Abstract
The abfraction theory states that under the action of the occlusal forces non-axially transmitted, the flexion of the tooth occurs in the cervical area, which initially leads to the appearance of cracks in the enamel and dentin, followed by the destruction of the dental structure. These lesions allow bacterial plaque retention, lead to dental hypersensitivity and can affect the vitality of the dental pulp. Thus, the study included 102 participants, of both sexes, 54% representing the male gender (55 subjects) and 46% the female gender (47 subjects), aged between 20 and 80, from the urban area 76% (77 subjects) and rural 24% (25 subjects), who came to the Dental Medicine office, between August 2018 and August 2019, representing 57.3%, of the total number of patients treated during the aforementioned period. They have been described the acid and abrasive processes involved in the generation of these lesions,and special attention was paid to the role of mechanical stress occurring at the occlusal level, due to the transmission of forces outside the dental axis.
Keywords: Cervical lesions, abfraction, dental abrasion, occlusal trauma
Introduction
The abfraction represents the pathological loss of the dental tissue structure caused by para-axial biomechanical forces, resulting in the tooth enamel, dentine and tooth pulp being distanced from the place of force application [1].
Specialized studies [2,3,4] indicate, as etiological factors for abfraction also: abrasion, erosion, corrosion or combinations thereof.
Abfraction represents a type of cervical non-carious lesion, charaterized by the loss of dental tissues with various clinical aspects.
Cervical wear can be accompanied by dental abrassion and erossion due to interaction of chemical, biological and behaviour factors.
The clinical aspect can vary based on the type and severity of the involved etiologic factors.
Special attention was paid to mechanical stress at the occlusal level due to the action of the forces transmitted outside of the dental axis.
Abfraction lessions can appear accompanied by pathological wear of the tooth as a consequence of the interaction of chemical, biological and behaviour factors [5].
The location of the abfraction lesions according to some authors [6] is mainly in the cervical area of the teeth, as this region is the most vulnerable part of the tooth. In this area the enamel has a lower quality with a lower protein and mineral content than the other dental areas.
Grippo suggested bruxism as a main cause of these lesions and described five categories of abfraction injuries: cracks, horizontal streaks, lesions in the form of a plate located at the enamel level, crescent-shaped lesions, depression on the tip of the cusp at the premolars and molars.
Depending on the damage to the dental tissue, the abfraction lesions are grouped into three types:
I.lesions present only at the enamel level;
II.enamel and dentin lesions;
III.lessions that have progressed to the level of the dental pulp.
Due to the fact that the destruction of the hard dental structures (enamel, dentine, cement) is progressive, the soft tissues of the tooth (dental pulp) can also be affected with the appearance of dental hypersensitivity.
Objectives
The purpose of this study was to analyze and highlight the different clinical aspects of the abfraction lesions, based on certain criteria of division of the studied group.
Material and Method
The study included 102 participants, of both sexes, 54% representing the male gender (55 subjects) and 46% the female gender (47 subjects), aged between 20 and 80, from the urban area 76% (77 subjects) and rural 24% (25 subjects), who came to the Dental Medicine office, between August 2018 and August 2019, representing 57.3%, of the total number of patients treated (Table 1).
Table 1.
Questionnaire regarding oral cavity hygiene and parafunctions.
|
NO. |
QUESTIONS |
ANSWER |
|
1 |
How many times per day do you perform dental brushing? |
|
|
2 |
How long does one dental brushing session last? |
|
|
3 |
What type of toothbrush do you use? (e.g. with whitening effect) |
|
|
4 |
Do you use abrasive toothpaste? |
|
|
5 |
What brushing technique do you use? (Describe how you brush your teeth) |
|
|
6 |
Do you use secondary means of oral cavity hygiene? (e.g. dental floss, mouthwash) |
|
|
7 |
Do you crack your jaws during your day or night? |
|
The analysis of the different clinical aspects of the abfraction lesions was based on the use of certain criteria of division, namely: oral cavity hygiene, type of tooth affected, age, sex, environment of origin, degree of damage of dental structures in occlusal trauma, distribution of the dental elements affected by cervical lesions.
