Abstract
Background:
Children in low income and minority populations are at risk for poor dietary quality. At least one-third of the calories consumed by children are eaten between meals (i.e. snacks). The contribution of snacking to diet quality among children is poorly understood.
Objective:
The current study examined associations between snacking and children’s diet quality along with differences across ethnicity/race, sex, and weight status.
Design:
Cross-sectional data came from Phase I of the Family Matters Study, an observational study.
Participants/setting:
This study included 150 families with children aged 5–7 years old from six ethnic/racial groups (n = 25 from each; African American, Hispanic, Hmong, Native American, Somali, non-Hispanic white); data were collected in Minneapolis/Saint Paul in 2017-2018.
Main outcome measures:
Total daily energy (kcal), overall diet quality using the Healthy Eating Index (HEI-2010), and food group intakes [e.g. fruit, vegetables, refined grains, sugar-sweetened beverages (SSB)] were assessed using three 24-hour dietary recalls.
Statistical Analyses Performed:
Conditional fixed effects estimators (within-child variation) were used in regression analyses to characterize the relationship between daily snacking and dietary intake relative to dietary intake at all other daily meal occasions. Mean (standard Deviation; ±) overall dietary intake including all meals and snacks was compared to mean (±) intake of meals only.
Results:
Among boys, snacking was found to contribute positively to HEI-2010 scores (HEI-2010: 57.6, HEI-2010 without snacks: 55.0; Effect Size (ES): 0.28, p=0.03). Snacking was an important source of fruit (ES: 0.71) and dairy (ES:0.53), but also contributed to children’s consumption of refined grains (ES: 0.68) and SSB (ES: 0.31). Very few vegetables were consumed as snacks. Further, snacks contributed more to the overall diet quality (HEI-2010) of Native American (ES: 0.30) and Somali (ES: 0.35) youth as compared to youth from other ethnic/racial backgrounds.
Conclusions:
Findings suggest that snacks have the potential to improve diet quality in children. Future research should examine influences on children’s food choices at snack times and barriers to serving more healthful foods as snacks that are faced by ethnically/racially diverse families.
Keywords: dietary intake, snacking, healthy eating index, school-aged children, quantitative study
National data indicate that overall diet quality among US children is poor, with the majority of children failing to meet current dietary recommendations for health,1 an issue further compounded for children from low-income families and ethnically/racially diverse backgrounds.1 Given the importance of a healthful diet during childhood, identifying factors that have potential to improve childhood dietary intake patterns, particularly among youth from low-income or ethnically/racially diverse backgrounds, is a public health priority.2,3 Over the past several decades, clinicians and public health advocates have become concerned by an observable increase in the frequency of snacking (i.e., eating between meals), daily energy intake from snacks, and number of energy-dense, nutrient-poor foods and beverages consumed as snacks among children.4-10 School-aged children consume approximately one-third of their total daily calories as snacks.10 The significant contribution of snacking to children’s total caloric intake highlights the need to understand how snacks contribute to overall diet quality.
Snacking has been defined and measured in a variety of ways. Some studies rely on participant-defined occasions (e.g. meal or snack), whereas others define snacking based on consumption of specific types of foods (e.g. cookies, cakes, chips).8 These varied definitions are important to consider when interpreting the results of research on snacking. To date, research suggests that more frequent snacking (measured by self-reported eating occasions) is associated with higher overall energy intake and higher energy intake from added sugars and fats.8,11 Indeed, data suggest that, for children, desserts and sugar-sweetened beverages are the two major sources of calories consumed during snacking occasions.4,9,10 Additionally, since the early 1990s, there has been a notable increase in the amount of salty snack foods and candy consumed during snacking occasions, increasing the overall role of these foods in children’s diet profile.4,8-10 At the same time, some research has found that foods consumed during snacking occasions also contribute positively to children’s intake of key vitamins and minerals and have been shown to make small, but meaningful contributions to children’s total protein intake.4,8-10 Taken together, these findings suggest that snacks substantially contribute to a child’s overall daily calorie intake and highlight that while much of this contribution may come from high calorie, low nutrient-dense foods, snacks also seem to contribute important nutrients to children’s overall dietary intake profile.
Overall, research exploring the impact of snacking on dietary intake has been relatively limited and mostly descriptive in nature. Further, the bulk of research has evaluated associations of snacking with children’s intakes of nutrients and consumption of specific food groups. With a few exceptions11-14, little attention has been given to understand the contributions of snacking to children’s overall diet quality. Indeed, a recent review article emphasized this research need, particularly within socioeconomically diverse populations;8 exploring differences in snacking patterns across diverse subgroups could help explain observed disparities in overall dietary quality found among youth from diverse backgrounds.
The current study aimed to evaluate associations of snacking with children’s total daily energy intakes, overall diet quality as reflected in Healthy Eating Index scores, and food group intakes [e.g. fruits, sugar-sweetened beverages (SSB)]. Specifically, diet quality outcomes for meals and snacks were compared to diet quality outcomes for meals alone to understand what and how snacks contributed to overall diet quality outcomes. A second aim was to examine differences in the contribution of snacking to children’s daily dietary intake across child ethnicity/race, sex, and weight status, within a diverse, metropolitan sample of children. Study findings will be used to inform future research aimed at understanding how to best design and tailor public health messages and nutrition guidelines regarding eating between meals.
MATERIALS AND METHODS
Data for the current study are from Phase I of Family Matters15, a National Institutes of Health-funded observational study, designed to identify novel risk and protective factors for childhood obesity in the home environments of ethnically/racially diverse and primarily low-income16 children (n=150). Phase I of the Family Matters study included in-depth observational research of a smaller sample of diverse families using a variety of methods (in-home observations, 24-hour dietary recalls, individual interviews, surveys) with the goal of using these observations to inform the development of a culturally appropriate survey to be conducted within a larger sample of families during Phase 2, as well as subsequent interventions geared towards families of elementary school-aged children. The University of Minnesota’s Institutional Review Board Human Subjects Committee approved all protocols used in the Family Matters study; all parent participants provided written informed consent and parental consent for their children, and all children assented to the study.
