Abstract
Background:
The referral system plays a crucial role in antenatal care and childbearing by providing access to emergency obstetric care. Excess referral from primary care and bypassing secondary levels of care leads to overcrowding of high risk and normal mothers in tertiary centers. Hence, this study aims to assess the gaps in the referral of patients with obstetric emergency from primary care to tertiary care.
Methodology:
In this hospital-based descriptive study, all obstetric patients referred to the Obstetric emergency facility and admitted in postnatal wards during the study period were included. They were interviewed using a pretested questionnaire. Data entry was performed using EpiData version 3.1 and analysis was done using SPSS version 22 software.
Results:
Of the 505 eligible women who attended the facility, 286 (56%) were referred from other institutions, while 44% were self-referred. Among those referred, one-third were from tertiary level facility and 40% from primary care facility. More than half of the referral was through verbal communication to the patient (60%); only one-third had referral slips. Around 40.4% chose bus and private vehicles (37.6%) as their means of transport; only around 10% traveled in 108 ambulances.
Conclusions:
Measures to improve the capacity building at primary setting, hierarchy of referral, quality of documentation, and emergency transport mechanism for obstetric patients are vital. The deficits identified in the existing referral system will be useful to give feedback to the health systems of the neighboring regions on emergency obstetrics referrals and to propose referral guidelines.
Keywords: Emergencies, obstetric delivery, primary care, referral and consultation, tertiary care
Introduction
The referral system is a core factor in health care delivery systems. It plays a crucial role in antenatal care and childbearing by providing access to emergency obstetric care, antenatal and delivery care in primary level facilities.[1] The term referral is used to indicate the recommendation of a health care provider at one level of the health system, having limited resources (medications, equipment, skilled professional) to manage a clinical condition for the assistance of an improved resourced facility which is of similar or higher level to assist in or take over the management of patient.[2] Usually, referral occurs in upward movements, i.e. persons are referred to higher institutions.[3] In an obstetric emergency, referral system is necessary due to the randomness of pregnancy complications and potentiality of its rapid progression to make life vulnerable.[4]
Pregnancy and parturation can cause risks to mother and child. Referral service should be done at the appropriate time and with rapidity in order to avoid such related risk and unfavorable outcomes. Referrals can lead to favorable outcomes.[5] Referrals in pregnancy and childbirth can be categorized depending on their pathway (institutional or self-referral), timing (antenatal, during labor or postnatal), and urgency (elective or emergency referral).[1] According to the concept of referral chain model proposed by Jahn et al., referral system composes of three main elements: sender, transport, and receiver.[1] Other elements of the referral system include counseling the pregnant mother and her relatives, organizing transport, escorting women, aiding admission, and supporting inpatient care.[6]
WHO guideline (revised in 2017) describes the management of obstetric complications at the district level with respect to the period of gestation.[7] However, the use of these guidelines at different levels of facilities, and referral systems, in low resource countries are not well understood. Obstetric care provided by primary health care system in India is not standardized.[8] Even basic conditions that can be managed within the existing system of primary health care, and closer to the community are unnecessarily referred to the Emergency Medical Services (EMS) of tertiary centers. In addition, secondary level of care is bypassed when people prefer specialist services for seemingly normal conditions, thereby increasing attendance at tertiary centers. Private hospitals shift high-risk pregnancies and women in labor in order to avoid poor outcomes. Apart from the huge caseloads, the quality of referrals in terms of timing and data documentation is very poor, thus limiting the provision of quality care to the patients. Due to such gaps in the referral system, EMS department at tertiary centers is overcrowded with both high risk and normal deliveries. This dilutes the quality of care which would otherwise be provided for more critical conditions. Better organization and planning of referrals to EMS can result in improved outcomes in an inexpensive fashion.
Even though active referral services constitutes an important component of effective Emergency Obstetric and Neonatal Care (EmONC), very few studies have examined the referral functions, especially from the perspective of a tertiary care facility (receiver hospital). Hence, this study aims to assess the gaps in the referral of patients from primary care arriving at the obstetric EMS of a tertiary hospital.
