Abstract
Socioeconomic status is an important determinant of health, the measurement of which is of great significance to population health research. However, individual-level socioeconomic factors are absent from much health administrative data, resulting in widespread use of area-level measures in their place. This study aims to clarify the role of individual- and area-level socioeconomic status in Ontario, Canada, through comparison of income measures.
Using data from four cycles (2005–2012) of the Canadian Community Health Survey, we assessed concordance between individual- and area-level income quintiles using percent agreement and Kappa statistics. Individual-level characteristics were compared at baseline. Cumulative adult premature mortality was calculated for 5-years following interview. Rates were calculated separately for area-level and individual-level income, and jointly for each combination of income groups. Multivariable negative binomial models were fit to estimate associations between area- and individual-level income quintile and premature mortality after adjustment for basic demographics (age, sex, interview cycle) and key risk factors (alcohol, smoking, physical activity, and body mass index).
Agreement between individual- and area-level income measures was low. Kappa statistics for same and similar (i.e. ±1 quintile) measures were 0.11 and 0.48, indicating low and moderate agreement, respectively. Socioeconomic disparities in premature mortality were greater for individual-level income than area-level income. When rates were stratified by both area- and individual-level income quintiles simultaneously, individual-level income gradients persisted within each area-level income group. The association between income and premature mortality was significant for both measures, including after full adjustment.
Area-level socioeconomic status is an inappropriate proxy for missing individual-level data. The low agreement between area- and individual-level income measures and differences in demographic profile indicate that the two socioeconomic status measures do not capture the same population groups. However, our findings demonstrate that both individual- and area-level income measures are associated with premature mortality, and describe unique socioeconomic inequities.
Keywords: Area-level measures, Individual-level measures, Premature mortality, Socioeconomic status
Highlights
-
•
Area- and individual-level income measures may not capture the same groups.
-
•
Area-level socioeconomic status is not a valid proxy for individual-level data.
-
•
Area- and individual-level income are independently meaningful for health outcomes.
-
•
Measures can be used together to fully contextualize socioeconomic status.
1. Background
Socioeconomic status, and in particular income, is well-established as a determinant of health (Braveman et al., 2005). Low socioeconomic status has been linked to many health-relevant risk behaviors, including food insecurity (Che & Chen, 2001), smoking (Hiscock, Bauld, Amos, Fidler, & Munafò, 2012), and physical inactivity (Giles-Corti & Donovan, 2002), and to poorer health outcomes such as chronic conditions (Agardh, Allebeck, Hallqvist, Moradi, & Sidorchuk, 2011; Gershon, Dolmage, Stephenson, & Jackson, 2012; Kaplan & Keil, 1993), multimorbidity (Moin, Moineddin, & Upshur, 2018; Pathirana & Jackson, 2018; Rosella et al., 2018) and premature mortality (Khan et al., 2017; Stringhini et al., 2017). Low income has also been linked with decreased access to and quality of medical care (Moin et al., 2018; Newacheck, Hughes, & Stoddard, 1996) – including in Ontario, where a single-payer health insurance plan is in place (Health Quality Ontario, 2015). Accurate assessment of socioeconomic status is necessary to enable the study of health of these and other health inequalities but is often challenged by the limited availability of appropriate socioeconomic measures. For example, individual measures of income and education are absent from most health administrative data (Krieger, 1992). In this scenario, area-level socioeconomic measures are often used in place of individual-level measures, by assigning individuals to the socioeconomic profile of their geographic area of residence. Neighbourhood income, for instance, is commonly deployed in the absence of household or individual income.
The validity of this proxy approach has been widely contested. Some comparisons suggest that area-level measures capture similar socioeconomic gradients as compared to individual-level income and should therefore be considered an appropriate proxy in the study of health inequalities (Mustard, Derksen, Berthelot, & Wolfson, 1999). However, interpretation of trends across area-level income groups may be vulnerable to the ecological fallacy, a type of cross-level bias that occurs when individual-level inferences are made based on associations at the aggregate level (Hanley & Morgan, 2008; Porta, 2014). Further, the mechanisms underlying the association between area-level income and health outcomes are often unclear, and may not appropriately represent the relationship between individual-level income and health (Pickett & Pearl, 2001).
Correspondence between individual- and area-level measures of income has been studied using two main approaches: by assessing the correlation (i.e. statistical agreement) between measures (Diez-Roux et al., 2001; Roblin, 2013), or by comparing the socioeconomic gradient associated with each type of measure for a given health characteristic (Domínguez-Berjón, Borrell, Rodríguez-Sanz, & Pastor, 2005; Subramanian, Chen, Rehkopf, Waterman, & Krieger, 2006). Overall, poor agreement between area- and individual-level income measures has been observed, with especially low correlation between measures noted in low-income and rural groups (Demissie, Hanley, Menzies, Joseph, & Ernst, 2000; Marra, Lynd, Harvard, & Grubisic, 2011; Narla et al., 2015; Sin, Svenson, & Man, 2001). Socioeconomic gradients associated with individual- and area-level income measures have been generally consistent, with comparable trends in risk factors and health outcomes (Locker & Ford, 1996; Pichora et al., 2018; Southern, McLaren, Hawe, Knudtson, & Ghali, 2005). Multilevel or joint-exposure analyses have shown significant effects of both area- and individual-level measures of socioeconomic status (DeRouen et al., 2018; Diez-Roux et al., 1997; Juhn et al., 1982; Li et al., 2010), although few studies of this type have been carried out in Canada or other single-payer health care jurisdictions. The relationship between area- and individual-level health inequalities in single-payer settings remains of interest. Further, a question remains regarding the potential joint effects of area- and individual-level income status.
Our goal was to assess the level of agreement between individual- and area-level income measures, and, secondly, to examine the risk of premature mortality across combinations of income groups. We leveraged a representative population-based survey cohort from the Canadian Community Health Survey (CCHS), linked to healthcare data from Ontario's single-payer health insurance program (OHIP). OHIP collects residential information to allow linkage with area-level income measures. Premature mortality outcomes were then calculated to describe the socioeconomic gradient according to both area- and individual-level income measures, and for all of their combinations. For premature mortality outcomes, we used multivariable negative binomial regression to estimate adjusted rate ratios associated with area- and individual-level income measures, after adjustment for key demographic and behavioural risk factors.
Overall, this study aims to clarify the role of area- and individual-level income in the context of premature mortality as a robust measure of population health, in order to support better understanding of the impact of area-level approximation on observed socioeconomic patterns.