Participants
The study recruited children and their families from the Minneapolis/St. Paul, MN area between 2015-2016 via a letter sent to them by their family physician. Children were eligible to participate in the study if they were between the ages of 5 and 7 years old, had a sibling between the ages of 2 and 12 years old living in the same home, lived with their parent/primary guardian more than 50% of the time, shared at least one meal (home-cooked or otherwise) per day with the parent/primary caregiver, and were from one of six racial/ethnic categories (non-Hispanic white, African American, Hispanic, Native American, Hmong, and Somali). Children were required to be away from home during the day (e.g. school, summer camp) in order to participate in the study. In total, 150 families with children aged 5–7 years old from six ethnic/racial groups participated in the study (n = 25 from each; African American, Hispanic, Hmong, Native American, Somali, non-Hispanic white). Further, the study implemented a stratified sampling strategy; within each ethnic/racial group, half of the sample children recruited had a body mass index (BMI) ≥85 percentile while the other half had a BMI between 5 and 85 percentile. Additional, in-depth details regarding recruitment and study design are published elsewhere.15
Procedures and Data Collection
Measures used in this analysis (detailed below) were collected from three 24-hour dietary recalls completed by the primary caregiver over the course of a seven day period.17
24-hour dietary recalls.
Certified researchers used the Nutrition Data System for Research (NDSR) 18 Version 2015 to collect three 24-hour dietary recalls on the target child; dietary intake data were collected in all months/seasons of the year, based on the time when each parent-child dyads were recruited into the study. Because young children are not considered reliable reporters of dietary intake, recalls were conducted with the target child’s parent. Recalls were conducted on nonconsecutive days; two of the recalls were weekdays, and one was a weekend day. The first and third dietary recalls were collected in-person as a part of the first and last data collection home visits; the second recall was conducted over the telephone. The dietary recalls collected were scheduled in advance, rather than random.
Several tools were used to assist parents in their reporting of the target child’s dietary intake, including, 1) food diaries to record the foods and drinks consumed by the target child the previous day, 2) a food amounts booklet to assist parents in recalling the amounts of foods consumed, and 3) school lunch and breakfast menus to provide guidance for parents of children who ate school breakfast and lunch. Additionally, parents were asked to involve their child in the recall process so their child could provide additional details when appropriate (e.g. reporting what they ate off of the school menu). Staff dietitians conducted quality assurance on 100% of dietary recalls; the quality assurance process used in this study mirrors the one used by the Nutrition Coordinating Center at the University of Minnesota.19
Food and Nutrient Categories:
NDSR18 combined foods eaten into food subgroups (e.g., dark green vegetables, whole-grain crackers). Similar subgroups were combined when appropriate to create an overall category. For example, soft drinks, sports and energy drinks, fruit drinks (e.g., SunnyD), sweetened coffees and teas (e.g., Frappuccino), and sweetened waters (e.g., Vitamin Water) were combined to create a SSB category. Food subgroups are available per day, per meal, or per eating occasion type. Healthy Eating Index (HEI-2010) scores were calculated using guidance from the Nutrition Coordinating Center.20-22 This score was calculated by averaging the dietary recall intake data, computing scores for each adequacy and moderation component, and summing the component scores to compute individual HEI-2010 scores (i.e. mean ratio method). The HEI-2010 was designed to measure how well diet quality conformed with the Dietary Guidelines for Americans, 2010. The HEI-2010 consists of 12 categories: Whole Fruit, Total Fruit, Whole Grains, Dairy, Total Protein Foods, Seafood and Plant Proteins, Greens and Beans, Total Vegetables, Fatty Acids, Refined Grains, Sodium, and Empty Calories. The first nine components are “adequacy” components, and final 3 (Fatty Acids, Refined Grains, Sodium) are “moderation” components. Each component is assigned a maximum point value and a standard for achieving the maximum score. The highest HEI-2010 score possible, calculated by summing all 12 component scores, is 100; a higher score indicates a higher quality diet. Detailed descriptions of how HEI-2010 scores were calculated are available elsewhere.22,23
Snacking Occasions:
Snacking occasions were self-identified by the parent. For each eating occasion reported during the three 24-hour dietary recalls, certified research staff asked the parent to label each eating occasion; options included breakfast, lunch, dinner or a snack.
Sex and Ethnicity/race.
Determination of sex and ethnicity/race were based on the primary caregiver’s report of child demographics at the time of recruitment.
Statistical Analysis
Descriptive statistics and demographic crosstabulations (e.g., frequency) were computed to assess overall completeness of dietary intake data by meal occasion. Diet quality outcomes and daily energy intake for meals and snacks were compared to diet quality outcomes and daily energy intake for meals alone to understand what and how snacks contributed to overall diet quality outcomes and daily energy intake. A decomposition strategy was implemented to examine how the frequency of snacking contributed to the overall healthfulness of child dietary intake using multiple linear regression and conditional fixed effects estimators to model within-child variation in the relationship between snacking and dietary intake. This analytical strategy controls for all static child characteristics because children are their own control. Because the effect of removing snacking constitutes a one-sided significance test, confidence intervals were calculated at the 97.5% level and standardized effect sizes (ES) were presented to focus on snacking effects with comparatively large effect sizes. Cohen’s D will be presented as the measure of ES; Cohen suggested that d=0.2 be considered a 'small' effect size, 0.5 represents a 'medium' effect size and 0.8 a 'large' effect size. This means that if two groups' means don't differ by 0.2 standard deviations or more, the difference is trivial, even if it is statistically significant. Adjustments for inflated type I error due to multiple testing were not made because eliminating foods consumed at snacks may jointly affect several macro-/micronutrient categories resulting in overly conservative significance testing. The effect of removing snacking on dietary intake (continuous dependent variables) was examined overall (i.e. for the total sample population), and interaction tests were performed to evaluate if the snacking effect depended on sex, race, and overweight status (i.e., child BMI percentile greater than 85th percentile). There were no statistically significant interactions between snacking and child weight status, therefore results are not shown. To capture how removing snacking affected the composition of average child daily intake of healthful and unhealthful foods, the Healthy Eating Index-2010 was calculated with and without the inclusion of snacking occasions. Robust standard errors were computed to account for any misspecification of the error term i.e. the model may not account for every important variable. All data analysis and management was performed in Stata 15.1MP.24
RESULTS
Characteristics of the study population
Children in the study sample were between 6 and 7 years of age. The study sample (n=150) was 52.2% (n=79) boys and split evenly across six ethnic/racial groups (25 each of African American, Hispanic, Hmong, Native American, Somali, and Non-Hispanic White). The mean BMI-percentile of children in the sample ranged from 70.9 (SD: 28.06), among Somali youth, to 80.9 (SD: 17.54) among Hmong youth. HEI-2010 scores were lower when only meals were included in the calculation, as compared to when meals and snacks were included in the calculation, for both boys and girls, as well as across all racial/ethnic groups. See Table 1 for additional details on the study sample.
