Abstract
Background
Post-operative range of motion (ROM) loss and pain can limit quality of life, prolong functional return to activity, and may be sport/career threatening. Dry needling (DN) is intended assist in the treatment of these complaints.
Purpose
To determine if the addition of upper quarter DN to a rehabilitation protocol is more effective in improving ROM, pain, and functional outcome scores when compared to a rehabilitation protocol alone after shoulder stabilization surgery.
Study Design
Single-Blind Randomized Clinical Trial
Methods
Thirty-nine post-operative shoulder patients were randomly allocated into two groups: (1) standard of care rehabilitation (control group) (2) standard of care rehabilitation plus dry needling (experimental group). Patient's pain, ROM, and functional outcome scores were assessed at baseline (4 weeks post-operative), and at 8 weeks, 12 weeks, and 6 months post-operative.
Results
Of 39 enrolled patients, 20 were allocated to the control group and 19 to the experimental group. At six-month follow up, there was a statistically significant improvement in shoulder flexion ROM in the control group. Aside from this, there were no significant differences in outcomes between the two treatment groups. Both groups showed improvement over time. No adverse events were reported.
Conclusion
Dry needling of the shoulder girdle in addition to standard of care rehabilitation after shoulder stabilization surgery did not significantly improve shoulder ROM, pain, or functional outcome scores when compared with standard of care rehabilitation alone. Both group's improvement was largely equal over time. The significant difference in flexion at the six-month follow up may be explained by additional time spent receiving passive range of motion (PROM) in the control group. These results provide preliminary evidence that dry needling in a post-surgical population is safe and without significant risk of iatrogenic infection or other adverse events.
Level of Evidence
Therapy, Level 2.
Keywords: Dry needling, glenohumeral instability, surgical shoulder stabilization, Movement System
INTRODUCTION
Patients often have limited range of motion following a post-operative immobilization period. Di-Silvestro noted that increased stiffness and loss of range of motion may lead to slower recovery times, decreased performance, and even early degeneration of the glenohumeral joint.1 In a sports or military population, a loss of glenohumeral range of motion can threaten the individuals ability to return to sport or his/ her military occupational specialty.2-4 Loss of glenohumeral range of motion after shoulder stabilization surgery may be the result of a decreased length of glenohumeral ligaments or increased tightness of the joint capsule.1,5 It has been proposed that loss of glenohumeral range of motion may also be due to scapulothoracic neuromotor abnormalities associated with trigger points, which may contribute to pain and subsequent range of motion loss in the shoulder girdle.6 Trigger points (TP) are described in the literature as localized hyperirritable areas associated with hypersensitive palpable taut bands located in muscle tissue that may be painful on compression and/or stretch and that can give rise to a typical referred pain pattern.7-11
TPs have been described as being either active or latent.12 An active TP produces spontaneous referred pain and frequently produces clinical symptoms. A latent TP is usually asymptomatic and may cause referred pain in response to compression, stretch or overload of the affected tissues.9,13 Latent TPs are also believed to alter muscle activation patterns which can result in limited range of motion or weakness of the muscles involved.12,14,15
Dry needling (DN) is an emerging treatment amongst physical therapists and involves the insertion of a solid monofilament needle into tissue for the management of pain and neuromusculoskeletal dysfunction.16 The needle is usually placed in muscle TPs, in the proximity of nerves, or placed in connective tissue.17,18 Some position statements by State Boards of Physical Therapy have specifically defined DN as an ‘intramuscular procedure involving the isolated treatment of myofascial (muscle) TPs’.18 A more expansive view of DN includes the target areas of muscles, ligaments, tendons, subcutaneous fascia, scar tissue, peripheral nerves, bones, and neurovascular bundles.17 DN can also be performed in tissues that vary in terms of the depth of needle penetration, with some DN performed at either a superficial or deep tissue level that may or may not include TPs. There are many theories associated with the proposed effects of DN but its effectiveness can likely be credited to a variety of factors.17 While the science behind the procedure continues to evolve, its use has gained substantial popularity over the past several years based on the number of articles in print. A review of the term ‘dry needling’ in the national PubMed database, by year, yielded one reference in 2000,19 seven new references in 2009, and 51 new references in 2014. This technique has advanced from being taught in one physical therapy curriculum at Georgia State University in 2006,20 to a technique that is introduced to entry level physical therapy students in many of the Physical Therapy programs in the United States. There are many studies available showing the benefits of this intervention treating myofascial pain.7,21-23 In contrast, there is a relatively small amount of literature examining the claim of improved range of motion, and to date, only one study has been performed to evaluate the benefit of DN in a postoperative setting.24 In case reports by Mason et al, and Dembowski et al, patients receiving DN demonstrated good improvement in range of motion as well as improved functional movement patterns.8,22
The primary purpose of this study was to determine if the addition of upper quarter DN to a rehabilitation protocol is more effective in improving range of motion, functional movement, and pain when compared to a rehabilitation protocol alone after shoulder stabilization surgery. The secondary purpose was to determine if the addition of upper quarter DN to a rehabilitation protocol is more effective in improving functional outcomes when compared to a rehabilitation protocol alone after shoulder stabilization surgery. It was hypothesized that the inclusion of DN would result in an increase in range of motion, increase in functional movement, and decrease in pain at an accelerated rate when compared to rehabilitation alone.
METHODS
A parallel single-blinded, randomized clinical trial was conducted. Subjects presenting status post shoulder stabilization surgery were recruited from a direct access physical therapy clinic. Using G Power 3.1.225 a sample size of 34 was determined prior to commencement of the trial. This sample size provides 80% power to detect an effect size of 1.0 at the eight-week follow-up with an alpha level of .05. To account for a potential 10-15% of subjects lost to follow-up, 38 subjects was the goal for recruitment.26 The effect size was determined based on prior studies on DN of upper quarter musculoskeletal disorders having reported very large changes (effect sizes > 1.5) in ROM after DN.22-24,27 This study was therefore adequately powered to detect differences in ROM. The study protocol was approved by the Keller Army Community Hospital institutional review board and registered with ClinicalTrials.gov (ClinicalTrials.gov Identifier: NCT02704975). Participants were drawn from a primarily homogeneous sample consisting of military cadets and Active Duty Army personnel. All participants signed an informed consent prior to inclusion in the study. Participants rights were protected throughout the duration of the study. To be included in the study subjects had to present status post shoulder stabilization repair surgery within the preceding four-week time period. Additional study inclusion and exclusion criteria can be found in Table 1.
Table 1.
Inclusion and exclusion criteria.
| Inclusion | Exclusion |
|---|---|
| • Age 18-40 DOD* beneficiaries • Status post shoulder stabilization repair surgery |
• Self-reported pregnancy • History of blood borne pathogens/infectious disease/active infection/metal allergy • Bleeding disorders or currently taking anti-coagulant medications • Participants who are not fluent in English |
DOD = Department of Defense
A screening and intake form was completed for each subject prior to enrollment to ensure they met inclusion and exclusion criteria. Subject flow diagram is presented in Figure 1.
Figure 1.