2. Materials and methods
2.1. Data sources
This study utilized data from 4 cycles of the CCHS, conducted by Statistics Canada in 2005–2006, 2007–2008, 2009–2010, and 2011–2012. The CCHS is a cross-sectional survey that gathers health-related information about the Canadian population, such as health status, health care utilization, and health determinants (Roos & Wajda, 1991). It is representative of 98% of the Canadian population ages 12 and older; exceptions include people living on First Nations Reserves and Crown Lands, institutionalized residents, full-time members of the Canadian Forces and people who reside in certain remote areas. All responses to questions were self-reported. Detailed descriptions of the CCHS survey methodology are documented elsewhere (Statistics Canada, 2018).
Eighty-four percent of CCHS respondents agreed to have their responses linked to health administrative data. The linked CCHS records are generally representative of the CCHS target population; although coverage is poorer for ages 75 and older (Rotermann, 2009), this population is excluded by definition from our analysis. These responses were linked deterministically (i.e. via exact matching) and probabilistically at ICES (previously the Institute for Clinical Evaluative Sciences) to death records from the Ontario Registrar General, via a central population registry of individuals eligible for the province's single-payer health insurance system at any point since 1992 (the Registered Persons' Database or RPDB). This linkage has been described elsewhere (Chiu et al., 2016).
2.2. Study population
CCHS respondents from the four identified cycles were included if they had not been interviewed for CCHS before, were between ages 18 and 74 at interview, resided in Ontario, could be linked to a valid RPDB record, and had both individual-level and area-level income measures available. Prior to exclusions, missingness for area-level income was less than 1 percent and missingness for individual-level income was 7.7%. In total, 97,025 unique respondents were included, representing a weighted population of 7,653,907.
2.3. Variable definitions
Individual-level income quintiles (i.e., five groups of similar population size) were assigned based on self-reported pre-tax household income at interview date. Quintiles represent a relative measure of self-reported household income to the household income of all other respondents within Ontario and for each distinct interview cycle; thus, quintiles are representative of relative socioeconomic position within Ontario at the time of interview.
Area-level income quintiles were assigned based on postal code of residence at interview. Using Statistics Canada's Postal CodeOM Conversion File Plus (PCCF+), postal codes were linked to census geography at the dissemination area level. Dissemination areas, most of which have a population between 400 and 700, are the smallest area at which population characteristics from the Canadian Census are reported. Each dissemination area was assigned to an area-level income quintile according to the nearest-census household income of the residents of that area.
The primary outcome of this analysis, premature mortality, was selected as it is an established indicator of population health which is routinely measured and robust to coding practices (Norheim et al., 2015; Shiels et al., 2017). Socioeconomic gradients in premature mortality have been reported in Ontario and elsewhere (Khan et al., 2017; Stringhini et al., 2017). Adult premature deaths were defined as those occurring between the ages of 18 and 74, consistent with the definition used by the Canadian Institute for Health Information (Canadian Institute for Health Information, 2012). All deaths were identified if they occurred within 5 years following CCHS interview date, and were registered in the province of Ontario.
2.4. Statistical analysis
We assessed agreement between individual- and area-level income quintiles using percent agreement and Kappa statistics. Kappa results can be interpreted as such: values ≤ 0 indicate no agreement; 0.01–0.20 as none to slight; 0.21–0.40 as fair; 0.41–0.60 as moderate; 0.61–0.80 as substantial; and 0.81–1.00 as almost perfect agreement (McHugh, 2012). Both percent agreement and Kappa scores were calculated separately for same agreement (i.e. an individual is assigned to the same area-level and individual-level income quintile) and similar agreement (i.e. an individual is assigned to an area-level and individual-level income quintile no more than one apart). This approach is recommended for categorical data that follows an ordinal structure as it takes into account both same agreement and similar agreement (Landis & Koch, 1977). To assess whether agreement changed over time, agreement statistics were calculated for each distinct CCHS cycle, and overall for the pooled cohort. In addition to the combined measures, separate agreement statistics were calculated for males and females.
To describe population differences associated with area- and individual-level income status, we summarized baseline cohort characteristics at interview date according to individual-level and area-level income quintiles. Characteristics measured include demographics (age, sex, immigrant status, visible minority status), socioeconomic indicators (marital status, education), and health and behavioral characteristics (BMI, physical activity, smoking, and alcohol consumption).
Cumulative 5-year adult premature mortality was measured for area- and individual-level income groups. Rates were calculated as premature (age 18–74) deaths per 1000 in the respondent population within 5 years of interview date. To ascertain area- and individual-level income gradients in premature mortality, rates were calculated separately for area- and individual-level income quintiles. To characterize joint individual- and area-level income effects, we also calculated premature mortality rates for each combination of income groups. Premature mortality rates were not age-standardized given that premature mortality is an age-specific rate.
Adjusted rate ratios for individual- and area-level income measures were estimated using multivariable negative binomial models. Minimally-adjusted rate ratios were adjusted for sex, age and interview date, and survey cycle. Fully-adjusted rate-ratios were adjusted additionally for alcohol consumption, smoking status, physical activity level, and body mass index. Covariate definitions are shown in Table 1.
Table 1.
Cohort characteristics at interview date according to individual- and area-level income quintiles (weighted percents).