Table 1.
Demographic Sample Characteristics and Dietary Intake (HEI-2010) for Meals Including Snacks and Meals Only (N=150 Children)
| Mean Age (yrs) ± sd |
BMI Percentile ± sd | HEI-2010 ± sd | ||
|---|---|---|---|---|
| Meals + Snacks |
Meals Only | |||
| Total | 6.4 ± 0.79 | 75.9 ± 23.14 | 57.1 ± 9.34 | 55.3 ± 8.99 |
| Sex | ||||
| Boys (n=79) | 6.4 ± 0.81 | 75.2 ± 23.65 | 57.6 ± 9.81 | 55.0 ± 9.07 |
| Girls (n=71) | 6.4 ± 0.78 | 76.8 ± 22.69 | 56.6 ± 8.83 | 55.6 ± 8.96 |
| Ethnicity/Race | ||||
| African American (n=25) | 6.4 ± 0.87 | 75.1 ± 23.52 | 49.5 ± 6.89 | 49.0 ± 8.29 |
| Hispanic (n=25) | 6.5 ± 0.85 | 76.8 ± 25.53 | 61.1 ± 8.34 | 59.1 ± 8.58 |
| Hmong (n=25) | 6.5 ± 0.69 | 80.9 ± 17.54 | 54.7 ± 9.28 | 53.4 ± 8.58 |
| Native American (n=25) | 6.4 ± 0.68 | 79.6 ± 19.87 | 56.0 ± 9.44 | 53.4 ± 9.05 |
| Somali (n=25) | 6.5 ± 0.78 | 70.9 ± 28.06 | 62.7 ± 6.92 | 60.2 ± 6.87 |
| Non-Hispanic White (n=25) | 6.2 ± 0.90 | 72.2 ± 23.37 | 58.6 ± 9.09 | 56.7 ± 8.10 |
Contribution of snacking occasions to the overall healthfulness of children’s dietary intake
Children consumed an average of 1.8 snacking occasions per day; each snacking occasion contributed a mean of 226 kcal ± 95, for a total of approximately 365 kcal from snacks per day (Table 2). Snacking contributed significantly to children’s overall mean daily energy intake; the mean difference between daily energy intake consumed at meals and snacks as compared to meals only was approximately 365 kcals (Table 2). Results focused on macro- and micro-nutrients consumed during meal and snacking occasions are in Table 3.
Table 2.
Within-Participant Average Daily Snacking Contribution to the Healthy Eating Index-2010 and Average Daily Whole Food and Nutrient Intake: Family Matters Phase I Study, N=150 Children Age 5-7
| Dietary Intake Variable | Meals + Snacks (mean intake ± sd) |
Meals Only (mean intake ± sd) |
Mean Differencea (97.5% CI) |
Effect Size Cohen's db |
|---|---|---|---|---|
| Healthy Eating Index 2010 | 57.1 ± 9.3 | 55.3 ± 9 | −1.79 (−2.63, −0.95) | 0.20 |
| Whole Foods (servings) | ||||
| Fruits | 1.08 ± 0.7 | 0.69 ± 0.5 | −0.38 (−0.46, −0.31) | 0.71 |
| Vegetables | 0.63 ± 0.5 | 0.59 ± 0.4 | −0.04 (−0.07, −0.01) | 0.09 |
| Whole grain (ozs) | 1.29 ± 1.1 | 0.96 ± 0.9 | −0.33 (−0.42, −0.23) | 0.36 |
| Refined grain (ozs) | 4.98 ± 1.9 | 3.92 ± 1.5 | −1.06 (−1.23, −0.89) | 0.68 |
| All Protein | 4.26 ± 2 | 3.88 ± 1.9 | −0.38 (−0.51, −0.25) | 0.20 |
| Seafood and Plant Protein | 0.81 ± 0.9 | 0.66 ± 0.8 | −0.15 (−0.24, −0.06) | 0.19 |
| Dairy | 2.15 ± 0.9 | 1.76 ± 0.7 | −0.39 (−0.48, −0.36) | 0.53 |
| Sugar Sweetened Beverage | 0.54 ± 0.6 | 0.4 ± 0.5 | −0.15 (−0.20, −0.10) | 0.31 |
| Macro-/Micronutrients | ||||
| Calories (kcal) | 1581.3 ± 427 | 1214.8 ± 319.1 | −366.5 (−408.1, −325.0) | 1.15 |
| Total fat (g) | 55.5 ± 21.2 | 42.3 ± 16.2 | −13.2 (−15.1, −11.3) | 0.81 |
| Cholesterol (mg) | 199.3 ± 100.6 | 180 ± 94 | −19.3 (−23.8, −14.7) | 0.21 |
| Sodium (mg) | 2414.5 ± 898.2 | 1991.1 ± 671.8 | −423.5 (−490.5, −356.4) | 0.63 |
| Total carbohydrates (g) | 213.8 ± 57 | 158.9 ± 43.2 | −54.9 (−60.7, −49.1) | 1.27 |
| Fiber (g) | 13.4 ± 5.2 | 10 ± 4.2 | −3.45 (−3.8, −3.1) | 0.82 |
| Total sugar (g) | 100.7 ± 33.2 | 71.2 ± 25.2 | −29.5 (−33.0, −25.9) | 1.17 |
| Added sugar (g) | 51.7 ± 28.4 | 35.5 ± 21 | −16.3 (−19.2, −13.4) | 0.77 |
| Protein (g) | 63 ± 17.8 | 53.5 ± 14.9 | −9.5 (−10.8, −8.1) | 0.64 |
| Vitamin D (mcg) | 6.5 ± 2.8 | 5.5 ± 2.2 | −1.0 (−1.25, −0.7) | 0.45 |
| Calcium (mg) | 973.8 ± 349.7 | 781 ± 270.3 | −192.8 (−226.0, −159.6) | 0.71 |
| Iron (mg) | 12.8 ± 4.7 | 10.5 ± 4 | −2.3 (−2.7, −1.9) | 0.58 |
| Potassium (mg) | 2067.2 ± 555.1 | 1645.2 ± 439.6 | −422.1 (−470.6, −373.5) | 0.96 |
Mean differences are presented at the 97.5% confidence level corresponding to a one-sided significance test.
