Abstract
Background
Despite noteworthy advancements in the design of the left ventricular assist device (LVAD), stroke remains one of the most significant adverse events. This study aims to analyze the incidence and short-term outcomes associated with stroke (ischemic and hemorrhagic) after implantation of LVAD.
Methods
Study cohorts were identified from the National Inpatient Sample database from January 2009 to September 2015 using the International Classification of Diseases, Ninth Revision codes. The primary outcome was an incidence of stroke, and secondary outcomes were the associated mortality, length of stay, and cost of hospitalization. A multivariate logistic regression analysis was performed to analyze adjusted in-hospital mortality.
Results
Use of LVADs increased significantly from 2009 to 2014 (2278 in 2009 to 3730 in 2014 [Ptrend <0.001]). From a total of 20,656 admissions who underwent LVAD implantation, 1518 (7.4%) developed stroke, among whom 1177 (5.7%) had an ischemic stroke and 426 (2.1%) had a hemorrhagic stroke. Adjusted in-hospital mortality was highest with hemorrhagic stroke. Incidence of stroke was associated with significantly longer length of stay and cost of hospitalization.
Conclusion
The incidence of stroke was ~7% after LVAD placement, and it was associated with significantly higher in-hospital mortality and resource utilization.
Keywords: LVAD, Ischemic stroke, Hemorrhagic stroke, In-hospital mortality
1. Introduction
Despite increasing incidence and prevalence of advanced heart failure (HF), there is limited availability of donor hearts for transplantation.1 Hence, mechanical circulatory devices have become an essential part in the management of advanced HF (class IIa American College of Cardiology/American Heart Association (ACC/AHA) recommendation), being a bridge to therapy or destination therapy.1, 2 There has been a noteworthy advancement in the design of left ventricular assist devices (LVADs) from pulsatile to continuous flow LVAD with smaller dimensions and improved longevity.3 More recently, an analysis from the multicenter study of maglev technology in patients undergoing mechanical circulatory support therapy with heartmate 3 (MOMENTUM 3) trial comparing centrifugal flow HeartMate III with the axial flow HeartMate II demonstrated excellent two years' outcomes with respect to the disabling stroke or malfunctioning of the device.4 However, nearly two-thirds of the patients experience major adverse events within the first year after LVAD implantation.5 Among them, stroke (both ischemic and hemorrhagic) is a significant adverse event associated with higher morbidity and mortality. Few studies with small cohorts have been published to define the incidence of stroke after LVAD placement.6, 7 However, studies describing the similar events on a larger scale are minimal.8, 9 Therefore, this retrospective study includes study cohorts from the National Inpatient Sample (NIS) database to analyze the incidence and associated mortality, hospital stay, and cost of care in hospitalizations for LVAD implantation.
2. Methods
To obtain study cohorts for analyses, this study utilized the NIS database from 2009 to September 2015. The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code for LVAD was not available before 2009.1 The NIS is developed by the Agency for Healthcare Research and Quality and has been described in the literature previously.1 This publicly available deidentified nationally representative data set consists of 20% of the stratified sample of inpatient hospitalizations in the United States. For this study, approval from the institutional review board and informed consents were not required because it included deidentified inpatient population.
This study used the 37.66 ICD-9-CM procedural code to identify LVAD hospitalizations (N = 21,121).1, 7 Then, inpatients younger than 18 years were excluded from the analysis (N = 465). The ICD-9-CM diagnostic codes 433×1, 434×1, and 436 for ischemic stroke and 430, 431, and 432.1 for hemorrhagic stroke were used with a previously validated strategy.7 This strategy has ~90% sensitivity and specificity in identifying stroke.7 The primary outcome was an incidence of stroke, and the secondary outcomes were mortality, length of stay, and cost of care.
This study used SAS 9.4 (SAS Institute, Cary, NC) for all the analyses. This study represents continuous variables as the median with interquartile range (nonnormal distribution), for which the Mood test was used, and categorical variables are represented as frequencies in percentages, for which the Person chi-square test was used. This study calculated the frequency of LVAD use as well as the frequency of overall, ischemic, and hemorrhagic stroke including per 1000 event rate for every year from 2009 to September 2015. The Jonckheere-Terpstra trend test was used to analyze the trend over the years. To adjust for differences in baseline risks, a multivariate logistic regression analysis for mortality was performed. All the analyses were performed for overall stroke, ischemic stroke, and hemorrhagic stroke.
