Abstract
Acute myocardial infarction during pregnancy is a very uncommon condition; atherosclerotic coronary artery disease is by far the most common cause of an acute coronary syndrome in the general population. The causes of an acute coronary syndrome in the pregnant patient are wide and varied. This has important implications with respect to the diagnosis of the etiology and the subsequent management of the cause of the acute coronary syndrome. There are a number of diagnostic tools for the diagnosis of coronary artery disease but it is important to understand their role in pregnant patients. Spontaneous coronary artery dissection is one of the most common causes of acute coronary syndrome in pregnant patients. Understanding its pathophysiology and knowing the natural history of this condition is paramount in the management of this condition. The article also lists the various therapeutic modalities available to the clinician faced with an acute coronary syndrome in the pregnant patient. Finally, we discuss the delivery of the baby and post partum care of these complex patients.
Keywords: Pregnancy, Acute myocardial infarction, Spontaneous coronary artery dissection
1. Epidemiology
Acute myocardial infarction (MI) during pregnancy is a rare event and the estimated incidence is one acute myocardial infarction for every 16,000 deliveries.1 Up to one in four of these infarctions is caused by coronary arterial dissection.2 The causes of MI during pregnancy are presented in Table 1.3 Spontaneous coronary dissection (SCAD) is the most common cause, found in 43%; atherosclerotic disease is the second most common cause and is found in 27%, a thrombus without angiographic evidence for atherosclerotic disease is found in 17%, no cause is found by angiography in 11%.3 Although SCAD is rare in the general population with an annual incidence is 0.26 per 100,000 persons or about 800 news cases per year in the United States (incidence in females and males −0.33 and 0.18 per 100,000 persons respectively),4 it is not uncommon in pregnant females presenting with an acute coronary syndrome.3 Thus SCAD and atherosclerotic coronary artery disease are the most common causes of MI in pregnancy.2,3
Table 1.
Causes of acute myocardial infarction during pregnancy.9
| Cause | Trimester | Percentage of cases (%) |
|---|---|---|
| SCAD | Third/post-partum | 43 |
| Atherosclerosis | Any | 27 |
| Thrombosis | Second and post-partum | 17 |
| Spasm | Third/postpartum | 2 |
Note: It is important to understand that any of the above causes of pregnancy associated myocardial infarction can present during any time in pregnancy or the post partum period.
2. Risk factors and etiology
It is interesting to note that the risk factors for atherosclerotic coronary artery disease are different from those of SCAD. From a clinical standpoint it is important to recognize this difference because oftentimes it is impossible to distinguish among the various causes of acute coronary syndrome in pregnant women based on the presentation alone. However, a reasonable guess can be made by paying attention to the underlying risk factors. An analysis from the national inpatient sample (NIS) found 859 cases of MI (rate of 6.2 (95% confidence interval [CI] 3.0–9.4) per 100,000 deliveries).1 In 73% of cases, MI occurred antepartum and in 27% the MI occurred postpartum.1 Risk factors identified were age (33 vs. 27 years) and the risk was higher among black women compared to Hispanics and white women (11.4 vs. 4.2 vs 7.6 per 100,000 deliveries, respectively).1 Independent predictors of MI included hypertension (odds ratio [OR] 21.7), thrombophilia (OR 25.6), diabetes mellitus (OR 3.6), smoking (OR 8.4), transfusion (OR 5.1), and postpartum infection (OR 3.2).1
The risk factors for SCAD in pregnancy differ from the risk factors for all-cause MI in pregnancy and include a history of smoking (23%), family history (16%), hypertension (9%), and lipid disorder (7%); only 9% had more than one risk factor, whereas 61% reported no known risk factors.5 This is similar to the findings of other studies of SCAD in non-pregnant patients which found that the most common risk factors associated with SCAD are smoking (31%), hypertension (18%), and a family history of coronary artery disease (25%).4 By contrast, the prevalence of other conventional risk factors such as diabetes (2.2%) and chronic kidney disease (1.7%) is significantly lower when compared to atherosclerotic coronary artery disease.3, 4, 5, 6
SCAD, in general, predominantly affects young white females (83%) and one study showed no significant difference in the baseline characteristics between postpartum and non-postpartum patients with SCAD.7 SCAD affects multiparous women as opposed to primipara and the average gravidity is 2.7, most cases present in the peripartum period with a range of 3–90 days post-partum.5 When the condition occurs antepartum it most commonly presents at 32 ± 4 weeks with a range of 23–36 weeks.5
3. Pathophysiology
A number of conditions listed below can cause an acute coronary syndrome in the pregnant patient.
