Abstract
Background:
Tooth loss has a negative impact on the person's life so this study was done to assess the impact of tooth loss on oral-health-related quality of life (OHRQoL) in adult patients seeking dental care in private university dental clinics using Arabic version of 14-item Oral Health Impact Profile (OHIP-14) questionnaire in Saudi Arabia.
Materials and Methods:
A cross-sectional study was conducted among 152 patients seeking dental care at a private university dental clinics in Riyadh city, Saudi Arabia. A structured and close-ended OHIP-14 questionnaire was self-administered by the study participants. Descriptive statistics, Kruskal–Wallis, Mann–Whitney, and Spearman's correlation tests were applied to the data.
Results:
Patients with categories 1–5, 6–10, and >10 teeth loss showed a mean OHIP-14 scores of 10.51 ± 10.36, 13.46 ± 10.06, and 21.46 ± 14.41, respectively. A statistically significant difference in OHIP-14 score was observed among different categories of tooth loss (P = 0.005). Participants with >10 teeth loss showed significantly higher OHIP-14 score compared with 1–5 and 6–10 teeth loss categories (P < 0.05). Teeth loss significantly affected the functional limitation (P = 0.000) and social disability (P = 0.044) subscales.
Conclusion:
Tooth loss adversely affected the OHRQoL among the dental patients. As the severity of teeth lost increased, the OHIP-14 score also increased with higher oral health impairments.
Keywords: OHIP-14, oral health, quality of life
Introduction
Loss of permanent teeth among humans is always implicated in progression of dental caries and periodontal diseases in the surrounding teeth. Furthermore, tooth loss can effect individual's psychological, social, and physical impairment thereby declining the quality of life.[1]
The World Health Organization (WHO) Global Oral Health Programme has identified dental caries, periodontal diseases, and dental trauma as the main causes of tooth loss.[2] Previous studies have highlighted early tooth loss in primary and permanent dentitions.[1,3,4] A recent study found tooth loss of 47.4% among adolescents in Eastern province of Saudi Arabia.[5] Contextual variables such as socioeconomic conditions, access to dental care, unhealthy diet, tobacco use, clinical oral health status, oral health knowledge, and behavioral factors have been implicated in prevalence of tooth loss in Saudi Arabia.[1,5,6,7]
Oral-health-related quality of life (OHRQoL) is a multidimensional concept that incorporates physical, psychological, and social well-being components.[8] Patient-based outcome measures are being used widely to get insight into people's perceptions and feelings about their health status to make provision of treatment of oral conditions and rehabilitation of tooth loss.[8,9,10,11] Of all the instruments developed to measure the OHRQoL, the 14-item Oral Health Impact Profile (OHIP-14)[12] is the most commonly used to evaluate the impact of oral health on quality life in adults and the elderly.[11] Recent systematic reviews have pointed out that the tooth loss has an impact on quality of life, irrespective of the type of instrument being used to measure the quality of life.[13,14]
Several studies have examined the impact of tooth loss on OHRQoL among adults and elderly population.[15,16,17,18] But none of the studies has reported the impact of tooth loss on OHRQoL of adults from Saudi Arabia. Hence, the main purpose of this study was to assess the impact of tooth loss on OHRQoL in adult patients seeking dental care in private university dental hospital in Saudi Arabia.
Materials and Methods
A cross-sectional study was conducted among the dental patients attending dental clinics of College of Dentistry, Riyadh Elm University (REU), Riyadh, Saudi Arabia, from September to December 2018. The study was registered with the research Centre of the Riyadh Elm University (FUGRP/2018/156) and ethical approval (RC/IRB/2018/1180) was obtained from the Institutional Review Board of REU (IRB approval received on 07-10-2018). Patient participation in the research was voluntary and an informed consent was obtained before start of the examination.
Sample selection
Only adult male and female patients attending Namuthajiya, Munasiya, and Olaya clinics were selected using convenient sampling methodology. Overall, 201 dental patients were screened, and of these 152 volunteers were invited to participate in the survey after meeting the inclusion criteria of having at least 18 years of age and at least one missing permanent tooth.
Sample size calculation
Considering effect size of F-test = 0.25, α error probability = 0.05, and power of the study 0.79 resulted in a sample size of 152 subjects. The sample size calculation was performed using G * 3.1.9.4 power sample size calculator.
