Abstract
Gastric cancer is the fifth most common cancer, and the third most prevalent cause of cancer-related deaths in the world. Voluminous evidence has demonstrated that phytochemicals play a critical role in the prevention and management of gastric cancer. Most epidemiological investigations indicate that the increased intake of phytochemicals could reduce the risk of gastric cancer. Experimental studies have elucidated the mechanisms of action, including inhibiting cancer cell proliferation, inducing apoptosis and autophagy, and suppressing angiogenesis as well as cancer cell metastasis. These mechanisms have also been related to the inhibition of Helicobacter pylori and the modulation of gut microbiota. In addition, the intake of phytochemicals could enhance the efficacy of anticancer chemotherapeutics. Moreover, clinical studies have illustrated that phytochemicals have the potential for the prevention and the management of gastric cancer in humans. To provide an updated understanding of relationships between phytochemicals and gastric cancer, this review summarizes the effects of phytochemicals on gastric cancer, highlighting the underlying mechanisms. This review could be helpful for guiding the public in preventing gastric cancer through phytochemicals, as well as in developing functional food and drugs for the prevention and treatment of gastric cancer.
Keywords: phytochemicals, gastric cancer, anticancer, mechanism of action
1. Introduction
According to the data from the World Health Organization in 2015, cancer has become an important cause of premature death in many countries [1]. Gastric cancer is the fifth most commonly diagnosed cancer in the world, and its mortality ranks third in cancers, with an estimated 783,000 deaths in 2018 [1,2]. Due to the high incidence and mortality rate, gastric cancer is considered a severe public health problem [3]. According to the anatomy of stomach, gastric cancer can be classified into cardia and noncardia gastric cancer. In histopathology, gastric cancer can be categorized into intestinal-type and diffuse-type [4]. Helicobacter pylori infection, high salt intake and smoking are considered to be the main risk factors for gastric cancer worldwide. In Europe, the amplification of HER-2 gene was found to be a risk factor [5]. In Asia, a study revealed that ethnicity plays a role in the onset of gastric cancer, and Chinese race was more susceptible to the cancer [6]. To date, chemotherapy, radiation therapy, and gastrectomy have been recognized as the main therapies for treating gastric cancer [7]. However, these therapies usually cause severe side effects or toxicity, thus restricting their application [8,9]. Additionally, the resistance of anticancer drugs also limits the success rate of chemotherapy [10]. Thus, it is urgent and necessary to find a more effective and less toxic strategy for the prevention and management of gastric cancer.
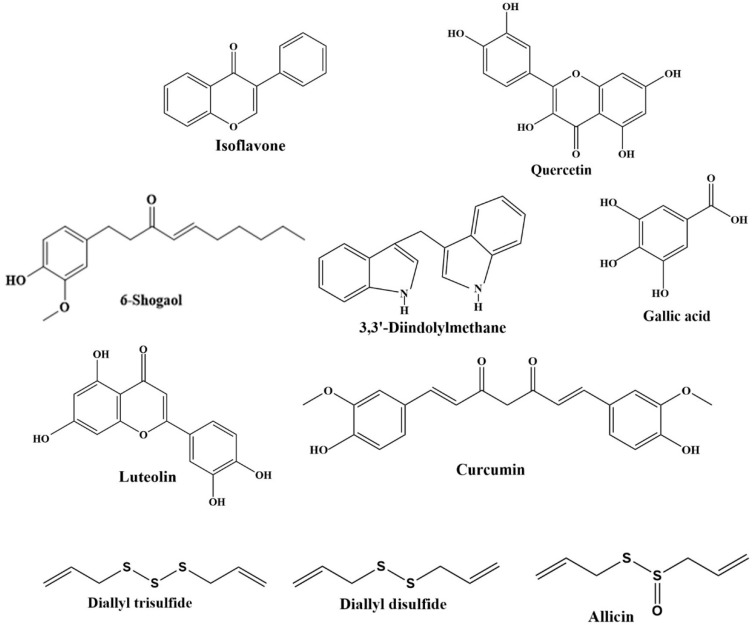
Diet plays a prominent role in gastric cancer prevention and management [11]. Increasing evidence from epidemiological studies indicated that natural dietary products have anticancer activity, such as fruits, vegetables, spices, soy, cereals, and edible macro-fungi [12,13,14,15]. Furthermore, many studies found that the risk of gastric cancer was inversely associated with the intake of natural products [16]. The beneficial effects of these natural products could be attributed to the phytochemicals [17,18,19], and the chemical structures of several phytochemicals are showed in Figure 1. In addition, experimental studies indicated that phytochemicals exhibited protective effects against gastric cancer through several mechanisms, including inhibition of cell proliferation [20], induction of apoptosis [21] and autophagy [22], anti-angiogenesis [23], suppression of cell metastasis [24], modulation of gut microbiota [25], and inhibition of Helicobacter pylori [26]. Moreover, the use of phytochemicals could be a promising adjuvant therapy for gastric cancer. This review aims to summarize the effects of phytochemicals on the prevention and management of gastric cancer, with the mechanisms of action intensively discussed, and it also illustrates the bioavailability and safety of phytochemicals.
Figure 1.
Chemical structures of several phytochemicals against gastric cancer.
2. Epidemiological Studies
Numerous epidemiological studies have demonstrated that the consumption of natural dietary products is essential to the prevention and management of gastric cancer [27,28]. A case-control study reported that the consumption of fresh fruits and vegetables could reduce the risk of gastric cancer with an odds ratio (OR) of 0.15 (95% CI, 0.04–0.64) [6]. In addition, the frequent intake of citrus fruits, vegetables, legumes, garlic, and olive oil showed protective effects against gastric cancer [29]. Additionally, the consumption of garlic, onion, and citrus fruits was reported to decrease the risk of gastric cancer with ORs of 0.35 (95% CI, 0.13–0.95), 0.34 (95% CI, 0.19–0.62), and 0.31 (95% CI, 0.17–0.59), respectively [30]. A meta-analysis also found that the high intake of citrus fruits could reduce the risk of gastric cancer (OR, 0.72; 95% CI, 0.64–0.81) [31]. Moreover, the increased intake of mushroom and soybean products was associated with a lower risk of gastric cancer with OR of 0.30 (95% CI, 0.15–0.62) and 0.35 (95% CI, 0.16–0.75), respectively [32].
Several cohort studies also reported that the intake of fresh fruits and vegetables was inversely associated with the risk of gastric cancer [33,34]. The intake of total plant food, including whole grains, vegetables, and citrus fruit, was negatively related to gastric cancer risk in men (RR, 0.79; 95% Cl, 0.67–0.93) [35]. Furthermore, higher consumption of brassica vegetables and citrus fruits was correlated with a decreased risk of gastric noncardia cancer with RRs of 0.51 (95% CI, 0.28–0.92) and 0.38 (95% CI, 0.21–0.69), respectively [34]. In addition, a meta-analysis revealed that high intake of allium vegetables could decrease the risk of gastric cancer (OR, 0.54; 95% CI, 0.43–0.65) [36]. Additionally, a decrease in gastric cancer risk was observed with increased intake of yellow vegetable and white vegetable with ORs of 0.64 (95% Cl, 0.45–0.92) and 0.48 (95% Cl, 0.25–0.89), respectively [33]. High consumption of green and yellow vegetables was associated with lower mortality of gastric cancer (RR, 0.4; 95% CI, 0.2–0.9) [34]. Moreover, soy products also had a protective effect against gastric cancer [18,37]. A prospective study suggested that the intake of total soy products could decrease the risk of gastric cancer death with hazard ratio (HR) of 0.5 (95% CI, 0.26–0.93) [28]. Additionally, the consumption of tofu was inversely associated with distal gastric cancer risk in men (HR, 0.64; 95% CI, 0.42–0.99), and the high intake of dry bean showed a protective effect against gastric cancer in postmenopausal women (HR, 0.63; 95% CI, 0.43–0.91) [38].
The phytochemicals in the dietary natural products played a critical role in reducing the risk of gastric cancer. For example, a case-control study suggested that the intake of total quercetin in foods and beverages was reversely related to the risk of noncardiac gastric adenocarcinoma, with an adjusted OR of 0.57 (95% CI, 0.40–0.83) [19]. Additionally, a nested case-control study revealed that the increased plasma level of β-carotene mainly from fruits and vegetables was associated with the reduced risk of gastric cancer (OR, 0.46; 95% CI, 0.28–0.75) [39]. Another study showed that the concentration of isoflavones in serum was negatively related to gastric cancer risk [37]. Moreover, the increased intake of total dietary flavonoids and lycopene was related to the decreased risk of gastric cancer with ORs of 0.49 (95% CI, 0.31–0.76) and 0.60 (95% CI, 0.42–0.85), respectively [40,41]. Furthermore, a high intake of anthocyanidins presented a reduction in the mortality of gastric cardia cancer (HR, 0.63; 95% CI, 0.42–0.95) [42]. In addition, another study found that isothiocyanates were effective in protecting against gastric cancer, particularly among those who were lack of genes GSTMI (glutathione S-transferase M1) and GSTTI (glutathione S-transferase T1) (OR, 0.44; 95% CI, 0.21–0.93) [43].
However, there are inconsistent results in some epidemiological studies regarding the association between the consumption of fruits and vegetables and gastric cancer risk [44,45]. A cohort study demonstrated that the intake of fruits was not significantly correlated with the risk of gastric cancer, while high consumption of green leafy vegetables and root vegetables significantly reduced the risk of gastric cancer with HRs of 0.64 (95% CI, 0.42–0.99) and 0.43 (95% CI, 0.27–0.69), respectively [46]. Additionally, a pooled analysis of four cohort studies demonstrated that the total vegetable consumption was inversely related to distal gastric cancer risk in men (multivariate HR, 0.78; 95%CI, 0.63–0.97), whereas there was no association between total fruit intake and the risk of gastric cancer [44]. Furthermore, an inverse association was observed between fruit consumption and distal gastric cancer risk in men (HR, 0.50; 95% CI, 0.29–0.84), while no relation was found in women [47]. In a prospective study, citrus fruit intake could decrease the risk of gastric cardia cancer, but the intake of vegetables was not related to the risk of gastric cancer [45]. Furthermore, evidence from cohort studies pointed out that the consumption of garlic was not correlated with gastric cancer risk, with a pooled multivariable RR of 1.39 (95% CI, 0.89–2.17) [48]. Additionally, it was inconsistent with the effects of some phytochemicals on the incidence of gastric cancer. The intake of isoflavone or flavonoid showed no relationship with gastric cancer risk [49,50]. Moreover, no association was found between the intake of carotenoids and the risk of gastric cancer [51]. The inconsistent results might be due to the consumed levels of phytochemicals and the differences in regions, dietary, and lifestyles, as well as the data accessing methods [37].
Overall, most epidemiological investigations have suggested that the consumption of natural dietary products is inversely associated with the risk of gastric cancer (Table 1). The protective effects of natural dietary products against gastric cancer could be attributed to the phytochemicals. However, several cohort studies have found that the intake of some vegetables, fruits, and phytochemicals had no effects on gastric cancer. Thus, more epidemiological studies with better design and quality control are needed in the future.
Table 1.
