Highlights
-
•
Dosimetric benefits to the penile bulb was seen in patients treated with IGRT and reduced CTV-PTV margins.
-
•
Patients who had a lower planned dose to the penile bulb reported less erectile dysfunction.
-
•
A threshold mean penile bulb dose for erectile dysfunction was determined to around 20 Gy.
Keywords: Prostate, Image-guided radiotherapy, Erectile dysfunction, Penile bulb
Abstract
Background and purpose
The penile bulb (PB) dose may be critical in development of post prostate radiotherapy erectile dysfunction (ED). This study aimed to generate PB dose constraints based on dose-volume histograms (DVHs) in patients treated with prostate radiotherapy, and to identify clinical and dosimetric parameters that predict the risk of ED post prostate radiotherapy.
Materials and methods
Penile bulb DVHs were generated for 276 patients treated within the randomised IGRT substudy of the multicentre randomised trial, CHHiP. Incidence of ED in relation to dose and randomised IGRT groups were evaluated using Wilcoxon rank sum, Chi-squared test and atlases of complication incidence. Youden index was used to find dose-volume constraints that discriminated for ED. Multivariate analysis (MVA) of effect of dosimetry, clinical and patient-related variables was performed.
Results
Reduced treatment margins using IGRT (IGRT-R) produced significantly reduced mean PB dose compared with standard margins (IGRT-S) (median: 25 Gy (IGRT-S) versus 11 Gy (IGRT-R); p < 0.0001). Significant difference in both mean (median: 23 Gy (ED) vs. 18 Gy (no ED); p = 0.011) and maximum (median: 59 Gy (ED) vs. 52 Gy (no ED); p = 0.018) PB doses between those with and without clinician reported ED were identified. Mean PB dose cut-point for ED was derived at around 20 Gy. On MVA, PB mean dose and age predicted for impotence.
Conclusion
PB dose appears predictive of post-radiotherapy ED with calculated threshold mean dose of around 20 Gy, substantially lower than published recommendations. IGRT-R enables favourable PB dosimetry and can be recommended provided prostate coverage is not compromised.
1. Introduction
The current management options for localised prostate cancer enable excellent local tumour control with long term survival [1]. However, prostate cancer and its treatment are the leading cause of cancer years lived with a disability [2]. Evaluating treatment related toxicities are essential to inform patient decisions. There are limited data on the association of erectile dysfunction (ED) to external beam radiotherapy for prostate cancer, despite ED being the most commonly reported toxicity [3]. ED can affect physical and psychosocial health and may profoundly impact the quality of life of patients and their partners [4], [5], [6].
Pelvic radiation-induced complications have been shown to be dose and volume dependent and have been extensively explored for bowel and urinary toxicity [7]. For ED post-radiotherapy there are uncertainties surrounding the most relevant normal tissues and the multifactorial causes of ED other than those attributable to the treatment. The penile bulb (PB) has attracted most interest as a critical normal tissue structure.
Treatment planning dose objectives for the PB have been varied and inconsistent within the literature [8] and developed from data using older prostate radiotherapy techniques and dose fractionation schedules. More recently, prostate cancer has been found to have radiobiological features atypical of most other cancers and hypofractionation has been hypothesised as a method to improve the therapeutic ratio [9], [10], [11]. In the largest randomised trial worldwide comparing conventional and hypofractionated prostate radiotherapy (CHHiP), the long term side effects were similar with 2 Gy and 3 Gy fractionation schedules [9]. Recommended PB dose constraints for hypofractionated schedules are not established [12] and those for standard fractionations within the QUANTEC papers need to be substantiated using data from patients treated with modern radiotherapy techniques [3].
The primary aim of this study was to determine whether relationships exist between reduced target volume margins, PB dose and ED as assessed by clinician reported outcomes using both conventional and hypofractionated radiotherapy. The secondary aims were to derive radiotherapy dose constraints that could be implemented into radiotherapy planning to potentially decrease incidence of ED. Additionally, multivariate analysis (MVA) was performed to identify clinical and dosimetric parameters that predict risk of ED in patients treated with prostate image guided radiotherapy (IGRT).
2. Materials and methods
The CHHiP (Conventional or Hypofractionated High-dose Intensity Modulated Radiotherapy in Prostate Cancer; CRUK/06/016) study is a multicentre randomised controlled trial which used a three-arm design comparing conventionally fractionated radiotherapy (74 Gy in 37 2 Gy fractions (f)) with high-quality radiation techniques delivered using two different 3 Gy hypofractionated radiotherapy dose schedules (60 Gy in 20f and 57 Gy in 19f) [9].
A multicentre randomised non-blinded IGRT substudy received approval by Central London REC1 Research Ethics Committee (10/H0718/31) on 25th June 2010 and was implemented within the main CHHiP trial protocol (v 9.0). This substudy assessed acute and late toxicity associated with daily online IGRT and the feasibility of daily online IGRT delivery in a national trial. In the main CHHiP trial patients were randomised 1:1:1 to the fractionation schedules. Patients consenting to the IGRT substudy were also randomly allocated by minimisation, to (a) no daily online IGRT (i.e. centre standard verification methods) – using standard treatment planning margins, (b) daily online IGRT using standard treatment planning margins (IGRT-S), or (c) daily online IGRT with reduced treatment planning margins (IGRT-R). Centres had the option to randomise among all 3 options or alternatively a versus b or b versus c to accommodate existing centre experience using IGRT (Figs. E1, E2). The radiotherapy planning techniques have been previously described [13], [14]. Target volume dose coverage was achieved using a simultaneous integrated boost technique with mandatory and optimal normal tissue dose constraints (Table E1).
