Abstract
Parkinson's disease cannot be cured but symptoms can be improved by making use of physical therapy. The objective of the study was to compare the effect of routine exercises and Tai Chi on physical and clinical performance in elderly people suffering from Parkinson's disease. Data from interviews, physical and clinical performance, and levodopa consumption of 500 patients with confirmed Parkinson's disease (severity level I to III) were collected and analyzed. Participants who received 80 min/day Tai Chi 3 times/week for 2 months were included in the Tai Chi (TC) group (n=250) and those who received 90 min/day routine exercise 3 times/week for 2 months were included in routine exercise (RE) group (n=250). Timed up-and-go, 50-foot speed walk, and functional reach were improved by Tai Chi and routine exercise (P<0.05 for all) but intensities of Tai Chi for improvement of such parameters was higher than routine exercise. Incidence of falls was decreased by both physical therapies (P<0.05 for all) but more for the TC group (P<0.0001, q=38.512). In the TC group, at the end of follow-up, 22 (9%) patients were successful in withdrawal of levodopa treatment. Also, the dose of levodopa was decreased in patients of the TC group who had to continue levodopa. Tai Chi had the potential to slow down the progression of symptoms of Parkinson's disease and delayed the introduction of levodopa (level of evidence: III).
Keywords: Exercise, Fall, Levodopa, Parkinson's disease, Physical therapy, Tai Chi
Introduction
Parkinson's disease (PD) is a neurodegenerative disorder that is highly prevalent, complex, and progressive. It is a disorder of the nervous system that severely impairs the motor role of the body. As the disease advances, motor and non-motor signs and symptoms get more observable (1). In some patients, problems related to thought and behavior also occur at an advanced stage of the disease. As the disease advances, dementia, anxiety, and depression become common. Other symptoms that appear in PD patients are sleeping and emotional disturbances. All these symptoms come collectively under one umbrella term: Parkinsonism (2).
PD is the second most prevalent neurodegenerative complex disorder and 4 million people are diagnosed with PD worldwide (1–2% of the world population). The disorder is dependent on the age of the patient and very few cases occur before the age of 50 years, and after the age of 60 years there is a severe rise in symptoms of the disease (3). It has affected more than 1% of the population older than 50 years (4). PD is more prevalent in males compared to females because the female-specific hormone estrogen has a neuroprotective effect that delays PD onset (5). The causative agent behind PD is still unknown but it is believed to be due to genetic and environmental factors including exposure to toxic chemicals, head trauma, dysfunction of the mitochondrion, and X-linked genetic factors. A reduced risk of PD in people who drink coffee and tea (6) has been reported. It is a challenging and complex disease because of its progressive nature. Impairments associated with gait and instability of posture are the hallmark of this disease. The person can also experience dementia (7). Despite medical advances, PD cannot be cured but symptoms can be improved by making use of several treatment options. PD patients place strains on society, finances, and health care (8).
Chronic symptoms of this disease lead patients to therapies that help alleviate the symptoms. One such treatment is physical therapy, which can be aerobic training, e.g., stationary bicycle and treadmill training (9), Tai Chi, a Chinese martial art that has been proven to enhance the physical and motor capability of PD patients (10), dance, which helps with partner support, social engagement, balance, and strength (11), and agility training, a sensorimotor agility program (12).
Physiotherapy has introduced non-pharmacological treatment options including conventional exercise and physical therapy. Both of these terms are often confused and used as synonyms (13). The American College of Sports Medicine has defined exercise as a sub-class that comes under the more general category of physical activity that involves structured and planned body movements to maintain or improve physical activity, whereas physical therapy is any activity performed via contraction of skeletal muscles and involves the expenditure of energy (14).
Tai Chi is an exercise based on balance maintenance guided by the yin-yang theory of traditional Chinese medicine originating 6000 years ago. Tai Chi is a safe and effective technique that helps the body and brain, and consists of approximately 108 intricate exercise steps (15) and 4 basic steps. Dao Yin consists of gentle stretches that help the body warm up; Chi Kung exercise consists of synchronized breathing to help maintain the body's balance, posture, and reduce stress; Tai Chi Chuan is a series of movements performed in a slow, flowing, and relaxed manner that spans over 20 min; and push hand practice, which is only recommended for certain cases where the participant wants to learn the philosophy of Tai Chi.