Subject Recruitment/Retention Flow Diagram. DN = dry needling; NPR = , numeric pain rating scale; ROM = range of motion.
INTERVENTIONS
The randomization sequence was created using Excel 2010 (Microsoft, Redmond, WA, USA) by an investigator not involved with subject recruitment or data collection. Randomized blocks of six were used to establish group assignment. The group assignment was recorded on an index card. This card was folded in half such that the label with the patient's group assignment was on the inside of the fold. The folded index card was then placed inside an envelope, and the envelope was sealed. The treating physical therapist opened the envelope and proceeded with treatment according to the group assignment. Investigators taking all measurements were blinded to the intervention group of the subject.
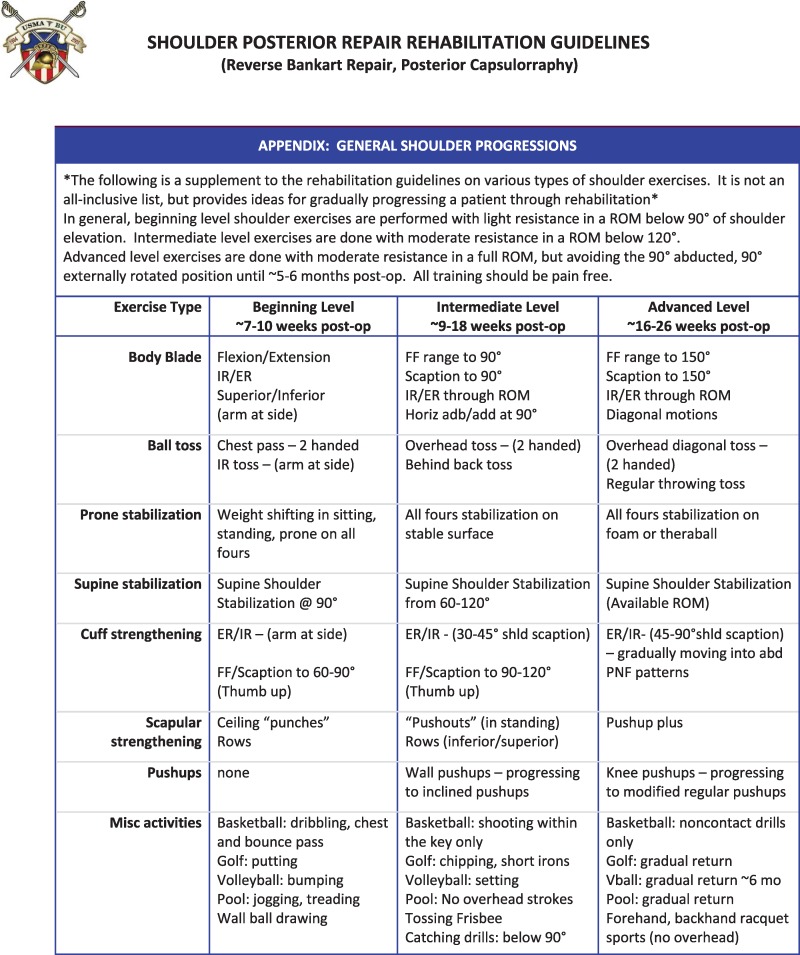
Subjects were assigned to one of two groups: a DN group or a control group. Immediately upon completion of all baseline measurements, group allocation was performed. Between post-operative weeks 4 and 8 subjects in the DN group received standard rehabilitation and weekly DN treatment for a total of four DN treatments. Treatment during this time period was chosen due to the frequent presence of trigger points in the shoulder girdle and upper trapezius during this time frame as a result of lengthy immobilization and sling wear.28 Subjects in the control group received standard rehabilitation alone. Standard rehabilitation protocols used throughout the study can be found in Appendices A and B. For subjects in the DN group, manual palpation of the shoulder girdle musculature was performed to determine the presence of TPs. A provider with greater than three years of DN experience performed DN to all detected TPs. Upon identification of a TP, a solid monofilament needle was inserted into the skin and directed towards the TP (Figure 2). Needling technique was chosen by the physical therapist according to patient tolerance and physical therapist preference. Needling techniques utilized included pistoning (inserting and withdrawing needle rapidly from each TP), needle left in situ for 10 to 15 minutes, needling with electrical stimulation, and a combination of these techniques.17 Treatment was performed until the physical therapist felt all areas of dysfunction had been addressed (i.e. reduced muscle twitch response, improvement in pain, improvement in patient tolerance, etc). To avoid performance bias, during rehabilitation, subjects in the control group received equal amounts of time with their treating therapist as the subjects in the DN group.29 To accomplish this, the therapist performed manual PROM into flexion, abduction, external rotation, and internal rotation for subjects in the control group for the same length of time that subjects in the DN group received their needling intervention. Therapists were instructed to perform this additional PROM at a “sub-therapeutic” level; that is, within current available range of the subject, without entering resistance.
Figure 2.
Dry needling directed at an intramuscular trigger point.
OUTCOMES
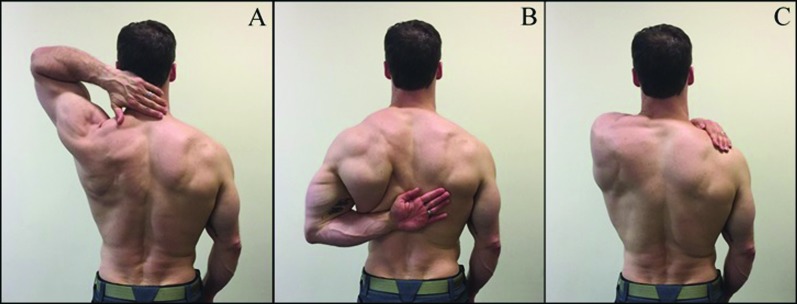
The primary outcome measures were passive range of motion of the glenohumeral joint, functional range of motion of the glenohumeral joint, and pain. Passive range of motion measures performed included shoulder flexion, glenohumeral external rotation, and internal rotation. (Figure 3) Composite shoulder flexion was performed with subject in supine. The elbow was extended, forearm relaxed, and wrist in neutral position. The subject's arm was raised into forward flexion by the practitioner. The stationary arm of the goniometer was placed parallel to the spine but at the lateral aspect of the body. The moving arm of the goniometer was placed along the midline of the humerus (Figure 3A).30-32 Glenohumeral external rotation was performed with subject in supine on the plinth. The tested arm was abducted to 90 degrees, the elbow flexed to 90 degrees, and the forearm in the mid-position between supination and pronation and perpendicular to the plinth. The subject's arm was externally rotated by the practitioner. The stationary arm of the goniometer was horizontal to the plinth with the axis on the olecranon process. The moving arm of the goniometer was in line with the styloid process of the ulna (Figure 3B).30-32 Glenohumeral internal rotation was performed with subject in supine on the plinth. The tested arm abducted to 90 degrees, the elbow flexed to 90 degrees, and the forearm in the mid-position between supination and pronation and perpendicular to the plinth. The subject's arm was internally rotated by the practitioner. The stationary arm of the goniometer was horizontal to the plinth with the axis on the olecranon process. The moving arm of the goniometer was in line with the styloid process of the ulna (Figure 3C). Goniometric measurement has been observed to be a valid and reliable measure of glenohumeral joint angle.30-32 Range of motion testing was performed twice and the average of the two trials was recorded.