After obtaining the informed consent of the patients, the condition of the dentition, the oral hygiene, the number of teeth and their mobility, the oral symptoms of parafunction were evaluated and analyzed.
After the clinical and paraclinical examination, the observation charts were drawn up, photographies were taken and the patients were being diagnosed with changes of hard dental structure located in the cervical area.
According to the objectives pursued, the criteria based on which the patients were included in this study were the following.
The criteria for inclusion in the study: age over 20 years old; the presence of structural changes of the teeth at cervical level; the possibility to come to the dental medicine office as many times as necessary; the health state to allow the dental treatments to be carried out.
The exclusion criteria: under 18 years old; presence of psychiatric disorders; lack of availability for repeated visits to the dental medicine office.
We proceeded to question the patients in order to obtain data on how they perform the oral cavity hygiene and to verify its accomplishment with the help of bacterial plaque detectors.
The patients, part of the study, have been given a questionnaire to obtain data about their brushing technique, frequency, duration and intensity of teeth brushing.
The aim was to establish how these, associated with the parafunctions, contribute to the production of abfraction injuries.
The way of hygiene of the oral cavities and the verification of its accomplishment was carried out with the help of bacterial plaque detectors.
These were in the form of sponge impregnated in solution dye, used by pressing on the faces of the teeth near the incisal edge or face occlusal, diffusing through capillary close to the gingival margin.
After the coloring of the bacterial plate, the dental surfaces with plaque were noted and plate index O’Leary was established as a percentage, dividing the number of surfaces by plate at the total number of surfaces examinated by 100.
Interpretation of values: IP<10-15% dental hygiene is good; 10-15%<IP<20-25% dental hygiene is satisfactory; 20-25%<IP<40% dental hygiene is deficient; IP >40% dental hygiene is a problem for the patient.
The oral and dental health status was evaluated and analyzed, the number of teeth affected by cervical lesions was determined by clinical examination on all surfaces, and the depth of the cervical defect was measured using the periodontal probe.
Wear surfaces generated by the parafunctions were detected.
Each patient was instructed to perform the radiological-orthopantomogram examination.
The study was approved by the University Ethics and Deontology and Scientific Commission of the University of Medicine and Pharmacy of Craiova (no.70/15.06.2018).
Results
The abfraction lesions detected showed different forms, affecting the premolars in a greater number compared to the other teeth.
Following the anamnesis, regarding the dental hygiene, it was established: 52% (53 subjects) performed the dental brushing twice a day, 37% (38 subjects) perform oral hygiene several times a day, and 11% (11 subjects) do not perform oral cavity brushing (Figure 1).
Figure 1.
Subject distribution according to the oral cavity hygiene.
135 cervical lesions were detected, each patient presenting with 1.2 or multiple lesions at different stages of progression.
There was a higher presence of the abfraction lesions in the premolars 77% (104), in the molars 5% (7), and 18% (24) were combined canine, premolar, molar lesions.
16% (17 subjects) stated the presence of nocturnal bruxism, and in terms of depth, 46% (62) of the lesions were present only at the enamel level, 38% (51) of the lesions showed simultaneous enamel-dentine damage, and 16% (22) of the lesions showed signs of pulpal damage.
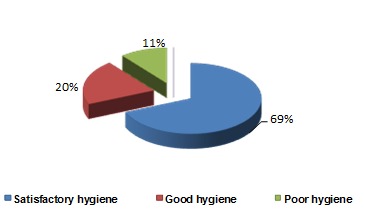
The oral hygiene was evaluated as a possible risk factor in the production of abfraction lesions and the distribution of the patients studied as follows: 69% (70 subjects) manage to remove, but not entirely the bacterial plaque using an incorrect brushing technique presenting a satisfactory hygiene, 20% (21 subjects) had an adequate brushing technique and a good hygiene, 11% (11 subjects) had poor hygiene because they did not perform oral cavity hygiene.
In the case of patients with poor hygiene, it was found the presence of untreated caries lesions, which are in various stages of progression, without experiencing pain, the presence in the treatment being imposed by the impairment of the aesthetic function.