Progressive resistance exercise can affect the balance maintenance in PD patients effectively (16,17). The National Parkinson Foundation has recommended Tai Chi for PD patients as complementary therapy but little evidence has been provided via clinical trials.
The primary objective of the study was to compare and analyze the effect of routine exercises and Tai Chi on physical and clinical performance of elderly people suffering from PD. The secondary objective was to test the hypothesis that Tai Chi delays the introduction of levodopa.
Material and Methods
Ethics approval and consent to participate
The original protocol (GPH/CL/15/2016 dated 15 June 2019) of the study had been approved by the Gaomi People's Hospital review board. An informed consent form was signed by all participating patients or their relative(s) (legally authorized person) regarding non-treatment interventions, evaluations, and publications of the study in all formats irrespective of time and language. The study adhered to the law of China, the strengthening the reporting of observational studies in epidemiology (STROBE), cohort study statement, and the 2008 Helsinki Declaration.
Inclusion and exclusion criteria
All patients aged 18 years and above with confirmed PD (diagnosed as per UK Brain Bank criteria (18)), severity level I to III (very early-stage, early-stage, and mild-stage), that could move independently, had no other severe neurological disorder, had not participated in any kind of physical therapy program in the previous 2 months, and did not have other severe orthopedic disorders were included in the analysis.
Patients with PD disease severity level IV (advanced-stage) and patients who had received any physical therapy exercise in the previous 2 months were excluded from the analysis.
Cohorts
PD patients who received 80 min per day Tai Chi training 3 times a week for 2 months were included in the TC group and those who received 90 min per day routine exercise (treadmill training, aerobic training, and dance) 3 times a week for 2 months were included in RE group.
Tai Chi program
Participants were instructed to perform 6 moves of Tai Chi that originated from the traditional Yang Tai Chi style. Six forms of moves were performed: wave hands like clouds, Taijiquan (part wild horse's mane), stepping up and then moving down, fists striking the ears of the opponent, repulse monkey, and grasping the peacock's tail. The exercise routine was to perform these six moves in a repetitive manner for 3 consecutive days in a week for two months.
Routine exercise (RE) program
Participants performed routine exercises including treadmill training, aerobic training, and dance for 3 consecutive days in a week over a period of 2 months.
Instructions to the class and monitoring
The investigators coached and supervised the training session for 2 months. Both investigators had more than 5 years of experience in physical therapy, cardiopulmonary resuscitation, and first aid. Participants were asked whether any discomfort was faced and their responses were recorded after the end of the training session. Changes were made on an individual basis in the program.
Outcome measurements
The investigators carried out pre-assessment and post-assessment (after 2 months of intervention) to assess the improvement in motor function.
Final interview
The final interview was conducted by the supervisors at the end of the 2-month trial period. Responses of the participants were recorded and summarized for both groups.
Measurement of physical performance
Physical performance was measured by three tests: the 50-foot speed test, which estimates the time by the patient takes to walk a 50-foot distance; the timed up-and-go test, which evaluates the time required by a participant to stand up from a chair, walk 10 feet, and come back and sit down on the chair; the functional reach test, which measures 16 common functional activities, e.g. unloading groceries, making a bed, climbing 3 steps onto a platform with luggage, etc. (9) (0: minimum and 100: maximum). Incidence of falls was also recorded before intervention (previous 6-months) and within 6-months (from the start of physical therapy and follow-up period). Participants were helped and assisted to perform the tasks whenever needed.
Clinical evaluations
Total number of patients who had to take levodopa or equivalent treatment and the dose per day were also noted before the intervention and within 6-months (from the start of treatment and follow-up period). Adverse events were also recorded.
Statistical analysis
SPSS (IBM, USA) was used for statistical analysis. Chi-squared independent test was used for categorical data and paired sample t-test for continuous data. Tukey test (considering critical value [q]>3.314 as significant) was used for post-hoc analysis. The results were considered significant at P<0.05.