| Variable | Level | Area-level income quintile (Q) |
Individual-level income quintile (Q) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
||
| Unweighted n = 18911 | Unweighted n = 19242 | Unweighted n = 19652 | Unweighted n = 19885 | Unweighted n = 19164 | Unweighted n = 17056 | Unweighted n = 17478 | Unweighted n = 19839 | Unweighted n = 20348 | Unweighted n = 22133 | ||
| Area-level income quintile (Q) | Q1 | – | – | – | – | – | 37.2 | 24.3 | 16.5 | 12.6 | 8.5 |
| Q2 | – | – | – | – | – | 22.1 | 23.2 | 20.3 | 17.0 | 13.0 | |
| Q3 | – | – | – | – | – | 17.5 | 21.6 | 22.0 | 21.3 | 18.2 | |
| Q4 | – | – | – | – | – | 12.8 | 17.6 | 21.9 | 24.6 | 24.6 | |
| Q5 | – | – | – | – | – | 10.5 | 13.4 | 19.3 | 24.5 | 35.7 | |
| Individual-level income quintile (Q) | Q1 | 35.5 | 21.4 | 15.9 | 11.4 | 9.0 | – | – | – | – | – |
| Q2 | 24.0 | 23.4 | 20.4 | 16.3 | 12.0 | – | – | – | – | – | |
| Q3 | 16.9 | 21.2 | 21.6 | 21.1 | 18.0 | – | – | – | – | – | |
| Q4 | 13.9 | 19.1 | 22.4 | 25.3 | 24.4 | – | – | – | – | – | |
| Q5 | 9.6 | 14.9 | 19.7 | 26.0 | 36.6 | – | – | – | – | – | |
| Sex | F | 50.1 | 50.9 | 50.3 | 50.7 | 47.9 | 57.1 | 53.0 | 50.0 | 47.0 | 44.0 |
| M | 49.9 | 49.1 | 49.7 | 49.3 | 52.1 | 42.9 | 47.0 | 50.0 | 53.0 | 56.0 | |
| Age (years) | 18–24 | 12.2 | 11.2 | 10.6 | 10.0 | 10.8 | 14.9 | 12.1 | 11.5 | 9.7 | 7.3 |
| 25–34 | 21.7 | 20.2 | 18.6 | 18.1 | 13.8 | 17.6 | 18.3 | 19.0 | 20.5 | 16.4 | |
| 35–44 | 22.3 | 22.1 | 22.7 | 23.2 | 22.2 | 22.3 | 21.3 | 22.6 | 23.3 | 23.0 | |
| 45–54 | 20.1 | 20.3 | 21.2 | 21.6 | 23.6 | 16.5 | 19.4 | 20.1 | 22.7 | 27.2 | |
| 55–64 | 14.4 | 16.4 | 16.6 | 17.0 | 19.9 | 14.8 | 15.3 | 16.7 | 16.9 | 20.4 | |
| 65–74 | 9.2 | 9.7 | 10.2 | 10.1 | 9.8 | 13.8 | 13.7 | 10.1 | 6.8 | 5.7 | |
| Immigranta | No | 73.3 | 82.1 | 84.7 | 87.0 | 91.5 | 70.8 | 76.4 | 85.9 | 90.7 | 93.2 |
| Yes | 26.7 | 17.9 | 15.3 | 13.0 | 8.5 | 29.2 | 23.6 | 14.1 | 9.3 | 6.8 | |
| Recent Immigranta,b | No | 92.5 | 95.6 | 97.1 | 97.4 | 98.3 | 90.8 | 94.7 | 97.1 | 98.8 | 99.0 |
| Yes | 7.5 | 4.4 | 2.9 | 2.6 | 1.7 | 9.2 | 5.3 | 2.9 | 1.2 | 1.0 | |
| Visible Minorityc | No | 64.2 | 74.1 | 76.3 | 82.1 | 86.4 | 58.4 | 68.0 | 79.4 | 85.6 | 89.4 |
| Yes | 35.8 | 25.9 | 23.7 | 17.9 | 13.6 | 41.6 | 32 | 20.6 | 14.4 | 10.6 | |
| Marital Statusc | Married or Common Law | 57.2 | 63.6 | 68.2 | 71.7 | 72.8 | 52.4 | 63.1 | 66.8 | 71.3 | 78.3 |
| Other | 42.8 | 36.4 | 31.8 | 28.3 | 27.2 | 47.6 | 36.9 | 33.2 | 28.7 | 21.7 | |
| Highest educational attainmentc | Some post-secondary | 77.5 | 81.7 | 85.5 | 88.5 | 91.5 | 70.2 | 80.4 | 85.9 | 91.2 | 94.9 |
| Secondary | 14.1 | 12.4 | 10.5 | 8.4 | 6.3 | 17.0 | 13.5 | 10.8 | 7.3 | 4.2 | |
| Less than secondary | 8.3 | 5.9 | 4.0 | 3.1 | 2.1 | 12.8 | 6.0 | 3.3 | 1.5 | 0.8 | |
| Body mass index (BMI; kg per m2)c | Underweight (less than 18.5) | 2.8 | 2.5 | 2.5 | 2.3 | 1.8 | 3.9 | 3.2 | 2.1 | 1.8 | 1.1 |
| Normal weight (18.5–24.9) | 44.6 | 43.4 | 43.6 | 44.6 | 47.0 | 46.2 | 45.4 | 44.5 | 42.9 | 44.7 | |
| Overweight (25.0–29.9) | 33.3 | 34.5 | 34.6 | 35.0 | 35.7 | 30.8 | 33.6 | 34.6 | 36.1 | 37.5 | |
| Moderately obese (30.0–34.9) | 13.0 | 13.6 | 13.4 | 13.4 | 11.4 | 12.6 | 12.3 | 13.2 | 13.8 | 12.6 | |
| Very obese (35.0–39.9) | 4.1 | 3.9 | 4.2 | 3.3 | 3.1 | 4.1 | 3.8 | 3.9 | 3.7 | 3.2 | |
| Severely obese (40.0 or greater) | 2.3 | 2.1 | 1.6 | 1.4 | 1.0 | 2.5 | 1.7 | 1.6 | 1.7 | 0.9 | |
| Physical activity levelc | Active | 21.7 | 23.5 | 25.3 | 28.3 | 31.6 | 20.2 | 21.3 | 24.9 | 28.5 | 34.6 |
| Moderate | 21.4 | 25.4 | 25.3 | 26.5 | 28.2 | 20.8 | 22.7 | 26.1 | 27.6 | 29.0 | |
| Inactive | 56.9 | 51.1 | 49.3 | 45.2 | 40.2 | 59.0 | 56.0 | 49.1 | 43.9 | 36.4 | |
| Smoking statusc | Heavy smoker | 4.9 | 4.1 | 3.3 | 2.7 | 2.1 | 5.4 | 3.3 | 3.1 | 3.3 | 2.2 |
| Light smoker | 24.1 | 21.2 | 19.3 | 18.6 | 15.2 | 25.5 | 20.6 | 20.0 | 18.0 | 14.8 | |
| Former heavy smoker | 5.5 | 6.1 | 6.0 | 6.2 | 6.2 | 4.6 | 6.1 | 6.6 | 6.1 | 6.5 | |
| Former light smoker | 14.1 | 15.1 | 16.4 | 17.9 | 18.8 | 11.5 | 15.5 | 17.3 | 17.5 | 20.0 | |
| Nonsmoker | 51.3 | 53.5 | 55.0 | 54.7 | 57.6 | 53.1 | 54.5 | 53.0 | 55.1 | 56.5 | |
| Alcohol consumptionc | Heavy drinker | 3.3 | 3.3 | 3.6 | 3.7 | 4.6 | 2.9 | 2.7 | 3.9 | 3.9 | 5.1 |
| Moderate drinker | 18.2 | 22.4 | 25.4 | 29.0 | 34.5 | 12.9 | 19.9 | 25.7 | 30.3 | 39.1 | |
| Light drinker | 13.4 | 14.6 | 15.2 | 16.2 | 17.7 | 10.0 | 14.1 | 14.9 | 18.6 | 18.8 | |
| Never drinker | 65.1 | 59.6 | 55.7 | 51.1 | 43.2 | 74.3 | 63.3 | 55.4 | 47.2 | 36.9 | |
Immigrant status from Immigration, Refugees and Citizenship Canada (IRCC) permanent resident file; captures immigrants landed in Ontario since 1985.
