Short abstract
Objective
With sensors, we are increasingly able to assess sitting behaviour during the day. However, there is no consensus among researchers on the best outcome measures for representing the accumulation of sedentary time during the day.
Methods
We analysed the pattern measures of sedentary behaviour. Articles reporting patterns measures in adults, in which behaviour data was collected with a sensor were included. We discuss the strengths and weaknesses of the pattern measures of sedentary behaviour and provide recommendations for choosing objective measures of sedentary behaviour.
Results
Most studies report the number of sitting bouts during the day. Others focus on the number of breaks and/or periods of physical activity. Simple measures of sedentary behaviour were most popular. More complex pattern measures, such as the Gini index or the half-life bout duration, that capture the distribution of lengths of sitting periods in a single number, were reported sparsely. The sedentary patterns that were reported in the various studies were difficult to compare, due to the differences among measurement devices, data analysis protocols and a lack of basic outcome parameters such as total wear-time and total sedentary time.
Conclusions
Objective sedentary measures can be grouped into simple and complex measures of sedentary time accumulation during the day. These measures serve different goals. The answer to the question as to which measures are most suitable to report, is strongly dependent on the research question. We have shown that the reported measures were dependent on (a) the sensing method, (b) the classification method, (c) the experimental and data cleaning protocol and (d) the applied definitions of bouts and breaks. We recommend that studies should always report total wear-time, total sedentary time, number of bouts and at least one measure describing the diversity of bout lengths in the sedentary behaviour such as the half-life bout duration. Additionally, we recommend reporting the measurement conditions and data processing steps.
Keywords: Pattern, objective assessment, sensor, accelerometer, inclinometer, adults, sedentary behaviour, bout, breaks, physical activity
Background
High levels of sedentary behaviour are associated with an increased risk for chronic diseases and poor health outcomes.1,2 This risk is unrelated to the amounts of moderate- to vigorous-intensive physical activity that a person achieves during the day.1–4 Moreover, there is little association between the time spent in sedentary behaviour and the time spent in moderate- to vigorous-intensive physical activity in the course of a day,5 meaning that an individual can be simultaneously very sedentary, while being sufficiently physically active.6 The focus of assessing sedentary behaviour has shifted over the last years from a focus on total sedentary time during a day towards approaches that focus on the pattern of accumulation of sedentary behaviour. This refers to a pattern which is a regular and intelligible form or sequence discernible in the way in which sedentary behaviour happens.7 Studies that apply these pattern measures indicate that the breaking up of sedentary time may be beneficial for cardiovascular disease risk. Prolonged sedentary time affects cardio-metabolic and inflammatory biomarkers, independent of the total sedentary time.8,9 In other words, sitting for many hours is a health risk, and the sedentary pattern affects this health risk.
Sedentary behaviour research has, until recently, predominantly relied on self-reported measures for determining total sitting time per day, for example by means of questionnaires and diaries. However, self-reported measures do not provide detailed information on the pattern of accumulation of sedentary behaviour, as they are hindered by recall and normative biases.10 The introduction of wearable activity sensors has radically expanded the range of measurement instruments, as sensors are extremely capable of recording data at a very high level of granularity suitable for uncovering the patterns of accumulation.
Wearable activity sensors are predominantly based on two different inertial sensing techniques: accelerometry and inclinometry. These two types of sensing techniques are reflected in the most widely adopted definition of sedentary behaviour: ‘sitting or reclining while expending ≤1.5 metabolic equivalents’,11 as the strength of accelerometry is measuring intensity of movement, while the strength of inclinometry is measuring posture.12 Accelerometry and inclinometry refer to how data are processed by the sensor, and not to the type of data collected by the sensor. For example, both can be based on the accelerations resulting from body movement and gravitation. Accelerometry-based sensors often use the intensity of accelerations to estimate energy expenditure during daily life. For this, accelerometer-based sensors use cut-points to distinguish intensity levels, which are most sensitive for moderate- to vigorous physical activity.13 Inclinometry-based sensors measure the inclination of body part(s) to estimate postural information such as standing, sitting, lying and walking. These types of sensors are very accurate in distinguishing sitting and lying from standing and stepping.14 Both sensing types have their strengths at the opposite ends of the activity spectrum. Where the whole spectrum of activities from sitting to high intensity physical activity is relevant, the choice for the best sensor type is less evident.
Properly measuring and interpreting sedentary behaviour will help in the development of health and clinical guidelines on sedentary behaviour.15 In this literature review, we assess which pattern measures have been used to capture daily sedentary behaviour (patterns) and determine how these measures disclose information on the accumulation of sedentary behaviour. This review will help researchers to understand the differences between the various pattern measures, as well as their strengths and weaknesses. We will provide general recommendations for the use of sedentary pattern measures in scientific research and clinical practice.
Methods
Search strategy and selection
Articles reporting sedentary behaviour patterns in adults, measured with wearable sensors, were included in this systematic review. Literature searches were conducted using ISI Web of Knowledge and Scopus (see Supplemental Material Additional File 1. Search strategy, conducted on 8 June 2016). Combinations of the following key terms were used to search the databases: sedentary behaviour terms (sedentary behaviour, sitting, sedentary time, sedentary lifestyle, and physical inactivity); pattern terms (pattern, bout, behaviour); sensor terms (sensor, accelerometer, pedometer, Actigraph, ActivPal); and objective measures terms (objective, monitor, measure, classification, pattern, accumulation). We applied the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines to report our findings.
Screening
Two authors (STB and LvV) individually screened the search results and identified studies based on (a) the study title and (b) the abstract. Studies were included if they described sedentary behaviour pattern measures within the timeframe of a day, based on wearable sensor data in adults (age ≥18 years) and were peer-reviewed journal articles, letters or conference proceedings. Studies were excluded if they described ambient sensing techniques (i.e. not on-body), provided graphical representations of sedentary patterns only, were not in English, were review articles or were published before 1989 (as modern wearable sensors were yet not available back then). If the authors did not agree, they discussed their arguments until agreement was reached.