Figure 3.
A: Passive range of motion testing into glenohumeral flexion B: Passive range of motion testing into glenohumeral external rotation C: Passive range of motion testing into glenohumeral internal rotation.
Functional movement measures performed included hand to neck (Figure 4A), hand to scapula (Figure 4B), and hand to opposite scapula (Figure 4C). Description of and scoring criteria for the three functional movement measures are provided in Table 233 Pain was not recorded or taken into consideration during the grading of these functional movements. The numeric pain rating scale (NPRS) was used to assess level of resting pain at each visit. This scale is scored from a 0-10, and the subject was asked to report their level of pain with the instruction that “0 is no pain, and 10 is the worst pain imaginable”. The NPRS is a valid and reliable tool in patients with shoulder pain.34,35 Secondary outcome measures included the global rating of change score (GROC), the patient specific functional scale (PSFS), and the shoulder pain and disability index (SPADI).
Figure 4.
A: Hand to neck functional movement test B: Hand to scapula functional movement test C: Hand to opposite scapula functional movement test.
Table 2.
Description and scoring criteria of three function-related tests.
| Score | Description of Scoring |
|---|---|
| Hand to neck (shoulder flexion and external rotation) * | |
| 0 1 2 3 4 |
• The fingers reach the posterior median line of the neck with the shoulder in full abduction and external rotation without wrist extension • The fingers reach the median line of the neck but do not have full abduction and/or external rotation • The fingers reach the median line of the neck, but with compensation by adduction in the horizontal plane or by shoulder elevation • The fingers touch the neck • The fingers do not reach the neck |
| Hand to scapula (shoulder extension and internal rotation)† | |
| 0 1 2 3 4 |
• The hand reaches behind the trunk to the opposite scapula or 5 cm beneath it in full internal rotation. The wrist is not laterally deviated • The hand almost reaches the opposite scapula, 6-15 cm beneath it • The hand reaches the opposite iliac crest • The hand reaches the buttock • Subject cannot move the hand behind the trunk |
| Hand to opposite scapula (shoulder horizontal adduction)‡ | |
| 0 1 2 3 |
• The hand reaches to the spine of opposite scapula in full adduction without wrist flexion • The hand reaches to the spine of the opposite scapula in full adduction • The hand passes the midline of the trunk • The hand cannot pass the midline of the trunk |
This test measures an action essential for daily activities, such as using the arm to reach, pull, or hang an object overhead or using the arm to pick up and drink a cup of water.
This test measures an action essential for daily activities, such as using the arm to pull an object out of a back pocket or tasks related to personal care.
This test measures an action important for daily activities, such as using the arm to reach across the body to get a car's seat belt or using the arm to turn a steering wheel.
The GROC is used to assess overall change from initial presentation and was recorded at each follow-up visit. This score is rated on a 15-point scale from -7 (a very great deal worse) to + 7 (a very great deal better) where subjects will select an answer that best describes their current perceived status since injury onset.36,37 The PSFS is a self-report questionnaire assessing pain, instability and activities of daily living (ADLs).34 The PSFS is a reliable and valid tool for assessing outcomes in shoulder injuries.34 The SPADI is a self-report questionnaire assessing pain and disability. The SPADI is a reliable and valid tool for assessing outcome in shoulder injuries.38,39 Repeat measurements of all variables were obtained at two additional time points post operatively, 8 weeks and 12 weeks. All measurements in both groups were repeated by the same investigator who remained blinded to group assignment.
STATISTICAL ANALYSIS
Data were analyzed with SPSS version 24 (SPSS Inc, Chicago, IL) and R version 3.3.1 (Comprehensive ‘R’ Archive Network – Kansas, USA). Means, standard deviations, and 95% confidence intervals (CIs) were calculated for each variable. Homogeneity of the data was assessed using Levene's test and all data were assessed for normal distribution using a Shapiro-Wilk test. Skewness, kurtosis, skewness ratio, and kurtosis ratio were also calculated to assess for normal distribution. Several dependent variables lacked normal distribution and homogeneity of variance.
Despite this, analysis of variance (ANOVA) was performed due to its robust nature and the lack of a non-parametric equivalent to the mixed model ANOVA. A 2x4 mixed model ANOVA was used for each outcome measure with time (baseline, follow-up 1, follow-up 2, and follow-up 3) as the within-subject factor and group (DN or control) as the between-subject factor. For the repeated measure, Mauchly's test for sphericity was performed and in the case of a significant result, a Greenhouse-Geisser correction was used. If a significant main effect for time was observed, post hoc testing (paired t-tests with Bonferroni correction) was employed.29 If a significant main effect for group or interaction effect between group and time were found, post hoc testing (unpaired t-tests with Bonferroni Holm correction) was employed. Despite a significant finding on the Shapiro-Wilk test and the lack of normal distribution for the data of flexion, external rotation, GROC, pain (NPRS), PSFS, and SPADI, parametric post hoc analysis was performed as described above. In an effort to be as thorough as possible, secondary analysis was performed using non-parametric tests, which yielded similar results. Data were also analyzed using both per protocol and intention to treat analysis methods. Again, both analysis methods yielded similar results. Results reported below are those of intention to treat analysis using parametric testing as described above.
RESULTS
Forty-three patients were screened for inclusion between March 2016 and April 2017 at which point the trial was ended due to completion of recruitment goal. Forty patients (34 male, 6 female) met the inclusion criteria and agreed to participate in the study. Additional demographic data can be found in Table 3. One patient who agreed to participate in the study was excluded prior to the initiation of treatment when it was discovered that he did not meet inclusion criteria. From baseline to follow-up two, no other patients were lost to follow-up and no adverse events were reported. Between follow-up two and three, three subjects were lost to follow-up, two of whom moved away from the area and one of whom began receiving treatment elsewhere. Subjects were randomly assigned to either the control group (n = 20) or the DN group (n = 19) and were all analyzed in the groups to which they were assigned using an intention to treat analysis. A per protocol analysis returned similar results to the intention to treat analysis. Baseline subject characteristics can be found in Table 4.
Table 3.
Demographics and Location/Type of Surgical Intervention Performed (N = 39).
| Gender | |
|---|---|
| Male | 33 |
| Female | 6 |
| Age* (years) | 20.78 ± 3.33 |
| Surgical Side | |
| Left | 25 |
| Right | 14 |
| Surgical Procedure | |
| Arthroscopic Bankart Repair (Anterior Labrum) | 26 |
| Arthroscopic Posterior Labral Repair | 4 |
| Arthroscopic Anterior and Posterior Labral Repair | 6 |
| Open Bankart Repair | 2 |
| Latarjet | 1 |
Values are mean ± standard deviation unless otherwise indicated.
Table 4.
