Abstract
Background:
The school health program is a flagship program of Government of India with a focus on improving the physical and mental health of school children, but there is no specific strategy to screen for mental health disorders under the school health program. Also, the estimation of the prevalence of common mental disorders (CMDs) such as anxiety, depression, and psychosocial distress among school children is lacking.
Methods:
The author conducted a cross-sectional study among 742 adolescent schoolgirls from one government, one government-aided, and one private school in an urban area in Gujarat. We used the pre-validated instrument, general health questionnaire-12 (GHQ-12) to screen for CMDs. We estimated adjusted odds of association between screening positive for CMDs and various determinants.
Results:
48.78% adolescent girls screened positive for CMDs which is alarming. Among sociodemographic characteristics, the type of school (adjusted odds of private is 1.8 and government 1.6), mother's higher education (3.0), father's less education (3.1), and working mother (1.5) had shown significant association with positive cases of the girls. Among psychosocial factors, abnormal sleep patterns (1.9) and disturbance in studies (2.3) have been found statistically significant for the presence of mental health problems among adolescent girls as per the GHQ score.
Conclusion:
CMDs such as anxiety, depression, and psychosocial distress were indeed very common among adolescent school-going girls in an urban area of Gujarat, India. There is an urgent need to focus attention on the mental health of adolescent girls.
Keywords: Adolescent, GHQ-12, mental health, school health
Introduction
Mental health is an integral part of health and is more than the mere absence of mental illnesses.[1] Nowadays, mental health problems are common in all age groups.[2] The challenge of adapting to one's own changing body and social role expectations contribute to negative affect and lead to mental disorders during adolescent development.[3] Adolescents experience a wide range of emotions as part of normal development. Adolescents often suffer from mild psychosocial problems such as anxiousness about school or friendship or experience a period of depression following the death of a close friend or family member.[4] Many of these problems are transient and are often not noticed. Several key transitional periods (moving from early elementary to middle school, moving from middle school to high school, or moving from high school to college) can present new challenges for these adolescents and the symptoms of dysfunction may occur. Heavy academic and social pressure may result in negative emotional states and more internalizing problems among adolescents.[5]
Depression and anxiety are the most common mental health problems among adolescents.[5,6] Between 20% and 50% of adolescents' self-report depressive symptoms with significant and regular co-occurrence of the anxiety symptoms.[7,8]
Poor awareness about the symptoms of psychiatric disorders, myths, and stigma related to it, the lack of knowledge of treatment availability and benefits from treatment compound the problem. Promoting positive mental health among adolescents can nip some of these problems in the bud itself. For adolescents who already have mental health disorders, screening, early intervention, and treatment can help lessen the impact of the disease on their lives.
Providing mental health services in primary healthcare involves diagnosis, treatment, and prevention of mental disorders. The inclusion of mental health screening will improve overall health outcomes among adolescents in primary healthcare. Primary care physicians of government primary health centers (PHC) are involved in the yearly exercise of assessing the health of school children during the school health program. Also, there is a provision of adolescent-friendly health services on designated days at the PHC so that adolescents can freely seek health services including screening for mental health issues and get requisite treatment. The school health program is a country-wide flagship program of Government of India with a focus on improving the physical and mental health of school children.[9] However, in the present scheme of things under this program, the component of mental health only focuses on learning and behavior disorders. There is no specific strategy to screen for mental health disorders, which is an opportunity lost. As a result, the estimates of the prevalence of common mental disorders (CMDs) among school children are not available. Therefore, this study aimed to screen for CMDs and find out sociodemographic and behavioral determinants for positive screened school-going adolescent girls in an urban area in Gujarat.
Materials and Methods
This was a school-based cross-sectional study conducted for 6 months among school-going adolescent girls of Jamnagar district, Gujarat. We estimated the sample size for this research study considering the proportion of adolescents girls in schools as 40%, a sample size of 576 was needed according to the table provided in the WHO practical manual for the estimation of sample size.[10] We considered a design effect of 1.2 and a nonresponse of 10% in the study; hence, the total sample size required for the study was 760.