Data extraction and synthesis
From each article, information about the type of sedentary behaviour pattern measures, specification and validation of the measure were extracted and synthesised. These measures were complemented with information about the study design, sample characteristics, sample size, sensor type, data cleaning, activity classification and analysis methods. The principal summary measures of this review are the number of times a specific pattern measure is reported and its implications for data analysis and interpretation. Results are summarised on total wear-time, bouts, breaks and composite measures.
Results
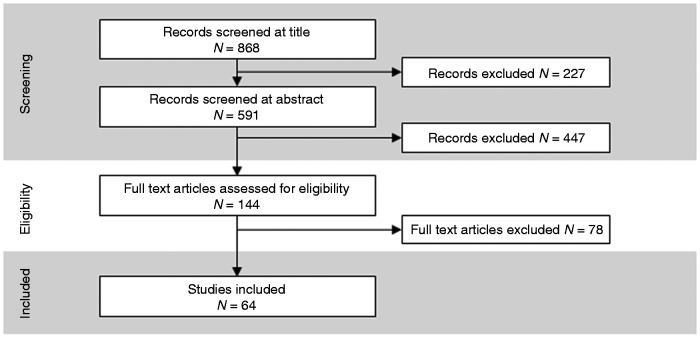
A total of 868 unique titles were identified and screened for inclusion. Full-text analysis was done on 144 records, of which 64 described pattern measures of sedentary behaviour (see Figure 1).
Figure 1.
Flow diagram of numbers of studies screened, assessed for eligibility, and included in the review.
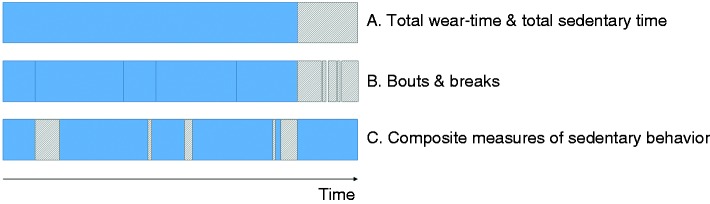
To review the pattern measures of sedentary behaviour from activity sensors, we first need to introduce the general approach of data analysis. We identify three levels of data aggregation to describe sedentary behaviour measures, as shown in Figure 2.
Figure 2.
Three levels of data aggregation for sedentary pattern measures.
Level A. The most basic information level of sedentary behaviour is total sedentary time. To interpret this measure it is best accompanied by the total wear-time. Relevant questions here are: Are results also considering sleep time or only waking time? For how many hours is the behaviour measured during waking time? Does it include evenings, for example watching television?
Level B. The total sedentary time is accumulated in sedentary bouts (periods of sitting and/or lying) which are interrupted by breaks (physically active periods). Outcome measures at this level describe, for example, the number of bouts during waking hours and the mean bout length.
Level C. Finally, we discern composite measures of sedentary behaviour. These measures are composed of bouts or breaks relative to another measure. This can be (a) relative to another sedentary pattern measure, such as total sedentary time; or (b) relative to its timing, describing the temporal aspects of sedentary behaviour; or (c) relative to the order of bouts and breaks, describing the sequential aspects of sedentary behaviour.
Our results will be described following these three levels of data aggregation. For each level we will discuss the general data processing steps, the most reported outcome measures, the various levels of detail, generalisability and complexity and challenges with these measures. Details of the described measures are reported in the detailed results table in the Supplemental Material Additional File 2.
Total sedentary time, total wear-time and sensor type
Total sedentary time was often reported as the sum of all sedentary minutes during the measurement day or as a percentage of wear-time. Sixty-two of the 64 included studies reported total sedentary time; total wear-time was reported by 34 studies.
The 64 studies reporting sedentary pattern measures most often used the Actigraph (n = 43) or ActivPal (n = 14) activity sensor. Other sensors were the Actical, Actiheart, Active stylePro, autonomous sensing unit recorder (ASUR), SenseWear Pro3 Armband, Stepwatch, Promove3D, and research devices. These various sensors are either accelerometry-based sensors or inclinometry-based sensors, see Table 1. These two sensing methods have their own specific limitations in measuring sedentary behaviour. These differences affect all of the outcome measures, making it difficult to compare, for example, the total sedentary time of various studies.
Table 1.
Overview of sensor types, the classification methods of sedentary behaviour and number of studies in which the sensor was reported.
| Sensing method | Output unit | Sensors | Classification of sedentary behaviour | n |
|---|---|---|---|---|
Accelerometry-based sensors 
|
Acceleration intensity | Actigraph | Cut-points: <100 cpm; ≤50 cpm; ≤150 cpm; 8 counts per 10 s.Classification algorithms: ActiLife;22 Soj-1x and Soj-3x by Lyden et al.23 | 43 |
| Actical | <100 cpm; ≤100 cpm<91 cpm; <50 cpm | 5 | ||
| Promove3D | ≤1.660 m·s−2 | 1 | ||
| Activity Intensity | Actiheart | <1.5 MET | 1 | |
| Active stylePro | ≤1.5 MET | 1 | ||
| SenseWear Pro3 (Armband) | ≤1.8 MET | 1 | ||
| Number of steps | Stepwatch | 0 steps | 1 | |
Inclinometry-based sensors 
|
Posture; Inclination | ActivPAL | Sitting; sitting + lying | 14 |
| ASUR | Sitting + lying | 1 | ||
| Research devices | Sitting + lying | 1 | ||
| Actigrapha | Inclination >45°; Sitting by Acti4 classification software | 2 |
cpm: counts per minute; MET: metabolic equivalent of task; n: number of studies reporting the specific sensor.
aThe Actigraph was attached to the upper leg and or trunk.
The most important advantage of accelerometry-based sensors is that they are predominantly worn on the clothes, such as on the waist belt or the wrist, which is convenient for users, can be self-applied, and is therefore a more practical option for large scale, longitudinal studies. These sensors are predominantly applied in protocols measuring sedentary behaviour during waking hours, with a minimum wear-time or minimum valid data of at least 10 h/day (n = 42). The most important disadvantage of accelerometery-based sensors is the vast variety of classification methods applied in the literature, which are listed in Table 1. This means that identical behaviour of sedentary and active time can be classified differently, resulting in differences in total sedentary time and the pattern measures that are derived from this. For example Kim et al.16 found that the performance of the Actigraph sensor for the assessment of sedentary behaviour improved when applying the Sojourn classification method or by applying a cutpoint of <150 counts per minute (cpm). This cutpoint classifies more minutes as being sedentary than the most commonly applied cutpoint (100 cpm) in the literature, likely resulting in more sedentary time.
