Abstract
Objective
This paper reports a qualitative study of a home-based stroke telerehabilitation system. The telerehabilitation system delivers treatment sessions in the form of daily guided rehabilitation games, exercises, and stroke education in the patient’s home. The aims of the current report are to investigate patient perceived benefits of and barriers to using the telerehabilitation system at home.
Methods
We used a qualitative study design that involved in-depth semi-structured interviews with 13 participants who were patients in the subacute phase after stroke and had completed a six-week intervention using the home-based telerehabilitation system. Thematic analysis was conducted to analyse the data.
Results
Participants mostly reported positive experiences with the telerehabilitation system. Benefits included observed improvements in limb functions, cognitive abilities, and emotional well-being. They also perceived the system easy to use due to the engaging experience and the convenience of conducting sessions at home. Meanwhile, participants pointed out the importance of considering technical support and physical environment at home. Further, family members’ support helped them sustain in their rehabilitation. Finally, adjusting difficulty levels and visualizing patients’ rehabilitation progress might help them in continued use of the telerehabilitation system.
Conclusion
Telerehabilitation systems can be used as an efficient and user-friendly tool to deliver home-based stroke rehabilitation that enhance patients’ physical recovery and mental and social-emotional wellbeing. Such systems need to be designed to offer engaging experience, display of recovery progress, and flexibility of schedule and location, with consideration of facilitating and social factors.
Keywords: stroke rehabilitation, telehealth, home-based, information technologies, qualitative study
Introduction
Stroke is a leading cause of serious and long-term disability in the United States [1]. After the initial days-weeks of acute care followed by rehabilitation therapy, patients with stroke still have a long and tedious recovery process in front of them, involving return of physical, speech, cognitive, and other functions. With the advance of information technologies (IT), numerous studies have investigated the feasibility and effectiveness of new tools and their design towards the purpose of facilitating additional methods to provide rehabilitation after stroke [2–12]. Telerehabilitation, which allows patients to conduct therapy with therapists using telecommunication technology, has been widely deployed for stroke recovery and opens up new opportunities for remote therapy that makes rehabilitation more accessible, especially for patients in rural areas and facing transportation obstacles [7, 10, 11]. Virtual reality has also been used in post-stroke therapy in upper limb motor functions, balance control and gait, lower limbs, and walking [12]. Additionally, prior work has also repurposed commercial video games, such as Kinect, and Wii, for stroke rehabilitation [13] to make the rehabilitation experience engaging.
In parallel, there has been an increasing amount of work that helps patients conduct rehabilitation at home. Home-based technologies allow flexibility of location and time in delivering rehabilitation therapy. Most systems and studies evaluate the success of a system by the clinical outcome such as motor and functional abilities. Very few works have addressed patients’ acceptance – beyond clinical requirements – in designing IT tools for stroke rehabilitation, which requires in-depth study on patients’ experiential data. Furthermore, the use of rehabilitation technologies in the home environment, independently, is a complex process, which requires contextual understanding of patients’ rehabilitation experience in the home setting. To this end, we aim to understand the acceptance of home-based stroke rehabilitation system from patients’ subjective experience.
In this paper, we explore the user acceptance of a home-based stroke rehabilitation system. A pilot study of an earlier version of this system found high compliance and significant motor gains [14]. The current system delivers treatment sessions in the form of daily guided rehabilitation games, exercises, and stroke education in the patients’ homes, with no live contact with study therapists. The telerehabilitation system also offers supervised therapy sessions guided by a study therapist through videoconferencing. To explore the subjective experience of the home-based stroke telerehabilitation system, we conduct a qualitative interview study with 13 patients who completed a six-week trial of using the telerehabilitation system.
Methods
We used a qualitative study design that involved in-depth semi-structured interviews with 13 patients with stroke who were enrolled in a clinical trial of arm motor rehabilitation therapy and were randomized at University X to receive a six-week intervention program using a novel home-based telerehabilitation system designed to improve motor recovery and patient education after stroke [15]. All interviews and data analysis were performed blinded to all study-related assessments. See Appendix 4 for COREQ Guidelines checklist.
Recruitment
The study was conducted in Southern California. Participants were recruited by referral from their doctors, therapists, and hospitals where they received health care services. Participants contacted the research team if they were interested in the study. They then underwent initial assessment on the functional abilities of their upper limbs by a licensed physical or occupational therapist who was part of the research team during the screening visit. The inclusion and exclusion criteria for study eligibility are shown in Table 2.