Results
Enrollment
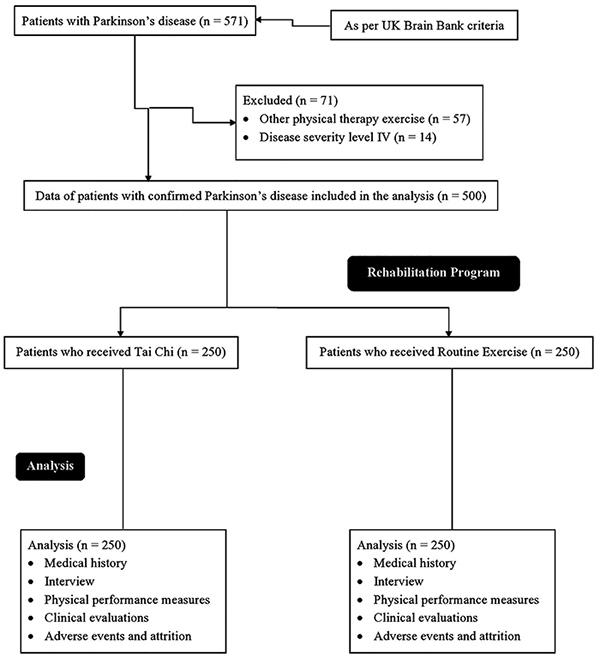
From December 1, 2017 to January 15, 2019, a total of 571 patients were diagnosed with PD in the Department of Neurology of the Gaomi People's Hospital, Gaomi, Shandong, China and the Lishui People's Hospital, Lishui, Zhejiang, China. All patients were subjected to exercise during the rehabilitation program in the Department of Rehabilitation Sciences of the institutes. Among them, 57 patients were subjected to physical therapy other than Tai Chi or routine exercise (e.g., yoga, the art of living, etc.) and 14 patients had PD level IV. Therefore, data of these patients were excluded from the analysis. Data regarding interview and physical measurements of 500 patients with confirmed PD who received Tai Chi (n=250) or routine exercise (n=250) were included in the analysis (Figure 1).
Figure 1. Flow diagram of the study.
Medical history of patients
Among the enrolled PD patients, male to female ratio was 2.5:1. Some of the patients had started levodopa or equivalent treatment in the previous 6 months. The other demographical and clinical parameters are reported in Table 1. There were no significant differences for the parameters between both groups at enrollment (P>0.05 for all).
Table 1. Demographical, anthropological, and clinical parameters of the enrolled Parkinson's disease patients who performed Tai Chi (TC) or routine exercise (RE) programs.
| Parameter | Total population (n=500) | Groups | P value | |
|---|---|---|---|---|
| TC (n=250) | RE (n=250) | |||
| Gender | ||||
| Male | 356 (71) | 182 (73) | 174 (70) | 0.489 |
| Female | 144 (29) | 68 (27) | 76 (30) | 0.489 |
| Ethnicity | ||||
| Han Chinese | 439 (88) | 220 (88) | 219 (88) | 0.918 |
| Mongolian | 35 (7) | 17 (7) | 18 (7) | 0.918 |
| Tibetan | 16 (3) | 7 (3) | 9 (3) | 0.918 |
| Taiwanese | 6 (1) | 4 (1) | 2 (1) | 0.918 |
| North Korean refugee | 4 (1) | 2 (1) | 2 (1) | 0.918 |
| Age (years) | 61.21±8.4 | 62.52±5.45 | 61.89±4.55 | 0.161 |
| Age at onset of PD (years) | 56.56±5.78 | 56.12±4.55 | 55.85±5.12 | 0.533 |
| Duration of disease (years) | 5.12±3.52 | 4.99±2.52 | 5.35±3.01 | 0.148 |
| Body mass index (kg/m2) | 25.07±1.14 | 24.87±1.11 | 25.07±1.21 | 0.055 |
| Parkinson's disease severity level | 256 (51) | 127 (51) | 129 (52) | 0.982 |
| I | 177 (35) | 89 (36) | 88 (35) | 0.982 |
| II | 67 (14) | 34 (13) | 33 (13) | 0.982 |
| III | ||||
| Incidence of falls in last 6 months | 7.52±2.15 | 7.45±1.18 | 7.65±1.26 | 0.068 |
| Levodopa or equivalent treatment in last 6 months | ||||
| Patients were put on levodopa or equivalent treatment | 112 (22) | 54 (22) | 58 (23) | 0.748 |
| Patients were not put on levodopa or equivalent treatment | 388 (78) | 196 (78) | 192 (77) | 0.748 |
| Levodopa or equivalent dose (mg/day) | 450±35 | 425±45 | 435±60 | 0.323 |
| Timed up-and-go test (s) | 17.01±2.22 | 17.09±2.31 | 16.82±3.52 | 0.311 |
| 50-foot walk test (s) | 10.55±2.85 | 10.49±2.79 | 10.78±3.71 | 0.324 |
| Functional reach (0: minimum and 100: maximum) | 27.25±5.85 | 26.46±5.71 | 27.49±6.52 | 0.061 |
Categorical data are reported as number (percentage) and continuous data are reported as means±SD. Parkinson's disease severity level: I: very-early stage; II: early stage; and III: mild-stage. Chi-squared independent test was used for categorical data and paired sample t-test for continuous data. P<0.05 was considered significant.