Landed within 5 years prior to interview date.
Based on self-report from CCHS interview.
All data preparation and analysis took place using SAS (version 9.4), Cary, NC. Negative binomial models were fit using the GENMOD procedure, using normalized survey weights provided by Statistics Canada. Statistical significance (α = 0.05) of categorical predictors was assessed using Wald statistics for Type III effects.
3. Results
3.1. Agreement between individual- and area-level income measures
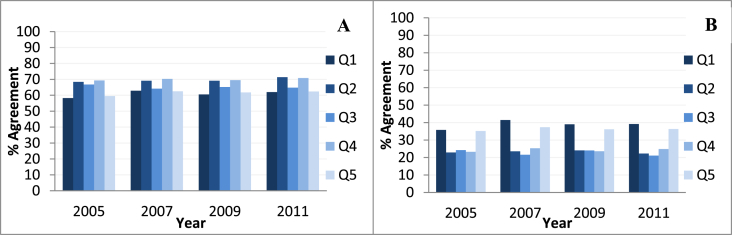
Overall, agreement between individual-level and area-level income measures was low. Across all four cycles of the CCHS, 29% of respondents were assigned to the same quintile for both area- and individual-level income (percent same agreement). The total Kappa statistic for same measures obtained for the pooled cohort was found to be 0.11, indicating little to no correlation. Percent agreement was 65% when counting respondents who were assigned within ±1 quintile for area- and individual-level income (similar agreement). The total Kappa statistic for similar measures was found to be 0.49, indicating moderate agreement.
When stratified by CCHS cycle (i.e. over time) or sex, agreement between area-level and individual income measures did not change. As measured by percent agreement and Kappa statistics, there was no change in agreement over time between 2005 and 2011. There was also no reportable difference in agreement between male and female CCHS respondents.
3.2. Cohort characteristics
Socioeconomic distributions across categories of visible minority status, marital status, body mass index, smoking, and alcohol consumption did not differ greatly between area- and individual-level quintiles (Table 1). Conversely, there were noticeable differences in the socioeconomic distribution of age, sex, immigrant status, recent immigrant status, educational attainment, and physical activity when stratified by area-versus individual-level income (Table 1). Specifically, the gap between low- and high-income groups was larger when measured with individual-level income than when measured with area-level for these characteristics.
3.3. 5-Year premature mortality
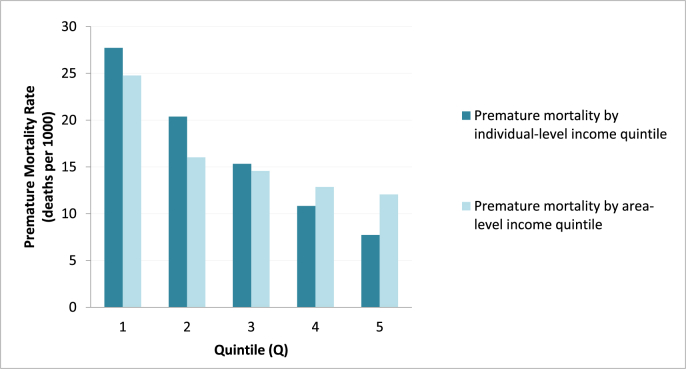
A socioeconomic gradient was observed for both individual- and area-level income, wherein 5-year premature mortality increased with each quintile decrease in income (Fig. 2). The gap between low- and high-income groups was demonstrably larger when measured with individual-versus area-level income. For individual income, 5-year premature mortality was 3.59 times as high in the lowest quintile compared to the highest income quintile (27.7 deaths per 1000 versus 12.1 deaths per 1000). For area-level income, 5-year premature mortality was 2.05 times as high in the lowest quintile compared to the highest (24.8 versus 12.1 deaths per 1000). When comparing the relative rates of the quintiles to Q5, individual-level measures report higher relative rates of premature mortality than area-level measures for every quintile.
Fig. 2.
Premature mortality rates according to individual- and area-level self-reported income measures.
The relationship between area-level income and premature mortality is non-linear in comparison to the relationship between individual-level income and premature mortality. Observed 5-year premature mortality was higher when measured with individual-level measures for quintiles 1 to 3, and higher for area-level measures in quintiles 4 and 5. However, the gap between area- and individual-level premature mortality rates is largest for quintiles 2 and 5, due to a relatively flat association between area-level income and premature mortality in that range.
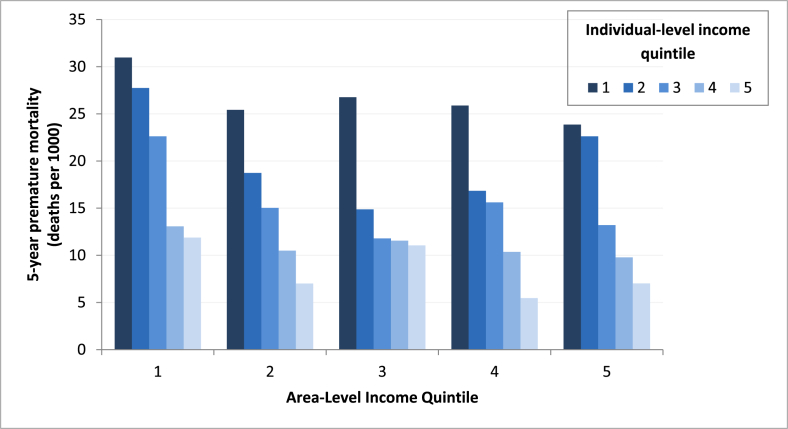
When stratified by both income measures combined, 5-year mortality rates suggest joint effects of individual- and area-level income status on adult premature mortality outcomes (Fig. 3). Within each area-level income group, a clear gradient was seen across individual-level income quintiles. This effect was not seen as clearly within individual-level income groups; no linear gradient was observed across area-level income quintiles (see Figure A1 in the appendix).
Fig. 3.
Comparison of 5-year adult premature mortality rates for individual- and area-level income quintile combinations.