The effects of natural dietary products against gastric cancer from epidemiological studies.
| Natural Products | Phytochemicals | Subjects | Study Type | Consumed Levels | Effects | Ref. |
|---|---|---|---|---|---|---|
| Fruits | ||||||
| Citrus fruits | NA | 217 Gastric cancer cases (mean age: 65.4; 151 men) and controls (mean age: 64.3; 265 men) in Iran | Case-control | ≥3 times/week vs. never or infrequently intake of citrus fruits | Reducing gastric cancer risk (OR, 0.31; 95% CI, 0.17–0.59) | [30] |
| Citrus fruits | NA | 120,852 Subjects in Netherlands (58,279 men and 62,573 women), 156 gastric cardia adenocarcinoma cases and 460 gastric noncardia adenocarcinoma cases; aged 55–69 years | Cohort study | The highest (median = 156 g/d) vs. the lowest quintile (median = 0 g/d) of citrus fruits | Reducing the risk of gastric noncardia cancer (RR, 0.38; 95% CI, 0.21–0.69) | [34] |
| Total fruits (except watermelon) | NA | 559,247 Chinese men in the cohort and 132 distal gastric cancer cases; aged 40–74 years | Cohort study | >104.2 vs. ≤20.1 g/d all fruits (except watermelon) | Reducing distal gastric cancer risk (HR, 0.50; 95% CI, 0.29–0.84) | [47] |
| Total fruits (except watermelon) | NA | 73,064 Chinese women in the cohort and 206 distal gastric cancer cases; aged 40–70 years | Cohort study | >208.0 vs. ≤61.5 g/d all fruits (except watermelon) | No association (HR, 1.02; 95% CI, 0.68–1.54) | |
| Total fruit | NA | 191,232 Japanese subjects, (87,771 men and 103,461 women) and 2995 gastric cancer cases (2104 men and 891 women) | Pooled analysis | The highest quintile vs. the lowest quintile of total fruit | No association (HR, 0.9; 95% CI, 0.67–1.22) | [44] |
| Vegetables | ||||||
| Brassica vegetables | NA | 120,852 Subjects in Netherlands (58,279 men and 62,573 women), 156 gastric cardia adenocarcinoma cases and 460 gastric noncardia adenocarcinoma cases; aged 55–69 years | Cohort study | The highest (median = 59 g/d) vs. the lowest quintile (median = 11 g/d) of Brassica vegetables | Reducing the risk of gastric noncardia cancer (RR, 0.51; 95% CI, 0.28–0.92) | [34] |
| Total vegetables | NA | 559,247 Chinese men in the cohort and 132 distal gastric cancer; aged 40–74 years | Cohort study | >429.3 vs. ≤212.9 g/d total vegetables | No association (HR, 1.00; 95% CI, 0.59–1.68) | [47] |
| Total vegetables | NA | 73,064 Chinese women in the cohort and 206 distal gastric cancer cases; aged 40–70 years | Cohort study | >373.7 vs. ≤179.5 g/d total vegetables | No association (HR, 0.89; 95% CI, 0.60–1.31) | |
| Total vegetables | NA | 191,232 Japanese subjects, (87,771 men and 103,461 women) and 2995 gastric cancer cases (2104 men and 891 women) | Pooled analysis | The highest quintile vs. the lowest quintile of total vegetable | Reducing distal gastric cancer risk in men (multivariate HR, 0.78; 95% CI, 0.63–0.97) | [44] |
| Fruits and vegetables | ||||||
| Fruits and vegetables | β-carotene | 511 Japanese gastric cancer cases (342 men) and 511 controls (342 men); aged 40–69 years | Nested case-control | ≥27.0 vs. ≤8.0 ug/dL β-carotene | Reducing gastric cancer risk (OR, 0.46; 95% CI, 0.28–0.75) | [39] |
| Vegetables, citrus fruits, and whole grains | NA | 970,045 American subjects (533,391 women and 436,654 men) and 439 women and 910 men died from gastric cancer | Cohort study | The highest vs. the lowest tertile of plant foods | Reducing gastric cancer risk in men (RR, 0.79; 95% CI, 0.67–0.93) | [35] |
| Fruits, vegetables and beverages | Quercetin | 505 Swedish gastric cancer cases (336 men) and 1116 controls (746 men); aged 40–79 years | Case-control | ≥11.9 vs. <4 mg /day quercetin | Reducing noncardia gastric adenocarcinoma risk (OR, 0.57; 95% CI, 0.40–0.83) | [19] |
| Spices | ||||||
| Allium vegetables | NA | 543,220 Total subjects | Meta-analysis | The highest vs. the lowest consumption category of allium vegetables | Reducing gastric cancer risk (OR, 0.54; 95% CI, 0.43–0.65) | [36] |
| Garlic | NA | 217 Gastric cancer cases (mean age: 65.4; 151 men) and controls (mean age: 64.3; 265 men) in Iran | Case-control | ≥3 times/week vs. never or infrequently intake of garlic | Reducing gastric cancer risk (OR, 0.35; 95% CI, 0.13–0.95) | [30] |
| Onion | NA | ≥ once per day vs. ≤2 times/week onion | Reducing gastric cancer risk (OR, 0.34; 95% CI, 0.19–0.62) | |||
| Soy and soy products | ||||||
| Soy | Isoflavone | 84,881 Japanese subjects (39,569 men and 45,312 women), 1249 gastric cancer cases; aged 45–74 years | Cohort study | The highest vs. the lowest quartile of isoflavone | No association (HR, 1.00; 95% CI, 0.81-1.24 for men and HR, 1.07; 0.77–1.50 for women) | [49] |
| Soy | Isoflavone | 30,792 Japanese subjects (14,219 men and 16,573 women), 678 gastric cancer cases (441 men and 237 women); aged ≥ 35 years | Cohort study | >53 vs. ≤28 mg/d isoflavone | Reducing gastric cancer risk in women (HR, 0.60; 95% CI, 0.37–0.98) | [18] |
| >122 vs. ≤62 g/d soy food | Reducing gastric cancer risk in men(HR, 0.71; 95% CI, 0.53–0.96) and women (HR, 0.58; 95% CI, 0.36–0.94) | |||||
| Tofu | NA | 128,687 Chinese subjects (70,446 women and 58,241 men), 493 distal gastric cancer cases; aged 40–74 years | Cohort study | >8.4 vs. <3.1 g/d tofu | Reducing distal gastric cancer risk in men (HR, 0.64; 95% CI, 0.42–0.99) | [38] |
| Dry bean | NA | >0.9 vs. 0.0 g/d dry bean | Reducing gastric cancer risk in postmenopausal women (HR, 0.63; 95% CI, 0.43–0.91) | |||
| Total soy product | NA | 30,304 Japanese subjects (13,880 men and 16,424 women) and 121 gastric cancer deaths; aged ≥ 35 years | Cohort study | The highest (median = 49.7 g/d) vs. the lowest tertile (median = 140 g/d) of total soy product | Reducing the risk of gastric cancer death (HR, 0.5; 95% CI, 0.26–0.93) | [28] |
| Cereals | ||||||
| Other | ||||||
| Flavonoids | 469,008 American subjects (275,982 men and 193,026 women), 1297 gastric cancer cases; aged 50–71 years | Cohort study | 438.0–4211.2 vs. 0–84.1 mg/d total flavonoids | No association (HR, 1.02; 95% CI, 0.78–1.34) for gastric cardia cancer; (HR, 1.11; 95% CI, 0.86–1.44) for gastric noncardia cancer | [50] | |
| Flavonoids | 334 Korean gastric cancer cases (208 men) and 334 controls (208 men); aged 35–75 years | Case-control study | The highest tertile (median = 152.3 mg/d) vs. the lowest tertile (median = 52.5 mg/d) of flavonoids | Reducing gastric cancer risk (OR, 0.49; 95% CI, 0.31–0.76) | [40] | |
| Anthocyanidins | 248 American gastric cardia cancer cases and 662 controls; aged 30–79 years | Case-control study | ≥18.48 vs. ≤7.21 mg/d anthocyanidins | Reducing the risk of mortality for gastric cardia cancer (HR, 0.63; 95% CI, 0.42–0.95) | [42] |
NA: not available.
3. Experimental Studies
The effects of phytochemicals against gastric cancer have been extensively investigated, and the mechanisms of action have been also explored. These anti-cancer effects and mechanisms will be intensively discussed below.
3.1. Inhibition of Cell Proliferation
It has been well documented that various phytochemicals can inhibit the proliferation of human gastric cancer cells and the growth of gastric tumors in mice. In several in vitro studies, allitridi [52], mycelia and polysaccharides of a mushroom [20], labdane diterpenes in Curcuma mangga rhizomes [53], poncirin [54], and apigenin [55] were found to inhibit the proliferation of human gastric cancer cell lines. Additionally, the extract of ramson could arrest AGS human gastric cancer cells in G2/M phase via the downregulation of cyclin B, resulting in the inhibition of proliferation [56]. Additionally, diallyl disulfide isolated from garlic could arrest MGC803 human gastric cancer cells at the G2/M phase by activating the expression of checkpoint kinase-1(Chk1), as well as ataxia telangiectasia and Rad3-related (ATR) protein kinases, and decreasing the expression of cell division cycle 25C (CDC25C) and cyclin B1 [57]. Another study found that the activation of p38 mitogen-activated protein kinase (MAPK) pathway was involved in diallyl disulfide-induced G2/M arrest [58]. It could also induce the differentiation of MGC803 cells by decreasing the phosphorylation of extracellular signal-regulated kinase (ERK1/2) protein [59]. Furthermore, diallyl trisulfide, a garlic organosulfide showed an antiproliferative effect on AGS cells by inducing mitotic arrest with increased expression of cyclin B1 and tumor suppressor p53 [60]. Moreover, latcripin 1 from a mushroom had an antiproliferative effect against SGC-7901 and BGC-823 gastric cancer cells by arresting cells at the S phase [61]. Furthermore, myricetin exhibited an antiproliferative effect against HGC-27 and SGC7901 cells by downregulating the expression of cyclinB1, cyclinD1, CDK1, and CDC25C [62]. An in vivo study pointed out that S-allylmercaptocysteine, one of the garlic derivatives, could suppress the growth of SGC-7901 xenografts in BALB/c nude mice [63]. In addition, 6-shogaol from ginger inhibited the gastric tumor growth in athymic nude mice, and it was also found to inhibit the viability of gastric cancer cells, damage microtubules and induce mitotic arrest [64]. Furthermore, (-)-epigallocatechin gallate (EGCG) inhibited the proliferation of SGC-7901 gastric cancer cells and the growth of gastric tumors in mice by suppressing Wnt/β-catenin signaling [65].
3.2. Induction of Apoptosis
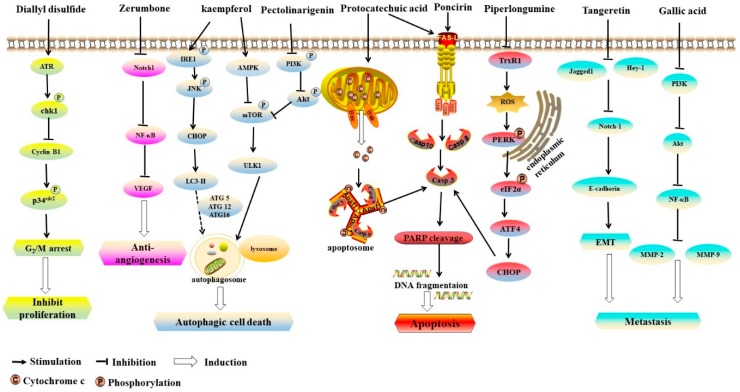
Induction of apoptosis has been found to be a pivotal mechanism of the inhibition on the initiation and the development of cancer [66,67,68]. It was found that protocatechuic acid could induce the apoptosis of AGS cells through Fas/Fas ligand (FasL) death receptor or mitochondrial pathways accompanied with phosphorylation of c-Jun N-terminal kinase (JNK), p38 mitogen-activating protein kinases (MAPK), and p53 [69]. Additionally, poncirin, rich in citrus fruits, could induce apoptosis in AGS cells via death receptor pathway with increased level of FasL protein, activation of Caspase-8 and Caspase-3, and cleavage of poly (ADP-ribose) polymerase (PARP) [70]. Additionally, the treatment of Citrus reticulata Blanco extract could increase apoptosis in SNU-668 human gastric cancer cells through upregulating the expression of B-cell lymphoma 2 (Bcl-2)-associated X protein (Bax) and Caspase-3 [71]. Furthermore, an in vitro study demonstrated that α-mangostin isolated from the pericarp of mangosteen induced apoptosis of BGC-823 and SGC-7901 human gastric cancer cell lines via the reduction of the mitochondrial membrane potential, and the suppression of STAT3 signaling pathway with decreased B-cell lymphoma-extralarge (Bcl-xL) and apoptosis regulator Mcl-1 protein levels [72]. In human gastric signet ring carcinoma cells, the extract of dried ripe fruit of Vitex agnus-castus induced apoptosis via intracellular oxidative stress and mitochondrial membrane damage [73]. Moreover, hispolon, a phenolic compound of Phellinus linteus, exhibited cytotoxic activity against human gastric cancer cells but not normal gastric cells via the induction of apoptosis, associated with the mitochondrial pathway [74]. Furthermore, the black soybean extracts induced apoptosis of AGS cells in a dose-dependent manner by increasing the levels of Bax and Caspase-3, as well as the cleavage of PARP [75]. It was found that piperlongumine (isolated from the fruit of long pepper) inhibited the activity of thioredoxin reductase 1 (TrxR1), resulting in the induction of apoptosis in human gastric cancer cells via reactive oxygen species (ROS)-triggered ER-stress and mitochondrial dysfunction [21]. In addition, it was observed that allitridi could lead to apoptosis by decreasing the expression of Bcl-2 and increasing the level and activity of Caspase-3 in BGC823 human gastric cancer cell line [52]. Furthermore, it was found that catechin extract and EGCG of green tea [76], theaflavins of black tea [77], and polyphenol extract of oolong tea [78] could induce apoptosis in KATO III human gastric cancer cells. In murine gastric cancer syngeneic model, bamboo-shaving polysaccharides inhibited tumor growth and prolonged the survival of mice bearing a gastric tumor by inducing tumor cell apoptosis [79]. Accumulating evidence has suggested that phytochemicals can induce apoptosis of gastric cancer cells mainly through death receptors or mitochondrial pathways (Figure 2).
Figure 2.