Final interview
In general, all the participants were happy with their exercise program and found exercise movements easy, safe, and appropriate. Participants reported that exercises helped them improve their confidence and balance. More patients in the RE group responded 'not sure' or 'no' in terms of stability during the final interview. The other results of the survey are summarized in Table 2.
Table 2. Response of Parkinson's disease (PD) patients who performed Tai Chi (TC) or routine exercise (RE) programs recorded in the final interview.
| Questions | TC group (n=250) | RE group (n=250) | P value | ||
|---|---|---|---|---|---|
| Yes (%) | No or not sure (%) | Yes (%) | No or not sure (%) | ||
| Enjoyment during program | 250 (100) | 0 (0) | 250 (100) | 0 (0) | N/A |
| Easy to learn | 245 (98) | 5 (2) | 250 (100) | 0 (0) | 0.07 |
| Safe to perform | 250 (100)* | 0 (0) | 240 (96) | 10 (4) | 0.004 |
| Enhanced my confidence | 250 (100) | 0 (0) | 250 (100) | 0 (0) | N/A |
| I feel more balanced and stable | 243 (97)* | 7 (3) | 230 (92) | 20 (8) | 0.018 |
| Intention to continue | 250 (100) | 0 (0) | 250 (100) | 0 (0) | N/A |
| Understood instructions | 243 (97) | 7 (3) | 245 (98) | 5 (2) | 0.77 |
| Would recommend it to other PD patients | 250 (100) | 0 (0) | 250 (100) | 0 (0) | N/A |
Data are reported as number (percentage). Chi-squared independent test was performed to statistical analysis. N/A: Not applicable.
*P<0.05 compared to RE group.
Physical performance measures
Results for the timed up-and-go test, 50-foot walk test, and functional reach were improved by Tai Chi and routine exercise (P<0.05 for all) but the TC group had greater improvements (Supplementary Table S1).
Clinical evaluations
In the TC group, at the end of follow-up, 22 (9%) patients were successful in withdrawing levodopa or equivalent treatment. Also, a decrease in the daily dose of levodopa or equivalent was seen in the TC group in those who continued on levodopa (Supplementary Table S2).
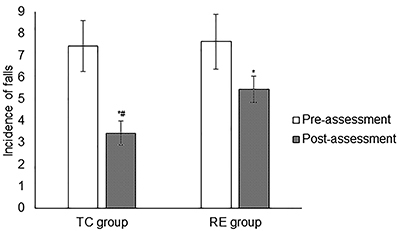
Incidence of falls
Incidence of falls within 6 months from the start of treatment to the follow-up period were decreased in the TC group (7.45±1.18 vs 3.45±0.55, P<0.0001, q=60.463) and RE group (7.65±1.26 vs 5.46±0.59, P<0.0001, q=32.876), but Tai Chi decreased incidence of falls significantly more than routine exercise (P<0.0001, q=38.512, Figure 2).