There are a total of 85 high schools in Jamnagar, Gujarat, of which 4 were government, 22 were government-aided (aided), and 59 were privately run schools. The total number of high schools-going adolescent girls were 18,061 during the study period. We used a multistage stratified random sampling technique to select one school from each category by a simple random method using a random number table. We adopted this method to ensure equal representation to adolescent girls belonging to three categories of schools (viz. government, government-aided, and private schools). Further from each of these chosen schools, we selected two classes each from classes 8–12 through the simple random method. All the girl students present on the day of the study visit and those agreed to participate in the study voluntarily were included in the study. Finally, 275 adolescent girls from a government school, 248 adolescent girls from aided school, and 219 adolescent girls from private school were included, thus, 742 adolescent girls (98%) were studied [Figure 1].
Figure 1.
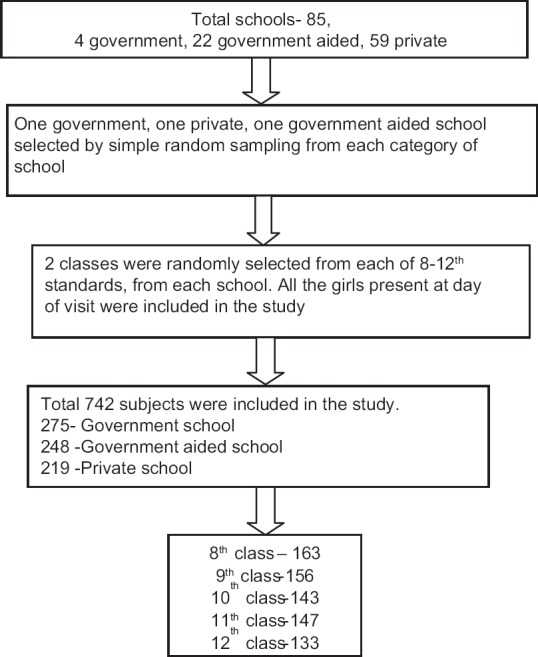
Sampling frame
The study tool was pretested, semi-structured, and prepared after an extensive review of available literature and consulting experts in the related field of our institution. We collected information on the sociodemographic profile and psychosocial health status of adolescent girls. Working definitions were used to assess psychosocial and other factors in the study after an extensive review of literature and consultation with experts. We collected the information on factors affecting mental health through self-reported responses by the study subjects. Sleep disturbance was considered when any of the following symptoms were reported: difficulty in initiation of sleep, maintenance of sleep, or early arousal. Disturbance in the study was recorded if a subject cannot focus on studies, inability to perform daily homework, and any specified reasons (e.g. conflicts or illness in the family, financial constraints, feeling of being in love, etc.). Similarly, for comparison to peers, we asked about any subjective experience of feeling pressured, urged, or dared by others to do certain things or doing things because others have pressured, urged, or challenged. For substance use, those who currently used or ever used it in the past were included.
General health questionnaire-12 (GHQ-12) is a self-administered questionnaire for screening common mental health problems. It is a 12-question tool with a 2-point scoring (yes and no) and is designed to identify the presence of possible nonpsychotic mental health disorders, that is, anxiety, depression, and psychological distress.[11,12] It has adequate sensitivity and specificity to identify disorders such as anxiety and depression.[13,14,15,16] The 12 questions of GHQ assess the extent to which a respondent experienced happiness, depression, anxiety, and sleep disturbance in 1 month preceding the interview.[11] A two-point scoring scale is reliable.[17] The presence of three or more is suggestive of mental health disorders, requiring further assessment.[11] GHQ-12 has been validated for use among adolescents.[18]
We entered the data in MS Excel and analyzed in SPSS version 17. Appropriate statistics including bivariate analysis (Chi-square test) was used to assess the association between various sociodemographic characteristics and psychosocial factors with the presence of mental health problems as per the GHQ score. Modeling was done using multiple logistic regressions to identify significant risk factors.
The ethical committee of the M P Shah Medical College, Jamnagar, Gujarat approved the study Ethics Committee approval had been obtained. Date of approval is 11.11.2010. Permission to conduct the study in high schools was taken from the district education officer and the school principals. Written informed consent was taken from the study subjects. Privacy and confidentiality were maintained during data collection and analysis.
Results
In our study, we studied a total of 742 adolescent girls from one government school, one private school, and one aided school randomly selected from the schools in Jamnagar, Gujarat. Out of 742 adolescent girls, 207 (27.90%) girls belonged to the stage of early adolescence (10–13 years), 241 (32.48%) girls belonged to middle adolescence (14–15 years), and 294 (39.62%) girls belonged to late adolescence (16–19 years).
