Highlights
-
•
40% of patients disagree that being overweight is a risk factor for cancer.
-
•
85% of patients would prefer multimodal weight loss approach to cancer care.
-
•
82.1% of patients would consider medical or surgical approaches to treatment.
Keywords: Obesity, Endometrial cancer, Metabolic surgery
Abstract
Obesity is the greatest risk factor for endometrial cancer. There is often a lack of recognition amongst patients about this risk. Evidence for weight-loss in the management of endometrial cancer is emerging. This was questionnaire-based study, that examined opinions and attitudes of patients with endometrial cancer and obesity towards obesity as a risk factor for cancer as well as examining their willingness to engage in weight loss interventions as an alternative treatment to endometrial cancer. This survey was conducted in a gynaeoncology out-patient department in Ireland. A total of 45/50 (90%) of questionnaires were completed. The majority of the patients questioned (86.7%; 39/45) agreed that obesity is a disease. Just over half of the cohort (53.3%; 24/45) believed that obesity can cause cancer. Over one-third, 39.9% (18/45) either disagreed or strongly disagreed that obesity is a risk factor for endometrial cancer while 35.5% (16/45) agreed or strongly agreed. Two-thirds (66.6%; 30/45) knew that the greatest amount of weight could be lost through metabolic surgery. Over three-quarters (82.1%; 37/45) of patients surveyed would be willing to engage in a combination of treatments in order to achieve weight-loss should it be proven to have a role in the management of endometrial cancer. This study demonstrates a need for patient education regarding the strong relationship between obesity and endometrial cancer risk. Patients are willing to consider weight loss interventions if they were proven to be as safe and effective as pelvic surgery in the management of endometrial cancer.
1. Introduction
Endometrial cancer is the most common cancer of the female genital tract and the fourth commonest cancer in women overall in the developed world (Torre et al., 2015). Obesity (BMI > 30 kg/m2) is the greatest risk factor for endometrial cancer and as a disease is reaching epidemic proportions (Mechanick et al., 2012). There are three main challenges that hinder the ability to treat obesity induced endometrial cancer, which include the lack of recognition by patients that obesity is a disease, lack of realisation that obesity contributes to cancer risk and the knowledge gap that exists amongst patients regarding the potential adjunctive treatments available (Mawardi et al., 2019). Thus, the question arises as to whether obesity is really perceived by patients as a risk factor for cancer?
Patient ‘perception’ is a significant determinant in how a population behaves and responds to health promotion (Visscher et al., 2005). Obese patients who seek out treatment for their disease are more likely to understand the impact of obesity on their health and are more likely to realise the social burden that obesity poses (Derksen et al., 2012).
Up to 90% of patients with endometrial cancer are overweight (BMI 25–30 kg/m2) or obese (Crosbie et al., 2012). How many of these patients consider their weight as a cause or underlying risk for their disease? Furthermore, recent evidence suggests that many healthcare professionals do not recognise obesity as a disease (Derksen et al., 2012) and find it difficult to initiate conversations with patients regarding their obesity and its management. Some healthcare professionals feel that obesity is an uncomfortable topic to raise with their patients, whilst others cite time constraints as the reason not to broach the subject (Blackburn et al., 2015).
With a growing body of experimental and clinical evidence suggesting that weight loss has the ability to greatly reduce risk and reverse pathology in obesity-related endometrial cancer, it is imperative that clinicians and patients alike increase their understanding of the various treatment options at their disposal (MacKintosh et al., 2019). Lifestyle modifications including exercise programs and supervised weight loss programs can achieve 4–6% loss of total body weight over 2–4 years, while a more impressive total body weight loss of 7–10% is achievable with the use of weight loss medications (Ryan et al., 2010). Metabolic surgery produces the most significant and sustainable results, with a 25–35% total body weight loss achievable over decades with both laparoscopic vertical sleeve gastrectomy and gastric bypass surgery (MacKintosh et al., 2019).
In this study, we sought to determine the opinions and attitudes of patients towards obesity as a disease and a risk factor for cancer in a population with obesity and endometrial cancer. We also sought to determine their knowledge base regarding various weight loss treatments and their willingness to engage in these treatments rather than the conventional treatment for endometrial cancer.
2. Methods
This questionnaire-based study examined opinions and attitudes of patients with endometrial cancer and obesity towards obesity as a disease and a risk factor for cancer. We also examined their knowledge of the efficacy of various weight loss treatments and their willingness to engage in these treatments in order to potentially treat endometrial cancer.
