Abstract
Aims
There has been significant interest in day-case and rapid discharge pathways for unicompartmental knee replacements (UKR). Robotic-assisted surgery has the potential to improve surgical accuracy in UKR. However, to date there are no published studies reporting results of rapid-discharge pathways in patients receiving UKR using the NAVIO◊ robotic system.
Methods
A retrospective analysis identified 19 patients who were safely discharged within 24 h following UKR using the NAVIO◊ robotic system between June 2017 and October 2019. All patients went through a standardised UKR pathway protocol. Pre-operatively patients underwent education sessions and anaesthetic assessment, with selected patients undergoing occupational/physiotherapy assessment prior to surgery. All patients received a general anaesthetic with local anaesthetic infiltration prior to closure; nerve blocks were not used routinely. A multi-modal analgesic regime was utilised. Patients were discharged home once they were safe to mobilise on ward, had normal vital signs and pain was adequately controlled. Patients were discharged with outpatient physiotherapy referral and consultant follow up at 6 weeks.
Results
All patients were discharged within 24 h; there were no post-operative complications and no readmissions to hospital. The mean length of stay was 19.5 h (SD = 6.8), with patients seen twice on average by physiotherapy post-operatively. Active range of motion at 6 weeks was 105.8°, with all patients mobilising independently. The median 6-month post-operative Oxford Knee Score was 44 out of 48.
Conclusion
This initial feasibility study suggests that patients may be safely discharged within 24 h of UKR using the NAVIO robotic system. Appropriate patient selection will ensure successful discharge. Further prospective studies are needed.
Keywords: Unicompartmental, Knee, Discharge, Daycase, NAVIO, Robotics
1. Introduction
The lifetime risk of developing knee osteoarthritis (OA) is around 45%,1 with 50% of cases being diagnosed by the age of 55 years.2 Knee OA places a significant burden on healthcare resources and the demand for knee arthroplasties is expected to rise in the UK by more than 600% by 2030.3 This is largely the result of an ageing population, the epidemic of obesity and a more sedentary lifestyle.4 In the United Kingdom, unicompartmental knee replacement accounts for between 8 and 10% of all knee arthroplasties performed.3