Inclinometry-based sensors are often attached to the skin of the upper leg with adhesive tape for 24 h per day for several days. The proprietary ActivPAL software that classifies the postures, lying, sitting, standing and walking, is overall more accurate in distinguishing standing and walking from sitting and lying than an accelerometry-based classification.16,17 Nevertheless, distinguishing sitting from lying remains a challenge and is often deduced from the behaviour preceding and succeeding the sitting or lying. This limitation is reflected in the applied definitions of sedentary behaviour when using the ActivPAL. Most of these studies define sedentary behaviour as the posture sitting (n = 6) while others sum sitting and lying (n = 9), see Table 1. This difference in definition can affect the sedentary measures significantly if during waking hours subjects lay down more, for example in patient-groups suffering from fatigue. Moreover, if sleeping at night is included in the sedentary behaviour, subjects will be sedentary for many more hours.18 However, in general only waking hours are analysed (n = 7).
The essential differences in sensing methods are reflected by the findings of articles that studied validity or sensitivity of accelerometry- and inclinometry-based sensors in measuring sedentary behaviour. ActivPAL was found to be more accurate than Actigraph and Actiheart for most measures of sedentary behaviour.16,19–21 Nevertheless, the performance of the Actigraph improved when only studying prolonged sedentary bouts.16 The cutpoint in accelometry-based sensors can be either too low or too high, as Actigraph overestimated and Actiheart underestimated the total sedentary time.21 Nevertheless, the number of breaks was overestimated by both Actigraph and Actiheart.19,21 The sensitivity to behaviour change in an intervention varied with the intervention and behaviour of a population.20 Chastin et al.20 found that ActivPAL was in general more sensitive, but not consistently so for all measures and intervention designs. And they conclude that ‘the instrument of choice should also take into consideration accuracy and validity characteristics' (p.146).20
Bouts
A continuous period of sedentary time is commonly called a (sedentary) bout and the length is most often in minutes. In general, a bout ends when a higher intensity activity is measured or when the posture changes from sitting to standing. However, there are some differences in definitions regarding the minimum duration and allowed minutes of higher intensity activity within a bout. An example of such a restriction is that a bout should last at least two minutes. The definitions applied in the included studies are listed in Supplemental Material Additional File 2. Detailed results can be found in Table 2.
Table 2.
Sedentary pattern measures based on sedentary bouts.
| Pattern measure | Unit | References |
|---|---|---|
| Bout length | Mean | 13,25,28–34 |
| Median | 13,20,26,29,30,33,35,36 | |
| Log mean | 25 | |
| Mean – stratifieda | 37 | |
| Median – stratifieda | 38 | |
| Total sedentary time, accumulated in bouts of specific bout lengths | 39–41 | |
| Longest bout length | 22,33 | |
| Number of bouts | Mean | 16,20,25,28,33,38,42–44 |
| Day-part (morning, afternoon, evening) | 42 | |
| Mean – stratifieda | 16,30--32,34,37,38,41,43,45–49 | |
| Diversity of bout lengths | coefficient of variation | 25 |
| Distribution of bout lengthsb | 20,26,38,50--52 | |
| Burstiness parameter | 53 | |
| Memory parameter | 53 |
aReported for various bout lengths; bvarious measures.
Bouts are the most reported measure of sedentary behaviour that describes a pattern (n = 33). Bouts were reported by direct measures such as the number of bouts, the bout length (its duration) or these measures stratified by bins of bout length of 1, 5, 10, 20, 30 or 60 min. ‘Prolonged bouts’ of lengths of 20 and 30 min24 were reported more frequently, as they have been found to mitigate health effects. For example, Dunstan et al.6 showed that breaking up sedentary time every 20 min can confer health benefits as it lowers postprandial glucose and insulin levels in overweight/obese adults.
A number of measures capture the diversity of bout lengths during a day. The distribution of bout lengths are reported in various measures such as the coefficient of variation (CoV=standard deviation of bout length/mean lognormal transformed bout length) of bout length25 and the cumulative distribution of bout lengths (α).26 The CoV is high when the bout length shows much within subject-variability. A low α indicates a larger proportion of long sedentary bouts. For example Chastin and Granat26 found that ‘the sedentary time of subjects with chronic diseases and sedentary occupation is made up of a larger proportion of long sedentary periods [low α] compared to healthy subjects with active occupation' (p.85). They linked this effect to a low ability to adapt to random challenges during the day regulated by either their occupation or the medical condition, rather than the individual freewill.
Single outcome measures, such as number of bouts and bout lengths, may hinder full understanding of the behaviour pattern. One method to overcome this is by visualization of the outcome measures and their relation.15,27
Breaks
Breaks from sedentary behaviour were reported in 27 articles. They are a relevant part of the sedentary behaviour pattern and we encountered various units in which breaks were reported in our review.
The period between two bouts is called a break. A break in sedentary time was often defined as the moment a data point was above the cut-point for sedentary behaviour or any instance where a sedentary behaviour was followed by a non-sedentary behaviour, such as standing or walking. Most studies classify each interruption in sedentary time as a break, which can be as short as one minute. Sometimes a break should have a minimum duration, for example at least three minutes.24 This difference affects the number of breaks as well as the number of bouts.
The most reported aspects of breaks are the number of breaks (n = 24) and their duration (n = 8). Additionally, break intensities are sometimes reported to discuss the relation between sedentary and specific active behaviour. For example Straker et al.15 found that prolonged sedentary bouts (≥30 min) and short light intensity breaks (0–5 min) were sensitive to differences between small groups, ‘suggesting adequate sensitivity for use in intervention studies’ (p. 662).15 For full details, see Table 3.
Table 3.