The anticancer mechanisms of phytochemicals on gastric cancer. Diallyl disulfide induced G2/M arrest by activating MAPK pathway. Zerumbone showed anti-angiogenesis activity via the inhibition of Notch1/NF-κB/VEGF pathway. Kaempferol induced autophagic cell death via IRE1/JNK/CHOP and AMPK/ULK1 pathways. Pectolinarigenin induced autophagic cell death via PI3K/Akt/mTOR pathway. Poncirin induced apoptosis via the death receptor pathway. Piperlongumine induced apoptosis via ROS-triggered ER-stress and mitochondrial dysfunction, while protocatechuic acid induced apoptosis either through Fas/FasL death receptor or mitochondrial pathways. Tangeretin inhibited migration and invasion by reducing the expressions of Notch-1, Jagged1/2 and Hey-1. Gallic acid could suppress metastasis by downregulating PI3K/Akt pathway.
3.3. Autophagy
Autophagy is an important process of intracellular material renewal and recycle. Some damaged proteins or organelles are engulfed by autophagosomes and sent to autolysosomes for degradation [80]. It has been demonstrated that autophagy plays a dual role in the development of cancer [22,81]. On one hand, under most conditions, autophagy can induce autophagic cancer cell death. On the other hand, autophagy can suppress apoptosis, contributing to the survival of cancer cells sometimes. In gastric cancer cells, the treatment of kaempferol, a natural flavonoid, induced autophagic cell death via inositol-requiring-1 (IRE1)/JNK/-CCAAT-enhancer-binding protein homologous protein (CHOP), AMPK/UNC-51-like autophagy activating kinase 1 (ULK1), and histone deacetylase (HDAC)/G9a (a histone lysine 9 dimethylation-specific methyltransferase) pathways [22]. Additionally, pectolinarigenin extracted from Cirsium chanroenicum showed anticancer activity by inducing autophagy in AGS and MKN-28 human gastric cancer cells, mainly through the downregulation of phoshatidylinositol-3-kinase (PI3K)/protein kinase B (Akt)/mammalian target of rapamycin (mTOR) pathway [82]. In addition, 3,3’-diindolylmethane isolated from cruciferous vegetables increased the expression of autophagy-related 5 (ATG5) and microtubule associated protein light chain 3 (LC3) in gastric cancer cells and decreased the level of microRNA-30e, which targets gene ATG5 to inhibit its translation [83]. Moreover, the treatment of latcripin 1 protein present in Lentinula edodes could lead to autophagy in SGC-7901 and BGC-823 gastric cancer cell lines accompanied with the formation of autophagosomes via the change of LC3I into LC3II [61]. Furthermore, perillaldehyde isolated from Perilla frutescens displayed anticancer effects against gastric cancer both in vitro and in vivo. In MFCs mouse and GC9811-P human gastric cancer cells, perillaldehyde increased the phosphorylation of AMPK, leading to autophagy in the cells [84]. In mice bearing gastric tumor, perilaldehyde treatment inhibited the growth of the gastric tumor and upregulated the levels of autophagy-associated proteins, such as beclin-1, LC3-II, and cathepsin. However, it was found that quercetin induced protective autophagy against the apoptosis of AGS and MKN-28 gastric cancer cells, suggesting that autophagy could contribute to the survival of cancer cells in certain circumstances [85].
3.4. Inhibition of Tumor Angiogenesis
It has been reported that angiogenesis is critical for tumor growth and survival prognosis of gastric cancer [86]. Vascular endothelial growth factor (VEGF), a cytokine produced by tumor cells, plays an important role in angiogenesis [87]. Luteolin, a dietary flavonoid, was found to inhibit angiogenesis and the formation of vasculogenic mimicry tube in MGC-803 and Hs-746T gastric cancer cells via the suppression of notch receptor 1 (Notch1)/VEGF signaling [88]. Additionally, zerumbone, a bioactive component of ginger, showed anti-angiogenesis activity in AGS cells by decreasing the expression of VEGF via the inhibition of nuclear factor kappa light chain-enhancer of activated B cells (NF-κB) [89]. Moreover, in SGC-7901 and AGS human gastric cancer cell lines, nitidine chloride, generated from Zanthoxylum nitidum (Roxb) DC, was found to inhibit signal transducer and activator of transcription 3 (STAT3) signaling, which was associated with tumor angiogenesis. In a xenograft mouse model induced by SGC-7901 cells, the treatment of nitidine chloride reduced the volume of tumors via the inhibition of angiogenesis with decreased levels of STAT3 and VEGF [23].
3.5. Suppression of Cell Metastasis
Invasion and metastasis play a crucial role in the progression of gastric cancer [90]. Several studies found that phytochemicals could inhibit the invasion and metastasis of gastric cancer cells. It was reported that erinacine A present in Hericium erinaceus mycelium could inhibit the viability and invasiveness of MKN-28 and TSGH 9201 human gastric cancer cells [91]. In addition, luteolin was effective in suppressing invasion and migration by inhibiting Notch1 signaling and reversing epithelial-mesenchymal transition (EMT) in Hs-746T and MKN-28 gastric cancer cells [92]. Additionally, in SGC7901 cells, tangeretin, a polymethoxylated flavonoid of citrus fruits, inhibited radiation-mediated EMT, migration, and invasion by reducing the expression of Notch-1, two serrate-like ligands (Jagged1/2), two transcription factors (Hey-1 and Hes-1), and increasing the level of miR-410, a tumor-suppressive microRNA [93]. Moreover, gallic acid could suppress the metastasis of AGS cells through decreasing the level of matrix metalloproteinase (MMP)-2, MMP-9, and the activity of NF-κB, and downregulating PI3K/Akt pathway [90]. Gallic acid decreased the expression of RAS, but increased the expression of RhoB. Furthermore, diallyl disulfide inhibited gastric adenocarcinoma cell motility and invasiveness by increasing the tightness of tight junctions and decreasing the levels of MMP-2 and MMP-9 [94].
3.6. Inhibition of Helicobacter Pylori
Accumulating studies have suggested that Helicobacter pylori infection can cause various gastric diseases, such as chronic gastritis, peptic ulcers, and atrophic gastritis. The Helicobacter pylori infection is highly related to the pathogenesis of gastric cancer, particularly the intestinal type [95,96,97]. It was reported that infection with cytotoxin-associated gene antigen cagA+ strains of Helicobacter pylori might lead to severe gastric inflammation and gastric cancer [98,99]. Moreover, the growth of Helicobacter pylori cagA+ strains could be suppressed by curcumin and gingerols in vitro [26,100]. In NCI-N87 gastric carcinoma cells, the expression of CD74 in Helicobacter pylori, an adhesion molecule to urease, decreased by bergamottin, a component of citrus fruit, leading to the inhibition of Helicobacter pylori adhesion [101]. In addition, the treatment of apigenin, a flavonoid rich in celery, could inhibit Helicobacter pylori colonization, and reduce the incidence rate of gastric cancer in Helicobacter pylori-infected Mongolian gerbils [102]. Additionally, an in vivo study revealed that curcumin was effective in eliminating Helicobacter pylori from infected mice and alleviating Helicobacter pylori-induced gastric damage [103].
3.7. Modulation of Gut Microbiota
In recent years, the relationship between gut microbiota and multiple diseases has attracted much attention. The role of gut microbiota on gastric cancer has also been investigated [104,105]. A study revealed that microbiota might be related to gastric cancer, since specific pathogen-free mice were easier to develop atrophic gastritis and gastric cancer than germ-free mice [106]. It was reported that phytochemicals could prevent and manage some cancers via the modulation of gut microbiota, such as colorectal cancer, liver cancer and breast cancer [66]. However, there have been few reports about the anti-gastric cancer of phytochemicals by modulating gut microbiota, which may warrant further elucidation.
3.8. Adjuvant Therapy
Numerous studies have indicated that phytochemicals can enhance the sensitivity of gastric cancer to therapy, and exert a synergistic anticancer effect. A study pointed out that gartanin, a bioactive compound isolated from mangosteen, enhanced the sensitization of AGS human gastric adenocarcinoma cells to tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) by increasing death receptor 5 [107]. In addition, curcumin was found to enhance the anticancer efficacy of etoposide and doxorubicin, two chemotherapeutic drugs, in SGC-7901 human gastric cancer cells by inhibiting the activation of NF-κB, and the expression of its related anti-apoptotic gene like Bcl-2 and Bcl-xL [10]. Additionally, the anticancer effects of fluorouracil and cisplatin were potentiated by genistein, an isoflavone present in soy products, which could decrease chemoresistance of MGC-803 cells through reducing the expression of adenosine triphosphate (ATP) binding cassette subfamily G member 2 (ABCG2) and the activity ERK1/2 [108]. Moreover, the combination of paclitaxel and 3,3’-diindolylmethane, a compound of cruciferous vegetables, enhanced the therapeutic efficacy via the inhibition of SNU638 cell proliferation and the induction of apoptosis, which was associated with the downregulation of the Akt/Forkhead box M1 (FOXM1) signaling [109]. Furthermore, combined treatment of diallyl trisulfide and docetaxel showed a synergistic effect against gastric cancer through inducing G2/M cell cycle arrest and apoptosis with increased level of metallothionein 2A (MT2A) and inhibition of NF-κB signaling in BGC823 cells [110]. In another study, diallyl trisulfide enhanced the potency of cisplatin against gastric cancer through the activation of p38 and JNK MAPK signaling pathway, and downregulation of the nuclear factor erythroid 2-related factor 2 (Nrf2)/Akt pathway in vitro and in vivo [111]. Additionally, 6-gingerol increased the cisplatin sensitivity of HGC-27 cells via the suppression of cell proliferation, migration, and invasion by inactivating PI3K/Akt signaling pathway [112].
Collectively, several phytochemicals exhibit anticancer effects against gastric cancer, such as curcumin, diallyl trisulfide, 3,3’-diindolylmethane and 6-shogaol (Table 2). The mechanisms of action are mainly inhibiting cell proliferation, inducing apoptosis and autophagy, suppressing angiogenesis and metastasis, reducing the Helicobacter pylori infection, and modulating the gut microbiota (Figure 2). Additionally, the combined treatment of phytochemicals and anticancer drugs exhibits synergistic effects against gastric cancer.
Table 2.
The effects of phytochemicals against gastric cancer from experimental studies.