Regarding the frequency order of dental brushing, 52% (53) of the subjects perform the dental brushing twice a day, 37% (38 subjects) several times a day and 11% (11 subjects) do not perform the daily dental brushing (Figure 2).
Figure 2.
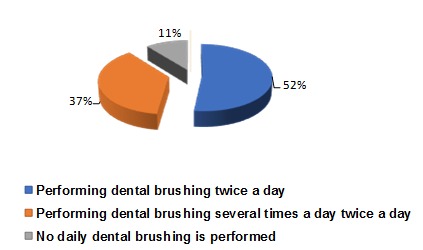
Frequency of dental brushing.
Regarding the duration of the dental brushing, 52% (47 subjects) of the ones that perform the brushing allocate 3-5 minutes for it and 48% (44 subjects) perform the dental brushing in less than 2 minutes (Figure 3).
Figure 3.
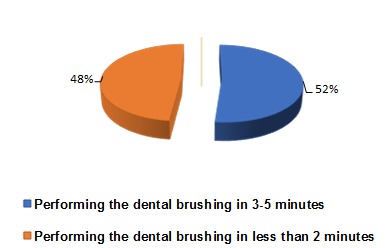
Time allocated to dental brushing.
The force acting on the teeth during brushing is high and the preference for toothbrushes with hard bristles was 78% (71 subjects) and 22% (20 subjects), prefers soft bristles toothbrushes and act gently during dental brushing (of the 91 who performed the daily brushing), noting the occurrence of cervical lesions with predominance in the males compared with the females (Figure 4).
Figure 4.
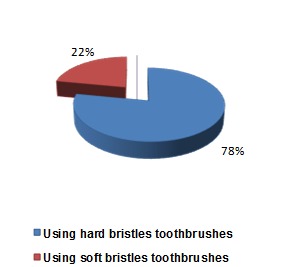
The acting forces on the teeth by means of the toothbrush.
The preference of some patients in the use of hard bristles toothbrushes associated with improper brushing techniques has resulted in cervical lesions.
The participants in this study presented abfraction lesions located on 1, 2, or more teeth, being in different stages of progression, having a total of 135 lesions.
Regarding the type of tooth affected, the study undertaken by us showed that: there was a significant damage due to the presence of abfraction lesions in large number at the level of premolars-77% (104 lesions) of the investigated cases; at the molar level such lesions were detected in a much smaller percentage-5% (7 lesions); and 18% (24) of the subjects had combined canine, premolar, and molar lesions (Figure 5).
Figure 5.
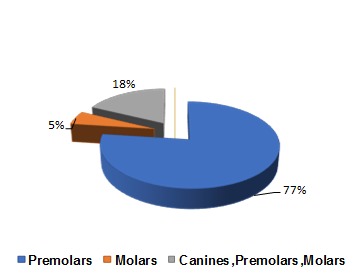
Distribution of the abfraction lesions according to the type of tooth affected.
There was no significant difference of the abfraction lesions present in the right or left quadrant.
The patient with abfraction lesions in the lower premolars, presenting complications due to the pain caused by inflammation of the dental pulp, so that the patient resorted to avoiding the oral cavity hygiene.
The analysis of the distributions of the abfraction lesions in the two sexes, revealed the greater presence in the male, 58% of the total of the abfraction lesions detected (78 lesions), compared with the female, 42% (57 lesions) (Figure 6).
Figure 6.
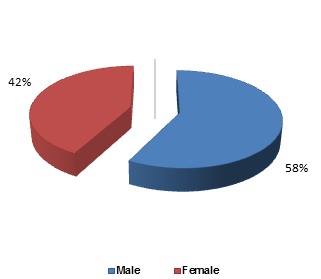
Distribution of abfraction lesions according to patients’ gender.
Referring to the distribution of abfraction lesions according to the age of the subjects in the studied group, it was found that the majority of patients with premolar lesions were between 30 and 65 years old, the percentage of molar damage was between 32 and 72 years, and regarding combined canine, premolar, molar lesions between 25 and 72 years old 2.
Table 2.