Sedentary pattern measures based on breaks from sedentary time.
| Pattern measure | Unit | References |
|---|---|---|
| Break length | Mean | 8,31,35,42,54 |
| Median | 35,55 | |
| Log mean | 20 | |
| Burstiness parameter | 53 | |
| Memory parameter | 53 | |
| Number of breaks | Mean | 8,18,19,21,23,31,39,42,45,49,54,56–67 |
| Median | 55 | |
| Break intensity | Mean | 42,54 |
Composite measures of sedentary behaviour
Finally, we report on the composite measures that we encountered in our review. These measures are composed of bouts or breaks relative to another measure, and provide the most detail of sedentary patterns.
Composite measures – related to total sedentary time
Thirty-two studies reported composite measures, related to total wear time, see Table 4. A common approach in this is reporting the contribution of specific bout lengths to the total sedentary time per day. For example Shiroma et al.38 reported that most of the sedentary time is accumulated in bouts of less than 10 minutes. Reporting the percentage of total sedentary time accumulated in prolonged bouts is also common, for example in bouts of ≥30 min. A more universal measure to report bout length related to total sedentary time is the half-life bout duration (W50), which is the bout length at which 50% of the total sedentary time is accumulated. Chastin et al.20 found that ‘measures of sedentary time accumulation, in particular W50%, were consistently more sensitive than total sedentary time [to changes in sedentary behaviour in intervention studies]’ (p.138). And they recommend that for sedentary behaviour interventions, measures of accumulation should be considered as outcomes.
Table 4.
Composite measures of sedentary behaviour.
| Pattern measure | Unit | References |
|---|---|---|
| Measures related to total wear-time | Percentage of wear-time – stratifieda | 69 |
| Break-rate | 15 | |
| Measures related to total sedentary time | Mean bout length (at specific % of sedentary time) | 70 |
| W50 | 13,20,22,33 | |
| Percentage of sedentary time – stratifieda | 20,24,27,29,30,33,36,43,45,47,55,68,70,71,71–75 | |
| Bout-rate | 20,25,36,42 | |
| Break-rate | 23,24,27,43,45,56,61,66,71,76 | |
| Gini index (G) | 25,26,29,50,58 | |
| Sedentary time per day-part | 77 | |
| Temporal pattern measures | Temporal diversity of sedentary bouts | 58 |
| Detrended fluctuation analysis | 52,68 | |
| (Approximate) entropy | 53,68 | |
| Sequential pattern measures | Fano factor analysis | 52,53 |
| Probability of specific sequences | 52 |
+W50: half-life bout duration.
aReported for various bout lengths.
Bout-rate is a composite measure from total sedentary time and the number of bouts and is also called the fragmentation of bouts (F = number of bouts/total sitting time (min)).25,36 This approximates the break-rate, when one assumes that each bout is followed by a break (which depends on the definition of a break). A higher fragmentation index indicates that the sedentary time is more fragmented with shorter bouts. Blikman et al.25 describe the sedentary pattern as follows: ‘There was a tendency for persons with multiple sclerosis to have a less fragmented pattern of sedentary behaviour’ (p. 26-27). These relative measures have the advantage of being less dependent on total wear-time or total sedentary time, improving the comparability of studies. However, break-rate is a composite measure from total sedentary time and number of breaks and therefore depended on biases in both measures that can have independent sources of variability. Lyden et al. (p.9)17 states that
[…] using a composite measure such as break rate also has limitations. Change in break-rate will indicate sedentary behaviour has changed, but this metric will provide no indication if the change was in total amount of sedentary time, how sedentary time is broken up, or both. When we measure total sedentary time and the number of breaks independently, we can use statistical adjustment to evaluate the independent effects. Break-rate cannot be statistically adjusted for because this would result in variables being entered in the model twice.
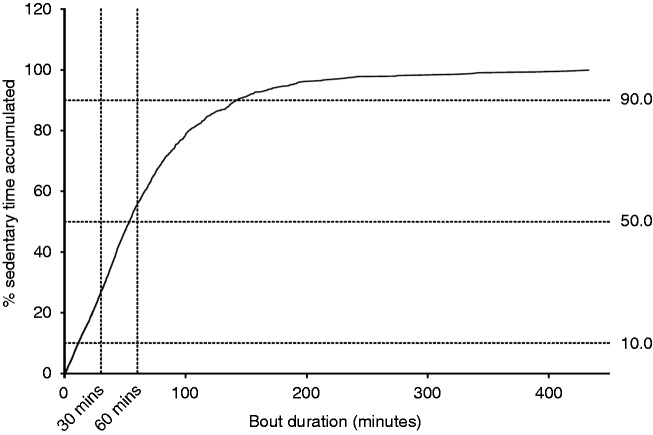
Other studies provided a visual representation of the relation between bout length and total sedentary time, by showing the accumulation graph of total sedentary time for increasing bout length, see for example Figure 3. This graphical representation provides a more intuitive feel for the distribution of bout length and its corresponding sitting pattern during the day than measures such as the bout-rate or fragmentation index. However, to make such a graphical representation suitable for statistical analysis, often specific points on the accumulation graph were analysed, such as: the bout lengths corresponding to 10%, 50% and 90% of total sitting time and the proportion of total sedentary time accumulated in bouts longer than 30 and 60 min.65
Figure 3.
Accumulation of total sedentary time versus increasing bout length. Reprinted with permission from Reid et al.65
One of the solutions to bridge the gap between the accumulation graph and the wish for a single value is the Gini (G) index. This is a composite measure that captures a relation between bout length and accumulation of total sedentary time.26 The G index appeared to be suitable for comparing diagnosis groups and healthy subjects. Chastin and Granat state that ‘The very high G index for chronic fatigue syndrome and low back pain groups suggest that these subjects seem to adopt a boom-bust behaviour with sedentary time mostly made of very long rest periods’ (p. 85-86).26 However, comparing G indexes between studies should be done with great care: the study protocol highly affects the pattern measure. Blikman et al.25 discussed how differences in reported G indexes may appear because of the inclusion of night as sedentary time. Finally, it is important to realise that the G index is a measure of bout length distribution and not of bout length itself. For this reason Ortlieb et al.29 additionally report measures like the mean and median bout length and the percentage of time spent in bouts longer than the median bout length to provide a more complete overview of the sedentary behaviour pattern.