The IGRT substudy commenced after the main CHHiP patient reported outcome (PRO) study had closed, an additional cross-sectional questionnaire study was approved by ethics (14/SW/1071) in September 2014.
2.1. Data collection
Patient demographic data was collected at trial entry. Clinician reported (CRO) ED, measured using Royal Marsden Hospital (RMH) erectile potency (EP) grading system, was prospectively recorded at baseline, pre-radiotherapy and at 6 monthly intervals up until 2 years post-radiotherapy and thereafter annually. Grade 0 represented normal erection, grade 1 decreased erectile potency and grade 2 absent erectile function. Clinician reported Grade 2 EP was used as a toxicity endpoint, and patients were excluded from the analysis if baseline scores were reported as Grade 2. In the PRO substudy, data was collected at a single time point (at least 3 years from completing treatment) and included the use of the Expanded Prostate Cancer Index Composite (EPIC) questionnaire (EPIC-26 for sexual and hormonal domains) [15]. A cut-point of 33 for EPIC-26 sexual summary group score [16] was used as an endpoint.
Dosimetry information, including full treatment planning data, was uploaded to a dedicated software platform, VODCA (MSS Inc, Hagendorn, Switzerland).
2.2. Penile bulb dosimetric analysis
PB was contoured retrospectively by one clinical oncologist (JM) (Fig. E3) combining RTOG consensus panel atlas for pelvic normal tissue contouring guidelines [17], well-established anatomic boundaries [18] and DUE-01 study guidelines [19]. The lateral borders of the PB included the paired crura, anteriorly the corpus spongiosum and posteriorly the levator ani. The PB was outlined posterior to the urethra, with a round shape. The anterior border of the PB contour in the most cranial slice was used to guide the anterior border on the more caudal slices. Three-dimensional physical dose distributions were converted into equivalent dose in 2 Gy/f (EQD2) distributions by applying Withers formula [20] with α/β = 3 Gy [12], [21] to each dose grid voxel. EQD2-based and physical dose-based PB dose-volume histogram data were exported from the analysis software.
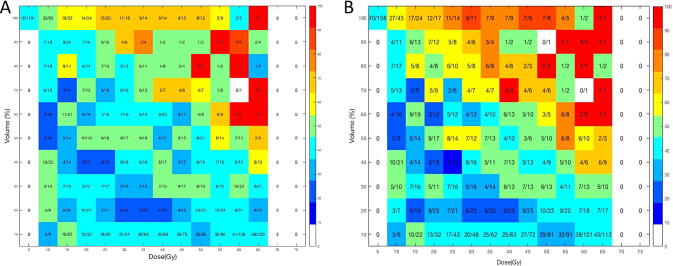
Dosimetric atlases of complication incidence (ACI) [22] were created using Matlab version R2016a (Mathworks, Natick, MA). ACI are a method of summarising toxicity and cumulative dose-volume data for an organ of interest, displayed as a dose-volume grid. Each box within the atlas describes a small range of dose and volume (5 Gy and 10%, respectively) and presents a numeric fraction (i.e. denominator = patients whose DVH falls within the range of dose and volume of the box; numerator = number of patients whose DVH falls within the range of dose and volume of the box and who experienced grade 2 EP). PB mean, maximum dose and volume of PB receiving at least a defined dose were summarised.
2.3. Statistical methods
PB dosimetry data were compared between patients with or without the toxicity endpoint using Wilcoxon rank sum with continuity correction. Exploratory analysis compared ED between the randomised groups using Chi-squared test of independence. Dose-volume constraints were derived using receiver operating characteristic (ROC) analysis for individual dose levels (EQD2 and physical dose) combined with toxicity data. The ‘Youden index’, J [23] was used to find the volume threshold for each dose level and the mean and maximum threshold doses that best discriminated between patients with or without toxicity. A dose metric was considered to be significantly better than chance at discriminating between patients with and without toxicity if the lower 95% confidence interval (CI) of the area under the ROC curve was greater than 0.5. The incidence of toxicity in patients who met the derived constraints was compared with patients who failed the constraints.
A correlation matrix was produced to check for high correlations between potential prognostic factors, in particular DVH parameters. Variables with Pearson correlation coefficients ≥0.80 were combined into a single variable (mean dose) to avoid the problem of multicollinearity, which may negatively affect generalisability of the model. PB mean and maximum dose and clinical variables listed in Table E8 were included in logistic regression models to predict RMH Grade 2 EP. To develop the prediction model, univariate logistic regression analysis assessed crude effect of each candidate variable on the defined endpoint of RMH Grade 2 EP at 2 years. 1000 bootstraps were used for each analysis. Multivariable prediction models used the variables significant from univariate analysis. Normal tissue complication probability (NTCP) model was developed using multivariate logistic regression (R Development Core Team, R: A language and Environment for statistical computing, Version 3.3.1). Models were fitted using the packages glm [24] and leaps with 1000 bootstrap samples of equal size drawn at random with replacement. Models were fitted using logistic regression of the form Probability = eA(x)/1 + eA(x) where A(x) = β0 + nxn, xn are the variables included in the model and βn are the associated regression coefficients. The final models to predict RMH Grade 2 EP were assessed using the area under the ROC (AUC) and the goodness-of-fit of the chosen NTCP model was evaluated by the Hosmer-Lemeshow test [25]. The chosen NTCP model for RMH Grade 2 EP was externally validated using a random patient cohort from the main CHHiP trial where the PB had been outlined by a single clinician (AW) using the same PB contouring guidelines.