Oral examination
All the oral health examination was carried out by two trained examiners. Training and calibration sessions were held on 10 patients to unify the examination method and to understand the criteria for recording various dental indices.
Plaque index (PI) (Silness and Loe), gingival index (GI) (Loe and Silness), and complete periodontal examination were performed. Numbers of teeth present and missing were noted.
Assessment of OHRQoL
The impact of tooth loss on health-related quality of life was assessed using Arabic version of OHIP-14,[19] which consisted of 14 items with responses rated using a Likert-type scale (0 = never, 1–4 = very often). In addition, socioeconomic, sociodemographic, oral health data, and self-rated oral health were recorded.
Total OHIP-14 score was calculated by addition of all responses of 14 items with scores ranging between 0 and 56. OHIP-14 subscale scores for seven dimensions were obtained by summing the scores for the two items in each subscale. The questionnaire was self-administered.
Statistical analysis
All the data analysis was performed using SPSS version 25.0 (SPSS® Inc., IBM Corp., Armonk, NY, USA) for Windows. Descriptive statistics of frequency distribution, percentages, and mean ± standard deviation (SD) values were calculated for the sample characteristics and OHIP-14 scores. Inferential statistics was done using Mann–Whitney U-test, Kruskal–Wallis H-test, and Spearman's correlation test. Level of statistical significance was set at probability values of less than 0.05.
Results
Most of the study participants were females [83 (54.6%)], age 40–49 years [46 (30.3%)], working in government sector [88 (57.9%)], having college level of education [85 (55.9%)], with income of 5000–10000 SAR [64 (42.1%)]. The study participants brushed their teeth twice daily [65 (42.8%)] using toothbrush and paste (69.7%), 65.1% visited the dentist within the past 6 months, and 76.3% visited for treatment reasons. Self-rated oral health varied among the study subjects, with majority mentioning fair oral health [69 (45.4%)] with more than half [78 (51.3%)] lost 6–10 teeth [Table 1].
Table 1.
Characteristics of the study participants (n=152)
| Variables | n | Percentage | |
|---|---|---|---|
| Age (years) | 18-29 | 40 | 26.3 |
| 30-39 | 44 | 28.9 | |
| 40-49 | 46 | 30.3 | |
| ≥50 | 22 | 14.5 | |
| Gender | Male | 69 | 45.4 |
| Female | 83 | 54.6 | |
| Occupation sector | Government | 88 | 57.9 |
| Private | 64 | 42.1 | |
| Education | ≤High school | 67 | 44.1 |
| College | 85 | 55.9 | |
| Income (SAR) | Less than 5000 | 53 | 34.9 |
| 5000-10,000 | 64 | 42.1 | |
| Above 10,000 | 35 | 23.0 | |
| Oral hygiene material | Toothbrush with paste only | 106 | 69.7 |
| Miswak only | 23 | 15.1 | |
| Tooth brush and floss | 23 | 15.1 | |
| Frequency of tooth brushing | Once/day | 59 | 38.8 |
| Twice/day | 65 | 42.8 | |
| Thrice/day | 28 | 18.4 | |
| Duration since last visit to dentist (months) | 1-6 | 99 | 65.1 |
| 7-12 | 30 | 19.7 | |
| >12 | 23 | 15.1 | |
| Reason for last visit | Pain | 29 | 19.1 |
| Checkup | 7 | 4.6 | |
| Treatment | 116 | 76.3 | |
| Self-rated oral health | Good | 51 | 33.6 |
| Fair | 69 | 45.4 | |
| Poor | 32 | 21.1 | |
| Severity of tooth loss | 1-5 teeth loss | 61 | 40.10 |
| 6-10 teeth loss | 78 | 51.30 | |
| More than 10 teeth loss | 13 | 8.60 |
The GI score (1.31 ± 0.73), PI score (1.16 ± 0.60), number of teeth present (25.07 ± 3.64), mean number of teeth lost (6.89 ± 3.45), clinical attachment loss (2.45 ± 0.77), and overall OHIP-14 score (12.96 ± 10.93) were observed in the study sample [Table 2].
Table 2.