Composite measures – temporal and sequential patterns of sedentary behaviour
Composite measures that describe temporal and sequential patterns were reported in four studies, see Table 4. These measures capture the most detailed aspects of the sedentary behaviour, can predict behaviour and are capable of distinguishing healthy subjects from patient groups.
The temporal diversity of bouts described by Lord et al.58 quantifies how many different lengths of bouts are present in the sedentary pattern and how regularly they are used. This calculation is based on Hill numbers, which are common in literature describing diversity in species. A high value indicates that sedentary bouts are spaced at irregular intervals.
Detrended fluctuation analysis and Fano factor analysis are both methods to describe the randomness of succeeding bout and break lengths. Both methods show in the studies that healthy subjects show a more random sedentary pattern than patient groups. Paraschiv-Ionescu et al.,52 for example, found a larger value of fluctuation in the sedentary pattern of chronic pain patients. They also suggested that ‘activity-to-rest transitions are randomly spread over time with pain patients as opposed to organised in healthy people’ (p.7). This bursty nature of (healthy) human behaviour was further analysed in a later publication.53
Cavanaugh et al.68 used entropy rate and approximate entropy to quantify the amount of uncertainty associated with whether step activity was recorded in any given minute. ‘Greater uncertainty implied that the ordering of active versus inactive minutes contained a greater amount of information, and, therefore, greater complexity' (p. 199).68 Cavanaugh et al. showed that the successive activity-rest pattern recorded from highly active participants was more complex than of less active participants. In other words: there was relatively more uncertainty about whether or not activity occurred in any given minute. The behaviour is less predictable.
A similar approach for predicting sedentary behaviour was described by Paraschiv-Ionescu et al.52 The symbolic sequence of successive rest-activity-rest periods is a binary code of ones and zeros for each break depending on the length of the preceding and successive bout. Paraschiv-Ionescu et al.52 found that the probability of ‘long activity followed by short rest’ was significantly greater for the healthy controls than for those in the chronic pain group.
Discussion
This review has shown that objective sedentary measures can be grouped into simple and complex measures of sedentary time accumulation during the day. These measures serve different goals, varying from a quick overview of the total behaviour to in-depth analysis of sedentary time accumulation and prediction of behaviour. The answer as to which measures are most suitable to report, is therefore strongly dependent on the research question. The measures of sedentary behaviour patterns that we identified in the literature are difficult, if not impossible, to compare, making the current body of knowledge fragmented, contradictory and difficult to build upon. We suggest it is appropriate to always report total wear-time, total sedentary time, number of bouts and one of the measures describing the diversity of bout lengths in the sedentary behaviour. The W50 measure seems very suitable here, as it is sensitive to changes in behaviour and is relatively easy to calculate. Additionally, we suggest it is necessary to report measurement conditions (the sensor used and measurement protocol) and the data processing steps (valid days, non-wear, classification method and applied definitions of bouts and breaks).
Reporting these measures does not solve the problem of incomparability of different studies. We identified various sources of errors, especially in the first steps of data processing, that can have significant effects on the results. The sensing method – accelerometry-based versus inclinometry-based sensors – and the classification method, have the strongest effect on the measured sedentary behaviour patterns. The succeeding data processing steps can strongly affect the results, such as the inclusion of sleep in the sedentary behaviour. Finally, some measures have multiple sources of biases. For example, a change in the break-rate does not clarify which aspect of the sedentary behaviour changed: the total sedentary time or the number of breaks. Most importantly, one should always consider the whole picture of sensor, protocol, classification, data processing and sensitivity of the outcome measure.
Limitations
We have seen that because sedentary behaviour pattern analysis is a new and fast emerging field of research, relevant pattern measures find their origin in other disciplines. Our search terms may have not been comprehensive, omitting relevant sedentary pattern measures from other domains. However, we have checked all references in the records and did not find any evidence in such a direction. Related to this, the various fields of research (accelerometry and inclinometry) are, although complementary to each other regarding insights in sedentary behaviour analysis, also diverse in terminology. This makes it difficult to fully capture both fields in one search strategy. To fully capture all possible publications, we have learned that this field requires a very extensive search with a very large and diverse range of search terms.
The rapid increase of commercial activity trackers such as the Fitbit, are not reflected in this study. They are not commonly applied in current scientific research. However, we do expect them to become adopted by the field both as an applied sensing method as well as valuable data source resulting from the consumer, quantified-self domain. As free-living, self-tracking of behaviour is becoming more and more common, this rapid rise of activity trackers demonstrates the time-sensitivity of reviews such as these. We therefore encourage the community to keep an eye on new developments and to, perhaps, replicate this review at some point in the future.
Conclusions
Sedentary behaviour research is a fast emerging field of study. Many sedentary pattern measures already show how they developed towards more robust, general measures and this development will probably continue in the upcoming years as has happened to physical activity measures.
This review has shown that objective sedentary measures described in literature are strongly dependent on (a) the sensing method (accelerometry-based or inclinometry-based sensors), (b) the method of classifying sedentary behaviour, (c) the experimental and data cleaning protocol and (d) the applied definitions of bouts and breaks. Differences in one or more of these steps can make it difficult or even impossible to compare reported sedentary pattern measures.
Nevertheless, the sedentary behaviour patterns studied in this review show us that the sedentary pattern can be best described by providing both general outcome measures and a measure of bout length distribution.
Supplemental Material
Supplemental material, DHJ905418 Supplemental Material1 for Pattern measures of sedentary behaviour in adults: A literature review by Simone T Boerema, Lex van Velsen, Miriam MR Vollenbroek and Hermie J Hermens in Digital Health
Supplemental material, DHJ905418 Supplemental Material2 for Pattern measures of sedentary behaviour in adults: A literature review by Simone T Boerema, Lex van Velsen, Miriam MR Vollenbroek and Hermie J Hermens in Digital Health
Acknowledgements
Icons were created by Simone Boerema based on Freepik from www.flaticon.com.