3. Results
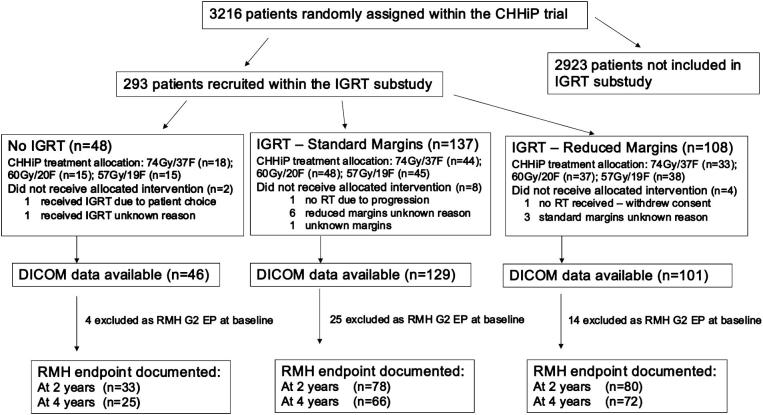
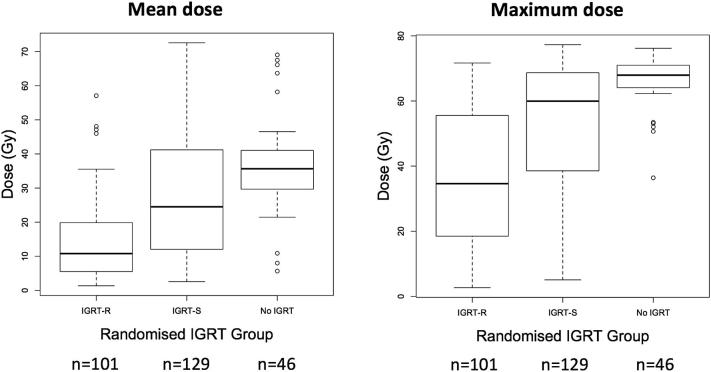
Baseline characteristics of the 276 patients analysed are detailed in Table 1 and available data summarised in Fig. 1. PB volume was similar (p = 0.71) across randomised groups: median (IQR) was 6.3 (4.8–7.6) cm3 in the no IGRT group, 6.0 (4.9–7.8) cm3 in the IGRT-S group and 6.1 (4.8–7.6) cm3 in the IGRT-R group. There were significant PB dose differences between patients treated with IGRT-S and IGRT-R for both mean and maximum PB dose (p < 0.0001). Median values of mean (EQD2, alpha/beta 3 Gy) PB doses were 35 Gy, 25.3 Gy and 10.8 Gy and of maximum doses 68.1 Gy, 61.1 Gy and 36.9 Gy for no IGRT, IGRT-S and IGRT-R respectively (Fig. 2).
Table 1.
Baseline demographics, clinical characteristics, and treatment details by randomised group.
| No IGRT N = 46 n (%) |
IGRT – S N = 129 n (%) |
IGRT – R N = 101 n (%) |
Main CHHiP trial N = 3216 n (%) |
|
|---|---|---|---|---|
| Age at registration (years) | ||||
| Median (IQR) | 70 (66–73) | 72 (66–75) | 71 (67–75) | 69 (44–85) |
| T stage (clinical assessment) | ||||
| T1 | 14 (30) | 41 (32) | 40 (40) | 1170 (36) |
| T2 | 27 (59) | 80 (62) | 54 (53) | 1766 (55) |
| T3 | 5 (11) | 8 (6) | 7 (7) | 277 (9) |
| PSA (pre-hormone treatment) (ng/ml) | ||||
| Median (IQR) | 9.5 (6.6–13.8) | 9.6 (6.5–12.5) | 8 (6.8–11.3) | 10 (7–15) |
| NCCN Risk group | ||||
| Low | 2 (4) | 13 (10) | 17 (17) | 484 (15) |
| Medium | 36 (78) | 104 (81) | 75 (74) | 2347 (73) |
| High | 8 (17) | 12 (9) | 9 (9) | 385 (12) |
| CHHiP treatment allocation | ||||
| 74 Gy/37 Fr | 16 (35) | 41 (32) | 30 (29) | 1065 (33) |
| 60 Gy/20 Fr | 15 (32.5) | 45 (35) | 35 (35) | 1074 (33) |
| 57 Gy/19 Fr | 15 (32.5) | 43 (33) | 36 (36) | 1077 (34) |
| Hormone therapy | ||||
| None | 1 (2) | 3 (2) | 4 (4) | 90 (3) |
| Bicalutamide monotherapy | 6 (13) | 29 (23) | 21 (21) | 403 (13) |
| LHRH agonist | 39 (85) | 96 (74) | 74 (73) | 2700 (83) |
| Unknown | 0 (0) | 1 (1) | 2 (2) | 9 (<1) |
| Duration of hormone therapy | ||||
| Median (IQR) in days | 107 (94–161) | 145 (112–178) | 147 (121–161) | 168 (133–196) |
| Diabetes | ||||
| Yes | 6 (13) | 14 (11) | 10 (10) | 342 (11) |
| No | 40 (87) | 107 (83) | 83 (82) | NA |
| Unknown | 8 (6) | 8 (8) | NA | |
| Hypertension | ||||
| Yes | 20 (43) | 53 (41) | 33 (33) | 1276 (40) |
| No | 25 (54) | 68 (53) | 60 (59) | NA |
| Unknown | 1 (2) | 8 (6) | 8 (8) | NA |
NCCN: National Comprehensive Cancer Network.