| Natural Products | Phytochemicals | Study Type | Models | Mechanisms | Molecular Targets | Ref. |
|---|---|---|---|---|---|---|
| Fruits | ||||||
| Citrus reticulata Blanco extract | NA | In vitro | SNU-668 cells | Induced apoptosis | ↓ Bcl-2 ↑ Bax and caspase-3 |
[71] |
| Cirsium chanroenicum | Pectolinarigenin | In vitro | AGS and MKN-28 cells | Induced autophagy and apoptosis Inhibited cell growth and proliferation |
↓ p-4EBP1, p-p70S6K, and p-eIF4E, ↑ LC3-II conversion |
[82] |
| Citrus fruits | Poncirin | In vitro | AGS cells | Induced apoptosis Inhibited cell proliferation | ↑ FasL, caspase-8, caspase-3 and PARP cleavage | [70] |
| Black currant | Phenolic compounds | In vitro | SGC-7901 cells | NA | [113] | |
| Blueberries | Pterostilbene | In vitro | AGS cells | ↓ p-Rb, cyclin A, cyclin E, Cdk2, Cdk4, and Cdk6, ↑ caspase-2, -3, -8, and -9, PARP cleavage, p53, p2l, p27, and p16 proteins |
[114] | |
| Citrus fruits | Tangeretin | In vitro | SGC7901 cells | Inhibited radiation-mediated EMT, migration and invasion | ↓ Notch-1, Jagged1/2, Hey-1 and Hes-1, ↑ miR-410 |
[93] |
| Mangosteen | α-Mangostin | In vitro | BGC-823 and SGC-7901 cells | Induced apoptosis Inhibited the cell viability | ↓ STAT3, Bcl-xL and Mcl-1, ↑ cytochrome c |
[72] |
| Mangosteen | Gartanin and TRAIL | In vitro | AGS cells | Enhanced the sensitization of AGS cells to TRAIL | ↑ death receptor 5 | [107] |
| Strawberry | NA | In vitro | SNU-638 cells | Inhibited cell growth | NA | [115] |
| Citrus reticulate cv. Suavissima | Poncirin | In vitro | SGC-7901 cells | [54] | ||
| Vegetables | ||||||
| Cruciferous vegetables | 3,3’-Diindolylmethane | In vitro | BGC-823 and SGC-7901 cells | Inhibited cell proliferation Induced autophagy |
↓ MicroRNA-30e, ↑ ATG5 and LC3 |
[83] |
| In vivo | Female nude mice | Inhibited the growth of gastric tumor | ↑ LC3 | |||
| Cruciferous vegetables | Paclitaxel and 3,3’-diindolylmethane | In vitro | SNU638 cell | Induced apoptosis Inhibited proliferation | ↑ PARP, caspase-9, ↓ CDK4, p53, cyclin D1 and p-Akt |
[109] |
| Spices | ||||||
| Fruit of long pepper | Piperlongumine | In vitro | SGC-7901, BGC-823 and KATO III cells | Induced apoptosis | ↓ TrxR1, ↑ ROS |
[21] |
| In vivo | Female BALB/cA athymic mice | Reduced tumor cell burden | ↓ TrxR1 | |||
| Allitridi | NA | In vitro | BGC823 cells | Induced apoptosis Inhibited cell proliferation | ↓ Bcl-2, ↑ caspase-3 |
[52] |
| Allium ursinum L | NA | In vitro | AGS cells | ↓ cyclin B | [56] | |
| Garlic | Diallyl trisulfide | In vitro | AGS cells | ↑ ROS, phosphorylation of AMPK and histone H3 | [60] | |
| Ginger | 6-Shogaol | In vitro | HGC, AGS and KATO III cells | Inhibited cell viability Induced mitotic arrest Damaged microtubules |
NA | [64] |
| In vivo | Athymic nude mice | Suppressed tumor growth | NA | |||
| Ginger | Zerumbone | In vitro | AGS cells | Anti-angiogenesis | ↓ VEGF and NF-κB | [89] |
| Ginger | 6-Gingerol and cisplatin | In vitro | HGC-27 cells | Inhibited cell proliferation, migration and invasion | ↑ P21 and P27, ↓ cyclin D1, cyclin A2, MMP-9, p-PI3K, Akt, and p-Akt |
[112] |
| Curcuma zedoaria rhizomes | Curcuzedoalide | In vitro | AGS cells | Induced apoptosis Inhibited cell viability | ↑ cleavage of caspase-8, caspase-9, caspase-3 and PARP | [116] |
| Curcuma mangga rhizomes | Labdane diterpenes | In vitro | AGS cells | Inhibited cell proliferation | NA | [53] |
| Turmeric | Curcumin, etoposide and doxorubicin | In vitro | SGC-7901 cells | Enhanced the anticancer efficacy of etoposide and doxorubicin | ↓ NF-κB, Bcl-2 and Bcl-xL | [10] |
| Garlic | Diallyl trisulfide and docetaxel | In vitro | BGC823 cells | Induced apoptosis Induced G2/M cell cycle arrest |
↑ MT2A, IκB-α, cyclin B1, activated caspase-3, and Bax, ↓ p-IκB-α, p-P65, cyclin D1, and XIAP |
[110] |
| In vivo | Female BALB/c athymic mice | Inhibited tumor growth | ↑ MT2A, IjB-a, CCNB1, and a-CASP3, ↓ CCND1 |
|||
| Garlic | Diallyl disulfide | In vitro | MGC803 cells | Inhibited cell growth Induced cell differentiation |
↓ CDC25C, cyclin B1, p-ERK1/2, ↑ p-Chkl |
[57,59] |
| Garlic | Diallyl disulfide | In vitro | AGS cells | Inhibited tumor cell motility and invasion | ↓ MMP-2, MMP-9, claudin proteins (claudin-2, -3, and -4), ↑ TIMP-1, TIMP-2 |
[94] |
| Garlic derivatives | S-allylmercaptocysteine | In vivo | Female BALB/c nude mice | Inhibited the growth of gastric tumor | NA | [63] |
| Zanthoxylum nitidum (Roxb) DC | Nitidine chloride | In vitro | SGC-7901 and AGS cells | Induced apoptosis Inhibited cell viability and angiogenesis | ↓ p-STAT3, cyclin D1, Bcl-2, Bcl-xL, and VEGF | [23] |
| In vivo | Male BALB/cA nude mice | Reduced the volume of tumors | ↓ STAT3 and VEGF | |||
| Mushroom | ||||||
| Liang Jin mushroom | 3’-azido-3’-deoxythymidine (AZT) and RNA-protein complex (FA-2-b-β) | In vitro | MKN-45 cells | Induced apoptosis Inhibited cell proliferation | ↓ tumor cell telomerase and Bcl-2, ↑caspase-3 |
[117] |
| Agaricus blazei Murrill | Blazein | In vitro | KATO III cells | Induced apoptosis Suppressed cell growth | NA | [118] |
| Phellinus linteus | Polyphenol compound hispolon | In vitro | SGC-7901, MGC-803, and MKN-45 cells | Induced apoptosis | ↓ Bcl-2, ↑ ROS, cytochrome c, caspase-3 and caspase-9 |
[74] |
| Hericium erinaceus mycelium | Erinacine A | In vitro | TSGH9201 and MKN-28 human gastric cancer cells | Induced apoptosis Inhibited the viability and invasiveness |
↓ Bcl-2 and Bcl-XL, ↑ ROS, MTUS2, TRAIL, caspase 8, caspase 9, caspase 3, cytochrome c and phosphorylation of FAK/Akt/p70S6K and PAK1 |
[91] |
| Lentinula edodes C91-3 | Latcripin 1 protein | In vitro | SGC-7901 and BGC-823 cells | Induced autophagy and apoptosis Inhibit cell growth and proliferation |
↓ Bcl-2, MMP-2 and MMP-9, ↑ Bax, caspase-3, ATG7, ATG5, ATG12, ATG14 and Beclin1 |
[61] |
| Ganoderma lucidum | NA | In vitro | AGS cells | ↑ LC3-II | [119] | |
| Recombinant Lz-8 protein | In vitro | SGC-7901 cells | Induced autophagic cell death Inhibited cell growth |
↑ CHOP, ATF4 and GRP78 | [120] | |
| Fomes Fomentarius | Polysaccharide | In vitro | SGC-7901 and MKN-45 cells | Inhibited cell proliferation | NA | [20] |
| Maitake (Grifola frondosa) | NA | In vitro | TMK-1, MKN-28, MKN-45 and MKN-74 cells | NA | [121] | |
| Soy | ||||||
| Black soybean | NA | In vitro | AGS cells | Induced apoptosis Inhibited cell proliferation | ↓ Bcl-2, ↑ Bax, caspase-3, PARP cleavage |
[75] |
| Soy products | Genistein, fluorouracil and ciplatin | In vitro | MGC-803 cells | Decreased chemoresistance | ↓ ABCG2, ERK1/2 | [108] |
| Traditional medicine | ||||||
| Gardenia jasminoides Ellis | Carotenoids | In vitro | MKN-28 cells | Inhibited cell proliferation | NA | [122] |
| Perilla frutescens | Perillaldehyde | In vitro | MFCs and GC9811-P cells | Induced autophagy | ↑ p-AMPK | [84] |
| In vivo | Female BAL B/c nude mice | Inhibited the growth of gastric tumor Induced autophagy |
↑ beclin-1, LC3-II, cathepsin, caspase-3 and p53 | |||
| Vitex agnus-castus fruit | NA | In vitro | KATO-III Cells | Induced apoptosis | ↓ Bcl-2, Bcl-XL, Bid, Mn-superoxide dismutase and catalase, GSH, ↑ Bad, cytochrome c, caspase-3 caspases-8, caspases-9, hemeoxygenase-1 and thioredoxin reductase |
[73] |
| Bamboo shavings | Polysaccharides | In vivo | Syngeneic murine gastric cancer model | Inhibited tumor growth Prolonged the survival | ↑ cleaved caspase 3, Bax and Bik | [79] |
| Other | ||||||
| Protocatechuic acid | In vitro | AGS cells | Induced apoptosis Inhibited cell proliferation | ↓ cyclin B, ↑ JNK and p38 MAPK |
[69] | |
| Kaempferol | In vitro | AGS, NCI-N87, SNU-638 and MKN-74 cells | Induced autophagic cell death Decreased cell viability |
↓ p62, ↑ LC3B, Beclin-1, ATG5, p-IRE1 and p-JNK |
[22] | |
| Myricetin | In vitro | HGC-27 and SGC7901 cells | Inhibited cell proliferation | ↑ Mad1 | [62] | |
| Apigenin | In vitro | SGC-7901 cells | Inhibited cell growth | NA | [55] | |
| Luteolin | In vitro | Hs-746T and MKN-28 cells | Induced cell apoptosis Inhibited cell proliferation, invasion, and migration | ↓ Notch1 | [92] | |
| In vivo | Male BALB/c nude mice | Reduced gastric tumor volume and tumor weight | ↓ β-catenin, Notch1 and Ki-67 | |||
| Gallic acid | In vitro | AGS cells | Inhibited cell metastasis | ↓ MMP-2, MMP-9, NF-κB, Ras, Cdc42, Rac1, RhoA, RhoB and PI3K | [90] | |
| Luteolin | In vitro | MGC-803 and Hs-746T cells | Anti-angiogenesis Inhibited the formation of vasculogenic mimicry tube |
↓ VEGF and Notch1 | [88] | |
| Quercetin and SN-38 (a metabolite of irinotecan) | In vivo | Female BALB/c nude mice | Reduced the volume of tumors Anti-angiogenesis and anti-metastasis | ↓ cyclooxygenase-2, Twist1, ITGβ6, VEGF-R2 and VEGF-A | [24] | |
| In vitro | AGS cells | Induced apoptosis | ↓ β-catenin |
NA: not available.
4. Clinical Trials
The efficacy of natural products against gastric cancer was also supported in clinical studies. A study reported that daily treatment of 900 mg of Rhus verniciflua Stokes extract decreased the polypoid mass and the flat elevated lesion in an old female patient with gastric adenocarcinoma [123]. Additionally, a randomized intervention trial including 3365 residents revealed that garlic (extract and oil) supplementation could also reduce the mortality of gastric cancer [124]. In a multi-institutional randomized prospective study, combined with clinical medicine tegafur and cisplatin, lentinan could prolong median survival and improve the quality of life in patients with gastric cancer [125]. In addition, a clinical study including 349 subjects with stage II/III gastric cancer revealed that adjuvant treatment of protein-bound polysaccharide K from the mushroom Coriolus versicolor could prolong the survival of major histocompatibility complex (MHC) class I-negative patients [126]. Generally, several natural products exhibited significant synergistic effects with anticancer drugs against gastric cancer. In the future, the anti-gastric cancer effects of more phytochemicals should be confirmed by clinical trials.
5. Bioavailability
Several phytochemicals displayed low bioavailability, such as 3,3’-diindolylmethane and curcumin [127,128,129,130]. Some technologies have been applied to increase the bioavailability of phytochemicals, which should improve the anti-gastric cancer action [131,132]. A study showed that 3,3’-diindolylmethane was microencapsulated in starch with d-α-tocopheryl acid succinate, phosphatidylcholine, and silica, which could enhance its bioavailability [127]. In addition, the pterostilbene was encapsulated in nanoemulsions containing carrier oil, which could increase its bioavailability [133]. Moreover, curcumin and genistein showed good solubility and stability after encapsulating within nanostructured lipid carriers [131]. Furthermore, the micellarization could enhance the bioaccessibility of isoflavonoid aglycones [134]. Generally, the bioavailability of phytochemicals can be increased by several methods, such as encapsulation in the nanostructured lipid carriers and micellarization.
6. Safety
Different from anticancer drugs, phytochemicals commonly have less toxicity, making them safer in the prevention and management of gastric cancer [83,135]. It has been reported that lentinan had low or zero toxicity, even at high doses [135]. In addition, the treatment of hispolon, which was isolated from a traditional medicinal mushroom, showed no adverse effects on human normal gastric cells [74]. In another in vivo study, no observable toxicity was found in rats with long-term exposure to 3,3’-diindolylmethane [136]. Furthermore, the extract of Hericium erinaceus exhibited anticancer activity against the xenograft model of NCI-87 gastric cancer cells without toxicity to the host [137]. However, some spices were found to have adverse effects. A study reported that piperine had reproductive toxicity in mice [133]. Additionally, turmeric and curcumin exhibited hepatotoxicity in mice [138].
Collectively, most experimental studies have suggested a lack or low level of toxicity of most phytochemicals. However, the toxicity and other adverse effects of some phytochemicals, such as allergic reactions, liver or kidney toxicity, have not been tested in humans. Therefore, it is necessary to determine the effective and safe doses of phytochemicals to prevent toxicity in human.
7. Conclusions
The effects of phytochemicals against gastric cancer have been extensively investigated. Numerous epidemiological studies have suggested that the consumption of natural dietary products such as fruits, vegetables, spices, isoflavone and quercetin is inversely related to the risk of gastric cancer. However, inconsistent results have also been reported in some cohort studies. Moreover, both in vitro and in vivo studies have revealed that some phytochemicals showed anti-gastric cancer activity by inhibiting cell proliferation, inducing apoptosis and autophagy, suppressing angiogenesis and metastasis, reducing Helicobacter pylori infection, and modulating the gut microbiota. In addition, phytochemicals enhanced the sensitivity to chemotherapy and had synergistic effects with anticancer drugs against gastric cancer. The clinical trials further verified the anticancer efficacy of several phytochemicals. However, the protective effects of natural products against gastric cancer by regulating gut microbiota have not yet been fully explored and understood. The effects of more natural products against gastric cancer should be evaluated, the phytochemicals should be isolated and identified, and the mechanisms of action should be elucidated. Furthermore, attention should be paid to the safety and bioavailability of phytochemicals. Overall, consumption of phytochemicals is a promising strategy for the prevention and management of gastric cancer, and the public is recommended to consume natural dietary products rich in diverse phytochemicals for the prevention of gastric cancer. These natural products could also be developed into functional foods and pharmaceuticals to prevent and treat gastric cancer.