Distribution of abfraction lesions according to age and type of tooth affected.
|
Age of the subjects |
Type of affected tooth |
Number of lesions |
|
30-65 years old |
PREMOLARS |
104 |
|
32-72 years old |
MOLARS |
7 |
|
25-72 years old |
CANINES, PREMOLARS, MOLARS |
24 |
The investigation of the existence of parafunctions and the transmission of occlusal forces outside the dental axis showed that 16.66% (17 subjects) presented nocturnal bruxism and 8.82% (9 subjects) presented dental abnormalities without establishing orthodontic treatment (Figure 7).
Figure 7.
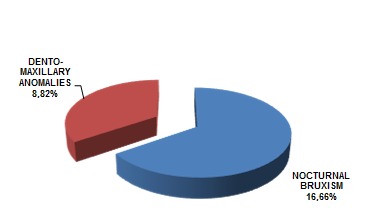
Investigation of the existence of parafunctions in patients with abfraction lesions.
The presence of abfraction lesions was found in patients with satisfactory oral hygiene, who had dento-maxillary abnormalities.
The occlusal forces generated in the patients with bruxism led to the occurrence of the abfraction lesions and the wear facets caught in different stages of evolution, accentuated by aging.
In patients who had untreated dento-maxillary abnormalities and implicitly the transmission of non-axial occlusal forces, cervical lesions were detected cervical lesions in various stages of progression unrelated to the oral cavity hygiene, the patients presenting a satisfactory hygiene.
The examination of the degree of damage of the dental structures revealed that: the percentage of the damage only at the enamel level was 46% (62 lesions); 38% (51 lesions) of the detected lesions progressed with dentine damage, and in 16% (22 lesions) there were signs of dental pulp damage, such as the hypersensitivity described in response to an osmotic, tactile, chemical stimulus (Figure 8).
Figure 8.
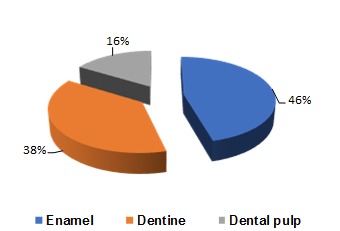
Analysis of the distribution of the abfraction lesions according to the degree of damage of the dental structures.
Frequently encountered were the cervical lesions with enamel and dentine damage without experiencing pain on the part of the patients, and only the aesthetic function was affected.
The action of the occlusal trauma caused by the parafunctions on the teeth for a long time resulted in the dental pulp being affected with the appearance of acute phenomena, such as the periodontal abscess with secondary genio-suborbital cellulitis (Figure 9).
Figure 9.

A 68-year-old female patient, affirmative nocturnal bruxism, with the presence of wear facets affecting the dental pulp.
Discussion
There are theories [7,8] that justify how stress forces occurring at the cervical level lead to the occurrence of abfraction lesions due to the poor quality of the tooth enamel at this level that does not withstand the concentrated traction forces near the cervical region.
Lee and Eakle [9] proposed as etiology for abfraction a combination of: occlusal stress, the presence of parafunctions, abrasion and erosion.
According to these authors, the location of the abfraction lesions is determined by the direction of the lateral forces acting on a tooth during mastication and parafunctions when three types of stress factors appear: compression, shearing and traction, due to the elasticity of the dentin and the reduced thickness of the HUNTER-SCHREGER band in the cervical area leading to the occurrence of abfraction lesions by a pathogenic mechanism that advances rapidly when the paraaxial occlusal forces act repeatedly.
Other studies [10] on the relation of occlusal forces, which act in bruxism, with abrasion, show that the teeth can flex in the cervical region due to occlusal stress, but they cannot cite the causes of this injury without the presence of an abrasive or erosive component.
Other authors [11] reported a direct correlation between occlusal wear facets and progression of cervical lesions.
It has also been hypothesized [12,13,14] that excessive occlusal forces are the causal factor in the occurrence of abfraction and gingival recession, but not supported by adequate evidence.