Differences for which standardized snacking effect sizes (Cohen's d) are at least small to moderate effect sizes of 0.20 are boldfaced to indicate a substantively meaningful result for whole foods. Macro-/micronutrient large effect sizes of at least 0.60 are boldfaced.
Table 3.
Interaction Analyses by Child Sex: Within-Participant Average Snacking Contribution to Average Daily Nutrient Intake in the Family Matters, Phase I Study (N=150 Children)
| INTERACTION ANALYSIS: GIRL AND BOY SNACKING IMPACT ON HEALTHFULNESS OF DIETARY INTAKE | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| GIRLS | BOYS | ||||||||
| Dietary Intake Variable | Meals + Snacks (mean intake ± sd) |
Meals Only (mean intake ± sd) |
Mean Differencea (97.5% CI) |
Effect Size Cohen's db |
Meals + Snacks (mean intake ± sd) |
Meals Only (mean intake ± sd) |
Mean Differencea (97.5% CI) |
Effect Size Cohen's db |
P-Interaction Testc |
| Macro-/Micronutrients | |||||||||
| Calories (kcal) | 1508.7 ± 368.8 | 1153.9 ± 263.7 | −354.8 (−416.8, −292.8) | 1.35 | 1646.6 ± 466.0 | 1269.5 ± 354.5 | −377.1 (−433.3, −320.9) | 1.06 | 0.55 |
| Total fat (g) | 52.7 ± 19.5 | 40.3 ± 14.9 | −12.4 (−15.1, −9.7) | 0.83 | 58.0 ± 22.6 | 44.1 ± 17.2 | −13.9 (−16.6, −11.2) | 0.81 | 0.38 |
| Cholesterol (mg) | 195.6 ± 86.6 | 178.7 ± 84.8 | −17.0 (−22.2, −11.8) | 0.20 | 202.6 ± 112.1 | 181.3 ± 102.1 | −21.3 (−28.5, −14.1) | 0.21 | 0.28 |
| Sodium (mg) | 2332.3 ± 829.2 | 1921.2 ± 620.1 | −411.2 (−507.4, −315) | 0.66 | 2488.4 ± 955.2 | 2053.9 ± 713.1 | −434.5 (−528.7, −340.3) | 0.61 | 0.70 |
| Total carbohydrates (g) | 203.7 ± 52.5 | 149.2 ± 38.3 | −54.5 (−63.6, −45.3) | 1.42 | 222.9 ± 59.6 | 167.6 ± 45.7 | −55.3 (−62.8, −47.9) | 1.21 | 0.87 |
| Fiber (g) | 12.5 ± 4.1 | 9.2 ± 3.1 | −3.3 (−3.9, −2.7) | 1.06 | 14.2 ± 5.9 | 10.7 ± 4.9 | −3.6 (−4.1, −3.0) | 0.74 | 0.51 |
| Total sugar (g) | 96.8 ± 32.0 | 68.2 ± 24.7 | −28.6 (−33.8, −23.5) | 1.16 | 104.2 ± 34.2 | 73.9 ± 25.5 | −30.2 (−35.1, −25.3) | 1.19 | 0.62 |
| Added sugar (g) | 49.6 ± 29.5 | 33.2 ± 21.7 | −16.4 (−20.7, −12.2) | 0.75 | 53.7 ± 27.5 | 37.5 ± 20.3 | −16.2 (−20.1, −12.2) | 0.80 | 0.92 |
| Protein (g) | 61.0 ± 14.8 | 52.3 ± 12.2 | −8.7 (−10.4, −6.9) | 0.71 | 64.8 ± 20.0 | 54.6 ± 17.0 | −10.2 (−12.1, −8.2) | 0.60 | 0.21 |
| Vitamin D (mcg) | 6.3 ± 2.4 | 5.4 ± 2.0 | −0.9 (−1.2, −0.6) | 0.46 | 6.8 ± 3.1 | 5.7 ± 2.5 | −1.1 (−1.5, −0.7) | 0.45 | 0.32 |
| Calcium (mg) | 917.9 ± 315.4 | 747.3 ± 248.6 | −170.7 (−209.1, −132.2) | 0.69 | 1024.0 ± 372.8 | 811.3 ± 286.6 | −212.7 (−265.3, −160.2) | 0.74 | 0.15 |
| Iron (mg) | 11.8 ± 4.0 | 9.6 ± 3.5 | −2.1 (−2.6, −1.6) | 0.60 | 13.7 ± 5.1 | 11.3 ± 4.2 | −2.5 (−3, −1.9) | 0.59 | 0.31 |
| Potassium (mg) | 2016.1 ± 515.5 | 1618.0 ± 431.1 | −398.1 (−464.3, −331.8) | 0.92 | 2113.2 ± 587.8 | 1669.5 ± 448.4 | −443.6 (−514, −373.2) | 0.99 | 0.29 |
Mean differences are presented at the 97.5% confidence level corresponding to a one-sided significance test.
Differences for which standardized moderate-to-large snacking effect sizes (Cohen's d) of at least 0.60 are boldfaced.
Interaction tests are presented to evaluate if the dietary intake effect due to removing snacking depended on child sex.