In this study, almost half (48.78%) adolescent girls reported three or more symptoms suggestive of mental health problems, which is an alarming observation [Table 1].
Table 1.
Distribution of adolescents based on total GHQ-12 Score
| GHQ score | Frequency | Percentage |
|---|---|---|
| Less than 3 | 380 | 51.21 |
| More than 3 | 362 | 48. 79 |
| Total | 742 | 100.0 |
GSQ-12: general health questionnaire-12
Table 2 shows multiple responses to various questions of GHQ as given by adolescent girls, suggested deviation from mental well-being.
Table 2.
Distribution of adolescent girls according to the responses to individual items on GHQ-12 screening tool (n=742)
| GHQ-12 | Yes (%) | No (%) |
|---|---|---|
| Are you able to concentrate on what you are doing? | 527 (71.02) | 215 (28.98) |
| Lost sleep over worry | 313 (42.18) | 429 (57.82) |
| Can you take decisions? | 431 (58.09) | 311 (41.91) |
| Do you feel you are under strain? | 133 (17.92) | 605 (81.54) |
| Can you face up to your problems? | 535 (72.10) | 207 (27.90) |
| Can you overcome your difficulties? | 535 (72.10) | 207 (27.90) |
| Do you enjoy day to day activities? | 639 (86.12) | 103 (13.88) |
| Have you been feeling unhappy and depressed? | 119 (16.04) | 623 (83.96) |
| Have you been losing confidence in yourself? | 89 (11.99) | 653 (88.01) |
| Do you feel you are not playing a useful role? | 113 (15.23) | 629 (84.77) |
| Do you feel you are worthless? | 113 (15.23) | 629 (84.77) |
| Do you feel reasonably happy? | 625 (84.23) | 117 (15.77) |
Several sociodemographic and psychosocial factors have shown significant association with the presence of mental illness symptoms as per the GHQ score. Among sociodemographic characteristics, type of school, mother's education, father's education, and working status of the mother have shown significant association with the presence of mental health problems among adolescent girls as per GHQ score [Table 3].
Table 3.
Distribution of adolescent girls based on their GHQ score and sociodemographic characteristics
| Sociodemographic factors | GHQ score | X2, df, P | |
|---|---|---|---|
| ≥3 | <3 | ||
| Type of school | n=362 | n=380 | χ2=17.768, df=2, P<0.001 |
| Aided | 94 (26.0) | 154 (40.5) | |
| Government | 151 (41.7) | 124 (32.6) | |
| Private | 117 (32.3) | 102 (26.8) | |
| Age group | |||
| 10-13 (early adolescents) | 79 (21.9) | 128 (34.0) | χ2=16.357, df=2, P<0.000 |
| 14-15 (Middle adolescents) | 138 (38.2) | 103 (27.3) | |
| 16-19 (Late adolescents) | 144 (39.9) | 146 (36.7) | |
| Class | |||
| Board | 144 (39.8) | 132 (34.7) | χ2=2.018, df=1, P=0.155 |
| Non-board | 218 (60.2) | 248 (65.3) | |
| Type of family | χ2 3.628, df=1, P<0.05 |
||
| Nuclear | 248 (68.5) | 235 (61.8) | |
| Joint | 114 (31.5) | 145 (38.2) | |
| Mother’s education | |||
| Less than primary | 238 (65.7) | 209 (55.0) | χ2=14.077, df=2, P=0.001 |
| Up to class 12th | 84 (23.3) | 136 (35.8) | |
| Graduate and above | 40 (11.0) | 35 (9.2) | |
| Father’s education | |||
| Less than primary | 176 (48.6) | 141 (37.1) | χ2=15.544, df=2, P=0.0001 |
| Up to class 12th | 134 (37.0) | 146 (38.4) | |
| Graduate and above | 52 (14.4) | 93 (24.5) | |
| Mother’s working status | |||
| Not working | 273 (45.7) | 325 (54.3) | χ2=12.120, df=1, P=0.001 |
| Working | 89 (61.8) | 55 (38.2) | |
Among psychosocial factors, abnormal sleep pattern, feeling of inferiority in looks and academics as compared to their peers, the presence of comparison with peers, and disturbance in studies have been found statistically significant to the presence of mental health problems among adolescent girls as per GHQ score [Table 4].