Table 2.
Inclusion and exclusion criteria for patients enrolled in the study program.
| Inclusion Criteria: |
| 1.Age ≥18 years at the time of randomization |
| 2.Stroke that is radiologically verified, due to ischemia or to intracerebral hemorrhage, |
| and with time of stroke onset 4–36 weeks prior to randomization |
| 3.Arm motor FM score of 22–56 (out of 66, higher is better) at the Screening Visit |
| 4.Box & Block Test score with affected arm is at least 3 blocks in 60 seconds at the |
| Screening Visit |
| 5.Informed consent signed by the subject |
| 6.Behavioral contract signed by the subject |
| Exclusion Criteria: |
| 1.A major, active, coexistent neurological or psychiatric disease, including alcoholism or dementia |
| 2.A diagnosis (apart from the index stroke) that substantially affects paretic arm function |
| 3.A major medical disorder that substantially reduces the likelihood that a subject will be able to comply with all study procedures |
| 4.Severe depression, defined as Geriatric Depression Scale Score >10 |
| 5.Significant cognitive impairment, defined as Montreal Cognitive Assessment score < 22 |
| 6.Deficits in communication that interfere with reasonable study participation |
| 7.A new symptomatic stroke has occurred since the index stroke that occurred 4–36 weeks prior to randomization |
| 8.Lacking visual acuity, with or without corrective lens, of 20/40 or better in at least one eye |
| 9.Life expectancy < 6 months |
| 10.Pregnant |
| 11.Receipt of Botox to arms, legs, or trunk in the preceding 6 months, or expectation that Botox will be administered to the arm, leg, or trunk prior to completion of the 30 Day Follow-Up Visit |
| 12.Unable to successfully perform all three of the rehabilitation exercise test examples |
| 13.Unable or unwilling to perform study procedures/therapy, or expectation of noncompliance with study procedures/therapy |
| 14.Concurrent enrollment in another investigational study |
| 15.Non-English speaking, such that subject does not speak sufficient English to comply with study procedures |
| 16.Expectation that subject cannot participate in study visits |
| 17.Expectation that subject will not have a single domicile address during the six weeks of therapy, within 25 miles of the central study site and with Verizon wireless reception. |
Intervention
The telerehabilitation system is comprised of four main components: games, exercises, education, and telecommunication (Table 1 Figure 1). The system delivers treatment sessions in the form of daily guided rehabilitation games, exercises, and stroke education in the patient’s home. See Appendix 2 for the procedure of the intervention. In this trial, for subjects randomized to the telerehabilitation group, members of the research team delivered the telerehabilitation system to the subject’s home, set it up, confirmed functionality, and reviewed use of the system with the subject. Patients were assigned a guided rehabilitation program using the system for 70 minutes at a fixed time every day, 6 days per week, over 6–8 weeks.
Table 1.
Key components of the telerehabilitation system.
| • Table |
| • Folding chair |
| • Computer with monitor, microphone, and speakers |
| • Verizon wireless modem |
| • Myo Band |
| • Wiimote in a pistol-shaped holder |
| • PowerMate |
| • PlayStation 3 Eye Move Controller |
| • Joystick |
| • Logitech Trackpad |
| • Standard rehabilitation therapy devices for the upper extremity |
Figure 1.
An example of a patient interacting with a treatment therapist using the telerehabilitation system during a supervised session
Data collection methods
We conducted interviews with 13 patients who completed the study and were randomized to the telerehabilitation group. All 13 participants who were contacted agreed to participate in the semi-structured interview. Among them, nine of the interviews were conducted at participants’ homes where the devices had been installed, and four interviews were conducted at the university enrolment site. Nine patient participants were accompanied by one caregiver who helped clarify or supplement the answers. The average age of the participants was 70.52. The patient participated in the clinical trial between 4 and 36 weeks after their stroke onset. Detailed demographic information was listed in Table 3.
Table 3.