Mean HEI-2010 scores were lower when only meals were included and snacks were excluded from the analysis, (mean difference: −1.79, ES= 1.15) (Table 1). Snacking contributed to children’s overall mean daily intake of fruit, refined grains and dairy, but not necessarily to the daily intake of all children in the study. For example, children consumed an average of 1.08 ± 0.7 servings of fruit per day from meal and snacking occasions; without snacking in-between meals, children would have consumed only a mean of 0.69 ± 0.5 servings of fruit per day (mean difference: 0.38, ES= 0.71). Snacking between meals also contributed to children’s mean daily intake of SSB; on average, children consumed just over half of a serving of SSB per day (0.54 servings ± 0.6) with the bulk of those SSB consumed during snacking occasions (0.4 servings ± 0.5; mean difference: 0.15, ES= 0.31). Snacking between meals did not make a statistically significant contribution to children’s mean daily intake of vegetables (mean difference: 0.04, ES=0.09).
Sex Differences
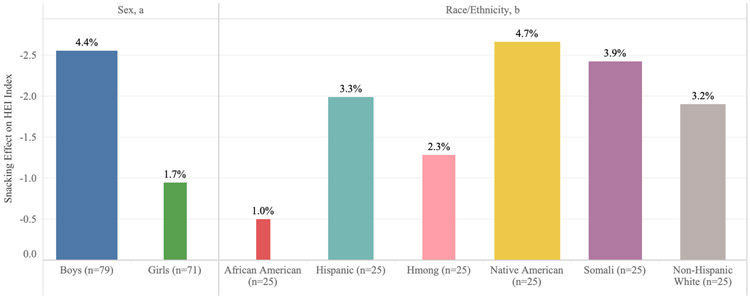
Although mean HEI-2010 decreased for the overall sample when the contribution of foods consumed during snacks was removed, snacking had a more favorable impact on the composition of dietary intake for boys compared to girls (sex interaction p-value = 0.031; Figure 1). Mean HEI-2010 was lower (−2.5 for boys, and −0.95 for girls) when using only meals and excluding snacks. This statistically significant interaction indicated that snacking contributes more to the overall healthfulness of daily dietary intake for boys as compared to girls accounting for caloric intake.
Figure 1. Snacking Contribution to the HEI-2010 Index of Overall Diet Quality Measured by Three Dietary Recalls (N=150 Children): Stratified by Child Sex and Child Race/Ethnicity, Family Matters Phase I Study.
a. Interpretation Example, Child Sex. Daily snacking had a more favorable impact on the composition of dietary intake for boys compared to girls (Interaction P Value = 0.031). Removing intake at snacks resulted in approximately a −2.5 reduction in calculated daily HEI-2010 for boys, and a −0.95 reduction in calculated daily Healthy Eating Index (HEI-2010) for girls.
b. Interpretation Example, Race/Ethnicity. Daily snacking was not found to differ statistically by the six race/ethnic groups (P = 0.57). The width of the bars indicates the relative size of the percent change in HEI-2010 when foods eaten at daily snacking occasions are removed. For African American children, the quality of intake at snacks was more similar to the quality of intake at all other meal occasions (1% decline in HEI) than observed for Native American (4.7% decline in HEI) and Somali children (3.9% decline in HEI). For the latter two groups, snacking had the most favorable impact on the overall quality of daily dietary intake.
Racial/ethnic Differences
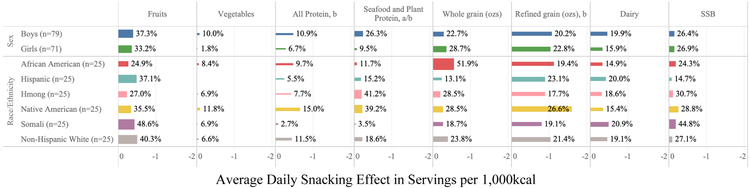
An examination of the contribution of snacks to the overall healthfulness of children’s dietary intake across ethnic/racial groups revealed several important differences (Figure 1). For African American children, the quality of dietary intake at snacks was more similar to the quality of intake at meal occasions; only a mean decline of 1% in HEI-2010 was observed when foods consumed as a snack were removed from the daily HEI-2010 calculation for African American children. Snacks contributed the most to the overall healthfulness of the mean daily dietary intake among Native American and Somali children, with these children having a 4.7% and 3.9% decline in mean daily HEI-2010 score, respectively when food consumed as snacks were removed from the calculation. Important differences in the contribution of specific food groups consumed during snacks were observed across racial groups (Figure 2). For example, the amount of refined grains consumed during snacks differed widely across racial/ethnic groups; African American youth consumed an average of 1.14 servings of refined grains per day during snacking occasions as compared to the 0.8 servings reported by Somali youth.
Figure 2. Snacking Contribution on Average Daily Child Dietary Intake of Nutrition Data System for Research (NDSR) Whole Food Categories (Servings per 1,000kcal) Measured by Three Dietary Recalls (N=150 Children): Stratified by Child Sex and Child Race/Ethnicity, Family Matters Phase I Study.
a. Snacking Intake that Differed by Child Sex (P < 0.05): Seafood and Plant Protein
b. Snacking Intake that Differed by Race/Ethnicity (P < 0.05): Refined Grains, All Protein, and Seafood and Plant Protein
Interpretation Example: Children consumed approximately 0.4 servings of fruits per 1,000kcal at daily snacking occasions. Boys consumed 37% of their daily fruit intake at snacks and girls consumed 33% of their daily fruit intake at snacks, but this result was not statistically different for boys compared with girls (Interaction P Value = 0.56).
DISCUSSION
The current study sought to understand the contribution of snacks to children’s overall diet quality (HEI-2010), as well as their daily energy and food group intakes. Findings indicated that snacking contributed positively to children’s diet quality as measured by the HEI-2010.