SCAD: SCAD is defined as a non-iatrogenic and non-traumatic separation of the coronary arterial walls, creating a false lumen.8 The pathognomonic feature of SCAD is the separation of the layers within the arterial wall by an intramural hematoma (IMH).9 The hematoma can arise by an intimal rupture initiating medial dissection or more commonly by a spontaneous intramedial hemorrhage due to a disruption of the vasa vasorum.9 The hematoma can then secondarily lead to an intimal tear.10 Excess levels of progesterone lead to a loss of normal corrugation of elastic fibers and a decrease in acid mucopolysaccharide ground substance and appear to play a major role in pathogenesis of the condition.10 Estrogen increases the release of matrix metalloproteinase which can lead to cystic medial necrosis and lack of structural support for the vasa vasorum and rupture leading to IMH.10
Spasm: A number of factors can contribute to the development of coronary spasm in pregnant women. It is postulated that there is endothelial dysfunction in pregnancy, an enhanced vascular reactivity to angiotensin II and norepinephrine, and an increased renin release and angiotensin production due to decreased uterine perfusion in the supine position.10 Coronary spasm can also be caused by ergot derivatives that are used to control post-partum hemorrhage or to suppress lactation.11
Thrombosis: A number of alterations in the coagulation system predispose to arterial thrombosis in pregnancy. These include a decreased releasable tissue plasminogen activator (tPA), increased fast-acting tPA inhibitor, change in the level of coagulation factors, and reduction in functional protein S levels.12 Smoking further increases platelet aggregability.12
4. Clinical presentation
The majority of patients present with STEMI (75%) and the remaining present with non-STEMI (NSTEMI).3 The majority of MI cases occur in the third trimester of pregnancy (STEMI, 25%; NSTEMI, 32%) or the postpartum period (STEMI, 45%; NSTEMI, 55%).3 The anterior wall is most commonly involved in 69%–78% of the patients, the inferior wall is involved in 27%, and the lateral wall is involved in 4%.2,3 The high percentage of involvement of the anterior wall is seen across a number of studies dealing with MI in pregnant women irrespective of what the most common cause of MI is in each study (Atherosclerotic or SCAD).1,3 This is an important finding and explains the relatively higher frequency of catastrophic presentation and complications of MI in pregnancy in general. The left ventricular ejection fraction was ≤40% in 54% of the cases, ≤30% in 24% of cases, and ≤20% in 9% of cases.3 Heart failure or cardiogenic shock occurred in 38% of the patients, ventricular arrhythmias in 12%, and recurrent angina or AMI in 20%.3
In the largest case review compiled by Elkayam et al, SCAD-associated MI in pregnancy involved the left main artery in 26%, left anterior descending (LAD) in 34%, left circumflex (LCX) in 3%, right coronary artery (RCA) in 14%, and multivessel involvement in 39%.3 This is similar to the vascular distribution seen in non-pregnant individuals where the most common vessels involved were LAD (61%), LCX (25%), RCA (25%), and LM (4%).13 Multivessel coronary involvement is seen in a significant number of patients (15–20%).13, 14, 15 Studies in non-pregnant individuals show that the middle segments are the most common site of involvement (54% mid, 27% distal, 19% proximal) and the number of vessels with TIMI 0–1 and 2–3 flow are almost equal at presentation (50–60% and 60–80%, respectively).13, 14, 15 The pathophysiological basis for the reason why the left coronary system, in particular the LAD artery is the most commonly affected artery is not clear. It is hypothesized that this is because of hemodynamic and anatomic differences between the right and left coronary arterial system (the higher number of branches in the left system subject it to a higher torsional force and the flow in the left system is mainly diastolic as opposed to a more uniform systolic and diastolic flow in the right system (RCA).16 SCAD presents in similar ways in pregnant and non-pregnant females. According to one study involving pregnant females, 81% presented with STEMI, 25% were hemodynamically unstable at the time of presentation. A total of 14% received advanced cardiac life support interventions and 26% required emergent intra-aortic balloon pump support.5 This is similar to the presentation in non-pregnant females where 80–90% present with an acute coronary syndrome, about 40% present with STEMI, and 40% present with NSTEMI. A total of 10–13% of episodes are complicated by cardiac arrest and cardiogenic shock occurs in 2–4%.13, 14, 15
It is helpful to classify the causes of acute coronary syndrome based on the trimester of presentation. It is important to understand this is not a strict iron clad classification and every cause can occur during any trimester, however, it provides a useful framework. The causes of MI in the first trimester are usually atherosclerotic MI, particularly in the presence of vascular risk factors.2,3 The most common causes of MI in the second trimester include atherosclerotic MI and thrombosis.2,3 SCAD is the most common cause of pregnancy-related MI in the third trimester, a small proportion of ACS in this period are caused by coronary spasm.2,3 In the post-partum period SCAD is once again the most common cause; a few cases are caused by spasm and thrombosis.3 Although atherosclerotic coronary artery disease can present during any trimester it is more common during the antepartum period whereas SCAD most commonly occurs peripartum (responsible for 50% of all MI in this time period) or postpartum.2
A number of hemodynamic changes that occur during pregnancy can serve as precipitating factors for SCAD in the presence of an underlying predisposition; these include an increase in plasma volume by 40% and cardiac output by 50%.17 Heart rate is a major ischemic determinant and therefore significantly increases myocardial oxygen requirements.17 During labor and delivery, several additional factors increase the cardiac oxygen requirements. Indeed, cardiac output is known to increase by 15% in early labor, 25% during stage 1, and by 50% during expulsive efforts.17 The maximal increase in output is seen in early postpartum period due to auto transfusion.17 This is possibly the reason why most pregnancy-related SCADS's present in the third trimester – early postpartum period.
5. Electrocardiographic changes and their significance
The majority of women without preexisting cardiovascular disease have completely normal electrocardiograms. Common variations that can be encountered include the following. Due to a rotation of the heart there can be a 15–20° left axis deviation. Transient ST segment and T wave changes can occur. T waves can be inverted in leads V1,2 and sometimes in lead V3. Q waves and inverted T waves can be detected in lead III. Changes mimicking left ventricular hypertrophy can occur.17 Furthermore, ST-segment depression mimicking myocardial ischemia has been observed in healthy women after the induction of anesthesia for cesarean section.18
6. Non-invasive modalities to diagnose coronary artery disease in pregnancy
The European committee recommends against the use of dobutamine stress testing.17 Nuclear stress test is contraindicated.17 There are several limitations to CT coronary angiography such as a need to decrease the heart rate for accurate ECG gating and lack of resolution for smaller arterial branches that may be involved by SCAD. These limitations (which are beyond the scope of this review) make this modality unattractive in pregnant women.19 The ESC guidelines state that intervention is targeted primarily at patients who demonstrate evidence of high-risk features; in all other situations conservative management is recommended. Therefore, in the absence of such high-risk features, demonstration of ischemia by stress testing or defining the coronary anatomy by CT coronary angiography does not alter the management.