Advantages of UKR over total knee replacement (TKR) include reduced operating time, quicker short-term recovery, reduced post-operative pain and improved functional outcomes.5, 6, 7, 8, 9, 10, 11 The main reported disadvantages of UKR are poorer implant survival and increased revision rates compared to TKR.12,13 However, it has been argued that the higher revision rate is a consequence of easier UKR revision and lower threshold for revision when compared to TKR and thus should not be considered a comparable disadvantage.14
R educed length of stay (LOS) following knee arthroplasty is associated with reduced peri-operative complications and improved clinical outcomes,15, 16, 17, 18, 19 as well as the potential financial advantages to health care providers. In recent years, reducing LOS after UKR has gained considerable interest.20 This has led to the introduction of ‘fast track’, ‘enhanced recovery’ and ‘outpatient surgery’ pathways, aimed at reducing cost and improving the safety of UKR. These protocols have been found to be successful compared with conventional pathways.21 Fast-track programmes for UKR reduced the LOS to around 1 day with good post-operative results.19 A natural progression was to develop a day-case surgery pathway for UKRs. Several authors to date have reported on the feasibility and safety of UKR as a day-case procedure.15,19,22,23 Complication and readmission rates were found to be comparable to established fast-track pathways.15,19,22
1.1. NAVIO◊
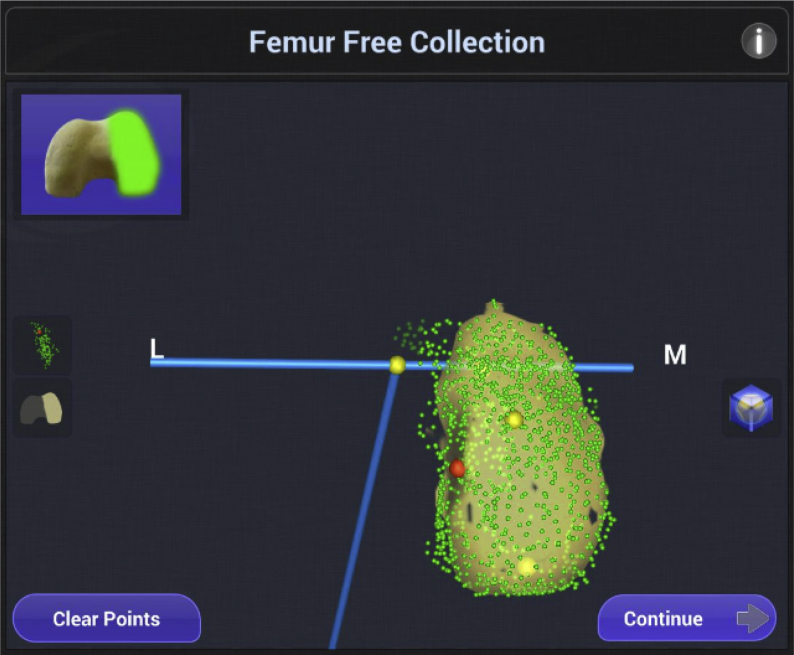
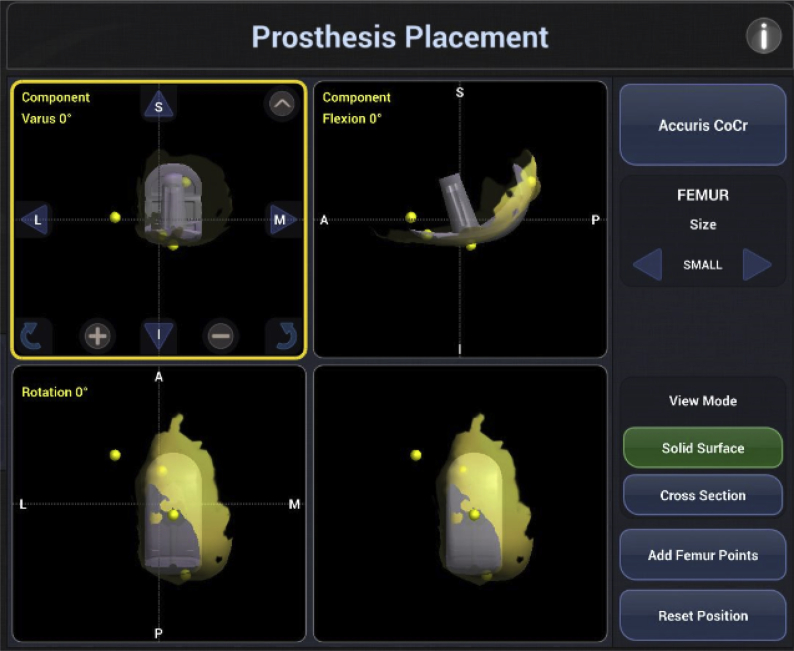
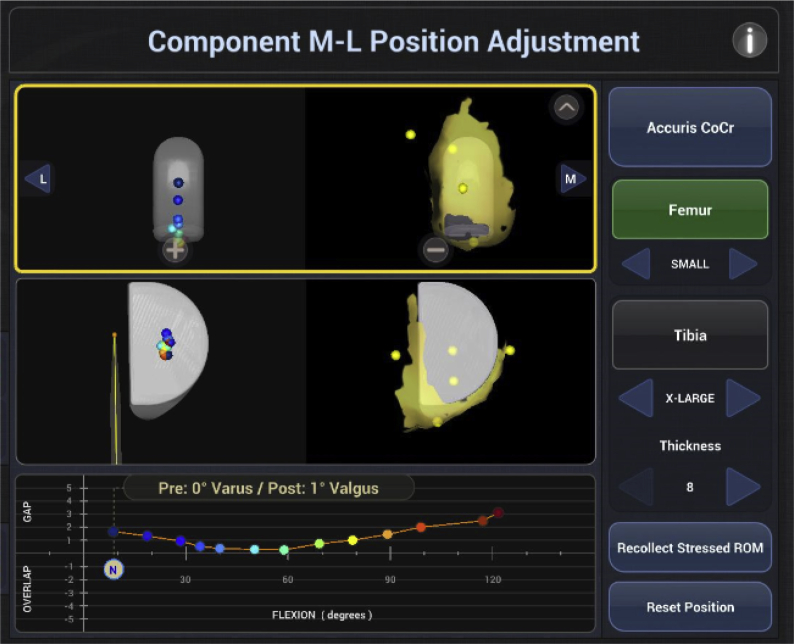
Limb alignment and implant positioning are key prognostic factors for implant survival following UKA.13,24,25 The NAVIO◊ system (Smith and Nephew, Memphis, USA) gathers patient-specific data using anatomic mapping without the need for pre-operative computed tomography (CT) scanning. Intra-operative registration using a freehand tool allows direct mapping of the articular surface to recreate a bespoke 3D model of the patient's anatomy. Additionally, soft-tissue tension is measured throughout a range-of-motion (ROM) (Fig. 1). The surgeon is then able to select the size, orientation and alignment of prosthesis based upon the 3D model (Fig. 2). Implant position can be fine-tuned to achieve optimal soft-tissue balancing using a quantitative ROM graph (Fig. 3). A robotic-controlled NAVIO handpiece burr is used to precisely resect bone, allowing accurate prosthesis implantation. This process provides a detailed personalized intraoperative plan based on the patients' soft tissue balance and anatomy, with the aim being the best possible anatomic and kinematic alignment of the prosthesis.
Fig. 1.
Intra-operative mapping femur.
Fig. 2.