Table 4.
Distribution of adolescent girls based on their GHQ score and psychosocial characteristics
| Psychosocial issues | GHQ score | X2, df, P | |
|---|---|---|---|
| ≥3 | <3 | ||
| Sleep pattern | 362 | 380 | χ2=18.96, df=1, P=0.001 |
| Abnormal | 65 (17.9) | 28 (7.4) | |
| Normal | 297 (82.1) | 352 (92.6) | |
| Substance use | |||
| Yes | 24 (6.6) | 17 (4.5) | χ2=1.651, df=1, P=0.119 |
| No | 338 (93.3) | 363 (95.5) | |
| Feeling of inferiority in academics as compared to their peers | |||
| Yes | 204 (56.4) | 158 (41.5) | χ2=16.197, df=1, P=0.001 |
| No | 158 (43.6) | 222 (58.4) | |
| Feeling of inferiority in looks as compared to their peers | χ2=13.281, df=1, P=0.001 |
||
| Yes | 99 (27.3) | 62 (16.3) | |
| No | 263 (72.7) | 318 (83.7) | |
| Comparison with peers | χ2=7.582, df=1, P=0.006 |
||
| Yes | 49 (13.5) | 28 (7.4) | |
| No | 313 (86.5) | 352 (92.6) | |
| Disturbance in studies | χ2=32.01, df=1, P=0.0001 |
||
| Yes | 135 (37.3) | 71 (18.7) | |
| No | 227 (62.7) | 309 (81.3) | |
Multiple logistic regressions were done to compute the corrected odds ratio for the effect of various sociodemographic and psychosocial factors on having a high GHQ score. GHQ score ≥3 (i.e. high) was taken as a dependent factor, and all the significant sociodemographic and psychosocial factors on bivariate analysis have been taken as independent factors. The omnibus test of model coefficients was highly significant (P = 0.000) indicating that the regression model was statistically significant. The goodness of fit of the logistic regression model was seen using the Hosmer and Lemeshow Test (Chi-square variable 10.217, df = 8, P = 0.250) which indicated a good fit. Cox and Snell R square (0.149) and Negelkerke R Square (0.199) indicated a weak correlation between the dependent variable and the set of independent variables included. Also, the model is correctly predicting the presence of mental health problems among those who were positive for the GHQ score ≥3 in 63.0% cases while the correct overall prediction was 64.2%.
The adjusted odds ratios revealed that girls studying in private schools were 1.84 times (P = 0.005) and those studying in government schools were 1.63 times (P = 0.015) more likely to have mental health problems as compared to the reference category, that is, aided schoolgirls. Adolescent girls in the age group of middle adolescence were 2.03 times more likely to have mental health problems (P = 0.001). The nuclear family also was found to be a positive predictor (P = 0.026). Girls whose mothers were educated till graduation and above were three times more likely to have these problems (P = 0.001). On the contrary, as the father's educational status decreased, the chances of having these problems increased (P = 0.001). Girls having disturbance in sleep (P = 0.01) and studies (P < 0.000) were more likely to have these issues. The feeling of inferiority in looks and academics and comparison to peers have not shown any significant association on logistic regression analysis [Table 5].
Table 5.