Our overall findings stand in contrast to previous research by Shriver, et al. that concluded that snacks contributed negatively to the overall dietary intake of the preschool-aged children in their sample; Shriver et al. cited high intake of processed snack foods, sweets (e.g. cookies and pastries), and sugar-sweetened beverages for snacks as contributing to this observed negative impact of snacks.11 Findings from three separate studies, one by Llaurado et al.14 and two by Murakami et al.12,13 help to provide some additional information into the different ways that snacks might impact overall diet quality. Using slightly different methodologies, these studies found that consumption of high energy-dense snacks contributed negatively to children’s mean overall dietary quality, whereas the mean frequency of high nutritional quality snacks, contributed positively to children’s mean overall diet quality. Further, Llaurado et al. found that children who ate more frequently throughout the day (i.e. snacks as well as meals) had a greater overall mean diet quality.14 Taken together, this handful of studies seem to suggest that snacking has the potential to yield improved mean dietary quality in young people, as long as the snacks consumed are of high nutritional quality. 12-14
In the current study, snacks were found to contribute both healthful and less healthful food groups to children’s mean overall dietary intake. Specifically, snacks contributed to the children’s mean daily intake of fruits, dairy, and whole grains. However, snacks also contributed to children’s mean dietary intake in less healthful ways, by adding to their mean daily intake of SSB, refined grains, and added sugar. Despite consumption of these less healthful foods as snacks, the diet quality of the children in the current study, as measured by the HEI-2010, was improved when foods consumed as snacks were included in the calculation, suggesting that consumption of snacks had an overall positive impact on children’s dietary intake. The current findings align with previous research studies on snacking that have found that snacks contribute substantially to children’s daily energy intake and extend existing knowledge by highlighting that while some of these calories come from high calorie, low nutrient-dense foods, snacks also seem to contribute in more healthful ways to children’s overall dietary intake profile.4,8-14,25
The current study highlighted important sex differences in the contribution of snacks to the healthfulness of children’s overall dietary intake. Importantly, boys’ HEI-2010 was lower when examining their total daily intake without the contribution of snacks. Girls’ HEI-2010 was not improved by foods consumed during snacks, suggesting that interventions focused on improving the dietary quality of snacks consumed by girls might yield substantial improvements to their overall dietary intake profile. The current study did not reveal any clear differences in snacking patterns between boys and girls that could explain this statistically significant difference in HEI-2010; instead, it is likely that this observed difference stems from many small differences in intake during snacking occasions or that with a larger sample size a more obvious pattern of differences in dietary intake between boys and girls would have emerged.
Statistically and meaningfully significant racial/ethnic differences in the contribution of snacks to dietary quality, as measured by HEI-2010, as well as food groups consumed as snacks, are another notable finding from this study. While a lower HEI-2010 was observed when snacks were removed from mean dietary intake calculation, the HEI-2010 was lowest for Native American and Somali youth, with the HEI-2010 for Hispanic and White youth not quite as low. These data suggest that youth from these backgrounds are consuming foods as snacks that are adding to their overall dietary quality. On the other hand, Hmong and African American youth were consuming far less nutritious snacks, illuminating a need for future research aimed at deepening our understanding of what foods are being consumed during snacking occasions by Hmong and African American youth. Future research should also seek to understand what factors (e.g. cultural, access, availability, taste preferences) are driving these observed differences.
Overall, children in the current study had a very low mean daily intake of vegetables and, of the small amount of vegetables consumed by children, only a negligible amount of this total was consumed during snacks. Availability and ease of accessibility of vegetables within the home environment have been previously identified as predictors of increased consumption of vegetables among children.26-35 Previous research has found that low-income families face numerous barriers to making healthful foods, such as limited availability and access to vegetables within their household; these barriers extend far beyond simply a lack of knowledge about healthful foods.36 For example, a study qualitative by Zachary et al. found that low-income families report struggling with the perishable nature of more healthful foods, such as fruits and vegetables, the distance and travel costs to grocery stores that provide lower-cost healthful foods, and the cost of specialized equipment needed to prepare fresh foods.36 The complex and numerous barriers faced by low-income families require the development and implementation of innovative solutions; findings from the current study provide evidence that future research should also seek to understand the need for cultural tailoring of interventions found to be successful at increasing vegetable consumption. Data from the current study also suggest that children are consuming a substantial portion of their total intake of SSB during snacking occasions. This finding is consistent with the paper by Popkin, et al. that explored top sources of snacking energy intake in children.37 While public health messages focused on decreasing the consumption of SSB are prevalent, understanding that these beverages are often consumed as snacks can be used to guide the creation of more tailored messages. Previous research on snacking suggests that while many parents place emphasis on the importance of nutrition at meals, many parents offer snacks to children for non-nutritive purposes, including celebrations and behavioral management of the child38; this difference in how parents approach meals versus snacks might serve to explain some of the current findings. Future research should explore culturally tailored ways to provide education to parents about healthy snack options, and ways to celebrate with children, give them praise, and manage children’s behavior that do not involve food. Further, given that many children consume multiple snacks outside of the home (e.g. school, after school care, recreation centers), there may be opportunities for changes to food policy that could increase access to healthy snack foods for children in these settings.
A strength of the study is the diversity of the sample population, which included ethnically/racially diverse and primarily low-income boys and girls; diversity within the sample allowed for an exploration of the impact of snacks on the overall healthfulness of children’s dietary intake within a population at high risk for poor dietary intake and across demographic subgroups. Another strength is the study’s reliance on parental reports of snacking occasions; this approach allowed us to capture the full range of foods consumed at snacking occasions, even if the food eaten was not a typical “snack food” (e.g. an apple, yogurt, nuts). Finally, evaluating how snacking affects the healthfulness of daily dietary intake rather than at the average snacking occasion minimizes bias from differential snacking frequency and caloric quantity and increases the external validity of our findings. A limitation of the study is the small sample size (n=150) that reduced our ability to detect differences in snacking effects for the interaction tests. For example, several large, although not statistically significant, effect sizes were observed; larger replication studies would provide an opportunity to better understand these effect sizes. Further, our findings are not generalizable to other populations beyond the sample studied; to determine external validity of the current study findings, study aims would need to be replicated within another study sample. Finally, we chose to use 24-hour dietary because this dietary assessment method is associated with the least error; however, two of the recalls were scheduled (rather than random), for all recalls we relied on parent report of child dietary intake, and previous research has demonstrated that afternoon snacks are most frequently underreported during dietary recalls.39-41 These limitations in our approach to collecting dietary intake data may have introduced some bias into results. 39-41
CONCLUSIONS
Among the children included in the current study, snacking was found to contribute positively to overall diet quality. However, snacking was also found to contribute to children’s mean consumption of refined grains and sugar-sweetened beverages. Future research should seek to better understand influences on children’s food choices at snack times and barriers to serving more healthful foods as snacks that are faced by ethnically/racially diverse families; long term, the development of interventions that aim to improve children’s consumption of healthful foods at snack times should be pursued. Finally, the positive contribution that snacking made to overall diet quality was lowest among girls and youth from Hmong and African American racial subgroups, suggesting a need for future research aimed at understanding how to best promote consumption of healthful snacks among these diverse youth.