Demographic data of interviewed patient participants
| ID | Gender | Side of stroke | Age | Accompany | Interview location |
|---|---|---|---|---|---|
| 1 | Male | Right | 67 | N/A | Home |
| 2 | Female | Left | 72 | Spouse | Home |
| 3 | Male | Left | 80 | Spouse | Home |
| 4 | Male | Right | 62 | Spouse | Home |
| 5 | Male | Right | 84 | Spouse | Home |
| 6 | Male | Right | 82 | Spouse | Home |
| 7 | Female | Right | 63 | Elder sister | University |
| 8 | Male | Right | 86 | Spouse | Home |
| 9 | Male | Right | 77 | Spouse | Home |
| 10 | Male | Left | 75 | Spouse | Home |
| 11 | Male | Left | 52 | N/A | University |
| 12 | Male | Left | 55 | N/A | University |
| 13 | Male | Left | 63 | N/A | University |
After obtaining informed consent from participants to take part in the current qualitative research study, we interviewed them and asked questions about their history of stroke and treatment, motivation in participating in their study, experience in using the telerehabilitation system, and intention to use the system in the future. See Appendix 3 for the complete list of questions. With participants’ permissions, we audio recorded the interviews. Participants were informed that they could discontinue the interview at any time. Each interview took around one hour. Subjects were provided $25 as compensation for their time.
Data Analysis
All interviews were transcribed verbatim. We removed identifiable data and replaced patient names with pseudonyms to protect participant’s privacy. We input the transcripts into DeDoose, a web application for qualitative data analysis.
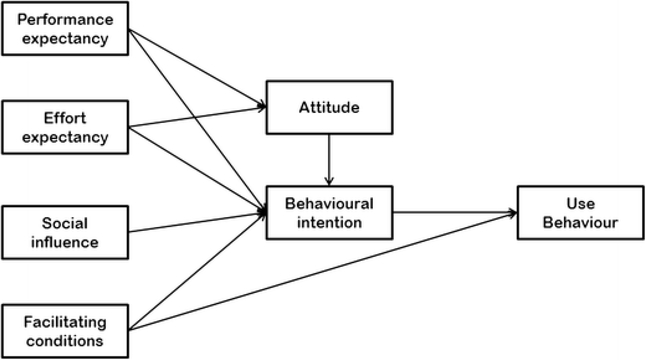
We analysed user acceptance of the telerehabilitation system based on the Unified Theory of Acceptance and Use of Technology (UTAUT) [16], a model of information system/information technology acceptance and use. The model describes four factors that would influence a user’s attitude, behavioural intention and use behaviour of an information system or information technology: performance expectancy, effort expectancy, social influence, and facilitating conditions. We present findings about these four factors when patients used the telerehabilitation system. Based on the results of open coding related to UTAUT about using the telerehabilitation system, we report the themes and sample interview quotes in the next section.
Results
We identified the following themes following the UTAUT model, which is presented and elaborated in this section: 1) performance expectance, 2) effort expectancy, 3) facilitating conditions, 4) social influence, 5) behavioural intention.
Performance expectancy
In the context of health information technology, we define performance expectancy as the degree to which the patients believe that using the system enhances their health conditions in physical, mental, and social/emotional aspects.
Perceived improvement in physical abilities
Patients reported different levels of improvement in their physical conditions after the six weeks of study therapy. Some participants demonstrated their enhanced dexterity, strength, and endurance by comparing how their arms functioned at the end of therapy in contrast with what they were like before therapy. For P1, she mentioned that “my arm started getting a little stronger I could reach more you know in and I practiced I started reaching for the refrigerator with my right hand and door knobs.”
Among all the components of the system, all participants rated highly their experience using the videoconference, which provided a channel for therapists to observe, correct, and provide feedback and encouragement. First, participants emphasized that they were able to obtain feedback from the therapist on their exercise. During the session, the therapists would go over many games and exercises with the patients and watch participant movements, and they could verbally correct exercise performance, make adjustments, and answer questions. Afterwards, offline, therapists could adjust game choices or game difficulty parameters (e.g., game speed, duration, or difficulty level) to adapt to a patient’s progress and preferences. For example, P7 appreciated that the therapist could watch her doing the exercises and correct them when necessary: “I enjoy giving clarification on how to do the exercises. … She would tell me start from the shoulder or whatever. If I could not do each exercise, she would watch, give some little corrections ...” Participants also liked that video-conferencing provides a visual feedback to the therapists to adjust the games and adapt to their preferences.