Contributorship
The search strategy was developed by two of the authors (STB and LvV). Two of the authors (STB and LvV) initially screened identified studies. STB analysed and aggregated all results and was major contributor in writing the manuscript. LvV, HJH and MMRV provided guidance on data analysis and aggregation. All authors have approved the final manuscript.
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
Not applicable.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work has been funded by two projects. First, the Platform for Ergonomic and motivating, ICT-based Age-friendly woRkpLaces (PEARL) project, funded by the European Ambient Assisted Living Joint Programme and the National Funding Agencies from Austria, Denmark, Germany, Netherlands, Romania, and Switzerland (PEARL; AAL-2013-6-091). And second, the Grey but Mobile project within the Creative Industry Scientific Programme (CRISP). CRISP is supported by the Dutch Ministry of Education, Culture and Science.
Guarantor
LV.
ORCID iDs
Simone T Boerema https://orcid.org/0000-0002-4760-3007
Lex van Velsen https://orcid.org/0000-0003-0599-8706
Peer review
This manuscript is reviewed by Philippa M Dall, Glasgow Caledonian University.
Supplemental material
Supplemental material for this article is available online.
References
- 1.Dunstan DW, Howard B, Healy GNet al. Too much sitting – a health hazard. Diabetes Res Clin Pract 2012; 97: 368–376. [DOI] [PubMed] [Google Scholar]
- 2.Chau JY, Grunseit AC, Chey Tet al. Daily sitting time and all-cause mortality: A meta-analysis. PLoS One 2013; 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van der Ploeg HP, Chey T, Korda RJet al. Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch Intern Med 2012; 172: 494–500. [DOI] [PubMed] [Google Scholar]
- 4.Biswas A, Oh PI, Faulkner GEet al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: A systematic review and meta-analysis. Ann Intern Med 2015; 162: 123. [DOI] [PubMed] [Google Scholar]
- 5.Tremblay MS, Colley RC, Saunders TJet al. Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab 2010; 35: 725–740. [DOI] [PubMed] [Google Scholar]
- 6.Owen N, Healy GN, Matthews CEet al. Too much sitting: The population health science of sedentary behavior. Exerc Sport Sci Rev 2010; 38: 105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oxford Dictionaries. Oxford dictionary of English. 3rd ed. Oxford: Oxford University Press, 2010. [Google Scholar]
- 8.Healy GN, Matthews CE, Dunstan DWet al. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 200306. Eur Heart J 2011; 32: 590–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dunstan DW, Kingwell BA, Larsen Ret al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care 2012; 35: 976–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chastin SFM, Dontje ML, Skelton DAet al. Systematic comparative validation of self-report measures of sedentary time against an objective measure of postural sitting (activPAL). Int J Behav Nutr Phys Act 2018; 15: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tremblay M. Letter to the editor: Standardized use of the terms ‘sedentary’ and ‘sedentary behaviours'. Appl Physiol Nutr Metab 2012; 37: 540–542. [DOI] [PubMed] [Google Scholar]
- 12.Haskell WL, Lee I-M, Pate RRet al. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc 2007; 39: 1423–1434. [DOI] [PubMed] [Google Scholar]
- 13.Boerema ST, Essink GB, Tönis TMet al. Sedentary behaviour profiling of office workers: A sensitivity analysis of sedentary cut-points. Sensors 2016; 16: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sellers C, Dall P, Grant Met al. Validity and reliability of the activPAL3 for measuring posture and stepping in adults and young people. Gait Posture 2016; 43: 42–47. [DOI] [PubMed] [Google Scholar]
- 15.Straker L, Campbell A, Mathiassen SEet al. Capturing the pattern of physical activity and sedentary behavior: Exposure variation analysis of accelerometer data. J Phys Act Health 2014; 11: 614–625. [DOI] [PubMed] [Google Scholar]
- 16.Kim Y, Barry VW and, Kang M. Validation of the ActiGraph GT3X and activPAL accelerometers for the assessment of sedentary behavior. Meas Phys Educ Exerc Sci 2015; 19: 125–137. [Google Scholar]
- 17.Lyden K, Kozey Keadle SL, Staudenmayer JWet al. Validity of two wearable monitors to estimate breaks from sedentary time. Med Sci Sports Exerc 2012; 44: 2243–2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scheers T, Philippaerts R and, Lefevre J. Variability in physical activity patterns as measured by the SenseWear Armband: How many days are needed? Eur J Appl Physiol 2012; 112: 1653–1662. [DOI] [PubMed] [Google Scholar]
- 19.Barreira TV, Zderic TW, Schuna JMet al. Free-living activity counts-derived breaks in sedentary time: Are they real transitions from sitting to standing? Gait Posture 2015; 42: 70–72. [DOI] [PubMed] [Google Scholar]
- 20.Chastin SFM, Winkler EAH, Eakin EGet al. Sensitivity to change of objectively-derived measures of sedentary behavior. Meas Phys Educ Exerc Sci 2015; 19: 138–147. [Google Scholar]
- 21.Júdice PB, Santos DA, Hamilton MTet al. Validity of GT3X and Actiheart to estimate sedentary time and breaks using ActivPAL as the reference in free-living conditions. Gait Posture 2015; 41: 917–922. [DOI] [PubMed] [Google Scholar]
- 22.Pettapiece-Phillips R, Kotlyar M, Chehade Ret al. Uninterrupted sedentary behavior downregulates BRCA1 gene expression. Cancer Prev Res (Phila Pa ) 2016; 9: 83–88. [DOI] [PubMed] [Google Scholar]
- 23.Lyden K, Keadle SK, Staudenmayer Jet al. A method to estimate free-living active and sedentary behavior from an accelerometer. Med Sci Sports Exerc 2014; 46: 386–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parry S, Straker L, Gilson NDet al. Participatory workplace interventions can reduce sedentary time for office workers – a randomised controlled trial. PLoS One 2013; 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blikman LJ, Van Meeteren J, Horemans HLet al. Is physical behavior affected in fatigued persons with multiple sclerosis? Arch Phys Med Rehabil 2015; 96: 24–29. [DOI] [PubMed] [Google Scholar]
- 26.Chastin SFM, Granat MH. Methods for objective measure, quantification and analysis of sedentary behaviour and inactivity. Gait Posture 2010; 31: 82–86. [DOI] [PubMed] [Google Scholar]