RESEARCH SNAPSHOT.
Research Question: Does snacking (i.e., eating between meals) improve children’s diet quality? Does the contribution of snacking to children’s diet quality differ by child ethnicity/race, sex, or weight status?
Key Findings: In this observational study, eating between meals (i.e., snacking) was found to contribute positively to children’s overall diet quality. Snacking was an important source of fruit and dairy, but it also contributed to children’s consumption of refined grains and sugar-sweetened beverages. Boys received more nutritional benefits from snacking compared to girls. Differences in the nutritional benefits of snacking were also observed across ethnic/racial categories.
Acknowledgements:
The Family Matters study is a team effort and could not have been accomplished without the dedicated staff who carried out the home visits, including: Awo Ahmed, Nimo Ahmed, Rodolfo Batres, Carlos Chavez, Mia Donley, Michelle Draxton, Carrie Hanson-Bradley, Sulekha Ibrahim, Walter Novillo, Alejandra Ochoa, Luis “Marty” Ortega, Anna Schulte, Hiba Sharif, Mai See Thao, Rebecca Tran, Bai Vue, and Serena Xiong. These individuals have given permission for this manuscript and other manuscripts stemming from data collected as a part of the Family Matters study to be submitted for publication in peer-reviewed journals, including the Journal of the Academy for Nutrition and Dietetics.
Funding/financial disclosures:
Research is supported by grant no. R01 HL126171-04 from the National Heart, Lung and Blood Institute (PI: Jerica Berge) and the first authors (KAL) time is supported by grant no. K23-HD090324-01A1 from the National Institute of Child Health and Human Development (PI: Katie Loth). Content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung and Blood Institute, the National Institute of Child Health and Human Development or the National Institutes of Health.
Footnotes
Conflict of interest disclosures:
All authors have no financial disclosures to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Katie A. Loth, Department of Family Medicine and Community Health, University of Minnesota, 717 Delaware Street, Suite 400, Minneapolis, MN 55414.
Allan Tate, Department of Family Medicine and Community Health, University of Minnesota, 717 Delaware Street, Suite 400, Minneapolis, MN 55414.
Amanda Trofholz, Department of Family Medicine and Community Health, University of Minnesota, 717 Delaware Street, Suite 400, Minneapolis, MN 55414.
Jennifer Orlet Fisher, Department of Social and Behavioral Sciences, College of Public Health, Temple University, 3223 N. Broad Street, Suite 175, Philadelphia, PA 19140.
Dianne Neumark-Sztainer, School of Public Health, University of Minnesota, 1300 South Second Street, Minneapolis, MN 55454.
Jerica M. Berge, Department of Family Medicine and Community Health, University of Minnesota, 717 Delaware Street, Suite 400, Minneapolis, MN 55414.
References
- 1.Banfield EC, Liu Y, Davis JS, Chang S, Frazier-Wood AC. Poor adherence to US dietary guidelines for children and adolescents in the national health and nutrition examination survey population. J Acad Nutr Diet. 2016;116(1):21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pratt CA, Stevens J, Daniels S. Childhood obesity prevention and treatment recommendations for future research. Am J Prev Med. 2008;35(3):249–252. doi: 10.1016/j.amepre.2008.05.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spiegel AM, Alving BM. Executive summary of the Strategic Plan for National Institutes of Health Obesity Research. Am J Clin Nutr. 2005;82(1):211S–214S. [DOI] [PubMed] [Google Scholar]
- 4.Piernas C, Popkin BM. Trends in snacking among US children. Health Aff (Millwood). 2010;29(3):398–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Piernas C, Popkin BM. Food Portion Patterns and Trends among US Children and the Relationship to Total Eating Occasion Size, 1977–2006–3. J Nutr. 2011; 141(6): 1159–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Piernas C, Popkin BM. Increased portion sizes from energy-dense foods affect total energy intake at eating occasions in US children and adolescents: patterns and trends by age group and sociodemographic characteristics, 1977–2006–. Am J Clin Nutr. 2011;94(5):1324–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jahns L, Siega-Riz AM, Popkin BM. The increasing prevalence of snacking among US children from 1977 to 1996. J Pediatr. 2001;138(4):493–498. [DOI] [PubMed] [Google Scholar]
- 8.Larson N, Story M. A review of snacking patterns among children and adolescents: what are the implications of snacking for weight status? Child Obes. 2013;9(2): 104–115. [DOI] [PubMed] [Google Scholar]
- 9.Hess J, Slavin J, Hess J, Slavin J. Snacking for a Cause: Nutritional Insufficiencies and Excesses of U.S. Children, a Critical Review of Food Consumption Patterns and Macronutrient and Micronutrient Intake of U.S. Children. Nutrients. 2014;6(11):4750–4759. doi: 10.3390/nu6114750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dunford EK, Popkin BM. 37 year snacking trends for US children 1977–2014. Pediatr Obes. 2017. http://onlinelibrary.wiley.com/doi/10.1111/ijpo.12220/full. Accessed October 13, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shriver LH, Marriage BJ, Bloch TD, et al. Contribution of snacks to dietary intakes of young children in the United States. Matern Child Nutr. 2018;14(1):e12454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murakami K, Livingstone MBE. Associations between energy density of meals and snacks and overall diet quality and adiposity measures in British children and adolescents: the National Diet and Nutrition Survey. Br J Nutr. 2016;116(9):1633–1645. [DOI] [PubMed] [Google Scholar]
- 13.Murakami K Associations between nutritional quality of meals and snacks assessed by the Food Standards Agency nutrient profiling system and overall diet quality and adiposity measures in British children and adolescents. Nutrition. 2018;49:57–65. [DOI] [PubMed] [Google Scholar]
- 14.Llauradó E, Albar SA, Giralt M, Solà R, Evans CEL. The effect of snacking and eating frequency on dietary quality in British adolescents. Eur J Nutr. 2016;55(4):1789–1797. [DOI] [PubMed] [Google Scholar]
- 15.Berge JM, Trofholz A, Tate AD, et al. Examining unanswered questions about the home environment and childhood obesity disparities using an incremental, mixed-methods, longitudinal study design: The Family Matters study. Contemp Clin Trials. 2017;62:61–76. doi: 10.1016/j.cct.2017.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.U.S. Low-Income Working Families Increasing – Population Reference Bureau. https://www.prb.org/us-working-poor-families/. Accessed April 11, 2019.