Perceived improvement in mental well-being
Some patients also experienced enhanced cognitive skills through playing games. As the caregiver of P3 helped add: “It was a great help mentally…. He was confused in a few things. He started your program, I noticed he started to become better… For example, what day is today? Monday? Remember? What month?” In addition, the education component also helped them learn about stroke that they were unaware of before. For most of the participants, the questions were rated as easy but nonetheless also helped them exercise their cognitive abilities. Some participants reported enhanced memory after playing the games.
Perceived improvement in social-emotional well-being
Some patients also felt more socially connected after using the system. They considered talking to the therapist as a way to socially connect with others. They described becoming more isolated after their stroke, often caused by their limitations in mobility. However, the video-conferencing allowed them to talk to their therapist and therefore feel more connected. As the caregiver of P2 added: “being alone here in the house with nobody but me and the dog, she would enjoy another woman coming ... and I think she really enjoyed that.” Most patients established a personal connection with the therapist through use of the telerehabilitation system. By doing so, they felt less isolated and more positive and connected.
Effort expectancy
Overall, participants considered the system easy to learn and easy to use because of the engaging exercise experience provided by the games, the external and internal motivation in using the system, as well as the convenience of conducting the exercises at home.
Perceived engaging experience
All participants agreed that playing games made the rehabilitation experience more enjoyable. In particular, participants liked the variety of the games they had been exposed, such as poker, shooting, and driving games. For example, many patients liked the game “Shooting Ducks” because they like doing action games, and some liked the driving game because the skills could be adapted to real life when they eventually returned to driving. As P7 mentioned, “I like to drive because I had to work a little bit to get in, … I really like the blackjack because I think it did better there than it did Vegas. And the poker was fun even though I don’t play poker.” Through choosing and playing a variety of games, participants perceived the exercises to be more engaging compared with conventional repetitive rehabilitation exercises.
Motivation to conduct the exercises
Patients reported both external and internal motivation for performing their exercises. Externally, communicating with therapists three times a week held patients accountable for conducting the exercises. Several patients mentioned that even though they were aware that their previous rehabilitation therapy exercises, prescribed prior to study participation, were essential for recovery, sometimes they had been too tired or busy, and therefore in the past they had tended to skip sessions at times. However, during study participation, they knew that a therapist would connect and talk with them, and so they felt more obliged to complete their assignments, including in comparison to working with the system by themselves. Internally, witnessing their progress over time helped participants maintain continued use of the telerehabilitation system. In particular, they noticed the progress when they could play the games faster, easier, and with higher scores, when they observed improvement in conducting their activities of daily living, and when they received evaluation and feedback from their therapists. Overall, the external and internal motivation that drove patients to stay in the telerehabilitation program reduced their perceived effort for engaging in this rehabilitation program.
Convenience in home-based rehabilitation
All patients commented that being able to conduct rehabilitation at home has made rehabilitation more convenient compared with having to travel to a healthcare professional. They could also adjust the time in using the system, which is more convenient than scheduling a specific time with their therapist. The convenience in location and time led to have higher doses of therapy compared to that achieved when having to travel to a therapist at a scheduled time. As P2 reported: “it was very convenient. You could go over there in your robe or pyjamas and do it if you didn’t want to get up at 8 o’clock in the morning …” Using home-based rehabilitation systems also saved effort for some caregivers. For example, C7 compared her experience as a caregiver in the telerehabilitation system with sessions with the therapists in person. “I would go with her to watch what was being done and what the goal was, how it was supposed to be, sort of continuity of care. In other words, I could learn enough to watch what she was doing at home.” Therefore, the home-based telerehabilitation system saved users’ effort in traveling to the therapists at specific time and freeing caregivers from accompanying them.
Facilitating conditions
Some participants wished that they could have better facilitating conditions in terms of technical issues, physical space, and schedule. Three participants reported minor technical issues at the beginning of the study but appreciated that they were able to receive support in time. For example, P7 reported that the camera used for video-conferencing occasionally fell, which made them frustrated. Being provided a channel where they could always reach out for technical support was considered essential for both patients and caregivers. Physical space is the second facilitating factor raised by the patients. Two patients mentioned that they had limited space in their homes. Therefore, despite of all the benefits of the telerehabilitation systems, they found it inconvenient at times. The third facilitating factor is the time. Two participants mentioned that even though they were able to receive larger dose of therapy compared with visiting the therapist, they also reported time constraints. For example, P4 mentioned he had to suspend some daily tasks if he was going to use the telerehabilitation system for six days a week. He wished for a less intense schedule, such as two days a week.