Descriptive statistics of clinical dental variables and overall OHIP-14 scores
| Clinical variables | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| GI score | 1.31 | 0.73 | 0.00 | 3.00 |
| PI score | 1.16 | 0.60 | 0.00 | 2.30 |
| Number of teeth | 25.07 | 3.64 | 7.00 | 31.00 |
| Tooth loss | 6.89 | 3.45 | 2.00 | 19.00 |
| Clinical attachment loss | 2.45 | 0.77 | 1.19 | 6.09 |
| Overall OHIP-14 score | 12.96 | 10.93 | 0.00 | 50.00 |
OHIP-14: 14-item Oral Health Impact Profile; SD: standard deviation; GI: gingival index; PI: plaque index
The mean and SD of OHIP-14 scores were compared across different age groups (P = 0.209), gender (P = 0.99), workplace (P = 0.797), education (P = 0.52), and income (P = 0.522) and they did not show any significant differences [Table 3].
Table 3.
Comparison of overall mean OHIP-14 score among different socioeconomic variables
| Variables | n | Mean | SD | SE | 95% CI for mean | Min | Max | P | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||||||
| Age (years) | 18-29 | 40 | 11.48 | 11.24 | 1.78 | 7.88 | 15.07 | 0.00 | 50.00 | 0.209 |
| 30-39 | 44 | 12.95 | 12.63 | 1.90 | 9.12 | 16.79 | 0.00 | 43.00 | ||
| 40-49 | 46 | 13.33 | 10.39 | 1.53 | 10.24 | 16.41 | 0.00 | 42.00 | ||
| 50 above | 22 | 14.91 | 7.65 | 1.63 | 11.52 | 18.30 | 0.00 | 29.00 | ||
| Total | 152 | 12.96 | 10.93 | 0.89 | 11.21 | 14.71 | 0.00 | 50.00 | ||
| Gender | Male | 69 | 12.74 | 10.50 | 1.26 | 10.22 | 15.26 | 0.00 | 43.00 | 0.99 |
| Female | 83 | 13.14 | 11.34 | 1.24 | 10.67 | 15.62 | 0.00 | 50.00 | ||
| Total | 152 | 12.96 | 10.93 | 0.89 | 11.21 | 14.71 | 0.00 | 50.00 | ||
| Workplace | Government | 88 | 12.65 | 10.76 | 1.15 | 10.37 | 14.93 | 0.00 | 50.00 | 0.797 |
| Private | 64 | 13.39 | 11.23 | 1.40 | 10.58 | 16.20 | 0.00 | 43.00 | ||
| Total | 152 | 12.96 | 10.93 | 0.89 | 11.21 | 14.71 | 0.00 | 50.00 | ||
| Education | ≤High school | 67 | 13.67 | 11.17 | 1.36 | 10.95 | 16.40 | 0.00 | 43.00 | 0.52 |
| College | 85 | 12.40 | 10.78 | 1.17 | 10.08 | 14.72 | 0.00 | 50.00 | ||
| Total | 152 | 12.96 | 10.93 | 0.89 | 11.21 | 14.71 | 0.00 | 50.00 | ||
| Income (SAR) | ≤5000 | 53 | 11.72 | 10.18 | 1.40 | 8.91 | 14.52 | 0.00 | 38.00 | 0.522 |
| 5000-10,000 | 64 | 14.41 | 11.99 | 1.50 | 11.41 | 17.40 | 0.00 | 50.00 | ||
| >10,000 | 35 | 12.20 | 9.97 | 1.69 | 8.78 | 15.62 | 0.00 | 35.00 | ||
| Total | 152 | 12.96 | 10.93 | 0.89 | 11.21 | 14.71 | 0.00 | 50.00 | ||
OHIP-14: 14-item Oral Health Impact Profile; SD: standard deviation; SE: standard error; CI: confidence interval
Physical pain (38.20%) was the most common response observed among the study participants followed by psychological disability (29.60%), with the least reported being functional limitation (5.90%).
The mean ± SD of OHIP-14 functional limitation subscale scores for 1–5, 6–10, and >10 teeth loss were found to be 0.03 ± 0.18, 0.04 ± 0.19, and 0.31 ± 0.48, respectively. When the severity of teeth loss is compared with the mean subscale OHIP-14 score, functional limitations showed statistically significant differences (P = 0.000). Functional limitation was significantly higher among participants with >10 teeth loss compared with the study subjects with 1–5 and 6–10 teeth loss. The severity of teeth loss in different categories compared with the mean social disability subscale OHIP-14 showed statistically significant differences (P = 0.044) [Table 4].
Table 4.