Sizing and alignment of prosthesis.
Fig. 3.
Adjustment of component using quantitative ROM graph.
To date there is no published experience with rapid discharge UKR patients using the NAVIO robotic system. We report our experience of 19 patients who have been safely discharged within 24 h of robotic UKR, and suggest factors that may help to predict this.
2. Material and methods
2.1. Patient selection
Following institutional approval a single center, single surgeons’ retrospective analysis of patients undergoing UKA was conducted. Perioperative records of all patients undergoing primary UKA using the NAVIO robotic system were reviewed between June 2017 and October 2019. Patients undergoing bilateral UKA or revision surgery were excluded. All operations were performed at Charing Cross Hospital, London, under one surgeon (DN). Patients underwent a standard pre, intra and post-operative pathway as outlined below.
2.2. Preoperative preparation
Prior to surgery patients were assessed clinically by the operating consultant in a specialised ‘mass knee’ clinic. All patients selected for surgery were offered pre-operative patient education sessions including presentations from nursing staff, occupational therapy, physiotherapy and junior doctors. Patients with complex social needs were assessed pre-operatively by occupational therapy to identify any discharge issues. All patients underwent separate pre-operative assessment by the anaesthetic team to identify and optimise medical co-morbidities.
2.3. Intra-operative procedure
On the day of surgery, patients were not allowed solid foods for 6 h and clear fluids for 2 h prior to surgery. All operations were performed under general anaesthesia with standard antibiotic prophylaxis consisting of cefuroxime 1.5 g given at induction then 8 and 16 h post-operatively. A standard parapatellar approach was employed. The ACCURIS◊ Genesis Unicompartmental Knee implant (Smith and Nephew GmbH, Tuttlingen, Germany) was used in all cases.
On-table ROM analysis of valgus/varus alignment and fixed flexion deformity was performed pre and post implantation using the NAVIO system (Smith and Nephew, Memphis, USA). Once the joint had been mapped and the ‘envelope of motion’ had been defined, an intra-operative plan was created by using the software to superimpose the implant onto the joint on both tibial and femoral sides. Adjustments were made to ensure correct size and balance of the knee was obtained before any cuts were executed. Bone resections were then performed under robotic guidance in accordance with the intra-operative plan. Verification of medial/lateral resection, varus/valgus alignment and posterior slope angle of the tibia was undertaken prior to implantation.
Following introduction of components, infiltration with a mixture of 60 mls 0.25% bupivacaine and 40 mls 0.9% normal saline into the posterior capsule/deep structures (50 mls) and superficial layers (50 mls) was performed. An adductor canal block was used in one patient; however, nerve blockade was not used uniformly. Following implantation assessment of the range of motion and joint kinematics was undertaken along with coronal and anterior-posterior stability. Drains and indwelling urinary catheters were not used in any of the patients. Closure was in layers with 1 looped polydioxanone to the capsule and extensor mechanism, 2-0 Vicryl® to the subcutaneous tissues and 3-0 Monocryl® (Ethicon, In) and Steri-strips (3 M, Two Harbors, MN, USA) to the skin. A wool and crepe bandage was then applied.
2.4. Post-operative procedure
Multi-modal pain relief was offered as part of an enhanced recovery programme of paracetamol 1 g (six hourly), celecoxib 200 mg (12 hourly), gabapentin 300 mg (8 hourly) and modified-release oxycodone 10–20 mg (12 hourly) with oral morphine sulphate (Oramorph) or immediate-release oxycodone 5–10 mg (4–6 hourly) for breakthrough pain. Early oral hydration and nutrition was encouraged. Post-operatively patients were mobilized full weight bearing and assessed by physiotherapy (unless seen pre-operatively on day of surgery). Patients were discharged once they were safe to mobilise with crutches, had passed a stairs assessment (if applicable), had adequate pain control and vital signs were within normal parameters. Patients were discharged home with 2–4 weeks of aspirin 150 mg OD with gastroprotection using a proton pump inhibitor, depending on thromboembolic risk. Analgesia on discharge included paracetamol and either oxycodone or dihydrocodeine and was combined with oral laxatives. Patients were reviewed at 6 weeks post-operatively by the operating surgeon and referred for outpatient physiotherapy on discharge.
3. Results
A total of 19 UKR patients (26.7%) were discharged within 24 h from a total of 71 UKRs performed in the study period. Average age was 66.8 years and median American Society of Anesthesiology (ASA) class was 2 (1–3). Average body mass index (BMI) was 26.5 kg/m2. There were 10 males and 9 females. Median pre-operative Oxford Knee Score (OKS) was 24.5 out of 48. Pre-operative baseline measurements and demographics are shown in Table 1.
Table 1.