Methodology
Study design and setting: A hospital-based descriptive study was conducted in the Women and Children's hospital of a tertiary care hospital in Puducherry, South India. The Department of Obstetrics caters to a large population from a wide area bordering Vellore, Cuddalore, Villupuram and Tiruvannamalai, Ariyalur, Nagapattinam and Krishnagiri districts of Tamilnadu. On an average, 1,20,000 out-patients and 20,000 in-patients are treated every year. The average number of deliveries and major surgeries per year are over 13000 and 1200, respectively. Monthly attendance at the EMS Department of Obstetrics is 1500 patients on an average.[9] Data collection and analysis was done from January to February 2015.
Study population: All obstetric patients referred to the EMS of Department of Obstetrics and Gynecology for emergency obstetric care and admitted in postnatal wards during the study period were included. This also included women reporting to JIPMER on their own without referral by any health facility (self-referred). Obstetric patients who received antenatal care (minimum 3 visits) at JIPMER and those below the age of 18 years were excluded.
Study tool: A structured questionnaire was developed based on three main elements of a referral chain-sender, transport, and receiver. The questionnaire was translated into the local language and back-translated to English. It was validated by pretesting it among a subset of the sample and modifications were done accordingly. The study variables were sectioned into sociodemographic details (age, education, occupation, per capita income, address, and source of antenatal care), clinical details (parity, period of gestation, presenting condition, and reason for referral), referring facility details (level of care), and transport characteristics (mode of transport, time to arrange transport, and costs involved). If the patient accessed the facility on her own, then reasons for self-referral was obtained.
Study procedure: The study was approved by the Institute Scientific and Ethics committee was obtained on 11-12-2014. Pilot study was done to test the feasibility and to assess coverage of the study population. Information of patients who attend the EMS during the study period was collected from the EMS register. Patient details such as name, hospital number, and time of arrival were collected from the register and they were traced in the postnatal wards. After obtaining informed consent, data was collected using the pretested questionnaire. Reasons for referral were noted from the referral slip or notebook available with the patients. In case of multiple reasons, the most important risk indications for referral were used for classification. The reasons were classified as obstetric condition, medical condition, fetal condition, and others.
Statistical analysis: Data entry was performed using EpiData version 3.1 and analysis was done using SPSS version 22 software. All the variables in the study were summarized in frequencies and proportions. Age was expressed in mean (standard deviation); time taken to arrange transport and to reach facility was expressed in median with interquartile range (as the data was skewed). Chi-square test was used to compare proportions between the different groups.
Operational definitions
Self-referral: It indicates approach of the patient to a health care facility with or without perceiving risk and without the suggestion of any health care provider.
Primary level of care: Primary level indicates the first level of connection between the patients with the health delivery system. In this study, Sub Center (SC) and Primary Health Centers (PHC) are included under primary level of care.
Secondary level of care: Secondary level of care denotes the higher grade hospitals where the service of specialists is provided, e.g. Community Health Center (CHC).
Tertiary level of care: Tertiary level of care indicates specialized centers with advanced technologies and highly specialized practitioners. In this study, Government hospitals, Government Taluk hospitals, and Medical colleges come under this level.
Private care: Private care includes the hospitals and clinics which come under the private sector.
Results
During the study period, a total of 1742 women presented to EMS, of which 970 women received antenatal care from the same hospital; 237 women were asked to review in OPD as their condition did not warrant emergency admissions. Of the remaining 505 women who had emergency admissions in JIPMER wards, 286 women were referred from other institutions (56%), while remaining 44% (n = 219) attended EMS on their own. Figure 1
Figure 1.