Fig. 1.
Trial profile (*endpoints assessable means those patients with DICOM data and complete endpoint data for evaluation). DICOM: Digital imaging and Communications in medicine and is a standard for storing and transmitting medical images; F: fractions.
Fig. 2.
Boxplots illustrating the dose distribution for the calculated dose (Gy) of the penile bulb by IGRT group. IGRT: image guided radiotherapy; IGRT-R: IGRT with reduced margins; IGRT-S: IGRT with standard margins.
3.1. Erectile potency
43/276 (16%) patients were excluded due to RMH Grade 2 EP at baseline. Of the remaining 233 patients, 191 patients reported year 2 RMH EP score. RMH Grade 2 EP at 2 years after radiotherapy was reported in 81/191 (42%) patients. 11/33 patients (33%) treated with no-IGRT had clinician reported ED compared to 37/78 (47%) in the IGRT-S and 33/80 (41%) in the IGRT-R groups (not significantly different, p = 0.37). The median (IQR) testosterone level at 12 months post randomisation in patients with Grade 2 EP was 9.9 (5.9–13.7)nmol/l compared with 12.2 (7.9–14.6)nmol/l in those reporting Grade 0/1 EP. Patient and clinical factors are grouped according to 2 year RMH EP score (Table E2). At 4 years, there were 70/163 (43%) patients with RMH Grade 2 EP, 31/66 (47%) were IGRT-S and 28/72 (39%) IGRT-R patients. Of those with Grade 2 EP at 2 years, 40/81 reported Grade 2 EP, 15/81 Grade 0 or 1 EP and the status unknown for 26 patients at 4 years. There were 146 patients where the RMH EP status at year 2 and year 4 were recorded. Of these 45/146 (31%) patients had Grade 0 EP at 2 years, with 24/45 (53%) patients retaining Grade 0 EP at 4 years, 17/45 (38%) reporting Grade 1 EP and 4/45 (9%) Grade 2 EP at this timepoint.
3.2. Relationship of PB dose to erectile function
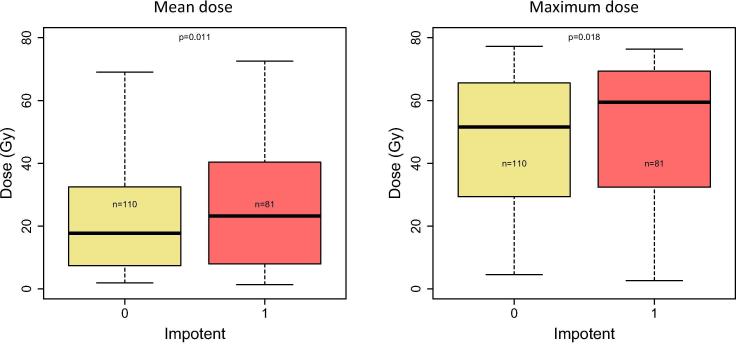
Mean and maximum PB doses were significantly lower in patients with less severe ED post-radiotherapy. In patients with Grade 2 EP, their median (IQR) mean and maximum PB doses were 23 Gy (8–40 Gy) and 59 Gy (32–69 Gy) and in those patients with Grade 0/1 EP, it was 18 Gy (8–32 Gy) and 52 Gy (30–66 Gy) respectively (Fig. 3). ACI demonstrate the impact of PB dose and volume on erectile potency and shows a greater incidence of impotence at 2 years in patients whose DVH fell within the top right of the atlas compared to those within the bottom left, suggesting a PB dose-volume response (Fig. 4). This association was also seen at year 3 and 4 endpoints (Fig. E4). The dose volume histogram profiles distinguishing between those patients with and without RMH Grade 2 EP at 2 years show the association of Grade 2 EP with higher PB volumes receiving higher doses (Fig. E5). Mean and maximum doses were 27.4 (11.1–38.7)Gy and 61.8 (42.6–69.0)Gy for patients with an EPIC-26 sexual summary group score ≤ 33 and 14.0 (6.8–21.8)Gy and 43.0 (20.5–63.5)Gy for patients with EPIC-26 sexual summary group score > 33 (p = 0.001; Table E3). Median PB DVH according to EPIC-26 sexual domain average standardised scores and ACI (Figs. E6/E7) further support a PB dose-volume response.
