119. [DOI] [PubMed] [Google Scholar]