Invasive evaluation and coronary angiography: Invasive coronary angiography remains the standard diagnostic procedure for conclusive evaluation of the cause of MI. The incidence of iatrogenic coronary dissection is increased during pregnancy and according to one study catheter-induced dissection complicated 2%–4% of pregnancies.3
The role of intravascular ultrasound (IVUS) and optical coherence tomography (OCT) in SCAD: IVUS with its ability to visualize the entire thickness of the wall albeit with limited spatial resolution and OCT with a superior spatial resolution but with a limited depth of penetration are both adjunctive to diagnostic angiography in SCAD.8 Although both can visualize IMH equally well OCT has the added advantage of detecting intimal tears.8 IVUS can provide visualization, even in patients without anterograde coronary flow and in those with occlusive intracoronary thrombus.8 It can also fully visualize large hematomas and also penetrates across red thrombi that can cause major shadowing on OCT.8 OCT requires a lumen free of blood and thus is not able to obtain good images in patients with severe lesions that impede adequate blood clearance.8 It is important to recognize that the risk benefit ratio of any complimentary intracoronary diagnostic or therapeutic strategy be carefully considered in these patients given the extremely high risk of propagating or causing an iatrogenic dissection.
Radiation and pregnancy: It is important to understand the radiation tolerance of pregnant women and the amount of exposure associated with each modality to assuage fears. The effects of radiation on the fetus depend on the radiation dose and the gestational age.17 Procedures should be delayed (if possible) until at least the completion of major organogenesis (12 weeks after menses). There is no risk of congenital malformations, intellectual disability, growth restriction, or pregnancy loss at of 50 mGy doses of radiation to the pregnant woman; however, doses more than 100 mGy are definitely harmful. The effect of exposures to doses between 50 and 100 mGy may be associated with harm.20 During the first 14 days after fertilization, intact survival without fetal abnormality or death are the most likely outcomes.20 After the first 14 days, there may be an increased risk of congenital malformations, growth restriction, and intellectual disability.20 The fetal dose from a chest radiograph is 0.01 mGy.21 CT Chest delivers about 0.3 mGy, coronary CT delivers between 1 and 3 mGy, a diagnostic coronary angiogram exposes the fetus to 1.5 mGy, and the fetal exposure with a percutaneous coronary intervention is about 3 mGy.17
7. Medical management of acute coronary syndrome and safety of medications
Medical management of the pregnant MI patient does not differ from guideline-directed management of acute coronary syndrome using aspirin (ASA), beta blockers, and anticoagulation.3 There is very little human data for the use of most thrombolytics but all of them appear to be compatible with use during pregnancy and lactation.22 Similarly, it is safe to use all anticoagulants in pregnancy and lactation if they are truly indicated.22 Among glycoprotein receptor blockers the use of abciximab is safer than eptifibatide and tirofiban, particularly during lactation (Table 2).22
Table 2.
Cardiac medications and safety profile in pregnancy.
| Drugs in pregnancy and lactation30: | |||
|---|---|---|---|
| Drug | Pregnancy (human vs animal studies) | Lactation (human vs animal studies) | Recommendations |
| Thrombolytics | |||
| Alteplase (10 case reports) | High molecular weight precludes transfer to the embryo | It is unknown if the drug crosses into placental milk. | Compatible with pregnancy and lactation |
| Reteplase (one case report) | Given the nature of the indication of use and short half-life it is unlikely that drug use during lactation will pose a significant problem. Reteplase is unlikely to cross into breast milk. | ||
| Urokinase (six case reports) |
Unsure if it crosses into the placenta. Proteinase inhibitors in placental tissue can inactivate urokinase |
Given the nature of the indication of use and short half-life it is unlikely that drug use during lactation will pose a significant problem | Low risk in pregnancy and probably compatible in lactation |
| Tenecteplase (no human data available) | |||
| Antiplatelet medications | |||
| Prasugrel | There is no human data available | No human data | There is no human data, animal data suggests low risk. Can be used in pregnancy if the benefits outweigh risks. Probably compatible with lactation. |
| Ticagrelor | There is no human data but animal data suggests risk to the fetus | No human data available | Animal data suggests risk, there is no human data available. If indicated in the mother the risks have to evaluated on a case-by-case basis Breastfeeding may be associated with potential toxicity |
| Clopidogrel | There is limited human data available, it is not teratogenic in animals. | No human data is available in breastfeeding. | There is limited human data, it is probably compatible with pregnancy, it is probably compatible with lactation. |
| Aspirin | With full dose aspirin human data suggests risk in the 1st and 3rd trimesters. Can be associated with IUGR, hemorrhage, teratogenic effects. Can prolong labor, premature closure of the ductus can occur in the premature infant. |
Limited human data available. Potential for salicylate toxicity | Low-dose aspirin is compatible with pregnancy. Limited human data suggests potential toxicity in the breast feeding infant. |
| Anticoagulants | |||
| Heparin | Does not cross the placenta | Not excreted into breast milk | Compatible with pregnancy and lactation |
| Bivalirudin | No human data, animal data suggests low risk | No human data | Can be used in pregnancy if the benefits outweigh risks. Probably compatible with lactation |
| Fondaparinux | Limited human data | No human data | Can be used if indicated in pregnancy. Probably compatible with lactation |
| Enoxaparin | Safe in pregnancy | No human data | Compatible with pregnancy and lactation |
| Glycoprotein receptor blockers | |||
| Abciximab | Does not reach the fetus in clinically significant amounts | Unlikely to be excreted in breast milk | Compatible with pregnancy and lactation |
| Eptifibatide, Tirofiban | Limited human data, animal data suggests low risk or is reassuring | The drug will likely be digested by the baby when ingested or no data available | Limited human data – animal data suggest low risk or compatible with pregnancy. Preferable to hold breastfeeding |
With respect to antiplatelet agents, the use of low dose (as opposed to full-dose aspirin) appears to be safe in pregnancy but has been linked to one case report of salicylate intoxication in a breast feeding new born.22 Both clopidogrel and prasugrel can be used in pregnancy and lactation if required.22 Ticagrelor has been associated with risk in pregnant animals and is probably unsafe in lactation.22 If truly indicated its use should be evaluated in a case-by-case basis.22
8. The roles and merits of PCI, CABG, and thrombolysis
In the largest series on this subject, 45% of patients who undergoing angiography for an MI during pregnancy were treated with PCI.3 The exact frequency with which BMS or DES is used is not known but it appears that the majority of pregnant patients are treated with a BMS.3 Approximately 6% of PCI procedures were complicated by iatrogenic dissection in pregnant women.3 On an average, PCI exposes the fetus to 3 mGy.17 The fetus should be shielded and a radial approach should be used whenever possible. PCI is preferable to thrombolysis.23 The safety of drug eluting stent (DES), clopidogrel, and newer antiplatelet medications is not established and in our opinion it is preferable to use bare metal stents (BMS) until further data are available because the benefit of a DES in the absence of traditional risk factors for restenosis in younger patients is unclear.