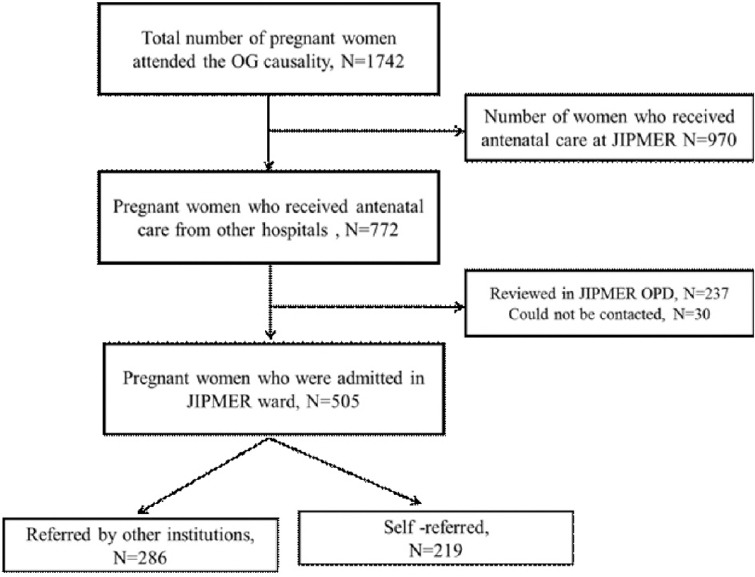
Flow chart showing the number of study subjects during the study period
Sociodemographic profile: Mean age of the study participants was 24.6 years (±3.6). Almost half of the subjects were in age group of 21–25 years. Majority (96.8%) of the women were unemployed. Most of the participants from rural areas (93.3%). [Table 1] Majority (96.4%) were from surrounding districts of Tamil Nadu namely, Villupuram (51.5%), Tiruvannamalai (20%) and Cuddalore (18.8%), and 6% were from Puducherry. Based on nearest health facility, half of the patients had access to primary level of care (48.3%), while 19% had CHCs (n = 95) and 15% had government hospitals close to their houses. All the subjects had antenatal care of minimum three visits and had antenatal follow-up slips or notebooks with records of their details. One-third patients (n = 159, 31.5%) received antenatal care in private sector. Among subjects receiving care from government sector, 55% received care from primary level facility, while one-fourth received care from secondary (23%).
Table 1.
Sociodemographic details of the study population (n=505)
| Characteristics | Frequency (n) | Percentage |
|---|---|---|
| Age | ||
| Up to 20 years | 70 | 13.9 |
| 21-25 years | 253 | 50.1 |
| 26-30 years | 159 | 31.4 |
| 31-35 years | 18 | 3.6 |
| 36-40 years | 4 | 0.8 |
| Above 40 years | 1 | 0.2 |
| Educational status | ||
| Illiterate | 69 | 13.7 |
| Primary school | 27 | 5.3 |
| Middle school | 86 | 17.0 |
| High school | 122 | 24.2 |
| Higher secondary | 118 | 23.4 |
| Graduate/Diploma | 62 | 12.2 |
| Postgraduate | 21 | 4.2 |
| Occupation | ||
| Employed | 16 | 3.2 |
| Unemployed | 489 | 96.8 |
| Religion | ||
| Hindu | 467 | 92.5 |
| Christian | 16 | 3.1 |
| Muslim | 22 | 4.4 |
| Socioeconomic status* | ||
| Class 4 (773-1546) | 26 | 5.1 |
| Class 3 (1547-2577) | 262 | 51.9 |
| Class 2 (2578-5155) | 148 | 29.3 |
| Class 1 (above 5156) | 69 | 13.7 |
| Residence | ||
| Rural | 471 | 93.3 |
| Urban | 34 | 6.7 |
| Total | 505 | 100 |
*Based on Prasad’s classification of Socioeconomic status 2014 (21)
Clinical profile: Two-thirds of the patients were primipara (66.5%) and around 83% were term gestation. Most of the patients presented during first stage of labor (88.3%) and around 11% presented without any symptoms of labor. [Table 2] Most of the patients had obstetric indications (76%), followed by medical (12.8%) and fetal indications (8.4%) as the reason for referral. [Table 3] Condition of risk was communicated to the patient and the family members (98.6%) and 97% were examined before referring.
Table 2.