Results of multiple logistic regression analysis with GHQ score ≥3 as a dependent variable
| Variable | P | Adjusted odds ratio | 95% confidence interval |
|---|---|---|---|
| Type of school | |||
| Aided(RC) | |||
| Private | 0.005 | 1.836 | 1.207-2.795 |
| Government | 0.015 | 1.631 | 1.101-2.417 |
| Family | |||
| Nuclear family | 0.026 | 1.462 | 1.047-2.043 |
| Joint family(RC) | |||
| Age (in completed years) | |||
| 10-13(RC) | |||
| 14-15 | 0.001 | 2.032 | 1.321-3.126 |
| 16-19 | 0.244 | 1.276 | 0.847-1.920 |
| Mother’s education | |||
| Less than primary | 0.308 | 1.228 | 0.827-1.823 |
| Up to class 12th(RC) | 1 | ||
| Graduate and above | 0.001 | 3.008 | 1.544-5.863 |
| Father’s education | |||
| Less than primary | 0.001 | 3.190 | 1.794-5.670 |
| Up to class 12th | 0.001 | 2.638 | 1.541-4.515 |
| Graduate and above(RC) | |||
| Mother’s working status | |||
| Working | 0.045 | 1.520 | 1.009-2.289 |
| Sleep pattern | |||
| Abnormal | 0.010 | 1.979 | 1.180-3.318 |
| Feeling of inferiority in academics as compared to their peers | |||
| Yes | 0.101 | 1.326 | 0.947-1.857 |
| Feeling of inferiority in looks as compared to their peers | |||
| Yes | 0.199 | 1.304 | 0.870-1.956 |
| Comparison with peers | |||
| Yes | 0.245 | 1.389 | 0.799-2.415 |
| Disturbance in studies | |||
| Yes | 0.001 | 2.252 | 1.549-3.272 |
RC: reference category
Discussion
Worldwide 10–20% of children and adolescents experience mental disorders.[19] Half of all mental illnesses begin by the age of 14 and three-quarters by mid-20s. Neuropsychiatric conditions are the leading cause of disability in young people in all regions.[19] If untreated, these conditions severely influence children's development, their educational status, and their potential to live fulfilling and productive lives. Children with mental disorders face major challenges with stigma, isolation, and discrimination, as well as lack of access to health care and education facilities, in violation of their fundamental human rights.[9] Mental health problems in adolescence have a significant impact on academic and social achievements, with negative consequences extending into adulthood.[20] A substantial proportion of mental health problems in adolescence persist into adulthood.[8]
Mental health problems are on the verge of being epidemic, not leaving a single section of life untouched. Most of the studies on mental health among adolescents have been on single disease entities such as depression, anxiety, or psychosocial distress. In a few studies, all three disorders have been included using different scales of measure which are practically difficult to apply for screening purposes. In this study, we tried to find the prevalence of common mental health problems among adolescent girls using GHQ-12, which has been validated for use as a screening tool among adolescents in India.[11] GHQ score helps in identifying probable depression, anxiety, and psychological distress at the same time. It is a short but reliable[13,14,17] tool, therefore, it can be incorporated in school health programs easily. Those who screened positive can be referred for definitive diagnosis using more definitive instruments or can be evaluated by a psychiatrist.
In this study, around half of the subjects (48.8%) were diagnosed as having a common mental health problem, which is very high as compared to other school-based studies conducted in schools elsewhere in India.[19,21,22] It could be due to several reasons: our study collected data anonymously; hence, there was no fear of anyone finding out who has responded to what. Therefore, the stigma of being labeled as mentally ill by classmates or teachers could be avoided. Another reason is the use of different scales to measure mental health problems in different studies and the absence of the gold standard screening test. Different studies have taken different age groups of adolescents or some included children in their study.[17,19,22,23] Being in “middle adolescence” age was found to be another significant factor among our study subjects for screening positive for mental distress. This might be due to the fact that in this stage, the psychological effects of risk-taking behavior and peer pressure are more pronounced as compared to early (who are more child-like) and late adolescents (who have adjusted to the changes of adolescence).[22]
Type of school was an important determinant of screening positive for mental health problems among adolescent girls. In government schools of Gujarat, the education of girls was free, aided schools usually charged less than private schools. So, the type of school served as a proxy indicator for socioeconomic status in the study which otherwise would have been difficult to assess by other criteria as exact information regarding the income of family could not be correctly reported by school students. On logistic regression, the government school's girls were most likely to have mental health issues. So, we assume that such higher odds of occurrence of mental illness in government school might be due to the higher probability of students coming from lower-income families. Though, we have not taken socioeconomic status directly; our findings were like other Indian studies where psychiatric morbidities have shown a significant positive association with lower socioeconomic class.[20,21,24]
In our study, education in private schools and higher education level of the mother were also found to put school-going girls at higher risk of suffering from mental distress. This might be because mothers of these girls were probably working outside the home to add income to their family corpus and due to which they spent less time with their children. An adolescent girl has a more emotional relationship with her mother. Lack of such emotional support might create emotional unbalance and lead to mental and behavioral issues. This is coherent with our finding that having a working mother was more likely to have a higher GHQ score suggesting mental health issues. The same reasons might explain the higher likelihood of mental illness in girls with the nuclear family in our study. Relationship with mother was found an important predictor in a study conducted by Mishra et al.[20] in school-going adolescent girls. Also, another school-based study by Anita et al.[25] and Kaur et al.[23] had shown a significant relationship with the nuclear family. Our study found an inverse relationship between father's educational status and mental distress among adolescent girls. Having a better-educated father meant better mental health for girls. This could be due to increased involvement of fathers in parenting with better education leading to more adjusted adolescents.