Abbreviations
| AMPK | AMP-activated protein kinase |
| ATF4 | activating transcription factor 4 |
| ATG5 | autophagy related 5; ABCG2 |
| ABCG2 | ATP binding cassette subfamily G member 2 |
| Bad | Bcl-2 associated agonist of cell death |
| Bax | Bcl-2-associated X protein |
| Bcl-2 | B-cell lymphoma 2 |
| Bcl-xL | B-cell lymphoma-extralarge |
| Bid | BH3 interacting domain death agonist |
| Bik | Bcl-2 interacting killer |
| Cdc42 | cell division cycle 42 |
| CDC25C | cell division cycle 25C |
| CDK4 | cyclin dependent kinase 4 |
| CHOP | -CCAAT-enhancer-binding protein homologous protein |
| EMT | epithelial-mesenchymal transition |
| ERK1/2 | extracellular signal-regulated kinase |
| FasL | Fas Ligand |
| GRP78 | glucose regulated protein 78 |
| GSH | glutathione |
| Hes-1 | hes family bHLH transcription factor 1 |
| Hey-1 | hes related family bHLH transcription factor with YRPW motif 1 |
| IκB-α | inhibitor of NF-κB |
| ITGβ6 | integrin subunit beta 6 |
| Jagged1/2 | 2 serrate-like ligands |
| JNK | c-Jun N-terminal kinase |
| ki-67 | a cell proliferation marker |
| LC3B | microtubule associated protein 1 light chain 3 beta |
| Mad1 | Mitotic arrest-deficient 1 |
| MAPK | mitogen-activating protein kinase |
| Mcl-1 | apoptosis regulator blongs to Bcl-2 family member |
| miR-410 | a tumor-suppressive microRNA |
| MMP-2 | matrix metallopeptidase 2 |
| MT2A | metallothionein 2A |
| MTUS2 | microtubule-associated tumor suppressor candidate 2 |
| NF-κB | nuclear factor kappa light chain-enhancer of activated B cells |
| Notch1 | notch receptor 1 |
| PARP | poly (ADP-ribose) polymerase |
| p-ERK1/2 | phosphorylation of extracellular signal-regulated kinase |
| p-Chkl | phosphorylation of checkpoint kinase-1 |
| p-IRE1 | phosphorylates inositol-requiring-1 |
| p-JNK | phosphorylates c-Jun N-terminal protein kinase |
| p-4EBP1 | phosphorylated 4E binding protein 1 |
| p-p70S6K | phosphorylated ribosomal protein S6 kinase |
| p-eIF4E | phosphorylated eukaryotic translation initiation factor 4E |
| PI3K | phoshatidylinositol-3-kinase |
| p-IκB-α | phosphorylation of p-IκB-α |
| Rac1 | Rac family small GTPase 1 |
| RhoA | ras homolog family member A |
| RhoB | ras homolog family member B |
| ROS | reactive oxygen species |
| STAT3 | signal transducer and activator of transcription 3 |
| TIMP | tissue inhibitor of metalloproteinase |
| TrxR1 | thioredoxin reductase 1 |
| TRAIL | tumour necrosis factor (TNF)-related apoptosis-inducing ligand |
| Twist1 | twist family bHLH transcription factor 1 |
| VEGF | vascular endothelial growth factor |
| VEGF-R2 | vascular endothelial growth factor receptor 2 |
| XIAP | X-linked inhibitor of apoptosis protein |
Author Contributions
Conceptualization, Q.-Q.M., R.-Y.G., and H.-B.L.; writing—original draft preparation, Q.-Q.M., X.-Y.X., and A.S.; writing—review and editing, R.-Y.G., D.-T.W., A.G.A., and H.-B.L.; supervision, R.-Y.G. and H.-B.L.; funding acquisition, R.-Y.G. and H.-B.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Key R&D Program of China (2018YFC1604405), Central Public-interest Scientific Institution Basal Research Fund (Y2020XK05), the Shanghai Pujiang Talent Plan (18PJ1404600), the Agri-X Interdisciplinary Fund of Shanghai Jiao Tong University (Agri-X2017004), and the Key Project of the Guangdong Provincial Science and Technology Program (2014B020205002).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Bertuccio P., Alicandro G., Rota M., Pelucchi C., Bonzi R., Galeone C., Bravi F., Johnson K.C., Hu J., Palli D., et al. Citrus fruit intake and gastric cancer: The stomach cancer pooling (StoP) project consortium. Int. J. Cancer. 2019;144:2936–2944. doi: 10.1002/ijc.32046. [DOI] [PubMed] [Google Scholar]
- 3.Yan S., Li B., Bai Z.Z., Wu J.Q., Xie D.W., Ma Y.C., Ma X.X., Zhao J.H., Guo X.J. Clinical epidemiology of gastric cancer in Hehuang valley of China: A 10-year epidemiological study of gastric cancer. World J. Gastroenterol. 2014;20:10486–10494. doi: 10.3748/wjg.v20.i30.10486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang G.S., Hu N., Yang H.H., Wang L.M., Su H., Wang C.Y., Clifford R., Dawsey E.M., Li J.M., Ding T., et al. Comparison of global gene expression of gastric cardia and noncardia cancers from a high-risk population in China. PLoS ONE. 2013;8:e63826. doi: 10.1371/journal.pone.0063826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donida B.M., Tomasello G., Ghidini M., Buffoli F., Grassi M., Liguigli W., Maglietta G., Pergola L., Ratti M., Sabadini G., et al. Epidemiological, clinical and pathological characteristics of gastric neoplasms in the province of Cremona: The experience of the first population-based specialized gastric cancer registry in Italy. BMC Cancer. 2019;19:212. doi: 10.1186/s12885-019-5366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goh K.L., Cheah P.L., Noorfaridah M., Quek K.F., Parasakthi N. Ethnicity and H. pylori as risk factors for gastric cancer in Malaysia: A prospective case control study. Am. J. Gastroenterol. 2007;102:40–45. doi: 10.1111/j.1572-0241.2006.00885.x. [DOI] [PubMed] [Google Scholar]
- 7.Izuishi K., Mori H. Recent strategies for treating stage IV gastric cancer: Roles of palliative gastrectomy, chemotherapy, and radiotherapy. J. Gastrointest. Liver. 2016;25:87–94. doi: 10.15403/jgld.2014.1121.251.rv2. [DOI] [PubMed] [Google Scholar]
- 8.Ren F., Li S.D., Zhang Y., Zhao Z.F., Wang H.M., Cui Y.X., Wang M.Y. Efficacy and safety of intensity-modulated radiation therapy versus three-dimensional conformal radiation treatment for patients with gastric cancer: A systematic review and meta-analysis. Radiat. Oncol. 2019;14:84. doi: 10.1186/s13014-019-1294-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Macdonald J.S., Smalley S.R., Benedetti J., Hundahl S.A., Estes N.C., Stemmermann G.N., Haller D.G., Ajani J.A., Gunderson L.L., Jessup J.M., et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N. Engl. J. Med. 2001;345:725–730. doi: 10.1056/NEJMoa010187. [DOI] [PubMed] [Google Scholar]
- 10.Yu L.L., Wu J.G., Dai N., Yu H.G., Si J.M. Curcumin reverses chemoresistance of human gastric cancer cells by downregulating the NF-κB transcription factor. Oncol. Rep. 2011;26:1197–1203. doi: 10.3892/or.2011.1410. [DOI] [PubMed] [Google Scholar]
- 11.Bertuccio P., Rosato V., Andreano A., Ferraroni M., Decarli A., Edefonti V., La Vecchia C. Dietary patterns and gastric cancer risk: A systematic review and meta-analysis. Ann. Oncol. 2013;24:1450–1458. doi: 10.1093/annonc/mdt108. [DOI] [PubMed] [Google Scholar]
- 12.Li Y., Li S., Meng X., Gan R.Y., Zhang J.J., Li H.B. Dietary natural products for prevention and treatment of breast cancer. Nutrients. 2017;9:728. doi: 10.3390/nu9070728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nouraie M., Pietinen P., Kamangar F., Dawsey S.M., Abnet C.C., Albanes D., Virtamo J., Taylor P.R. Fruits, vegetables, and antioxidants and risk of gastric cancer among male smokers. Cancer Epidemiol. Biomark. 2005;14:2087–2092. doi: 10.1158/1055-9965.EPI-05-0038. [DOI] [PubMed] [Google Scholar]
- 14.Zhou Y., Li Y., Zhou T., Zheng J., Li S., Li H.B. Dietary natural products for prevention and treatment of liver cancer. Nutrients. 2016;8:156. doi: 10.3390/nu8030156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zheng J., Zhou Y., Li Y., Xu D.P., Li S., Li H.B. Spices for prevention and treatment of cancers. Nutrients. 2016;8:495. doi: 10.3390/nu8080495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fang X.X., Wei J.Y., He X.Y., An P., Wang H., Jiang L., Shao D.D., Liang H., Li Y., Wang F.D., et al. Landscape of dietary factors associated with risk of gastric cancer: A systematic review and dose-response meta-analysis of prospective cohort studies. Eur. J. Cancer. 2015;51:2820–2832. doi: 10.1016/j.ejca.2015.09.010. [DOI] [PubMed] [Google Scholar]
- 17.Palli D., Russo A., Saieva C., Salvini S., Amorosi A., Decarli A. Dietary and familial determinants of 10-year survival among patients with gastric carcinoma. Cancer Am. Cancer Soc. 2000;89:1205–1213. doi: 10.1002/1097-0142(20000915)89:6<1205::AID-CNCR3>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 18.Wada K., Tsuji M., Tamura T., Konishi K., Kawachi T., Hori A., Tanabashi S., Matsushita S., Tokimitsu N., Nagata C. Soy isoflavone intake and stomach cancer risk in Japan: From the Takayama study. Int. J. Cancer. 2015;137:885–892. doi: 10.1002/ijc.29437. [DOI] [PubMed] [Google Scholar]
- 19.Ekstrom A.M., Serafini M., Nyren O., Wolk A., Bosetti C., Bellocco R. Dietary quercetin intake and risk of gastric cancer: Results from a population-based study in Sweden. Ann. Oncol. 2011;22:438–443. doi: 10.1093/annonc/mdq390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen W., Zhao Z., Li Y.Q. Simultaneous increase of mycelial biomass and intracellular polysaccharide from Fomes fomentarius and its biological function of gastric cancer intervention. Carbohyd. Polym. 2011;85:369–375. doi: 10.1016/j.carbpol.2011.02.035. [DOI] [Google Scholar]
- 21.Zou P., Xia Y.Q., Ji J.S., Chen W.Q., Zhang J.S., Chen X., Rajamanickam V., Chen G.Z., Wang Z., Chen L.F., et al. Piperlongumine as a direct TrxR1 inhibitor with suppressive activity against gastric cancer. Cancer Lett. 2016;375:114–126. doi: 10.1016/j.canlet.2016.02.058. [DOI] [PubMed] [Google Scholar]
- 22.Kim T.W., Lee S.Y., Kim M., Cheon C., Ko S.G. Kaempferol induces autophagic cell death via IRE1-JNK-CHOP pathway and inhibition of G9a in gastric cancer cells. Cell Death Dis. 2018;9:875. doi: 10.1038/s41419-018-0930-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen J., Wang J.Q., Lin L., He L.J., Wu Y.Y., Zhang L., Yi Z.F., Chen Y.H., Pang X.F., Liu M.Y. Inhibition of STAT3 signaling pathway by nitidine chloride suppressed the angiogenesis and growth of human gastric cancer. Mol. Cancer Ther. 2012;11:277–287. doi: 10.1158/1535-7163.MCT-11-0648. [DOI] [PubMed] [Google Scholar]
- 24.Lei C.S., Hou Y.C., Pai M.H., Lin M.T., Yeh S.L. Effects of quercetin combined with anticancer drugs on metastasis-associated factors of gastric cancer cells: In vitro and in vivo studies. J. Nutr. Biochem. 2018;51:105–113. doi: 10.1016/j.jnutbio.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 25.Nowak R., Nowacka-Jechalke N., Juda M., Malm A. The preliminary study of prebiotic potential of Polish wild mushroom polysaccharides: The stimulation effect on Lactobacillus strains growth. Eur. J. Nutr. 2018;57:1511–1521. doi: 10.1007/s00394-017-1436-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mahady G.B., Pendland S.L., Yun G., Lu Z. Turmeric (Curcuma longa) and curcumin inhibit the growth of Helicobacter pylori, a group 1 carcinogen. Anticancer Res. 2002;22:4179–4181. [PubMed] [Google Scholar]