Obstetric details of the study subjects at the time of presentation (n=505)
| Obstetric characteristics | Frequency (n) | Percentage |
|---|---|---|
| Parity | ||
| Primipara | 336 | 66.5 |
| Multipara | 169 | 33.5 |
| Presenting Condition | ||
| Without labor pain | 54 | 10.9 |
| First stage | 437 | 88.3 |
| Third stage | 4 | 0.8 |
| Period of gestation | ||
| Preterm (<37 weeks) | 62 | 12.3 |
| Term (37-40 weeks) | 420 | 83.1 |
| Postdate (>40 weeks) | 23 | 4.6 |
| Total | 505 | 100 |
Table 3.
Reasons for institutional referral by health care provider (n=286)
| Reasons for referral | Frequency | Percentage | Cumulative % |
|---|---|---|---|
| OBSTETRIC CONDITIONS | |||
| Premature rupture of membranes (PROM) | 36 | 12.6 | 76.0 |
| Oligohydraminos | 25 | 8.7 | |
| Pregnancy-induced hypertension (PIH) | 21 | 7.3 | |
| Post dates | 20 | 7.0 | |
| Previous LSCS | 19 | 6.6 | |
| Cervix not dilated | 15 | 5.2 | |
| Cephalo-pelvic disproportion (CPD) | 14 | 4.9 | |
| Precious pregnancy | 13 | 4.5 | |
| Preterm labor | 13 | 4.5 | |
| Malpresentation | 13 | 4.5 | |
| Placenta previa | 10 | 3.5 | |
| Multiple pregnancy | 9 | 3.2 | |
| Gestational diabetes with hypertension | 5 | 1.7 | |
| Non expulsion of placenta | 3 | 1.0 | |
| Eclampsia | 1 | 0.4 | |
| Postpartum hemorrhage | 1 | 0.4 | |
| MEDICAL CONDITIONS | |||
| Severe anaemia | 15 | 5.2 | 12.8 |
| Rh incompatibility | 7 | 2.5 | |
| Seizure history | 3 | 1.1 | |
| Cardiac disease/heart surgery of mother | 3 | 1.1 | |
| High-grade fever, cough | 3 | 1.1 | |
| Jaundice | 2 | 0.7 | |
| Thyroid disorders | 2 | 0.7 | |
| HTN with nephrosclerosis | 1 | 0.4 | |
| FETAL CONDITIONS | |||
| Intrauterine death (IUD) | 9 | 3.1 | 8.4 |
| Fetal distress | 4 | 1.4 | |
| Intrauterine growth retardation | 4 | 1.4 | |
| Fetal congenital diseases | 3 | 1.1 | |
| Meconium aspiration | 2 | 0.7 | |
| Macrosomia | 2 | 0.7 | |
| MISCELLANEOUS | 8 | 2.8 | 2.8 |
| Total | 286 | 100 | 100 |
Referring facility: Among the 286 patients who were referred, around 30% were from tertiary level facility, 40% from primary level facility and 17% from private hospitals. Most of the referrals were done by the doctor/Medical officer.
Referral communication: In this study, 171 subjects were referred through verbal communication; among 115 patients with some form of written communication, 77% had referral slips which varied from printed referral slips, prescription form, to a piece of paper and 23% in their antenatal follow-up notebooks. Most of the referral communication described reasons for referral (95.7%), signature of the medical officer (89.6%), the date of referral (88.7%), and about the patient's history (74.8%). Only a few requests contained patient identification details (12.2%), treatment given (13.9%), and clinical judgment of the care provider (21.7%).
Self-referrals: On comparing the characteristics of self-referred patients and institutional referrals, it was found that women from high socioeconomic status and who sought antenatal care from private facilities were significantly higher among the self-referred group. The most important reason for self-referrals was “to have normal delivery” (39%) and “for better care” (19%). Around 13% patients preferred to come back to the same hospital for their subsequent delivery, as they were satisfied with their previous delivery, and also due to their high-risk status in their current pregnancy. Financial problems (12%) and advice of family members (7%) were other reasons. Around 10% of patients sought care at this facility due to self-perceived risk of current pregnancy such as bleeding, past dates, high blood pressure, low fluid, breech position, etc., or fetal death or operative delivery during the previous pregnancy. Around 7% patients sought JIPMER for quality care on advice of family members or neighbors.