Demographic and pre-operative baseline measurements.
| Characteristic | Category | Navio (n = 19) |
|---|---|---|
| Mean Age (yrs) | – | 66.8 (40.7–85.0) |
| Gender (%) | Male | 10 (52.6) |
| Female | 9 (47.4) | |
| Mean BMI (kg/m2) | – | 26.5 (19.1–33.2) |
| ASA score (%) | I | 4 (21.1) |
| II | 14 (73.7) | |
| III | 1 (5.3) | |
| Laterality (%) | Right | 10 (52.6) |
| Left | 9 (47.4) | |
| Compartment (%) | Medial | 2 (78.9) |
| Lateral | 4 (21.1) | |
| Median pre-operative OKS | /48 | 24.5 (10–43) |
BMI, body mass index; ASA, American Society of Anaesthesiologists; OKS, Oxford Knee Score.
All patients were independent for all activities of daily living (ADLs) and had good social support at home. 16 patients (84.2%) mobilized independently without walking aids and the remaining 3 patients (15.8%) mobilized with a single walking stick. No patients required equipment installation at home or a package of care to be implemented.
Mean operating time was 92.6 min (SD = 17.5). No patients required a post-operative transfusion. 16 patients underwent a post-operative haemoglobin check as an inpatient. Of these, the mean fall in haemoglobin was 12.4 g/L (SD = 8.6) with an average post-operative haemoglobin of 124.1 g/L (SD = 15.6). Operative times and blood loss analysis are shown in Table 2.
Table 2.
Operative time and blood loss.
| Outcome | Navio (n = 11) |
|---|---|
| Mean Operating Time (mins) | 92.6 (64–132) |
| Mean fall in Hb (g/L)* | 12.4 (5–23) |
| Mean post-operative Hb (g/L)* | 124.1 (96–160) |
| Number of patients requiring post-op transfusion (%) | 0 (0) |
* 3 patients were sent home with haemoglobin check post-operatively. Thus for * analysis n = 16. Hb, Haemoglobin.
4 patients underwent pre-operative physiotherapy assessment on the day of surgery and were discharged home without post-operative physiotherapy assessment – following safe mobilisation on the ward. The remaining 15 patients mobilized with physiotherapy post-operatively at a mean of 12.6 h (SD = 8.7), 7 (36.8%) were able to straight leg raise at discharge at a mean time of 7.7 h post-operatively (SD = 7.1). Patients received an average of 2 physiotherapy sessions prior to discharge (range 0–3). The average time to hospital discharge was 19.5 h (SD = 6.8). Results of physiotherapy and discharge are shown in Table 3.
Table 3.
Analysis of physiotherapy and discharge.
| Outcome | Navio (n = 11) |
|---|---|
| Mean time to mobilise with Physiotherapy (hrs) * | 12.6 (2–22) |
| Able to straight leg raise at discharge (%)* | 7 (36.8) |
| Mean time to straight leg-raise (hrs)* | 7.7 (3–19) |
| Median no. of inpatient physiotherapy sessions | 2 (0–3) |
| Mean time to hospital discharge (hrs) | 19.5 (6–23) |
* 4 patients were seen pre-operatively by physiotherapy and sent home without physiotherapy assessment post-operatively. Thus for * analysis n = 15.
No post-operative complications were reported in this group and there were no readmissions to hospital within a 6-week post-operative period. The mean active range of movement at 6 weeks post-operatively was 10 5.8° (SD = 18.4). Oxford Knee Score (OKS) was available in 16 patients at 6 months post operatively with a median score of 44 out of 48 and an average increase in score of 14.
4. Discussion
This study demonstrates that patients could safely undergo UKR using the NAVIO system within 24 h. Day-case joint replacements are one of many innovative methods to safely decrease healthcare costs, whilst maintaining quality care. Reducing LOS with day case-surgery can improve available bed space whilst reducing high inpatient care costs. Day-case arthroplasty has been shown in several studies to have similar complication rates, improved clinical outcomes and patient satisfaction compared to conventional arthroplasty pathways.15,17,19,26, 27, 28, 29, 30
There are several factors to take into consideration regarding feasibility of day-case UKR for NHS trusts. One of the crucial elements to successful day-case surgery is to identify those at high risk of complications and rehospitalisation, which may prevent successful discharge. A comprehensive study by Sher et al. (2017)30 looked at around 7500 patients who underwent primary total joint arthroplasty. They found that patients discharged within 24 h were significantly (p < 0.05) more likely to be younger (<50 years), be ASA class 1 or 2, have fewer significant co-morbidities and not taking steroid medication. Obesity, smoking and presence of bleeding-disorders were all predictors of increased readmission rates. In our cohort, patients had an average age of 66.8 years and BMI at 26.5 kg/m2; the median ASA score was 2 and no patients had a history of bleeding disorders. Whilst these findings broadly agree with those of Sher et al., one patient had a BMI of 33.2 kg/m2 and another had an ASA score of 3 owing to cirrhosis and oesophageal varices. Therefore, exclusion criteria for future studies should not be based on a single baseline characteristic alone and should assess overall pre-operative baseline. The Outpatient Arthroplasty Risk Assessment (OARA) score has been developed with a positive predictive value of 81.6% for the same day or next day discharge.31
In our study, all patients received comprehensive counselling pre-operatively at ‘joint-school’, the aim of which is to adequately prepare patients for their operation, giving realistic expectations about duration of hospital stay and rehabilitation. This is another important process to ensure patients are prepared and engaged in a rapid-discharge pathway. Alongside this, pre-operative assessment by occupational therapy aims to identify social factors that may prevent rapid discharge in selected patients.