- 17.Shiffman S, Stone AA, Hufford MR. Ecological Momentary Assessment. Annu Rev Clin Psychol. 2008;4(1): 1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415 [DOI] [PubMed] [Google Scholar]
- 18.Nutrition Data System for Research. Minneapolis, MN: Nutrition Coordinating Center [Google Scholar]
- 19.NDSR Support. NCC Nutr Coord Cent. http://www.ncc.umn.edu/ndsr-support/. Accessed July 10, 2019.
- 20.Healthy Eating Index (HEI). NCC Nutr Coord Cent. http://www.ncc.umn.edu/healthy-eating-index-hei/. Accessed October 31, 2018.
- 21.Guenther PM, Kirkpatrick SI, Reedy J, et al. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J Nutr. 2014:jn–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guenther PM, Casavale KO, Reedy J, et al. Update of the healthy eating index: HEI-2010. J Acad Nutr Diet. 2013;113(4): 569–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Choosing a Method. https://epi.grants.cancer.gov/hei/tools.html. Accessed April 11, 2019. [Google Scholar]
- 24.Stata.
- 25.Johnson GH, Anderson GH. Snacking definitions: impact on interpretation of the literature and dietary recommendations. Crit Rev Food Sci Nutr. 2010;50(9):848–871. [DOI] [PubMed] [Google Scholar]
- 26.Wyse R, Campbell E, Nathan N, Wolfenden L. Associations between characteristics of the home food environment and fruit and vegetable intake in preschool children: a cross-sectional study. BMC Public Health. 2011;11(1):938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hanson NI, Neumark-Sztainer D, Eisenberg ME, Story M, Wall M, others. Associations between parental report of the home food environment and adolescent intakes of fruits, vegetables and dairy foods. Public Health Nutr. 2005;8(1):77–85. [DOI] [PubMed] [Google Scholar]
- 28.Cullen KW, Baranowski T, Rittenberry L, Cosart C, Hebert D, de Moor C. Child-reported family and peer influences on fruit, juice and vegetable consumption: reliability and validity of measures. Health Educ Res. 2001;16(2):187–200. [DOI] [PubMed] [Google Scholar]
- 29.Neumark-Sztainer D, Wall M, Perry C, Story M. Correlates of fruit and vegetable intake among adolescents:: Findings from Project EAT. Prev Med. 2003;37(3):198–208. [DOI] [PubMed] [Google Scholar]
- 30.Nicklas TA, Baranowski T, Baranowski JC, Cullen K, Rittenberry L, Olvera N. Family and child-care provider influences on preschool children’s fruit, juice, and vegetable consumption. Nutr Rev. 2001;59(7):224–235. [DOI] [PubMed] [Google Scholar]
- 31.Loth KA, MacLehose RF, Larson N, Berge JM, Neumark-Sztainer D. Food availability, modeling and restriction: How are these different aspects of the family eating environment related to adolescent dietary intake? Appetite. 2016;96:80–86. doi: 10.1016/j.appet.2015.08.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arcan C, Neumark-Sztainer D, Hannan P, van den Berg P, Story M, Larson N. Parental Eating Behaviours, Home Food Environment and Adolescent Intakes of Fruits, Vegetables and Dairy Foods: Longitudinal Findings from Project EAT. Public Health Nutr. 2007;10(11): 1257–1265. doi: 10.1017/S1368980007687151 [DOI] [PubMed] [Google Scholar]
- 33.Orlet Fisher J, Mitchell DC, Wright HS, Birch LL. Parental influences on young girls’ fruit and vegetable, micronutrient, and fat intakes. J Am Diet Assoc. 2002;102(1):58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Trofholz AC, Tate AD, Draxten ML, et al. What’s Being Served for Dinner? An Exploratory Investigation of the Associations between the Healthfulness of Family Meals and Child Dietary Intake. J Acad Nutr Diet. 2017;117(1):102–109. doi: 10.1016/j.jand.2016.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Neumark-Sztainer D, MacLehose R, Loth K, Fulkerson JA, Eisenberg ME, Berge J. What’s for dinner? Types of food served at family dinner differ across parent and family characteristics. Public Health Nutr. 2012;FirstView:1–11. doi: 10.1017/S1368980012004594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zachary DA, Palmer AM, Beckham SW, Surkan PJ. A framework for understanding grocery purchasing in a low-income urban environment. Qual Health Res. 2013;23(5):665–678. [DOI] [PubMed] [Google Scholar]
- 37.Dunford EK, Popkin BM. 37 year snacking trends for US children 1977-2014. Pediatr Obes. 2018;13(4):247–255. doi: 10.1111/ijpo.12220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fisher JO, Wright G, Herman AN, et al. “Snacks are not food”. Low-income, urban mothers’ perceptions of feeding snacks to their preschool-aged children. Appetite. 2015;84:61–67. [DOI] [PubMed] [Google Scholar]
- 39.Gemming L, Ni Mhurchu C. Dietary under-reporting: what foods and which meals are typically under-reported? Eur J Clin Nutr. 2016;70(5):640–641. doi: 10.1038/ejcn.2015.204 [DOI] [PubMed] [Google Scholar]
- 40.Foster E, Bradley J. Methodological considerations and future insights for 24-hour dietary recall assessment in children. NutrRes. 2018;51:1–11. doi: 10.1016/j.nutres.2017.11.001 [DOI] [PubMed] [Google Scholar]
- 41.Thompson FE, Kirkpatrick SI, Subar AF, et al. The National Cancer Institute’s Dietary Assessment Primer: A Resource for Diet Research. J Acad Nutr Diet. 2015;115(12): 1986–1995. doi: 10.1016/j.jand.2015.08.016 [DOI] [PMC free article] [PubMed] [Google Scholar]