2.1. Study setting
This study was conducted in the Gynaecological Oncology outpatient department of the Mater Misericordiae University Hospital, Dublin, Ireland. This study was granted full ethical approval by the Medical Research and Ethics Committee at the Mater Misericordiae Hospital, Dublin, Ireland: protocol 1, December 2017 - Institutional Review Board Reference: 1/378/1978. Patients provided written informed consent before completing the questionnaire.
Inclusion Criteria
-
•
Current or previous history of endometrial cancer (within the last five years)
-
•
BMI > 30 kg/m2
-
•
Over 18 years of age
-
•
Patient must be capable to give consent and not require the use of an interpreter
Exclusion Criteria
-
•
BMI < 30 kg/m2
-
•
Unable to provide informed consent or complete questionnaires
-
•
No history/diagnosis of endometrial cancer
2.2. Questionnaire
As no validated questionnaires existed on this topic, a novel, 8 item questionnaire was developed to explore patient understanding about the relationship between obesity and endometrial cancer and their willingness to engage in weight loss treatments as part of the management for endometrial cancer if these treatments were proven to be safe and effective(Appendix A). This consisted of free-text, binomial, multi-choice and 5-point Likert scale responses. The first three questions were designed to ascertain the patient’s understanding of obesity as a disease and determine whether patients felt obesity was a risk factor for endometrial cancer. Questions 4–6 assessed the patients understanding of the efficacy of different weight loss interventions. Questions 7 and 8 assessed the patients’ willingness to consider diet, medication and metabolic surgery as an alternative to hysterectomy in the treatment of endometrial cancer.
Patients who met the inclusion criteria were approached consecutively in the gynaeoncology outpatient clinic and the study was conducted over a three month period.
3. Results
A total of 50 questionnaires were distributed with 45 complete questionnaires returned for analysis (45/50; 90%). The questionnaire started by determining whether patients considered obesity to be a disease or not. The vast majority of the patients questioned (86.7%; 39/45) agreed that obesity is a disease (Fig. 1A). However, just over half of the cohort (53.3%; 24/45) believed that obesity can cause cancer (Fig. 1B). This opinion was divided further when patients were asked about their view of obesity as a risk factor for endometrial cancer specifically, with 39.9% (18/45) either disagreeing or strongly disagreeing with the statement while 35.5% (16/45) agreed or strongly agreed. Twenty-four percent (11/45) were neutral with regards to this question (Fig. 1C).
Fig. 1.
Patient understanding of Obesity as a disease and risk factor. (A) The vast majority of patients questioned (86.7%) agreed that obesity is considered to be a disease. (B) However just over half of the patients (53.3%) felt that obesity had the ability to increase cancer risk. (C) When asked about how they felt about increased weight being a risk factor for developing endometrial cancer 40% (18/45) either disagreed or strongly disagreed that being overweight was a risk factor for obesity while 35.5% (16/45) agreed or strongly agreed that being overweight could lead to an increased risk of endometrial cancer. Weight converter: One stone = 14 lb or 6.3 kg.
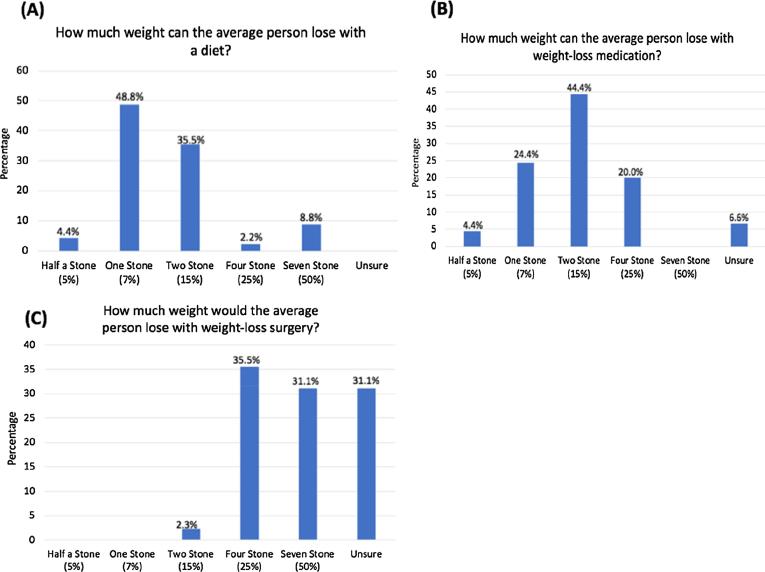
Knowledge of the extent of weight loss possible with each approach was assessed within our cohort (Fig. 2). When asked what the expected weight loss could be expected from engaging in a diet, 48.8% (22/45) of respondents believed that one-stone (6.3 kg) weight-loss could be possible with a further 35.5%(16/45) believing two stone (12.7 kg) weight loss to be possible with the use of a dietary approach (Fig. 2A). When the same question was asked with respect to medical weight loss interventions, there was a belief that a greater amount of weight loss could be achieved with this approach, as 64.4% (29/45) of patients felt the expected weight loss would be ≥2 stone (12.7 kg) with medication (Fig. 2B). Similarly when asked about the potential weight-loss attainable by metabolic surgery, there was a belief that this was the means by which the greatest weight loss could be achieved, as 66.6% (30/45) felt the expected weight loss would be ≥4 stone (25.4 kg), however 31.1% (14/45) were unsure about the percentage weight loss achievable from metabolic surgery (Fig. 2C).
