Abstract
Social connection is robustly associated with physical and mental health. So important is social connection that it features prominently in several etiological theories of serious psychopathology. Most notably, the social deafferentation hypothesis of schizophrenia posits that social anhedonia (SA) and isolation cause neural changes that produce psychosis. Here, we test several tenants of this theory by examining the relation between SA, psychotic-like experiences (PLE), and social networks. We find that SA and PLE are related to social networks, and that the relation between SA and PLE can be explained, in part, by the impact of SA on social networks.
Keywords: social deafferentation, social networks, schizophrenia
1. Introduction
Social connectedness carries profound consequences for our mental and physical health (Holt-Lunstad et al 2015; Kawachi, 2001; Yang et al., 2016). So consequential is our extent of social connection that a lack thereof has been proposed as an etiological factor in the development of psychopathology. Most notably, Hoffman (2007) describes a social deafferentation hypothesis of schizophrenia akin to neurological syndromes involving the loss of sensory input, and subsequent cortical reorganization that produces aberrant sensory experiences (e.g., phantom limb). According to this hypothesis, predisposing factors for social withdrawal, such as social anhedonia (SA), lead to social isolation and a loss of social input, which curtails information to the social brain. Neural changes occur as a result, causing the brain to endogenously produce aberrant experiences and cognitions with social meaning (i.e., psychotic experiences). Beyond neural changes, social isolation may foster psychotic experiences by removing a buffer from stress (Nuechterlein and Dawson, 1984) and a source for reality-testing (Garety et al., 2001). Whatever the mechanism, a key factor in this model is a characteristic or experience (e.g., SA) that leads to diminished social networks.
Support for the social deafferentation hypothesis comes from several lines of work. People with psychotic disorders and psychotic-like experiences (PLE) have smaller social networks (Gayer-Anderson and Morgan, 2013) and fewer social interactions (Granholm et al., 2019). Moreover, SA and accompanying withdrawal and isolation often precede and predict the onset of psychotic disorders (Gooding et al., 2005; Kwapil, 1998; Matheson et al., 2013; Tarbox and Pogue-Geile, 2008; Velthorst and Meijer, 2012; Wiles et al., 2006), proving themselves to be robust risk factors. Finally, among those diagnosed with a psychotic disorder, psychotic symptoms are more likely to occur when one is alone (Myin-Germeys et al., 2001).
If loss of social connectedness, by way of SA, contributes to PLE, it would bolster characterizations of social withdrawal and isolation as a public health crisis and calls for improving social connection as a public health priority (Holt-Lunstad et al., 2017). Thus, here, we evaluate the relations between SA, PLE, and social networks in a large international sample from the general population assuming a continuous, dose- response relation between these factors (van Os et al., 2009). Further, we conduct a formal test of a major component of the social deafferentation hypothesis by evaluating whether SA impacts PLE through its effect on social networks.
2. Methods
2.1. Participants
Participants were an international sample of 2,512 individuals who visited TestMyBrain.org. Inclusion criteria were 18-65 years of age and fluent/native English- speaking. Participants were on average in their early 30s (M=33.4±13.1), predominantly female (59.2%), White (68.7%), and from the United States (51.5%). Consent and study procedures were reviewed by the Harvard Committee for the Use of Humans Subjects.
2.2. Measures
Participants completed three self-report measures: the Social Network Index (SNI; Cohen, 1997), the short form of the Revised Social Anhedonia Scale (RSAS; Winterstein et al., 2011), and the Prodromal Questionnaire—Brief (PQB; Loewy et al., 2011). We selected these measures because they are widely used in their respective fields, and exhibit adequate psychometric properties (e.g., Loewy et al., 2011; Winterstein et al., 2011). Critically, elevated scores on the RSAS and PQB are associated with increased risk for psychosis-risk syndromes and psychotic-spectrum disorders (e.g., Kwapil, 1998; Savill et al., 2018). The SNI assesses engagement in 12 different relationships from which three social network metrics are derived: number of people in one’s social network (number of people), number of high-contact social roles in which the participant has regular contact (network diversity), and the number of social domains in which the participant is highly active (i.e., has at least 4 high-contact people in a given domain; embedded networks). The RSAS is a 15-item true/false questionnaire that assess social amotivation and lack of social pleasure (α=.83). The PQB is a 21-item questionnaire that assess the frequency and associated distress of 21 positive symptoms of psychotic disorders. Participants who endorse an item on the frequency scale (a=.87) are asked a follow-up question about distress using a 5-point Likert scale (strongly disagree—scored 1—to strongly agree—scored 5; α=.93).