Baseline subject characteristics assessed at 4-weeks postoperative (N = 39)*.
| Control Group, (n = 20) | Experimental Group, (n = 19) | |
|---|---|---|
| Gender (Male/Female), n | 17/3 | 16/3 |
| Age, y | 21.6 ± 4.5 | 19.9 ± 1.1 |
| Pain Intensity (0-10) | 2.55 ± 1.8 | 2.21 ± 1.8 |
| Flexion PROM | 128 ± 14.5 | 134.2 ± 15.1 |
| External Rotation PROM | 28.67 ± 21.4 | 30.0 ± 15.9 |
| Internal Rotation PROM | 36.8 ± 17.9 | 44.5 ± 12.6 |
| Functional ROM | ||
| Hand To Neck | 2.1 ± 1.2 | 2.3 ± 1.2 |
| Hand To Scapula | 2.3 ± .98 | 2.5 ± .84 |
| Hand To Opposite Scapula | 1.2 ± .76 | 1.4 ± .68 |
| GROC | 4.8 ± 1.1 | 4.5 ± 2.0 |
| PSFS | 3.5 ± 2.1 | 2.9 ± 2.2 |
| SPADI | 41.4 ± 17.0 | 42.8 ± 21.9 |
| Surgical Side (R/L), n | 8/12 | 6/13 |
| Surgical Procedure, n | ||
| Anterior Stabilization/ Bankart | 14 | 12 |
| Posterior Stabilization | 1 | 3 |
| Anterior and Posterior Stabilization | 3 | 3 |
| Open Bankart/ Latarjet | 2 | 1 |
y = years of age; PROM = Passive Range of Motion; ROM = Range of Motion; GROC = Global Rating of Change Functional Outcome Score; PSFS = Patient Specific Functional Scale; SPADI = Shoulder Pain and Disability Index Functional Outcome Measure.
Values are mean ± standard deviation unless otherwise indicated
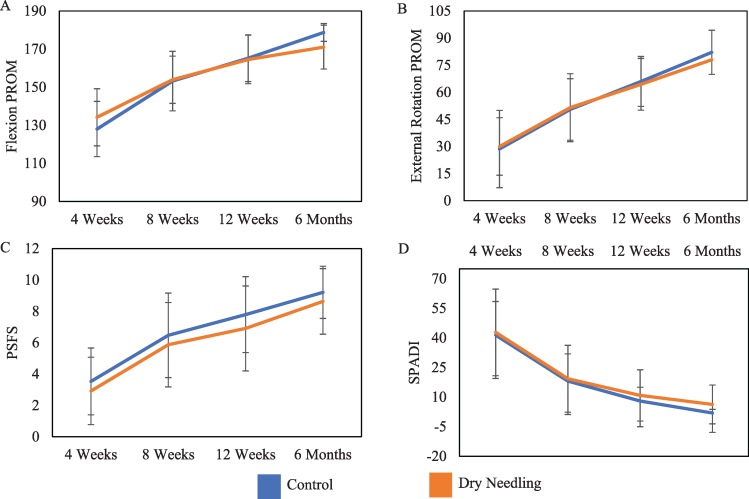
The 2x4 mixed model ANOVA revealed a significant main effect for time for all dependent variables, but that there was no significant main effect for group (p > 0.05). A significant interaction between time and group was observed in shoulder flexion only (p = 0.019). No other interaction effect between time and group was observed. Post hoc analysis using unpaired t-tests with Bonferroni correction revealed an improvement in the shoulder flexion control group at the six-month time point only. During post hoc analysis using paired t-tests with Bonferroni correction for pairwise comparisons, the significant main effect for time was observed across all time points for the dependent variables of shoulder flexion ROM, shoulder ER ROM, PSFS, and SPADI (p ≤ 0.003), however, for the dependent variables of shoulder IR ROM, hand to neck functional ROM, hand to scapula functional ROM, hand to opposite scapula functional ROM, GROC, and NPRS, the significant main effect for time was not observed across all time points.
Visual representation of the significant main effect over time but lack of interaction effect between the groups for dependent variables for flexion ROM, external rotation ROM, PSFS, and SPADI are presented in Figure 5.
Figure 5.
(A) Flexion passive range of motion change from 4 weeks (baseline) to 6 Months; (B) External rotation passive range of motion change from 4 weeks (baseline) to 6 Months; (C) Patient Specific Functional Scale change from 4 weeks (baseline) to 6 Months; (D) Shoulder pain and disability index change from 4 weeks (baseline) to 6 Months.
*Significant main effect for time across all time points; Significant interaction effect found only at 6-month Flexion ROM follow-up.
DISCUSSION
The purpose of this study was to determine if the addition of upper quarter DN to a rehabilitation protocol is more effective in improving range of motion, functional movement, and pain when compared to a rehabilitation protocol alone after shoulder stabilization surgery. This is the first research study that has investigated the addition of DN to a rehabilitation protocol following shoulder stabilization surgery. The results of the current randomized clinical trial suggest that the addition of DN of the shoulder girdle to a standard rehabilitation program does not improve range-of-motion, pain, or self-reported outcome measures more than a standard rehabilitation program alone in young, athletic individuals who have recently undergone shoulder stabilization surgery.
The only statistically significant interaction effect found between time and group occurred at the six-month follow up for the measure of flexion ROM. Although both groups improved significantly over time, contrary to the original hypothesis, the improvement in ROM observed in the control group was greater than that seen in the experimental group. The between group mean change observed in this study was 13.83 degrees of shoulder flexion range of motion with lower and upper bounds of the 95% confidence interval of 3.81 degrees and 23.86 degrees respectively. If the true mean does fall within the upper and lower bounds of the observed confidence interval, it is possible that it lies at the lower bound of 3.81 degrees and does not represent a meaningful difference.40 It is also possible that the difference between the two groups could be explained by the additional time spent on PROM between weeks four and eight. Despite the efforts made by therapists to perform “sub-therapeutic” PROM to prevent bias,29 the additional time spent on PROM in the control group may have provided long term benefit in shoulder flexion ROM.
These results differ slightly from the only other study examining the effects of DN in post-operative shoulders.24 Arias-Buria et al observed that subjects receiving DN and physical therapy experienced statistically significant and clinically meaningful changes in self-reported functional outcome scores, activities of daily living, and strength when compared to subjects receiving physical therapy alone. However, they observed no statistically significant difference between the groups in the measures of pain or ROM.24 Similarly, no statistically significant difference was observed in the measure of pain and no clinically meaningful difference between the groups in the measure of ROM.