Fig. 2.
Patient knowledge of efficacy of weight loss interventions. (A) Almost half of the patients questioned (44.4%; 20/45) felt that 15% body weight could be lost with the use of weight-loss medication with one-fifth (20%; 9/45) believing 25% body weight could be shed with a medical approach. (B) Just under half (48.8%; 22/45) believed that 7% body weight could be lost with the use of diet alone with over one-third (35.5%; 16/45) feeling 15% weight loss was achievable with diet alone. (C) Two-thirds patients (66.6%; 30/45) and believed that at least 25% body weight could be lost with bariatric. Weight converter: One stone = 14 lb or 6.3 kg.
Weight loss has the potential to reverse endometrial pathology in certain patients (MacKintosh et al., 2019). However, would there be a willingness amongst patients to engage in medical or surgical weight-loss treatments as an alternative to the conventional hysterectomy should they be found to be safe and effective? The final part of this study aimed to assess whether patients with endometrial cancer and obesity would consider ‘if diet, medication and weight loss surgery were proven to be just as effective and as safe as a hysterectomy for the treatment of their endometrial cancer’ which option they would prefer? The majority 84.4% (38/45) of patients preferred a multimodal weight loss intervention compared to conventional surgical treatment (Fig. 3A). We also asked ‘if 25% weight-loss is proven as a treatment for endometrial cancer, what weight loss treatments would you be willing to engage with, in order to treat your cancer?’ Over three-quarters (82.1%; 37/45) of patients surveyed would be willing to engage in a treatment combination in order to achieve this weight-loss; with the majority choosing diet and medication (46.6%) while 35.5% would consider metabolic surgery (Fig. 3B).
Fig. 3.
Patient willingness for alternatives to pelvic surgery in the management of endometrial cancer. (A) The majority of patients questioned (84%; 38/45) would have a preference for weight-loss treatment over hysterectomy if proven to be equally as effective in the treatment of endometrial cancer. (B) Over one-third (35.5%; 16/45) of patients would be willing to engage in a combination of diet, medication and weight-loss surgery in order to lose the weight required to treat endometrial cancer. Weight converter: One stone = 14 lb or 6.3 kg.
4. Discussion
It is predicted that the incidence of endometrial cancer is likely to increase by 55% in the United States by 2030, owing in large part, to the exponential increase in the incidence of obesity (Sheikh et al., 2014). The understanding and perception amongst patients surrounding obesity as a disease and as a potential risk factor for cancer is variable (Crosbie et al., 2012, Fader et al., 2009) and is poorly documented in women with endometrial cancer.
We found that the vast majority (86.7%; 39/45) of obese women with endometrial cancer classified obesity as a disease, however this did not translate into understanding obesity as a cancer risk factor with only 53.3% (24/45) recognising the link between obesity and carcinogenesis(Fig. 1). Patient’s perception is incredibly important when it comes to treatment of disease and health promotion irrespective of the medical condition involved (Visscher et al., 2005). Patients who perceive a disease as severe enough to cause cancer are more willing to engage in lifestyle modifications than patients who aren’t aware of the link (Visscher et al., 2005, Rosenstock, 1966). Over one-third (39.9%:18/45) of patients questioned disagreed with the idea that being overweight could be a risk factor for the cancer they had developed. This finding is concordant with recent findings in a study by Sekhon et al. where only 39% (19/45) of endometrial cancer patients linked obesity to endometrial cancer risk and concluded that there was a general lack of understanding amongst endometrial cancer patients about risk factors for their cancer (Sekhon et al., 2019).