Revascularization by PCI is suboptimal in the setting of SCAD.13 The PCI success rate is about 65–70%, the rate of complicated PCI requiring multiple additional stents is about 4%, the restenosis rate is about 15%, and the rate of CABG bailout is 11%.13, 14, 15 Dissections frequently extend (25–60%) and a high number of new dissections involve previously unaffected vessels, this decreases the long-term durability of PCI which is only 30%.13,24 There is a high rate of iatrogenic dissection and according to one study 11 out of 87 procedures were complicated by such dissections in the general population.13
It is important to understand the reasons for the suboptimal PCI results in this group of patients. It can be difficult to determine the true lumen, technically challenging to wire the artery without risking an extension of the intimal tear, and there is a risk of under sizing the stent leading to malapposition and associated problems such as stent thrombosis.13, 14, 15 Furthermore, multiple stents may be required in an overlapping fashion to cover the entire length of the intimal tear.13, 14, 15
CABG: CABG is reserved for patients with multivessel involvement, LM dissection, failed PCI (as bailout strategy).9 The surgeon faces a number of technical challenges.9 Data on the safety of CABG in pregnancy is rare with a potential for high mortality rate.1
9. Thrombolysis
Several studies have demonstrated that placental transfer of streptokinase and tPA is too low to cause fibrinolytic effects in the fetus.23 However, they are associated with a number of adverse maternofetal outcomes and hence relatively contraindicated in pregnancy.17 Thrombolysis is a double-edged sword with the capacity to increase the degree of IMH and propagation of dissection.2,3 Caution is warranted in pregnant patients with acute MI as majority of these cases are related to SCAD.
Management of spontaneous coronary artery dissection in pregnancy: A conservative strategy seems to be associated with very favorable outcomes, in general, for patients with SCAD.6,13, 14, 15,24 Most studies have compared conservative treatment in patients with isolated distal lesions with TIMI 2–3 flow with revascularization using PCI and or CABG in patients with proximal lesions with TIMI 1–2 flow presenting as STEMI with or without shock.13, 14, 15 Thus there are marked differences in the baseline characteristics of the patients with the patients in the revascularization arm being far sicker than their conservative counterparts.6,13, 14, 15 In spite of these important differences there were no significant differences in short or long-term MACE (death, progression during treatment, recurrent SCAD, heart failure) and event free survival between the groups.13 The only finding that reached significance was increased revascularization (TVR P = 0.06) and increased utilization of CABG (P = 0.01) in the revascularization arm.13 According to a European registry of non-pregnant SCAD patients, the overall in-hospital MACE (death, MI, cardiogenic shock, stent thrombosis, TIA/stroke) was higher in the revascularization group (16% vs 4% p = 0.028) and the difference was driven by increased rate of repeated revascularization (9.4 vs. 1.3%, p = 0.03) in the revascularization group.6
In our opinion, conservative management is a reasonable option for management of SCAD-related MI in pregnancy due to the lack of suitable revascularization techniques, high rate of recurrence, and favorable outcomes with spontaneous healing in the majority of patients, particularly in relatively stable patients with a small myocardial area at risk. Most studies have documented the safety of this strategy in SCAD's presenting with distal lesions involving small branches with TIMI2-3 flow and/or no ongoing ischemia.6,13, 14, 15,24 Revascularization should be considered in the presence of proximal lesions with TIMI 0–1 flow, presenting with ongoing ischemia and or in STEMI/shock/cardiac arrest settings.6,9,13, 14, 15,24
Mode of delivery and its timing: Older data reported a maternal mortality rate of 14% following vaginal deliveries and 23% for caesarean sections after a MI; hence vaginal route was emphasized. However, in more recent reviews, no convincing support for one method of delivery over the other has been found.25,26 Vaginal delivery is associated with less blood loss and infection risk, cesarean delivery may be associated with an increased risk of venous thrombosis and thromboembolism.17 Although vaginal delivery is still preferred, caesarian section under regional anesthesia is preferred in the presence of severe cardiac illness including severe aortic stenosis, pulmonary arterial hypertension, and aortic dissection to avoid the prolonged hemodynamic stresses associated with vaginal delivery.27 Furthermore, the guidelines add that preterm delivery can be induced in cases of recurrent SCAD if the fetus is viable.17 If vaginal delivery is sought, induction with pharmacological agents such as misoprostol and dinoprostone should be avoided, particularly in SCAD as they can increase the risk of coronary spasm.17 It is safe to continue beta blockers which do not interfere with uterine contractions.28
Timing is individualized according to the gravida's cardiac status, Bishop Score, fetal well-being, and lung maturity.17 Due to a lack of prospective data and the influence of individual patient characteristics, standard guidelines do not exist, and the timing should therefore be individualized.17 Most maternal deaths occur at the time of infarction or within 2 weeks of infarction, usually in association with labor and delivery; for this reason it is safe to delay delivery for at least 2 weeks following a MI.17 However, in cases of MI, particularly reinfarction if the fetal is viable, it is best to proceed with delivery in our opinion.