Arias-Buria41 et al conducted a randomized clinical trial comparing DN and physical therapy and physical therapy alone in patients with subacromial impingement syndrome. The investigators observed changes in functional outcome measures (Disabilities of the Arm, Shoulder, and Hand questionnaire) but no significant results between groups for changes in pain.41 Another randomized clinical trial performed on subjects with a diagnosis of non-specific shoulder pain also failed to show a difference in pain, ROM, and functional outcome measures between a DN and physical therapy group when compared to a group who received physical therapy alone.42 Clewley et al6 demonstrated significant changes in both pain and ROM in a patient with adhesive capsulitis of the shoulder after the inclusion of DN to the individuals physical therapy program in a case report. While these results are promising, their case report does not allow inference of a causal relationship between DN and improvement in pain and ROM.6,29
These prior reports are largely consistent with the results of the current study, but it must be mentioned that both the pathology and demographics of the previously mentioned studies are far different than this one. This study was performed on a young, active, and otherwise healthy population of individuals who had recently undergone shoulder stabilization surgery while the others were performed on older individuals with differing pathology than this population. Secondarily, the three randomized trials mentioned above24,41,42 used the Hong technique for DN43 (“fast in, fast out”), and the techniques used in the current study were variable and left to provider choice. Because there is no strong consensus on the superiority of one DN technique over another,17 it is possible that a more standardized DN protocol in the current study would have yielded different results in the measured outcomes. The differences in study population and needling technique may provide a possible explanation for the lack of significant differences noted in this study while others have observed significant differences in functional outcomes and pain with the inclusion of DN in their treatment plans.6,24,41
Further examination of the change scores and confidence intervals provided in Table 5 may be useful in determining if further research is warranted or if a larger sample size would yield significant results. For the dependent variable of flexion, between weeks 4 and 8 and weeks 4 and 12, not only do the confidence intervals include the value of zero, but the values do not include the possibility of a clinically meaningful change in favor of the DN group. Between four weeks and six months, the confidence intervals do include the value of zero, but likely do not represent a clinically meaningful change as discussed above. For the dependent variable of pain, across all time points, the confidence intervals include the value of zero and also fail to meet the clinically important difference value of 2.0 for the NPRS.44,45 Therefore, although the possibility that a true difference does exist between the two groups in the current study cannot be ruled out, it is very likely that the magnitude of the true difference is, in the case of pain, less than 2.0 on the NPRS. The need to conduct subsequent studies examining the difference between DN plus rehabilitation and rehabilitation alone in young, otherwise healthy individuals who have recently undergone shoulder stabilization surgery is likely to be un-necessary. If such a study were to be performed with a larger sample size, while additional statistically significant differences may be found, it is likely that these results would not be clinically meaningful.46
Table 5.
Outcome Data By Group*.
| Group Means | Within‐Group Mean Change | Between Group Mean Difference | |||
|---|---|---|---|---|---|
| Control | DN | Control | DN | ||
| 8 Week Follow‐Up | |||||
| Flexion PROM | 153.2 ± 15.60 | 153.9 ± 12.40 | 25.2 (19.58, 30.71) | 19.7 (11.85, 27.62) | ‐5.5 (‐14.77, 3.95) |
| ER PROM | 50.5 ± 17.00 | 51.5 ± 18.80 | 21.9 (15.68, 28.11) | 21.5 (16.46, 26.59) | ‐0.40 (‐8.13, 7.38) |
| IR PROM | 55 ± 15.44 | 57.3 ± 11.36 | 18.2 (10.15, 26.14) | 12.8 (6.39. 19.33) | ‐5.40 (‐15.23, 4.67) |
| Hand to Neck | 0.8 ± .95 | 0.68 ± .67 | ‐1.30 (‐1.78, ‐0.81) | ‐1.62 (‐2.26, ‐1.00) | ‐0.32 (‐1.09, 0.43) |
| Hand to Scapula | 1.35 ± .93 | 1.16 ± .83 | ‐1.0 (‐1.34, ‐.066) | ‐1.37 (‐1.73. ‐1.00) | ‐0.37 (‐0.85, 0.11) |
| Hand to Opp. Scapula | 0.30 ± .57 | 0.42 ± .61 | ‐0.90 (‐1.23, ‐0.56) | ‐0.95 (‐1.28, ‐0.61) | ‐0.05 (‐0.51, 0.41) |
| GROC | 5.5 ± 1.53 | 5.32 ± 1.29 | 0.65(‐.021, 1.51) | 0.79 (‐0.04, 1.62) | 0.14 (‐1.01, 1.29) |
| NPRS | 1.8 ± 1.87 | 2.2 ± 1.71 | ‐0.75 (‐1.32, ‐0.13) | ‐0.01 (‐1.20, 1.14) | 0.74 (‐0.58, 1.98) |
| PSFS | 6.47 ± 2.69 | 5.87 ± 2.69 | 2.94 (2.09, 3.77) | 2.95 (2.28, 3.62) | 0.01 (‐1.03, 1.06) |
| SPADI | 18.1 ± 13.79 | 19.3 ± 16.92 | ‐23.3 (‐28.17, ‐18.34) | ‐23.5 (‐32.20, ‐14,76) | ‐0.20 ( ‐9.98, 9.53) |
| 12 Week Follow‐Up | |||||
| Flexion PROM | 165.2 ± 12.30 | 164.5 ± 12.70 | 37.2 (30.53, 43.81) | 30.3 (24.19, 36.54) | ‐6.90 (‐15.56, 1.96) |
| ER PROM | 66.0 ± 13.8 | 64.4 ± 14.30 | 37.4 (28.47, 46.22) | 34.4 (29.15, 39.74) | ‐3.00 (‐12.96, 7.16) |
| IR PROM | 63.8 ± 9.6 | 68.9 ± 10.03 | 27.0 (19.26, 34.78) | 24.4 (16.28, 32.67) | ‐2.60 (‐13.45, 8.35) |
| Hand Neck | 0.20 ± .52 | 0.32 ± .48 | ‐1.9 (‐2.42, ‐1.37) | ‐1.98 (‐2.64, ‐1.35) | ‐0.08 (‐0.90, 0.70) |
| Hand to Scapula | 0.80 ± .69 | 0.74 ± .73 | ‐1.55 (‐1.91, ‐1.19) | ‐1.79 (‐2.20, ‐1.37) | ‐0.24 (‐0.76, 0.29) |
| Hand to Opp. Scapula | 0.15 ± .37 | 0.11 ± .32 | ‐1.05 (‐1.37, ‐0.73) | ‐1.26 (‐1.58, ‐0.95) | ‐0.21 (‐0.65, 0.22) |