Fig. 1.
Percent of (A) similar and (B) same income quintile between individual- and area-level self-reported income.
3.4. Model output
Unadjusted, minimally-adjusted and fully-adjusted rate ratio estimates from negative binomial models are shown in Table 2. When adjusted for age, sex and survey cycle, the strength of the observed association between individual-level income and premature mortality was attenuated, while the observed association between area-level income and premature mortality was strengthened (Table 2). When further adjusted for smoking, physical activity, alcohol consumption and body mass index, the observed associations between income and premature mortality were greatly attenuated for both area- and individual-level measures. After full adjustment, the effect of individual income on premature mortality was attenuated for all quintiles. Similarly, the effect of area-level income on premature mortality, which was lower begin with, was also attenuated after full adjustment. In the case of area-level income, the fully-adjusted effect sizes for Q3 and Q4 were close to the null and confidence intervals spanned 1.0. Wald statistics for Type III effects of area- or individual-level income on premature mortality were statistically significant in all models (p < 0.0001), including after adjustment for individual-level risk factors.
Table 2.
Unadjusted and adjusted rate ratios (RRs) and 95% confidence intervals (CIs) for premature mortality according to area- and individual-level income measures.
| Income Quintile | Unadjusted RR (95%CI) |
Minimally-adjusted RRa (95%CI) |
Fully-adjusted RRb (95%CI) |
|||
|---|---|---|---|---|---|---|
| Individual-level income | Area-level income | Individual-level income | Area-level income | Individual-level income | Area-level income | |
| Q1 | 3.60 (2.98, 4.34) | 1.64 (1.37, 1.96) | 3.45 (2.93, 4.05) | 1.91 (1.65, 2.21) | 2.19 (1.89, 2.53) | 1.41 (1.24, 1.61) |
| Q2 | 2.25 (1.85, 2.73) | 1.30 (1.08, 1.57) | 1.92 (1.62, 2.28) | 1.38 (1.19, 1.61) | 1.47 (1.26, 1.71) | 1.14 (1.00, 1.31) |
| Q3 | 1.78 (1.46, 2.16) | 1.08 (0.90, 1.31) | 1.68 (1.41, 1.99) | 1.13 (0.97, 1.33) | 1.39 (1.19, 1.62) | 1.02 (0.89, 1.17) |
| Q4 | 1.34 (1.09, 1.64) | 1.05 (0.87, 1.27) | 1.37 (1.15, 1.64) | 1.10 (0.94, 1.28) | 1.20 (1.02, 1.42) | 1.03 (0.89, 1.18) |
| Q5 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
Minimally-adjusted models were adjusted for age, sex and survey cycle.
Fully-adjusted models were adjusted for age, sex, survey cycle, smoking status, alcohol consumption, body mass index, and physical activity level.
4. Discussion
4.1. Key findings
The aim of this study was to compare individual- and area-level income measures using a population-based survey cohort linked with routinely collected health data that lacks individual-level income. The results show low agreement between individual- and area-level income measures and suggest that these measures may capture meaningfully different populations, with substantive differences in demographic profile. While both area- and individual-level income quintiles were associated with a clear socioeconomic gradient in premature mortality, the profile of these gradients differed between measures. Further, joint effects indicated when rates were stratified by both area- and individual-level income simultaneously suggest that area- and individual-level income status may act independently on premature mortality outcomes. After adjustment for individual-level risk factors, statistically significant associations with premature mortality outcomes persisted for both area- and individual-level income measures. However, the nature of these associations was highly dissimilar – individual-level income was more strongly associated with premature mortality than area-level income, and the observed effect of area-level income approached the null for some quintiles after adjustment for individual-level factors.
Low agreement between individual- and area-level measures of socioeconomic status has been consistently seen, in Canada (Demissie et al., 2000; Southern et al., 2005) and other jurisdictions (Marra et al., 2011; Narla et al., 2015; Soobader, LeClere, Hadden, & Maury, 2001). Our study findings are consistent with this existing research. Further, previous comparisons in Canada have primarily focused on narrow clinical populations or subgroups (e.g. children) – our findings demonstrate low correspondence between individual- and area-level income groups in a large, representative Canadian cohort.
While agreement between measures is consistently reported as low, comparisons of population characteristics and health outcomes have had inconsistent findings. The most comprehensive comparison conducted in Canada – a cross-sectional study of income inequalities in smoking, obesity and diabetes – reported comparable trends for individual- and area-level measures (Pichora et al., 2018). However, other work in Canada (Pampalon, Hamel, & Gamache, 2009; Southern et al., 2005) and elsewhere (Mather et al., 2014; Pardo-Crespo et al., 2013) found stronger associations with individual-versus area-level income for outcomes including life expectancy, smoking and obesity (in the US), and health-related quality of life. We note that in our study, discrepancies between area- and individual-level income gradients were small for some health-relevant characteristics, including smoking, BMI and alcohol consumption. In general, however, the differences in population characteristics and health outcomes captured by area-versus individual-level income were large and warrant considerable attention.
Our findings support others indicating that area-level socioeconomic status measures must not be considered a reasonable proxy for individual measurement. However, area-level measures can provide unique information about socioeconomic position that is independent of individual-level income. Area-based measures can provide information about a resident population that cannot be captured at the individual level, including: areas of poverty, access to health services, environmental exposures and other contextual factors (Mather et al., 2014; Southern et al., 2005). Additionally, our analysis showed significant associations between area-level income and premature mortality outcomes, after adjustment for individual-level risk factors. Thus area-level measures of socioeconomic status, while not an applicable proxy for individual-level factors, are of value for understanding the socioeconomic experience of populations.
4.2. Strengths and limitations
This study is the first comparison of individual- and area-level income measures in Canada to consider both baseline agreement and demographics and subsequent population health outcomes. We used a robust cohort of over 97,000 CCHS respondents, surveyed over a 7-year time period, which are representative of 98% of the Ontario population. We also benefited from complete outcome information because we used comprehensive mortality records with a high linkage rate to our study population. As a result, we were able to evaluate a robust population health outcome prospectively across income groups, including combinations of area- and individual-level income quintiles, for the entire Ontario population.