Fig. 3.
Boxplots summarising the impact of penile bulb dosimetry on the defined toxicity endpoints using clinician (RMH) reported outcomes. Defined endpoints: RMH Grade 2 EP; 0 = no; 1 = yes. p values determined by Wilcoxon rank sum.
Fig. 4.
Atlases of complication incidence for RMH Grade 2 erectile potency at 2 years in (A) all patients with recorded erectile potency at 2 years and (B) patients treated with IGRT (standard and reduced margins) with recorded erectile potency at 2 years. Dose (Gy) is the equivalent dose in 2 Gy/F using alpha/beta ratio of 3 Gy. The colour of the box is determined by the fractional incidence of the endpoint, with the orange to red representing 70–100%. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3.3. Derivation of dose constraints
Dose-volume constraints for ED using RMH scoring system over the range of 10–70 Gy were derived (Table E4). The dose constraints (EQD2, alpha/beta 3 Gy) derived for PB mean dose for CRO (RMH) severe ED was 20 Gy (AUC (95%CI): 0.61(0.53–0.70)). The derived constraint for maximum PB dose was 56 Gy (AUC (95%CI): 0.60(0.52–0.69)) for CRO (RMH). Patients who met these mean and maximum dose constraints were less likely to have RMH Grade 2 EP (OR: 0.38; 95%CI, 0.21–0.71 and 0.44; 95%CI, 0.24–0.82 respectively; Table E5). Similar derived PB mean dose constraints were seen for PRO (EPIC-26 sexual domain) severe ED of 22 Gy (AUC (95% CI): 0.66(0.57–0.74)) and maximum PB dose of 55 Gy (AUC (95% CI): 0.57(0.65–0.74)); Table E6.
Dose-volume constraints were also derived using physical dose and RMH EP scoring system. Analysis from patients whose prescription dose was 74 Gy had a statistically significant derived mean dose constraint of 24 Gy in 37 fractions (AUC (95% CI): 0.71(0.58–0.86), p = 0.002). There was no statistically significant constraint using physical dose for patients prescribed 3 Gy per fraction (Table E7).
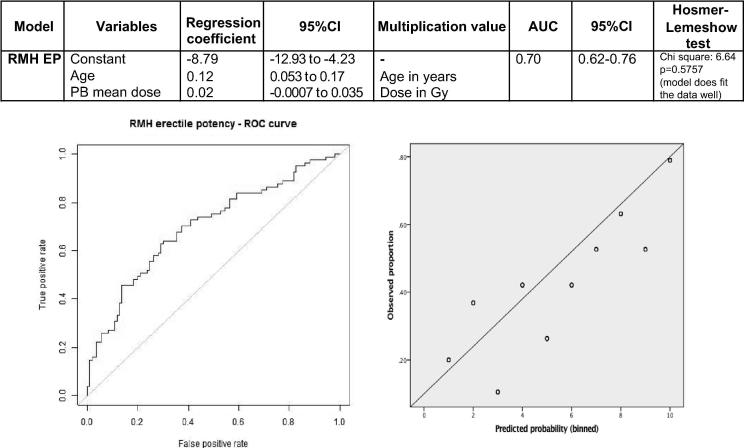
3.4. Development of NTCP model
Univariate analysis demonstrated an association between age, diabetes, NCCN risk group and PB (EQD2, alpha/beta 3 Gy) mean dose and impotence using the RMH EP grading scale (Table E8). Multivariate logistic regression analysis including these variables showed a relationship between PB mean dose and age (AUC (95%CI): 0.70(0.62–0.76)); (Fig. 5). External validation of this model for ED using the RMH EP scale was performed using data from a random cohort of 232 patients treated within the main CHHiP trial (Table E9). 48 patients were not included as they had Grade 2 RMH EP at baseline, therefore 184 patients were evaluated in the NTCP model. The calculated AUC (95%CI) was 0.68(0.60–0.76); Fig. E8.
Fig. 5.
(A) Chosen model variables, regression coefficient, multiplication values for the variables included in the model and metrics exploring the performance of the model. (B) ROC curve obtained applying model for RMH Grade 2 EP and calibration plot for internal validation. The circles represent the Hosmer-Lemeshow groups, the solid line represents the identity line.
4. Discussion
ED is a critical health-related quality of life outcome in men treated for prostate cancer and the potential structures implicated in ED need to be determined. Previous data have suggested PB dose is associated with radiotherapy-induced ED [3], [26]. Modern radiotherapy techniques enable dose sculpting, causing steep dose gradients at the edge of the target volume (i.e. region of the PB) and IGRT improves treatment accuracy which permits reduced radiotherapy margins. The CHHiP IGRT trial provides a unique dataset to determine effect of PB dose on erectile function.