Sleep disturbance and disturbance in studies were found to be strong predictors of mental illness in our study. Similarly, being unable to cope up with studies was significantly associated with mental illness (as per their GHQ score) in a study by Bansal et al.[24] Inferiority complex (in looks and academics) was not found to be a significant factor causing mental distress.
Child mental health policy and school mental health programs had provided an excellent opportunity to enhance mental health programs for children and adolescents.[26] The focus was on preventing illness and possibly promote positive mental health. Also to ensure a reduction in behavior disorders in children and prevent adult psychopathology in the long run.[27] Previously also it has been noted that it is crucial to partner with services whose primary function is not mental health care, such as general practitioners and school health programs instead of just depending on specialist psychiatric care. Schools could contribute by identifying mental health problems early, offering general supportive advice, and prompt referral for treatment.[28] But, in India, school health programs have become almost defunct because of the administrative, managerial, and logistic problems.[29] Also, mental health has remained elusive even after implementing the National Mental Health Program (launched way back in 1982).[29]
There were three main limitations of our study. First, we could not use predesigned questionnaires to measure various psychosocial factors such as inferiority complex, comparison with peers, sleep disturbance, and disturbance in studies. The use of such questionnaires would have made our instrument very lengthy and difficult to understand for students. Our objective was to find out as much as possible about the magnitude of the issues faced by adolescent girls. A more specific and detailed study could be planned to address each one of these issues separately. A second important limitation is that the study favorably included girl students present on the day of the study due to which chronic absentees and sick children were left out (sickness absenteeism). There was no possible way to assess these adolescents. The third limitation was that the study did not include out-of-school adolescents.
We conclude that common mental health problems such as anxiety, depression, and psychosocial distress were indeed very common among adolescent school-going girls in an urban area of Gujarat, India. There is an urgent need to focus our attention on the positive mental health of adolescent girls. Insight about the cause of CMDs can be obtained by studying important determinants such as poor interpersonal relationships with parents, the pressure of studies, peer pressure, etc., There is an urgent need to tackle the modifiable risk factors of CMDs among this vulnerable age group via a multipronged approach.
Schools can play a very important role as children spend a lot of time of their day there. Teachers could be trained to identify children having symptoms of CMDs or those having trouble at home, faring poorly in academics, etc., Prompt referral for such students could help manage CMDs early with positive health outcomes. Also, there is an urgent need to implement strategies to incorporate life skill education in the academic curriculum of schools. Lastly, mental health screening should be seriously incorporated in the school health program protocol so that at least once a year students are screened for mental health problems. Health and wellness centers, which are the first point of care both in urban and rural areas could be strengthened to include a screening of mental health diseases for all age groups to identify these diseases at an early stage and managed at the community level.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization. Mental health: Strengthening our response: Fact sheet. 2018. [Last accessed on 2018 Apr. 11]. Available from: http://www.who.int/mediacentre/factsheets/fs220/en/
- 2.National Institute of Mental Health and Neurosciences. National Mental Health Survey of India, 2015-16: Summary. Bengaluru: NIMHANS; 2016. [Google Scholar]
- 3.Kaltiala-Heino R, Marttunenc M, Rantanen P, Rimpela M. Early puberty is associated with mental health problems in middle adolescence. Soc Sci Med. 2003;57:1055–64. doi: 10.1016/s0277-9536(02)00480-x. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Department of Health and Human Services. Mental Health in Adolescents. Available from: https://www.hhs.gov/ash/oah/adolescent-development/mental-health/index.html .