- 27.Bastos J., Lunet N., Peleteiro B., Lopes C., Barros H. Dietary patterns and gastric cancer in a Portuguese urban population. Int. J. Cancer. 2010;127:433–441. doi: 10.1002/ijc.25013. [DOI] [PubMed] [Google Scholar]
- 28.Nagata C., Takatsuka N., Kawakami N., Shimizu H. A prospective cohort study of soy product intake and stomach cancer death. Br. J. Cancer. 2002;87:31–36. doi: 10.1038/sj.bjc.6600349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Palli D., Russo A., Ottini L., Masala G., Saieva C., Amorosi A., Cama A., D’Amico C., Falchetti M., Palmirotta R., et al. Red meat, family history, and increased risk of gastric cancer with microsatellite instability. Cancer Res. 2001;61:5415–5419. [PubMed] [Google Scholar]
- 30.Pourfarzi F., Whelan A., Kaldor J., Malekzadeh R. The role of diet and other environmental factors in the causation of gastric cancer in Iran-A population-based study. Int. J. Cancer. 2009;125:1953–1960. doi: 10.1002/ijc.24499. [DOI] [PubMed] [Google Scholar]
- 31.Bae J.M., Lee E.J., Guyatt G. Citrus fruit intake and stomach cancer risk: A quantitative systematic review. Gastric Cancer. 2008;11:23–32. doi: 10.1007/s10120-007-0447-2. [DOI] [PubMed] [Google Scholar]
- 32.Kim H.J., Chang W.K., Kim M.K., Lee S.S., Choi B.Y. Dietary factors and gastric cancer in Korea: A case-control study. Int. J. Cancer. 2002;97:531–535. doi: 10.1002/ijc.10111. [DOI] [PubMed] [Google Scholar]
- 33.Kobayashi M., Tsubono Y., Sasazuki S., Sasaki S., Tsugane S., GRP J.S. Vegetables, fruit and risk of gastric cancer in japan: A 10-year follow-up of the JPHC Study Cohort I. Int. J. Cancer. 2002;102:39–44. doi: 10.1002/ijc.10659. [DOI] [PubMed] [Google Scholar]
- 34.Steevens J., Schouten L.J., Goldbohm R.A., van den Brandt P.A. Vegetables and fruits consumption and risk of esophageal and gastric cancer subtypes in the Netherlands cohort study. Int. J. Cancer. 2011;129:2681–2693. doi: 10.1002/ijc.25928. [DOI] [PubMed] [Google Scholar]
- 35.McCullough M.L., Robertson A.S., Jacobs E.J., Chao A., Calle E.E., Thun M.J. A prospective study of diet and stomach cancer mortality in United States men and women. Cancer Epidemiol. Biomark. 2001;10:1201–1205. [PubMed] [Google Scholar]
- 36.Zhou Y., Zhuang W., Hu W., Liu G.J., Wu T.X., Wu X.T. Consumption of large amounts of allium vegetables reduces risk for gastric cancer in a meta-analysis. Gastroenterology. 2011;141:80–89. doi: 10.1053/j.gastro.2011.03.057. [DOI] [PubMed] [Google Scholar]
- 37.Ko K.P., Park S.K., Park B., Yang J.J., Cho L.Y., Kang C., Kim C.S., Gwack J., Shin A., Kim Y., et al. Isoflavones from Phytoestrogens and gastric cancer risk: A nested case-control study within the Korean multicenter cancer cohort. Cancer Epidemiol. Biomark. 2010;19:1292–1300. doi: 10.1158/1055-9965.EPI-09-1004. [DOI] [PubMed] [Google Scholar]
- 38.Kweon S.S., Shu X.O., Xiang Y.B., Cai H., Yang G., Ji B.T., Li H.L., Gao Y.T., Zheng W., Epplein M. Intake of specific nonfermented soy foods may be inversely associated with risk of distal gastric cancer in a Chinese population. J. Nutr. 2013;143:1736–1742. doi: 10.3945/jn.113.177675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Persson C., Sasazuki S., Inoue M., Kurahashi N., Iwasaki M., Miura T., Ye W., Tsugane S., Grp J.S. Plasma levels of carotenoids, retinol and tocopherol and the risk of gastric cancer in Japan: A nested case-control study. Carcinogenesis. 2008;29:1042–1048. doi: 10.1093/carcin/bgn072. [DOI] [PubMed] [Google Scholar]
- 40.Woo H.D., Lee J., Choi I.J., Kim C.G., Lee J.Y., Kwon O., Kim J. Dietary Flavonoids and gastric cancer risk in a Korean population. Nutrients. 2014;6:4961–4973. doi: 10.3390/nu6114961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim J.H., Lee J., Choi I.J., Kim Y.I., Kwon O., Kim H., Kim J. Dietary carotenoids intake and the risk of gastric cancer: A case control study in Korea. Nutrients. 2018;10:1031. doi: 10.3390/nu10081031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Petrick J.L., Steck S.E., Bradshaw P.T., Trivers K.F., Abrahamson P.E., Engel L.S., He K., Chow W.H., Mayne S.T., Risch H.A., et al. Dietary intake of flavonoids and oesophageal and gastric cancer: Incidence and survival in the United States of America (USA) Br. J. Cancer. 2015;112:1291–1300. doi: 10.1038/bjc.2015.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moy K.A., Yuan J.M., Chung F.L., Wang X.L., Van Den Berg D., Wang R.W., Gao Y.T., Yu M.C. Isothiocyanates, glutathione S-transferase M1 and T1 polymorphisms and gastric cancer risk: A prospective study of men in Shanghai, China. Int. J. Cancer. 2009;125:2652–2659. doi: 10.1002/ijc.24583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shimazu T., Wakai K., Tamakoshi A., Tsuji I., Tanaka K., Matsuo K., Nagata C., Mizoue T., Inoue M., Tsugane S., et al. Association of vegetable and fruit intake with gastric cancer risk among Japanese: A pooled analysis of four cohort studies. Ann. Oncol. 2014;25:1228–1233. doi: 10.1093/annonc/mdu115. [DOI] [PubMed] [Google Scholar]
- 45.Gonzalez C.A., Lujan-Barroso L., Bueno-de-Mesquita H.B., Jenab M., Duell E.J., Agudo A., Tjonneland A., Boutron-Ruault M.C., Clavel-Chapelon F., Touillaud M., et al. Fruit and vegetable intake and the risk of gastric adenocarcinoma: A reanalysis of the European prospective investigation into cancer and nutrition (EPIC-EURGAST) study after a longer follow-up. Int. J. Cancer. 2012;131:2910–2919. doi: 10.1002/ijc.27565. [DOI] [PubMed] [Google Scholar]
- 46.Larsson S.C., Bergkvist L., Wolk A. Fruit and vegetable consumption and incidence of gastric cancer: A prospective study. Cancer Epidemiol. Biomark. 2006;15:1998–2001. doi: 10.1158/1055-9965.EPI-06-0402. [DOI] [PubMed] [Google Scholar]
- 47.Epplein M., Shu X.O., Xiang Y.B., Chow W.H., Yang G., Li H.L., Ji B.T., Cai H., Gao Y.T., Zheng W. Fruit and vegetable consumption and risk of distal gastric cancer in the Shanghai women’s and men’s health studies. Am. J. Epidemiol. 2010;172:397–406. doi: 10.1093/aje/kwq144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kim H., Keum N., Giovannucci E.L., Fuchs C.S., Bao Y. Garlic intake and gastric cancer risk: Results from two large prospective US cohort studies. Int. J. Cancer. 2018;143:1047–1053. doi: 10.1002/ijc.31396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hara A., Sasazuki S., Inoue M., Iwasaki M., Shimazu T., Sawada N., Yamaji T., Tsugane S., Ctr-Based J.P.H. Isoflavone intake and risk of gastric cancer: A population-based prospective cohort study in Japan. Am. J. Clin. Nutr. 2012;95:147–154. doi: 10.3945/ajcn.111.020479. [DOI] [PubMed] [Google Scholar]
- 50.Sun L., Subar A.F., Bosire C., Dawsey S.M., Kahle L.L., Zimmerman T.P., Abnet C.C., Heller R., Graubard B.I., Cook M.B., et al. Dietary flavonoid intake reduces the risk of head and neck but not esophageal or gastric cancer in US men and women. J. Nutr. 2017;147:1729–1738. doi: 10.3945/jn.117.251579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Botterweck A.A.M., van den Brandt P.A., Goldbohm R.A. Vitamins, carotenoids, dietary fiber, and the risk of gastric carcinoma—Results from a prospective study after 6.3 years of follow-up. Cancer Am. Cancer Soc. 2000;88:737–748. [PubMed] [Google Scholar]
- 52.Lan H., Lu Y.Y. Allitridi induces apoptosis by affecting Bcl-2 expression and caspase-3 activity in human gastric cancer cells. Acta Pharmacol. Sin. 2004;25:219–225. [PubMed] [Google Scholar]
- 53.Liu Y.B., Nair M.G. Labdane diterpenes in Curcuma mangga rhizomes inhibit lipid peroxidation, cyclooxygenase enzymes and human tumour cell proliferation. Food Chem. 2011;124:527–532. doi: 10.1016/j.foodchem.2010.06.064. [DOI] [Google Scholar]
- 54.Zhu X.Y., Luo F.L., Zheng Y.X., Zhang J.K., Huang J.Z., Sun C.D., Li X., Chen K.S. Characterization, purification of poncirin from edible Citrus Ougan (Citrus reticulate cv. Suavissima) and its growth inhibitory effect on human gastric cancer cells SGC-7901. Int. J. Mol. Sci. 2013;14:8684–8697. doi: 10.3390/ijms14058684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wu K., Yuan L.H., Xia W. Inhibitory effects of apigenin on the growth of gastric carcinoma SGC-7901 cells. World J. Gastroenterol. 2005;11:4461–4464. doi: 10.3748/wjg.v11.i29.4461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xu X.Y., Song G.Q., Yu Y.Q., Ma H.Y., Ma L., Jin Y.N. Apoptosis and G2/M arrest induced by Allium ursinum (ramson) watery extract in an AGS gastric cancer cell line. OncoTargets Ther. 2013;6:779–783. doi: 10.2147/OTT.S45865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ling H., Lu L.F., He J., Xiao G.H., Jiang H., Su Q. Diallyl disulfide selectively causes checkpoint kinase-1 mediated G2/M arrest in human MGC803 gastric cancer cell line. Oncol. Rep. 2014;32:2274–2282. doi: 10.3892/or.2014.3417. [DOI] [PubMed] [Google Scholar]
- 58.Yuan J.P., Wang G.H., Ling H., Su Q., Yang Y.H., Song Y., Tang R.J., Liu Y., Huang C. Diallyl disulfide-induced G2/M arrest of human gastric cancer MGC803 cells involves activation of p38 MAP kinase pathways. World J. Gastroenterol. 2004;10:2731–2734. doi: 10.3748/wjg.v10.i18.2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ling H., Zhang L.Y., Su Q., Song Y., Luo Z.Y., Zhou X.T., Zeng X., He J., Tan H., Yuan J.P. ERK is involved in the differentiation induced by diallyl disulfide in the human gastric cancer cell line MGC803. Cell. Mol. Biol. Lett. 2006;11:408–423. doi: 10.2478/s11658-006-0034-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Choi Y.H. Diallyl trisulfide induces apoptosis and mitotic arrest in AGS human gastric carcinoma cells through reactive oxygen species-mediated activation of AMP-activated protein kinase. Biomed. Pharmacother. 2017;94:63–71. doi: 10.1016/j.biopha.2017.07.055. [DOI] [PubMed] [Google Scholar]
- 61.Batool S., Joseph T.P., Hussain M., Vuai M.S., Khinsar K.H., Din S.R.U., Padhiar A.A., Zhong M., Ning A.H., Zhang W., et al. LP1 from Lentinula edodes C91-3 induces autophagy, apoptosis and reduces metastasis in human gastric cancer cell line SGC-7901. Int. J. Mol. Sci. 2018;19:2986. doi: 10.3390/ijms19102986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Feng J.F., Chen X.N., Wang Y.Y., Du Y.W., Sun Q.Q., Zang W.Q., Zhao G.Q. Myricetin inhibits proliferation and induces apoptosis and cell cycle arrest in gastric cancer cells. Mol. Cell. Biochem. 2015;408:163–170. doi: 10.1007/s11010-015-2492-1. [DOI] [PubMed] [Google Scholar]
- 63.Zhu X.S., Jiang X.Y., Li A., Sun Y.Y., Liu Y., Sun X., Feng X.L., Li S.Y., Zhao Z.X. S-allylmercaptocysteine suppresses the growth of human gastric cancer xenografts through induction of apoptosis and regulation of MAPK and PI3K/Akt signaling pathways. Biochem. Biophys. Res. Commun. 2017;491:821–826. doi: 10.1016/j.bbrc.2017.06.107. [DOI] [PubMed] [Google Scholar]