2.3. Analysis
Data were analyzed in R (R Core Team, 2018). We performed a 5% Winsorization of the three SNI metrics and PQB-Distress scores after identifying outlying scores (>3 SD+M) on these measures. Pearson r correlations are accompanied by 95% bias-corrected-and-accelerated (BCa) CIs generated from 10,000 bootstrap samples with the package boot (Canty and Ripley, 2017; Davison and Hinkley, 1997). Correlations are interpreted using the guidelines described in Gignac and Szodorai (2016). We used the package psych (Revelle, 2018) to conduct a multiple mediation analysis evaluating the effect of social anhedonia on psychotic-like experiences (separately for frequency and distress) through the three SNI metrics; that is, the indirect effect of RSAS on PQB through SNI-Number of People, SNI-Embedded Networks, and SNI-Network Diversity. We provide a bootstrapped estimate of the total indirect effect and specific indirect effects (RSAS-→SNI-→PQB) along with 95% BCa CIs derived from 10,000 bootstrap samples (Preacher and Hayes, 2008). As recommended by others (Miočević et al., 2018), we report fully standardized estimates which can be interpreted as the SDs change in PQB for every 1 SD increase in RSAS indirectly through SNI.
3. Results
First, we examined the relation between the measures of psychosis-proneness and social networks (Table 1). The association between SA and the social network metrics were large and similar across the SNI metrics. These correlations were larger than those observed for PLE and the social network metrics, which were relatively small, similar between the three social network metrics, and slightly higher for frequency versus distress. Thus, both SA and PLE are related to one’s social network such that greater SA and PLE are associated with smaller and less diverse social networks, and fewer highly active social domains.
Table 1.
Descriptive statistics and measure correlations.
| M | SD | Min-Max | Pearson r [95% CI]* | |||||
|---|---|---|---|---|---|---|---|---|
| 2. | 3. | 4. | 5. | 6. | ||||
| 1. SNI-Network Diversity | 4.6 | 2.0 | 0-12 | .77 [.75, .78] | .69 [.67, −.71] | −.18 [−.22, −.14] | −.14 [−.18, −.11] | −.35 [−.39, −.32] |
| 2. SNI-Number of People | 15.0 | 8.4 | 2-37 | .89 [.88, −.89] | −.18 [−.22, −.15] | −.15 [−.19, −.11] | −.38 [−.41, −.35] | |
| 3. SNI-Embedded Networks | 1.6 | 1.2 | 0-5 | −.17 [−.21, −.13] | −.12 [−.16, −.08] | −.37 [−.40, −.34] | ||
| 4. PQB-Frequency | 7.6 | 5.1 | 0-21 | .78 [.76, .80] | .31 [.27, .34] | |||
| 5. PQB-Distress | 29.3 | 22.4 | 0-75 | .27 [.23, .30] | ||||
| 6. RSAS | 5.3 | 3.8 | 0-15 | |||||
All correlations p<.0001.
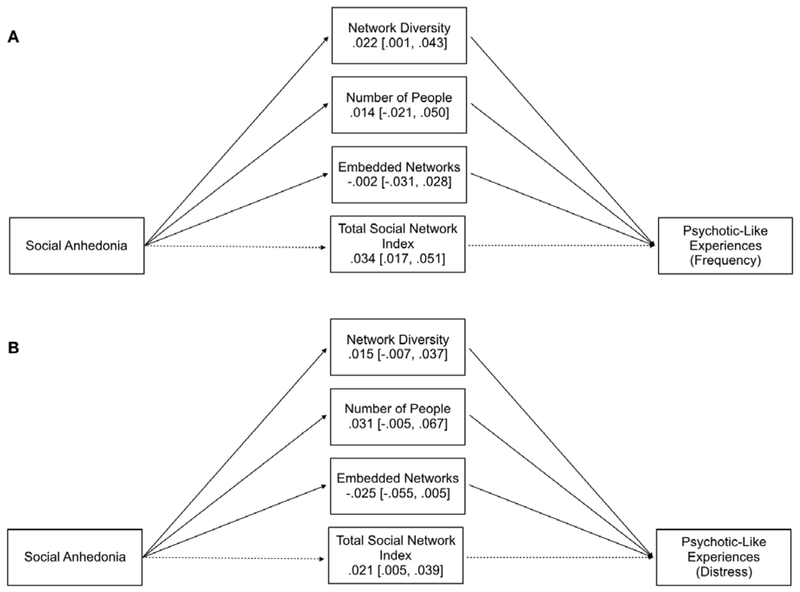
Next, we used mediation analysis to evaluate the hypothesis that, consistent with the social deafferentation hypothesis, SA would impact PLE through its deleterious impact on social networks. In line with this idea, for both frequency and distress, the bootstrapped CI of the total indirect effect did not contain zero indicating that social networks mediated the association between SA and PLE, with the mediation effect being slightly larger for frequency (Figure 1). Examination of the specific indirect effects revealed that for frequency, only network diversity was a mediator; for distress, none of the individual indirect effects were different from zero.