Mean subscale OHIP-14 scores and frequencies of “fairly often” or “very often” responses in relation to the number of missing teeth
| OHIP-14 items | Distribution of “often” or “very often” responses (%) | Mean subscale OHIP score (±SD) 1-5 | Severity of teeth loss | ||||
|---|---|---|---|---|---|---|---|
| 6-10 | >10 | P¶ | |||||
| Functional limitation | 1. Trouble pronouncing any words | 5.90% | 0.06 (±0.24) | 0.03a (±0.18) | 0.04a (±0.19 | 0.31b (±0.48) | 0.000 |
| 2. Sense of taste has worsened | |||||||
| Physical pain | 3. Had painful aching in your mouth | 38.20% | 0.47 (±0.65) | 0.36 (±0.61) | 0.50 (±0.64) | 0.77 (±0.83) | 0.116 |
| 4. Uncomfortable to eat any foods | |||||||
| Psychological discomfort | 5. Been self-conscious | 21.00% | 0.22 (±0.45) | 0.18 (±0.43) | 0.24 (±0.46) | 0.31 (±0.48) | 0.449 |
| 6. Felt tense | |||||||
| Physical disability | 7. Diet has been unsatisfactory | 16.40% | 0.20 (±0.49) | 0.13 (±0.34) | 0.24 (±0.56) | 0.31 (±0.63) | 0.523 |
| 8. Had to interrupt meals | |||||||
| Psychological disability | 9. Difficult to relax | 29.60% | 0.36 (±0.59) | 0.28 (±0.52) | 0.36 (±0.58) | 0.69 (±0.85) | 0.176 |
| 10. Been a bit embarrassed | |||||||
| Social disability | 11. Been a bit irritable with other people | 22.40% | 0.30 (±0.61) | 0.21a (±0.49) | 0.29a (±0.61) | 0.77b (±0.93) | 0.044 |
| 12. Had difficulty doing your usual jobs | |||||||
| Handicap | 13. Felt that life in general was less satisfying | 13.80% | 0.16 (±0.44) | 0.13 (±0.43) | 0.14 (±0.35) | 0.46 (±0.78) | 0.114 |
| 14. Been totally unable to function | |||||||
Significant for bold values P<0.05. OHIP-14: 14-item Oral Health Impact Profile; SD: standard deviation. Note: Different letters (a, b) in the same row indicate significant differences between groups (P<0.05), and same letter in the single row indicates no significant differences (P>0.05). ¶Kruskal–Wallis test
Comparison of the overall OHIP-14 score among different categories of tooth loss showed statistically significant differences (P = 0.005). Study participants with more than 10 teeth loss showed significantly higher overall OHIP-14 scores compared with the 6–10 and 1–5 teeth loss. While study participants with 6–10 teeth loss showed significantly higher overall mean OHIP-14 score compared with the 1–5 teeth loss [Figure 1].
Figure 1.
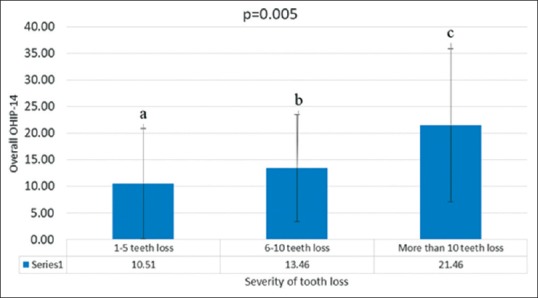
Comparison of the overall OHIP-14 score in different tooth loss categories
The overall OHIP-14 score showed a significant positive correlation (r = 0.325, P = 0.001) with tooth loss and clinical attachment loss (r = 0.346, P = 0.001) [Table 5].
Table 5.
Correlation between overall OHIP-14 score and clinical variables
| Variables | Correlation coefficient | Sig. (two-tailed) |
|---|---|---|
| Tooth loss | 0.325** | 0.001 |
| GI score | 0.027 | 0.745 |
| PI score | 0.125 | 0.125 |
| CAL | 0.346** | 0.001 |
**P<0.01. OHIP-14: 14-item Oral Health Impact Profile; GI: gingival index; PI: plaque index; CAL: Clinical attachment loss
Discussion
Studies conducted elsewhere in the past have shown an impact of tooth loss on OHRQoL.[20] However, this concept is new with few studies being published from Saudi Arabia, especially on tooth loss and OHRQoL.