Transport characteristics: Most of the patients (40.4%) chose bus and private vehicles like car or taxi (37.6%) as their means of transport. Only 10% of the study population traveled in 108 ambulances, while a few patients arrived in private ambulances (2.6%). Other modes of conveyance to the hospital included auto, own vehicles, etc., While comparing each district with the mode of transport, it was found that in Cuddalore and Villupuram, around 20% and 10% patients, respectively, utilized 108 ambulances. Among the institutional referrals, around 20% patients arrived in ambulances (15% in 108 service and 4.2% in private ambulances). There was hardly any time lag to board a bus and they traveled on average 3 h to reach JIPMER. Time to arrange 108 ambulance was about 10 min and 15 min in case of private ambulance. There were no costs incurred on 108 Ambulance facilities and no bribery was involved. Cost involved in arranging transportation was highest in case of private ambulance, followed by private vehicles like cars and taxis based on kilometers traveled. [Table 4]
Table 4.
Transport characteristics among the study population (n=505)
| Transport vehicle | n (%) | Average cost (in INR) | Time taken to arrange transport, Median (IQR)* | Time taken to reach facility, Median (IQR) |
|---|---|---|---|---|
| Bus | 204 (40.4) | 285 | Immediately | 3 h (3-3.5 h) |
| Private vehicle | 190 (37.6) | 2000 | 10 min (0-30 min) | 2.5 h (2-3 h) |
| 108 Ambulance service | 47 (9.3) | 0 | 10 min (0-10 min) | 48 min (30 min-1.5 h.) |
| Private ambulance | 13 (2.6) | 2800 | 15 min (10-30 min) | 2 h (1.25 h-2.5 h) |
| Other modes | 51 (10.1) | 0 | Immediately (6-30 mins) | 30 min (30 min-1.25 h) |
*IQR is Interquartile range
Majority (92.3%) were accompanied by their family members. Only 4% of study subjects were escorted by ambulance staff and 3.8% by nursing assistant. However, among the 47 subjects who arrived by 108 ambulance service more than three-fourths were escorted by trained staff (40% by ambulance staff and 38% by Nursing assistant). In case of private ambulance service, almost all were escorted by family members. About 2.4% patients (n = 8) approached an intermediate care facility for labor pains.
Discussion
In this study, most of the patients were aged between 20 and 30 years, similar to other studies as it is the prime reproductive age group.[10] Majority of the patients were educated up to higher secondary, in contrast to other studies[11] mainly because of the high literacy rates in Puducherry (85.8%) and Tamil Nadu (80%) compared to Indian average (74%).[12] In this study, majority of patients (65.6%) come under low socioeconomic status similar to a study done in a tertiary facility.[11] The study participants were mainly from surrounding districts, with average travel time of 45 min to 2 h. This institution serves as referral facility for many of these Government and Taluk hospitals in these districts. Only 6% of the study subjects came from Puducherry because of a large network of health facilities, both Government and Private.
In this study, 38%, 15%, 30%, and 17% referrals were from primary, secondary, tertiary, and private facilities, respectively. In contrast, Chaturvedi et al. found that 62% women in tertiary emergency facility were referred from secondary level and 26% from primary level.[3] The altered pattern of higher referrals from primary facilities in this study could be due to the proximity of a tertiary care facility and preferential referring, thus bypassing the traditional referral hierarchy. Very few studies have dealt with gap analysis in the referral system and reasons for overcrowding, which pose barriers to quality care. Matteson et al. found that one-third of patients approached emergency facility due to self-perceived risk as against referral by doctor in 42%.[13] Similarly, Kruk et al. in Tanzania observed the tendency of patients to bypass the adjacent hospital and approach other facilities. This resulted in higher expenditure for the patients as well.[14] When referral pathway (from primary to secondary to tertiary facility) is not followed, it may cause overcrowding in the tertiary centers and reduction in quality of care. Significant determinants of self-referral were high socioeconomic status and source of antenatal care being at private hospitals. However, in other studies, it was either due to poor awareness[11] or poor socioeconomic status.[15]
In this study, most of the patients had obstetric conditions (76.3%), followed by medical (12.8%) and fetal conditions (8.5%) as the reason for referral. These findings were comparable to other studies.[3,5,11,16,17] Most of the referrals were by Medical officers in comparison with another study which showed that untrained dais (34.7%) and female health workers (27.3%) were the other sources of referral.[11] Almost 98% were examined before referring to this study setting. This was comparable to another study, where patients either admitted (60%) or examined before referral (38%).[3] However, documentation at the time of examination is available only in three-fourths of them. If this documentation is strengthened, further management protocols at the receiving facility can be facilitated.