Our findings may be influenced by the use of self-reported income measures. Error in self-reported income is generally low for wages and salaries, but may be significantly greater for other sources (Meyer, Mok, & Sullivan, 2009). In particular, government transfer payments are frequently underestimated in self-reported income, which has important implications for measurement in the low-income population (Moore & Welniak, 2000). This impact may be exacerbated by the use of different data sources for individual- and area-level income measures, if respondents tend to report income differently when responding to the census (which informed area-level income measures) than when responding to the CCHS. However, self-reported income is frequently used, particularly in settings such as Canada where routine linkages to tax-based income are not available. Therefore, this comparison is relevant for the many studies that use self-reported income. Furthermore, self-reported measures of SES are robust predictors of health outcomes and the absolute accuracy of the individual-level measures does not affect the conclusions regarding their agreement with area-level measures (Lantz, Golberstein, House, & Morenoff, 1982).
Our analysis does not provide direct insight into the area-versus individual-level concordance of other measures of socioeconomic position, such as educational attainment or occupation. Future comparisons may provide insight into the implications of using alternative area-level measures. Our analysis also does not necessarily establish an independent effect of area- and individual-level income on premature mortality, which could be substantiated through multilevel analysis of income measures. This would be an important contribution of future work.
4.3. Implications and next steps
Understanding the differences between individual- and area-level income is becoming increasingly important, as the income gap has steadily widened in Canada (Hajizadeh, Mitnitski, & Rockwood, 2016), and in most other developed countries (OECD, 2011). Our ability to measure this gap and to determine how individual and/or area-level income affects health outcomes hinges on our understanding of these two constructs.
Future work should focus on identifying alternative socioeconomic measures for use in the absence of individual-level income data. For example, in Olmstead County, Minnesota, researchers successfully developed a socioeconomic index based on housing characteristics (HOUSES), which correlates moderately with other individual-level socioeconomic indices, can be linked to population health data using address information, and was shown to be generalizable to other US jurisdictions (Harris et al., 2014; Juhn et al., 2011). The HOUSES index has been used to describe socioeconomic inequalities in indicators of population health (Bjur et al., 2019; Hammer et al., 2016; Ryu et al., 2017; Thacher et al., 2020; Wi et al., 2016) and health service delivery (Barwise et al., 2018; Takahashi et al., 2016). In the absence of individual-level socioeconomic data, address data may enable reporting on individual-level socioeconomic inequalities. Likewise, other opportunities may exist to leverage existing individual-level data sources and create novel indicators of socioeconomic status.
The results of our study call for caution when using area-level data as measure of individual-level socioeconomic status. The low agreement between measures and differing demographic profiles suggests that the two approaches may not capture the same population. Thus interpretation of findings based on area-level data should be clear that the observed trends may not be generalizable to individual-level associations. That said, our analysis shows that area-level measures of socioeconomic status are nonetheless meaningful for population health outcomes. Recognizing the limitations of area-level socioeconomic status, with appropriate interpretation, area-level measures need to be cautiously used to understand socioeconomic health disparities. Area- and individual-level measures may further be used together, as joint effects or through multilevel modelling, to fully contextualize the role of individual- and area-level socioeconomic characteristics in specific health outcomes.
Funding
This study was funded by the Canadian Institutes for Health Research Operating Grant (FRN-142498). LR is supported by a Canada Research Chair in Population Health Analytics.
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
Ethics statement
This study was approved by the University of Toronto Health Sciences Research Ethics Board (Protocol 32505).
CRediT authorship contribution statement
Emmalin Buajitti: Conceptualization, Methodology, Formal analysis, Writing - original draft. Sabrina Chiodo: Formal analysis, Writing - original draft, Visualization. Laura C. Rosella: Conceptualization, Methodology, Writing - review & editing, Supervision.
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2020.100553.
Appendix A. Supplementary Figure
The following are the Supplementary data to this article:
References
- Agardh E., Allebeck P., Hallqvist J., Moradi T., Sidorchuk A. Type 2 diabetes incidence and socio-economic position: A systematic review and meta-analysis. International Journal of Epidemiology. 2011;40(3):804–818. doi: 10.1093/ije/dyr029. [DOI] [PubMed] [Google Scholar]
- Barwise A., Juhn Y.J., Wi C.-I., Novotny P., Jaramillo C., Gajic O. An individual housing-based socioeconomic status measure predicts advance care planning and nursing home utilization. American Journal of Hospice and Palliative Medicine. 2018;36(5):362–369. doi: 10.1177/1049909118812431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjur K.A., Wi C.-I., Ryu E., Derauf C., Crow S.S., King K.S. Socioeconomic status, race/ethnicity, and health disparities in children and adolescents in a mixed rural-urban community—Olmsted county, Minnesota. Mayo Clinic Proceedings. 2019;94(1):44–53. doi: 10.1016/j.mayocp.2018.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P.A., Cubbin C., Egerter S., Chideya S., Marchi K.S., Metzler M. Socioeconomic status in health Research One size does not fit all. Journal of the American Medical Association. 2005;294(22):2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- Canadian Institute for Health Information . 2012. Health indicators 2012. Ottawa, ON. [Google Scholar]
- Che J., Chen J. Food insecurity in Canadian households. Health Reports. 2001;12(4):11–22. [PubMed] [Google Scholar]
- Chiu M., Lebenbaum M., Lam K., Chong N., Azimaee M., Iron K. Describing the linkages of the immigration, refugees and citizenship Canada permanent resident data and vital statistics death registry to Ontario's administrative health database. BMC Medical Informatics and Decision Making. 2016;16(1):135. doi: 10.1186/s12911-016-0375-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demissie K., Hanley J.A., Menzies D., Joseph L., Ernst P. Agreement in measuring socio-economic status: Area-based versus individual measures. Chronic Diseases in Canada. 2000;21(1):1–7. [PubMed] [Google Scholar]