Postpartum care: While a slow infusion of oxytocin to prevent hemorrhage is reasonable to enhance uterine involution, prostaglandin F analogues should be reserved for PPH and methyl ergonovine analogues are contraindicated.11 Close hemodynamic monitoring is recommended for a minimum of 24 h.10
Implication for future pregnancies: Following an MI due to atherosclerotic coronary artery disease it is advisable for patients with previous revascularization or infarction to delay pregnancy until the risks of recurrent ischemia and restenosis have reduced significantly, this is generally a period of one year after the event.29 The estimation of the risk should take into consideration factors such as residual left ventricular function, degree of residual ischemia, the cause of MI, and the time between MI and previous pregnancy.
10. SCAD and future pregnancies
Limited information is available on the rate of recurrence in future pregnancies. One small series studied the rate of recurrence with subsequent pregnancies and demonstrated that one of seven SCAD survivors suffered recurrent SCAD at 9 weeks postpartum.30 Given the catastrophic presentation in pregnant women, it is our opinion that subsequent pregnancies should be avoided with non-hormonal contraceptive methods.
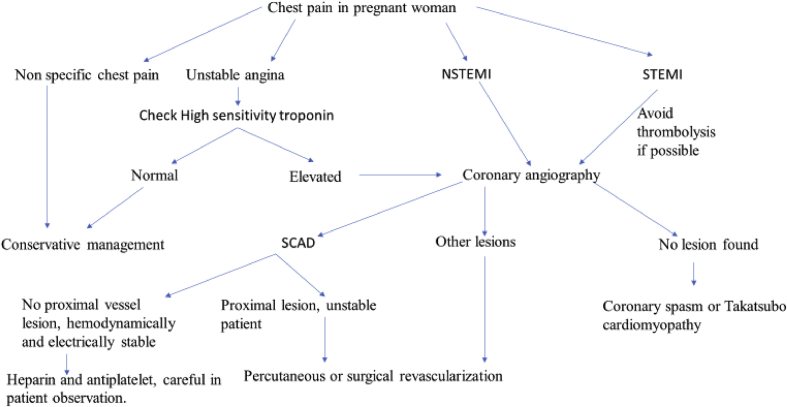
10.1. Putting it all together (Approach to acute myocardial infarction during pregnancy)
In conclusion, pregnancy-associated MI carries a grave prognosis with a mortality rate significantly higher than that in the general population.8 Unfortunately, the use of invasive strategies continues to be dismally low.31 The management approaches of an acute coronary syndrome are similar to the general population with a few important differences understanding which will likely improve outcomes for the mother and the child.
11. New-generation troponin assays and other biomarkers can be elevated in other pregnancy-associated conditions
New-generation assays offer the advantage of diagnosing an acute coronary syndrome faster than conventional assays. However, one has to be mindful of the fact that these assays can be elevated in the presence of pregnancy-induced hypertension and preeclampsia.32 Creatine kinase myocardial band is present in the uterus and placenta. It can be elevated up to four times the upper limit of normal after delivery making it less reliable in this setting.33
12. Thrombolytics for acute ST segment elevation myocardial infarction are relatively contraindicated
A significant number of acute coronary syndromes in pregnancy are a result of spontaneous coronary artery dissections and administering thrombolytics carries a risk worsening the IMH.8 Thrombolytics are also associated with placental abruption and post-partum hemorrhage.34 Their association with fetal bleeding merits caution.34 Therefore, every effort needs to be made to transport the patient to the nearest cardiac catheterization laboratory in a timely fashion failing which thrombolytics should be considered as a last resort.