- 27.Parry S, Straker L. The contribution of office work to sedentary behaviour associated risk. BMC Public Health 2013; 13: 296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chastin SFM, Mandrichenko O, Helbostadt JLet al. Associations between objectively-measured sedentary behaviour and physical activity with bone mineral density in adults and older adults, the NHANES study. Bone 2014; 64: 254–262. [DOI] [PubMed] [Google Scholar]
- 29.Ortlieb S, Dias A, Gorzelniak Let al. Exploring patterns of accelerometry-assessed physical activity in elderly people. Int J Behav Nutr Phys Act 2014; 11: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Diaz KM, Howard VJ, Hutto Bet al. Patterns of sedentary behavior in US middle-age and older adults: The REGARDS Study. Med Sci Sports Exerc 2016; 48: 430–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ezeugwu V, Klaren RE, Hubbard EAet al. Mobility disability and the pattern of accelerometer-derived sedentary and physical activity behaviors in people with multiple sclerosis. Prev Med Rep 2015; 2: 241–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Judice PB, Silva AM, Sardinha LB. Sedentary bout durations are associated with abdominal obesity in older adults. J Nutr Health Aging 2015; 19: 798–804. [DOI] [PubMed] [Google Scholar]
- 33.Bellettiere J, Carlson JA, Rosenberg Det al. Gender and age differences in hourly and daily patterns of sedentary time in older adults living in retirement communities. PLoS One 2015; 10: e0136161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van der Berg JD, Stehouwer CDA, Bosma Het al. Associations of total amount and patterns of sedentary behaviour with type 2 diabetes and the metabolic syndrome: The Maastricht Study. Diabetologia 2016; 59: 709–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Manns P, Ezeugwu V, Armijo-Olivo Set al. Accelerometer-derived pattern of sedentary and physical activity time in persons with mobility disability: National Health and Nutrition Examination Survey 2003 to 2006. J Am Geriatr Soc 2015; 63: 1314–1323. [DOI] [PubMed] [Google Scholar]
- 36.Tieges Z, Mead G, Allerhand Met al. Sedentary behavior in the first year after stroke: A longitudinal cohort study with objective measures. Arch Phys Med Rehabil 2015; 96: 15–23. [DOI] [PubMed] [Google Scholar]
- 37.Barber SE, Forster A, Birch KM. Levels and patterns of daily physical activity and sedentary behavior measured objectively in older care home residents in the United Kingdom. J Aging Phys Act 2015; 23: 133–143. [DOI] [PubMed] [Google Scholar]
- 38.Shiroma EJ, Freedson PS, Trost SGet al. Patterns of accelerometer-assessed sedentary behavior in older women. Med Sci Sports Exerc 2013; 45: 102–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carson V, Wong SL, Winkler Eet al. Patterns of sedentary time and cardiometabolic risk among Canadian adults. Prev Med 2014; 65: 23–27. [DOI] [PubMed] [Google Scholar]
- 40.Gupta N, Heiden M, Aadahl Met al. What is the effect on obesity indicators from replacing prolonged sedentary time with brief sedentary bouts, standing and different types of physical activity during working days? A cross-sectional accelerometer-based study among blue-collar workers. PLoS One 2016; 11: e0154935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Helgadóttir B, Forsell Y, Ekblom O. Physical activity patterns of people affected by depressive and anxiety disorders as measured by accelerometers: A cross-sectional study. PLoS One 2015; 10: e0115894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baruth M, Sharpe PA, Hutto Bet al. Patterns of sedentary behavior in overweight and obese women. Ethn Dis 2013; 23: 336–342. [PMC free article] [PubMed] [Google Scholar]
- 43.Jefferis BJ, Sartini C, Shiroma Eet al. Duration and breaks in sedentary behaviour: Accelerometer data from 1566 community-dwelling older men (British Regional Heart Study). Br J Sports Med 2015; 49: 1591–1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Leask CF, Harvey JA, Skelton DAet al. Exploring the context of sedentary behaviour in older adults (what, where, why, when and with whom). Eur Rev Aging Phys Act 2015; 12: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.García-Hermoso A, Notario-Pacheco B, Recio-Rodríguez JIet al. Sedentary behaviour patterns and arterial stiffness in a Spanish adult population – the EVIDENT trial. Atherosclerosis 2015; 243: 516–522. [DOI] [PubMed] [Google Scholar]
- 46.Kim Y, Welk GJ, Braun SIet al. Extracting objective estimates of sedentary behavior from accelerometer data: Measurement considerations for surveillance and research applications. PLoS One 2015; 10: e0118078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lynch BM, Boyle T, Winkler Eet al. Patterns and correlates of accelerometer-assessed physical activity and sedentary time among colon cancer survivors. Cancer Causes Control 2016; 27: 59–68. [DOI] [PubMed] [Google Scholar]
- 48.Prince SA, Blanchard CM, Grace SLet al. Objectively-measured sedentary time and its association with markers of cardiometabolic health and fitness among cardiac rehabilitation graduates. Eur J Prev Cardiol 2015; 23: 818–825. [DOI] [PubMed] [Google Scholar]
- 49.Prioreschi A, Makda MA, Tikly Met al. Habitual physical activity, sedentary behaviour and bone health in rheumatoid arthritis. Int J Sports Med 2015; 36: 1021–1026. [DOI] [PubMed] [Google Scholar]
- 50.Chastin SF, Baker K, Jones Det al. The pattern of habitual sedentary behavior is different in advanced Parkinson’s disease. Mov Disord 2010; 25: 2114–2120. [DOI] [PubMed] [Google Scholar]
- 51.Sartini C, Wannamethee SG, Iliffe Set al. Diurnal patterns of objectively measured physical activity and sedentary behaviour in older men. BMC Public Health 2015; 15: 609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Paraschiv-Ionescu A, Buchser E, Rutschmann Bet al. Nonlinear analysis of human physical activity patterns in health and disease. Phys Rev E - Stat Nonlinear Soft Matter Phys 2008; 77: 021913. [DOI] [PubMed] [Google Scholar]
- 53.Paraschiv-Ionescu A, Perruchoud C, Buchser Eet al. Multidimensional analysis of human activity patterns in health and disease. In: Hanza MH (ed.) Proceedings of the 2nd IASTED International Conference on Telehealth and Assistive Technology, TAT 2009 ACTA Press: Cambridge, MA, 2009. pp.31–36.