Figure 1.
Results of the multiple mediation analysis. Values represent fully standardized point estimates of the indirect effect and their bias-corrected-and-accelerated 95% CIs derived from 10,000 bootstrap samples. The top panel (A) depicts the results for psychotic-like experiences (Prodromal Questionnaire—Brief) frequency; the bottom panel (B) depicts the results for psychotic-like experiences distress.
4. Discussion
Here, we find that SA and PLE are related to smaller, less diverse, and less embedded social networks. These findings converge with those from other studies evaluating patient, at-risk, and healthy samples (Horan et al., 2006; Robustelli et al., 2017; Velthorst and Meijer, 2012). Further, in support of the social deafferentation hypothesis, we find that the relation between SA and PLE can be explained, in part, by the impact of SA on social networks. Interestingly, for at least the frequency of PLE, this effect was largely driven by network diversity; that is, the number of different social roles in which the participant has regular social contact. This finding converges with a number of brain imaging studies suggesting that network diversity—as opposed to the number of people in one’s network—may be particularly important for the structural and functional development of the social brain (Dziura and Thompson, 2014; Molesworth et al., 2015). Thus, the diversity of social roles one plays in their social network may be a better proxy for social support, social connectedness, or other factors that might protect against neural changes and concomitant PLE.
Beyond the inherent limitations of performing mediation analyses with cross-sectional data (Maxwell and Cole, 2007), we note that these data cannot be taken to demonstrate causal relations among the variables, including the hypothesized direction of causation (i.e., SA-→social networks-→PLE). Indeed, other research suggests reverse causation such that psychotic symptoms precipitate a social “network crisis” (Lipton et al., 1981) possibly by way of odd/eccentric behavior, paranoia, or social skills deficits that ultimately serve to isolate an individual. Conversely, other studies suggest that disturbed social networks and social withdrawal predate the onset of psychotic symptoms (Gayer-Anderson and Morgan, 2013; Gooding et al., 2005; Kwapil, 1998; Matheson et al., 2013; Tarbox and Pogue-Geile, 2008; Wiles et al., 2006). Of course, causation may be a dynamic, reciprocal process operating in both directions, such that social withdrawal contributes to the onset of symptoms, and the onset of symptoms (odd/eccentric behavior, paranoia, poor social skills) further negatively impacts social networks. The present findings cannot adjudicate between these possibilities; longitudinal data are needed. We also note that just under half of the participants (49.5%) were within the peak age range of risk for psychotic disorders (i.e., 29 years of age or younger; van der Werf et al., 2014) meaning that the majority of our participants would not be expected to develop a psychotic disorder. This also means that the interplay of SA, social networks, and PLE is still detectable in a non-high-risk, general population sample. Finally, the mediation effect was extremely small suggesting that processes related to PLE, but not explicitly tested here (e.g., social defeat; Selten et al., 2013) may be at work or that aspects of our study sample (e.g., a non-high-risk, general population sample) may have attenuated the relations among these variables.
Notwithstanding these considerations, the data from the current study add to a growing body of literature demonstrating the importance of social networks for psychological health. Together, these findings suggest that social isolation, and factors that contribute to social isolation, whether through deliberate social withdrawal as in SA or through exclusion and social defeat (e.g., Selten et al., 2013) should be a public health priority (Holt-Lunstad et al., 2017).
Highlights.