| GROC | 5.95 ± 1.09 | 5.58 ± 2.14 | 1.1 (0.46, 1.74) | 1.05 (‐0.37, 2.47) | ‐0.05 (‐1.58, 1.48) |
| NPRS | 1.45 ± 2.04 | 1.07 ± 1.54 | ‐1.1 (‐1.85, ‐0.35) | ‐1.14 (‐1.76, ‐0.51) | ‐0.04 (‐0.98, 0.92) |
| PSFS | 7.79 ± 2.42 | 6.91 ± 2.71 | 4.26 (3.42, 5.09) | 3.99 (3.09, 4.89) | ‐0.27 (‐1.45, 0.93) |
| SPADI | 8.0 ± 7.01 | 10.87 ± 13.00 | ‐33.4 (‐39.69, ‐27.01) | ‐31.9 (‐40.47, ‐23.42) | 1.47 (‐8.87, 11.70) |
| 6 Month Follow‐Up | |||||
| Flexion PROM | 178.7 ± 4.66 | 171.02 ± 11.49 | 50.7 (43.62, 57.68) | 36.8 (29.19, 44.44) | ‐13.83 (‐23.86, ‐3.81) |
| ER PROM | 82.13 ± 12.21 | 77.97 ± 16.32 | 53.45 (43.17, 63.74) | 47.97 (39.38, 56.57) | ‐5.47 (‐18.44, 7.49) |
| IR PROM | 66.13 ± 12.64 | 71.92 ± 10.29 | 29.33 (21.44, 37.21) | 27.45 (19.45. 35.44) | ‐1.87 (‐12.73, 8.97) |
| Hand to Neck | 0.0 ± 0.0 | 0.16 ± 0.37 | ‐2.10 (‐2.67, ‐1.53) | ‐2.16 (‐2.74, ‐1.57) | ‐0.06(‐0.85, 0.73) |
| Hand to Scapula | 0.45 ± .51 | 0.63 ± 0.59 | ‐1.9 (‐2.3, ‐1.5) | ‐1.89 (‐2.32. ‐1.47) | ‐0.01 (‐0.56, 0.57) |
| Hand to Opp. Scapula | 0.0 ± 0.0 | 0.10 ± 0.32 | ‐1.2 (‐1.56, ‐0.84) | ‐1.26 (‐1.58, ‐0.95) | ‐0.06 (‐0.53, 0.40) |
| GROC | 6.6 ± 0.60 | 5.48 ± 2.72 | 1.75(1.23, 2.27) | 0.95 (‐0.63, 2.53) | ‐0.80 (‐2.44, 0.84) |
| NPRS | 0.90 ± 1.65 | 1.52 ± 2.17 | ‐1.65 (‐2.55, ‐0.75) | ‐0.68 (‐1.66, 0.29) | 0.97 (‐0.32, 2.24) |
| PSFS | 9.21 ± 1.66 | 8.63 ± 2.09 | 5.67 (4.69, 6.65) | 5.69 (4.63, 6.76) | 0.02 (‐1.38, 1.42) |
| SPADI | 1.96 ± 1.83 | 6.29 ± 9.83 | ‐39.43 (‐47.29, ‐31.5) | ‐36.53 (‐46.98, ‐26.07) | 2.91 ( ‐9.76, 15.57) |
DN = Dry Needling; SD = standard deviation; Within Group Mean Change = Change from baseline to follow‐up; PROM = Passive range of motion; Hand to Neck = Hand to neck functional range of motion; Hand to Scapula = Hand to scapula functional range of motion; Hand to Opp. Scapula = Hand to opposite scapula functional range of motion; GROC = Global rating of change functional outcome score; NPRS = Numeric pain rating scale; PSFS = Patient specific functional scale; SPADI = Shoulder pain and disability index functional outcome measure.
*Outcome values at each time point are mean ± SD (95% confidence interval) and values for change scores are mean (95% confidence interval) and values for change scores are mean (95% confidence interval). Values reported represent intention to treat analysis.
The main strength of this study is that it was the first study attempting to determine if the addition of upper quarter DN to a rehabilitation protocol is more effective in improving range of motion, pain, and functional movement when compared to a rehabilitation protocol alone after shoulder stabilization surgery. Also, while the power analysis indicated we needed only to recruit 34 individuals to have enough power to detect a change, an additional 15% were recruited with the recruitment of 39 subjects, of whom only three were lost to long term follow-up and none of whom were lost to short and intermediate term follow-up.
There are several limitations to this study. The most meaningful weakness may simply be the differences in manual therapy (PROM) intervention received between the groups. It could be argued that the additional PROM received by the control group may have improved long term outcomes in shoulder flexion PROM. This group may therefore have acted as a “manual therapy” group rather than a true control. Another limitation is the nature of single blinded randomized clinical trials. While the assessor remained blinded throughout the study period, the individuals receiving treatment were not blinded to the group they were in. This may have resulted in a compensatory increase in the performance of the members of the control group, thus biasing the results of the study.29,47 Also, the follow-up period may be considered relatively short; longer follow-up periods may be necessary to determine the possibility that long term differences could exist between these two groups. Perhaps most importantly, the inclusion criteria in this study were very specific and our resultant sample population represented a very specific subset of the population. For this reason, these results cannot be generalized outside of the population included in this study. Finally, it has been proposed that a specific subset of individuals who would respond best to DN does exist, but that the population in the current study may not fit those parameters.48 For this reason, future research is needed to elucidate the subset of individuals who would respond most favorably to this intervention.
While not mentioned directly in the purpose of the study, it should be noted that throughout the course of treatment of our DN group (76 DN treatments in total), no adverse events were reported. The possibility that DN may increase the likelihood of iatrogenic infection after surgery has been raised in the literature and the validity of this argument has not been fully refuted.49,50 The current study provides preliminary evidence that the inclusion of DN into a post-operative rehabilitation program as early as four weeks after surgery carries with it little to no risk of iatrogenic infection in the post-surgical population.
CONCLUSION
The results of this investigation indicate that DN of the shoulder girdle in addition to standard of care rehabilitation after shoulder stabilization surgery did not significantly improve shoulder range of motion, functional range of motion, pain, or functional outcome scores when compared with standard of care rehabilitation alone. These results do not support the addition of DN into the standard post-operative treatment regime in individuals who have recently undergone shoulder stabilization surgery.