- 54.Healy GN, Dunstan DW, Salmon Jet al. Breaks in sedentary time – beneficial associations with metabolic risk. Diabetes Care 2008; 31: 661–666. [DOI] [PubMed] [Google Scholar]
- 55.Chapman JJ, Fraser SJ, Brown WJet al. Physical activity and sedentary behaviour of adults with mental illness. J Sci Med Sport 2016; 19: 579--584. [DOI] [PubMed]
- 56.Cooper AR, Sebire S, Montgomery AAet al. Sedentary time, breaks in sedentary time and metabolic variables in people with newly diagnosed type 2 diabetes. Diabetologia 2012; 55:589–599. [DOI] [PubMed] [Google Scholar]
- 57.Gardiner PA, Eakin EG, Healy GNet al. Feasibility of reducing older adults’ sedentary time. Am J Prev Med 2011; 41: 174–177. [DOI] [PubMed] [Google Scholar]
- 58.Lord S, Chastin SFM, McInnes Let al. Exploring patterns of daily physical and sedentary behaviour in community-dwelling older adults. Age Ageing 2011; 40: 205–210. [DOI] [PubMed] [Google Scholar]
- 59.Maddocks M, Wilcock A. Exploring physical activity level in patients with thoracic cancer: Implications for use as an outcome measure. Support Care Cancer 2012; 20: 1113–1116. [DOI] [PubMed] [Google Scholar]
- 60.Chen T., Narazaki K., Haeuchi Yet al. Associations of sedentary time and breaks in sedentary time with disability in instrumental activities of daily living in community-dwelling older adults. J Phys Act Health 2016; 13: 303–39. [DOI] [PubMed] [Google Scholar]
- 61.Claridge EA, McPhee PG, Timmons BWet al. Quantification of physical activity and sedentary time in adults with cerebral palsy. Med Sci Sports Exerc 2015; 47: 1719–26. [DOI] [PubMed] [Google Scholar]
- 62.Davis MG, Fox KR, Stathi Aet al. Objectively measured sedentary time and its association with physical function in older adults. J Aging Phys Act 2014; 22: 474–481. [DOI] [PubMed] [Google Scholar]
- 63.Fanning J, Porter G, Awick EAet al. Effects of a DVD-delivered exercise program on patterns of sedentary behavior in older adults: A randomized controlled trial. Prev Med Rep 2016; 3: 238–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gennuso KP, Gangnon RE, Thraen-Borowski KMet al. Dose-response relationships between sedentary behaviour and the metabolic syndrome and its components. Diabetologia 2014; 58: 485–492. [DOI] [PubMed] [Google Scholar]
- 65.Reid N, Eakin E, Henwood Tet al. Objectively measured activity patterns among adults in residential aged care. Int J Environ Res Public Health 2013; 10: 6783–6798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sardinha LB, Ekelund U, dos Santos Let al. Breaking-up sedentary time is associated with impairment in activities of daily living. Exp Gerontol 2015; 72: 57–62. [DOI] [PubMed] [Google Scholar]
- 67.Sardinha LB, Santos DA, Silva AMet al. Breaking-up sedentary time is associated with physical function in older adults. J Gerontol - Series A 2015; 70: 119–124. [DOI] [PubMed] [Google Scholar]
- 68.Cavanaugh JT, Kochi N, Stergiou N. Nonlinear analysis of ambulatory activity patterns in community-dwelling older adults. J Gerontol - Series A 2010; 65: 197–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hallman DM, Mathiassen SE, Gupta Net al. Differences between work and leisure in temporal patterns of objectively measured physical activity among blue-collar workers. BMC Public Health 2015; 15: 976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Reid RER, Carver TE, Andersen KMet al. Physical activity and sedentary behavior in bariatric patients long-term post-surgery. Obes Surg 2015; 25: 1073–1077. [DOI] [PubMed] [Google Scholar]
- 71.Shiroma EJ, Freedson PS, Trost SGet al. Patterns of accelerometer-assessed sedentary behavior in older women. JAMA 2013; 310: 2562–2563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Falconer CL, Page AS, Andrews RCet al. The pote impact of displacing sedentary time in adults with type 2 diabetes. Med Sci Sports Exerc 2015; 47: 2070–2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.García-Hermoso A, Martínez-Vizcaíno V, Recio-Rodríguez JIet al. Sedentary behaviour patterns and carotid intima-media thickness in Spanish healthy adult population. Atherosclerosis 2015; 239: 571–576. [DOI] [PubMed] [Google Scholar]
- 74.Jefferis BJ, Parsons TJ, Sartini Cet al. Does duration of physical activity bouts matter for adiposity and metabolic syndrome? A cross-sectional study of older British men. Int J Behav Nutr Phys Act 2016; 13: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Van Dommelen P, Coffeng JK, Van Der Ploeg HPet al . Objectively measured total and occupational sedentary time in three work settings. PLoS One 2016; 11: e0149951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Spinney R, Smith L, Ucci Met al. Indoor tracking to understand physical activity and sedentary behaviour: Exploratory study in UK office buildings. PLoS One 2015; 10: e0127688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Van Cauwenberg J, Van Holle V, De Bourdeaudhuij Iet al. Diurnal patterns and correlates of older adults’ sedentary behavior. PLoS One 2015; 10: e0133175. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, DHJ905418 Supplemental Material1 for Pattern measures of sedentary behaviour in adults: A literature review by Simone T Boerema, Lex van Velsen, Miriam MR Vollenbroek and Hermie J Hermens in Digital Health
Supplemental material, DHJ905418 Supplemental Material2 for Pattern measures of sedentary behaviour in adults: A literature review by Simone T Boerema, Lex van Velsen, Miriam MR Vollenbroek and Hermie J Hermens in Digital Health