Figure 2. Incidence of falls for Parkinson's disease patients who performed Tai Chi (TC) or routine exercise (RE) programs. Data are reported as means±SD. Total number of patients enrolled were 250 for both groups. *P<0.05 compared to pre-assessment; #P<0.05 compared to RE group. Paired sample t-test was performed for statistical analysis. Pre-assessment: Incidence of falls in previous 6-months. Post-assessment: Incidence of falls within 6-months from start of physical therapy and follow-up period.
Adverse events and attrition
No attrition occurred during the whole program period or during follow-up. Also, no injury or fall was observed in patients of the TC group. Among the participants of the RE group, just 2 subjects experienced a fall during the first week of intervention.
Discussion
Patients' response towards Tai Chi and routine exercises
All the enrolled participants showed interest and enjoyed physical therapy. Participants of both groups reported satisfaction. Participants of both groups felt more balanced with better stability in their gait. The results of the study were consistent with a previous study (19). The program was safe and successful in terms of achieving the objective of making elderly PD patients familiar with Tai Chi and other exercises.
Physical performance measures
The results of our study were consistent with randomized controlled trials (9,10). In early and mild-stage PD, when the development of disease starts, symptoms like shaking of hands, difficulty in walking, slowness in movement, and rigidity become obvious (1). Exercise (20) and dance (11) help PD patients in the improvement of both motor and non-motor complications. Tai Chi is a common Chinese martial art that involves posture maintenance and controlled movements in a slow and flowing fashion. This exercise technique includes movements such as extension of knees and hips, weight shifting and flexion, rotation of the trunk, and coordinated movement of arms (21). Treadmill training might be better suited for young and fit people than for elderly PD patients (22). The Tai Chi program together with proper medication resulted in improved motor function and mobility (23). Routine exercise does not change basic symptomatology (24). The study showed that routine exercises do not help in the enhancement of stability and Tai Chi does help in improving motor activity of PD patients.
Incidence of falls
Tai Chi decreased chances of fall more than routine exercise. The results of the study were consistent with the community-based falls prevention program (25) and randomized controlled trials (10,26). PD patients develop dysrhythmic, slow, and shuffling gait (27). Loss of balance also occurs as disease advances (8). Tai Chi is a balance-based exercise. In this exercise, the center of gravity varies with each movement, challenging the balance control system (28). This exercise involves gentle and slow movements along with relaxation induced via deep breathing. Tai Chi has been reported to be very effective in preventing falls in elderly individuals (26). PD patients that perform Tai Chi experience body awareness and balance improvement (15). Tai Chi is recommended for PD patients who have experienced postural instability and are at an increased risk of falling.
Clinical evaluations
In PD patients, loss in motor function occurs due to the death of neurons in the substantia nigra, which is a region of the central nervous system. Mechanisms behind the occurrence of PD are not well understood but it is believed that it is due to insufficient production of dopamine, which results in successive aggregation of protein and alpha-synuclein in Lewy bodies present in neurons (1). The efficacy of Tai Chi specifically in case of PD is explained by its role in normalizing the levels of neurotransmitters including dopamine and acetylcholine in various regions of the brain, i.e., cortex, basal ganglia, and motor cortex feedback loop. When Tai Chi is practiced daily, it promotes the development of various de novo neural pathways in a PD patient that results in fast response to posture challenges (10). Tai Chi exercise delayed the introduction of levodopa.
Adverse effects
No adverse effect of the physical therapy was observed in the patients. All the exercises were safe for PD patients, except for dance, which disturbed the balance of 2 PD patients and they experienced a fall; however, no exercise-related injury occurred.
Limitations
Although the study spanned over a short period of time, its results supported Tai Chi as an effective therapy for PD patients. This retrospective study indicated a direction for future studies that would involve post-therapy measurements. The other limitations of the study were that all participants agreed voluntarily and the results of the study might suffer from the placebo effect (29). Generalizability of results can also be a problem as Tai Chi is popular in China but not in other populations, resulting in implementation issues. The effect of exercise on other parameters related to PD like rigidity of skeletal muscles, depression, etc. was not evaluated. Duration of exercise time was relatively short. A randomized clinical trial is required for a longer period of exercise time.