In a randomised control trial of patients undergoing total hip replacement in 2015, general anaesthesia (GA) was found to have a shorter LOS and more favourable recovery profile compared to regional anaesthesia.32 All of our patients underwent operations using a short acting GA that has been recommended in other rapid discharge pathways in the United States.15,19,22 Local infiltration analgesia (LIA) was used post implantation with a long acting local anaesthetic, which is of well-recognised benefit in TKR operations.33, 34, 35, 36 One patient received peripheral nerve blockade (adductor canal block), however this is not routine procedure. This was combined with a multimodal pain analgesia regime as recommended in recent studies.37
Intra- and post-operative blood loss is another aspect to consider. In our study, 0 patients required post-operative transfusion, with an average post-op Hb of 124.1 g/dL. Three of the patients were discharged home with a post-operative blood test performed with their general practitioner. Studies have shown that the maximum post-operative haemoglobin decrease is around 4 days post primary hip and knee arthroplasty.38 In a study at our own institution we found a 0% transfusion rate in a population sample of 155 patients undergoing UKR.39 Whilst post-operative anaemia is an important complication, haemoglobin checks within the first 24 h should not delay discharge. Patients with high pre-operative haemoglobin, minimal intra-operative bleeding and low bleeding risk may potentially be safely discharged home with a blood test performed later by their GP. Other key functional aspects include the avoidance of use of surgical drains40 and urinary catheters that may increase risk of infection. Neither were used in any of our patients; allowing easy mobilisation without attachment of unnecessary tubing.
In our study all patients received aspirin 150 mg for 2–4 weeks post-operatively as per trust protocol. This is in line with a recent randomised control trial showing no-difference in venous thromboembolism (VTE) between aspirin and low molecular weight heparin after total hip arthroplasty.41 Aspirin prophylaxis is more convenient for patients and reduces need for injection training and administration post-operatively. High-risk VTE patients, prior history of VTE and pre-existing bleeding disorders would require careful selection for inclusion as rapid-discharge candidates.
Key aspects for effective discharge include early post-operative mobilisation and pain control.37 Pre-operative occupational therapy consultations may help to identify unsuitable candidates for same day discharge. Lack of support at home, excessive number of stairs and transportation issues should all be addressed prior to offering the patient day-case surgery. All patients underwent physiotherapy assessment either pre-operatively (n = 4) or post-operatively (n = 15). Patients who were able to mobilise safely were discharged home with 6-week outpatient follow up. Importantly 4 out of the 19 patients did not undergo post-operative physiotherapy and the remaining 15 patients had an average number of 2 post-operative physiotherapy sessions. A meta-analysis performed by Henderson et al. (2018)42 showed low level evidence that inpatient physiotherapy can decrease the length of stay in TKAs. A further study identified that physiotherapy can be performed as effectively via home telephone advice compared with inpatient physiotherapy.43 Inpatient physiotherapy is an effective tool to help reduce length of stay, however, further studies are needed to look at the benefit in a subgroup of high-performing day-case patients – who are expected to mobilise early. Physiotherapy and occupational therapy consultation pre-operatively can be used to identify rapid-discharge candidates and give robust post-operative exercise regimes. This may have the added benefit of safely discharging patients within 24 h without the need for vigorous inpatient physiotherapy, allowing reallocation of resources to more complex, longer stay patients.
Discharge criteria for post-operative UKR patients vary.22,30,44,45 In our study patients were discharged following safe mobilisation on the ward, normal vital sign parameters and adequate pain control in keeping with other studies.22,30 A study by Lazic (2018)46, recommended several factors for day-case UKR pathways including; immediate mobilisation; early nutrition and hydration; self-directed physiotherapy at home; crystalloid rehydration if volume depleted; aspirin for low-risk patients; novel oral anti-coagulant and mechanical thrombo-prophylaxis for high risk patients; discharge home if < 500 ml blood loss and a haemoglobin check 0–4 days post-operatively.
One of the limitations of the study is a lack of effective pain scores to objectively analyze post-operative pain. This would provide useful information on the efficacy of our pain control regime for further comparison. However it should be noted that all 19 patients were successfully discharged without re-admission for any reason, including uncontrolled pain.