Optical coherence tomography revealed the relationship between the incidence of occlusal wear and the demineralization of the cervical region of the tooth. It has also been found that in the early stages, the demineralization of the dentine leads to lesions at the parcel level, and the occlusal stress contributes to the progression of these lesions [15].
From our study it appears that the most affected by the abfraction lesions were the premolars (77.45%), which confirms the findings of other studies [16] that speak of the lower capacity of the premolars compared with the canines, to counteract the forces acting non-axially and are prone to loss of dental tissue in the cervical region.
According to other authors [17,18] occlusal forces generated at the time of exercising oral functions and parafunctions and premature contacts lead to cervical lesions. As a result, there are authors [19,20] who assert that clinical and radiographic indicators can be used to establish the presumptive diagnosis of occlusive trauma, and it is difficult to determine whether the wear facets are caused by functional contacts or parafunctional habits, such as bruxism.
Previous studies [21] have shown that the toothbrush does not cause abfraction damage alone, but together with the toothpaste, confirmed in our study by the presence of abfraction lesions in patients with good oral hygiene who have performed dental brushing several times per day.
There are studies [22,23] that have shown that there are patients who did not perform the dental brushing, also encountered in our study, but showed lesions at the cervical level, indicating that brushing is not an element of triggering these lesions but can intensify this process.
Another clinical study [24] found that the progression of cervical lesions was associated with occlusal forces, without the contribution of dietary habits, dental hygiene, wear facets or parafunctional habits.
There are studies [25] that have associated abfraction and occlusal wear with bruxism, other authors [26] with occlusal pathology, supporting the presence of several etiological factors and suggesting that dental wear is related to the anatomy of the tooth, the distribution of forces, the development of caries lesions, occlusion and parafunctions.
Other authors [27,28] found that the abfraction lesions changed with aging, influencing the prevalence and severity of these lesions, reporting a direct correlation between the occlusal wear facets and the progression of the cervical lesions.
The study carried out by us revealed the presence of the abfraction lesions in various stages of progression in the elderly but also in the young people, who presented dento-maxillary anomalies with the transmission of the paraxial occlusal forces.
Other studies [29] related to occlusal wear have associated the dehydration of the patient with the reduction of salivary protection against dental erosion, which is of greater importance in the etiology of abfractionn than bruxism.
The associations between occlusal pathology and cervical lesions are primarily the result of dental erosion in contrast to the abfraction hypothesis, which emphasizes that harmful forces that cause wear on the occlusal surfaces and are transmitted at the cervical level do not cause abfraction damage without the presence of biocorrosion [30].
Von et al. [31] evaluated in 2004 the histological changes that occur in the periodontal structures during the use of non-axial forces, discovering the presence of areas of hyalinization and necrotic tissue, and in 2009 [32] they discovered hyalinization as an undesirable side effect in the dental orthodontics displacements.
Vier et al. [33] evaluated the effects of occlusal trauma on the dental pulp, finding that hyalinization is an irreversible response if excessive forces act for a long time.
There are authors [34] who have sought evidence to establish a causal relationship between occlusion and abfraction lesions, and other studies [35,36,37] indicate associations between non-carious lesions, bruxism and occlusal factors such as wear facets, premature contacts, but does not confirm the cause of the abfraction.
According to these studies [38,39,40], there is a correlation between bruxism and cervical lesions, but the relationship between excessive occlusal forces and the evolution of abfraction lesions is still uncertain.
There are bioengineering studies which have explored the association of occlusal stress with cervical wear, using photoelastic methods, without confirming a positive relation with abfraction lesions [41,42].
It has been argued that an occlusal trauma situated far from cervical lesions, cannot be considered as a single cause of abfractions [43].
A number of theories have been issued [44] on the etiology of these lesions, but the real causes underlying their production are still unclear, which is reflected in the specialty literature that describes acid and abrasive processes as etiological factors of these lesions, but pay special attention to occlusal stress due to forces transmitted outside the axis of the teeth.
Conclusions
The abfraction lesions in combination with other factors progress through the loss of protection of the natural tissues and evolve into the soft tissue of the tooth, the dental pulp.