The findings of this study revealed that tooth loss has a definite impact on OHRQoL of the patients. The severity of impact on OHRQoL increased with higher number of teeth loss leading to greater oral impairment. Study participants with more than 10 teeth lost showed highest OHIP-14 score indicating higher oral impairment. Tooth loss was related to the gradient of OHIP severity based on the number of teeth lost as shown in Figure 1. This result is similar to the study reported by Batista et al., in which the impact on OHRQoL was higher with loss of more than 13 teeth. Furthermore, the same study reported that tooth loss of up to 12 teeth including anterior teeth also had higher impact on OHRQoL compared with fully dentulous adults.[15] Similar findings of impaired subjective oral health were more frequently reported among individuals with fewer natural teeth.[21]
In this study, physical pain, psychological disability, psychological discomfort, social disability, and physical disability are the most common oral impacts affecting 38.2%–16.40% of the participants. Functional limitations and handicaps were the least severe impacts. This finding is in line with other reported study.[9]
While other studies have reported substantial impact of socioeconomic factors on self-perceived OHRQoL[15,22] that was not seen in this study. In this study, females perceived higher effects on OHRQoL to a greater extent compared with males.
In this study, we observed that the total OHIP-14 score was significantly higher in subjects with more than 10 teeth loss compared with 6–10 and 1–5 teeth loss. This implies that as the number of teeth loss increased, the OHIP-14 score also increased. Presence of adequate number of functional teeth has positive relationship with chewing ability of an individual. Hence any conciliation in chewing ability might have negative affect on nutritional intake, OHRQoL, and improper food habits leading to poor general health outcomes.[23]
We consider convenient sampling methodology and relatively small number of patients selected from single-university dental clinics and self-reported responses to the questionnaire are the limitations of our study.
Tooth loss significantly impacts the OHRQoL. Certain oral health awareness-related policies and camps should be organized so that people can retain their natural dentition for longer periods. This study highlights the need for more stringent primary preventive measures such oral health education and oral health promotion by the dentists to reach wider population base.
Conclusion
Within the limitations of the study, it can concluded that tooth loss has a definite negative impact on OHRQoL of dental patients. As the severity of teeth loss increased, the OHIP-14 score also amplified indicating higher oral health impairments. Functional limitations and social disability were the most affected domains of OHRQoL among the dental patients with teeth loss. Hence, dentist should be well-aware of the consequences of teeth loss while treating the patients.
Financial support and sponsorship
Nil.
Conflict of interest
There is no conflict of interest.
References
- 1.Atieh M. Tooth loss among Saudi adolescents: Social and behavioural risk factors. Int Dent J. 2008;58:103–8. doi: 10.1111/j.1875-595x.2008.tb00184.x. [DOI] [PubMed] [Google Scholar]
- 2.Petersen PE, Yamamoto T. Improving the oral health of older people: The approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2005;33:81–92. doi: 10.1111/j.1600-0528.2004.00219.x. [DOI] [PubMed] [Google Scholar]
- 3.Al Shammery A, El Backly M, Guile EE. Permanent tooth loss among adults and children in Saudi Arabia. Community Dent Health. 1998;15:277–80. [PubMed] [Google Scholar]
- 4.Al-Shahrani N, Al-Amri A, Hegazi F, Al-Rowis K, Al-Madani A, Hassan KS. The prevalence of premature loss of primary teeth and its impact on malocclusion in the Eastern Province of Saudi Arabia. Acta Odontol Scand. 2015;73:544–9. doi: 10.3109/00016357.2014.939709. [DOI] [PubMed] [Google Scholar]