3. Results
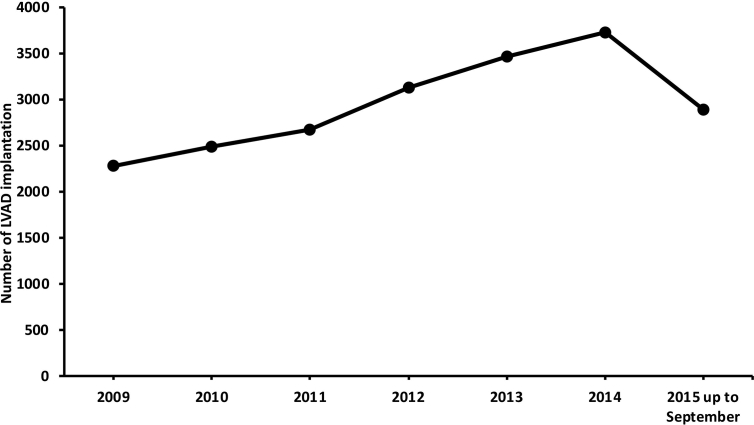
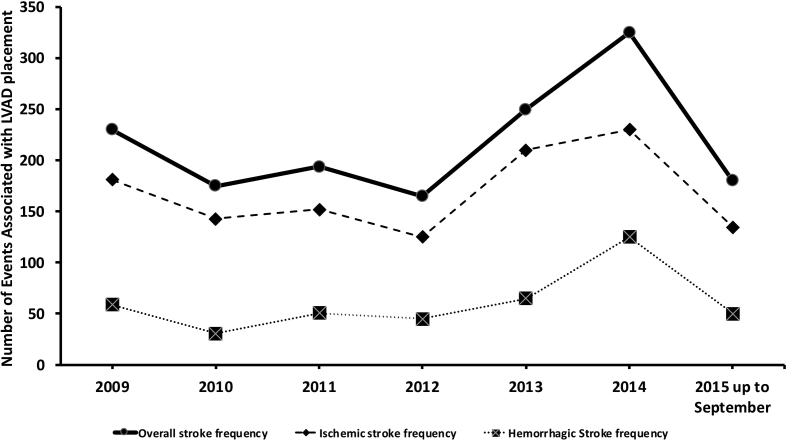
A total of 21,121 inpatients underwent LVAD implantation from the year 2009 to September 2015, of whom 20,656 hospitalizations were older than 18 years. The use of LVADs increased significantly from 2009 to 2014 (2278 in 2009 to 3730 in 2014, Ptrend <0.001; Fig. 1). From these 20,656 admissions, 1518 (7.4%) developed stroke, among whom 1177 (5.7%) had an ischemic stroke and 426 (2.1%) had a hemorrhagic stroke trend which significantly increased during the study period (Fig. 2). Mortality in patients with stroke was significantly higher than that in patients without stroke (36.1% vs 11%, risk adjusted odds ratio [aOR]: 4.48, confidence interval [CI]: 3.39–5.92, P < 0.001). Mortality rate in patients with ischemic stroke was 29.8% (2.72 [1.96–3.51]), P < 0.001), and that in patients with hemorrhagic stroke was 58% (9.59 [5.94–15.46], P < 0.001). Length of hospital stay was longer in patients with stroke than in those without stroke (42 vs 28 days, P < 0.001); and among patients with stroke, hospital stay was higher in those with hemorrhagic stroke than in those with ischemic stroke (47 vs 40 days). This translated to a higher cost of care for patients with stroke than that for those without stroke ($244,224 vs $197,369, P ≤ 0.001); and among patients with stroke, cost of care was higher for those with hemorrhagic stroke than for those with ischemic stroke ($301,944 vs 223,620, P ≤ 0.001).
Fig. 1.
Temporal trends of LVAD implantation per year from 2009 to September 2015. LVAD = left ventricular assist device.
Fig. 2.
Temporal trends of stroke events associated with LVAD placement. Ptrend = <0.001 for all 3 types. LVAD = left ventricular assist device.
4. Discussion
This study demonstrated that the use of LVADs has continuously increased from 2009 to 2014, and about 7% of admissions were associated with stroke. Among them, ischemic stroke was more than twice as common as hemorrhagic stroke. This study also adds that the mortality rate was significantly higher in patients who developed stroke. Furthermore, hemorrhagic stroke was more fatal than ischemic stroke. The length of hospital stay and cost of care were also higher in patients with stroke than in those without stroke, and among stroke, hemorrhagic stroke was associated with longer hospital stay and higher cost of care than ischemic stroke.