13. Heparin is the safest anticoagulant
The anticoagulant of choice is intravenous unfractionated heparin as it is protein bound and crosses the placenta minimally reducing the risk of fetal bleeding.35 The pharmacokinetics of low molecular weight heparin are too unpredictable in pregnancy and monitoring factor Xa levels is recommended which is not always feasible.36 Although bivalirudin is traditionally associated with the least risk of bleeding, it is not well-studied and is a category B drug, hence, its administration is not recommended.35 Glycoprotein IIb/IIIa (category B with no reported adverse events in pregnancy so far) inhibitor use is associated with a higher risk of bleeding complications which is particularly concerning in the pregnant woman; therefore abundant caution should be exercised before utilizing these agents which should be considered nevertheless in the presence of complex PCI with a high thrombus burden.35
14. Aspirin and clopidogrel are the preferred antiplatelet agents
NSAIDS have been linked to a variety of adverse effects in pregnancy but there are no case reports linked to use of aspirin at doses of 80–150 mg per day.37 In our opinion, the potential benefits of aspirin usage far outweigh the risks. Although case reports have demonstrated an association between the use of clopidogrel and maternal thrombocytopenia, maternal hemorrhage and fetal demise, it is still the most widely used thienopyridine.35 Ticagrelor (category c) and Prasugrel (category b) are both more potent than clopidogrel but are associated with a higher bleeding risk and therefore are not preferred.35
15. Radial access is better than femoral access
Radial access is preferred for ease of use and comfort to the patient given the presence of a gravid uterus and positioning difficulties; furthermore, it allows the patient to lie in a left lateral decubitus position to relieve the uterine compression of the inferior vena cava after 20 weeks gestation.35 Although radial access is associated with a slightly higher radiation dose to the operator this can be mitigated by the careful use of collimation, lower frame rates, and lower magnifications.35
16. Contrast media is safe to use
The risk of fetal congenital hypothyroidism related to the use of contrast media is mainly theoretical and there are no other reported teratogenic effects.38
17. The choice of the stent depends on the gestational age
The main determinant of the choice of stent in pregnancy is the temporal proximity of the procedure to the birth of the child. Drug eluting stents can be used when delivery is at least 3–6 months away and BMS are safer closer to due date given that they afford the option of discontinuing dual antiplatelet therapy after 4 weeks.35 Furthermore, given the young age of patients and the low atherosclerotic burden, the chance of restenosis with BMS may not be a problem but this aspect has never been evaluated systematically.
18. The goal of a successful coronary intervention in the setting of spontaneous coronary artery dissection is improvement in flow
Spontaneous coronary artery dissection makes percutaneous coronary intervention challenging due to a number of reasons. The aims of intervention in this setting are to achieve TIMI 3 flow with electric and hemodynamic stability.35 Stenting may not always be suitable or feasible in the presence of SCAD, and non-flow limiting dissections, particularly in non-left main or major proximal vessel locations may be left alone for spontaneous healing to occur.35 The conventional definition of successful percutaneous coronary intervention includes <30% residual stenosis after stent placement, including non-stented segment of dissection or <50% residual stenosis for angioplasty.10 The SCAD-specific definition of success must include improvement in baseline thrombolysis in myocardial infarction (TIMI) grade 0 to 1 flow (≥1 grade improvement) or maintenance/improvement of TIMI grade 2 to 3 flow.10
19. Management of unanticipated interruption of dual antiplatelets after stent implantation is unclear
A number of events around delivery may require temporary suspension of dual antiplatelet agents. Performance of caesarian section and administration of neuraxial anesthesia are two such examples. Administration of neuraxial anesthesia during labor requires discontinuation of clopidogrel 5–7 days and LMWH at least 24 h before the procedure.35 One approach would be to continue aspirin and discontinue clopidogrel temporarily with the addition of either heparin anticoagulation or glycoprotein IIB/IIIA inhibitor or using intravenous cangrelor.35 Unfortunately heparin use in this situation has not been found to prevent stent thrombosis, no major trials have demonstrated the efficacy of IIB/IIIA inhibitors to prevent stent thrombosis and they increase the risk of bleeding, finally cangrelor is a category C drug that is associated with intrauterine growth retardation, fetal loss, and incomplete ossification in animal studies.35,39,40 It is recommended that clopidogrel be discontinued 5 days prior to planned delivery and bridging with tirofiban or eptifibatide in suggested in instances in which the risk of stent thrombosis is high.35 Tirofiban and eptifibatide should be continued up to 4–6 h before delivery.35 GP IIb/IIIa inhibitors can be resumed after delivery on a case-by-case basis and clopidogrel can be usually resumed within 24 h after consultation with the obstetricians and the anesthetists.35
19.1. Takatsubo cardiomyopathy
The major features include left ventricular apical hypokinesis to akinesis, with sparing of the basal segments, causing ballooning of the left ventricle in systole and was described in the late 1980s.41 Common triggers include psychosocial stressors with greater occurrence in those with premorbid psychiatric illness.42 Management is similar to management of acute coronary syndrome, including use of beta blockers, aspirin, afterload reduction, diuretics, and anticoagulation to prevent thrombus formation with severe apical dilation.41
Declaration of competing interest
All authors have none competing interests to declare.
Algorithm for the management of acute coronary syndrome in pregnancy.
STEMI: ST elevation myocardial infarction, NSTEMI: non-ST elevation myocardial infarction.