Social influence
Three participants mentioned social influence when using the telerehabilitation system. Besides caregivers, social influence mainly came from family members. For example, For P2, “I have a son who comes in and out of the house about once a week and he was thrilled over anything that I was getting to help.” Even though the system was used by a single user and not in a social model, our participants reflected that being able to receive attention from their friends and family motivated them to continue engaging in their therapy using this system.
Behavioural intention
We asked about their behavioural intention: whether they will continue to use the system in the future. Most participants agreed they would want to use the system in the future. However, participants also expected a number of improvements to the system to enable long-term usage, particularly improved ability to adapt game difficulty and to show progress over time.
First, participants expected that the difficulty of the games and exercises could be adapted to their progress over time. As our participants reflected, they had experienced improvement after using the system for six weeks. If they were to continue using the system in the long run, the system would need to keep challenging them.
Second, participants wished to visually see their progress over time. As mentioned earlier, participants were motivated when they subjectively experienced progress or their caregivers observed the progress. However, they also wished to view their data in the long run. Being able to see the progress over time could motivate them to make continuous improvement.
Discussion
Based on the findings, we discuss three major implications for designing home-based stroke telerehabilitation systems.
Design for holistic post-stroke recovery
Our qualitative findings on patients’ perceived performance expectancy further reveals that even though the telerehabilitation system was originally designed to help patients conduct physical rehabilitation, some participants had also reported visible improvement in their social and emotional well-being, as well as cognitive abilities. Chatting with the therapist at home via video-conferencing made them feel less isolated and more connected. Such outcome might come from the affordance of games in enhancing cognitive abilities and telecommunication in promoting social interaction. Therefore, it could be helpful to consider multiple dimensions of patients’ stroke recovery.
Designing for engagement
Rehabilitation usually involves repeating exercises that could be tedious over time, and a number of studies have investigated various ways to make the rehabilitation experience more engaging and enhance patients’ compliance in the exercises [14, 17]. Our findings on patients’ perceived effort expectancy showed three dimensions that reflected how patients felt regarding telerehabilitation system effects in reducing their effort: playful game experience, motivating to use, and convenience in location and time.
The engaging rehabilitation experience offered by the games had transformed the traditional tedious exercises into playful games that patients enjoyed playing and found challenging. The playfulness when interacting with the system leads to the first layer of engagement. Additionally, the systems offered both external and internal motivations for patients to engage over time: externally by having a therapist keep them accountable in completing the sessions and internally by the their own progress.. When patients were motivated, they perceived less resistance and burden in completing the rehabilitation sessions. Furthermore, the flexibility in location and time of rehabilitation session further tend to reduce some burdens imposed by traditional therapy sessions.
Designing for the home environment
Our findings on patients’ facilitating conditions and social influence also lead to the consideration of home environment. Different from clinical-based therapy sessions, usually conducted by professionals in an environment that offers all necessary technical conditions, our participants reported barriers in their technical skills, limited living space to place the devices. Fortunately, these barriers were mostly addressed by contacting the research team, usually happened in the first week of the study. Therefore, when deploying home-based stroke rehabilitation technologies, it is crucial to consider these potential patients’ barriers in the home environment and provide in-time support especially during the early stage.
Conclusion
This article reports the findings of a qualitative study of a telerehabilitation system for patients to conduct upper limb therapy sessions at home through therapy games, exercises, videoconferencing with therapists, and education. We conducted interviews with 13 patients who had completed a 6-week trial with the telerehabilitation system. We qualitatively analysed the data in four aspects that determine a user’s acceptance towards a technology following the UTAUT technology acceptance model. We further present users’ intention and suggestions when considering theoretical use of the system for a longer term. Finally, drawn from the findings, we discussed three implications in designing technologies that facilitate stroke rehabilitation: design for holistic rehabilitation plan, design for engagement, and design for the home environment.
Figure 2.
The Unified Theory of Acceptance and Use of Technology (UTAUT) [15]
Acknowledgements
This work was supported by the National Science Foundation [grant number HCC-1219197] and National Institutes of Health [grant number K24HD074722].
Appendixes
Appendix 1: Definition of constructs in UTAUT model
Performance expectancy: the degree to which an individual believes that using the system will help him or her to attain gains in job performance.