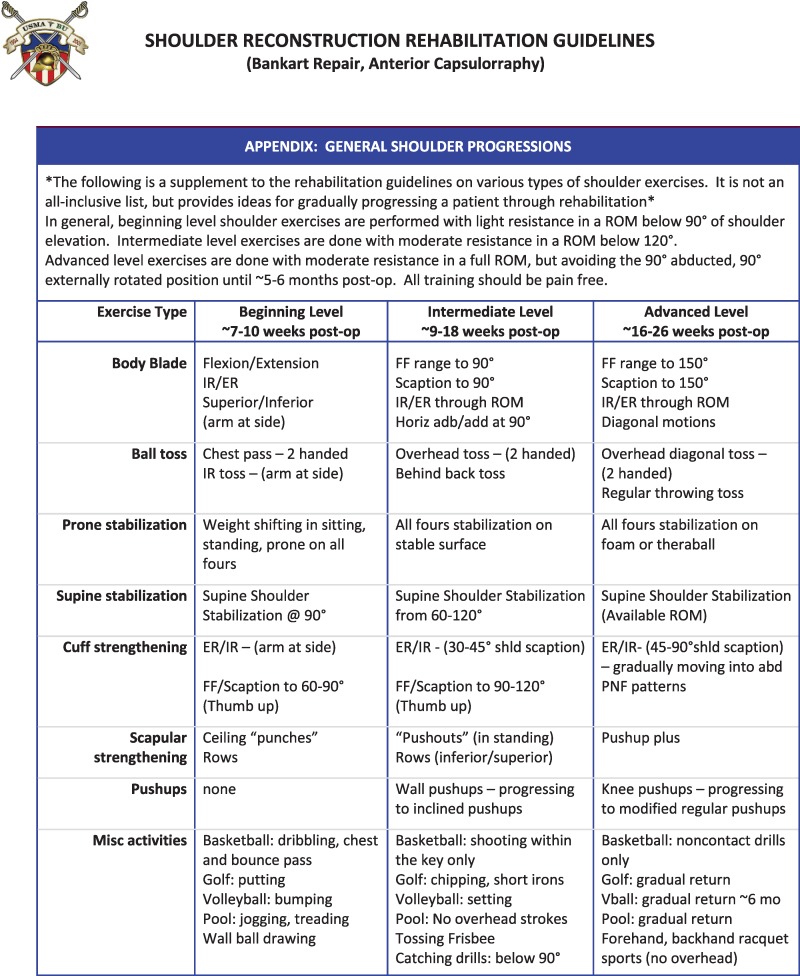
APPENDIX A
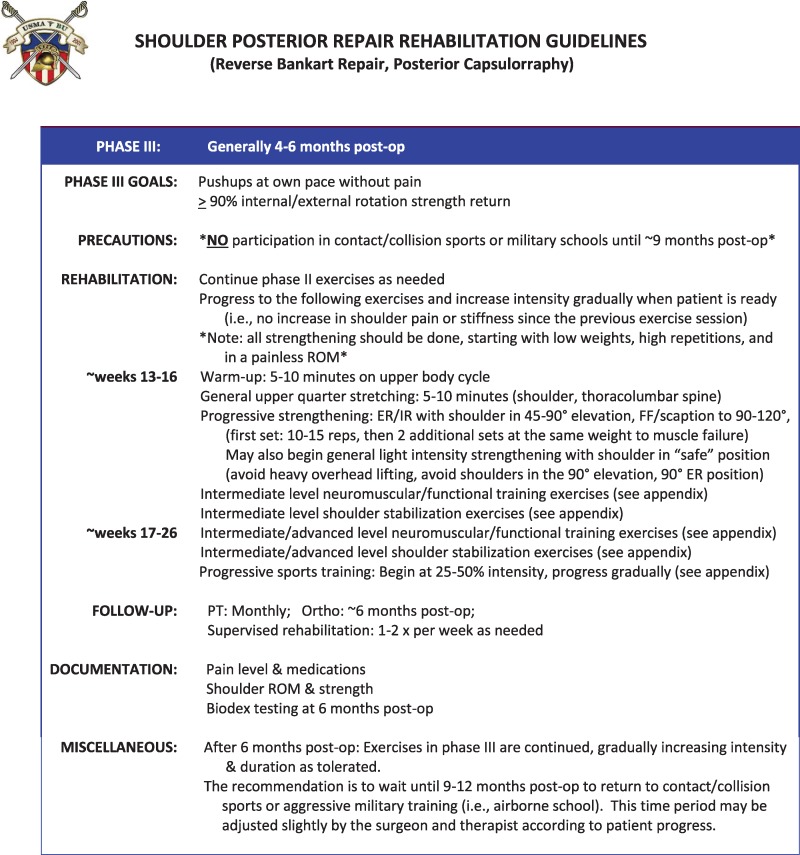
APPENDIX B
REFERENCES
- 1.Di Silvestro MD Lo IK Mohtadi N Pletsch K Boorman RS. Patients undergoing stabilization surgery for recurrent, traumatic anterior shoulder instability commonly have restricted passive external rotation. J Should Elbow Surg. 2007;16(3):255-259. [DOI] [PubMed] [Google Scholar]
- 2.Army U. Field manual 7-22: army physical readiness training. Washington, DC2012 2018.
- 3.Garcia GH Wu H-H Liu JN Huffman GR Kelly IV JD. Outcomes of the remplissage procedure and its effects on return to sports: average 5-year follow-up. Am J Sports Med. 2016;44(5):1124-1130. [DOI] [PubMed] [Google Scholar]
- 4.Abdul-Rassoul H Galvin JW Curry EJ Simon J Li X. Return to sport after surgical treatment for anterior shoulder instability: a systematic review. Am J Sports Med. 2018:0363546518780934. [DOI] [PubMed] [Google Scholar]
- 5.Branch TP Avilla O London L Hutton WC. Correlation of medial/lateral rotation of the humerus with glenohumeral translation. Br J Sports Med. 1999;33(5):347-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clewley D Flynn TW Koppenhaver S. Trigger point dry needling as an adjunct treatment for a patient with adhesive capsulitis of the shoulder. J Orthop Sports Phys Ther. 2014;44(2):92-101. [DOI] [PubMed] [Google Scholar]
- 7.Tekin L Akarsu S Durmus O Cakar E Dincer U Kiralp MZ. The effect of dry needling in the treatment of myofascial pain syndrome: a randomized double-blinded placebo-controlled trial. Clin Rheumatol. 2013;32(3):309-315. [DOI] [PubMed] [Google Scholar]
- 8.Dembowski SC Westrick RB Zylstra E Johnson MR. Treatment of hamstring strain in a collegiate pole-vaulter integrating dry needling with an eccentric training program: a resident's case report. Int J Sports Phys Ther. 2013;8(3):328-339. [PMC free article] [PubMed] [Google Scholar]
- 9.Simons DG Travell JG Simons LS. Travell & Simons’ myofascial pain and dysfunction: upper half of body. Vol 1: Lippincott Williams & Wilkins; 1999.
- 10.Srbely JZ Dickey JP Lee D Lowerison M. Dry needle stimulation of myofascial trigger points evokes segmental anti-nociceptive effects. J Rehabil Med. 2010;42(5):463-468. [DOI] [PubMed] [Google Scholar]
- 11.Westrick RB Zylstra E Issa T Miller JM Gerber JP. Evaluation and treatment of musculoskeletal chest wall pain in a military athlete. Int J Sports Phys Ther. 2012;7(3):323-332. [PMC free article] [PubMed] [Google Scholar]
- 12.Bennett R. Myofascial pain syndromes and their evaluation. Best Pract Res Clin Rheumatol. 2007;21(3):427-445. [DOI] [PubMed] [Google Scholar]
- 13.Fernández-de-las-Peñas C Alonso-Blanco C Fernández-Carnero J Miangolarra-Page JC. The immediate effect of ischemic compression technique and transverse friction massage on tenderness of active and latent myofascial trigger points: a pilot study. J Bodyw Mov Ther. 2006;10(1):3-9. [Google Scholar]
- 14.Dommerholt J. Persistent myalgia following whiplash. Curr Pain Headache Rep. 2005;9(5):326-330. [DOI] [PubMed] [Google Scholar]
- 15.Lucas KR Polus BI Rich PA. Latent myofascial trigger points: their effects on muscle activation and movement efficiency. J Bodyw Mov Ther. 2004;8(3):160-166. [Google Scholar]
- 16.Halle JS Halle RJ. Pertinent Dry Needling Considerations for Minimizing Adverse effects - Part One. Int J Sports Phys Ther. 2016;11(4):651. [PMC free article] [PubMed] [Google Scholar]
- 17.Dunning J Butts R Mourad F Young I Flannagan S Perreault T. Dry needling: a literature review with implications for clinical practice guidelines. Phys Ther Rev. 2014;19(4):252-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Therapists AP. the Performance of Dry Needling. Alexandria, VA: American Physical Therapy Association 2012.