Early and correct identification of the main mechanism of production of cervical lesions will allow the adoption of preventive or therapeutic measures increasing the chances of success in the management of these lesions.
The simultaneous occurrence of wear and the presence of the bacterial plaque may be an indicator in the progression of abfraction injuries.
The abfraction lesions need to be restored to prevent their further progression, exposure of the dental pulp, coronary tooth fracture and to improve the aesthetics.
Conflict of interests
None to declare.
References
- 1.Sarode GS, Sarode SC. Abfraction: A review. J Oral Maxillofacial Pathology. 2013;17(2):222–227. doi: 10.4103/0973-029X.119788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grippo JO. Abfractions: a new classification of hard tissue lesions of teeth. J Esthet Dent. 1991;3(1):14–19. doi: 10.1111/j.1708-8240.1991.tb00799.x. [DOI] [PubMed] [Google Scholar]
- 3.Grippo JO. Noncarious cervical lesions:the decision to ignore or restore. J Esthet Dent. 1992;4(1):155–164. doi: 10.1111/j.1708-8240.1992.tb00721.x. [DOI] [PubMed] [Google Scholar]
- 4. American Academy of Periodontology . Glossary of periodontal terms . Chicago : American Academy of Periodontology ; 2001 . [Google Scholar]
- 5.Nascimento M, Dilbone D, Pereira P, Duarte W, Geraldeli S, Delgado A. Abfraction lesions: etiology, diagnosis, and treatment options. J Clinical Cosmetic and Investigational Dentistry. 2016;3(8):79–87. doi: 10.2147/CCIDE.S63465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Walter C, Kress E, Gotz H, Taylor H, Willershausen I, Zampelis A. The anatomy of non-carious cervical lesions. Clin Oral Investig. 2014;8(1):139–46. doi: 10.1007/s00784-013-0960-0. [DOI] [PubMed] [Google Scholar]
- 7.McCoy G. On the longevity of teeth. J Oral Implantol. 1983;11(2):248–267. [PubMed] [Google Scholar]
- 8.Walter C, Kress E, Gotz H, Taylor H, Willershausen I, Zampelis A. The anatomy of non-carious cervical lesions. Clin Oral Investig. 2014;18(1):139–146. doi: 10.1007/s00784-013-0960-0. [DOI] [PubMed] [Google Scholar]
- 9.Lee WC, Eakle WS. Possible role of tensile stress in the etiology of cervical erosive lesions of teeth. J Prosthet Dent. 1984;52(3):374–380. doi: 10.1016/0022-3913(84)90448-7. [DOI] [PubMed] [Google Scholar]
- 10.Grippo JO, Simring M. Dental ‘’erosion’’ revisited. J Am Dent Assoc. 1995;126(5):619–630. doi: 10.14219/jada.archive.1995.0241. [DOI] [PubMed] [Google Scholar]
- 11.Grippo JO, Simring M, Schreiner S. Attrition, abrasion, corrosion and abfraction revisited: a new perspectiveon tooth surface lesions. J Am Dent Assoc. 2004;135(8):1109–1118. doi: 10.14219/jada.archive.2004.0369. [DOI] [PubMed] [Google Scholar]
- 12.Stillman PR. The management of pyorrhea. Dent Cosm. 1917;59(4):405–414. [Google Scholar]
- 13.Stillman PR. What is traumatic occlusion and how can it be diagnosed and corrected. J Am Dent Assoc. 1925;12(11):1330–1338. [Google Scholar]
- 14.Rodier P. Clinical research on the etiopathology of gingival recession. J Periodontology. 1990;9(3):227–234. [PubMed] [Google Scholar]
- 15.Wada I, Shimada Y, Ikeda M, Sadr A, Nakashima S, Tagami J, Sumi Y. Clinical assessment of non carious cervical lesion using swept-source optical coherence tomography. J Biophotonics. 2014;7(7):506–513. doi: 10.1002/jbio.201400113. [DOI] [PubMed] [Google Scholar]