- DeRouen M.C., Schupp C.W., Yang J., Koo J., Hertz A., Shariff-Marco S. Impact of individual and neighborhood factors on socioeconomic disparities in localized and advanced prostate cancer risk. Cancer Causes & Control : Cancer Causes & Control. 2018;29(10):951–966. doi: 10.1007/s10552-018-1071-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez-Roux A.V., Kiefe C.I., Jacobs D.R., Jr., Haan M., Jackson S.A., Nieto F.J. Area characteristics and individual-level socioeconomic position indicators in three population-based epidemiologic studies. Annals of Epidemiology. 2001;11(6):395–405. doi: 10.1016/s1047-2797(01)00221-6. [DOI] [PubMed] [Google Scholar]
- Diez-Roux A.V., Nieto F.J., Muntaner C., Tyroler H.A., Comstock G.W., Shahar E. Neighborhood environments and coronary heart disease: A multilevel analysis. American Journal of Epidemiology. 1997;146(1):48–63. doi: 10.1093/oxfordjournals.aje.a009191. [DOI] [PubMed] [Google Scholar]
- Domínguez-Berjón F., Borrell C., Rodríguez-Sanz M., Pastor V. The usefulness of area-based socioeconomic measures to monitor social inequalities in health in Southern Europe. The European Journal of Public Health. 2005;16(1):54–61. doi: 10.1093/eurpub/cki069. [DOI] [PubMed] [Google Scholar]
- Gershon A.S., Dolmage T.E., Stephenson A., Jackson B. Chronic obstructive pulmonary disease and SocioEconomic status: A systematic review. COPD: Journal of Chronic Obstructive Pulmonary Disease. 2012;9(3):216–226. doi: 10.3109/15412555.2011.648030. [DOI] [PubMed] [Google Scholar]
- Giles-Corti B., Donovan R.J. Socioeconomic status differences in recreational physical activity levels and real and perceived access to a supportive physical environment. Preventive Medicine. 2002;35(6):601–611. doi: 10.1006/pmed.2002.1115. [DOI] [PubMed] [Google Scholar]
- Hajizadeh M., Mitnitski A., Rockwood K. Socioeconomic gradient in health in Canada: Is the gap widening or narrowing? Health Policy. 2016;120(9):1040–1050. doi: 10.1016/j.healthpol.2016.07.019. [DOI] [PubMed] [Google Scholar]
- Hammer R., Capili C., Wi C.-I., Ryu E., Rand-Weaver J., Juhn Y.J. A new socioeconomic status measure for vaccine research in children using individual housing data: A population-based case-control study. BMC Public Health. 2016;16(1):1000. doi: 10.1186/s12889-016-3673-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanley G.E., Morgan S. On the validity of area-based income measures to proxy household income. BMC Health Services Research. 2008;8(1):79. doi: 10.1186/1472-6963-8-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris M.N., Lundien M.C., Finnie D.M., Williams A.R., Beebe T.J., Sloan J.A. Application of a novel socioeconomic measure using individual housing data in asthma research: An exploratory study. npj Primary Care Respiratory Medicine. 2014;24(1):14018. doi: 10.1038/npjpcrm.2014.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Quality Ontario . Queen's Printer for Ontario; Toronto, ON: 2015. Quality matters: Realizing excellent care for all. [Google Scholar]
- Hiscock R., Bauld L., Amos A., Fidler J.A., Munafò M. Socioeconomic status and smoking: A review. Annals of the New York Academy of Sciences. 2012;1248(1):107–123. doi: 10.1111/j.1749-6632.2011.06202.x. [DOI] [PubMed] [Google Scholar]
- Juhn Y.J., Beebe T.J., Finnie D.M., Sloan J., Wheeler P.H., Yawn B. Development and initial testing of a new socioeconomic status measure based on housing data. Journal of Urban Health. 2011;88(5):933–944. doi: 10.1007/s11524-011-9572-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juhn Y.J., Sauver J.S., Katusic S., Vargas D., Weaver A., Yunginger J. The influence of neighborhood environment on the incidence of childhood asthma: A multilevel approach. Social Science & Medicine. 1982;60(11):2453–2464. doi: 10.1016/j.socscimed.2004.11.034. 2005. [DOI] [PubMed] [Google Scholar]
- Kaplan G.A., Keil J.E. Socioeconomic factors and cardiovascular disease: A review of the literature. Circulation. 1993;88(4 Pt 1):1973–1998. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- Khan A.M., Urquia M., Kornas K., Henry D., Cheng S.Y., Bornbaum C. Socioeconomic gradients in all-cause, premature and avoidable mortality among immigrants and long-term residents using linked death records in Ontario, Canada. 2017;71(7):625–632. doi: 10.1136/jech-2016-208525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N. Overcoming the absence of socioeconomic data in medical records: Validation and application of a census-based methodology. American Journal of Public Health. 1992;82(5):703–710. doi: 10.2105/ajph.82.5.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landis J.R., Koch G.G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- Lantz P.M., Golberstein E., House J.S., Morenoff J. Socioeconomic and behavioral risk factors for mortality in a national 19-year prospective study of U.S. adults. Social Science & Medicine. 1982;70(10):1558–1566. doi: 10.1016/j.socscimed.2010.02.003. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Kirby R.S., Sigler R.T., Hwang S.-S., Lagory M.E., Goldenberg R.L. A multilevel analysis of individual, household, and neighborhood correlates of intimate partner violence among low-income pregnant women in Jefferson county, Alabama. American Journal of Public Health. 2010;100(3):531–539. doi: 10.2105/AJPH.2008.151159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locker D., Ford J. Using area-based measures of socioeconomic status in dental health services research. Journal of Public Health Dentistry. 1996;56(2):69–75. doi: 10.1111/j.1752-7325.1996.tb02399.x. [DOI] [PubMed] [Google Scholar]
- Marra C.A., Lynd L.D., Harvard S.S., Grubisic M. Agreement between aggregate and individual-level measures of income and education: A comparison across three patient groups. BMC Health Services Research. 2011;11(1):69. doi: 10.1186/1472-6963-11-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mather T., Banks E., Joshy G., Bauman A., Phongsavan P., Korda R.J. Variation in health inequalities according to measures of socioeconomic status and age. Australian & New Zealand Journal of Public Health. 2014;38(5):436–440. doi: 10.1111/1753-6405.12239. [DOI] [PubMed] [Google Scholar]
- McHugh M.L. Interrater reliability: The kappa statistic. Biochemia Medica. 2012;22(3):276–282. [PMC free article] [PubMed] [Google Scholar]
- Meyer B., Mok W.K.C., Sullivan J. National Bureau of Economic Research, Inc; 2009. The under-reporting of transfers in household surveys: Its nature and consequences. [Google Scholar]