Effort expectancy: the degree of ease associated with the use of the system.
Social influence: the degree to which an individual perceives that important others believe he or she should use the system.
Facilitating conditions: the degree to which an individual believes that an organizational and technical infrastructure exists to support use of the system.
Appendix 2: procedure of the clinical trail
Subjects received a total of 36 treatment sessions, half supervised and half unsupervised. At the beginning of each supervised session, at the agreed upon time, a treatment therapist at the study site initiated a videoconference (Figure 1) with the subject’s telerehabilitation system. The treatment therapist then supervised the subject, using a structured approach, for a 30-minute period during which the therapist observed the patient performing assigned home-based telerehabilitation exercises and tasks, answered questions, reviewed the treatment plan, and on selected days performed brief study assessments. After 30 minutes, the therapist disconnected from the videoconference and the subject completed the remaining 40 minutes of therapy guided by the telerehabilitation system. The 18 unsupervised therapy sessions were performed by the subject at home using the same telerehabilitation system but with no contact with a study therapist. Instead, all 70 minutes of therapy were guided only by the telerehabilitation system. Each unsupervised session began with five minutes of stroke education that was focused on prevention, recognition, response, and management of stroke. This was followed by games and exercises that had been assigned by the treatment therapist previously, offline.
Appendix 3: Interview Questions
Part 1: Introduction
Demographic questions: age, stroke history.
Tell me about your stroke. What happened?
What types of treatment have you received?
What kind of rehabilitation therapy did you get? Was it hard to travel to your rehabilitation therapy? What kind of assistance did you need to take you to/from the therapy? Regarding the rehabilitation therapy, what was easy about it and what was difficult? Why? We are mainly referring to a program overseeing by a licensed therapist.
Are you currently receiving any rehabilitation therapy?
How good are your skills with computers, smartphones, etc?
Part 2: Questions regarding using the system
[Motivation] How did you learn about the study? Why is it of interest to you?
[How they use it] What was your experience with using the system? How did it go? What was easy? What was hard? Among the four modes of the telerehabilitation program (1. game, 2. exercises, 3. education, 4. videoconferences), what did you like and what did you dislike? Why? Which pieces of hardware did you like and dislike? Did you use the system by yourself or together with caregivers or both?
When did you use it and how do you remember to use it?
[Video-conference] What did you enjoy and not enjoy about the video conference? What did you talk about during these videoconferences? Did they help? If so, how? Were there any ways that communication was difficult because you were using the videoconference method? Was there anything you were embarrassed to say over the videoconference?
[UTAUT related questions: usefulness, ease of use, social factors, facilitating conditions] How would the attitudes of your family, friends influence your usage of the system? Any other factors might influence your usage of the system, such as resources, physical environment?
[Changes] Did you observe improvement or changes in how you used the system over time? Did you observe any changes in motivations and attitudes for using the system over time?
[Usage intention] After the system was removed from your home, how did you feel? Would you consider resuming using this system? Why (not)? Imagine you will use it for six months, what barriers and additional factors would make this process even more enjoyable.
[Socialization module, functional goals, mhealth independent variable] How might the system help you connect with other people, including family, friends, other stroke survivors? How might the system help you improve your ability to do your everyday household activities? Your self-care activities? If the system came with a smartphone, how could that be useful? How did you track your progress? How did you monitor your diet, medication, etc?
Appendix 4: Checklist demonstrating that the manuscript conforms to the COREQ Guidelines
Domain 1: Research team and reflexivity
Personal Characteristics
1. Interviewer/facilitator
Which author/s conducted the interview or focus group?
- All interviews were conducted by the first author of this research.
2. Credentials
What were the researcher’s credentials? E.g. PhD, MD
- The author holds a PhD at the time of study.
3. Occupation
What was their occupation at the time of the study?
- The first author was a postdoctoral researcher at the time of the study.
4. Gender
Was the researcher male or female?
- The first author was a female.
5. Experience and training
What experience or training did the researcher have?
- The first author was trained by professors (the second and the third author) who were experienced in conducting qualitative studies.
Relationship with participants
6. Relationship established
Was a relationship established prior to study commencement?
- The participants participated in a clinical trial prior to the qualitative interview.
7. Participant knowledge of the interviewer
What did the participants know about the researcher? e.g. personal goals, reasons for doing the research
- To set time for interviews, some participants received call contacts. Research subject, objectives, and identity of author were given in contacts. Additionally, author 4–10 were the main researchers in the clinical trial.