- 16.Borcic J, Anic I, Urek MM, Ferreri S. The prevalence of non-carious lesions in permanent dentition. J Oral Rehabil. 2004;31(2):117–123. doi: 10.1046/j.0305-182x.2003.01223.x. [DOI] [PubMed] [Google Scholar]
- 17.Kornfeld B. Preliminary report of clinical observations of cervical erosions, a suggested analysis of the cause and the treatment for its relief. Dent Items Interest. 1982;54:905–909. [Google Scholar]
- 18.Chen KK, Miyake K, Terashita M. Cervical strains induced by occlusal loading. J Dent Res. 1999;78:474–474. [Google Scholar]
- 19.Pihlstrom BL, Anderson KA, Aepli D, Schaffer EM. Association between Signs of trauma from occlusion and periodontitis. J Periodontol. 1986;57(1):1–6. doi: 10.1902/jop.1986.57.1.1. [DOI] [PubMed] [Google Scholar]
- 20.Jin LJ, Cao CF. Clinical diagnosis of trauma from occlusion and its relation with severity of periodontitis. J Clin Periodontol. 1992;19(2):92–97. doi: 10.1111/j.1600-051x.1992.tb00446.x. [DOI] [PubMed] [Google Scholar]
- 21.Abrahamsen TC. The worn dentition-pathognomonic patterns of abrasion and erosion. Int Dent J. 2005;(4 Suppl 1):268–76. doi: 10.1111/j.1875-595x.2005.tb00064.x. [DOI] [PubMed] [Google Scholar]
- 22.Faye B, Kane AW, Sarr M, Lo C, Ritter AV, Grippo JO. Noncarious cervical lesions among a non-toothbrushing population with Hansen’s disease (leprosy) initial findings. Quintessence Int. 2006;37(8):613–619. [PubMed] [Google Scholar]
- 23.Ritter AV, Grippo JO, Coleman TA, Morgan ME. Prevalence of carious and non-carious cervical lesions in archaeological populations from North America and Europe. J Esthet Restor Dent. 2009;21(5):324–334. doi: 10.1111/j.1708-8240.2009.00285.x. [DOI] [PubMed] [Google Scholar]
- 24.Sawlani K, Lawson NC, Burgess JO, Lemons JE, Kinderknecht KE, Givan DA, Ramp L. Factors influencing the progression of noncarious cervical lesions: a 5-year prospective clinical evaluation. J Prosthet Dent. 2016;115(5):571–577. doi: 10.1016/j.prosdent.2015.10.021. [DOI] [PubMed] [Google Scholar]
- 25.Xonga FA, Sognnaes RF, Wolcott RB. Efficacy of fluoride varnishe in the prophylaxis of dental erosion. Magazyn Stomat. 1997;39(1):49–52. [Google Scholar]
- 26.Bergstrom J, Eliasson S. Cervical abrasion in relation to toothbrushing and periodontal health. J Dent Res. 1988;96(5):405–411. doi: 10.1111/j.1600-0722.1988.tb01575.x. [DOI] [PubMed] [Google Scholar]
- 27.Smith WA, Marchan S, Rafeek RN. The prevalence and severity of non-carious cervical lesions in a group of patients attending a university hospital in Trinidad. J Oral Rehabil. 2008;35(2):128–134. doi: 10.1111/j.1365-2842.2007.01763.x. [DOI] [PubMed] [Google Scholar]
- 28.Brandini DA, Trevisan CL, Panzarini SR, Pedrini D. Clinical evaluation of association between noncarious cervical lesions and occlusal forces. J Prosthet Dent. 2012;108(5):298–303. doi: 10.1016/S0022-3913(12)60180-2. [DOI] [PubMed] [Google Scholar]
- 29.Young WG, Khan F. Sites of dental erosion are saliva-dependent. J Oral Rehabil. 2002;29(1):35–43. doi: 10.1046/j.1365-2842.2002.00808.x. [DOI] [PubMed] [Google Scholar]
- 30.Bartlett DW, Shah P. Acritical review of non-carious cervical (wear) lesions and the role of abfraction, erosion, and abrasion. J Dent Res. 2006;85(4):306–312. doi: 10.1177/154405910608500405. [DOI] [PubMed] [Google Scholar]