- 64.Ishiguro K., Ando T., Maeda O., Ohmiya N., Niwa Y., Kadomatsu K., Goto H. Ginger ingredients reduce viability of gastric cancer cells via distinct mechanisms. Biochem. Biophys. Res. Commun. 2007;362:218–223. doi: 10.1016/j.bbrc.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 65.Yang C.G., Du W.F., Yang D.G. Inhibition of green tea polyphenol EGCG((-)-epigallocatechin-3-gallate) on the proliferation of gastric cancer cells by suppressing canonical wnt/β-catenin signalling pathway. Int. J. Food Sci. Nutr. 2016;67:818–827. doi: 10.1080/09637486.2016.1198892. [DOI] [PubMed] [Google Scholar]
- 66.Xu X.Y., Zhao C.N., Cao S.Y., Tang G.Y., Gan R.Y., Li H.B. Effects and mechanisms of tea for the prevention and management of cancers: An updated review. Crit. Rev. Food Sci. Nutr. 2019:1–13. doi: 10.1080/10408398.2019.1588223. [DOI] [PubMed] [Google Scholar]
- 67.Shang A., Cao S.Y., Xu X.Y., Gan R.Y., Tang G.Y., Corke H., Mavumengwana V., Li H.B. Bioactive compounds and biological functions of garlic (Allium sativum L.) Foods. 2019;8:246. doi: 10.3390/foods8070246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fesik S.W. Promoting apoptosis as a strategy for cancer drug discovery. Nat. Rev. Cancer. 2005;5:876–885. doi: 10.1038/nrc1736. [DOI] [PubMed] [Google Scholar]
- 69.Lin H.H., Chen J.H., Huang C.C., Wang C.J. Apoptotic effect of 3,4-dihydroxybenzoic acid on human gastric carcinoma cells involving JNK/p38 MAPK signaling activation. Int. J. Cancer. 2007;120:2306–2316. doi: 10.1002/ijc.22571. [DOI] [PubMed] [Google Scholar]
- 70.Saralamma V.V.G., Nagappan A., Hong G.E., Lee H.J., Yumnam S., Raha S., Heo J.D., Lee S.J., Lee W.S., Kim E.H., et al. Poncirin induces apoptosis in AGS human gastric cancer cells through extrinsic apoptotic pathway by up-regulation of Fas Ligand. Int. J. Mol. Sci. 2015;16:22676–22691. doi: 10.3390/ijms160922676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kim M.J., Park H.J., Hong M.S., Park H.J., Kim M.S., Leem K.H., Kim J.B., Kim Y.J., Kim H.K. Citrus reticulata Blanco induces apoptosis in human gastric cancer cells SNU-668. Nutr. Cancer. 2005;51:78–82. doi: 10.1207/s15327914nc5101_11. [DOI] [PubMed] [Google Scholar]
- 72.Shan T., Cui X.J., Li W., Lin W.R., Lu H.W., Li Y.M., Chen X., Wu T. α-Mangostin suppresses human gastric adenocarcinoma cells In Vitro via blockade of STAT3 signaling pathway. Acta Pharmacol. Sin. 2014;35:1065–1073. doi: 10.1038/aps.2014.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ohyama K., Akaike T., Imai M., Toyoda H., Hirobe C., Bessho T. Human gastric signet ring carcinoma (KATO-III) cell apoptosis induced by Vitex agnus-castus fruit extract through intracellular oxidative stress. Int. J. Biochem. Cell Biol. 2005;37:1496–1510. doi: 10.1016/j.biocel.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 74.Chen W., Zhao Z., Li L., Wu B., Chen S.F., Zhou H., Wang Y., Li Y.Q. Hispolon induces apoptosis in human gastric cancer cells through a ROS-mediated mitochondrial pathway. Free Radic. Biol. Med. 2008;45:60–72. doi: 10.1016/j.freeradbiomed.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 75.Zou Y.P., Chang S.K.C. Effect of black soybean extract on the suppression of the proliferation of human ags gastric cancer cells via the induction of apoptosis. J. Agric. Food Chem. 2011;59:4597–4605. doi: 10.1021/jf104945x. [DOI] [PubMed] [Google Scholar]
- 76.Hibasami H., Komiya T., Achiwa Y., Ohnishi K., Kojima T., Nakanishi K., Akashi K., Hara Y. Induction of apoptosis in human stomach cancer cells by green tea catechins. Oncol. Rep. 1998;5:527–529. doi: 10.3892/or.5.2.527. [DOI] [PubMed] [Google Scholar]
- 77.Hibasami H., Komiya T., Achiwa Y., Ohnishi K., Kojima T., Nakanishi K., Sugimoto Y., Hasegawa M., Akatsuka R., Hara Y. Black tea theaflavins induce programmed cell death in cultured human stomach cancer cells. Int. J. Mol. Med. 1998;1:725–727. doi: 10.3892/ijmm.1.4.725. [DOI] [PubMed] [Google Scholar]
- 78.Hibasami H., Jin Z.X., Hasegawa M., Urakawa K., Nakagawa M., Ishii Y., Yoshioka K. Oolong tea polyphenol extract induces apoptosis in human stomach cancer cells. Anticancer Res. 2000;20:4403–4406. [PubMed] [Google Scholar]
- 79.Li G.Y., Zhang Y.R., Xie E.J., Yang X., Wang H., Wang X.J., Li W.W., Song Z.J., Mu Q.D., Zhan W.H., et al. Functional characterization of a potent anti-tumor polysaccharide in a mouse model of gastric cancer. Life Sci. 2019;219:11–19. doi: 10.1016/j.lfs.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 80.Song X., Zhang X., Wang X., Zhu F., Guo C., Wang Q., Shi Y., Wang J., Chen Y., Zhang L. Tumor suppressor gene PDCD4 negatively regulates autophagy by inhibiting the expression of autophagy-related gene ATG5. Autophagy. 2013;9:743–755. doi: 10.4161/auto.24069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gump J.M., Thorburn A. Autophagy and apoptosis: What is the connection? Trends Cell Biol. 2011;21:387–392. doi: 10.1016/j.tcb.2011.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lee H.J., Saralamma V.V.G., Kim S.M., Ha S.E., Raha S., Lee W.S., Kim E.H., Lee S.J., Heo J.D., Kim G.S. Pectolinarigenin induced cell cycle arrest, autophagy, and apoptosis in gastric cancer cell via PI3K/AKT/mTOR signaling pathway. Nutrients. 2018;10:1043. doi: 10.3390/nu10081043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ye Y., Fang Y.F., Xu W.X., Wang Q., Zhou J.W., Lu R.Z. 3,3‘-Diindolylmethane induces anti-human gastric cancer cells by the miR-30e-ATG5 modulating autophagy. Biochem. Pharmacol. 2016;115:77–84. doi: 10.1016/j.bcp.2016.06.018. [DOI] [PubMed] [Google Scholar]
- 84.Zhang Y., Liu S.S., Feng Q., Huang X.Y., Wang X.Y., Peng Y., Zhao Z.H., Liu Z. Perilaldehyde activates AMP-activated protein kinase to suppress the growth of gastric cancer via induction of autophagy. J. Cell. Biochem. 2019;120:1716–1725. doi: 10.1002/jcb.27491. [DOI] [PubMed] [Google Scholar]
- 85.Wang K., Liu R., Li J.Y., Mao J.L., Lei Y.L., Wu J.H., Zeng J., Zhang T., Wu H., Chen L.J., et al. Quercetin induces protective autophagy in gastric cancer cells Involvement of Akt-mTOR- and hypoxia-induced factor 1 α-mediated signaling. Autophagy. 2011;7:966–978. doi: 10.4161/auto.7.9.15863. [DOI] [PubMed] [Google Scholar]
- 86.Gao J.H., Wang C.H., Tong H., Wen S.L., Huang Z.Y., Tang C.W. Targeting inhibition of extracellular signal-regulated kinase pathway with AZD6244 (ARRY-142886) suppresses growth and angiogenesis of gastric cancer. Sci. Rep. 2015;5:16382. doi: 10.1038/srep16382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zhang Y., Han J., Yang X., Shao C., Xu Z., Cheng R., Cai W., Ma J., Yang Z., Gao G. Pigment epithelium-derived factor inhibits angiogenesis and growth of gastric carcinoma by down-regulation of VEGF. Oncol. Rep. 2011;26:681–686. doi: 10.3892/or.2011.1318. [DOI] [PubMed] [Google Scholar]
- 88.Zang M.D., Hu L., Zhang B.G., Zhu Z.L., Li J.F., Zhu Z.G., Yan M., Liu B.Y. Luteolin suppresses angiogenesis and vasculogenic mimicry formation through inhibiting Notchl-VEGF signaling in gastric cancer. Biochem. Biophys. Res. Commun. 2017;490:913–919. doi: 10.1016/j.bbrc.2017.06.140. [DOI] [PubMed] [Google Scholar]
- 89.Tsuboi K., Matsuo Y., Shamoto T., Shibata T., Koide S., Morimoto M., Guha S., Sung B., Aggarwal B.B., Takahashi H., et al. Zerumbone inhibits tumor angiogenesis via NF-κB in gastric cancer. Oncol. Rep. 2014;31:57–64. doi: 10.3892/or.2013.2842. [DOI] [PubMed] [Google Scholar]
- 90.Ho H.H., Chang C.S., Ho W.C., Liao S.Y., Wu C.H., Wang C.J. Anti-metastasis effects of gallic acid on gastric cancer cells involves inhibition of NF-κB activity and downregulation of PI3K/AKT/small GTPase signals. Food Chem. Toxicol. 2010;48:2508–2516. doi: 10.1016/j.fct.2010.06.024. [DOI] [PubMed] [Google Scholar]
- 91.Kuo H.C., Kuo Y.R., Lee K.F., Hsieh M.C., Huang C.Y., Hsieh Y.Y., Lee K.C., Kuo H.L., Lee L.Y., Chen W.P., et al. A comparative proteomic analysis of erinacine A’s inhibition of gastric cancer cell viability and invasiveness. Cell. Physiol. Biochem. 2017;43:195–208. doi: 10.1159/000480338. [DOI] [PubMed] [Google Scholar]
- 92.Zang M.D., Hu L., Fan Z.Y., Wang H.X., Zhu Z.L., Cao S., Wu X.Y., Li J.F., Su L.P., Li C., et al. Luteolin suppresses gastric cancer progression by reversing epithelial-mesenchymal transition via suppression of the Notch signaling pathway. J. Transl. Med. 2017;15:52. doi: 10.1186/s12967-017-1151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zhang X.K., Zheng L.M., Sun Y.G., Wang T.X., Wang B.C. Tangeretin enhances radiosensitivity and inhibits the radiation-induced epithelial-mesenchymal transition of gastric cancer cells. Oncol. Rep. 2015;34:302–310. doi: 10.3892/or.2015.3982. [DOI] [PubMed] [Google Scholar]
- 94.Park H.S., Kim G.Y., Choi I.W., Kim N.D., Hwang H.J., Choi Y.W., Choi Y.H. Inhibition of matrix metalloproteinase activities and tightening of tight junctions by diallyl disulfide in AGS human gastric carcinoma cells. J. Food Sci. 2011;76:T105–T111. doi: 10.1111/j.1750-3841.2011.02114.x. [DOI] [PubMed] [Google Scholar]
- 95.Liu Q., Meng X., Li Y., Zhao C.N., Tang G.Y., Li S., Gan R.Y., Li H.B. Natural products for the prevention and management of Helicobacter pylori infection. Compr. Rev. Food Sci. Food. 2018;17:937–952. doi: 10.1111/1541-4337.12355. [DOI] [PubMed] [Google Scholar]
- 96.Covacci A., Telford J.L., Del Giudice G., Parsonnet J., Rappuoli R. Helicobacter pylori virulence and genetic geography. Science. 1999;284:1328–1333. doi: 10.1126/science.284.5418.1328. [DOI] [PubMed] [Google Scholar]
- 97.Overby A., Zhao C.M., Chen D. Plant phytochemicals: Potential anticancer agents against gastric cancer. Curr. Opin. Pharmacol. 2014;19:6–10. doi: 10.1016/j.coph.2014.05.010. [DOI] [PubMed] [Google Scholar]
- 98.Wang Y.C. Medicinal plant activity on Helicobacter pylori related diseases. World J. Gastroenterol. 2014;20:10368–10382. doi: 10.3748/wjg.v20.i30.10368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Vale F.F., Oleastro M. Overview of the phytomedicine approaches against Helicobacter pylori. World J. Gastroenterol. 2014;20:5594–5609. doi: 10.3748/wjg.v20.i19.5594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mahady G.B., Pendland S.L., Yun G.S., Lu Z.Z., Stoia A. Ginger (Zingiber officinale Roscoe) and the gingerols inhibit the growth of Cag A+ strains of Helicobacter pylori. Anticancer Res. 2003;23:3699–3702. [PMC free article] [PubMed] [Google Scholar]
- 101.Sekiguchi H., Washida K., Murakami A. Suppressive effects of selected food phytochemicals on CD74 expression in NCI-N87 gastric carcinoma cells. J. Clin. Biochem. Nutr. 2008;43:109–117. doi: 10.3164/jcbn.2008054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kuo C.H., Weng B.C., Wu C.C., Yang S.F., Wu D.C., Wang Y.C. Apigenin has anti-atrophic gastritis and anti-gastric cancer progression effects in Helicobacter pylon-infected Mongolian gerbils. J. Ethnopharmacol. 2014;151:1031–1039. doi: 10.1016/j.jep.2013.11.040. [DOI] [PubMed] [Google Scholar]