Social anhedonia and psychotic-like experiences are related to social networks
Social anhedonia may impact psychotic-like experiences through social networks
Social anhedonia and isolation should be a public health priority
Acknowledgments
We thank the TestMyBrain.org volunteers for their participation. This work was supported indirectly by a grant from National Institutes of Health to D.D.-F. (1L30MH117569-01).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Canty A, Ripley B, 2017. boot: Bootstrap R (S-Plus) Functions. R package version 1.3–20. [Google Scholar]
- Cohen S, 1997. Social Ties and Susceptibility to the Common Cold. JAMA J. Am. Med. Assoc 277, 1940 10.1001/jama.1997.03540480040036 [DOI] [PubMed] [Google Scholar]
- Davison AC, Hinkley DV, 1997. Bootstrap methods and their application. Cambridge University Press, Cambridge; New York, NY, USA. [Google Scholar]
- Dziura SL, Thompson JC, 2014. Social-Network Complexity in Humans Is Associated With the Neural Response to Social Information. Psychol. Sci 25, 2095–2101. https://doi.Org/10.1177/0956797614549209 [DOI] [PubMed] [Google Scholar]
- Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE, 2001. A cognitive model of the positive symptoms of psychosis. Psychol. Med 31 https://doi.Org/10.1017/S0033291701003312 [DOI] [PubMed] [Google Scholar]
- Gayer-Anderson C, Morgan C, 2013. Social networks, support and early psychosis: a systematic review. Epidemiol. Psychiatr. Sci 22, 131–146. 10.1017/S2045796012000406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gignac GE, Szodorai ET, 2016. Effect size guidelines for individual differences researchers. Personal. Individ. Differ 102, 74–78. https://doi.Org/10.1016/j.paid.2016.06.069 [Google Scholar]
- Gooding DC, Tallent KA, Matts CW, 2005. Clinical Status of At-Risk Individuals 5 Years Later: Further Validation of the Psychometric High-Risk Strategy. J. Abnorm. Psychol 114, 170–175. https://doi.Org/10.1037/0021-843X.114.1.170 [DOI] [PubMed] [Google Scholar]
- Granholm E, Holden JL, Mikhael T, Link PC, Swendsen J, Depp C, Moore RC, Harvey PD, 2019. What Do People With Schizophrenia Do All Day? Ecological Momentary Assessment of Real-World Functioning in Schizophrenia. Schizophr. Bull, 10.1093/schbul/sbz070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman RE, 2007. A Social Deafferentation Hypothesis for Induction of Active Schizophrenia. Schizophr. Bull 33, 1066–1070. https://doi.Org/10.1093/schbul/sbm079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Robles TF, Sbarra DA, 2017. Advancing social connection as a public health priority in the United States. Am. Psychol 72, 517–530. https://doi.Org/10.1037/amp0000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D, 2015. Loneliness and Social Isolation as Risk Factors for Mortality: A Meta-Analytic Review. Perspect. Psychol. Sci 10, 227–237. 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- Horan WP, Subotnik KL, Snyder KS, Nuechterlein KH, 2006. Do Recent-Onset Schizophrenia Patients Experience a “Social Network Crisis”? Psychiatry Interpers. Biol. Process 69, 115–129. https://doi.Org/10.1521/psyc.2006.69.2.115 [DOI] [PubMed] [Google Scholar]
- Kawachi I, 2001. Social Ties and Mental Health. J. Urban Health Bull. N. Y. Acad. Med 78, 458–467. https://doi.Org/10.1093/jurban/78.3.458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwapil TR, 1998. Social anhedonia as a predictor of the development of schizophrenia-spectrum disorders. J. Abnorm. Psychol 107, 558–565. 10.1037/0021-843X.107.4.558 [DOI] [PubMed] [Google Scholar]
- Lipton FR, Cohen CI, Fischer E, Katz SE, 1981. Schizophrenia: A Network Crisis. Schizophr. Bull 7, 144–151. https://doi.Org/10.1093/schbul/7.1.144 [DOI] [PubMed] [Google Scholar]
- Loewy RL, Pearson R, Vinogradov S, Bearden CE, Cannon TD, 2011. Psychosis risk screening with the Prodromal Questionnaire — Brief Version (PQ- B). Schizophr. Res 129, 42–46. https://doi.Org/10.1016/j.schres.2011.03.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson SL, Vijayan H, Dickson H, Shepherd AM, Carr VJ, Laurens KR, 2013. Systematic meta-analysis of childhood social withdrawal in schizophrenia, and comparison with data from at-risk children aged 9–14 years. J. Psychiatr. Res 47, 1061–1068. https://doi.Org/10.1016/j.jpsychires.2013.03.013 [DOI] [PubMed] [Google Scholar]