- 31.Von Bohl M, Maltha J, Von den Hoff H, Kuijpers-Jagtman AM. Changes in the periodontal ligament after experimental tooth movement using high and low continuous forces in beagle dogs. Angle orthod. 2004;74(1):16–25. doi: 10.1043/0003-3219(2004)074<0016:CITPLA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 32.Von Bohl M. Am hyalinization during orthodontic tooth movement. J Orthod. 2009;31(1):30–36. doi: 10.1093/ejo/cjn080. [DOI] [PubMed] [Google Scholar]
- 33.Vier-Pelisser FV, Figueiredo MA, Cherubini K, Braga Filho A, Figueiredo JA. The effect of head-fractioned teletherapy on pulp tissue. Int Endod J. 2007;40:859–865. doi: 10.1111/j.1365-2591.2007.01294.x. [DOI] [PubMed] [Google Scholar]
- 34.Telles D, Pegoraro LF, Pereira JC. Incidence of noncarious cervical lesions and their relation to the presence of wear facets. J Esthet Restor Dent. 2006;18:178–183. doi: 10.1111/j.1708-8240.2006.00015.x. [DOI] [PubMed] [Google Scholar]
- 35.Horning GM, Cohen ME, Neils TA. Bucal alveolar exostoses: prevalence, characteristics and evidence for buttressing bone formation. J Periodontol. 2000;71(6):1032–1042. doi: 10.1902/jop.2000.71.6.1032. [DOI] [PubMed] [Google Scholar]
- 36.Piotrowski BT, Gillette WB, Hancock EB. Examining the prevalence and characteristics of abfractionlike cervical lesions in a population of U.S.veterans. J Am Dent Assoc. 2001;132(12):1694–1701. doi: 10.14219/jada.archive.2001.0122. [DOI] [PubMed] [Google Scholar]
- 37.Pegoraro LF, Scolaro JM, Conti PC, Telles D, Pegoraro TA. Noncarious cervical lesions in adults: prevalence and occlusal aspects. J Am Dent Assoc. 2005;136:1694–1700. doi: 10.14219/jada.archive.2005.0113. [DOI] [PubMed] [Google Scholar]
- 38.Ommerborn MA, Scheider C, Giraki M, Schafer R, Handschel J. In vivo evaluation of noncarious cervical lesions in sleep bruxism subjects. J Prosthet Dent. 2007;98:150–158. doi: 10.1016/S0022-3913(07)60048-1. [DOI] [PubMed] [Google Scholar]
- 39.Tsiggos N, Tortopidis D, Hatzikyriakos A, Menexes G. Association between self-reported bruxism activity and occurrence of dental attrition, abfraction and occlusal pits on natural teeth. J Prosthet Dent. 2008;100:41–46. doi: 10.1016/S0022-3913(08)60135-3. [DOI] [PubMed] [Google Scholar]
- 40.Fan J, Caton JG. Occlusal trauma and excessive occlusal forces: Narrative review, case definitions, and diagnostic considerations. J Clin Periodontol. 2018;40:59–66. doi: 10.1111/jcpe.12949. [DOI] [PubMed] [Google Scholar]
- 41.Rees JS, Hammadeh M, Jagger DC. Abfraction lesion formation in maxillary incisors, canines and premolars: a finite element study. Eur J Oral Sci. 2003;111(2):149–154. doi: 10.1034/j.1600-0722.2003.00018.x. [DOI] [PubMed] [Google Scholar]
- 42.Wood ID, Kassir ASA, Brunton PA. Effect of lateral excursive movements on the progression of abfraction lesions. Oper Dent. 2009;34(3):273–279. doi: 10.2341/08-100. [DOI] [PubMed] [Google Scholar]
- 43.Levrini L, Di Benedetto, Raspanti M. Dental wear: a scanning electron microscope study. Biomed Res Int. 2014;2014:340425–340425. doi: 10.1155/2014/340425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pereira AFV, Poiate IA, Poiate E Jr, Miranda WG Jr. Abfraction lesions reviewed: current concepts. RGO. 2008;56(3):321–326. [Google Scholar]