- Moin J.S., Moineddin R., Upshur R.E.G. Measuring the association between marginalization and multimorbidity in Ontario, Canada: A cross-sectional study. Journal of Comorbidity. 2018;8(1) doi: 10.1177/2235042X18814939. 2235042X18814939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore J.C., Welniak E.J. Income measurement error in surveys: A review. Journal of Official Statistics. 2000;16(4):331. [Google Scholar]
- Mustard C.A., Derksen S., Berthelot J.-M., Wolfson M. Assessing ecologic proxies for household income: A comparison of household and neighbourhood level income measures in the study of population health status. Health & Place. 1999;5(2):157–171. doi: 10.1016/s1353-8292(99)00008-8. [DOI] [PubMed] [Google Scholar]
- Narla N.P., Pardo-Crespo M.R., Beebe T.J., Sloan J., Yawn B., Williams A.R. Concordance between individual vs. Area-level socioeconomic measures in an urban setting. Journal of Health Care for the Poor and Underserved. 2015;26(4):1157–1172. doi: 10.1353/hpu.2015.0122. [DOI] [PubMed] [Google Scholar]
- Newacheck P.W., Hughes D.C., Stoddard J.J. Children's access to primary care: Differences by race, income, and insurance status. 1996;97(1):26–32. [PubMed] [Google Scholar]
- Norheim O.F., Jha P., Admasu K., Godal T., Hum R.J., Kruk M.E. Avoiding 40% of the premature deaths in each country, 2010-30: Review of national mortality trends to help quantify the UN sustainable development goal for health. Lancet (London, England) 2015;385(9964):239–252. doi: 10.1016/S0140-6736(14)61591-9. [DOI] [PubMed] [Google Scholar]
- OECD . OECD; Paris, France: 2011. Growing income inequalitiy in OECD countries: What drives it and how can policy tackle it? [Google Scholar]
- Pampalon R., Hamel D., Gamache P. A comparison of individual and area-based socio-economic data for monitoring social inequalities in health. Health Reports. 2009;20(4):85–94. [PubMed] [Google Scholar]
- Pardo-Crespo M.R., Narla N.P., Williams A.R., Beebe T.J., Sloan J., Yawn B.P. Comparison of individual-level versus area-level socioeconomic measures in assessing health outcomes of children in Olmsted County, Minnesota. Journal of Epidemiology & Community Health. 2013;67(4):305–310. doi: 10.1136/jech-2012-201742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pathirana T.I., Jackson C.A. Socioeconomic status and multimorbidity: A systematic review and meta-analysis. 2018;42(2):186–194. doi: 10.1111/1753-6405.12762. [DOI] [PubMed] [Google Scholar]
- Pichora E., Polsky J.Y., Catley C., Perumal N., Jin J., Allin S. Comparing individual and area-based income measures: Impact on analysis of inequality in smoking, obesity, and diabetes rates in Canadians. Canadian Journal of Public Health. 2018;109(3):410–418. doi: 10.17269/s41997-018-0062-5. 2003–2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett K.E., Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: A critical review. Journal of Epidemiology & Community Health. 2001;55(2):111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porta M. Oxford University Press; 2014. Ecological fallacy. [Google Scholar]
- Roblin D.W. Validation of a neighborhood SES index in a managed care organization. Medical Care. 2013;51(1):e1–8. doi: 10.1097/MLR.0b013e3182349b97. [DOI] [PubMed] [Google Scholar]
- Roos L.L., Wajda A. Record linkage strategies. Part I: Estimating information and evaluating approaches. Methods of Information in Medicine. 1991;30(2):117–123. [PubMed] [Google Scholar]
- Rosella L., Kornas K., Huang A., Bornbaum C., Henry D., Wodchis W.P. Accumulation of chronic conditions at the time of death increased in Ontario from 1994 to 2013. Health Affairs (Project Hope) 2018;37(3):464–472. doi: 10.1377/hlthaff.2017.1150. [DOI] [PubMed] [Google Scholar]
- Rotermann M. Evaluation of the coverage of linked Canadian Community Health Survey and hospital inpatient records. Health Reports. 2009;20(1):45. [PubMed] [Google Scholar]
- Ryu E., Juhn Y.J., Wheeler P.H., Hathcock M.A., Wi C.-I., Olson J.E. Individual housing-based socioeconomic status predicts risk of accidental falls among adults. Annals of Epidemiology. 2017;27(7):415–420. doi: 10.1016/j.annepidem.2017.05.019. e2. [DOI] [PubMed] [Google Scholar]
- Shiels M.S., Chernyavskiy P., Anderson W.F., Best A.F., Haozous E.A., Hartge P. Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: An analysis of death certificate data. Lancet (London, England) 2017;389(10073):1043–1054. doi: 10.1016/S0140-6736(17)30187-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin D.D., Svenson L.W., Man S.F. Do area-based markers of poverty accurately measure personal poverty? Canadian Journal of Public Health = Revue Canadienne de Sante Publique. 2001;92(3):184–187. doi: 10.1007/BF03404301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soobader M., LeClere F.B., Hadden W., Maury B. Using aggregate geographic data to proxy individual socioeconomic status: Does size matter? American Journal of Public Health. 2001;91(4):632–636. doi: 10.2105/ajph.91.4.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southern D.A., McLaren L., Hawe P., Knudtson M.L., Ghali W.A. Individual-level and neighborhood-level income measures: Agreement and association with outcomes in a cardiac disease cohort. Medical Care. 2005;43(11):1116–1122. doi: 10.1097/01.mlr.0000182517.57235.6d. [DOI] [PubMed] [Google Scholar]
- Statistics Canada . 2018. Canadian community health survey - annual component (CCHS) [Google Scholar]
- Stringhini S., Carmeli C., Jokela M., Avendaño M., Muennig P., Guida F. Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: A multicohort study and meta-analysis of 1·7 million men and women. The Lancet. 2017;389(10075):1229–1237. doi: 10.1016/S0140-6736(16)32380-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian S.V., Chen J.T., Rehkopf D.H., Waterman P.D., Krieger N. Comparing individual- and area-based socioeconomic measures for the surveillance of health disparities: A multilevel analysis of Massachusetts births, 1989-1991. American Journal of Epidemiology. 2006;164(9):823–834. doi: 10.1093/aje/kwj313. [DOI] [PubMed] [Google Scholar]
- Takahashi P.Y., Ryu E., Hathcock M.A., Olson J.E., Bielinski S.J., Cerhan J.R. A novel housing-based socioeconomic measure predicts hospitalisation and multiple chronic conditions in a community population. Journal of Epidemiology & Community Health. 2016;70(3):286. doi: 10.1136/jech-2015-205925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thacher T.D., Dudenkov D.V., Mara K.C., Maxson J.A., Wi C.-I., Juhn Y.J. The relationship of 25-hydroxyvitamin D concentrations and individual-level socioeconomic status. The Journal of Steroid Biochemistry and Molecular Biology. 2020;197:105545. doi: 10.1016/j.jsbmb.2019.105545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wi C.-I., St Sauver J.L., Jacobson D.J., Pendegraft R.S., Lahr B.D., Ryu E. Ethnicity, socioeconomic status, and health disparities in a mixed rural-urban US community—Olmsted county, Minnesota. Mayo Clinic Proceedings. 2016;91(5):612–622. doi: 10.1016/j.mayocp.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.