We have demonstrated a relationship between reduced PTV margins enabled by IGRT and PB dose and the relationship between PB dose and ED using CRO and PRO. Dose constraints for the PB have been derived which are generalisable and could be implemented in radiotherapy planning. A consistent mean dose constraint of around 20 Gy equivalent dose in 2 Gy per fraction (Biologically Effective Dose = 33.6 Gy using α/β = 3 Gy) was found. When using the physical dose data for 2 Gy fractionation, a statistically significant mean dose constraint of 24 Gy was calculated, with a suggestion of a mean dose constraint of 22 Gy for 3 Gy fractionation (Table E7). These constraints are similar to the PB mean dose threshold of 20 Gy determined in a smaller cohort (n = 41) treated with moderate hypofractionation (around 2.5 Gy/f) [12]. However, these thresholds are a significant reduction from the mean dose limit of 50 Gy recommended in QUANTEC [3], and the 50 Gy limit to 90% of PB suggested in the MRC RT01 trial [26]. In our dataset, less than 7% of patients had PB mean doses of >50 Gy. The more favourable dose distributions in the present patient cohort may have enabled identification of lower discriminatory thresholds. Other potential reasons for these significant differences within the literature may include variation in penile bulb definition and contouring, different fractionation schedules and treatment techniques. In this study, we used a single outlining clinician for hypotheses generating and validation cohorts to remove inter-observer variability inherent in PB contouring, which has been shown to impact on DVH parameters [19]. Fractionation schedules were protocol defined and IMRT +/− IGRT was used in all cases. Our results are in accord with an interim analysis of the DUE-01 study which found maximum PB dose as a predictive factor for ED [21]. However, due to the small PB volume and potential substantial impact inter-observer contouring variability has on dose-volume parameters [19], we suggest that mean PB dose is likely to be a more robust metric for use in radiotherapy planning.
ED post-radiotherapy is multifactorial and although PB dose is associated with ED, it may be a surrogate for surrounding structures, such as neurovascular bundles and internal pudendal arteries, which are not easily visualised on CT, but can be seen on MRI [27]. Further studies using MR planning will enable interrogation of these structures to determine associated dose volume relationships with ED. Although the PB is best identified on MRI, it is visible on CT and, hence, a recognised structure of interest within the RTOG contouring atlas [17]. The introduction of MRI-based treatment planning and image guidance permits more accurate identification of the prostate apex and PB during treatment planning and delivery, which may enable PB sparing. Additionally, although planning target volume coverage should not be jeopardised, the creation of PB as an objective function for prostate radiotherapy optimisation should be considered. This goal appears feasible as around 50% of patients within the whole cohort achieved a PB mean dose < 20 Gy, approaching 80% for patients within the IGRT-R group.
Radiotherapy dose constraints provide a practical means of using dose–response relationships to inform radiotherapy planning in an evidence-based manner. A dose threshold constraint is the best cut point in the data, being used as a proxy for the whole dose-volume complication distribution. Further benefit may be seen reducing the mean PB dose as far as possible, without compromising other aspects of the treatment plan.
Limitations of this study include that the sub-study was not powered to compare the randomised groups and that there was only a single time-point assessment of PRO. However, this is the largest reported multicentre series of patients evaluating ED post-radiotherapy using both CRO and PRO. Results have shown significant and consistent association between PB dose and ED independent of scoring system, strengthening validity of these findings.
To our knowledge this predictive model for EBRT induced erectile dysfunction is the first to include PB dose. The derived model also included age, which is an established risk factor for ED after treatment [28], [29]. The discriminative power of the final multivariable model was good, with AUC = 0.70. External validation of the model showed moderate discriminative power (AUC = 0.68), giving a very favourable optimism factor with this model (0.02). However, the similar radiotherapy treatment characteristics and inclusion/exclusion criteria for both cohorts may partly explain this concordance in model performance described. Further analyses with additional datasets should be pursued.
ED is multifactorial and this study has explored limited clinical factors, with patients who reported baseline impairment being excluded from analysis. In addition, the median 12 month testosterone levels in those patients with reported RMH Grade 2 EP was above the postulated threshold of 8 nmol/l, where the relationship between testosterone and sexual functioning is very low [30]. Larger studies interrogating role of PB dose in post-radiotherapy ED should be encouraged, with further refinement and validation of clinical prediction models. The aim will be to enable personalised discussion of the risks for radiation-related ED and support clinical decision-making.
Funding
Cancer Research UK, Department of Health, and the National Institute for Health Research Cancer Research Network.
Conflict of interest
None.
Acknowledgements
We thank the patients and all investigators and research support staff at the participating centres, Trial Management Group members past and present and the Independent Data Monitoring Committee (Matthew Sydes [chair], Christopher Tyrell, Peter Barrett-Lee and, previously, Peter Hoskin, Christopher Nutting) and Trial Steering Committee (Anthony Zietman [chair], Soren Bentzen, Vivian Cosgrove, Heather Payne) for overseeing the trial. We acknowledge support of Cancer Research UK (C8262/A7253, C1491/A9895, C1491/A15955, SP2312/021), the National Institute for Health Research (NIHR) Cancer Research Network, and DD, JM, SG, CG, EH acknowledge NHS funding to the NIHR Biomedical Research Centre at the Royal Marsden NHS Foundation Trust and The Institute of Cancer Research, London which specifically funded the PRO study (A84).