- Maxwell SE, Cole DA, 2007. Bias in cross-sectional analyses of longitudinal mediation. Psychol. Methods 12, 23–44. 10.1037/1082-989X.12.1.23 [DOI] [PubMed] [Google Scholar]
- Miočević M, O’Rourke HP, MacKinnon DP, Brown HC, 2018. Statistical properties of four effect-size measures for mediation models. Behav. Res. Methods 50, 285–301. 10.3758/s13428-017-0870-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molesworth T, Sheu LK, Cohen S, Gianaros PJ, Verstynen TD, 2015. Social network diversity and white matter microstructural integrity in humans. Soc. Cogn. Affect. Neurosci 10, 1169–1176. 10.1093/scan/nsv001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myin-Germeys I, Nicolson NA, Delespaul PA, 2001. The context of delusional experiences in the daily life of patients with schizophrenia. Psychol. Med 31, 489–498. https://doi.Org/10.1017/S0033291701003646 [DOI] [PubMed] [Google Scholar]
- Nuechterlein KH, Dawson ME, 1984. A Heuristic Vulnerability/Stress Model of Schizophrenic Episodes. Schizophr. Bull 10, 300–312. https://doi.Org/10.1093/schbul/10.2.300 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF, 2008. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 40, 879–891. https://doi.Org/10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- R Core Team, 2018. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. [Google Scholar]
- Revelle W, 2018. psych: Procedures for Personality and Psychological Research, Northwestern University, Evanston, Illinois, USA, https://CRAN.R-project.org/package=psych. Version = 1.8.12 [Google Scholar]
- Robustelli BL, Newberry RE, Whisman MA, Mittal VA, 2017. Social relationships in young adults at ultra high risk for psychosis. Psychiatry Res. 247, 345–351. https://doi.Org/10.1016/j.psychres.2016.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savill M, D’Ambrosio J, Cannon TD, Loewy RL, 2018. Psychosis risk screening in different populations using the Prodromal Questionnaire: A systematic review: SAVILL et al. Early Interv. Psychiatry 12, 3–14. 10.1111/eip.12446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selten J-P, van der Ven E, Rutten BPF, Cantor-Graae E, 2013. The Social Defeat Hypothesis of Schizophrenia: An Update. Schizophr. Bull 39, 1180–1186. https://doi.Org/10.1093/schbul/sbt134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarbox SI, Pogue-Geile MF, 2008. Development of social functioning in preschizophrenia children and adolescents: A systematic review. Psychol. Bull 134, 561–583. https://doi.Org/10.1037/0033-2909.34.4.561 [DOI] [PubMed] [Google Scholar]
- van der Werf M, Hanssen M, Kohler S, Verkaaik M, Verhey FR, RISE Investigators, van Winkel R, van Os J, Allardyce J, 2014. Systematic review and collaborative recalculation of 133 693 incident cases of schizophrenia. Psychol. Med 44, 9–16. 10.1017/S0033291712002796 [DOI] [PubMed] [Google Scholar]
- van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L, 2009. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol. Med 39, 179–195. 10.1017/S0033291708003814 [DOI] [PubMed] [Google Scholar]
- Velthorst E, Meijer C, 2012. The association between social anhedonia, withdrawal and psychotic experiences in general and high-risk populations. Schizophr. Res 138, 290–294. https://doi.Org/10.1016/j.schres.2012.03.022 [DOI] [PubMed] [Google Scholar]
- Wiles NJ, Zammit S, Bebbington P, Singleton N, Meltzer H, Lewis G, 2006. Self-reported psychotic symptoms in the general population: Results from the longitudinal study of the British National Psychiatric Morbidity Survey. Br. J. Psychiatry 188, 519–526. 10.1192/bjp.bp.105.012179 [DOI] [PubMed] [Google Scholar]
- Winterstein BP, Silvia PJ, Kwapil TR, Kaufman JC, Reiter-Palmon R, Wigert B, 2011. Brief assessment of schizotypy: Developing short forms of the Wisconsin Schizotypy Scales. Personal. Individ. Differ 51,920–924. https://doi.Org/10.1016/j.paid.2011.07.027 [Google Scholar]
- Yang YC, Boen C, Gerken K, Li T, Schorpp K, Harris KM, 2016. Social relationships and physiological determinants of longevity across the human life span. Proc. Natl. Acad. Sci 113, 578–583. 10.1073/pnas.1511085112 [DOI] [PMC free article] [PubMed] [Google Scholar]