8. Interviewer characteristics
What characteristics were reported about the interviewer/facilitator? e.g. Bias, assumptions, reasons and interests in the research topic.
- The assumptions and research motivation of the researcher was reported in the manuscript.
Domain 2: study design
Theoretical framework
9. Methodological orientation and Theory
What methodological orientation was stated to underpin the study? e.g. grounded theory, discourse analysis, ethnography, phenomenology, content analysis
- Content analysis was used to analyze the qualitative data.
Participant selection
10. Sampling
How were participants selected? e.g. purposive, convenience, consecutive, snowball
- All of the participants were from the participants of a prior clinical trial, who had used the telerehabilitation system studied in this paper.
11. Method of approach
How were participants approached? e.g. face-to-face, telephone, mail, email
- The participants were contacted by telephone.
12. Sample size
How many participants were in the study?
- There were 13 participants in the study. See Table 3.
13. Non-participation
How many people refused to participate or dropped out? Reasons?
- No one.
Setting
14. Setting of data collection
Where was the data collected? e.g. home, clinic, workplace
- The data of nine participants were collected at their homes and four were collected at a university conference room. See Table 3.
15. Presence of non-participants
Was anyone else present besides the participants and researchers?
- Eight participants were accompanied by their spouse, one by a sister, and four by themselves. See Table 3.
16. Description of sample
What are the important characteristics of the sample? e.g. demographic data, date
- The demographic information of the sample was provided in Table 3.
Data collection
17. Interview guide
Were questions, prompts, guides provided by the authors? Was it pilot tested?
- The questions, prompts, guides were provided by the authors. They were pilot tested with non-participants.
18. Repeat interviews
Were repeat interviews carried out? If yes, how many?
- No.
19. Audio/visual recording
Did the research use audio or visual recording to collect the data?
- The research used audio-recording.
20. Field notes
Were field notes made during and/or after the interview or focus group?
- The researcher took field notes during the interview.
21. Duration
What was the duration of the interviews or focus group?
- Each interview took around one hour.
22. Data saturation
Was data saturation discussed?
- We coded the data until it reached saturation.
23. Transcripts returned
Were transcripts returned to participants for comment and/or correction?
- No.
Domain 3: analysis and findings
Data analysis
24. Number of data coders
How many data coders coded the data?
- Two coders coded the data: the first author and a research assistant.
25. Description of the coding tree
Did authors provide a description of the coding tree?
- Yes.
26. Derivation of themes
Were themes identified in advance or derived from the data?
- The themes were developed by following the UTAUT model and then the sub-themes were derived from the data.
27. Software
What software, if applicable, was used to manage the data?
- Dedoose was used to manage the data.
28. Participant checking
Did participants provide feedback on the findings?
- No.
Reporting
29. Quotations presented
Were participant quotations presented to illustrate the themes / findings? Was each quotation identified? e.g. participant number
- Yes.
30. Data and findings consistent
Was there consistency between the data presented and the findings?
- Yes.
31. Clarity of major themes
Were major themes clearly presented in the findings?
- Yes.
32. Clarity of minor themes
Is there a description of diverse cases or discussion of minor themes?
- Yes.
Footnotes
Conflicts of interest
Dr. Cramer has consulted for MicroTransponder, Dart Neuroscience, Roche, Neurolutions, Regenera, Abbvie, SanBio, and TRCare.
References
- 1.Stroke Information | cdc.gov. https://www.cdc.gov/stroke/index.htm Accessed October 26, 2018.