Patients with obesity and endometrial cancer experience increased surgical morbidity and are more likely to die from a non-cancer related illness, such as cardiovascular disease, than their non-obese counterparts (Orekoya et al., 2016). Furthermore, the incidence of endometrial cancer in premenopausal women is also increasing due to the rising obesity rates amongst this population. There is a growing need for an alternative approach to the management of endometrial cancer in order to avoid the increased morbidity associated with hysterectomy in obese patients but also to provide fertility sparing options where they’re desired.
The evidence supporting weight-loss as a potential treatment for endometrial cancer remains sparse. A recent Cochrane review concluded that there was currently insufficient evidence to suggest that lifestyle and dietary intervention has any impact on the survival or quality of life in patients with endometrial cancer (Kitson et al., 2018). This was however, based on low-quality evidence and they concluded that adequately powered RCTs to evaluate medical and surgical interventions for weight loss in the context of endometrial cancer are greatly needed. This study needs to be expanded to include metabolic surgery and repeated in larger cohorts on an international setting.
The patients we questioned recognised that only moderate weight loss results can be achieved by diet alone and that more substantial results can be achieved with medical or surgical intervention (Fig. 2), with metabolic surgery producing the most significant weight loss results. A combination of all three weight-loss approaches could play a role, should weight-loss management become an alternative or adjunct to the management of endometrial cancer. From our study we noted patients generally overestimated the weight loss from these management strategies, but correctly identified that surgery would produce the greatest weight loss, followed by medication and diet.
Perhaps the most important finding from this questionnaire was that 84.5% (38/45) of patients questioned would prefer a combined weight loss approach over conventional hysterectomy if weight loss was proven to be equally efficacious in the treatment of endometrial cancer. This is a critical finding, demonstrating that weight loss treatments are considered an acceptable option to patients. Equally important was the finding that 82.1% (37/45) of patients would be willing to use medical or surgical approaches, not just conservative approaches, in order to achieve the necessary weight loss to treat their endometrial cancer. These findings are encouraging and suggest a willingness from this patient population to engage in weight-loss treatments as part of treatment programmes for endometrial cancer. They need to be taken into account as we design future clinical trials in this area.
This questionnaire is the first of its kind and served to act as a scoping study to determine our patient population’s perceptions of obesity and endometrial cancer. While the small number of participants and single site distribution of the questionnaire are undoubtedly weaknesses, it has offered a useful insight into patient opinion and attitudes toward the role of weight loss in cancer treatment and will act as a springboard for further research work. Social and cultural attitudes to weight loss interventions may differ across different populations and this type of study needs to be expanded and repeated in larger cohorts and on an international setting. It would be beneficial to see how patient perception of cancer as a risk factor changes over time and whether the diagnosis of cancer would serve as a ‘wake-up call’ and lead to an improved understanding. Further research in this area looking at the difference in perception, if any, that may exist between younger patients with obesity and endometrial cancer is warranted as is a comparison to patients with obesity without a diagnosis of cancer.
In conclusion, this study demonstrates a need for patient education regarding the strong relationship between obesity and endometrial cancer risk. Patients with endometrial cancer are willing to consider weight loss interventions, including metabolic surgery as an alternative to standard surgical treatment, if it was proven to be as safe and effective as pelvic surgery. It is therefore incumbent on the gynaecological oncology community to conduct randomised studies in this area as our data suggests that recruiting patients to these studies may not be as difficult as previously considered.
CRediT authorship contribution statement
M. Wilkinson: Conceptualization, Data curation, Formal analysis, Methodology, Writing - original draft. S. Murphy: Conceptualization, Data curation, Methodology. P. Sinclair: Conceptualization, Data curation, Methodology. H Heneghan: Conceptualization, Methodology. C.W. le Roux: Conceptualization. D.J. Brennan: Conceptualization, Formal analysis, Methodology, Writing - review & editing.
Declaration of Competing Interest
The Authors of this manuscript declare absolutely no conflict of interest. No financial gain was received by any author nor was any patient financially rewarded for their participation in this study. This study received no sponsorship from industry.
Appendix A.