References
- 1.James A.H., Jamison M.G., Biswas M.S., Brancazio L.R., Swamy G.K., Myers E.R. Acute myocardial infarction in pregnancy: a United States population-based study. Circulation. 2006;113:1564–1571. doi: 10.1161/CIRCULATIONAHA.105.576751. [DOI] [PubMed] [Google Scholar]
- 2.Roth A., Elkayam U. Acute myocardial infarction associated with pregnancy. J Am Coll Cardiol. 2008;52:171–180. doi: 10.1016/j.jacc.2008.03.049. [DOI] [PubMed] [Google Scholar]
- 3.Elkayam U., Jalnapurkar S., Barakkat M.N. Pregnancy-associated acute myocardial infarction: a review of contemporary experience in 150 cases between 2006 and 2011. Circulation. 2014;129:1695–1702. doi: 10.1161/CIRCULATIONAHA.113.002054. [DOI] [PubMed] [Google Scholar]
- 4.Tweet M.S., Hayes S.N., Pitta S.R. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation. 2012;126:579–588. doi: 10.1161/CIRCULATIONAHA.112.105718. [DOI] [PubMed] [Google Scholar]
- 5.Higgins G.L., 3rd, Borofsky J.S., Irish C.B., Cochran T.S., Strout T.D. Spontaneous peripartum coronary artery; dissection presentation and outcome. J Am Board Fam Med. 2013;26:82–89. doi: 10.3122/jabfm.2013.01.120019. [DOI] [PubMed] [Google Scholar]
- 6.Lettieri C., Zavalloni D., Rossini R. Management and long-term prognosis of spontaneous coronary artery dissection. Am J Cardiol. 2015;116:66. doi: 10.1016/j.amjcard.2015.03.039. [DOI] [PubMed] [Google Scholar]
- 7.Ito H., Taylor L., Bowman M., Fry E.T., Hermiller J.B., Van Tassel J.W. Presentation and therapy of spontaneous coronary artery dissection and comparisons of postpartum versus nonpostpartum cases. Am J Cardiol. 2011;107:1590–1596. doi: 10.1016/j.amjcard.2011.01.043. [DOI] [PubMed] [Google Scholar]
- 8.Alfonso F., Bastante T., Cuesta J., Rodríguez D., Benedicto A., Rivero F. Spontaneous coronary artery dissection: novel insights on diagnosis and management. Cardiovasc Diagn Ther. 2015;5(2):133–140. doi: 10.3978/j.issn.2223-3652.2015.03.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vijayaraghavan R., Verma S., Gupta N., Saw J. Pregnancy-related spontaneous coronary artery dissection. Circulation. 2014;130:1915–1920. doi: 10.1161/CIRCULATIONAHA.114.011422. [DOI] [PubMed] [Google Scholar]
- 10.Nisell H., Hjemdahl P., Linde B. Cardiovascular responses to circulating catecholamines in normal pregnancy and in pregnancy-induced hypertension. Clin Physiol. 1985;5:479–493. doi: 10.1111/j.1475-097x.1985.tb00779.x. [DOI] [PubMed] [Google Scholar]
- 11.Lin Y.H., Seow K.M., Hwang J.L. Myocardial infarction and mortality caused by methylergonovine. Acta Obstet Gynecol Scand. 2005;84:1022. doi: 10.1111/j.0001-6349.2005.0058d.x. [DOI] [PubMed] [Google Scholar]
- 12.Härtel D., Sorges E., Carlsson J., Römer V., Tebbe U. Myocardial infarction and thromboembolism during pregnancy. Herz. 2003;28(3):175–184. doi: 10.1007/s00059-003-2453-4. [DOI] [PubMed] [Google Scholar]
- 13.Tweet M.S., Eleid M.F., Best P.J. Spontaneous coronary artery dissection revascularization versus conservative therapy. Circ Cardiovasc Interv. 2014;7:777–786. doi: 10.1161/CIRCINTERVENTIONS.114.001659. [DOI] [PubMed] [Google Scholar]
- 14.Mortensen K.H., Thuesen L., Kristensen I.B., Christiansen E.H. Spontaneous coronary artery dissection: a Western Denmark heart registry study. Cathet Cardiovasc Interv. 2009;74(5):710–717. doi: 10.1002/ccd.22115. [DOI] [PubMed] [Google Scholar]
- 15.Alfonso F., Paulo M., Lennie V. Long-term follow-up of a large series of patients prospectively managed with a “conservative” therapeutic strategy. JACC Cardiovasc Interv. 2012;5(10):1062–1070. doi: 10.1016/j.jcin.2012.06.014. [DOI] [PubMed] [Google Scholar]
- 16.Yiannis S., Chatzizisis Y.S., Gianmoglon G.D., George D. Is left coronary system more susceptible to atherosclerosis than right? A pathophysiological insight. Int J Cardiol. 2007;116:7–13. doi: 10.1016/j.ijcard.2006.03.029. [DOI] [PubMed] [Google Scholar]
- 17.European Society of Gynecology (ESG); Association for European Paediatric Cardiology (AEPC); German Society for Gender Medicine (DGesGM), Regitz-Zagrosek V., Blomstrom Lundqvist C. ESC Guidelines on the management of cardiovascular diseases during pregnancy. Eur Heart J. 2011 Dec;32(24):3147–3197. doi: 10.1093/eurheartj/ehr218. [DOI] [PubMed] [Google Scholar]
- 18.Mathew J.P., Fleisher L.A., Rinehouse J.A. ST segment depression during labor and delivery. Anesthesiology. 1993;78:997–998. doi: 10.1097/00000542-199210000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Leber A.W., Knez A., von Ziegler F. Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol. 2005;46(1):147. doi: 10.1016/j.jacc.2005.03.071. [DOI] [PubMed] [Google Scholar]
- 20.Brent R.L. The effect of embryonic and fetal exposure to x-ray, microwaves, and ultrasound: counseling the pregnant and nonpregnant patient about these risks. Semin Oncol. 1989;16:347–368. 23. [PubMed] [Google Scholar]
- 21.Damilakis J., Theocharopoulos N., Perisinakis K. Conceptus radiation dose and risk from cardiac catheter ablationprocedures. Circulation. 2001;104:893–897. doi: 10.1161/hc5790.094909. [DOI] [PubMed] [Google Scholar]
- 22.Gerald G. Briggs, Roger K. Freeman, Sumner J. Yaffe; Drugs in Pregnancy and Lactation: A Reference Guide to Fetal and Neonatal Risk; 10th ed..