ISRCTN: 97182923
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ctro.2019.12.006.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Hamdy F.C., Donovan J.L., Lane J.A., Mason M., Metcalfe C., Holding P. 10-Year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med [Internet] 2016;375(15):1415–1424. doi: 10.1056/NEJMoa1606220. http://www.nejm.org/doi/10.1056/NEJMoa1606220 Available from. [DOI] [PubMed] [Google Scholar]
- 2.Soerjomataram I., Lortet-Tieulent J., Parkin D.M., Ferlay J., Mathers C., Forman D. Global burden of cancer in 2008: a systematic analysis of disability-adjusted life-years in 12 world regions. Lancet. 2012;380(9856):1840–1850. doi: 10.1016/S0140-6736(12)60919-2. [DOI] [PubMed] [Google Scholar]
- 3.Roach M., III, Nam J., Gagliardi G., El Naqa I., Deasy J.O., Marks L.B. Radiation dose-volume effects and the penile bulb. Int J Radiat Oncol Biol Phys [Internet] 2010;76(3 Suppl):S130–S134. doi: 10.1016/j.ijrobp.2009.04.094. http://www.ncbi.nlm.nih.gov/pubmed/20171507 Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feldman H.A., Goldstein I., Hatzichristou D.G., Krane R.J., McKinklay J.B. Impotence and its medical and physiological correlates: results of the Massacheusetts male aging study. J Urol. 1994;151:54–61. doi: 10.1016/s0022-5347(17)34871-1. [DOI] [PubMed] [Google Scholar]
- 5.Fisher W.A., Eardley I., McCabe M., Sand M. Erectile dysfunction (ED) is a shared sexual concern of couples I: couple conceptions of ED. J Sex Med. 2009;6(10):2746–2760. doi: 10.1111/j.1743-6109.2009.01457.x. [DOI] [PubMed] [Google Scholar]
- 6.Salonia A., Castagna G., Saccà A., Ferrari M., Capitanio U., Castiglione F. Is erectile dysfunction a reliable proxy of general male health status? The case for the international index of erectile function-erectile function domain. J Sex Med. 2012;9(10):2708–2715. doi: 10.1111/j.1743-6109.2012.02869.x. [DOI] [PubMed] [Google Scholar]
- 7.Fiorino C., Valdagni R., Rancati T., Sanguineti G. Dose-volume effects for normal tissues in external radiotherapy: pelvis. Radiother Oncol [Internet] 2009;93(2):153–167. doi: 10.1016/j.radonc.2009.08.004. http://www.ncbi.nlm.nih.gov/pubmed/19765845 Available from. [DOI] [PubMed] [Google Scholar]
- 8.Rivin del Campo E., Thomas K., Weinberg V., Roach M. Erectile dysfunction after radiotherapy for prostate cancer: a model assessing the conflicting literature on dose-volume effects. Int J Impot Res [Internet] 2013;25(5):161–165. doi: 10.1038/ijir.2013.28. http://www.ncbi.nlm.nih.gov/pubmed/23784555 Available from. [DOI] [PubMed] [Google Scholar]
- 9.Dearnaley D., Syndikus I., Mossop H., Khoo V., Birtle A., Bloomfield D. Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: 5-year outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol [Internet] 2016;17(8):1047–1060. doi: 10.1016/S1470-2045(16)30102-4. http://linkinghub.elsevier.com/retrieve/pii/S1470204516301024%5Cnhttp://www.ncbi.nlm.nih.gov/pubmed/27339115%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4961874 Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee W.R., Dignam J.J., Amin M.B., Bruner D.W., Low D., Swanson G.P. Randomized phase III noninferiority study comparing two radiotherapy fractionation schedules in patients with low-risk prostate cancer. J Clin Oncol. 2016;34(20):2325–2332. doi: 10.1200/JCO.2016.67.0448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pollack A., Walker G., Horwitz E.M., Price R., Feigenberg S., Konski A.A. Randomized trial of hypofractionated external-beam radiotherapy for prostate cancer. J Clin Oncol [Internet] 2013;31(31):3860–3868. doi: 10.1200/JCO.2013.51.1972. http://www.ncbi.nlm.nih.gov/pubmed/24101042 Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McDonald A.M., Baker C.B., Shekar K., Popple R.A., Clark G.M., Yang E.S. Reduced radiation tolerance of penile structures associated with dose-escalated hypofractionated prostate radiotherapy. Urology. 2014;84(6):1383–1388. doi: 10.1016/j.urology.2014.07.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.South C.P., Khoo V.S., Naismith O., Norman A. Dearnaley DP. A comparison of treatment planning techniques used in two randomised UK external beam radiotherapy trials for localised prostate cancer. Clin Oncol (R Coll Radiol) [Internet] 2008;20(1):15–21. doi: 10.1016/j.clon.2007.10.012. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18054471 Available from: [DOI] [PubMed] [Google Scholar]
- 14.Khoo V.S., Dearnaley D.P. Question of dose, fractionation and technique: ingredients for testing hypofractionation in prostate cancer–the CHHiP trial. Clin Oncol (R Coll Radiol) [Internet] 2008;20(1):12–14. doi: 10.1016/j.clon.2007.10.008. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18036791 Available from: [DOI] [PubMed] [Google Scholar]