In this study we examined patients discharged within 24 h of their operation. Day-case surgery may be alternatively defined as discharge on the same day of surgery. A prospective study by Bradley et al. 201747, looked at 72 patients undergoing UKR as ‘day-case surgery’. They concluded that the most critical element of same day discharge was the timing of procedure, stating that the procedure must be started before 12pm in order for same day discharge. In our series 7 patients were operated on after 12pm. If aiming for discharge on the same day of surgery an earlier operative time would be a much more important factor to consider.
5. Conclusion
The findings of this study suggest that discharge within 24 h of UKA using the NAVIO surgical system is a safe and feasible option in selected, motivated patients. Careful patient selection combined with extensive patient education and occupational health/physiotherapy assessment is imperative pre-operatively. Multi-modal pain control strategies should be administered with appropriate VTE prophylaxis and early post-operative mobilisation. If utilised correctly day-case UKR could be an efficient cost-reducing procedure within resource-limited healthcare systems.
Declaration of competing interest
None.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
B.M. Sephton, Email: b.sephton@nhs.net.
N. De la Cruz, Email: nina.delacruz@nhs.net.
A. Shearman, Email: ashearman@nhs.net.
D. Nathwani, Email: Dinesh.nathwani@nhs.net.
References
- 1.Rodríquez-Merchán E.C., Gómez-Cardero P. Unicompartmental knee arthroplasty: current indications, technical issues and results. Effort: Open Rev. 2018;3(6):363–373. doi: 10.1302/2058-5241.3.170048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murphy L., Schwartz T.A., Helmick C.G. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum. 2008;59:1207–1213. doi: 10.1002/art.24021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.11th annual report of the national joint registry for England, Wales and Northern Ireland. http://www.njrcentre.org.uk/njrcentre/default.aspx No authors listed. National Joint Registry.
- 4.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 5.Brown N.M., Sheth N.P., Davis K. Total knee arthroplasty has higher postoper- ative morbidity than unicompartmental knee arthroplasty: a multicenter analysis. J Arthroplasty. 2012;27:86–90. doi: 10.1016/j.arth.2012.03.022. [DOI] [PubMed] [Google Scholar]
- 6.Sikorski J.M., Sikorska J.Z. Relative risk of different operations for medial compartment osteoarthritis of the knee. Orthopedics. 2011;34:847–854. doi: 10.3928/01477447-20111021-04. [DOI] [PubMed] [Google Scholar]
- 7.Lyons M.C., MacDonald S.J., Somerville L.E., Naudie D.D., McCalden R.W. Unicompartmental versus total knee arthroplasty database analysis: is there a winner? Clin Orthop Relat Res. 2012;470:84–90. doi: 10.1007/s11999-011-2144-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chassin E.P., Mikosz R.P., Andriacchi T.P., Rosenberg A.G. Functional analysis of cemented medial unicompartmental knee arthroplasty. J Arthroplasty. 1996;11:553–559. doi: 10.1016/s0883-5403(96)80109-4. [DOI] [PubMed] [Google Scholar]
- 9.Isaac S.M., Barker K.L., Danial I.N. Does arthroplasty type influence knee joint proprioception? A longitudinal prospective study comparing total and unicompart- mental arthroplasty. Knee. 2007;14:212–217. doi: 10.1016/j.knee.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 10.Jeer P.J., Cossey A.J., Keene G.C. Haemoglobin levels following unicompartmental knee arthroplasty: influence of transfusion practice and surgical approach. Knee. 2005;12:358–361. doi: 10.1016/j.knee.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 11.Price A.J., Webb J., Topf H. Rapid recovery after Oxford unicompartmental arthroplasty through a short incision. J Arthroplasty. 2001;16:970–976. doi: 10.1054/arth.2001.25552. [DOI] [PubMed] [Google Scholar]
- 12.Koskinen E., Eskelinen A., Paavolainen P., Pulkkinen P., Remes V. Comparison of survival and cost-effectiveness between unicondylar arthroplasty and total knee arthroplasty in patients with primary osteoarthritis: a follow-up study of 50,493 knee replacements from the Finnish Arthroplasty Register. Acta Orthop. 2008;79:499–507. doi: 10.1080/17453670710015490. [DOI] [PubMed] [Google Scholar]
- 13.Hernigou P., Deschamps G. Alignment influences wear in the knee after medial uni- compartmental arthroplasty. Clin Orthop Relat Res. 2004;423:161–165. doi: 10.1097/01.blo.0000128285.90459.12. [DOI] [PubMed] [Google Scholar]