More than half of the referral was mainly through verbal communication (60%). One-third of the total subjects (31%) had referral slips and 9% cases referral request was done in the antenatal follow-up notebooks. This is low when compared to other studies.[3,16] Non-availability of standardized referral documents and poor documentation are important referral challenges. Another finding in this study was the poor referral documentation from private hospitals (only one-third had written referrals).
Three-fourths of the available referral slips mentioned the reasons for referral, history of the patient, signature of medical officer, date of referral, and examination done during referral. However, only 45.2% had name of referring facility while others just mentioned as “Referring to higher institution.” An ideal referral slip should contain name and address of the patient, history, investigations done with date and report, examination, name of referring facility, reason for referral, brief note on treatment given, name of medical officer, date of referral, phone number of referring facility, and facility referred.[2] Most of the referral slips did not have any details on assessment of risk, clinical judgment, and investigations done which would be very useful to the referral facility for prompt treatment.
Despite a good network of emergency transport facility in the area, only around 10% of the study population traveled in 108 ambulances. This is similar to other studies that showed usage of private transport and additional expenditure due to scarcity of transport facilities in referring facility.[16,18] As family members can only provide moral support to the patient in such emergency cases, there is a need for trained personnel in such referral transport.[16]
A study from two states of India shows that there is sub-optimal knowledge about screening of common high-risk conditions and early complications of pregnancy, leading unnecessary referral.[8] The main gaps identified in referral include bypassing the secondary and tertiary facilities, referral documentation, transport system, and notification to the receiving facility. Measures to improve the quality of referral documentation are vital, especially from private facilities. Proper referral reporting system from health facilities to district hospitals and state should be maintained. Capacity building of health care providers on referral protocols, documentation, and referral communication can improve the current status. Awareness on availability of free transport system in Tamil Nadu needs to be created at all levels of care. Community awareness needs to be created regarding availability of health care facility during their antenatal care and discourage self-referrals due to “want of good care,” “for normal delivery” or “perceived risk.” Further, feedback from the receiving facility to the initiating facility will enable health system strengthening and improve health care delivery.
Conclusion
In this study, 40% of the antenatal cases were referred from primary care setting followed by private setup and secondary level care. Capacity building of the medical officers and ANM in primary care is very much needed to improve deliveries in PHCs. Periodic training program may be arranged for medical officers and ANM at nearest tertiary care institute. Measures to improve the hierarchy of referral and quality of referral documentation and emergency transport mechanism for obstetric patients are vital. The deficits identified in the existing referral system will be useful to give feedback to the health systems of the neighboring regions on emergency obstetrics referrals and to propose referral guidelines.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Brouwere VD, Lerberghe W van. Safe motherhood strategies : a review of the evidence. 2001. Cited 2015 Mar 30. Available from: http://filesgivewellorg/files/DWDA%202009/Interventions/Maternal%20Mortality/SafeMotherhoodStrategiespdf .