- 5.Ahmad A, Khalique N, Khan ZA, Amir A. Prevalence of psychosocial problems among school going male adolescents. Indian J Community Med. 2007;32:219–21. [Google Scholar]
- 6.World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 7.Jaisoorya TS, Geetha D, Beena KV, Beena M, Ellangovan K, Thennarasu K. Prevalence and correlates of psychological distress in adolescent students from India. East Asian Arch Psychiatry. 2017;27:56–62. [PubMed] [Google Scholar]
- 8.World Health Organization. Mental health: Child and adolescent mental health. 2017. Available from: http://www.who.int/mental_health/maternal-child/child_adolescent/en/
- 9.Ministry of Health and Family Welfare, GoI. Operational Guidelines on School Health Programme under Ayushman Bharat. 2018 [Google Scholar]
- 10.Lwanga SK, Lemeshow S. Sample size determination in health studies- a practical manual. WHO; 1991. [Google Scholar]
- 11.International Institute for Population Sciences (IIPS) and Population Council, 2010. Youth in India: Situation and Needs 2006-2007- EXECUTIVE SUMMARY. Mumbai: IIPS; [Google Scholar]
- 12.General Health questionnaire. Available from: http://chipts.cch.ucla.edu/node/381 . 38. Goldberg DP.
- 13.Baksheev GN, Robinson J, Cosgrave EM, Baker K, Yung AR. Validity of the 12-item General Health Questionnaire (GHQ-12) in detecting depressive and anxiety disorders among high school students. Psychiatry Res. 2011;187:291–6. doi: 10.1016/j.psychres.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 14.Gilbody SM, House AO, Sheldon TA. Routinely administered questionnaires for depression and anxiety: Systematic review. BMJ. 2011;322:406–9. doi: 10.1136/bmj.322.7283.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blackwell B. Psychiatric illness in general practice. A detailed study using a new method of case identification. Br Med J. 1970;1:439–43. doi: 10.1136/bmj.2.5707.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, et al. The validity of two versions of GHQ in the WHO study of mental illness in general health care. Psychol Med. 1997;27:191–7. doi: 10.1017/s0033291796004242. [DOI] [PubMed] [Google Scholar]
- 17.Hankins M. The reliability of the twelve-item general health questionnaire (GHQ-12) under realistic assumptions. BMC Public Health. 2008;8:355. doi: 10.1186/1471-2458-8-355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tait RJ, French DJ, Hulse GK. Validity and psychometric properties of the General Health Questionnaire-12 in young Australian adolescents. Aust N Z J Psychiatry. 2003;37:374–81. doi: 10.1046/j.1440-1614.2003.01133.x. [DOI] [PubMed] [Google Scholar]
- 19.Adolescent Mental Health. Retrieved from World Health Organization; 2019. Available from: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health . [Google Scholar]
- 20.Mishra A, Sharma AK. A clinico-social study of psychiatric morbidities in 12-18 years school going girls in Urban Delhi. Indian J Community Med. 2001;26:71–5. [Google Scholar]
- 21.Balgir RS, Sidhu BS, Garg M, Wats A, Sohal S. Distribution of psychiatric morbidity among school going adolescents in a district of North India. Int J Med Res Health Sci. 2016;5:1–9. [Google Scholar]
- 22.Malhotra S, Patra BN. Prevalence of child and adolescent psychiatric disorders in India. A systematic review and metanalysis. Child Adolesc Psychiatry Ment Health. 2014;8:1–9. doi: 10.1186/1753-2000-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaur S, Thapar SK, Shandilya V. The prevalence of psychiatric morbidity among school children. IJMDS. 2015;4:834–1. [Google Scholar]
- 24.Bansal V, Goyal S, Kalpana S. Study of prevalence of depression in adolescent students of a public school. Ind Psychiatry J. 2009;18:43–6. doi: 10.4103/0972-6748.57859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anita, Gaur DR, Vohra AK, Subash S, Khurana H. Prevalence of psychiatric morbidity among 6 to 14 year old children. Indian J Community Med. 2007;28:7–9. [Google Scholar]
- 26.GoI. (2017, September 20). Ministry of Health and Family Welfare. Retrieved from https://mohfw.gov.in/sites/default/files/Final%20Draft%20Rules%20MHC%20Act%2C%202017%20%281%29.pdf .
- 27.Shastri PC, Shastri JP, Shastri D. Research in child and adolescent psychiatry in India. Indian J Psychiatry. 2010;52(Suppl 1):S219–23. doi: 10.4103/0019-5545.69235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bansal PD, Burman R. Psychopathology of school going children age group 10-15 yrs. Int J Applied Basic Med Res. 2011;1:43–7. doi: 10.4103/2229-516X.81980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lakshminarayanan S. Role of government in public health: Current scenario in India and future scope. J Family Community Med. 2011;18:26–30. doi: 10.4103/1319-1683.78635. [DOI] [PMC free article] [PubMed] [Google Scholar]