- 103.De R., Kundu P., Swarnakar S., Ramamurthy T., Chowdhury A., Nair G.B., Mukhopadhyay A.K. Antimicrobial activity of curcumin against Helicobacter pylori isolates from india and during infections in mice. Antimicrob. Agents Chemother. 2009;53:1592–1597. doi: 10.1128/AAC.01242-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Qi Y.F., Sun J.N., Ren L.F., Cao X.L., Dong J.H., Tao K., Guan X.M., Cui Y.N., Su W. Intestinal microbiota is altered in patients with gastric cancer from Shanxi province, China. Digest. Dis. Sci. 2019;64:1193–1203. doi: 10.1007/s10620-018-5411-y. [DOI] [PubMed] [Google Scholar]
- 105.Nagano T., Otoshi T., Hazama D., Kiriu T., Umezawa K., Katsurada N., Nishimura Y. Novel cancer therapy targeting microbiome. OncoTargets Ther. 2019;12:3619–3624. doi: 10.2147/OTT.S207546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lofgren J.L., Whary M.T., Ge Z.M., Muthupalani S., Taylor N.S., Mobley M., Potter A., Varro A., Eibach D., Suerbaum S., et al. Lack of commensal flora in Helicobacter pylori-infected INS-GAS mice reduces gastritis and delays intraepithelial neoplasia. Gastroenterology. 2011;140:210–220. doi: 10.1053/j.gastro.2010.09.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kikuchi H., Ohtsuki T., Koyano T., Kowithayakorn T., Sakai T., Ishibashi M. Activity of mangosteen xanthones and teleocidin A-2 in death receptor expression enhancement and tumor necrosis factor related apoptosis-inducing ligand assays. J. Nat. Prod. 2010;73:452–455. doi: 10.1021/np900404e. [DOI] [PubMed] [Google Scholar]
- 108.Huang W.F., Wan C.P., Luo Q.C., Huang Z.J., Luo Q. Genistein-Inhibited cancer stem cell-like properties and reduced chemoresistance of gastric cancer. Int. J. Mol. Sci. 2014;15:3432–3443. doi: 10.3390/ijms15033432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jin H., Park M.H., Kim S.M. 3,3‘-Diindolylmethane potentiates paclitaxel-induced antitumor effects on gastric cancer cells through the Akt/FOXM1 signaling cascade. Oncol. Rep. 2015;33:2031–2036. doi: 10.3892/or.2015.3758. [DOI] [PubMed] [Google Scholar]
- 110.Pan Y.M., Lin S.Y., Xing R., Zhu M., Lin B.N., Cui J.T., Li W.M., Gao J., Shen L., Zhao Y.Y., et al. Epigenetic upregulation of metallothionein 2a by diallyl trisulfide enhances chemosensitivity of human gastric cancer cells to docetaxel through attenuating NF-κB activation. Antioxid. Redox Sign. 2016;24:839–854. doi: 10.1089/ars.2014.6128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Jiang X.Y., Zhu X.S., Xu H.Y., Zhao Z.X., Li S.Y., Li S.Z., Cai J.H., Cao J.M. Diallyl trisulfide suppresses tumor growth through the attenuation of Nrf2/Akt and activation of p38/JNK and potentiates cisplatin efficacy in gastric cancer treatment. Acta Pharmacol. Sin. 2017;38:1048–1058. doi: 10.1038/aps.2016.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Luo Y.J., Zha L., Luo L.M., Chen X., Zhang Q., Gao C.X., Zhuang X.B., Yuan S.J., Qiao T.K. [6]-Gingerol enhances the cisplatin sensitivity of gastric cancer cells through inhibition of proliferation and invasion via PI3K/Akt signaling pathway. Phytother. Res. 2019;33:1353–1362. doi: 10.1002/ptr.6325. [DOI] [PubMed] [Google Scholar]
- 113.Jia N., Xiong Y.L.L., Kong B.H., Liu Q., Xia X.F. Radical scavenging activity of black currant (Ribes nigrum L.) extract and its inhibitory effect on gastric cancer cell proliferation via induction of apoptosis. J. Funct. Foods. 2012;4:382–390. doi: 10.1016/j.jff.2012.01.009. [DOI] [Google Scholar]
- 114.Pan M.H., Chang Y.H., Badmaev V., Nagabhushanam K., Ho C.T. Pterostilbene induces apoptosis and cell cycle arrest in human gastric carcinoma cells. J. Agric. Food Chem. 2007;55:7777–7785. doi: 10.1021/jf071520h. [DOI] [PubMed] [Google Scholar]
- 115.Hong J.Y., Song S.H., Park H.J., Cho Y.J., Pyee J.H., Lee S.K. Antioxidant, antiinflamatory, and antiproliferative activities of strawberry extracts. Biomol. Ther. 2008;16:286–292. doi: 10.4062/biomolther.2008.16.3.286. [DOI] [Google Scholar]
- 116.Jung E.B., Trinh T.A., Lee T.K., Yamabe N., Kang K.S., Song J.H., Choi S., Lee S., Jang T.S., Kim K.H., et al. Curcuzedoalide contributes to the cytotoxicity of Curcuma zedoaria rhizomes against human gastric cancer AGS cells through induction of apoptosis. J. Ethnopharmacol. 2018;213:48–55. doi: 10.1016/j.jep.2017.10.025. [DOI] [PubMed] [Google Scholar]
- 117.Olivas-Aguirre F.J., Rodrigo-Garcia J., Martinez-Ruiz N.D., Cardenas-Robles A.I., Mendoza-Diaz S.O., Alvarez-Parrilla E., Gonzalez-Aguilar G.A., de la Rosa L.A., Ramos-Jimenez A., Wall-Medrano A. Cyanidin-3-O-glucoside: Physical-chemistry, foodomics and health effects. Molecules. 2016;21:1264. doi: 10.3390/molecules21091264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Itoh H., Ito H., Hibasami H. Blazein of a new steroid isolated from Agaricus blazei Murrill (himematsutake) induces cell death and morphological change indicative of apoptotic chromatin condensation in human lung cancer LU99 and stomach cancer KATO III cells. Oncol. Rep. 2008;20:1359–1361. [PubMed] [Google Scholar]
- 119.Oliveira M., Reis F.S., Sousa D., Tavares C., Lima R.T., Ferreira I.C.F.R., dos Santos T., Vasconcelos M.H. A methanolic extract of Ganoderma lucidum fruiting body inhibits the growth of a gastric cancer cell line and affects cellular autophagy and cell cycle. Food Funct. 2014;5:1389–1394. doi: 10.1039/C4FO00258J. [DOI] [PubMed] [Google Scholar]
- 120.Liang C.Y., Li H.R., Zhou H., Zhang S.Q., Liu Z.Y., Zhou Q.L., Sun F. Recombinant Lz-8 from Ganoderma lucidum induces endoplasmic reticulum stress-mediated autophagic cell death in SGC-7901 human gastric cancer cells. Oncol. Rep. 2012;27:1079–1089. doi: 10.3892/or.2011.1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Shomori K., Yamamoto M., Arifuku I., Teramachi K., Ito H. Antitumor effects of a water-soluble extract from Maitake (Grifola frondosa) on human gastric cancer cell lines. Oncol. Rep. 2009;22:615–620. doi: 10.3892/or_00000480. [DOI] [PubMed] [Google Scholar]
- 122.Oliveira H., Cai X.S., Zhang Q., de Freitas V., Mateus N., He J.R., Fernandes I. Gastrointestinal absorption, antiproliferative and anti-inflammatory effect of the major carotenoids of Gardenia jasminoides Ellis on cancer cells. Food Funct. 2017;8:1672–1679. doi: 10.1039/C7FO00091J. [DOI] [PubMed] [Google Scholar]
- 123.Lee S.H., Choi W.C., Kim K.S., Park J.W., Lee S.H., Yoon S.W. Shrinkage of gastric cancer in an elderly patient who received Rhus verniciflua stokes extract. J. Altern. Complem. Med. 2010;16:497–500. doi: 10.1089/acm.2008.0237. [DOI] [PubMed] [Google Scholar]
- 124.Li W.Q., Zhang J.Y., Ma J.L., Li Z.X., Zhang L., Zhang Y., Guo Y., Zhou T., Li J.Y., Shen L., et al. Effects of Helicobacter pylori treatment and vitamin and garlic supplementation on gastric cancer incidence and mortality: Follow-up of a randomized intervention trial. BMJ Br. Med. J. 2019;366:15016. doi: 10.1136/bmj.l5016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ina K., Kataoka T., Ando T. The use of lentinan for treating gastric cancer. Anti-Cancer Agents Med. Chem. 2013;13:681–688. doi: 10.2174/1871520611313050002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Ito G., Tanaka H., Ohira M., Yoshii M., Muguruma K., Kubo N., Yashiro M., Yamada N., Maeda K., Sawada T., et al. Correlation between efficacy of PSK postoperative adjuvant immunochemotherapy for gastric cancer and expression of MHC class I. Exp. Ther. Med. 2012;3:925–930. doi: 10.3892/etm.2012.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Banerjee S., Kong D.J., Wang Z.W., Bao B., Hillman G.G., Sarkar F.H. Attenuation of multi-targeted proliferation-linked signaling by 3,3‘-diindolylmethane (DIM): From bench to clinic. Mutat. Res. Rev. Mutat. 2011;728:47–66. doi: 10.1016/j.mrrev.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Mannava M.K.C., Suresh K., Bommaka M.K., Konga D.B., Nangia A. Curcumin-artemisinin coamorphous solid: Xenograft model preclinical study. Pharmaceutics. 2018;10:7. doi: 10.3390/pharmaceutics10010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Correa-Betanzo J., Allen-Vercoe E., McDonald J., Schroeter K., Corredig M., Paliyath G. Stability and biological activity of wild blueberry (Vaccinium angustifolium) polyphenols during simulated in vitro gastrointestinal digestion. Food Chem. 2014;165:522–531. doi: 10.1016/j.foodchem.2014.05.135. [DOI] [PubMed] [Google Scholar]
- 130.Fang J. Bioavailability of anthocyanins. Drug Metab. Rev. 2014;46:508–520. doi: 10.3109/03602532.2014.978080. [DOI] [PubMed] [Google Scholar]
- 131.Aditya N.P., Shim M., Lee I., Lee Y., Im M.H., Ko S. Curcumin and genistein coloaded nanostructured lipid carriers: In vitro digestion and antiprostate cancer activity. J. Agric. Food Chem. 2013;61:1878–1883. doi: 10.1021/jf305143k. [DOI] [PubMed] [Google Scholar]
- 132.Sun Y., Xia Z.Y., Zheng J.K., Qiu P.J., Zhang L.J., McClements D.J., Xiao H. Nanoemulsion-based delivery systems for nutraceuticals: Influence of carrier oil type on bioavailability of pterostilbene. J. Funct. Foods. 2015;13:61–70. doi: 10.1016/j.jff.2014.12.030. [DOI] [Google Scholar]
- 133.Daware M.B., Mujumdar A.M., Ghaskadbi S. Reproductive toxicity of piperine in Swiss albino mice. Planta Med. 2000;66:231–236. doi: 10.1055/s-2000-8560. [DOI] [PubMed] [Google Scholar]
- 134.Walsh K.R., Zhang Y.C., Vodovotz Y., Schwartz S.J., Failla M.L. Stability and bioaccessibility of isoflavones from soy bread during in vitro digestion. J. Agric. Food Chem. 2003;51:4603–4609. doi: 10.1021/jf0342627. [DOI] [PubMed] [Google Scholar]
- 135.Reis F.S., Martins A., Vasconcelos M.H., Morales P., Ferreira I.C.F.R. Functional foods based on extracts or compounds derived from mushrooms. Trends Food Sci. Technol. 2017;66:48–62. doi: 10.1016/j.tifs.2017.05.010. [DOI] [Google Scholar]
- 136.Leibelt D.A., Hedstrom O.R., Fischer K.A., Pereira C.B., Williams D.E. Evaluation of chronic dietary exposure to indole-3-carbinol and absorption-enhanced 3,3‘-diindolylmethane in Sprague-Dawley rats. Toxicol. Sci. 2003;74:10–21. doi: 10.1093/toxsci/kfg103. [DOI] [PubMed] [Google Scholar]
- 137.Li G., Yu K., Li F.S., Xu K.P., Li J., He S.J., Cao S.S., Tan G.S. Anticancer potential of Hericium erinaceus extracts against human gastrointestinal cancers. J. Ethnopharmacol. 2014;153:521–530. doi: 10.1016/j.jep.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 138.Balaji S., Chempakam B. Pharmacokinetics prediction and drugability assessment of diphenylheptanoids from turmeric (Curcuma longa L) Med. Chem. 2009;5:130–138. doi: 10.2174/157340609787582873. [DOI] [PubMed] [Google Scholar]