- 2.Referral Systems-A summary of key processes to guide health services managers. WHO; cited 2015 Jul 4. Available from: www.who.int/management/Referralnotes.doc . [Google Scholar]
- 3.Chaturvedi S, Randive B, Diwan V, De Costa A. Quality of obstetric referral services in India's JSY cash transfer programme for institutional births: A study from Madhya Pradesh province. PLoS One. 2014;9:e96773. doi: 10.1371/journal.pone.0096773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hussein J, Kanguru L, Astin M, Munjanja S. The Effectiveness of Emergency Obstetric Referral Interventions in Developing Country Settings: A Systematic Review. [Last cited on 2019 Nov 28];PLoS Med [Internet] 2012 9:7. doi: 10.1371/journal.pmed.1001264. Available from: https://wwwncbinlmnihgov/pmc/articles/PMC3393680/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel HC, Singh BB, Moitra M, Kantharia SL. Obstetric referrals: Scenario at a primary health centre in Gujarat. NJCM. 2012;4:711–4. [Google Scholar]
- 6.Iyengar K, Iyengar SD. Emergency obstetric care and referral: Experience of two midwife-led health centres in rural Rajasthan, India. Reprod Health Matters. 2009;17:9–20. doi: 10.1016/S0968-8080(09)33459-X. [DOI] [PubMed] [Google Scholar]
- 7.WHO UNICEF. UNFPA. Managing Complications in Pregnancy and Childbirth: A Guide for Midwives and Doctors. 2nd ed. Geneva: World Health Organization; 2017. [Google Scholar]
- 8.Singh S, Doyle P, Campbell OMR, Murthy GVS. Management and referral for high-risk conditions and complications during the antenatal period: Knowledge, practice and attitude survey of providers in rural public healthcare in two states of India. Reprod Health. 2019;16:100. doi: 10.1186/s12978-019-0765-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hospital Statistics | JIPMER. Cited 2015 Mar 28. Available from: http://jipmer.edu.in/departments/ancillary-services/mrd/hospital-statistics/
- 10.Fournier P. Improved access to comprehensive emergency obstetric care and its effect on institutional marternal mortality in rural Mali. Bull World Health Organ. 2009;87:30–8. doi: 10.2471/BLT.07.047076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Najam R, Gupta S, Chowdhury H. Pattern of obstetrical emergencies and fetal outcomes in a tertiary care center. Acta Medica Int. 2015;2:105–10. [Google Scholar]
- 12.Census of India 2011, Figure at a glance 2011- Puducherry, Ministry of Home affairs, office of the Registrar General and Census commissioner, New Delhi. India. 2011. cited 2015 Mar 30. Available from: http://www.census2011.co.in/literacy.php .
- 13.Matteson KA, Weitzen SH, Lafontaine D, Phipps MG. Accessing care: Use of a specialized women's emergency care facility for nonemergent problems. J Womens Health. 2002;2008(17):269–77. doi: 10.1089/jwh.2006.0292. [DOI] [PubMed] [Google Scholar]
- 14.Kruk ME, Mbaruku G, McCord CW, Moran M, Rockers PC, Galea S. Bypassing primary care facilities for childbirth: A population-based study in rural Tanzania. Health Policy Plan. 2009;24:279–88. doi: 10.1093/heapol/czp011. [DOI] [PubMed] [Google Scholar]
- 15.Murray SF, Davies S, Phiri RK, Ahmed Y. Tools for monitoring the effectiveness of district maternity referral systems. Health Policy Plan. 2001;16:353–61. doi: 10.1093/heapol/16.4.353. [DOI] [PubMed] [Google Scholar]
- 16.Afari H, Hirschhorn LR, Michaelis A, Barker P, Sodzi-Tettey S. Quality improvement in emergency obstetric referrals: Qualitative study of provider perspectives in Assin North district, Ghana. BMJ Open. 2014;4:e005052. doi: 10.1136/bmjopen-2014-005052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prinja S, Jeet G, Kaur M, Aggarwal AK, Manchanda N, Kumar R, et al. Impact of referral transport system on institutional deliveries in Haryana, India. Indian J Med Res. 2014;139:883. [PMC free article] [PubMed] [Google Scholar]
- 18.Gupta S, Naithani U, Doshi V, Bhargava V, Vijay BS. Obstetric critical care: A prospective analysis of clinical characteristics, predictability, and fetomaternal outcome in a new dedicated obstetric intensive care unit. Indian J Anaesth. 2011;55:146–53. doi: 10.4103/0019-5049.79895. [DOI] [PMC free article] [PubMed] [Google Scholar]