Conclusions
The results of this study supported that Tai Chi was an effective meditation technique for people who have mild to moderate Parkinson's disease. The incorporation of Tai Chi in the daily life of Parkinson's disease patients allowed them to stay functionally and physically active. Improvement of physical parameters indicated that Tai Chi had the potential to slow down the progression of Parkinson's disease and delay the introduction of levodopa.
Acknowledgments
The authors are thankful for the medical and non-medical staff of the Gaomi People's Hospital and the Lishui People's Hospital.
Supplementary Material.
Click here to view [pdf].
References
- 1.Kalia LV, Lang AE. Parkinson's disease. Lancet. 2015;386:896–912. doi: 10.1016/S0140-6736(14)61393-3. [DOI] [PubMed] [Google Scholar]
- 2.Sveinbjornsdottir S. The clinical symptoms of Parkinson's disease. J Neurochem. 2016;139:318–324. doi: 10.1111/jnc.13691. [DOI] [PubMed] [Google Scholar]
- 3.Tysnes OB, Storstein A. Epidemiology of Parkinson's disease. J Neural Transm. 2017;124:901–905. doi: 10.1007/s00702-017-1686-y. [DOI] [PubMed] [Google Scholar]
- 4.Poewe W, Seppi K, Tanner CM, Halliday GM, Brundin P, Volkmann J, et al. Parkinson disease. Nat Rev Dis Primers. 2017;3:17013. doi: 10.1038/nrdp.2017.13. [DOI] [PubMed] [Google Scholar]
- 5.Miller IN, Cronin-Golomb A. Gender differences in Parkinson's disease: clinical characteristics and cognition. Mov Disord. 2010;25:2695–2703. doi: 10.1002/mds.23388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barranco Quintana JL, Allam MF, Del Castillo AS, Navajas RF. Parkinson's disease and tea: a quantitative review. J Am Coll Nutr. 2009;28:1–6. doi: 10.1080/07315724.2009.10719754. [DOI] [PubMed] [Google Scholar]
- 7.Toh SM. A systematic review on the effectiveness of Tai Chi exercise in individuals with Parkinson's disease from 2003 to 2013. Hong Kong J Occup Th. 2013;23:69–81. doi: 10.1016/j.hkjot.2013.11.001. [DOI] [Google Scholar]
- 8.Allen NE, Sherrington C, Paul SS, Canning CG. Balance and falls in Parkinson's disease: a meta-analysis of the effect of exercise and motor training. Mov Disord. 2011;26:1605–1615. doi: 10.1002/mds.23790. [DOI] [PubMed] [Google Scholar]
- 9.Schenkman M, Hall DA, Baron AE, Schwartz RS, Mettler P, Kohrt WM. Exercise for people in early- or mid-stage Parkinson disease: a 16-month randomized controlled trial. Phys Ther. 2012;92:1395–1410. doi: 10.2522/ptj.20110472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li F, Harmer P, Fitzgerald K, Eckstrom E, Stock R, Galver J, et al. Tai Chi and postural stability in patients with Parkinson's disease. N Engl J Med. 2012;366:511–519. doi: 10.1056/NEJMoa1107911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Earhart GM. Dance as therapy for individuals with Parkinson disease. Eur J Phys Rehabil Med. 2009;45:231–238. [PMC free article] [PubMed] [Google Scholar]
- 12.King LA, Horak FB. Delaying mobility disability in people with Parkinson disease using a sensorimotor agility exercise program. Phys Ther. 2009;89:384–393. doi: 10.2522/ptj.20080214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tomlinson CL, Patel S, Meek C, Herd CP, Clarke CE, Stowe R, et al. Physiotherapy intervention in Parkinson's disease: Systematic review and meta-analysis. BMJ. 2012;345:e5004. doi: 10.1136/bmj.e5004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American College of Sports Medicine. Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, et al. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41:1510–1530. doi: 10.1249/MSS.0b013e3181a0c95c. [DOI] [PubMed] [Google Scholar]