- 15.Szymanski K.M., Wei J.T., Dunn R.L., Sanda M.G. Development and validation of an abbreviated version of the expanded prostate cancer index composite instrument for measuring health-related quality of life among prostate cancer survivors. Urology [Internet] 2010;76(5):1245–1250. doi: 10.1016/j.urology.2010.01.027. http://www.ncbi.nlm.nih.gov/pubmed/20350762 Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wheat J.C., Hedgepeth R.C., He C., Zhang L., Wood D.P. Clinical interpretation of the expanded prostate cancer index composite-short form sexual summary score. J Urol. 2009;182(6):2844–2849. doi: 10.1016/j.juro.2009.08.088. [DOI] [PubMed] [Google Scholar]
- 17.Gay H.A., Barthold H.J., O’Meara E., Bosch W.R., El Naqa I., Al-Lozi R. Pelvic normal tissue contouring guidelines for radiation therapy: a radiation therapy oncology group consensus panel atlas. Int J Radiat Oncol Biol Phys [Internet] 2012;83(3):e353–e362. doi: 10.1016/j.ijrobp.2012.01.023. http://www.ncbi.nlm.nih.gov/pubmed/22483697 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wallner K.E., Merrick G.S., Benson M.L., Butler W.M., Maki J., Tollenaar B.G. Penile bulb imaging. Int J Radiat Oncol Biol Phys [Internet] 2002;53(4):928–933. doi: 10.1016/s0360-3016(02)02805-5. http://www.ncbi.nlm.nih.gov/pubmed/12095559 Available from: [DOI] [PubMed] [Google Scholar]
- 19.Perna L., Cozzarini C., Maggiulli E., Fellin G., Rancati T., Valdagni R. Inter-observer variability in contouring the penile bulb on CT images for prostate cancer treatment planning. Radiat Oncol [Internet] 2011;6:123. doi: 10.1186/1748-717X-6-123. http://www.ncbi.nlm.nih.gov/pubmed/21943002 Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Withers H.R., Thames H.D., Peters L.J. A new isoeffect curve for change in dose per fraction. Radiother Oncol. 1983;1(2):187–191. doi: 10.1016/s0167-8140(83)80021-8. [DOI] [PubMed] [Google Scholar]
- 21.Cozzarini C., Rancati T., Badenchini F., Palorini F., Avuzzi B., Claudio, Baseline status and dose to the penile bulb predict impotence 1 year after radiotherapy for prostate cancer. Strahlenther Onkol. 2016;192:297–304. doi: 10.1007/s00066-016-0964-1. [DOI] [PubMed] [Google Scholar]
- 22.Jackson A., Yorke E.D., Rosenzweig K.E. The atlas of complication incidence: a proposal for a new standard for reporting the results of radiotherapy protocols. Semin Radiat Oncol. 2006;16(4):260–268. doi: 10.1016/j.semradonc.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 23.Youden W.J. Index for rating diagnostic tests. Cancer. 1950;3(1):32–35. doi: 10.1002/1097-0142(1950)3:1<32::aid-cncr2820030106>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 24.Morgan J.A., Tatar J.F. Calculation of the residual sum of squares for all possible regressions. Technometrics [Internet] 1972;14(2):317–325. http://links.jstor.org/sici?sici=0040-1706(197205)14:2%3C317:COTRSO%3E2.0.CO;2-7 Available from. [Google Scholar]
- 25.Hosmer D.W., Hosmer T., Le Cessie S., Lemeshow S. A comparison of goodness-of-fit tests for the logistic regression model. Stat Med. 1997;16(9):965–980. doi: 10.1002/(sici)1097-0258(19970515)16:9<965::aid-sim509>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 26.Mangar S.A., Sydes M.R., Tucker H.L., Coffey J., Sohaib S.A., Gianolini S. Evaluating the relationship between erectile dysfunction and dose received by the penile bulb: using data from a randomised controlled trial of conformal radiotherapy in prostate cancer (MRC RT01, ISRCTN47772397) Radiother Oncol [Internet] 2006;80(3):355–362. doi: 10.1016/j.radonc.2006.07.037. http://www.ncbi.nlm.nih.gov/pubmed/16949694 Available from. [DOI] [PubMed] [Google Scholar]
- 27.Rabbani F., Stapleton A.M., Kattan M.W., Wheeler T.M., Scardino P.T. Factors predicting recovery of erections after radical prostatectomy. J Urol. 2000;164(6):1929–1934. [PubMed] [Google Scholar]
- 28.Hollenbeck B.K., Dunn R.L., Wei J.T., McLaughlin P.W., Han M., Sanda M.G. Neoadjuvant hormonal therapy and older age are associated with adverse sexual health-related quality-of-life outcome after prostate brachytherapy. Urology [Internet] 2002;59(4):480–484. doi: 10.1016/s0090-4295(01)01664-8. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11927294 Available from. [DOI] [PubMed] [Google Scholar]
- 29.Huyghe E., Delaunay B., Njomnang Soh P., Delannes M., Walschaerts M., Delavierre D. Proposal for a predictive model of erectile function after permanent 125 i prostate brachytherapy for localized prostate cancer. Int J Impot Res [Internet] 2013;25:121–126. doi: 10.1038/ijir.2013.3. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L52465468 Available from. [DOI] [PubMed] [Google Scholar]
- 30.O’Connor D.B., Lee D.M., Corona G., Forti G., Tajar A., O’Neill T.W. The relationships between sex hormones and sexual function in middle-aged and older European men. J Clin Endocrinol Metab. 2011;96(10) doi: 10.1210/jc.2010-2216. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.