- 23.Leonhardt G., Gaul C., Nietsch H.H., Buerke M., Schleussner E. Thrombolytic therapy in pregnancy. J Thromb Thrombolysis. 2006;21:271–276. doi: 10.1007/s11239-006-5709-z. [DOI] [PubMed] [Google Scholar]
- 24.Saw J., Aymong E., Buller C.E. Spontaneous coronary artery dissection: association with predisposing arteriopathies and precipitating stressors, and cardiovascular outcomes. Circ Cardiovasc Interv. 2014;7:645–655. doi: 10.1161/CIRCINTERVENTIONS.114.001760. [DOI] [PubMed] [Google Scholar]
- 25.Roth A., Elkayam U. Acute myocardial infarction associated with pregnancy. Ann Intern Med. 1996;125:751–762. doi: 10.7326/0003-4819-125-9-199611010-00009. [DOI] [PubMed] [Google Scholar]
- 26.Hankins G.D., Wendel G.D., Jr., Leveno K.J., Stoneham J. Myocardial infarction during pregnancy: a review. Obstet Gynecol. 1985;65:139–146. [PubMed] [Google Scholar]
- 27.Bonow R.O., Carabello B.A., Chatterjee K. 2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American college of cardiology/American heart association task force on practice guidelines (writing committee to revise the 1998 guidelines for the management of patients with valvular heart disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2008;118:e523–e661. doi: 10.1161/CIRCULATIONAHA.108.190748. [DOI] [PubMed] [Google Scholar]
- 28.Zipes D.P., Camm A.J., Borggrefe M. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death—executive summary: a report of the American College of Cardiology/American Heart Association task Force and the European Society of cardiology committee for practice guidelines (writing committee to develop guidelines for management of patients with ventricular arrhythmias and the prevention of Sudden cardiac death) developed in collaboration with the European Heart rhythm Association and the Heart rhythm Society. Eur Heart J. 2006;27:2099–2140. doi: 10.1093/eurheartj/ehl199. [DOI] [PubMed] [Google Scholar]
- 29.Wilson A.M., Boyle A.J., Fox P. Management of ischaemic heart disease in women of child-bearing age. Intern Med J. 2004;34:694–697. doi: 10.1111/j.1445-5994.2004.00698.x. [DOI] [PubMed] [Google Scholar]
- 30.Tweet M.S., Hayes S.N., Gulati R., Best P.J. The risk of pregnancy after spontaneous coronary artery dissection. J Am Coll Cardiol. 2014;63:A5. doi: 10.1016/j.jacc.2017.05.055. [DOI] [PubMed] [Google Scholar]
- 31.Smilowitz Nathaniel R., Gupta Navdeep, Guo Yu. Acute myocardial infarction during pregnancy and the puerperium in the United States. Mayo Clin Proc. 2018 October;93(10):1404–1414. doi: 10.1016/j.mayocp.2018.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ravichandran J., Woon S.Y., Quek Y.S. High-sensitivity cardiac troponin I levels in normal and hypertensive pregnancy. Am J Med. 2019 Mar;132(3):362–366. doi: 10.1016/j.amjmed.2018.11.017. [DOI] [PubMed] [Google Scholar]
- 33.Shivvers S.A., Wians F.H., Jr., Keffer J.H., Ramin S.M. Maternal cardiac troponin I levels during normal labor and delivery. Am J Obstet Gynecol. 1999;180(1 pt 1):122. doi: 10.1016/s0002-9378(99)70161-4. [DOI] [PubMed] [Google Scholar]
- 34.Tawfik M.M., Taman M.E., Motawea A.A., Abdel-Hady E. Thrombolysis for the management of massive pulmonary embolism in pregnancy. Int J Obstet Anesth. 2013;22:149–152. doi: 10.1016/j.ijoa.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 35.Ismail Sahar, Wong Cynthia, Priya Rajan, Mladen I. Vidovich; ST-elevation acute myocardial infarction in pregnancy: 2016 update. Clin Cardiol. 2017;40:399–406. doi: 10.1002/clc.22655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bates S.M., Greer I.A., Hirsh J., Ginsberg J.S. Use of antithrombotic agents during pregnancy: the Seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest. 2004;126(suppl 3):627S–644S. doi: 10.1378/chest.126.3_suppl.627S. [DOI] [PubMed] [Google Scholar]
- 37.Marchetti T., Cohen M., de Moerloose P. Obstetrical antiphospholipid syndrome: from the pathogenesis to the clinical and therapeutic implications. Clin Dev Immunol. 2013;2013:159124. doi: 10.1155/2013/159124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thomsen H.S. European Society of Urogenital Radiology (ESUR) guidelines on the safe use of iodinated contrast media. Eur J Radiol. 2006;60:307–313. doi: 10.1016/j.ejrad.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 39.Vicenzi M.N., Meislitzer T., Heitzinger B., Halaj M., Fleisher L.A., Metzler H. Coronary artery stenting and non-cardiac surgery—a prospective outcome study. Br J Anaesth. 2006;96:686–693. doi: 10.1093/bja/ael083. [DOI] [PubMed] [Google Scholar]
- 40.Alshawabkeh L.I., Prasad A., Lenkovsky F. Outcomes of a preoperative “bridging” strategy with glycoprotein IIb/IIIa inhibitors to prevent perioperative stent thrombosis in patients with drug-eluting stents who undergo surgery necessitating interruption of thienopyridine administration. EuroIntervention. 2013;9:204–211. doi: 10.4244/EIJV9I2A35. [DOI] [PubMed] [Google Scholar]
- 41.Purgason K. Broken hearts: differentiating stress-induced cardiomyopathy from acute myocardial infarction in the patient presenting with acute coronary syndrome. Dimens Crit Care Nurs. 2006;25:247–253. doi: 10.1097/00003465-200611000-00001. [DOI] [PubMed] [Google Scholar]
- 42.Nayeri A., Rafla-Yuan E., Farber-Eger E. Pre-existing psychiatric illness is associated with increased risk of recurrent Takotsubo cardiomyopathy. Psychosomatics. 2017 Sep - Oct;58(5):527–532. doi: 10.1016/j.psym.2017.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]