- 15.Zhou J, Yin T, Gao Q, Yang XC. A meta-analysis on the efficacy of Tai Chi in patients with Parkinson's disease between 2008 and 2014. Evid Based Complement Alternat Med 2015; 2015:593263. doi: 10.1155/2015/593263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sumec R, Filip P, Sheardova K, Bares M. Psychological benefits of nonpharmacological methods aimed for improving balance in Parkinson's disease: a systematic review. Behav Neurol. 2015;2015:620674. doi: 10.1155/2015/620674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brienesse LA, Emerson MN. Effects of resistance training for people with Parkinson's disease: a systematic review. J Am Med Dir Assoc. 2013;14:236–241. doi: 10.1016/j.jamda.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 18.Li J, Jin M, Wang L, Qin B, Wang K. MDS clinical diagnostic criteria for Parkinson's disease in China. J Neurol. 2017;264:476–481. doi: 10.1007/s00415-016-8370-2. [DOI] [PubMed] [Google Scholar]
- 19.Cheon SM, Chae BK, Sung HR, Lee GC, Kim JW. The efficacy of exercise programs for Parkinson's disease: Tai Chi versus combined exercise. J Clin Neurol. 2013;9:237–243. doi: 10.3988/jcn.2013.9.4.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van der Kolk NM, King LA. Effects of exercise on mobility in people with Parkinson's disease. Mov Disord. 2013;28:1587–1596. doi: 10.1002/mds.25658. [DOI] [PubMed] [Google Scholar]
- 21.Amano S, Nocera JR, Vallabhajosula S, Juncos JL, Gregor RJ, Waddell DE, et al. The effect of Tai Chi exercise on gait initiation and gait performance in persons with Parkinson's disease. Parkinsonism Relat Disord. 2013;19:955–960. doi: 10.1016/j.parkreldis.2013.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mehrholz J, Kugler J, Storch A, Pohl M, Elsner B, Hirsch K. Treadmill training for patients with Parkinson's disease. Cochrane Database Syst Rev. 2015;22:CD007830. doi: 10.1002/14651858.CD007830.pub4. [DOI] [PubMed] [Google Scholar]
- 23.Ni X, Liu S, Lu F, Shi X, Guo X. Efficacy and safety of Tai Chi for Parkinson's disease: A systematic review and meta-analysis of randomized controlled trials. PLoS One. 2014;19:e99377. doi: 10.1371/journal.pone.0099377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Dreu MJ, van der Wilk AS, Poppe E, Kwakkel G, van Wegen EE. Rehabilitation, exercise therapy and music in patients with Parkinson's disease: a meta-analysis of the effects of music-based movement therapy on walking ability, balance and quality of life. Parkinsonism Relat Disord. 2012;18:S114–S119. doi: 10.1016/S1353-8020(11)70036-0. [DOI] [PubMed] [Google Scholar]
- 25.Li F, Harmer P, Glasgow R, Mack KA, Sleet D, Fisher KJ, et al. Translation of an effective Tai Chi intervention into a community-based falls-prevention program. Am J Public Health. 2008;98:1195–1198. doi: 10.2105/AJPH.2007.120402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li F, Harmer P, Fitzgerald K, Eckstrom E, Akers L, Chou LS, et al. Effectiveness of a therapeutic Tai Ji Quan intervention vs a multimodal exercise intervention to prevent falls among older adults at high risk of falling: a randomized clinical trial. JAMA Intern Med. 2018;178:1301–1310. doi: 10.1001/jamainternmed.2018.3915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dibble LE, Addison O, Papa E. The effects of exercise on balance in persons with Parkinson's disease: a systematic review across the disability spectrum. J Neurol Phys Ther. 2009;33:14–26. doi: 10.1097/NPT.0b013e3181990fcc. [DOI] [PubMed] [Google Scholar]
- 28.Huang Y, Liu X. Improvement of balance control ability and flexibility in the elderly Tai Chi Chuan (TCC) practitioners: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2015;60:233–238. doi: 10.1016/j.archger.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 29.Whalley B, Hyland ME, Kirsch I. Consistency of the placebo effect. J Psychosom Res. 2008;64:537–541. doi: 10.1016/j.jpsychores.2007.11.007. [DOI] [PubMed] [Google Scholar]