- 14.Murray D., Liddle A., Dodd C., Pandit H. Unicompartmental knee arthroplasty – is the glass half full or half empty? Bone Joint Lett J. 2015;97(10):3–8. doi: 10.1302/0301-620X.97B10.36542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gondusky J.S., Choi L., Khalaf N. Day of surgery discharge after unicompartmental knee arthroplasty: an effective perioperative pathway. J Arthroplasty. 2014;29:516–519. doi: 10.1016/j.arth.2013.08.021. [DOI] [PubMed] [Google Scholar]
- 16.Kim S., Losina E., Solomon D.H., Wright J., Katz J.N. Effectiveness of clinical path- ways for total knee and total hip arthroplasty: literature review. J Arthroplasty. 2003;18:69–74. doi: 10.1054/arth.2003.50030. [DOI] [PubMed] [Google Scholar]
- 17.Mabrey J.D., Toohey J.S., Armstrong D.A., Lavery L., Wammack L.A. Clinical path- way management of total knee arthroplasty. Clin Orthop Relat Res. 1997;345:125–133. [PubMed] [Google Scholar]
- 18.Pearson S., Moraw I., Maddern G.J. Clinical pathway management of total knee arthroplasty: a retrospective comparative study. Aust N Z J Surg. 2000;70:351–354. doi: 10.1046/j.1440-1622.2000.01819.x. [DOI] [PubMed] [Google Scholar]
- 19.Berger R.A., Kusuma S.K., Sanders S.A., Thill E.S., Sporer S.M. The feasibility and perioperative complications of outpatient knee arthroplasty. Clin Orthop Relat Res. 2009;467:1443–1449. doi: 10.1007/s11999-009-0736-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kayani B., Konan S., Pietrzak J.R., Huq S.S., Tahmassebi J., Haddad F.S. The learning curve associated with robotic-arm assisted unicompartmental knee arthroplasty. Bone Joint Lett J. 2018;100:1033–1042. doi: 10.1302/0301-620X.100B8.BJJ-2018-0040.R1. [DOI] [PubMed] [Google Scholar]
- 21.Sutton J.C., III, Antoniou J., Epure lM. Hospital discharge within 2 days following total hip or knee arthroplasty does not increase major-complication and readmission rates. J Bone Joint Surg. 2016;98:1419–1428. doi: 10.2106/JBJS.15.01109. [DOI] [PubMed] [Google Scholar]
- 22.Cross M.B., Berger R. Feasibility and safety of perform- ing outpatient unicompartmental knee arthroplasty. Int Orthop. 2017;38:443–447. doi: 10.1007/s00264-013-2214-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dervin G.F., Madden S.M., Crawford-Newton B.A., Lane A.T., Evans H.C. Outpatient unicompartment knee arthroplasty with indwelling femoral nerve catheter. J Arthroplasty. 2012;27:1159–1165. doi: 10.1016/j.arth.2012.01.009. [DOI] [PubMed] [Google Scholar]
- 24.Emerson R.H., Jr., Higgins L.L. Unicompartmental knee arthroplasty with the Oxford prosthesis in patients with medial compartment arthritis. J Bone Joint Surg. 2008;90-A:118–122. doi: 10.2106/JBJS.F.00739. [DOI] [PubMed] [Google Scholar]
- 25.Collier M.B., Eickmann T.H., Sukezaki F., McAuley J.P., Engh G.A. Patient, implant, and alignment factors associated with revision of medial compartment unicondylar arthroplasty. J Arthroplasty. 2006;21(Suppl 2):108–115. doi: 10.1016/j.arth.2006.04.012. [DOI] [PubMed] [Google Scholar]
- 26.Kim S., Losina E., Solomon D.H., Wright J., Katz J.N. Effectiveness of clinical path- ways for total knee and total hip arthroplasty: literature review. J Arthroplasty. 2003;18:69–74. doi: 10.1054/arth.2003.50030. [DOI] [PubMed] [Google Scholar]
- 27.Otero J.E., gholson J.J., Pugely aJ. Length of hospitalization after joint arthroplasty: does early discharge affect complications and readmission rates? J Arthroplasty. 2016;31:2714–2725. doi: 10.1016/j.arth.2016.07.026. [DOI] [PubMed] [Google Scholar]
- 28.Kort nP., Bemelmans Yf, schotanus Mg. Outpatient surgery for unicompartmental knee arthroplasty is effective and safe. Knee Surg Sports Traumatol Arthrosc. 2017;25:2659–2669. doi: 10.1007/s00167-015-3680-y. [DOI] [PubMed] [Google Scholar]
- 29.Hoorntje a, Koenraadt Kl, Boevé Mg, van geenen rC. Outpatient unicompartmental knee arthroplasty: who is afraid of outpatient surgery? Knee Surg Sports Traumatol Arthrosc. 2017;25:759–766. doi: 10.1007/s00167-017-4440-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sher a, Keswani a, Yao dH. Predictors of same-day discharge in primary total joint arthroplasty patients and risk factors for post-discharge complications. J Arthroplasty. 2017;32:S150–S156. doi: 10.1016/j.arth.2016.12.017. [DOI] [PubMed] [Google Scholar]