- 19.Ingber RS. Shoulder impingement in tennis/racquetball players treated with subscapularis myofascial treatments. Arch Phys Med Rehabil. 2000;81(5):679-682. [DOI] [PubMed] [Google Scholar]
- 20.Dommerholt J Mayoral del Moral O Gröbli C. Trigger point dry needling. J Man Manip Ther. 2006;14(4):70E-87E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rainey CE. The use of trigger point dry needling and intramuscular electrical stimulation for a subject with chronic low back pain: a case report. Int J Sports Phys Ther. 2013;8(2). [PMC free article] [PubMed] [Google Scholar]
- 22.Mason JS Tansey KA Westrick RB. Treatment of subacute posterior knee pain in an adolescent ballet dancer utilizing trigger point dry needling: a case report. Int J Sports Phys Ther. 2014;9(1):116-124. [PMC free article] [PubMed] [Google Scholar]
- 23.Mejuto-Vazquez MJ Salom-Moreno J Ortega-Santiago R Truyols-Dominguez S, Fernandez-de-Las-Penas C. Short-term changes in neck pain, widespread pressure pain sensitivity, and cervical range of motion after the application of trigger point dry needling in patients with acute mechanical neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2014;44(4):252-260. [DOI] [PubMed] [Google Scholar]
- 24.Arias-Buria JL Valero-Alcaide R Cleland JA, et al. Inclusion of trigger point dry needling in a multimodal physical therapy program for postoperative shoulder pain: a randomized clinical trial. J Manipulative Physiol Ther. 2015;38(3):179-187. [DOI] [PubMed] [Google Scholar]
- 25.Faul F Erdfelder E Lang AG Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175-191. [DOI] [PubMed] [Google Scholar]
- 26.Kolber MJ Vega Jr F Widmayer K Cheng M-SS. The reliability and minimal detectable change of shoulder mobility measurements using a digital inclinometer. Physiother Theory Pract. 2011;27(2):176-184. [DOI] [PubMed] [Google Scholar]
- 27.Hsieh YL Kao MJ Kuan TS Chen SM Chen JT Hong CZ. Dry needling to a key myofascial trigger point may reduce the irritability of satellite MTrPs. Am J Phys Med Rehabil. 2007;86(5):397-403. [DOI] [PubMed] [Google Scholar]
- 28.Bruzga B Speer K. Challenges of rehabilitation after shoulder surgery. Clin Sports Med. 1999;18(4):769-793. [DOI] [PubMed] [Google Scholar]
- 29.Portney LG Watkins MP. Foundations of clinical research: applications to practice. Vol 2: Prentice Hall; Upper Saddle River, NJ; 2000. [Google Scholar]
- 30.Riddle DL Rothstein JM Lamb RL. Goniometric reliability in a clinical setting. Shoulder measurements. Phys Ther. 1987;67(5):668-673. [DOI] [PubMed] [Google Scholar]
- 31.Gajdosik RL Bohannon RW. Clinical measurement of range of motion. Review of goniometry emphasizing reliability and validity. Phys Ther. 1987;67(12):1867-1872. [DOI] [PubMed] [Google Scholar]
- 32.Hayes K Walton JR Szomor ZR Murrell GA. Reliability of five methods for assessing shoulder range of motion. Aust J Physiother. 2001;47(4):289-294. [DOI] [PubMed] [Google Scholar]
- 33.Yang JL Lin JJ. Reliability of function-related tests in patients with shoulder pathologies. J Orthop Sports Phys Ther. 2006;36(8):572-576. [DOI] [PubMed] [Google Scholar]
- 34.Abbott JH Schmitt J. Minimum important differences for the patient-specific functional scale, 4 region-specific outcome measures, and the numeric pain rating scale. J Orthop Sports Phys Ther. 2014;44(8):560-564. [DOI] [PubMed] [Google Scholar]
- 35.Williamson A Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14(7):798-804. [DOI] [PubMed] [Google Scholar]
- 36.Schmitt J Di Fabio RP. The validity of prospective and retrospective global change criterion measures. Arch Phys Med Rehabil. 2005;86(12):2270-2276. [DOI] [PubMed] [Google Scholar]
- 37.Jaeschke R Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10(4):407-415. [DOI] [PubMed] [Google Scholar]
- 38.MacDermid JC Solomon P Prkachin K. The Shoulder Pain and Disability Index demonstrates factor, construct and longitudinal validity. BMC Musculoskelet Disord. 2006;7:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schmitt JS Di Fabio RP. Reliable change and minimum important difference (MID) proportions facilitated group responsiveness comparisons using individual threshold criteria. J Clin Epidemiol. 2004;57(10):1008-1018. [DOI] [PubMed] [Google Scholar]
- 40.Mullaney MJ McHugh MP Johnson CP Tyler TF. Reliability of shoulder range of motion comparing a goniometer to a digital level. Physiother Theor Pract. 2010;26(5):327-333. [DOI] [PubMed] [Google Scholar]
- 41.Arias-Buria JL Fernandez-de-Las-Penas C Palacios-Cena M Koppenhaver SL Salom-Moreno J. Exercises and Dry Needling for Subacromial Pain Syndrome: A Randomized Parallel-Group Trial. J Pain. 2017;18(1):11-18. [DOI] [PubMed] [Google Scholar]
- 42.Perez-Palomares S Olivan-Blazquez B Perez-Palomares A, et al. Contribution of Dry Needling to Individualized Physical Therapy Treatment of Shoulder Pain: A Randomized Clinical Trial. J Orthop Sports Phys Ther. 2017;47(1):11-20. [DOI] [PubMed] [Google Scholar]
- 43.Hong CZ. Lidocaine injection versus dry needling to myofascial trigger point. The importance of the local twitch response. Am J Phys Med Rehabil. 1994;73(4):256-263. [DOI] [PubMed] [Google Scholar]
- 44.Farrar JT Young JP Jr. LaMoreaux L Werth JL Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149-158. [DOI] [PubMed] [Google Scholar]
- 45.Hawker GA Mian S Kendzerska T French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res). 2011;63 Suppl 11(S11):S240-252. [DOI] [PubMed] [Google Scholar]
- 46.Stratford PW. The added value of confidence intervals. Phys Ther. 2010;90(3):333-335. [DOI] [PubMed] [Google Scholar]
- 47.Conrad KM Conrad KJ. Compensatory rivalry. Encyclopedia of Statistics in Behavioral Science. 2005. [Google Scholar]
- 48.Mason JS Crowell MS Dolbeer JA, et al. The Effectiveness of Dry Needling and Stretching on Hamstring Flexibility: A Randomized Controlled Trial.: 3155 Board# 220 June 3, 3: 30 PM-5: 00 PM. Med Sci Sports Exerc. 2016;48(5 Suppl 1):898. [PMC free article] [PubMed] [Google Scholar]
- 49.Steentjes K de Vries L Ridwan B Wijgman A. Infection of a hip prosthesis after dry needling. Nederlands tijdschrift voor geneeskunde. 2014;160:A9364-A9364. [PubMed] [Google Scholar]
- 50.Halle JS Halle RJ. Pertinent Dry Needling Considerations for Minimizing Adverse effects - Part Two. Int J Sports Phys Ther. 2016;11(5):810. [PMC free article] [PubMed] [Google Scholar]