References
- Blackburn M., Stathi A., Keogh E., Eccleston C. Raising the topic of weight in general practice: perspectives of GPs and primary care nurses. BMJ Open. 2015;5(8):e008546. doi: 10.1136/bmjopen-2015-008546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crosbie E.J., Roberts C., Qian W., Swart A.M., Kitchener H.C., Renehan A.G. Body mass index does not influence post-treatment survival in early stage endometrial cancer: results from the MRC ASTEC trial. Eur. J. Cancer. 2012;48(6):853–864. doi: 10.1016/j.ejca.2011.10.003. [DOI] [PubMed] [Google Scholar]
- Derksen R.E., Brink-Melis W.J., Westerman M.J., Dam J.J., Seidell J.C., Visscher T.L. A local consensus process making use of focus groups to enhance the implementation of a national integrated health care standard on obesity care. Family Pract. 2012;29(Suppl 1):i177–i184. doi: 10.1093/fampra/cmr072. [DOI] [PubMed] [Google Scholar]
- Fader A.N., Arriba L.N., Frasure H.E., von Gruenigen V.E. Endometrial cancer and obesity: epidemiology, biomarkers, prevention and survivorship. Gynecol. Oncol. 2009;114(1):121–127. doi: 10.1016/j.ygyno.2009.03.039. [DOI] [PubMed] [Google Scholar]
- Kitson S., Ryan N., MacKintosh M.L., Edmondson R., Duffy J.M., Crosbie E.J. Interventions for weight reduction in obesity to improve survival in women with endometrial cancer. Cochrane Database Syst. Rev. 2018;2:Cd012513. doi: 10.1002/14651858.CD012513.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKintosh M.L., Derbyshire A.E., McVey R.J., Bolton J., Nickkho-Amiry M., Higgins C.L. The impact of obesity and bariatric surgery on circulating and tissue biomarkers of endometrial cancer risk. Int. J. Cancer. 2019;144(3):641–650. doi: 10.1002/ijc.31913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mawardi G., Kirkland E.B., Zhang J., Blankinship D., Heincelman M.E., Schreiner A.D. Patient perception of obesity versus physician documentation of obesity: A quality improvement study. Clin. Obesity. 2019;9(3):e12303. doi: 10.1111/cob.12303. [DOI] [PubMed] [Google Scholar]
- Mechanick J.I., Garber A.J., Handelsman Y., Garvey W.T. American Association of Clinical Endocrinologists' position statement on obesity and obesity medicine. Endocrine Pract.: Off. J. Am. Coll. Endocrinol. Am. Assoc. Clin. Endocrinol. 2012;18(5):642–648. doi: 10.4158/EP12160.PS. [DOI] [PubMed] [Google Scholar]
- Orekoya O., Samson M.E., Trivedi T., Vyas S., Steck S.E. The impact of obesity on surgical outcome in endometrial cancer patients: a systematic review. J. Gynecol. Surg. 2016;32(3):149–157. doi: 10.1089/gyn.2015.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstock I.M. Why people use health services. Milbank Memor. Fund Quart. 1966;44(3):94–127. [PubMed] [Google Scholar]
- Ryan D.H., Johnson W.D., Myers V.H., Prather T.L., McGlone M.M., Rood J. Nonsurgical weight loss for extreme obesity in primary care settings: results of the Louisiana Obese Subjects Study. Archiv. Internal Med. 2010;170(2):146–154. doi: 10.1001/archinternmed.2009.508. [DOI] [PubMed] [Google Scholar]
- Sekhon S., Massad L.S., Hagemann A.R., Dick R., Leon A., Zamorano A.S. Patients with endometrial cancer continue to lack understanding of their risks for cancer. Gynecol. Oncol. Rep. 2019;29:106–110. doi: 10.1016/j.gore.2019.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheikh M.A., Althouse A.D., Freese K.E., Soisson S., Edwards R.P., Welburn S. USA endometrial cancer projections to 2030: should we be concerned? Future Oncol. (Lond., Engl.) 2014;10(16):2561–2568. doi: 10.2217/fon.14.192. [DOI] [PubMed] [Google Scholar]
- Torre L.A., Bray F., Siegel R.L., Ferlay J., Lortet-Tieulent J., Jemal A. Global cancer statistics, 2012. CA: A Cancer J. Clin. 2015;65(2):87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- Visscher T.L., Heitmann B.L., Rissanen A., Lahti-Koski M., Lissner L. A break in the obesity epidemic? Explained by biases or misinterpretation of the data? Int. J. Obesity. 2015;39(2):189–198. doi: 10.1038/ijo.2014.98. [DOI] [PubMed] [Google Scholar]