- 2.Kwakkel G, Kollen BJ, Krebs HI. Effects of robot-assisted therapy on upper limb recovery after stroke: a systematic review. Nnr. 2007:1–11. doi: 10.1177/1545968307305457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prange GB, Jannink MJ a, Groothuis-Oudshoorn CGM, Hermens HJ, Ijzerman MJ. Systematic review of the effect of robot-aided therapy on recovery of the hemiparetic arm after stroke. J Rehabil Res Dev. 2006;43(2):171–184. doi: 10.1682/JRRD.2005.04.0076. [DOI] [PubMed] [Google Scholar]
- 4.Sivan M, O’Connor RJ, Makower S, Levesley M, Bhakta B. Systematic review of outcome measures used in the evaluation of robot-assisted upper limb exercise in stroke. J Rehabil Med. 2011;43(3):181–189. doi: 10.2340/16501977-0674. [DOI] [PubMed] [Google Scholar]
- 5.Pascual-Leone A Training modalities in robot-mediated upper limb rehabilitation in stroke: a framework for classification based on a systematic review. J Neuroeng Rehabil. 2014;11(1):111. doi: 10.1186/1743-0003-11-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sheng B, Zhang Y, Meng W, Deng C, Xie S. Bilateral robots for upper-limb stroke rehabilitation: State of the art and future prospects. Med Eng Phys. 2016;38(7):587–606. doi: 10.1016/j.medengphy.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 7.King M, Hijmans J, Sampson M, Satherley J, Hale L. Bilateral movement training with computer games for stroke rehabilitation. Proc 4th Int Conv Rehabil Eng \& Assist Technol (iCREATe ‘10) 2010:Article 20, pp 1–4. doi:j.jns.2006.01.005. [Google Scholar]
- 8.Swinnen E, Beckwée D, Meeusen R, Baeyens J-P, Kerckhofs E. Does robot-assisted gait rehabilitation improve balance in stroke patients? A systematic review. Top Stroke Rehabil. 2014;21(2):87–100. doi: 10.1310/tsr2102-87. [DOI] [PubMed] [Google Scholar]
- 9.Geroin C, Mazzoleni S, Smania N, et al. Systematic review of outcome measures of walking training using electromechanical and robotic devices in patients with stroke. J Rehabil Med. 2013;45(10):987–996. doi: 10.2340/16501977-1234. [DOI] [PubMed] [Google Scholar]
- 10.Rubin MN, Wellik KE, Channer DD, Demaerschalk BM. Systematic review of telestroke for post-stroke care and rehabilitation. Curr Atheroscler Rep. 2013;15(8). doi: 10.1007/s11883-013-0343-7. [DOI] [PubMed] [Google Scholar]
- 11.Johansson T, Wild C. Telerehabilitation in stroke care - a systematic review. J Telemed Telecare. 2011;17(1):1–6. doi: 10.1258/jtt.2010.100105. [DOI] [PubMed] [Google Scholar]
- 12.Lohse KR, Hilderman CGE, Cheung KL, Tatla S, Van Der Loos HFM. Virtual reality therapy for adults post-stroke: A systematic review and meta-analysis exploring virtual environments and commercial games in therapy. PLoS One. 2014;9(3). doi: 10.1371/journal.pone.0093318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dos Santos LRA, Carregosa AA, Masruha MR, et al. The Use of Nintendo Wii in the Rehabilitation of Poststroke Patients: A Systematic Review. J Stroke Cerebrovasc Dis. 2015;24(10):2298–2305. doi: 10.1016/j.jstrokecerebrovasdis.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 14.Dodakian L, McKenzie AL, Le V, See J, Pearson-Fuhrhop K, Burke Quinlan E, Zhou RJ, Augsberger R, Tran XA, Friedman N, Reinkensmeyer DJ, Cramer SC. A home-based telerehabilitation program for patients with stroke. Neurorehabil Neural Repair. 2017;31:923–933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cramer SC, Dodakian L, Le V, See J, Augsburger R, McKenzie A, Zhou RJ, Chiu NL, Heckhausen J, Cassidy JM, Scacchi W, Smith MT, Barrett AM, Knutson J, Edwards D, Putrino D, Agrawal K, Ngo K, Roth EJ, Tirschwell DL, Woodbury ML, Zafonte R, Zhao W, Spilker J, Wolf SL, Broderick JP, Janis S; National Institutes of Health StrokeNet Telerehab Investigators. Efficacy of Home-Based Telerehabilitation vs In-Clinic Therapy for Adults After Stroke: A Randomized Clinical Trial. JAMA Neurol. 2019. June 24. doi: 10.1001/jamaneurol.2019.1604 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Venkatesh V, Morris MG, Davis GB, & Davis FD (2003). User acceptance of information technology: Toward a unified view. MIS quarterly, 425–478. [Google Scholar]
- 17.Saposnik G, Levin M. Virtual reality in stroke rehabilitation: A meta-analysis and implications for clinicians. Stroke. 2011;42:1380–1386 [DOI] [PubMed] [Google Scholar]