- 5.Al-Harbi F, El Tantawi M. Normative prosthodontic care need: Does it impact the daily life of young Saudis with high level of oral diseases? A cross sectional study. BMC Oral Health. 2017;17:128. doi: 10.1186/s12903-017-0418-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Almutlaqah MA, Baseer MA, Ingle NA, Assery MK, Al Khadhari MA. Factors affecting access to oral health care among adults in Abha City, Saudi Arabia. J Int Soc Prev Community Dent. 2018;8:431–8. doi: 10.4103/jispcd.JISPCD_205_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alshammari MS, Alshammari AS, Siddiqui AA, Mirza AJ, Mian RI. Patients' knowledge and perceived barriers toward replacement of missing teeth among respondents of Hail City, Kingdom of Saudi Arabia. J Contemp Dent Pract. 2018;19:86–9. doi: 10.5005/jp-journals-10024-2216. [DOI] [PubMed] [Google Scholar]
- 8.John MT, LeResche L, Koepsell TD, Hujoel P, Miglioretti DL, Micheelis W. Oral health-related quality of life in Germany. Eur J Oral Sci. 2003;111:483–91. doi: 10.1111/j.0909-8836.2003.00079.x. [DOI] [PubMed] [Google Scholar]
- 9.Lalić M, Melih I, Aleksić E, Gajić M, Kalevski K, Ćuković A. Oral health related quality of life and dental status of adult patients. Balk J Dent Med. 2017;21:93–99. [Google Scholar]
- 10.Locker D, Allen F. What do measures of “oral health-related quality of life” measure? Community Dent Oral Epidemiol. 2007;35:401–11. doi: 10.1111/j.1600-0528.2007.00418.x. [DOI] [PubMed] [Google Scholar]
- 11.Locker D, Quiñonez C. To what extent do oral disorders compromise the quality of life? Community Dent Oral Epidemiol. 2011;39:3–11. doi: 10.1111/j.1600-0528.2010.00597.x. [DOI] [PubMed] [Google Scholar]
- 12.Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 13.Gerritsen AE, Allen PF, Witter DJ, Bronkhorst EM, Creugers NHJ. Tooth loss and oral health-related quality of life: A systematic review and meta-analysis. Health Qual Life Outcomes. 2010;5:126. doi: 10.1186/1477-7525-8-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haag DG, Peres KG, Balasubramanian M, Brennan DS. Oral conditions and health-related quality of life: A Systematic review. J Dent Res. 2017;96:864–74. doi: 10.1177/0022034517709737. [DOI] [PubMed] [Google Scholar]
- 15.Batista MJ, Lawrence HP, de Sousa M da LR. Impact of tooth loss related to number and position on oral health quality of life among adults. Health Qual Life Outcomes. 2014;30:165. doi: 10.1186/s12955-014-0165-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Masood M, Newton T, Bakri NN, Khalid T, Masood Y. The relationship between oral health and oral health related quality of life among elderly people in United Kingdom. J Dent. 2017;56:78–83. doi: 10.1016/j.jdent.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 17.Pakpour AH, Lin C-Y, Kumar S, Fridlund B, Jansson H. Predictors of oral health-related quality of life in Iranian adolescents: A prospective study. J Investig Clin Dent. 2017;00:e12264. doi: 10.1111/jicd.12264. [DOI] [PubMed] [Google Scholar]
- 18.Tan H, Peres KG, Peres MA. Retention of teeth and oral health-related quality of life. J Dent Res. 2016;95:1350–7. doi: 10.1177/0022034516657992. [DOI] [PubMed] [Google Scholar]
- 19.Al Habashneh R, Khader YS, Salameh S. Use of the Arabic version of oral health impact profile-14 to evaluate the impact of periodontal disease on oral health-related quality of life among Jordanian adults. J Oral Sci. 2012;54:113–20. doi: 10.2334/josnusd.54.113. [DOI] [PubMed] [Google Scholar]
- 20.Echeverria MS, Wünsch IS, Langlois CO, Cascaes AM, Ribeiro Silva AE. Oral health-related quality of life in older adults-Longitudinal study. Gerodontology. 2019;36:118–24. doi: 10.1111/ger.12387. [DOI] [PubMed] [Google Scholar]
- 21.Lahti S, Suominen-Taipale L, Hausen H. Oral health impacts among adults in Finland: Competing effects of age, number of teeth, and removable dentures. Eur J Oral Sci. 2008;116:260–6. doi: 10.1111/j.1600-0722.2008.00540.x. [DOI] [PubMed] [Google Scholar]
- 22.Adams C, Slack-Smith LM, Larson A, O'Grady MJ. Edentulism and associated factors in people 60 years and over from urban, rural and remote Western Australia. Aust Dent J. 2003;48:10–4. doi: 10.1111/j.1834-7819.2003.tb00002.x. [DOI] [PubMed] [Google Scholar]
- 23.Brennan DS, Spencer AJ, Roberts-Thomson KF. Tooth loss, chewing ability and quality of life. Qual Life Res Int J Qual Life Asp Treat Care Rehabil. 2008;17:227–35. doi: 10.1007/s11136-007-9293-2. [DOI] [PubMed] [Google Scholar]