- 31.Meneghini rM., Ziemba-davis M., Ishmael M.K., al Kuzma, Caccavallo P. Safe selection of outpatient joint arthroplasty patients with medical risk stratification: the “Outpatient Arthroplasty Risk Assessment Score”. J Arthroplasty. 2017;32:2325–2331. doi: 10.1016/j.arth.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 32.Harsten a, Kehlet H., ljung P., toksvig-larsen s. Total intravenous general anaesthesia vs. spinal anaesthesia for total hip arthroplasty: a randomised, controlled trial. Acta Anaesthesiol Scand. 2015;59:298–309. doi: 10.1111/aas.12456. [DOI] [PubMed] [Google Scholar]
- 33.Kerr D.R., Kohan L. Local infiltration analgesia: a technique for the control of acute postoperative pain following knee and hip surgery: a case study of 325 patients. Acta Orthop. 2008;79:174–183. doi: 10.1080/17453670710014950. [DOI] [PubMed] [Google Scholar]
- 34.Essving P., Axelsson K., Kjellberg J. Reduced hospital stay, morphine consumption, and pain intensity with local infiltration analgesia after unicompartmental knee arthroplasty. Acta Orthop. 2009;80:213–219. doi: 10.3109/17453670902930008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chisholm M.F., Bang H., Maalouf D.B. Postoperative analgesia with saphenous block Appears equivalent to femoral nerve block in ACL reconstruction. HSS J. 2014;10:245–251. doi: 10.1007/s11420-014-9392-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ilfeld B.M., Duke K.B., Donohue M.C. The association between lower extremity continuous peripheral nerve blocks and patient falls after knee and hip arthroplasty. Anesth Analg. 2010;111:1552–1554. doi: 10.1213/ANE.0b013e3181fb9507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Halawi M.J., grant sa, Bolognesi M.P. Multimodal analgesia for total joint arthroplasty. Orthopedics. 2015;38:e616–625. doi: 10.3928/01477447-20150701-61. [DOI] [PubMed] [Google Scholar]
- 38.Chen Z.Y., Wu H.Z., Zhu P., feng X.B. Postoperative changes in hemoglobin and hematocrit in patients undergoing primary total hip and knee arthroplasty. Chin Med J. 2015;128:1977–1979. doi: 10.4103/0366-6999.160620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sephton B.M., Edwards T.C., Bakhshayesh P., Nathwani D. Should we routinely perform a post-operative haemoglobin check following unicompartmental knee arthroplasty? Knee. 2020 doi: 10.1016/j.knee.2019.10.002. [Epub ahead of print], pii:S0968-0160(19)30229-7. [DOI] [PubMed] [Google Scholar]
- 40.Sharma gM., Palekar g, tanna dd. Use of closed suction drain after primary total knee arthroplasty–an overrated practice. SICOT J. 2016;2:39. doi: 10.1051/sicotj/2016034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Anderson D.R., Dunbar M.J., Bohm E.R. Aspirin versus low-molecular- weight heparin for extended venous thromboembolism prophylaxis after total hip arthroplasty a randomized trial. Ann Intern Med. 2013;158:800–806. doi: 10.7326/0003-4819-158-11-201306040-00004. [DOI] [PubMed] [Google Scholar]
- 42.Henderson K.G., Wallis J.A., Snowdon D.A. Active physiotherapy interventions following total knee arthroplasty in the hospital and inpatient rehabilitation settings: a systematic review and meta-analysis. Physiotherapy. 2018;104:25–35. doi: 10.1016/j.physio.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 43.Florez-garcía M., García-Pérez F., Curbelo R. Efficacy and safety of home-based exercises versus individualized supervised outpatient physical therapy programs after total knee arthroplasty: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2017;25:3340–3353. doi: 10.1007/s00167-016-4231-x. [DOI] [PubMed] [Google Scholar]
- 44.Hartog Y.M., Mathijssen nM., Vehmeijer sB. Total hip arthroplasty in an outpatient setting in 27 selected patients. Acta Orthop. 2015;86:667–670. doi: 10.3109/17453674.2015.1066211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gromov K., Kjærsgaard-andersen P., revald P., Kehlet H., Husted H. Feasibility of outpatient total hip and knee arthroplasty in unselected patients. Acta Orthop. 2017;88:516–521. doi: 10.1080/17453674.2017.1314158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lazic S., Boughton O., Kellett C.F., Kader D.F., Villet L., Riviere C. Day-case surgery for total hip and knee replacement: how safe and effective is it? Effort: Open Rev. 2018;3:130–135. doi: 10.1302/2058-5241.3.170031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bradley B., Middleton S., Davis N. Discharge on the day of surgery following unicompartmental knee arthroplasty within the United Kingdom NHS. J Bone Joint Surg. 2017;99:788–792. doi: 10.1302/0301-620X.99B6.BJJ-2016-0540.R2. [DOI] [PubMed] [Google Scholar]