Several aspects can possibly explain the increased number of LVAD implantations such as high prevalence of patients with stage D HF, rapid progression in the technology of LVAD devices having favorable outcomes and lesser complications, and limited availability of the donor hearts compared with the increasing demand.1, 3 LVAD implantation and increased risk of stroke can be explained by several factors—(i) device-related factors and postoperative management: intrinsic thrombogenicity of pump results in hypercoagulation, thrombosis, and ischemic events and chronic anticoagulation and related bleeding complications result in hemorrhagic events, device-related infection, and sepsis; (ii) patient-related factors: associated comorbidities including, but not limited to, atrial fibrillation, ventricular arrhythmias and associated embolisms, hyperlipidemia, hypertension, and coagulation disorders; (iii) device-patient interphase: cleavage of large molecules of von Willebrand factor which leads to acquired von Willebrand disease development and bleeding complications.8, 9, 10
A previous small study (N = 1813) demonstrated 8.7% incidence rate of stroke associated with LVADs, among which 5.5% had ischemic stroke and 3.1% had hemorrhagic stroke.7 This study with much larger patient population demonstrated 7.4% incidence of stroke associated with LVAD implantation, among which 5.7% had ischemic stroke and 2.1% had hemorrhagic stroke. Previous studies noted no difference in survival between hemorrhagic and ischemic stroke, while this study observed higher mortality with hemorrhagic stroke.7, 11 This might explain the longer hospital stay and higher cost of care with hemorrhagic stroke than with ischemic stroke. Hypertension is thought to be the major driver of stroke after LVAD placement.12 Guideline-directed medical management of blood pressure with close follow-up after LVAD transplant should be considered for all patients.
This study has few limitations. There is a lack of key baseline information such as the type of the device, mean INR value to interpret the degree of anticoagulation, and longitudinal survival rate. Considering the retrospective nature of our study, it represents only association and not causation.
In conclusion, the use of LVADs has continuously increased. Even after a substantial improvement in the technology, its use is associated with several major complications and stroke is one of them which increases mortality significantly. Among overall stroke, hemorrhagic stroke has more catastrophic outcomes than ischemic stroke. Strategies to reduce stroke are warranted, which include, but are not limited to, optimal antithrombotic therapy, appropriate patient selection, and possible newer LVAD devices that are associated with less risk.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Patel N., Kalra R., Doshi R., Bajaj N.S., Arora G., Arora P. Trends and cost of heart transplantation and left ventricular assist devices: Impact of proposed federal cuts. JACC Heart Fail. 2018;6(5):424–432. doi: 10.1016/j.jchf.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 2.Yancy C.W., Jessup M., Bozkurt B. ACCF/AHA guideline for the management of heart failure: a report of the American college of cardiology foundation/American heart association task force on practice guidelines. J Am Coll Cardiol. 2013;62(16):147–239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 3.Miller L.W., Rogers J.G. Evolution of left ventricular assist device therapy for advanced heart failure: a review. JAMA Cardiol. 2018;3(7):650–658. doi: 10.1001/jamacardio.2018.0522. [DOI] [PubMed] [Google Scholar]
- 4.Hanke J.S., Dogan G., Zoch A. One-year outcomes with the HeartMate 3 left ventricular assist device. J Thorac Cardiovasc Surg. 2018;156(2):662–669. doi: 10.1016/j.jtcvs.2018.01.083. [DOI] [PubMed] [Google Scholar]
- 5.Kirklin J.K., Naftel D.C., Pagani F.D. Seventh INTERMACS annual report: 15,000 patients and counting. J Heart Lung Transplant. 2015;34(12):1495–1504. doi: 10.1016/j.healun.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 6.Mathis M.R., Sathishkumar S., Kheterpal S. Complications, risk factors, and staffing patterns for noncardiac surgery in patients with left ventricular assist devices. Anesthesiology. 2017;126(3):450–460. doi: 10.1097/ALN.0000000000001488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parikh N.S., Cool J., Karas M.G., Boehme A.K., Kamel H. Stroke risk and mortality in patients with ventricular assist devices. Stroke. 2016;47(11):2702–2706. doi: 10.1161/STROKEAHA.116.014049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shahreyar M., Bob-Manuel T., Khouzam R.N. Trends, predictors and outcomes of ischemic stroke and intracranial hemorrhage in patients with a left ventricular assist device. Ann Transl Med. 2018;6(1):5. doi: 10.21037/atm.2017.12.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Acharya D., Loyaga-Rendon R., Morgan C.J. INTERMACS analysis of stroke during support with continuous-flow left ventricular assist devices: risk factors and outcomes. JACC Heart Fail. 2017;5(10):703–711. doi: 10.1016/j.jchf.2017.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pinney S.P., Anyanwu A.C., Lala A., Teuteberg J.J., Uriel N., Mehra M.R. Left ventricular assist devices for lifelong support. J Am Coll Cardiol. 2017;69(23):2845–2861. doi: 10.1016/j.jacc.2017.04.031. [DOI] [PubMed] [Google Scholar]
- 11.Harvey L., Holley C., Roy S.S. Stroke after left ventricular assist device implantation: outcomes in the continuous-flow era. Ann Thorac Surg. 2015;100(2):535–541. doi: 10.1016/j.athoracsur.2015.02.094. [DOI] [PubMed] [Google Scholar]
- 12.Willey J.Z., Boehme A.K., Castagna F. Hypertension and stroke in patients with left ventricular assist devices (LVADs) Curr Hypertens Rep. 2016;18(2):12. doi: 10.1007/s11906-015-0618-1. [DOI] [PMC free article] [PubMed] [Google Scholar]